Abstract
Background:
Patients undergoing unicompartmental knee arthroplasty (UKA) often want to return to sport (RTS) after surgery. However, the time taken to RTS and proportion of patients who RTS after UKA remain unknown.
Purpose:
To determine the time to RTS and proportion of patients who RTS after UKA.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A search was performed using PubMed, Medline, Embase, SPORTDiscus and the Cochrane Library databases for clinical trials reporting on RTS after UKA published between database inception and September 2021. In addition, a manual search was performed of relevant sports medicine and orthopaedic journals, and bibliographies were reviewed for eligible trials. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines were used to undertake this study.
Results:
This meta-analysis included 11 studies (749 patients) that reported on RTS after UKA. The proportion of patients returning to sports increased over time: 6 studies (432 patients) demonstrated an overall pooled proportion of 48.1% (95% CI, 36.3%-60.2%) of patients who returned to sport at 3 months after surgery, while 7 studies (443 patients) demonstrated an overall pooled proportion of 76.5% (95% CI, 63.9%-87.1%) of patients who returned to sport at 6 months after surgery. Overall, 92.7% (95% CI, 85.8%-97.4%) of 749 patients were able to RTS at 4 years after surgery. Overall excellent patient-reported functional outcomes scores and low risk of complications with RTS after UKA were reported.
Conclusion:
The authors found that 48.1% of patients were able to RTS at 3 months after surgery and 76.5% were able to RTS at 6 months after UKA. Pooled proportion analysis showed that >90% of patients undergoing UKA were able to RTS at 48 months after surgery. The majority of patients who were able to RTS after UKA did so at a lower level of intensity than their preoperative level. RTS after UKA was associated with good patient-reported functional outcomes scores and a low risk of complications.
Keywords: arthroplasty, arthroplasty and sports, knee arthroplasty, knee surgery, return to sport, sports, unicompartmental knee arthroplasty
Unicompartmental knee arthroplasty (UKA) is an effective surgical treatment for end-stage arthritis confined to a single compartment of the knee joint. 1,3 Within the United Kingdom, UKA accounts for 8% to 10% of all knee arthroplasties undertaken, with >10,000 primary UKAs performed annually. 39 Patients who undergo UKA have been shown to have faster postoperative rehabilitation, better restoration of native knee kinematics, earlier restoration of gait, and improved patient-reported outcomes compared with those undergoing a total knee arthroplasty (TKA). 14,26,28 –30,32,36,43 Studies have shown UKA in professional athletes enabled a return to competitive sports with a relatively low risk of complications at short-term follow-up. 16,54 UKA is undertaken conventionally in patients who are younger and more active, with increased physiological demands compared with those undergoing a TKA. 32,37 Often, these patients would like to return to sport (RTS) after surgery, but there is no uniform consensus on the time at which this may be safely achieved.
There is a paucity of high-quality studies reporting on RTS after UKA. Studies that have specifically focused on this topic, such as those by Naal et al, 38 Lo Presti et al, 33 and Panzram et al, 40 are retrospective case series with no level 1 evidence presented. Studies with higher quality evidence have focused on patient-reported outcome measures (PROMs) and other outcomes. In their 2020 meta-analysis of RTS after knee arthroplasty, Konings et al 31 reported the level of participation with several postoperative sporting activities and a greater focus on TKA than UKA. 31 Belsey et al 4 compared RTS after UKA and high-tibial osteotomy (HTO) in their meta-analysis, with a singular focus on PROMs and the ability to return to physical activity between these 2 groups. The only similar high-quality study to date is by Witjes et al, 52 who performed a meta-analysis in 2016 comparing RTS in both TKA and UKA but with a greater focus on PROMs. Time to RTS was reported in this study, but with only 3 studies in their meta-analysis reporting this outcome, no meaningful significance was achieved.
An improved understanding of time to RTS after UKA would facilitate more informed preoperative discussions between health care professionals and patients and provide evidence-based timeframes for postoperative rehabilitation. The objective of this meta-analysis was to determine the time and proportion of patients who RTS after UKA.
Methods
Eligibility Criteria
This study was performed using the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. The study protocol was published online at the PROSPERO international prospective register of systematic reviews and meta-analyses (CRD42020206119). Inclusion criteria for this meta-analysis were studies published in English with the following characteristics: (1) patients who participated in sports before and after surgery, (2) patients who underwent primary UKA, and (3) results for time to RTS after UKA. Exclusion criteria were (1) review articles, (2) articles without results or full-text available for analysis, and (3) articles without any outcome data relating to the time to RTS.
Data Search
A search was performed using PubMed, Medline, Embase, SPORTDiscus, and the Cochrane Library databases for trials on UKA and RTS in the English language published between the inception of the database and September 2021. The search MeSH terms used were “unicompartmental knee arthroplasty” or “unicompartmental knee replacement” and “return to sport” or “return to activities” or “time to return to sport” or “activity” or “sport.” In addition, a manual search was performed of relevant sports medicine and orthopaedic journals. The reference lists of papers were also reviewed for eligible trials.
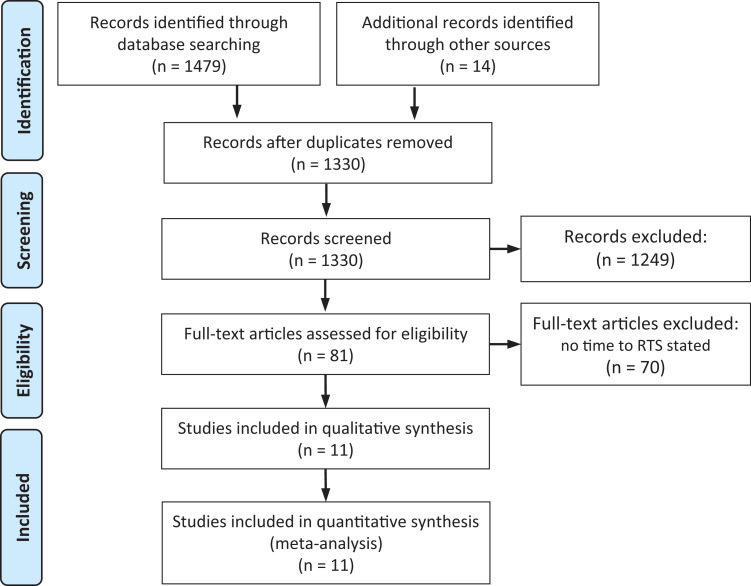
The initial literature search revealed 1479 studies, and a further 14 articles were added from additional sources. Of these, 163 duplicates were deleted, and 1249 articles were immediately excluded, as they did not meet the parameters for study. The remaining 81 articles underwent full-text analysis, and 70 were excluded, as they did not include data on the primary outcome. In total, 11 studies remained for the meta-analysis. § The flowchart of study inclusion is presented in Figure 1.
