Abstract
We report the case of a patient in Massachusetts with early-stage Alzheimer’s disease who was treated with low doses of ionizing radiation to the brain. He requested this treatment after reading about a patient with severe Alzheimer’s in Michigan who improved remarkably after receiving 4 CT scans. After his first treatment in April 2016, mental clarity improved. His impaired conversation, reading, and sense of humor were restored, especially his virtuosic clarinet jazz-playing. However, executive function remained deficient. He requested a treatment every 2 weeks, but his neurologist denied this, fearing opposition to this treatment, a diagnostic procedure that used ionizing radiation. Limited recovery was observed after each CT scan, lasting from several weeks to months, depending on the endpoints/behavior and the periodicity. Despite the positive responses, the physician was reluctant to continue beyond 6 due to concerns about adverse effects and disapproval for prescribing them. The patient began hyperbaric oxygen therapy as an alternative. But after 43 treatments, no conclusive benefit was observed. The patient died in September 2020 at age 77. This experience suggests CT scans may have value in treating Alzheimer’s patients and restoring, at least temporarily, important aspects of normal life activities. Such observations need testing and validation.
Keywords: alzheimer’s disease, low dose ionizing radiation, CT scan treatments, adaptive protection systems, oxidative DNA damage, reactive oxygen species
Introduction
Alzheimer’s disease (AD) is a neurodegenerative disorder of uncertain cause and pathogenesis that primarily affects older adults. It accounts for more than 50% of the cases of dementia and is one of the leading sources of morbidity and mortality in the aging population. The most essential and often earliest clinical manifestation of AD is selective memory impairment, although there are exceptions. While treatments are available that can ameliorate some symptoms of the illness, there is no cure, and the disease inevitably progresses in all patients. The survival after diagnosis ranges from 3 to 20 years, with an average life expectancy of 8 to 10 years. Patients with advanced AD often are admitted to hospice for palliative care as their end-of-life approaches. 1
The first approval by the US Food and Drug Administration of a therapy that is potentially disease-modifying provides a mandate for a specific diagnosis of AD in patients with cognitive impairment and dementia. The hallmark neuropathologic changes of AD are diffuse and neuritic plaques, marked by extracellular amyloid beta deposition and neurofibrillary tangles. The study of AD is being transformed by the availability of new biomarker technologies to measure such changes in vivo. Large clinical trials are evaluating anti-amyloid and other disease-based therapies for AD utilizing these imaging or cerebrospinal fluid biomarkers (Clinical Trials.gov). However, autopsy data suggest that symptomatic AD does not occur in every patient with amyloid deposition and neurofibrillary tangles in the brain. 1
Numerous publications have shown that low-dose radiation has been historically successful in the treatment of many diseases and other conditions with an inflammatory foundation.2-5 Since it had been established that low-dose radiation could reliably mitigate inflammation and facilitate healing by the polarization of macrophages from the M1 phenotype to the anti-inflammatory M2 phenotype in a wide range of tissues, this has been suggested as the underlying mechanism for these reported historical successes.2,6 There is also a substantial animal model literature that supports these clinical observations.7,8 In light of this literature, the suggestion was raised that low dose radiation may have a therapeutic effect in conditions such as AD, which have an important inflammatory component. 9
In 2015, a woman in hospice with severe AD was treated with low doses of ionizing radiation (LDIR). 10 Her husband had read about non-targeted LDIR for diseases of the aged. After speaking with the lead author (JMC), he requested LDIR to the trunk of her body. Her physician indicated he could prescribe only an accepted procedure, so they agreed on a standard CT scan of her brain. The patient moved; the scan was repeated, and the total dose was 80 mGy. The next day, her caregiver reported remarkable changes in her cognition and behavior. She began to rise from her wheelchair, say a few words, and feed herself. She remembered experiences with friends who visited her at the hospice. 10
The lead author was delighted and advised repeating the scan twice each week to prolong the stimulation. The physician prescribed the second, 2 weeks after the first, and the third, 2 weeks later. Her progress was encouraging; however, a major setback to her former condition, after the fourth scan, was a shocking surprise. But she gradually recovered and was soon transferred to a home for seniors with a stimulating day program. A case report was submitted to a journal and published in April 2016. 3 Ongoing booster treatments and information updates on her improved quality of life continued until she died on May 18, 2018.11,12
