Abstract
Background:
Radiographic and cadaveric studies have suggested that anatomic anterior cruciate ligament reconstruction (ACLR) femoral tunnel drilling with the use of a flexible reaming system through an anteromedial portal (AM-FR) may result in a different graft and femoral tunnel position compared with using a rigid reamer through an accessory anteromedial portal with hyperflexion (AAM-RR). No prior studies have directly compared clinical outcomes between the use of these 2 techniques for femoral tunnel creation during ACLR.
Purpose:
To compare revision rates at a minimum of 2 years postoperatively for patients who underwent ACLR with AM-FR versus AAM-RR. The secondary objectives were to compare functional testing and patient-reported outcomes between the cohorts.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Included were consecutive patients at a single academic institution between 2013 and 2018 who underwent primary ACLR without additional ligamentous reconstruction. Patients were separated into 2 groups based on the type of anatomic femoral tunnel drilling: AM-FR or AAM-RR. Graft failure, determined by revision ACLR, was assessed with a minimum 2 years of postoperative follow-up. The authors also compared patient-reported outcome scores (International Knee Documentation Committee [IKDC] and Knee injury and Osteoarthritis Outcome Score [KOOS]) and functional performance testing performed at 6 months postoperatively.
Results:
A total of 284 (AAM-RR, 232; AM-FR, 52) patients were included. The mean follow-up time was 3.7 ± 1.5 years, with a minimum 2-year follow-up rate of 90%. There was no significant difference in the rate of revision ACLR between the AAM-RR and AM-FR groups (10.8% vs 9.6%, respectively; P = .806). At 6 months postoperatively, there were no significant between-group differences in peak knee extension strength, peak knee flexion strength, limb symmetry indices, or hop testing, as well as no significant differences in IKDC (AAM-RR, 81.1; AM-FR, 78.9; P = .269) or KOOS (AAM-RR, 89.0; AM-FR, 86.7; P = .104).
Conclusion:
In this limited study, independent femoral tunnel drilling for ACLR using rigid or flexible reaming systems resulted in comparable rates of revision ACLR at a minimum of 2 years postoperatively, with no significant differences in strength assessments or patient-reported outcomes at 6 months postoperatively.
Keywords: anterior cruciate ligament, ligament reconstruction, femoral tunnel, flexible reaming, rigid reaming; revision ACLR
While numerous controversies remain regarding the optimal surgical technique for or perioperative management of patients undergoing anterior cruciate ligament (ACL) reconstruction (ACLR), the position of the femoral and tibial tunnels is known to be of critical importance to outcome because of their effect on the resultant translational and rotational stability of the knee. 2,13 In particular, a malpositioned femoral tunnel is cited as being the most common cause of graft failure after surgery. 2,13,32 Despite recognition of this importance, it is acknowledged that there remains discrepancy between intended and achieved femoral tunnel position during ACLR. 23
Numerous studies have demonstrated that anatomic positioning of the femoral tunnel at the footprint of the native ACL more accurately re-creates the native knee kinematics and improves translational and rotational stability by better restoring graft tensioning throughout knee range of motion. 29,34,35 Specifically, femoral tunnel positioning that is too vertical in the coronal plane may lead to rotational instability, and positioning that is too anterior or posterior in the sagittal plane may inadequately restore the length-tension relationship of the native ACL. 29,34,35 As a result, there has been an increased emphasis placed on achieving anatomic positioning of the femoral tunnel over the last decade. 7,10,11,27,33 This emphasis on achieving anatomic tunnel placement has caused many surgeons to abandon transtibial (TT) femoral tunnel drilling in favor of less constrained or “independent” techniques for creating the femoral tunnel, as TT drilling has been repeatedly demonstrated to result in more vertical graft positioning and inferior rotational stability by comparison. 1,3,10,27
Several methods for independent femoral tunnel drilling exist, including the use of a rigid reamer through an accessory anteromedial portal with hyperflexion (AAM-RR) or via an outside-in drilling technique and the use of flexible reaming systems through a standard anteromedial portal (AM-FR). 10 Most existing studies evaluating clinical outcomes after ACLR have grouped AAM-RR and AM-FR together as “independent femoral tunnel drilling,” despite several technical differences in their use. 11,21,22 AAM-RR requires hyperflexion of the knee to 120°, which can be challenging in revision ACLR or depending on a patient’s intrinsic flexibility, musculature, and body habitus. 21,22 Additionally, the placement of the anteromedial portal itself relative to the patient’s femoral notch anatomy can constrain the ability to anatomically re-create the femoral tunnel relative to the ACL footprint when using an inflexible guide and reamer. 10,21,22,27
More recent radiographic and cadaveric studies have suggested that these technical differences may result in AM-FR producing a more radiographically anatomic ACL graft position; longer, more anteverted femoral tunnels; and a theoretically decreased likelihood of posterior wall breakage or damage to posterolateral knee structures. ‡ To date, however, no studies have directly compared clinical outcomes between the use of AAM-RR and AM-FR for femoral tunnel creation.