Figure 1.
PRISMA flowchart of the study search strategy. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; RTS, return to sport.
Assessment of Study Quality
A quality assessment for the studies was conducted using the methodological index for nonrandomized studies (MINORS). 45 This scoring system has 12 items that are used to grade the methodology of each study using predefined criteria with scores of 0 (not reported), 1 (poorly reported/inadequately reported), or 2 (well reported). For noncomparative studies, only the initial 8 items are graded, for a maximum score of 16. For comparative studies, all 12 items are graded, and so the maximum possible score is 24.
Outcomes Measured
The following outcomes were assessed in this study: time to RTS, proportion of patients who returned to sport after UKA, PROMs after RTS, and complications after RTS.
Data Extraction
All potentially eligible studies were screened independently by 2 observers (A.M. and G.T.R.), and data relating to the following outcomes were recorded from each study: patient characteristics, methodological quality, operation type, time to RTS, proportion of patients who achieved RTS, PROM scores after RTS, and complications after RTS. The data were recorded in an electronic data collection form. Any discrepancies in the data recorded were resolved after discussion with a third reviewer (A.A.). The authors of the individual trials were not contacted for further information.
Statistical Analysis
Interobserver agreement on the screening and selection of articles and assessment of quality was assessed using kappa coefficients. The proportion of patients who returned to sport at different time intervals from all the studies was gathered and recorded in contingency tables (ie, the number of patients who returned to sport from the entire cohort). For each time interval, the overall adjusted pooled proportion was calculated using meta-analysis of proportions. This provided the overall pooled proportional rate of RTS as time elapsed during the follow-up period after surgery. The overall proportion of patients who returned to sport at the end of the follow-up from each study was assessed using the same meta-analysis method. Heterogeneity was examined using the I 2 statistic index and Cochran chi-square test (Q test). Due to the significant heterogeneity in the quality and type of the studies, a random-effects model was used for the meta-analysis calculation of the overall proportions at the different time intervals and the end of the follow-up. All calculations were performed using StatsDirect software (Version 3).
Results
Characteristics of the Included Studies
All 11 included studies were published between 2006 and 2021, with a follow-up time of between 1 and 49 months postoperatively (Table 1). One study 33 collected data prospectively, and the remaining studies collected data retrospectively using a follow-up questionnaire or assessment.
Table 1.
Characteristics of Included Studies (n = 11) a
| Lead Author (Year) | Country | Study Design | Sample Size | Sex, F/M, n | Age, y | Indication | Active Preoperatively, n b | Rate of RTS, % | Maximum Follow-up, mo |
|---|---|---|---|---|---|---|---|---|---|
| Walton (2006) 51 | Australia | Retrosp | 150 | 74/76 | 71.53 | NR | 150 | 86 | NR |
| Naal (2007) 38 | Switzerland | Retrosp | 83 | 38/45 | 65.5 | 72 OA, 11 osteonecrosis |
77 | 94.8 | 18 |
| Wylde (2008) 54 | UK | Retrosp | 100 | 52/48 | 66 | NR | 36 | 75 | 36 |
| Hopper (2008) 22 | UK | Retrosp | 34 | 14/20 | 62.9 | NR | 30 | 90 | 12 |
| Pietschmann (2013) 41 | Germany | Retrosp | 78 | 43/35 | 65.3 | OA | 78 | 88.4 | 49 |
| Ho (2016) 19 | USA | Retrosp | 36 | 24/12 | 60 | NR | 30 | 87 | 24 |
| Walker (lat) (2015) 49 | Germany | Retrosp | 45 | 26/19 | 60.1 | OA | 43 | 98 | 24 |
| Walker (med) (2015) 50 | Germany | Retrosp | 93 | 47/46 | 55 | OA | 86 | 93 | 24 |
| Lo Presti (2019) 33 | Italy | Prosp | 58 | 39/15 | 59.7 | OA | 53 | 90 | 48 |
| Canetti (2018) 7 | France | Retrosp | 27 | 21/6 | 66.5 | OA | 25 | 100 (robot) 94 (jig) |
24 |
| Panzram (2021) 40 | Germany | Retrosp | 211 | NR | 64.4 | OA and rheumatism | 141 | 92.9 | 37.1 |
a F, female; lat, lateral; M, male; med, medial; NR, not reported; OA, osteoarthritis; Prosp, prospective; Retrosp, retrospective; RTS, return to sport.
b Patients who participated in at least 1 form of activity preoperatively.
Quality Assessment
Table 2 shows the MINORS scores for all studies. The mean MINORS score was 8.125 of 16 for the 8 noncomparative studies, 7,33,38,40,41,49,50,53 indicating low quality, and 16 of 24 for the remaining 3 comparative studies, indicating fair quality. 19,22,51
Table 2.