Based on the findings of this case report, a pilot study (2017–2020) was undertaken, treating patients with severe AD by employing low doses of ionizing radiation (80 and 40 mGy) to the brain. 13 Minor improvements on quantitative measures were noted in 3 of the 4 patients, following treatment. However, the qualitative observations of cognition and behavior suggested remarkable improvements within days post-treatment, including greater overall alertness. One patient showed no change. The hypothesis of the present study is that oxidative stress is a major factor in the development of AD and that stimulation of the patient’s adaptive protection systems, by low doses of radiation, reverses or delays progression of AD. The doses were the same as those administered to the 2015 case previously described herein.10,13 The study mentions proposals by others to use 2 Gy doses of radiation, based on a different hypothesis―a history of success in treating systemic amyloidosis and chronic inflammatory disease, and studies on a transgenic murine model.13,14
Report about a Case of Early-Stage Alzheimer’s in Massachusetts
This case report is about a 73-year-old patient with early-stage Alzheimer’s disease, who received normal CT scans of the brain in 2016 and 2017. The patient requested one treatment to be provided every 2 weeks, as was done for the patient in Michigan. His neurologist prescribed one scan, saw immediate improvements in her patient’s condition, but would not repeat them every 2 weeks because she feared opposition from the medical community to the use of a diagnostic procedure that employed ionizing radiation for treatment. The interval between each scan was months—too long for the build up of a long-lasting increase in the activity of the patient’s adaptive protection systems.
This case began in early 2016, after a journal editor read the article about the Alzheimer’s case in Michigan. The editor immediately informed a nearby couple about this treatment that seemed promising. The husband, at 73 years of age with early-stage Alzheimer’s disease, was deteriorating rapidly. The lead author, who had been working in Boston, responded to the couple’s invitation. He visited them on January 23 and described the couple in Michigan, the X-ray treatments, and the remarkable improvements observed. He pointed out that many thousands of patients with various kinds of cancer and other diseases had been treated with low radiation doses, for more than a century, and experienced little or no pain, nor symptomatic side effects. The couple decided to request these treatments for his mild cognitive impairment, which had been diagnosed in January 2015. The patient had been diagnosed with hearing loss in 2007.
CT Scan Treatment on April 7, 2016
For baseline evaluation, a battery of neuropsychological tests was carried out on February 26. The patient was diagnosed to be at stage 3 of Alzheimer’s disease. His MMSE 15 score was 22/30. 1
On March 31, the neurologist prescribed a CT scan that was delivered on Thursday, April 7. The dose was 46 mGy. The patient reported improved mental clarity on the following morning. Based on detailed daily diaries, his wife observed that he was like his old normal self; his conversational abilities had recovered; his reading aloud was much better, and his sense of humor had returned. However, his problem-solving ability on non-routine tasks continued to be challenging, requiring her intervention.
On Friday (April 8), the patient gave his wife and daughters a typical nature update on the neighborhood—something he had not done in a long time. The weekend was similarly positive, including a report from a friend, who was amazed by her conversation with him, after church on Sunday.
On Friday, his piano-playing jazz partner commented on the patient’s much stronger clarinet performance overall, especially his reading the score and conversing about the music. Much of what they did was improvisation, and that had always remained strong. Since he knew the patient very well, his jazz partner was asked to document his new observations. He wrote:
“S….… played melodies more cleanly and completely than he has over the past couple of months. Our usual structure is for him to play the melody through, then I play it through (or partly through), then we improvise. I’ve noticed over the past several weeks that he wasn’t able to get all the way through the melody and would break into improvisation after a few bars. On Friday (4/8) he played the melodies more clearly than he’s done in a couple of months. He didn’t always make it all the way through a tune, but I was really struck by the difference. He has been having trouble reading music. A couple of times in past weeks he said that we should learn a particular tune, and I asked him to play it for me. He wasn’t able to play smoothly from the music (which he’s always been so good at), and we just went on to a tune we knew. A few times, when we resurrected a tune, we hadn’t played in a long time, he struggled with reading. I suggested we play “Avalon” on Friday, a tune we haven’t played in who knows how long, and he read quite a bit better than he has been able to in the past few months. Our conversation was more fluid than it has been for awhile. He told stories and seemed to remember all the details of the stories he was telling. I really noted the difference here too. Finally, he said himself that he felt “clearer” than he had in some time, and he seemed more cheerful and upbeat.”