The primary objective of this study was to compare revision ACLR rates at a minimum of 2 years postoperatively for patients undergoing ACLR between the AAM-RR and AM-FR femoral tunnel drilling techniques. The secondary objectives were to compare functional testing and 6-month postoperative patient-reported outcome scores between the 2 techniques. We hypothesized that there would be no difference in revision ACLR rates between the 2 techniques.
Methods
This retrospective cohort study was approved by the academic center’s institutional review board. A total of 316 consecutive patients who underwent ACLR at a single academic institution between March 2013 and August 2018 were evaluated. All eligible patients underwent surgery performed by 1 of 6 attending orthopaedic surgeons at a single institution, all of whom are fellowship trained in orthopaedic sports medicine. Retrospective chart review was performed to evaluate patients for study inclusion. Operative notes were evaluated to identify the surgical technique and reaming system used for femoral tunnel creation during ACLR. Choice of femoral tunnel drilling was by surgeon preference and did not change during the study period. Two surgeons performed exclusively rigid reaming, and the remaining 4 surgeons performed flexible reaming.
Included in the study were patients who underwent a primary ACLR without additional ligamentous reconstruction. Patients were excluded from final analysis of revision ACLR if they underwent any additional ligamentous reconstruction or if they had <2 years of postoperative follow-up. Patients without Lower Extremity Assessment Protocol (LEAP) testing were also excluded. LEAP testing is a standard part of the treatment and rehabilitation recommendation for all patients undergoing ACLR at our institution. The patients excluded for this reason represented a very small portion of the overall cases, as it was deemed standard of care for ACLR at the beginning of this study. All patients provided informed consent.
The primary outcome measure was graft rupture, which was identified via retrospective chart review to determine whether the patient had undergone a revision ACLR. When graft integrity beyond 2 years postoperatively was not able to be confirmed via chart review, the patient was contacted via telephone to determine whether or not revision ACLR had occurred. It can be assumed that both groups had a similar likelihood of undergoing revision within the minimum 2-year follow-up period, minimizing detection bias between groups.
The secondary outcome measures were examined by assessing functional performance per LEAP testing, which consisted of a battery of testing that directly evaluated the operative limb and the noninjured, contralateral side. These tests were performed at 6 months postoperatively for all included patients.
Lower Extremity Assessment Protocol
The LEAP at our institution consists of 3 parts: recording of patient-reported outcomes, measurement of flexion and extension strength, and hop testing.
Patient-Reported Outcomes
Upon enrollment, all participants completed the International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form and the Knee injury and Osteoarthritis Outcome Score (KOOS). The IKDC and KOOS are both well-established and validated patient-reported outcome scoring systems designed to assess patients' knee symptoms and function based on their pain, performance, quality of life, and activity level. 4,24
Knee Flexion and Extension Strength
Isokinetic, concentric knee extension and flexion strength was measured bilaterally using a Biodex Systems 4 multimode dynamometer (Biodex Medical Systems, Inc) at a speed of 90 deg/s. All testing was performed on the uninvolved limb, followed by testing of the involved limb. The participants completed practice trials on each limb for practice and familiarization. The participants provided maximal effort through their full range of motion for 8 trials. Measures of peak torque for knee extension and flexion were exported using the Biodex software and normalized to the participant’s body mass (N·m/kg). Symmetry measures were calculated as a ratio between the reconstructed limb and the contralateral limb and expressed as a percentage of the contralateral limb, where 100% indicated perfect symmetry.
Hop Testing
Each participant performed 4 single-leg hopping trials on each limb. Hop tests included single hop for maximal distance where participants were instructed to perform a single-hop straight forward as far as possible with a balanced on the landing (single hop). Participants also performed 3 consecutive hops in a straight line for maximal distance (triple hop) and 3 consecutive hops in a zigzag pattern for maximal distance. Finally, participants performed a timed hop where they were instructed to hop as quickly as possible for 6 m. Distances were measured in centimeters, time was measured in seconds, and symmetry was expressed as a percentage of the contralateral limb, as described.