MINORS Scores for Included Studies a
| MINORS Items for Noncomparative Studies b | Additional MINORS Items for Comparative Studies b | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study (Year) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | Total Score c |
| Walton (2006) 51 | 2 | 0 | 0 | 2 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | 14 |
| Naal (2007) 38 | 2 | 0 | 0 | 1 | 0 | 1 | 0 | 2 | N/A | N/A | N/A | N/A | 6 |
| Wylde (2008) 54 | 2 | 0 | 0 | 1 | 0 | 0 | 0 | 2 | N/A | N/A | N/A | N/A | 5 |
| Hopper (2008) 22 | 2 | 0 | 0 | 1 | 0 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | 15 |
| Pietschmann (2013) 41 | 2 | 2 | 0 | 1 | 0 | 0 | 0 | 2 | N/A | N/A | N/A | N/A | 7 |
| Ho (2016) 19 | 2 | 2 | 0 | 2 | 0 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 19 |
| Walker (lateral) (2015) 49 | 2 | 1 | 2 | 1 | 0 | 1 | 2 | 2 | N/A | N/A | N/A | N/A | 11 |
| Walker (medial) (2015) 50 | 2 | 1 | 2 | 1 | 0 | 2 | 0 | 2 | N/A | N/A | N/A | N/A | 10 |
| Lo Presti (2019) 33 | 2 | 1 | 2 | 1 | 0 | 2 | 0 | 2 | N/A | N/A | N/A | N/A | 10 |
| Canetti (2018) 7 | 2 | 1 | 0 | 0 | 1 | 2 | 0 | 2 | N/A | N/A | N/A | N/A | 8 |
| Panzram (2021) 40 | 2 | 1 | 0 | 1 | 0 | 2 | 0 | 2 | N/A | N/A | N/A | N/A | 8 |
a MINORS, methodological index for nonrandomized studies; N/A, not applicable. The MINORS scoring system has 12 items that are used to grade the methodology of each study using predefined criteria with scores of 0 (not reported), 1 (poorly reported/inadequately reported), or 2 (well reported). For noncomparative studies, only the initial 8 items are graded, for comparative studies 12 items can be graded.
b MINORS items: (1) clearly stated aim, (2) inclusion of consecutive patients, (3) prospective collection of data, (4) endpoints appropriate to the aim of the study, (5) unbiased assessment of the study endpoint, (6) follow-up period appropriate to the aim of the study, (7) loss to follow-up <5%, and (8) prospective calculation of the study size. Additional criteria for comparative studies: (9) adequate control group, (10) contemporary groups, (11) baseline equivalence of groups, and (12) adequate statistical analyses.
c Scores are interpreted as follows: for noncomparative studies, 0-4 = very low, 5-8 = low, 9-12 = fair, and 13-16 = high; for comparative studies, 0-6 = very low, 7-12 = low, 13-18 = fair, and 19-24 = high. 45
Data Extraction and Calculations
Of the 11 studies, 8 provided data on RTS as time intervals ranging between 1 and 24 months. 7,22,33,38,40,49 –51 One study provided the time to RTS as a “one-time interval.” This was incorporated into the time to RTS as well as overall RTS at the end of follow-up. 19 Two studies were not included, as they did not specify a time period 41,55 ; however, they were included in the overall calculation of RTS at the end of the follow-up period. Data from all the studies were included to provide an overall proportion of patients who returned to sport after UKA, regardless of the follow-up period. Six studies expressed the time for RTS using means and SDs, 22,33,38,40,49,50 and 3 reported data as medians and ranges. 7,19,51 When the mean was reported, 2 SDs were added to the mean to determine the maximum time interval. When the median and range were used, the maximum range was used as the time interval in the calculations.
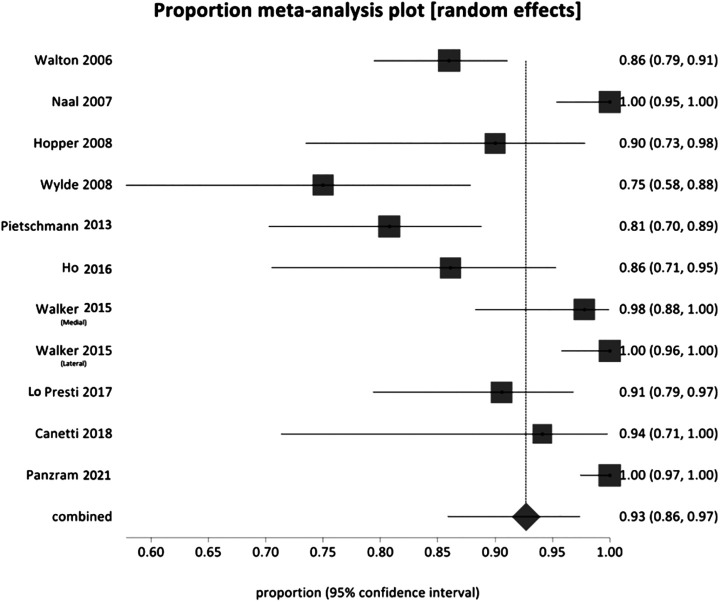
Return to Sports
Of the 11 included studies, the overall adjusted pooled proportion of RTS was 92.7% (95% CI, 85.8%-97.4%). The pooled proportion of patients returning to sports was shown to increase over time: the RTS of 6 studies at 3 months postoperatively was 48.1% (432 patients) (95% CI, 36.3%-60.2%; P < .001), and after 6 months postoperatively, the pooled proportion of RTS of 7 studies was 76.5% (443 patients) (95% CI, 63.9%-87.1%; P < .001) (Table 3 and Figure 2). 19,22,33,38,40,49,51 Wylde et al 54 reported the lowest proportion of patients returning to sport; 75% of the total cohort were able to RTS at 1 to 3 years after UKA. In contrast, Naal et al 38 and Canetti et al 7 reported RTS rates of 94.8% and 94% at 24 months. Canetti et al 7 further highlighted that the 11 patients undergoing robotic-assisted UKA had a 100% rate of RTS and the time taken to RTS was significantly less than that for those undergoing conventional jig-based UKA (4.2 ± 1.8 vs 10.5 ± 6.7 months; P < .01).
Table 3.
