Abstract
Context
Mindfulness practices are effective for injury or illness recovery, decreasing stress and anxiety, and strengthening emotional resilience. They are also beneficial for health care professionals' wellbeing and improving patient outcomes and safety. However, mindfulness has not been studied in athletic trainers.
Objective
To investigate athletic trainers' use of mindfulness practices and their perceptions of its importance for self-care and patient or client care.
Design
Cross-sectional study.
Setting
All athletic training practice settings.
Patients and Other Participants
A total of 547 athletic trainers who were currently practicing completed the survey.
Main Outcome Measure(s)
We developed an 18-item survey that measured use (1 = never to 6 = very frequently) and perceptions (1 = strongly disagree to 7 = strongly agree) of mindfulness practices. Mann-Whitney U or Kruskal-Wallis tests with post hoc pairwise comparisons were performed to assess differences in use (P < .05). A related-samples Wilcoxon signed rank test was calculated to assess differences in participants' perceptions between self-care and patient or client care.
Results
Overall, 86% (n = 471) of respondents reported involvement in some form of mindfulness practice, with females (median [interquartile range] = 4 [2–5] versus males: 3 [2–4]; P < .002), those not in a committed relationship (4 [2–5] versus those in such a relationship: 3 [2–4]; P = .048), and those without children in the home (4 [2–5] versus those with children in the home: 3 [2–4]; P = .040) describing the highest frequency of use for self-care. Females (4 [2–4] versus males: 3 [2–4]; P < .001), those without children in the home (3 [2–4] versus those with children in the home: 3 [2–4]; P = .036), and those in emerging (4 [2–4]; P = .003) or collegiate (3 [2–4]; P = .006) settings most frequently incorporated mindfulness into patient or client care. Overall frequency of use for self-care was higher than for patient or client care (4 = occasionally [2–4] versus 3 = rarely [2–4]; P < .001). Mindfulness practices were perceived as more important for self-care than for patient or client care (6 [5–7] versus 5 [5–6]; P < .001).
Conclusions
Athletic trainers perceived mindfulness practices as more important for personal wellbeing and used them, albeit occasionally, more for self-care than for patient or client care. Differences in gender, relationship status, children, and setting were observed. Mindfulness-based interventions for athletic trainer wellbeing and patient-centered care and implementation barriers should be explored.
Keywords: complementary health, meditation, occurrence, attitudes
Key Points
Athletic trainers used mindfulness practices more frequently for self-care than for patient or client care but only occasionally for the former and rarely for the latter.
Athletic trainers perceived mindfulness practices as important yet more for self-care than for patient or client care.
Participants who identified as female, those who were not in a committed relationship, and those with no children living in the home reported the highest use of mindfulness practices for self-care, while those in the collegiate and emerging settings incorporated these practices more frequently in patient or client care.
The concept of mindfulness originated from Buddhism in fifth century BCE and became prominent in the West in the 1980s.1 This movement was led by Jon Kabat-Zinn, a molecular biologist who founded the now world-renowned Mindfulness-Based Stress Reduction (MBSR) Clinic in 1979. For decades, Kabat-Zinn and colleagues researched various mind-body interactions for healing, including the first studies on the impact of an MBSR program on chronic pain. According to Kabat-Zinn, mindfulness is “the awareness that arises through paying attention on purpose, in the present moment, and nonjudgmentally to the unfolding of experience moment by moment.”1(p12) This greater sense of awareness and wellbeing is perceived to have mental and physical impacts. Kabat-Zinn focused on the importance of the “mind-body connection” and the belief that mental and emotional health can have a significant positive or negative effect on our physical health, including one's capacity for recovering from illness and injury.1
Mindfulness practices have been incorporated into diverse environments, including business,1 athletics,2 and health care.3 Techniques used to achieve and maintain this mind-body connection vary. Some of the most common practices are meditation, MBSR courses, mindfulness-based cognitive therapy, metacognition techniques, progressive relaxation, breathing and body-scanning techniques, and mind-body exercise activities such as yoga, tai chi, and qigong.4 Mindfulness is now considered a form of complementary health that integrates unconventional or alternative medicine with mainstream Western medicine to achieve holistic health and wellness.5
Interest in the concept of mindfulness has grown exponentially worldwide, and scientific interest in mindfulness practices has surged in the last 2 decades. Although the quality of evidence is still improving, the research suggests that mindfulness practices can be effective for many illnesses and disorders, including chronic pain, depression, and anxiety,3 and for fostering emotional resilience and empathy, strengthening coping strategies, and decreasing stress.6 Specifically in the realms of athletics and sports medicine, investigators7,8 have demonstrated positive effects of mindfulness practices on athletic and academic performance, as well as reductions in stress, burnout, and injury rates. A meta-analysis7 of the effects of mindfulness-based interventions (eg, meditation, yoga, and breathing or relaxation techniques) on sports performance demonstrated the potential for these practices to improve athletic and physical outcome measures, especially in precision sports, and decrease psychological stress. Bühlmayer et al7 proposed that mindfulness may positively affect motor learning at multiple developmental stages in novice- to elite-level athletes. Moen et al8 found that elite youth athletes' degrees of mindfulness were positively correlated with their performance in academics and various sports, and mindfulness served as a buffer to stress and early burnout.