Statistical Analysis
A post hoc power analysis was performed to determine the number of patients necessary to determine a significant difference in revision ACLR rates. To determine a 5% difference in the incidence of revision ACLR between the 2 groups, assuming an even distribution of patients in each group, alpha of .05, and 80% power, a total of 868 patients would be necessary. As this was a sample of opportunity with fewer patients available, a risk of underpowering was present.
Descriptive statistics, including mean, standard deviation, median, minimum, and maximum values, were calculated for all quantitative variables. Comparison of categorical data was performed using chi-square and Fisher exact tests for comparisons with small sample sizes. Comparisons of continuous data were performed using the Student t test for those that were normally distributed and the Mann-Whitney test as a nonparametric alternative for those that were not normally distributed. Statistical analyses were performed using IBM SPSS Statistics Version 26 (IBM Corp). For all comparisons, P < .05 was considered statistically significant.
Results
Cohort Characteristics
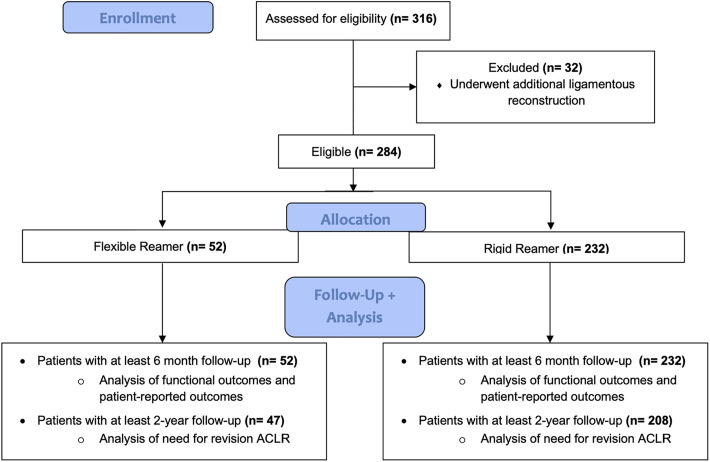
A total of 284 patients were identified for inclusion to this study, with 232 patients undergoing femoral tunnel creation using AAM-RR and 52 using AM-FR (Figure 1). The overall mean follow-up time was 3.7 ± 1.5 years. The mean follow-up time was significantly different between groups (AAM-RR, 4.0 ± 1.5 years; AM-FR, 2.5 ± 0.7 years; P < .001). Two-year follow-up was confirmed in 89.8% of patients overall. All data were present for all included patients, except for identification of minimum 2-year revision ACLR in patients without confirmed follow-up beyond 2 years.
Figure 1.
A flowchart of the study participants assessed for eligibility and determination of inclusion for final analysis. ACLR, anterior cruciate ligament reconstruction.
The flexible reamer and rigid reamer groups did not differ with regard to mean age, sex, body mass index (BMI), or patients who underwent concomitant surgical intervention on the meniscus (Table 1). Groups did differ significantly with regard to graft type, with 61.2% of patients in the AAM-RR group receiving a bone–patellar tendon–bone graft versus 76.9% of patients in the AM-FR group (P = .033). All other patients included in this analysis received a hamstring tendon graft.
TABLE 1.
Patient Characteristics a
| Overall (N = 284) | Flexible Reamer (n = 52) | Rigid Reamer (n = 232) | P | |
|---|---|---|---|---|
| Age, y | 21.6 ± 9.5 | 22.3 ± 9.1 | 21.5 ± 9.6 | .584 |
| Female sex | 157 (55.3) | 27 (51.9) | 130 (56.0) | .590 |
| BMI | 24.8 ± 4.6 | 25.4 ± 4.4 | 24.7 ± 4.6 | .318 |
| Graft type, BTB:HS, n | 182:102 | 40:12 | 142:90 | .033 |
| Meniscectomy | 84 (29.6) | 12 (23.1) | 72 (31.0) | .256 |
| Meniscal repair | 124 (43.7) | 18 (34.6) | 106 (45.7) | .211 |
| Timing of LEAP, mo | 6.7 ± 2.3 | 6.2 ± 2.1 | 6.8 ± 2.5 | .109 |
| Follow-up, y | 3.7 ± 1.5 | 2.5 ± 0.7 | 4.0 ± 1.5 | <.001 |
a Data are reported as mean ± SD or n (%) unless otherwise indicated. Bolded P values indicate a statistically significant difference between the study groups (P < .05). BMI, body mass index; BTB, bone–patellar tendon–bone; HS, hamstring; LEAP, Lower Extremity Assessment Protocol.