Importance of Short Intervals Between Treatments
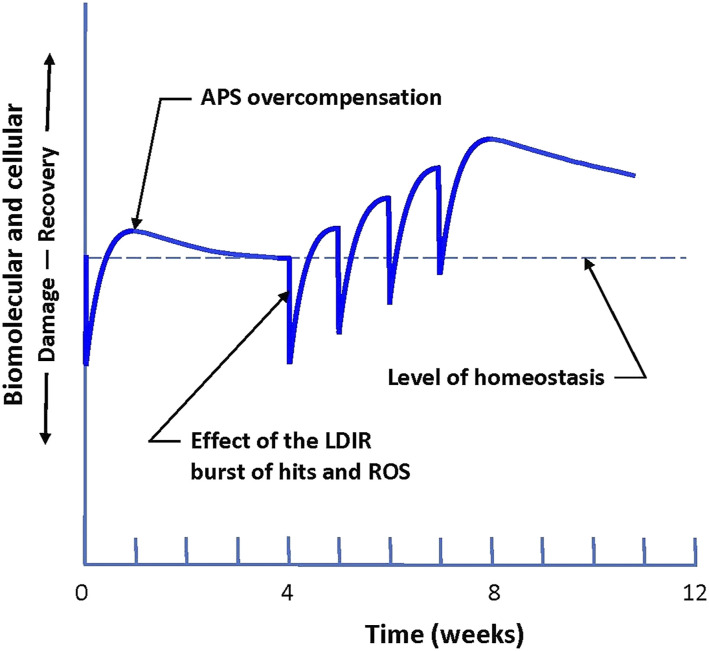
The lead author of this article informed the couple that a radiation scan may be expected to stimulate the adaptive protection systems for a limited but uncertain period of time. However, additional treatments are hypothesized to enhance the likelihood of a longer lasting boost of protective system activity, as shown in Figure 1. 13 It was important to repeat the experience in Michigan as closely as possible. That patient received one treatment every 2 weeks, initially.
Figure 1.
Patient response to a burst of biomolecular damage caused by one CT scan. 13 Repeated treatments of a low dose of ionizing radiation (LDIR) induce a hypothetical long-lasting increase in activity of the adaptive protection systems (APS). They adapt to the bursts of direct hits and reactive oxygen species (ROS). Higher protection system activity lowers the buildup of endogenous oxidative damage, which causes Alzheimer’s disease. Increased APS performance is expected to last for months. 13
Further Treatments and Disease Progression in 2016
On April 28, 3 weeks after the April 7th treatment, the neurologist administered the Folstein MMSE. The score was 24/30, up from 22/30 on February 26. The couple reported that cognition and behavior were much improved. The patient informed his neurologist that he did not want to lose ground in the summer. However, she booked the second CT scan for June 6, more than 8 weeks after the first one. Then she went on maternity leave from May until mid-September. The couple moved to their summer home in Maine. The couple noticed a plateauing of the positive effects of the April 7th treatment. However, the patient lost ground in one of the gains―executive function―planning and implementing, in which a recovery had been so important. The improvements in fluent conversation and reading aloud went downhill but were still better than before the first CT scan. During the 3–4 weeks after the April scan, he physically saw with glasses and heard with his hearing aids, but his mind was not processing what was seen and heard, as well as before. His music partner still found his playing stronger, and, at times, he had the improved clarity back.
The impact of the CT scan with its striking improvements and then the uncertainty of how long they would last were difficult for the couple to adjust to. Nevertheless, they remained committed to getting these treatments. They thought this treatment was more important for a person with mildly impaired cognitive function, like their case, than for a more severe case because he still had much more function. These were not complaints, just an observation. The patient had accepted his diagnosis much better intellectually than emotionally. Thus, they discovered that the patient seemed to display a lack of emotional resilience.