Mindfulness practices may also help prevent injuries, decrease the time lost to injury, and improve overall wellbeing in high school and collegiate athletes9 and elite soccer players.10,11 Notably, Naderi et al11 determined that mindfulness training was twice as likely to reduce the acute injury risk than no mindfulness training. Also, preliminary evidence12 showed that MBSR courses may increase pain tolerance, and awareness, and improve mental health in injured athletes.
Health care professionals face challenges in their home and work environments that can be detrimental to their physical and mental wellbeing13 and lead to compassion fatigue.14 Mindfulness practices have been associated with positive outcomes for health care professionals in regard to burnout,13–15 anxiety,13,15 and stress.15–18 Researchers19,20 suggested that the health care professional's personal use of mindfulness practices fosters empathy, compassion, and enhanced communication, which can thereby improve patient outcomes. Mindfulness has been proposed as essential to professional competence because it reduces the clinician's psychological distress and promotes greater regulation of emotions, resulting in clearer decision making and fewer medical errors.21 Although health care degree programs have incorporated mindfulness into their curricula,22,23 barriers such as time limitations and perceived knowledge have made the implementation of mindfulness techniques and programs in routine clinical practice challenging.15,24 Evidence of the efficacy and importance of mindfulness practices and its health benefits continues to increase, yet the integration into health care systems appears to lag.25
The most comprehensive data examining general use of mindfulness practices in the United States come from the Centers for Disease Control and Prevention's National Health Interview Survey (NHIS).5 Since 2002, these data have provided insight into patterns and sociodemographic characteristics of mindfulness users. Simonsson et al,4 in a recent analysis of the 2017 NHIS data, showed that, during the 12 months before the survey, 5% of adults, or approximately 13 million adults, used mindfulness practices, a significant increase compared with 2% of adults in the 2012 NHIS data. Self-reported mindfulness users were less likely to be married and more likely to identify as women, White, young to middle aged, of a sexual minority, employed, without minor children, and from the Western region of the United States. Women were more likely to have used meditation and twice as likely to have participated in yoga. Comparisons of the NHIS data from 2002 to 2017 demonstrated significant increases in yoga (6% to 14%) and meditation (4% to 14%) among United States adults.26,27
Few authors of studies have focused on the use and perceptions of mindfulness practices among practicing health care professionals for self-care and patient or client care. Most have focused on mindfulness-based interventions and their effects on the provider's wellbeing.13,15 In 2002, Schoenberger et al28 found that occupational therapists had a more positive attitude toward meditation, followed by physical therapists and physicians. Older professionals had more positive attitudes toward meditation than younger professionals. Being a meditator was the strongest predictor for incorporating meditation in patient or client care. Authors of a more recent mixed-methods study29 showed that mindfulness practices were effective for emotional regulation and stress reduction in occupational therapists, yet only 16 participants were assessed.
Athletic trainers are health care professionals who navigate high-stress and high-demand work environments. Multiple investigators30,31 have demonstrated that athletic trainers experience burnout, job-related stress and dissatisfaction, and conflict between their personal and professional lives. Although many strategies30 for improving athletic trainer retention and work-life balance have been suggested and evaluated, the concept and practice of mindfulness have not been studied. The use of mindfulness practices may be beneficial to the athletic trainer by decreasing burnout, anxiety, and stress13 and increasing work-life balance and overall quality of life. Incorporating these practices for self-care may foster compassion, empathy, and emotional regulation for clearer, sounder clinical reasoning. Mindfulness practice in athletic trainers' personal lives as well as their professional practices may improve their and their patients' wellbeing and promote patient-centered care; the latter is a core competency in athletic training education and a desired attribute of quality health care. However, little is known regarding athletic trainers' use of and attitudes toward mindfulness.
To better study the impact and effectiveness of and any implementation barriers to mindfulness-based interventions in athletic training, we must first establish athletic trainers' use and perceptions of mindfulness in their personal and professional practice. Therefore, the purpose of our study was 2-fold: to investigate athletic trainers' (1) use of mindfulness practices for self-care and patient or client care and (2) perceptions of the importance of mindfulness practices for self-care and as a tool to achieve optimal outcomes in patient or client care. We hypothesized the following:
Based on data from other health care providers and established time and knowledge barriers, athletic trainers' use of mindfulness practices would be greater for self-care than for patient or client care.
Based on the established association between personal use and professional application, no differences would exist in athletic trainers' perceptions regarding the importance of mindfulness practices for self-care or patient or client care.
Our results would be comparable with the NHIS data4,26,27: Athletic trainers who identified as female, White, not in a committed relationship, and with no children living in the home would show greater use of mindfulness practices for self-care.