Revision ACLR Rate
With regard to the primary outcome of interest, there was no significant difference observed in the rate of revision ACLR between the use of AAM-RR and AM-FR for femoral tunnel creation during ACLR (AM-FR, 9.6%; AAM-RR, 10.8%; P = .806) (Table 2). The revision ACLR rate was also compared at 2.5 years postoperatively in both cohorts and was similarly not found to be significantly different (AM-FR, 9.1%; AAM-RR, 8.6%).
TABLE 2.
Outcome Comparisons Between the Study Groups a
| Overall | Flexible Reamer | Rigid Reamer | P | |
|---|---|---|---|---|
| Primary outcome | ||||
| Revision ACLR rate | 30 (10.6) | 5 (9.6) | 25 (10.8) | .806 |
| Extension measures | ||||
| Normalized peak extension torque of 90° | 1.55 ± 0.47 | 1.47 ± 0.47 | 1.57 ± 0.46 | .159 |
| LSI extension, % | 69.5 ± 17.3 | 65.7 ± 17.2 | 70.3 ± 17.2 | .126 |
| Flexion measures | ||||
| Normalized peak flexion torque of 90° | 0.90 ± 0.27 | 0.89 ± 0.29 | 0.90 ± 0.27 | .812 |
| LSI flexion, % | 93.1 ± 18.0 | 90.0 ± 19.6 | 93.8 ± 17.6 | .157 |
| Hop tests, % | ||||
| LSI single hop | 89.0 ± 13.0 | 89.2 ± 14.5 | 88.9 ± 12.6 | .989 |
| LSI triple hop | 91.7 ± 11.1 | 91.4 ± 10.3 | 91.8 ± 11.2 | .814 |
| LSI timed hop | 108.3 ± 22.5 | 108.5 ± 17.9 | 108.3 ± 23.3 | .954 |
| PRO scores at 6 mo | ||||
| IKDC | 80.7 ± 13.0 | 78.9 ± 11.7 | 81.1 ± 13.2 | .269 |
| KOOS | 88.6 ± 9.2 | 86.7 ± 8.6 | 89.0 ± 9.3 | .104 |
a Data are reported as mean ± SD or n (%). ACLR, anterior cruciate ligament reconstruction; IKDC, International Knee Documentation Committee; LSI, limb symmetry index; KOOS, Knee injury and Osteoarthritis Outcome Score; PRO, patient-reported outcome.
LEAP and Patient-Reported Outcome Measures
Additionally, there were no significant differences found in 6-month knee extension strength and symmetry, knee flexion strength and symmetry, or hop testing between cohorts (Table 2). Additionally, no significant differences existed in mean IKDC score (AAM-RR, 81.1; AM-FR, 78.9; P = .269) or KOOS (AAM-RR, 89.0; AM-FR, 86.7; P = .104) between the use of AAM-RR and AM-FR for femoral tunnel creation (Table 2). There were no reported occurrences of posterior wall breakage or injuries to the posterolateral ligamentous or neurovascular structures in either group.
Discussion
The most important finding of this study was that the choice between AAM-RR and AM-FR did not result in a significant difference in revision ACLR rates at a minimum of 2 years postoperatively in this study. Additionally, no differences were found in functional testing or patient-reported outcomes at 6 months postoperatively. While radiographic and cadaveric studies have suggested that using AM-FR may result in a more anatomic ACL graft position with longer and more anteverted tunnels when compared with AAM-RR, this should only affect graft tunnel mismatch and not revision ACLR rates. §
The use of AM-FR and AAM-RR has historically not been subdivided when comparing outcomes among various methods for femoral tunnel creation. Recently, however, several studies have suggested that AM-FR may result in a different ACL graft and femoral tunnel position compared with AAM-RR. A study by Jamsher et al 11 compared sagittal and coronal graft inclination angles on magnetic resonance imaging scans in patients in whom ACLR was performed using AM-FR and AAM-RR and compared measurements to healthy controls. Those authors found that the sagittal graft inclination was significantly different between the AAM-RR (56.0° ± 6.1°) group and the healthy control group (49.3° ± 4.2°) but was not different between the AM-FR group (49.9° ± 5.0°) and the control group. 11 Additionally, the mean angle reported for the AAM-RR group in that study fell outside the anatomic range validated by Illingworth et al, 9 suggesting that AAM-RR resulted in tunnel placement outside of an anatomic range. 11 Other studies by Steiner et al, 27 Wein et al, 31 and Larson et al 17 have similarly found that AAM-RR results in a more vertical position of the femoral tunnel compared with AM-FR.