They looked forward with hope to the second treatment on June 6, knowing that it would be an additional 15 weeks until they would again meet with the neurologist, on September 19. They were hopeful that the observations, after that treatment, would be sufficiently positive to convince her to provide a third CT. The patient’s wife asked the author to send published articles about treatments with low doses of radiation for other conditions and diseases, which they could present in support of their request for additional CT scans.
After the June 6th treatment, the couple observed improved clarity, focus and good humor. His 23/30 MMSE score on June 20 was about the same as his 24/30 score on May 28.
During the summer, the patient had maintained strong intellectual interests by reading books and newspapers and conversing about complex subjects. He had difficulty in a group of people where the many voices and the uncertainty of when to break into the conversation cause him to clam up. His music skills, reading music, and improvising jazz were robust. However, he found it harder and harder to focus on art projects that he would have liked to complete. He noticed that impulses both verbal and in actions were hard to resist, sometimes feeling like a child with attention deficit hyperactivity disorder. Random memory failures became a persistent problem.
On September 19, at the neurologist, his score was 26/30, which was an improvement over the February 26 baseline of 22/30. She was given a copy of the papers about various diseases and conditions remediated by low doses of radiation. The third scan, scheduled for October 4, was 17 weeks after the June 6th treatment. He complained that, instead of focusing for hours on a drawing, he worked for a short time and thought of another thing to do, such as a household chore, which distracted him. The neurologist suggested he write down the chore and continue with the drawing, but he had never been a list maker. Spatial confusion and difficulty following simple directions increased, and short-term memory lapses occurred more regularly. He used to make bread regularly but lost his cooking skills. He had to make major adjustments in driving between their summer and winter homes and in requiring assistance to close the summer home.
The third CT scan that had been booked for October 4 was moved to January 18 because the patient crashed and destroyed the car on October 3. Although the impact was significant, his injuries were minor because the air bags had deployed. His discharge on the same day followed a chest X-ray and a CT scan. This accident ended the patient’s driving.
On October 14, the patient was diagnosed with post-concussive syndrome by his internist. The prognosis: symptoms like worsening dementia (fatigue, irritability, lack of focus, confusion) with recovery in 2–3 months. This was accurate, as observed by the couple and their friends. On November 3, his neurologist examined him and advised against treatments for 3 months after that injury.
Treatments and Progression in 2017
The neurologist examined the patient on January 12. His MMSE score was 26/30 verbal and 21/30 in math, lower overall than in September. The MoCA test 16 was administered to obtain his baseline score of 17/30.
Following the January 18th CT scan, improved clarity, focus, good humor, clarinet playing, and conversation were perceived by the couple and their friends. Executive function was still the principal area of impairment.
On February 9, the neurologist examined the patient. His MMSE and MoCA scores did not improve after the January 18th treatment. They were the same as the January 12th scores.
On March 28, the patient reported feeling angry at being more distracted, more impulsive, and more cognitively rigid. The neurologist replied that he was still in early to mid-stage; his MMSE score was 25/30 and his MoCA score was 18/30.
A battery of neuropsychological tests was performed on April 13; his results were discussed on May 9. His MMSE score was 24/30.
Even though the ride on May 23 to the CT scanner was pleasant, the patient was sullen and unresponsive. However, after receiving the treatment, he came out smiling broadly and was in very good spirits on the ride home. His wife observed improved cognition and behavior, and a better sense of timing in conversation. He even picked up the thread of a story on the radio and commented. Again, as in the past, his wonderful sense of humor, which had never totally vanished but appeared less often, was really in action. When asked how he felt after the treatment, he suggested getting his own scanner, with a laugh, and later proposed looking for a device that would do treatments when needed.
June 6 was not a good day, and the neurologist decided not to test him. He was very depressed. The discussion focused on whether he should take anti-depressants. The collective decision was to exercise more and not take drugs for mood control at this time.
On September 14, the neurologist performed the MoCA; the score was 16/30.