Given the novelty of our study and to paint a broader picture of mindfulness use in athletic training, we also explored the relationship between frequency of use and perceptions, common mindfulness practices used by athletic trainers, potential differences in age and athletic training setting, and the potential impact the coronavirus pandemic has had on athletic trainers' use of mindfulness practices for self-care and patient or client care.
METHODS
Study Design
We used a cross-sectional design. Data were collected using an online survey software program (Qualtrics). The university's institutional review board determined that our study was exempt from oversight.
Procedures
We performed a review of the literature and found no comparable survey instrument that measured perceptions, opinions or attitudes, or use (including current and all-time use) of mindfulness. Therefore, the lead author (A.G.) developed a questionnaire and assessed its face and content validity and reliability before distributing it to the main sample pool. The formation is discussed in the Questionnaire section.
We recruited individuals to participate in our study using 2 sample pools. (1) We used a list of 4000 emails of athletic trainers in the college or university or secondary school setting that were obtained from the review of organizational websites in the public domain that identified athletic trainers and provided their email addresses (eg, colleges, universities, high schools, athletic conferences). To obtain this list, the National Collegiate Athletic Association Divisions I, II, and III; National Association of Intercollegiate Athletics; and National Junior College Athletic Association membership lists32 were randomized using a random number generator, and emails of athletic trainers were obtained from institutional websites in the randomly generated order until 2500 addresses were collected. The National Athletic Trainers' Association (NATA) Athletic Training Locations and Services Database33 maintained by the Korey Stringer Institute at the University of Connecticut was used to identify email addresses for 1500 secondary school athletic trainers. The number of athletic trainers identified by random school selection per state were weighted based on 2017 United States Census Bureau population data.34 (2) From the NATA Research Survey Service, we purchased access to a random sample of 2000 athletic trainers in the clinic or hospital, professional sports, or emerging settings (eg, military, performing arts, occupational health, and public safety).
We contacted individuals using the online survey program's distribution option. Individuals received an email explaining the purpose of our study and a web link to the online questionnaire. The questionnaire began with an informed consent page and an option to accept or decline participation. We sent reminder emails to respondents who had not finished the survey at 3, 7, and 14 days after the initial request for participation. To ensure participant confidentiality, no identifiable information was collected.
Participants
The inclusion criterion for our study, as stated in the informed consent document, was that the participant must have been currently practicing athletic training. Of 5621 potential participants with eligible email addresses, a total of 589 athletic trainers responded to our questionnaire, for a response rate of 10.5%. After a review of the data, we found and discarded 42 incomplete responses. A total of 547 athletic trainers completed the survey, for a rate of 10%.
Questionnaire
The lead author (A.G.) developed an 18-item questionnaire to investigate athletic trainers' perceptions of mindfulness practices and the frequency of their use for self-care and patient or client care. This questionnaire included 2 items on use that were adapted from the NHIS. The introduction to the first item began with a short explanation of mindfulness, as defined by Kabat-Zinn,1 and a brief list of common mindfulness practices. Participants then answered questions on use and perceptions. The survey ended with 8 demographic questions to collect the participant's age, gender, race or ethnicity, relationship status, status of children in the home, education level, athletic training setting, and years of athletic training experience.
Use
We measured the participants' frequency of participation in mindfulness practices via 2 items using a 6-point Likert scale (eg, 1 = never to 6 = very frequently). All scale options, except for never, included examples of frequency in parentheses (eg, very frequently [daily to multiple times a day], very rarely [1–5 times per year]). Respondents were asked (1) “How frequently do you participate in the practice of mindfulness?” and (2) “How frequently do you incorporate mindfulness practices into patient or client care, including suggestions for their home care plan?” These were the items adapted from NHIS items that asked about the use of specific mindfulness practices within the last 12 months.5
We incorporated skip logic into the questionnaire so that a participant who chose never for these items skipped items that asked about which specific mindfulness practices he or she had pursued personally and incorporated into patient or client care. We asked individuals to select the specific mindfulness practices they have ever participated in and ones in which they were currently participating. Mindfulness practice options were meditation, yoga, qigong, tai chi, progressive relaxation, breathing or body scanning techniques, MBSR or related formal courses, and metacognition techniques. We chose these practices based on the options used in the NHIS survey as well as in other mindfulness survey research.16 Participants also had an other option with space to type in a practice not listed. During data collection, participants were navigating the coronavirus pandemic. Therefore, we asked if their personal practice or incorporation into patient or client care had increased, decreased, or not changed or if they had started mindfulness practices during the pandemic.
Perceptions
To investigate the participants' perceptions about mindfulness, we asked them to rate their agreement with 2 statements: (1) “Mindfulness practices are important for the athletic trainer's self-care and wellbeing,” and (2) “Mindfulness practices are an important tool to incorporate in patient or client care to achieve optimal outcomes.” Participants rated their agreement using a 7-point Likert scale (eg, 1 = strongly disagree to 7 = strongly agree). Overall, the questionnaire took approximately 4 to 6 minutes to complete. A participant who answered never to both use items answered only 12 of the 18 survey questions.