There is also evidence to suggest that the decreased constraint arising from using a flexible reamer in comparison with a rigid reamer may allow for longer femoral tunnels to be created while also placing tunnels at a greater distance from critical posterolateral knee structures. 8,12,14,16,26,28,31 These differences in tunnel length are even more pronounced when the knee is placed in lesser degrees of flexion for femoral tunnel creation. 5,8,14 Collectively, these findings suggest that the differences in technical constraint between the 2 techniques may result in a varying ability to anatomically re-create the ACL and therefore clinically affect knee kinematics and function, which could manifest in differing rates of revision ACLR.
Despite the aforementioned radiologic and anatomic differences reported, we found no difference in revision ACLR rates at a minimum of 2 years postoperatively or early outcomes between flexible and rigid reaming systems for independent femoral tunnel creation during ACLR. The revision ACLR rates reported at the final follow-up were similar in the AM-FR group (9.6%) and the AAM-RR group (10.8%). Because of the significantly longer mean follow-up time in the AAM-RR group, the revision ACLR rate was also compared at 2.5 years postoperatively in both cohorts and was similarly not found to be significantly different (AM-FR, 9.1%; AAM-RR, 8.6%). This finding of clinical equivalence with regard to revision ACLR rates, performance testing, and patient-reported outcomes is an important addition to the literature, as there are no previous studies that have directly compared revision ACLR rates or other clinical outcomes between the use of AM-FR and AAM-RR. Interestingly, while more anatomic graft positioning has consistently been demonstrated to improve knee kinematics and rotational stability, this has not always been demonstrated to translate into improved clinical outcomes.
A cohort study of 17,682 overall patients by Desai et al 6 that was published in 2017 using data from the Swedish National Knee Ligament Register found that nonanatomic femoral tunnel placement via TT drilling resulted in a decreased risk of need for revision surgery compared with anatomic tunnel placement via transportal drilling. Another prospective study composed of data from the Danish Knee Ligament Reconstruction Register including 1945 and 6430 ACLR procedures performed either from an independent anteromedial portal or via TT drilling, respectively, found a greater risk of needing revision ACLR in the anteromedial cohort. 20 One explanation for this finding is that transportal femoral tunnel drilling may result in a higher graft bending angle compared with TT drilling, therefore leading to increased stress on the bone-graft interface. 30 Other studies have contradicted this finding, however. 14,30 Given the discordance between these database studies and the biomechanical analyses, further large, prospective, randomized studies are warranted to better understand the effect of these techniques on biomechanical and clinical outcome.
Limitations
The methodology of this study has several limitations that may affect the findings. First, this study was underpowered, and a significant possibility of type 2 error exists. It was a sample of opportunity, and unfortunately the power cannot be improved. Second, its retrospective nature introduces the possibility that there exist confounding factors that were not adequately controlled between groups. One variable that differed between the groups is mean follow-up, which was significantly longer in the AAM-RR group, as this technique was used before AM-FR. This could potentially bias the results to have a greater incidence of failure in the AAM-RR group. There are additional factors that have been demonstrated to affect incidence of ACL graft failure postoperatively, such as graft size or patient activity level. The study groups were similar with regard to age, sex, BMI, and incidence of concomitant meniscal repair, however, which is suggestive that many potential patient and surgical characteristics may also have been relatively equivalent between groups.
Although there was a significant difference between groups with regard to graft type, prior study has not shown a difference in revision ACLR rates between bone–patellar tendon–bone and hamstring tendon grafts according to a much larger meta-analysis. 25 While all included patients underwent primary ACLR without concomitant ligamentous reconstruction, it is important to highlight that no significant difference in incidence of meniscal repair existed between groups. At our institution, patients undergoing concomitant meniscal repair are managed with a different rehabilitation protocol than are patients undergoing ACLR without meniscal repair. The study cohorts also differed with regard to size. This discrepancy existed based on the preferred surgical technique of the respective surgeons at our institution, which also may have introduced bias. It remains unclear how having less disparate cohort sizes would have affected our results; however, given the minimal differences in the outcomes observed in this study, there would need to be significantly more included patients in order to detect any significant difference.