Time to RTS at 1, 3, 5, 6, and 24 Months Postoperatively a
| Time Interval | No. of Studies | Patients, RTS/Total, n | Pooled Proportion Rate of RTS % (95% CI) | I 2 % (95% CI) | Q Statistic (P Value) |
|---|---|---|---|---|---|
| 1 mo | 2 | 57/227 | 25.3 (19.9-31.2) | 0 | 0.208 (.649) |
| 3 mo | 6 | 223/432 | 48.1 (36.3-60.2) | 83.7 (60.8-90.7) | 30.59 (<.001) |
| 5 mo | 1 | 31/36 | 87 | – | – |
| 6 mo | 7 | 340/443 | 76.5 (63.9-87.1) | 87.4 (75.4-92.1) | 47.60 (<.001) |
| 24 mo | 1 | 16/17 | 94 | – | – |
| End of follow-up | 11 | 689/749 | 92.7 (85.8-97.4) | 89.1 (82.-92.4) | 92.14 (<.001) |
a RTS, return to sports. Dashes indicate not recorded.
Figure 2.
Forest plot depicting the overall RTS at the end of the follow-up from all the studies: I 2 = 89.1% (95% CI, 82.9%-92.4%); Q = 92.137812 (df = 10); P < .0001. RTS, return to sports.
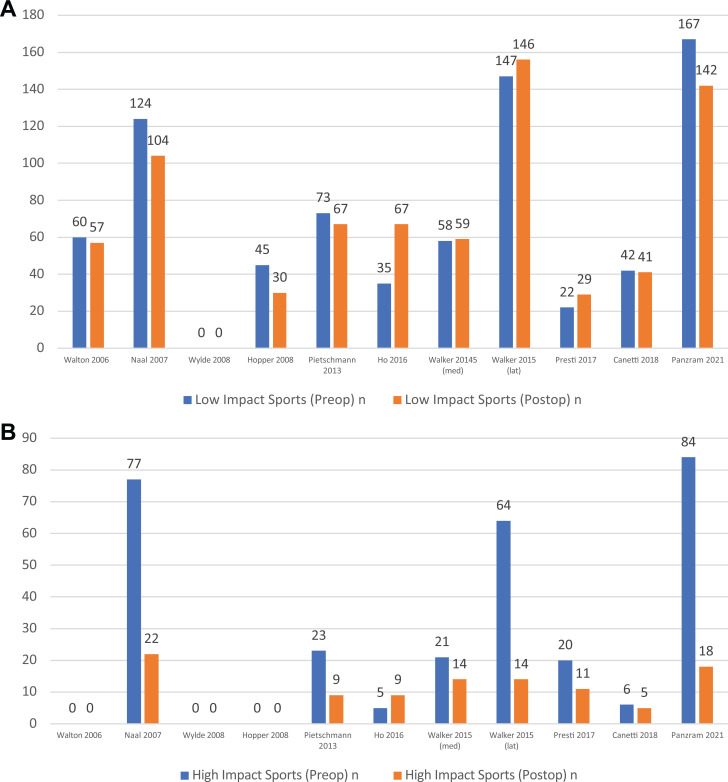
Postoperative Sporting Activities
Common sporting activities undertaken in all 11 studies were swimming, cycling, walking, soccer, jogging, and downhill skiing. The proportion of patients who continued to engage in higher impact sports declined. Naal et al 38 and Walker et al 49,50 showed a statistically significant decrease in soccer and skiing. Low impact sports, including cycling, hiking, and swimming, experienced a 2% decrease throughout all 11 studies, which is reflective of the rate of RTS. Lo Presti et al 33 highlighted that there had been a move toward sports such as cycling and swimming, which had increases in participation postoperatively of 29% and 31%, respectively (Figure 3).
Figure 3.
Participation in (A) high-impact (soccer, skiing, and jogging) and (B) low-impact (walking, cycling, and swimming) sports before and after UKA. NR, not reported; Postop, postoperative; Preop, preoperative.
Patient-Reported Outcome Measures
All 11 studies reported PROM data for their cohort, with postoperative PROMs showing overall improvement across all patients in this meta-analysis. The University of California-Los Angeles (UCLA) score was used in 6 of the studies. 7,19,40,41,49,50 Panzram et al 40 reported a significant increase from a preoperative mean of 2.9 ± 1.7 (range, 1-10) to 6.3 ± 1.4 (range, 2-10) at mean 37.1-month follow-up (P < .001). The mean change was 3.5 ± 2.0, and postoperatively 53.7% of the population were defined as highly active, as they achieved a UCLA score >7. 40 In their study on medial compartment UKA, Walker et al 50 highlighted that their mean UCLA score also improved significantly from 3.3 ± 1.5 to 6.8 ± 1.5 after 24 months (P < .001). Furthermore, in this study, there was no statistically significant difference in UCLA scores among patients who had had a unilateral replacement as well as a bilateral replacement. In their study on lateral compartment UKA, Walker et al 50 also found that the UCLA activity score improved from 5.3 ± 2.3 to 6.7 ± 1.5; 66% of their cohort was highly active, with a UCLA score of >7. One study 19 showed an overall decrease in the UCLA score; the preoperative cohort had a score of 8.1 ± 1.5, which dropped postoperatively to 7.4 ± 1.6 (Table 4).
Table 4.