Establishing Instrument Validity and Reliability
Before data collection, we established the face and content validity of the questionnaire. Four individuals participated: (1) an athletic training researcher with experience in mindfulness, consciousness, and survey research; (2) an athletic training researcher with experience in survey research; (3) a public health researcher with experience in mindfulness practices; and (4) a practicing athletic trainer with experience in mindfulness practices and alternative therapies. We provided the purpose of our study and asked them to review each questionnaire item and the overall intent of the survey. Suggestions for content, clarity, and flow were discussed with each participant, and edits were incorporated to produce a final draft of the questionnaire.
We established reliability of the instrument using the test-retest method. Forty-two individuals from the database of 4000 and 15 individuals from a convenience sample were contacted in the same manner as described earlier. Once they completed the survey, they were prompted to complete the questionnaire again at least 3 days later. Ten individuals participated in the reliability portion of the study. For this portion, individuals were informed that email addresses would be collected to match the participant's 2 responses. Once the match was completed, their responses, including their email addresses, were deleted from the online survey program and from the data analysis.
Data Analysis
Data were downloaded from the online survey program into SPSS (version 26.0; IBM Corp). We then cleaned the data and removed incomplete responses. We set the a priori level of significance at P < .05. Spearman correlations were performed to assess test-retest reliability and examine the relationship between frequency of use and perceptions of self-care and patient or client care. Descriptive statistics were conducted on all survey items. Given the ordinal nature of the data, Mann-Whitney U or Kruskal-Wallis tests with post hoc pairwise comparisons for significant main effects were performed to assess differences in the use and perceptions of mindfulness practices for self-care and patient or client care based on age, gender, race or ethnicity, relationship status, having children in the home, and athletic training setting. A related-samples Wilcoxon signed rank test was conducted to assess differences in participants' perceptions of the importance of mindfulness practices for self-care compared with patient or client care.
RESULTS
Reliability and Demographics
Spearman correlation results for test-retest reliability demonstrated that the questionnaire had sufficient reliability (ρ = 0.82–1.000, P < .05). Overall, demographics reflected a population sample that was overwhelmingly White (87%, n = 474), predominantly aged 40 or younger (61%, n = 335), in a committed relationship (72%, n = 396), and with a master's-level education (76%, n = 414). Demographic data are presented in Table 1.
Table 1.
Demographic Data
| Descriptive |
No. (%) |
| Gender | |
| Female | 280 (51) |
| Male | 263 (48) |
| Other | 4 (1) |
| Age, y | |
| 20–30 | 129 (24) |
| 31–40 | 206 (38) |
| 41–50 | 106 (19) |
| 51–60 | 86 (16) |
| 61–70 | 20 (4) |
| Race or ethnicity | |
| White | 474 (87) |
| Black or African American | 16 (3) |
| Latinx or Hispanic | 25 (5) |
| Other | 32 (6) |
| Currently in a committed relationship? | |
| Yes | 396 (72) |
| No | 151 (28) |
| Children under 18 in the home? | |
| Yes | 202 (37) |
| No | 345 (63) |
| Primary setting | |
| Clinic or hospital | 67 (12.0) |
| Collegiate | 260 (48.0) |
| Emerging | 37 (7.0) |
| Professional sports | 13 (2.0) |
| Secondary school | 170 (31.0) |
| Highest level of education | |