Another limitation of this study is that while previous literature 18 exists to suggest that ACLR using AM-FR for femoral tunnel trends toward resulting in a more anatomic ACLR, this study lacks direct radiologic evidence that this difference manifested within our study population. Finally, as a literature review 18 shows that the radiologic and anatomic differences resulting from AM-FR and AAM-RR are more evident when deep flexion is unable to be achieved, it is possible that there would have been a difference observed in patients with less intrinsic flexibility, such as patients who are more muscular or have larger body habitus. This study is more representative of the overall population undergoing ACLR, however, and is therefore more translatable than isolated subgroup analysis based on revision procedures or a certain population characteristic.
Despite these limitations, the novelty and clinical significance of the findings in this study make it an important addition to the literature. Further, the validity of the study is strengthened by its mean follow-up time of 3.7 years, with an overall 2-year follow-up of 90.8%. This excellent follow-up time and incidence greatly decreases the possibility that not capturing the incidence of revision ACLR would have affected the findings of the study. Additionally, the use of both structured performance testing and validated patient-reported outcome scores reinforces this study’s finding that no significant differences in clinical functional outcome arose based on the choice of flexible versus rigid reamers for ACLR.
Conclusion
In this limited study, independent femoral tunnel drilling for ACLR using rigid or flexible reaming systems resulted in comparable rates of revision ACLR at a minimum of 2 years postoperatively and no significant differences in strength assessments or patient-reported outcomes at 6 months postoperatively.
Footnotes
Final revision submitted November 30, 2021; accepted December 8, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: T.E.M. has received royalties from Zimmer Biomet. J.M.H. has received research support from DJO and royalties from Elsevier and has stock/stock options in Springbok. B.C.W. has received research support from Arthrex, Biomet, Integra LifeSciences, and Flexion Therapeutics and consulting and speaking fees from Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the University of Virginia (reference No. 17399).
References
- 1. Arnold MP, Kooloos J, van Kampen A. Single-incision technique misses the anatomical femoral anterior cruciate ligament insertion: a cadaver study. Knee Surg Sports Traumatol Arthrosc. 2001;9(4):194–199. doi:10.1007/s001670100198 [DOI] [PubMed] [Google Scholar]
- 2. Carson EW, Anisko EM, Restrepo C, Panariello RA, O’Brien SJ, Warren RF. Revision anterior cruciate ligament reconstruction: etiology of failures and clinical results. J Knee Surg. 2004;17(3):127–132. doi:10.1055/s-0030-1248210 [DOI] [PubMed] [Google Scholar]
- 3. Chang CB, Yoo JH, Chung BJ, Seong SC, Kim TK. Oblique femoral tunnel placement can increase risks of short femoral tunnel and cross-pin protrusion in anterior cruciate ligament reconstruction. Am J Sports Med. 2010;38(6):1237–1245. doi:10.1177/0363546509357608 [DOI] [PubMed] [Google Scholar]
- 4. Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM. Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee injury and Osteoarthritis Outcome Score (KOOS), Knee injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res (Hoboken). 2011;63(suppl 11):S208–S228. doi:10.1002/acr.20632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dave LY, Nyland J, Caborn DN. Knee flexion angle is more important than guidewire type in preventing posterior femoral cortex blowout: a cadaveric study. Arthroscopy. 2012;28(10):1381–1387. doi:10.1016/j.arthro.2012.03.008 [DOI] [PubMed] [Google Scholar]