On October 19, the patient had a treatment and agai emerged smiling and upbeat. He quipped about asking for a CT scanner for Christmas.
On October 24, significant deterioration was observed at the visit to the neurologist. The MoCA score was 11/30, down from 16/30 in September. He had entered the moderate or mid-range of Alzheimer’s. This corresponded to the observation of his increased distraction or difficulty in staying focused. He paid less attention; his memory and his vision were worse. The couple saw some improvement after the October 19th treatment. They were hopeful that a shorter interval between scans would be beneficial. The neurologist was sympathetic to this, but she expected institutional barriers because it would need to be reviewed as an experimental therapy. The couple had hoped that frequent treatments at an early stage would stabilize the patient at a high level.
Summary of the Treatments
2016 Apr 7 (46 mGy), Jun 6, Oct 3 (CT scan after collision) 2017 Jan 18 (50 mGy), May 23, Oct 19
Lead Author’s Conversation with the Neurologist
The author spoke with the neurologist on November 7, 2017. She was receptive to this method of treatment, i.e., a series of CT scans to build up a long-lasting increase of protection system activity against oxidative damage. However, she was apprehensive about opposition from the medical community to the use of a diagnostic procedure that employs ionizing radiation, for treatment.
Due to a number of factors, including professional job security fears, lack of organizational and professional peer support, intervening pregnancy leave of absence, and an automobile accident affecting the patient, the treatments were limited and sporadic. Nonetheless, the treatments appear to have yielded a series of consistent patterns of remarkable recovery, of complex behaviors, and performance activities, despite being of a prolonged (up to several months) but transitory nature.
Ongoing Progression of the Patient’s Condition
During 2018, the patient’s condition declined, becoming progressively worse.
In January 2019, the lead author sent the couple a case report about hyperbaric oxygen therapy (HBOT) for Alzheimer’s disease. 17 The patient received 43 HBOT treatments; however, no conclusive benefit was observed. (The HBOT case report 17 shows many radiation scans to image the brain, which suggests that it was the radiation not the oxygen that caused the benefit in that study.)
The patient died on September 7, 2020, at age 77.
Discussion
Assessing this case, a patient in Massachusetts had been suffering from early-stage Alzheimer’s disease, for which there is no known cure. He was informed about a novel and harmless treatment, a series of CT scans of the brain that gave remarkable, long-lasting improvements in cognition and behavior to a patient, in Michigan, with severe Alzheimer’s disease. The patient and his wife found a young neurologist practicing in their local medical center, presented the case report about the Michigan patient, and asked for the same treatment, a CT scan every 2 weeks. The neurologist prescribed one treatment and observed the immediate benefit.
The physician’s fear in prescribing CT scans, low-dose radiotherapy, to this patient is one of the serious consequences of the ionizing radiation health scare that was created and disseminated from 1954 to 1960 by the Rockefeller Foundation and the National Committee on Radiation Protection and Measurement (NCRP). 18 Worldwide publicity of this radiation scare 19 impacted the many low-dose medical therapies that had been used for more than 60 years, prior, to treat serious diseases, such as inflammations, infections, and different kinds of cancers. 5
An influential international “scientific” consensus developed, at that time, on the biological mechanism through which radiation exposures can induce harm, and it exists to this day. It still assumes that the risk of radiation-induced cancer is proportional to the dose, to be calculated by the linear no-threshold (LNT) dose-response model. It still ignores the biological evidence that every organism has powerful adaptive protection systems that prevent damage, repair damage, remove damage, and restore health, as shown in Figure 1. So, physicians still shun radiation treatments that stimulate a patient’s protection systems. High-dose radiotherapy has always been acceptable for destroying tumors and killing cancer cells. Low doses are only for diagnostic imaging, and each exposure must now be as low as reasonably achievable, to minimize the hypothetical risk of radiation-induced cancer, still calculated by the LNT model.5,18