| Bachelor's degree | 105 (19) |
| Master's degree | 414 (76) |
| Doctorate | 27 (5) |
| Other | 1 (0.0) |
Use and Perceptions
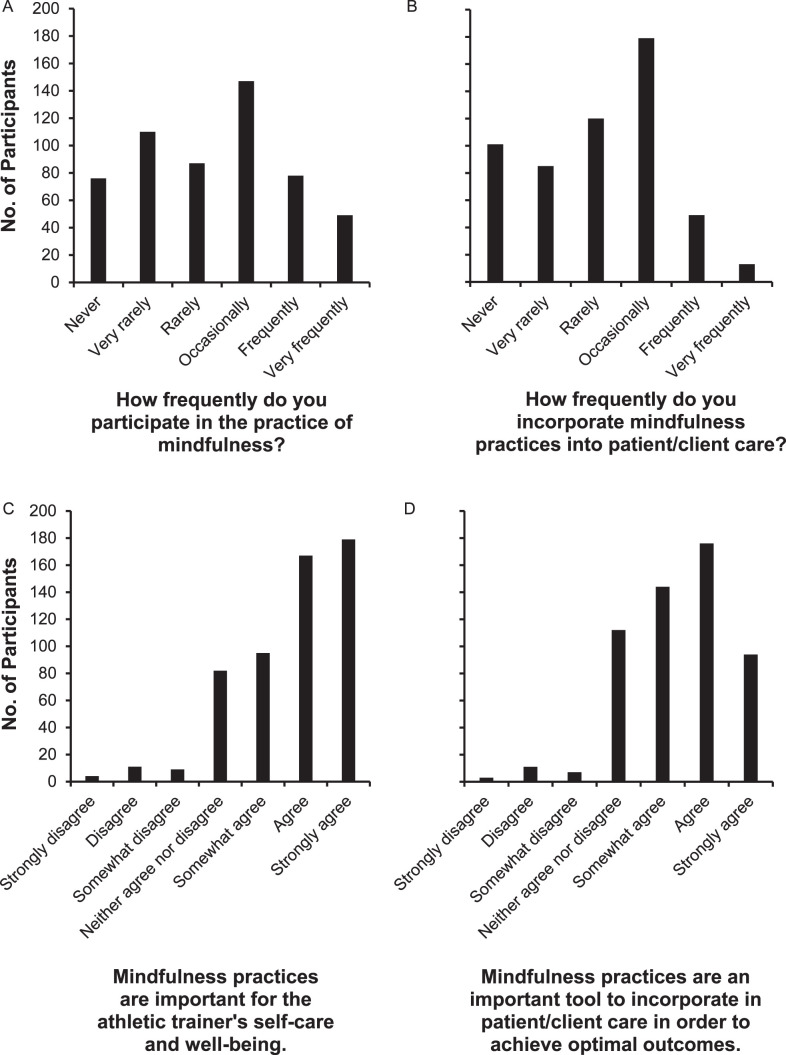
Histograms representing participants' frequency of use and perceptions regarding mindfulness practices are provided in the Figure. Median responses and interquartile ranges (IQRs; 25th–75th) by subgroups are shown in Table 2. Overall, 86% (n = 471) of respondents reported participating in some form of mindfulness practice, and 81% (n = 446) reported some incorporation of mindfulness practices into patient or client care. Overall frequency of use for self-care was greater than use for patient or client care (Z = −4.553, P < .001) with a median response of 4 = occasionally (a couple of times a month up to 1–2 times a week) for self-care and 3 = rarely (to a few patients or clients) for patient or client care. Similarly, participants perceived the use of mindfulness as more important to self-care than to patient or client care (Z = −8.548, P < .001), with a median response of 6 = agree for the self-care statement and 5 = somewhat agree for the patient or client care statement.
Figure.
Participants' uses and perceptions of mindfulness practices for self-care and patient or client care. A, Frequency of use across all participants for self-care was greater than, B, frequency of use for patient care (P < .001). C, Mindfulness practices were also perceived to be more important for self-care than, D, for patient or client care (P < .001).
Table 2.
Frequency of Use and Perceptions of Mindfulness Practice for Self-Care and Patient or Client Care
| Descriptive |
Item, Median (Interquartile Range) |
|||
| How Frequently do you Participate in the Practice of Mindfulness for Self-Care?a |
How Frequently do you Incorporate Mindfulness Practices into Patient or Client Care?a |
Mindfulness Practices are Important for the Athletic Trainer's Self-Care and Wellbeing.b |
Mindfulness Practices are an Important Tool to Incorporate in Patient or Client Care to Achieve Optimal Outcomes.b |
|
| Genderc,d,e,f | ||||
| Female | 4 (2–5) | 4 (2–4) | 6 (5–7) | 6 (5–6) |
| Male | 3 (2–4) | 3 (2–4) | 6 (5–6) | 5 (4–6) |
| Other | 3 (2–4) | 2.5 (1.5–4) | 6 (4–6.5) | 5.5 (3.5–6.5) |
| Age, ye,f | ||||
| 20–30 | 4 (2–5) | 3 (2–4) | 6 (5–7) | 6 (5–6) |
| 31–40 | 4 (2–4) | 3 (2–4) | 6 (5–7) | 6 (5–6) |
| 41–50 | 3 (2–4) | 3 (1–4) | 6 (4–7) | 5 (4–6) |
| 51–60 | 3 (1–5) | 3 (2–4) | 6 (4–7) | 5 (4–6) |
| 61–70 | 2.5 (1.5–4.5) | 2.5 (1–4) | 6 (4.5–7) | 5.5 (5–6) |
| Race or ethnicitye | ||||
| Black or African American | 3 (2–4) | 3 (1–3.5) | 7 (6–7) | 6 (4.5–7) |
| Latinx or Hispanic | 4 (2–4) | 3 (3–4) | 6 (6–7) | 6 (5–6) |
| White | 4 (2–4) | 3 (2–4) | 6 (5–7) | 5 (4–6) |
| Other | 3.5 (2–4) | 3.5 (2.5–4) | 6 (6–7) | 6 (5–6.5) |
| Currently in a committed relationship?c | ||||
| Yes | 3 (2–4) | 3 (2–4) | 6 (5–7) | 5 (5–6) |
| No | 4 (2–5) | 4 (2–4) | 6 (5–7) | 6 (5–6) |
| Children under 18 in the home?c,d,e,f | ||||
| Yes | 3 (2–4) | 3 (2–4) | 6 (5–7) | 5 (4–6) |
| No | 4 (2–5) | 3 (2–4) | 6 (5–7) | 6 (5–6) |
| Athletic training settingd | ||||
| Clinic or hospital | 4 (2.5–4.5) | 3 (2–4) | 6 (5.5–7) | 6 (5–6) |
| Collegiate | 3 (2–4) | 3 (2–4) | 5 (5–7) | 6 (5–6) |
| Emerging | 4 (2–5) | 4 (2–4) | 6 (5–7) | 6 (5–7) |
| Professional sports | 3 (3–5) | 3 (2–4) | 6 (6–7) | 6 (5–7) |
| Secondary school | 3 (2–4) | 3 (1–4) | 6 (5–7) | 5 (4–6) |
| Highest level of educatione | ||||
| Bachelor's degree | 4 (2–4) | 3 (2–4) | 6 (5–7) | 6 (4–7) |
| Master's degree | 3 (2–4) | 3 (2–4) | 6 (5–7) | 5 (5-6) |
| Doctorate | 4 (2–4.5) | 4 (3–4.5) | 7 (5–7) | 6 (5–6.5) |
| Other | (n = 1, excluded from analysis) | |||
Frequency rated 1 = never to 6 = very frequently (daily to multiple times per day).