- 6. Desai N, Andernord D, Sundemo D, et al. Revision surgery in anterior cruciate ligament reconstruction: a cohort study of 17,682 patients from the Swedish National Knee Ligament Register. Knee Surg Sports Traumatol Arthrosc. 2017;25(5):1542–1554. doi:10.1007/s00167-016-4399-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fitzgerald J, Saluan P, Richter DL, Huff N, Schenck RC. Anterior cruciate ligament reconstruction using a flexible reamer system: technique and pitfalls. Orthop J Sports Med. 2015;3(7):23259 67115592875. doi:10.1177/2325967115592875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Forsythe B, Collins MJ, Arns TA, et al. Optimization of anteromedial portal femoral tunnel drilling with flexible and straight reamers in anterior cruciate ligament reconstruction: a cadaveric 3-dimensional computed tomography analysis. Arthroscopy. 2017;33(5):1036–1043. doi:10.1016/j.arthro.2016.11.004 [DOI] [PubMed] [Google Scholar]
- 9. Illingworth KD, Hensler D, Working ZM, Macalena JA, Tashman S, Fu FH. A simple evaluation of anterior cruciate ligament femoral tunnel position: the inclination angle and femoral tunnel angle. Am J Sports Med. 2011;39(12):2611–2618. doi:10.1177/0363546511420128 [DOI] [PubMed] [Google Scholar]
- 10. Irarrázaval S, Kurosaka M, Cohen MFF. Anterior cruciate ligament reconstruction. J ISAKOS. 2016;1:38–52. doi:10.1136/jisakos-2015-000001 [Google Scholar]
- 11. Jamsher M, Ballarati C, Viganò M, et al. Graft inclination angles in anterior cruciate ligament reconstruction vary depending on femoral tunnel reaming method: comparison among transtibial, anteromedial portal, and outside-in retrograde drilling techniques. Arthroscopy. 2020;36(4):1095–1102. doi:10.1016/j.arthro.2019.09.040 [DOI] [PubMed] [Google Scholar]
- 12. Kadija M, Milovanović D, Bumbaširević M, Carević Z, Dubljanin-Raspopović E, Stijak L. Length of the femoral tunnel in anatomic ACL reconstruction: comparison of three techniques. Knee Surg Sports Traumatol Arthrosc. 2017;25(5):1606–1612. doi:10.1007/s00167-015-3670-0 [DOI] [PubMed] [Google Scholar]
- 13. Kamath GV, Redfern JC, Greis PE, Burks RT. Revision anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39(1):199–217. doi:10.1177/0363546510370929 [DOI] [PubMed] [Google Scholar]
- 14. Kim JG, Chang MH, Lim HC, et al. An in vivo 3D computed tomographic analysis of femoral tunnel geometry and aperture morphology between rigid and flexible systems in double-bundle anterior cruciate ligament reconstruction using the transportal technique. Arthroscopy. 2015;31(7):1318–1329. doi:10.1016/j.arthro.2015.01.021 [DOI] [PubMed] [Google Scholar]
- 15. Kim NK, Kim JM. The three techniques for femoral tunnel placement in anterior cruciate ligament reconstruction: transtibial, anteromedial portal, and outside-in techniques. Arthrosc Orthop Sports Med. 2015;2(2):77–85. doi:10.14517/aosm14021 [Google Scholar]
- 16. Kosy JD, Walmsley K, Anaspure R, Schranz PJ, Mandalia VI. Flexible reamers create comparable anterior cruciate ligament reconstruction femoral tunnels without the hyperflexion required with rigid reamers: 3D-CT analysis of tunnel morphology in a randomised clinical trial. Knee Surg Sports Traumatol Arthrosc. 2020;28(6):1971–1978. doi:10.1007/s00167-019-05709-7 [DOI] [PubMed] [Google Scholar]
- 17. Larson AI, Bullock DP, Pevny T. Comparison of 4 femoral tunnel drilling techniques in anterior cruciate ligament reconstruction. Arthroscopy. 2012;28(7):972–979. doi:10.1016/j.arthro.2011.12.015 [DOI] [PubMed] [Google Scholar]
- 18. Moran TE, Ignozzi AJ, Werner BC. Comparing the use of flexible and rigid reaming systems through an anteromedial portal for femoral tunnel creation during anterior cruciate ligament reconstruction: A systematic review. Orthop J Sports Med. 2021;9(10):23259671211035741. doi:10.1177/23259671211035741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Muller B, Hofbauer M, Atte A, van Dijk CN, Fu FH. Does flexible tunnel drilling affect the femoral tunnel angle measurement after anterior cruciate ligament reconstruction? Knee Surg Sports Traumatol Arthrosc. 2015;23(12):3482–3486. doi:10.1007/s00167-014-3181-4 [DOI] [PubMed] [Google Scholar]
- 20. Rahr-Wagner L, Thillemann TM, Pedersen AB, Lind MC. Increased risk of revision after anteromedial compared with transtibial drilling of the femoral tunnel during primary anterior cruciate ligament reconstruction: results from the Danish Knee Ligament Reconstruction Register. Arthroscopy. 2013;29(1):98–105. doi:10.1016/j.arthro.2012.09.009 [DOI] [PubMed] [Google Scholar]