PROM Scores After UKA a
| Study (Year) | PROM Score, Mean ± SD | |
|---|---|---|
| Preoperative | Postoperative | |
| Walton (2006) 51 | NR | OKS: 22.17 ± 9.03 |
| Naal (2007) 38 | KSS: 129.9 ± 24.8 | KSS: 186.9 ± 18.3 |
| Wylde (2008) 54 | NR | WOMAC: 81.6 |
| Hopper (2008) 22 | OKS: 17.9 | OKS: 39.4 |
| Pietschmann (2013) 41 | NR | UCLA: 7.1 ± 1, OKS: 40.8 ± 5.2 |
| Ho (2016) 19 | UCLA: 8.1 ± 1.5 | ULCA: 7.4 ± 1.6 |
| Walker (lateral) (2015) 49 | UCLA: 5.3 ± 2.3 OKS: 30 |
UCLA: 6.7 ± 1.5 OKS: 43 |
| Walker (medial) (2015) 50 | UCLA: 3.3 ± 1.5 | UCLA: 6.8 ± 1.5 |
| Lo Presti (2019) 33 | HSS: 52 | HSS: 88 |
| Canetti (2018) 7 | UCLA (robot-assisted): 6.4 ± 1.6 UCLA (jig-based): 5.8 ± 0.9 |
UCLA (robot-assisted): 6.6 ± 1.4 UCLA (jig-based): 6.2 ± 1 |
| Panzram (2021) 40 | UCLA: 2.9 ± 1.7 | UCLA: 6.3 ± 1.4 |
a HSS, Hospital for Special Surgery score; KSS, Knee Society Score; NR, not reported; OKS, Oxford Knee Score; PROM, patient-reported outcome measure; UCLA, University of California-Los Angeles activity score; UKA, unicompartmental knee arthroplasty; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index.
Complications
Of the 11 studies, 7 reported postoperative complications, with no mortality. A total of 17 (3.72%) patients were recorded as having complications. The majority of these complications resulted in revision to TKA. No study reported complications as a result of RTS (Table 5). 7,19,33,40,41,49,50
Table 5.
Complications After UKA a
| Study (Year) | Laterality | Complications Resulting in Revision | Time to Complications | Related to Sports |
|---|---|---|---|---|
| Pietschmann (2013) 41 | 78 medial | Revision to UKA (n = 2): 1 for impingement, 1 for suspected infection | NR | No |
| Ho (2016) 19 | NR | Type not documented (n = 2) | NR | No |
| Walker (lateral) (2015) 49 | 43 lateral | Revision to TKA (n = 2): both for dislocation | NR | No |
| Walker (medial) (2015) 50 | 86 medial | Revision to TKA (n = 5): 3 for pain, 1 for periprosthetic fracture, 1 for suspected infection | Pain: 10, 13, and 32 mo Periprosthetic fracture: 96 mo Suspected infection: 0.5 mo |
No |
| Lo Presti (2019) 33 | 53 medial | 0 | N/A | No |
| Canetti (2018) 7 | 25 lateral | 0 | N/A | No |
| Panzram (2021) 40 | 141 medial | Revision to TKA (n = 3): all for progression of OA Revision to UKA (n = 1) for tibial overstuffing Dislocation (n = 2): 1 from arthrofibrosis, 1 from wound infection |
N/A | No |
a N/A, not applicable; NR, not reported; OA, osteoarthritis; TKA, total knee arthroplasty; UKA, unicompartmental knee arthroplasty.
Discussion
The most pertinent findings from this study are that 48.1% of patients were able to RTS at 3 months after UKA and 76.5% were able to RTS at 6 months after UKA. Pooled proportion analysis showed that 92.7% of patients undergoing UKA were able to RTS at 48 months after surgery. The majority of patients who were able to RTS after UKA did so at a lower level of intensity than their preoperative level. RTS after UKA was associated with excellent PROMs and low risk of complications at short-term follow-up.
Patients undergoing UKA have better restoration of native limb alignment and knee kinematics compared with those undergoing conventional TKA with neutral mechanical alignment. 22 This has been attributed to UKA better preserving the native intra-articular knee ligaments, soft tissue envelope, joint line, and Q angle. 9,20,47,48 The rapid RTS after UKA may reflect the reduced invasiveness and surgical trauma of this procedure compared with conventional TKA. Yang et al have shown that UKA is associated with reduced need for analgesia, faster postoperative functional rehabilitation, earlier hospital discharge, and less time to normalization of gait compared with TKA. 55
HTO is an alternative to UKA in patients with medial compartment osteoarthritis. 23 Its use is confined to strict patient criteria including younger and active (<65 years of age), normal body mass index, mild articular degeneration, no patellofemoral arthrosis, and good range of motion (ROM) with a stable joint. 2,17 It has a heavy bias toward younger patients, and much of the research evaluating RTS after HTO is biased toward the male population. 6,13 A systematic review evaluating RTS after HTO had a mean age of 46.2 years (range, 16-80 years), and 63.6% were male. Of 250 patients, 218 (87.2%) returned to sport postoperatively overall. Although 89% returned within 1 year, this outcome was only reported in 37 patients. Comparatively, in our study, 92.7% of patients returned to sport overall, with 76.5% returning to sport within 6 months. The younger age and male bias of HTO compared with UKA should be acknowledged, with UKA providing a successful outcome in a broader demographic of patients.
Complications have been noted after both UKA and HTO. Complications associated with UKA are typically worsening arthritic changes compared with those associated with HTO, including intra-articular fractures, nonunion, and peroneal nerve palsy, which are arguable more significant and difficult to rectify. 21,44 HTO aims to preserve the integrity of the knee joint, leading to increased postoperative ROM 8 ; however, this benefit is confined to the early postoperative period, with studies at 1-, 5-, and 10 -year follow-up showing no superiority of HTO over UKA. 6,18,46 Furthermore, novel techniques such as robotic-assisted arthroplasty and functional alignment have already begun to show improved preservation of the soft-tissue envelope with greater postoperative ROM. 10,25,27 Thus, the higher and more severe complication rate in HTO, with limited benefit and strict patient selection, mean UKA may be a better choice for more patients who wish to RTS.
This meta-analysis also showed that progressively more patients were able to RTS over the first year after surgery, with 92.7% of patients (n = 689) returning after 1 year compared with 48.1% (n = 223) at 3 months. The wide variation in RTS at each of the time intervals is likely to reflect the intrastudy heterogeneity in the rehabilitation protocols, preoperative level of sporting intensity, and definition of full RTS.