Perceived importance rated 1 = strongly disagree to 7 = strongly agree.
P > .05 for frequency of practice for self-care.
P < .05 for frequency of practice for patient or client care.
P < .05 for perceived importance for self-care.
P < .05 for perceived importance for patient or client care.
Characteristics of Athletic Trainers Who Used Mindfulness Practices
Gender
Those identifying as female reported greater frequency of mindfulness use for self-care (H = 12.051, P = .002) and patient or client care (H = 16.616, P < .001) than those identifying as male (post hoc Z = 3.442, P < .001; and Z = 4.049, P < .001). Female-identifying individuals also perceived mindfulness practices as more important for self-care (H = 18.699, P < .001) and patient or client care (H = 14.785, P < .001) than those identifying as male (post hoc Z = 4.320, P < .001; and Z = 3.845, P < .001). No statistical differences existed between those identifying as other than male or female and those identifying as male or those identifying as female.
Race or Ethnicity
Differences in perceptions of importance of self-care (H = 13.479, P = .004) were observed, with individuals identifying as African American or Black perceiving mindfulness as more important for self-care than those identifying as White (Z = 3.146, P = .002). No other differences were noted based on race or ethnicity.
Relationship Status
Those not in a committed relationship reported using mindfulness practices for self-care more often than those who reported being in a committed relationship (U = 33 099, P = .048). No other differences were seen based on relationship status.
Children
Participants without children in their home reported greater frequency of use of mindfulness practices for both self-care (U = 38 445.5, P = .040) and for patient or client care (U = 38 480.5, P = .036) than those with children in the home. Similarly, those without children in the home perceived mindfulness practices as more important for self-care (U = 39 353, P = .009) and for patient or client care (U = 38 415, P = .038) than those with children in the home.
Exploratory Results
Relationship Between Use and Perceptions
Mindfulness use for self-care was correlated with use in patient or client care (ρ = 0.493, P < .001), perceptions regarding the importance of mindfulness practice to self-care (ρ = 0.581, P < .001), and perceptions regarding the importance of mindfulness practice to patient or client care (ρ = 0.416, P < .001). Similarly, use in patient or client care was correlated with perceptions of self-care (ρ = 0.480, P < .001) and patient or client care (ρ = 0.584, P < .001). Finally, perceptions regarding self-care were correlated with perceptions regarding patient or client care (ρ = 0.741, P < .001).
Common Mindfulness Practices
The most common currently used mindfulness practice for self-care was progressive relaxation and breathing or body-scanning techniques (63%, n = 344). This was also the most used practice for patient or client care (55%, n = 300; Table 3). Prayer was the most frequent participant-provided other response among mindfulness practices participants were currently using (3%, n = 19). Additionally, 23% (n = 128) of respondents reported having previously participated in an MBSR or related formal course.
Table 3.
Mindfulness Practices for Self-Care or Patient or Client Care, No. (%)
| Mindfulness Practice |
Self-Care |
Patient or Client Care |
|
| Ever |
Currently |
||
| Meditation | 267 (49) | 151 (28) | 153 (28) |
| Yoga | 285 (52) | 141 (26) | 243 (44) |
| Qigong | 9 (2) | 1 (0) | 2 (0) |
| Tai chi | 33 (6) | 1 (0) | 10 (2) |
| Progressive relaxation, breathing or body-scanning techniques | 344 (63) | 275 (50) | 300 (55) |
| Metacognition | 128 (23) | 138 (25) | 141 (26) |
| Other | 46 (8) | 75 (14) | 36 (7) |
Age
Based on age, differences in perceptions of importance for self-care (H = 11.000, P = .027) and patient or client care (P = .021) were observed. Those between 20 and 30 years old perceived mindfulness practices as more important for self-care than did those aged 41 to 50 (Z = 2.797, P = .005) or 51 to 60 (Z = 2.394, P = .017) years. Similarly, those 31 to 40 years of age also reported higher perceived importance for self-care than did those aged 41 to 50 years (Z = 2.173, P = .030). Differences in perceptions of importance were also observed for patient or client care between participants 20 to 30 years and 31 to 40 years of age and those 41 to 50 years of age (Z = 2.089, P = .037; and Z = 2.063, P = .039) and 51 to 60 years of age (Z = 2.674, P = .007; and Z = 2.687, P = .007), respectively.