The widespread evidence that contradicts the LNT model has been ignored by all government regulators since 1960, even though many scientists have been presenting old and new facts. 20 The 2012 article by Fliedner et al 21 reviewed the medical histories of the victims of 10 accidental chronic radiation exposures and studies on irradiated rodents and dogs. Radiation is an extremely weak carcinogen. “There is a great discrepancy between recommended dose rate limits, for instance, of 1 mGy/year for the general public … and … the observed dose rate of 3 mGy/day (1,100 mGy/year) at which the hematopoietic system in beagle dogs keeps providing homeostasis and full function in the service to the whole body (the incidence of fatal tumors in the experimental dogs being the same as for the control dogs).” 21 In the U.S. DOE Nuclear Shipyard Workers Study, the high-dose workers demonstrated significantly lower circulatory, respiratory, and all-cause mortality than did the unexposed workers. Mortality from all cancers combined was also lower in the exposed cohort.22,23 Studies by the lead author on the Hiroshima atomic bomb survivors have revealed the acute threshold dose for the onset of radiation-induced leukemia to be quite high, about 1.1 Gy.5,18
Lauriston Taylor, founder, and long-time president of the NCRP, proclaimed in his 1980 Sievert Lecture that studies “calculating the numbers of people who will die as a result of having been subjected to diagnostic X-ray procedures (using the LNT model) … These are deeply immoral uses of our scientific knowledge.” 24
This case has limitations; it is not a case study with a rigorous experimental design. The patient requested CT scan treatments, one every 2 weeks, plus booster treatments, as given to the case in Michigan. However, he received only 3 scans in 2016 and only 3 scans in 2017, spaced months apart. While the MMSE and MoCA test results were quantitative and objective, the observations by the patient, his relatives, and his friends were qualitative and subjective. Nevertheless, their information is of value because a dementia patient likely has no desire to communicate or cooperate with an objective investigator whose voice, accent, and appearance are unfamiliar. The goal of a therapy for all Alzheimer’s patients (and their families) should be to improve the quality of their lives by optimizing their well-being, staying brain health, and restoring communication with family and friends, to avoid social isolation, loneliness, and under stimulation.
Progress in this field of study will require medical scientists to objectively examine and evaluate the historical and scientific foundations that support the current LNT risk assessment policies. Our detailed examinations and evaluations have found them to be extremely disturbing, being based largely on voluminous mistakes, and numerous myths that have grossly misrepresented the risks of ionizing radiation in the low dose zone. 25
Notes
Cognitive impairment: recognition, diagnosis, and management in primary care, is often measured by the Standardized Mini-Mental State Examination (MMSE). The range for early stage, mild impairment is 25–20; the range for a normal person is 30–26.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Jerry M Cuttler https://orcid.org/0000-0001-9532-9818
Edward J Calabrese https://orcid.org/0000-0002-7659-412X
References
- 1.Wolk DA, Dickerson BC. Clinical Features and Diagnosis of Alzheimer Disease. UpToDate; 2022. https://www.uptodate.com/contents/clinical-features-and-diagnosis-ofalzheimer-disease. [Google Scholar]
- 2.Calabrese E, Dhawan G, Kapoor R, Kozumbo W. Radiotherapy treatment of human inflammatory diseases and conditions: Optimal Dose. Hum Exp Toxicol. 2019;38:888-898. [DOI] [PubMed] [Google Scholar]
- 3.Janiak MK, Pocięgiel M, Welsh JS. Time to rejuvenate ultra-low dose whole-body radiotherapy of cancer. Crit Rev Oncol Hematol. 2021;160:103286. [DOI] [PubMed] [Google Scholar]
- 4.Vaiserman A, Cuttler JM, Socol Y. Low-dose ionizing radiation as a hormetin: Experimental observations and therapeutic perspective for age-related disorders. Biogerontology. 2021;22:145-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cuttler JM. Application of low doses of ionizing radiation in medical therapies. Dose Response. 2020;18(1):1-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Calabrese EJ, Kozumbo WJ. The hormetic dose-response mechanism: Nrf2 activation. Pharmacol Res. 2021;167:105526. [DOI] [PubMed] [Google Scholar]