Pooled proportion analysis found that >90% of patients were able to RTS within 24 months of surgery. It is important to acknowledge that the majority of patients did not return to their preinjury level of sporting activity, with all 11 studies showing a decline in patients participating in high-impact sports after surgery compared with preoperatively. The reasons for this are likely to be multifactorial. First, the views of the operating surgeons on postoperative sporting abilities may have limited the patients’ postoperative level of activity. 11,35 Pietschmann et al 41 highlighted that, between 3 and 6 months after surgery, surgeons actively discouraged their patients from participating in high-impact sports such as soccer, tennis, and jogging, and instead encouraged patients to return to low- or medium-impact sports such as swimming or cycling. 35 Second, patients’ apprehension about complications such as polyethylene wear, dislocation, or fracture may have limited their return to presurgery levels of sporting function. 15,24 Furthermore, the population of patients undergoing UKA are generally younger, healthier, and more active compared with those undergoing TKA. These patients are more likely to be motivated to RTS but also to have higher expectations of their abilities after surgery. Motivation and higher expectations have been shown to have a positive effect on a patient’s level of activity and sporting abilities after arthroplasty surgery. 5,31,42
Patients who underwent UKA were able to RTS with improvements in their PROMs at short-term follow-up after surgery. Walker et al 49 reported that, in their cohort of 45 patients undergoing lateral UKA, 66% of patients were highly active and participating in triathlons or marathons, with a UCLA score >7 at 24-month follow-up. Hopper et al 22 reported that, in their study of 30 patients undergoing UKA, the Oxford Knee Score improved from 17.9 preoperatively to 39.4 postoperatively at 12-month follow-up. Similarly, in their cohort of 53 patients of undergoing medial UKA, Lo Presti et al 33 found >90% of patients were able to RTS with a Hospital for Special Surgery score improving from 52 preoperatively to 88 points at 48 months after surgery. These studies provide a useful insight into improvements in functional outcomes with RTS but should be interpreted with caution. The PROMs within these studies have ceiling effects, and the studies did not perform subgroup analysis on functional outcomes in high-, moderate-, or low-impact sports. It is therefore important to perform a more detailed analysis or stratification of functional outcomes based on level of sporting activity. 12,34
A total of 17 patients in the entire cohort reported a complication after UKA, and 13 of those underwent revision. The most common causes of the revision were pain (n = 4), progression to bicondylar osteoarthritis (n = 3), and infection (n = 2). Of note, no study patients developed implant collapse or polyethylene wear. In the study by Walker et al, 50 5 patients developed postoperative complications, which included 3 patients with pain of unknown cause requiring TKA at 10, 13, and 32 months postoperatively. One patient developed infection requiring change of polyethylene liner at 1 and 8 years after surgery. 50 Pietschmann et al 41 reported that 2 patients underwent revision UKA surgery: 1 patient with impingement and 1 patient with infection. To the best of our knowledge, there are no studies showing increased risk of complications or premature implant failure following RTS after UKA. Further studies with 3-dimensional imaging and radiostereometric analysis may enable collection of more comprehensive data on implant migration or subsidence after RTS.
The limitations of this meta-analysis must be appreciated when interpreting the findings. The majority of studies included were retrospective studies that collated only a limited number of clinical outcomes with limited follow-up times. There was marked intrastudy heterogeneity owing to variations in rehabilitation protocols and definitions of full RTS. Furthermore, the surgeon and patient perspectives regarding RTS were not recorded in this study, which may have affected the timing and proportion of patients who were able to RTS. Studies were also limited in their follow-up times, and therefore the long-term effects of increased loading and RTS after UKA remain unknown. Despite these limitations, this study will enable more informed preoperative discussions between patients and their clinicians. It will facilitate better planning of postoperative rehabilitation for RTS and better guide long-term monitoring of complications after RTS.
Conclusion
Findings from this meta-analysis indicate that patients are able to RTS after UKA, with the pooled proportion analysis highlighting 90% RTS at 48 months. It has been shown that 48.1% of patients RTS within 3 months and 76.5% return within 6 months. However, patients did RTS at a lower level of intensity than their preoperative level. RTS after UKA was associated with excellent patient-reported functional outcomes and low risk of complications at short-term follow-up.
Footnotes
Final revision submitted October 8, 2021; accepted November 8, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: F.S.H. has received speaking fees from Smith & Nephew and Stryker and consulting fees and royalties from Smith & Nephew, Corin, MatOrtho, and Stryker. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Ackroyd CE. Medial compartment arthroplasty of the knee. J Bone Joint Surg Br. 2003;85(7):937–942. [DOI] [PubMed] [Google Scholar]
- 2. Akizuki S, Shibakawa A, Takizawa T, Yamazaki I, Horiuchi H. The long-term outcome of high tibial osteotomy: a ten- to 20-year follow-up. J Bone Joint Surg Br. 2008;90(5):592–596. [DOI] [PubMed] [Google Scholar]