Athletic Training Setting
Differences existed based on setting for incorporating mindfulness into patient or client care (H = 13.314, P = .010), with those in emerging (Z = 2.957, P = .003) and collegiate (Z = 2.732, P = .006) settings reporting more frequent use than those in the secondary school setting. Those in emerging settings also more often incorporated mindfulness into patient or client care than did those in clinic or hospital settings (Z = −2.341, P = 0.019). No other differences based on athletic training setting were observed.
Impact of the Coronavirus Pandemic
Among those who reported participating in mindfulness activities for self-care, 34% (n = 159) reported increased frequency during the coronavirus pandemic; 8% (n = 46), decreased frequency; 49% (n = 232), no change in frequency; and 7% (n = 34), starting their mindfulness practice since the pandemic began. With respect to the frequency of incorporating mindfulness practices into patient or client care, among those who reported incorporating mindfulness practices, 20% (n = 88) reported increased frequency during the pandemic; 9% (n = 41), decreased frequency; 67% (n = 300), no change in frequency; and 4% (n = 17), starting to incorporate mindfulness practices since the pandemic began.
DISCUSSION
Athletic trainers experience burnout, work-life conflict, and job dissatisfaction.30 The reported benefits6,13,14,17,21 of mindfulness practices may help athletic trainers mitigate these concerns, foster empathy and self-compassion, and improve their quality of life as well as the lives of the patients or clients they serve. The purpose of our study was to investigate athletic trainers' use and perceptions of mindfulness practices in self-care and patient or client care. Our results highlight a disconnect between athletic trainers' use and perceptions of mindfulness practices. Most of our participants strongly agreed or agreed that mindfulness practices are important for self-care, and they somewhat agreed, agreed, or strongly agreed that these practices are important for patient or client care. These findings are comparable to the literature15,18,28,29 on health care professionals' positive perceptions of mindfulness practices. Furthermore, the top 3 mindfulness practices (Table 3) used by our participants (yoga; meditation; and progressive relaxation, breathing, or body-scanning techniques) are consistent with national trends in mindfulness use.4,26,27 However, although our participants viewed mindfulness as important, the majority used these practices only occasionally (ie, a couple of times a month up to 1 to 2 times per week) or less for self-care and rarely (ie, to a few patients or clients) or less for patient or client care. Our findings add to the recent concerns in health care about the lack of implementation of mindfulness-based programs and techniques for clinicians and patients or clients.24,25 We discuss specific differences in use and perceptions with regard to self- and patient or client care and in accordance with the hypotheses of our study.
Athletic Trainers and Mindfulness: Self-Care Versus Patient or Client Care
Most of our participants perceived mindfulness practices as more important for self-care than for patient or client care, and they used these practices more for self-care. Therefore, we accepted our first hypothesis and rejected our second hypothesis. Given the helping nature of the profession, we expected athletic trainers would view the benefits of mindfulness as equally important for themselves and their patients or clients, regardless of their use. However, our data suggest that participating athletic trainers prioritized their personal use of mindfulness practices over professional use. Based on the clear evidence supporting the positive effects of mindfulness on the wellbeing and performance7–12 of the individuals who comprise most of their patient or client base, athletic trainers should strongly consider incorporating mindfulness practices into their clinical practice. Authors15,24,25 have noted that implementation barriers for clinicians include time limitations (eg, time-intensive MBSR courses and limited time with patients or clients), perceived knowledge of the best mindfulness techniques to offer and teach to patients or clients, and cost effectiveness. Our findings expose the need to investigate potential barriers to the use of mindfulness practices specific to athletic training clinical practice and to educate athletic trainers and students on the most useful practices that are time and cost effective.
We must note that athletic trainers prioritizing mindfulness practice for self-care over patient or client care is not necessarily a negative finding for 2 reasons. First, researchers28 suggested that the strongest predictor of professional mindfulness use was personal use. Therefore, as athletic trainers continue to use mindfulness practices for self-care, they are more likely to incorporate them into patient or client care, and this is supported by the correlation between self-care and patient or client care observed in our results. Second, researchers have demonstrated that health care professionals' use of mindfulness for self-care can improve patient or client outcomes and safety. Braun et al,19 in a recent review of studies on the impact of mindfulness-based interventions in health care professionals, found moderate support for improved patient safety, treatment outcomes, and patient-centered care. Amutio-Kareaga et al,20 in a research review, proposed that compassion- and mindfulness-based strategies are effective for fostering physicians' empathy, compassion, patient communication, and patient-reported quality of care. Given the reported benefits of mindfulness practices for health care professionals and their patients or clients, we strongly encourage athletic trainers to explore and incorporate practical, brief mindfulness-based programs and techniques more consistently into their personal and professional care. Examples of these techniques are discussed later in the “Recommendations for Practice” section.