- 21. Robin BN. Editorial commentary: is it time to make a change? Don’t throw out the old rigid anterior cruciate ligament femoral reamers just yet. Arthroscopy. 2020;36(4):1103–1104. doi:10.1016/j.arthro.2020.01.055 [DOI] [PubMed] [Google Scholar]
- 22. Robin BN, Jani SS, Marvil SC, Reid JB, Schillhammer CK, Lubowitz JH. Advantages and disadvantages of transtibial, anteromedial portal, and outside-in femoral tunnel drilling in single-bundle anterior cruciate ligament reconstruction: a systematic review. Arthroscopy. 2015;31(7):1412–1417. doi:10.1016/j.arthro.2015.01.018 [DOI] [PubMed] [Google Scholar]
- 23. Robinson J, Inderhaug E, Harlem T, Spalding T, Brown CH. Anterior cruciate ligament femoral tunnel placement: an analysis of the intended versus achieved position for 221 international high-volume ACL surgeons. Am J Sports Med. 2020;48(5):1088–1099. doi:10.1177/0363546520906158 [DOI] [PubMed] [Google Scholar]
- 24. Roos EM, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1:64. doi:10.1186/1477-7525-1-64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Samuelsen BT, Webster KE, Johnson NR, Hewett TE, Krych AJ. Hamstring autograft versus patellar tendon autograft for ACL reconstruction: is there a difference in graft failure rate? A meta-analysis of 47,613 patients. Clin Orthop Relat Res. 2017;475(10):2459–2468. doi:10.1007/s11999-017-5278-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Silver AG, Kaar SG, Grisell MK, Reagan JM, Farrow LD. Comparison between rigid and flexible systems for drilling the femoral tunnel through an anteromedial portal in anterior cruciate ligament reconstruction. Arthroscopy. 2010;26(6):790–795. doi:10.1016/j.arthro.2009.10.012 [DOI] [PubMed] [Google Scholar]
- 27. Steiner ME, Battaglia TC, Heming JF, Rand JD, Festa A, Baria M. Independent drilling outperforms conventional transtibial drilling in anterior cruciate ligament reconstruction. Am J Sports Med. 2009;37(10):1912–1919. doi:10.1177/0363546509340407 [DOI] [PubMed] [Google Scholar]
- 28. Steiner ME, Smart LR. Flexible instruments outperform rigid instruments to place anatomic anterior cruciate ligament femoral tunnels without hyperflexion. Arthroscopy. 2012;28(6):835–843. doi:10.1016/j.arthro.2011.11.029 [DOI] [PubMed] [Google Scholar]
- 29. Sukur E, Akman YE, Senel A, Unkar EA, Topcu HN, Ozturkmen AY. Comparing transtibial and anteromedial drilling techniques for single-bundle anterior cruciate ligament reconstruction. Open Orthop J. 2016;10:481–489. doi:10.2174/1874325001610010481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Tashiro Y, Sundaram V, Thorhauer E, et al. In vivo analysis of dynamic graft bending angle in anterior cruciate ligament-reconstructed knees during downward running and level walking: comparison of flexible and rigid drills for transportal technique. Arthroscopy. 2017;33(7):1393–1402. doi:10.1016/j.arthro.2017.01.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wein F, Osemont B, Goetzmann T, et al. Anteversion and length of the femoral tunnel in ACL reconstruction: in-vivo comparison between rigid and flexible instrumentation. J Exp Orthop. 2019;6(1):26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wright RW MARS Group, Huston LJ, et al. Descriptive epidemiology of the Multicenter ACL Revision Study (MARS) cohort. Am J Sports Med. 2010;38(10):1979–1986. doi:10.1177/0363546510378645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Yoon KH, Kim JH, Kwon YB, Kim EJ, Lee SH, Kim SG. A two-portal technique using a flexible reamer system is a safe and effective method for transportal anterior cruciate ligament reconstruction. Arch Orthop Trauma Surg. 2020;140(3):383–390. doi:10.1007/s00402-020-03343-4 [DOI] [PubMed] [Google Scholar]
- 34. Zavras TD, Race A, Amis AA. The effect of femoral attachment location on anterior cruciate ligament reconstruction: graft tension patterns and restoration of normal anterior-posterior laxity patterns. Knee Surg Sports Traumatol Arthrosc. 2005;13(2):92–100. doi:10.1007/s00167-004-0541-5 [DOI] [PubMed] [Google Scholar]
- 35. Zhang Q, Zhang S, Li R, Liu Y, Cao X. Comparison of two methods of femoral tunnel preparation in single-bundle anterior cruciate ligament reconstruction: a prospective randomized study. Acta Cir Bras. 2012;27(8):572–576. doi:10.1590/s0102-86502012000800010 [DOI] [PubMed] [Google Scholar]