- 7.Xing X, Zhang C, Shao M, et al. Low-dose radiation activates Akt and Nrf2 in the kidney of diabetic mice: A potential mechanism to prevent diabetic nephropathy. Oxid Med Cell Longev. 2012;2012:1-12. doi: 10.1155/2012/291087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cuttler JM, Feinendegen LE, Socol Y. Evidence that lifelong low dose rates of ionizing radiation increase lifespan in long- and short-lived dogs. Dose-Response. 2017;15(1):1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Doss M. Low dose radiation adaptive protection to control neurodegenerative diseases. Dose-Response. 2014;12(2):277-287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cuttler JM, Moore ER, Hosfeld VD, Nadolski DL. Treatment of alzheimer disease with CT scans: A case report. Dose-Response. 2016;14(2):1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cuttler JM, Moore ER, Hosfeld VD, Nadolski DL. Update on a Patient with alzheimer disease treated with CT scans. Dose-Response. 2017;15(1):1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cuttler JM, Moore ER, Hosfeld VD, Nadolski DL. Second update on a patient with alzheimer disease treated by CT scans. Dose-Response. 2018;16(1):1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cuttler JM, Abdellah E, Goldberg Y, et al. Low doses of ionizing radiation as a treatment for alzheimer’s disease: A pilot study. J Alzheim Dis. 2021;80:1119-1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chung M, Rhee HY, Chung WK. Clinical approach to low-dose whole-brain ionizing radiation treatment in alzheimer’s disease dementia patients. J Alzheim Dis. 2921;80:941-947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tombaugh TNand McIntyre NJ. The Mini-Mental State Examination: A Comprehensive Review. Journal of the American Geriatrics Society 1992;40(9):922-935. doi: 10.1111/j.1532-5415.1992.tb01992.x. [DOI] [PubMed] [Google Scholar]
- 16.Nasreddine ZS, Philips NA, Bedirian V, et al. The Montreal Cognitive Assessment, MoCA: A Brief Screening Tool For Mild Cognitive Impairment. Journal of the American Geriatrics Society 2005;53(4):695-699. doi: 10.1111/j.1532-5415.2005.53221.x. [DOI] [PubMed] [Google Scholar]
- 17.Harch P, Fogarty E. Hyperbaric oxygen therapy for Alzheimer’s dementia with positron emission tomography imaging: A case report. Med Gas Res. 2018;8(4):181-184. doi: 10.4103/2045-9912.248271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cuttler JM, Calabrese EJ. What would become of nuclear risk if governments changed their regulations to recognize the evidence of radiation’s beneficial health effects for exposures that are below the threshold for detrimental effects? Dose-Response. 2021;19(4):1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.The New York Times . Text of Genetics Committee Report Concerning Effects of Radioactivity on Heredity; FOREWORD What Are We worried about? June 13, 1956. https://www.nytimes.com/1956/06/13/archives/text-of-genetics-committee-report-concerning-effects-of.html [Google Scholar]
- 20.Cuttler JM. The NRC wrongfully rejected 3 petitions requesting that it end use of LNT model. Newsline. J Nuclear Med. 2022;63(1):19N-20N. [PMC free article] [PubMed] [Google Scholar]
- 21.Fliedner TM, Graessle DH, Meineke V, Feinendegen LE. Hemopoietic response to low dose-rates of ionizing radiation shows stem cell tolerance and adaptation. Dose-Response. 2012;10(4):644-663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sponsler R, Cameron JR. Nuclear shipyard worker study (1980 1988): A large cohort exposed to low-dose-rate gamma radiation. Int J Low Radiat. 2005;1(4):463-478. [Google Scholar]
- 23.Matanoski G. Health Effects of Low-Level radiation in Shipyard Workers, Final Report. Baltimore, MD: DOE DE-AC02. -79 EV10095. 1991. http://www.osti.gov/bridge/product.biblio.jsp?osti_id=10103020. [Google Scholar]
- 24.Taylor LS. Some nonscientific influences on radiation protection standards and practice. The 1980 Sievert Lecture. Health Phys. 1980;39(12):851-74. [PubMed] [Google Scholar]
- 25.Calabrese EJ. Ethical failings: The problematic history of cancer risk assessment. Environ Res. 2021;193:110582. [DOI] [PubMed] [Google Scholar]