- 3. Begum FA, Kayani B, Morgan SDJ, et al. Robotic technology: current concepts, operative techniques and emerging uses in unicompartmental knee arthroplasty. EFORT Open Rev. 2020;5(5):312–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Belsey J, Yasen SK, Jobson S, Faulkner J, Wilson AJ. Return to physical activity after high tibial osteotomy or unicompartmental knee arthroplasty: a systematic review and pooling data analysis. Am J Sports Med. 2021;49(5):1372–1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bradley B, Middleton S, Davis N, et al. Discharge on the day of surgery following unicompartmental knee arthroplasty within the United Kingdom NHS. Bone Joint J. 2017;99-B(6):788–792. [DOI] [PubMed] [Google Scholar]
- 6. Börjesson M, Weidenhielm L, Mattsson E, Olsson E. Gait and clinical measurements in patients with knee osteoarthritis after surgery: a prospective 5-year follow-up study. Knee. 2005;12(2):121–127. [DOI] [PubMed] [Google Scholar]
- 7. Canetti R, Batailler C, Bankhead C, et al. Faster return to sport after robotic-assisted lateral unicompartmental knee arthroplasty: a comparative study. Arch Orthop Trauma Surg. 2018;138(12):1765–1771. [DOI] [PubMed] [Google Scholar]
- 8. Cao Z, Mai X, Wang J, Feng E, Huang Y. Unicompartmental knee arthroplasty vs high tibial osteotomy for knee osteoarthritis: a systematic review and meta-analysis. J Arthroplasty. 2018;33(3):952–959. [DOI] [PubMed] [Google Scholar]
- 9. Chalmers BP, Mehrotra KG, Sierra RJ, et al. Reliable outcomes and survivorship of unicompartmental knee arthroplasty for isolated compartment osteonecrosis. Bone Joint J. 2018;100-B(4):450–454. [DOI] [PubMed] [Google Scholar]
- 10. Chang JS, Kayani B, Wallace C, Haddad FS. Functional alignment achieves soft-tissue balance in total knee arthroplasty as measured with quantitative sensor-guided technology. Bone Joint J. 2021;103-B(3):507–514. [DOI] [PubMed] [Google Scholar]
- 11. Dagneaux L, Bourlez J, Degeorge B, Canovas F. Return to sport after total or unicompartmental knee arthroplasty: an informative guide for residents to patients. EFORT Open Rev. 2017;2(12):496–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dunbar MJ, Robertsson O, Ryd L, Lidgren L. Appropriate questionnaires for knee arthroplasty: results of a survey of 3600 patients from The Swedish Knee Arthroplasty Registry. J Bone Joint Surg Br. 2001;83(3):339–344. [DOI] [PubMed] [Google Scholar]
- 13. Ekhtiari S, Haldane CE, de Sa D, et al. Return to work and sport following high tibial osteotomy: a systematic review. J Bone Joint Surg Am. 2016;98(18):1568–1577. [DOI] [PubMed] [Google Scholar]
- 14. Emerson RH, Alnachoukati O, Barrington J, Ennin K. The results of Oxford unicompartmental knee arthroplasty in the United States: a mean ten-year survival analysis. Bone Joint J. 2016;98-B(10)(suppl B):34–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Epinette JA, Brunschweiler B, Mertl P, et al. Unicompartmental knee arthroplasty modes of failure: wear is not the main reason for failure. A multicentre study of 418 failed knees. Orthop Traumatol Surg Res. 2012;98(6)(suppl):S124–S130. [DOI] [PubMed] [Google Scholar]
- 16. Ethgen O, Bruyère O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty: a qualitative and systematic review of the literature. J Bone Joint Surg Am. 2004;86(5):963–974. [DOI] [PubMed] [Google Scholar]
- 17. Gstöttner M, Michaela G, Pedross F, et al. Long-term outcome after high tibial osteotomy. Arch Orthop Trauma Surg. 2008;128(1):111–115. [DOI] [PubMed] [Google Scholar]
- 18. Han SB, Kyung HS, Seo IW, Shin YS. Better clinical outcomes after unicompartmental knee arthroplasty when comparing with high tibial osteotomy. Medicine (Baltimore). 2017;96(50):e9268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ho JC, Stitzlein RN, Green CJ, Stoner T, Froimson MI. Return to sports activity following UKA and TKA. J Knee Surg. 2016;29(3):254–259. [DOI] [PubMed] [Google Scholar]
- 20. Hollinghurst D, Stoney J, Ward T, et al. No deterioration of kinematics and cruciate function 10 years after medial unicompartmental arthroplasty. Knee. 2006;13(6):440–444. [DOI] [PubMed] [Google Scholar]
- 21. Hoorntje A, Witjes S, Kuijer PPFM, et al. High rates of return to sports activities and work after osteotomies around the knee: a systematic review and meta-analysis. Sports Med. 2017;47(11):2219–2244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hopper GP, Leach WJ. Participation in sporting activities following knee replacement: total versus unicompartmental. Knee Surg Sports Traumatol Arthrosc. 2008;16(10):973–979. [DOI] [PubMed] [Google Scholar]
- 23. Jackson JP, Waugh W. Tibial osteotomy for osteoarthritis of the knee. J Bone Joint Surg Br. 1961;43:746–751. [DOI] [PubMed] [Google Scholar]
- 24. Jassim SS, Douglas SL, Haddad FS. Athletic activity after lower limb arthroplasty: a systematic review of current evidence. Bone Joint J. 2014;96-B(7):923–927. [DOI] [PubMed] [Google Scholar]
- 25. Kayani B, Haddad FS. Robotic total knee arthroplasty: clinical outcomes and directions for future research. Bone Joint Res. 2019;8(10):438–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kayani B, Konan S, Pietrzak JRT, Haddad FS. Iatrogenic bone and soft tissue trauma in robotic-arm assisted total knee arthroplasty compared with conventional jig-based total knee arthroplasty: a prospective cohort study and validation of a new classification system. J Arthroplasty. 2018;33(8):2496–2501. [DOI] [PubMed] [Google Scholar]
- 27. Kayani B, Konan S, Tahmassebi J, et al. Robotic-arm assisted medial unicondylar knee arthroplasty versus jig-based unicompartmental knee arthroplasty with navigation control: study protocol for a prospective randomised controlled trial. Trials. 2020;21(1):721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kayani B, Konan S, Tahmassebi J, Rowan FE, Haddad FS. An assessment of early functional rehabilitation and hospital discharge in conventional versus robotic-arm assisted unicompartmental knee arthroplasty: a prospective cohort study. Bone Joint J. 2019;101-B(1):24–33. [DOI] [PubMed] [Google Scholar]
- 29. Koh YG, Lee JA, Chung HS, Kim HJ, Kang KT. Restoration of normal knee kinematics with respect to tibial insert design in mobile bearing lateral unicompartmental arthroplasty using computational simulation. Bone Joint Res. 2020;9(7):421–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Koh YG, Lee JA, Lee HY, et al. Reduction in tibiofemoral conformity in lateral unicompartmental knee arthroplasty is more representative of normal knee kinematics. Bone Joint Res. 2019;8(12):593–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Konings MJ, De Vroey H, Weygers I, Claeys K. Effect of knee arthroplasty on sports participation and activity levels: a systematic review and meta-analysis. BMJ Open Sport Exerc Med. 2020;6(1):e000729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Liddle AD, Pandit H, Judge A, Murray DW. Patient-reported outcomes after total and unicompartmental knee arthroplasty: a study of 14,076 matched patients from the National Joint Registry for England and Wales. Bone Joint J. 2015;97-B(6):793–801. [DOI] [PubMed] [Google Scholar]
- 33. Lo Presti M, Costa GG, Cialdella S. Return to sports after unicompartmental knee arthroplasty: reality or utopia? A 48-month follow-up prospective study. J Knee Surg. 2019;32(2):186–191. [DOI] [PubMed] [Google Scholar]
- 34. Maempel JF, Clement ND, Brenkel IJ, Walmsley PJ. Validation of a prediction model that allows direct comparison of the Oxford Knee Score and American Knee Society clinical rating system. Bone Joint J. 2015;97-B(4):503–509. [DOI] [PubMed] [Google Scholar]
- 35. McGrory BJ, Stuart MJ, Sim FH. Participation in sports after hip and knee arthroplasty: review of literature and survey of surgeon preferences. Mayo Clin Proc. 1995;70(4):342–348. [DOI] [PubMed] [Google Scholar]
- 36. Murray DW, Liddle AD, Liddle A, Dodd CA, Pandit H. Unicompartmental knee arthroplasty: is the glass half full or half empty? Bone Joint J. 2015;97-B(10)(suppl A):3–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Murray DW, Parkinson RW. Usage of unicompartmental knee arthroplasty. Bone Joint J. 2018;100-B(4):432–435. [DOI] [PubMed] [Google Scholar]
- 38. Naal FD, Fischer M, Preuss A, et al. Return to sports and recreational activity after unicompartmental knee arthroplasty. Am J Sports Med. 2007;35(10):1688–1695. [DOI] [PubMed] [Google Scholar]
- 39. National Joint Registry. The National Joint Registry 17th Annual Report 2020. https://reports.njrcentre.org.uk/Portals/0/PDFdownloads/NJR%2017th%20Annual%20Report%202020.pdf [PubMed]
- 40. Panzram B, Mandery M, Reiner T, et al. Fast return to sports and high level of activity after cementless Oxford unicompartmental knee arthroplasty. J Knee Surg. 2021;34(11):1212–1219. [DOI] [PubMed] [Google Scholar]
- 41. Pietschmann MF, Wohlleb L, Weber P, et al. Sports activities after medial unicompartmental knee arthroplasty Oxford III - what can we expect? Int Orthop. 2013;37(1):31–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Ponzio DY, Chiu YF, Salvatore A, et al. An analysis of the influence of physical activity level on total knee arthroplasty expectations, satisfaction, and outcomes: increased revision in active patients at five to ten years. J Bone Joint Surg Am. 2018;100(18):1539–1548. [DOI] [PubMed] [Google Scholar]
- 43. Robinson PG, Clement ND, Hamilton D, et al. A systematic review of robotic-assisted unicompartmental knee arthroplasty: prosthesis design and type should be reported. Bone Joint J. 2019;101-B(7):838–847. [DOI] [PubMed] [Google Scholar]
- 44. Santoso MB, Wu L. Unicompartmental knee arthroplasty, is it superior to high tibial osteotomy in treating unicompartmental osteoarthritis? A meta-analysis and systemic review. J Orthop Surg Res. 2017;12(1):50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Slim K, Nini E, Forestier D, et al. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. [DOI] [PubMed] [Google Scholar]
- 46. Stukenborg-Colsman C, Wirth CJ, Lazovic D, Wefer A. High tibial osteotomy versus unicompartmental joint replacement in unicompartmental knee joint osteoarthritis: 7-10-year follow-up prospective randomised study. Knee. 2001;8(3):187–194. [DOI] [PubMed] [Google Scholar]
- 47. Tew M, Waugh W. Tibiofemoral alignment and the results of knee replacement. J Bone Joint Surg Br. 1985;67(4):551–556. [DOI] [PubMed] [Google Scholar]
- 48. Wada K, Hamada D, Takasago T, et al. Native rotational knee kinematics is restored after lateral UKA but not after medial UKA. Knee Surg Sports Traumatol Arthrosc. 2018;26(11):3438–3443. [DOI] [PubMed] [Google Scholar]
- 49. Walker T, Gotterbarm T, Bruckner T, Merle C, Streit MR. Return to sports, recreational activity and patient-reported outcomes after lateral unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2015;23(11):3281–3287. [DOI] [PubMed] [Google Scholar]
- 50. Walker T, Streit J, Gotterbarm T, et al. Sports, physical activity and patient-reported outcomes after medial unicompartmental knee arthroplasty in young patients. J Arthroplasty. 2015;30(11):1911–1916. [DOI] [PubMed] [Google Scholar]
- 51. Walton NP, Jahromi I, Lewis PL, et al. Patient-perceived outcomes and return to sport and work: TKA versus mini-incision unicompartmental knee arthroplasty. J Knee Surg. 2006;19(2):112–116. [DOI] [PubMed] [Google Scholar]
- 52. Witjes S, Gouttebarge V, Kuijer PP, et al. Return to sports and physical activity after total and unicondylar knee arthroplasty: a systematic review and meta-analysis. Sports Med. 2016;46(2):269–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Wylde V, Blom A, Dieppe P, Hewlett S, Learmonth I. Return to sport after joint replacement. J Bone Joint Surg Br. 2008;90(7):920–923. [DOI] [PubMed] [Google Scholar]
- 54. Wylde V, Livesey C, Blom AW. Restriction in participation in leisure activities after joint replacement: an exploratory study. Age Ageing. 2012;41(2):246–249. [DOI] [PubMed] [Google Scholar]
- 55. Yang KY, Wang MC, Yeo SJ, Lo NN. Minimally invasive unicondylar versus total condylar knee arthroplasty-early results of a matched-pair comparison. Singapore Med J. 2003;44(11):559–562. [PubMed] [Google Scholar]