Characteristics of Athletic Trainers and Mindfulness Use
Our final hypothesis stated that our results would be comparable with the NHIS data,4 and athletic trainers who identified as female, White, not in a committed relationship, and with no children living in the home would show higher use of mindfulness practices for self-care. Our results supported this hypothesis for every characteristic except race or ethnicity. Similar to the self-reported mindfulness use in the general United States population, our results showed that athletic trainers who used mindfulness practices most frequently were more likely to identify as female, were not in a committed relationship, and had no children living in their home. Females and those with no children in the home also perceived mindfulness practices to be more important for both self-care and patient or client care. However, no differences existed based on relationship status for use in patient or client care or for perceptions related to self-care or patient or client care.
Although several proposals exist as to why females use mindfulness practices more than males, no known empirical studies have been published on gender-specific mindfulness use.35 Female athletic trainers experienced higher levels of burnout and exhaustion30,31 and may be more inclined to use mindfulness practices to combat these problems. Regarding social and familial status, significant others and children often contend with one's personal and professional time, so it is not surprising that participants who were in committed relationships and who had children living in the home used mindfulness practices less often because, as stated earlier, one of the main barriers to health care professionals' mindfulness use is the perceived time commitment.15,25
In contrast with the NHIS data, we observed no differences in race or ethnicity for use of mindfulness practices for both self-care and patient or client care or for perceived importance for patient or client care. We must acknowledge a confounding factor in this observation: our participants were disproportionately White (87%), which is comparable with the race or ethnicity demographics of the NATA (80%).36 An interesting finding in our results was that, although no differences in use existed, participants identifying as African American or Black perceived the personal use of mindfulness practices as more important than those identifying as White. The median response for Black participants was strongly agree that personal mindfulness use was important and agree that professional use was important, both of which surpassed the overall group medians of agree and somewhat agree. However, their median personal and professional use was only rarely. At the time of administration of our survey, the Black community in the United States was disproportionately affected by national events, conversations, and protests related to social injustices and racism, and an unequal rate of infections and death from the coronavirus pandemic. This has been termed a “pandemic within a pandemic”37 for Blacks, which is and will continue to be profoundly detrimental to their health and wellbeing. These combined injustices and disparities may contribute to Black athletic trainers' heightened awareness that the state and improvement of their wellbeing, as well as their patients' wellbeing, are critical for navigating such difficult and challenging times and concerns. Given the ongoing nature of these challenges, this topic warrants further investigation.
Regarding age differences, our findings were not comparable with the NHIS data,4 which showed that young and middle-aged adults were more likely to report mindfulness use. Although young and middle-aged participants in our study were more likely to perceive mindfulness practices as important for both self-care and patient or client care, no differences existed in the frequency of personal or professional use. The trend toward younger participants, along with an upper limit of age 70 in our sample, may have contributed to the lack of differences observed in frequency of use.
Our results demonstrated that participating athletic trainers in the university or collegiate and emerging settings used mindfulness practices more frequently for patient or client care than those in the secondary school setting. A potential contributing factor for this difference could be the clinician-to-patient ratio. Secondary school athletic trainers are often assigned to 1 or more schools as the sole athletic trainer providing medical care for hundreds of student-athletes. Therefore, the time commitment barrier to incorporating mindfulness techniques into patient or client care, many instances of which require some degree of one-on-one attention, may be more of a factor in secondary schools than in other settings with lower clinician or patient ratios. Interest in and implementation of mindfulness-based programs in secondary schools has grown considerably as school administrators and teachers attempt to provide students with early self-regulation skills, and individual and group-based mindfulness programs have been shown to be effective in a variety of outcomes from emotional regulation to enhanced athletic and academic performance.9,38 To reduce the time commitment, in addition to implementing the low-cost, brief mindfulness practices discussed later, group-based mindfulness programs could be implemented in the secondary school setting with the assistance of the school counselor. Schools may also participate in projects38 such as Mindful Schools (https://www.mindfulschools.org) or the Mindfulness in Schools Project (https://mindfulnessinschools.org), and athletic trainers can gain access to training and other materials or access their websites for free resources.
Limitations, Future Directions for Research, and Recommendations for Practice
Limitations
Our study was not without limitations. First, our response and completion rates were quite low and may not represent the entire athletic training profession. Even though the survey was short, and we sent multiple reminders, data were collected during a time when potential participants were navigating a coronavirus pandemic, subsequent economic and job uncertainty, social and racial injustices and unrest, and a polarized presidential election. These factors likely had negative effects on our response and completion rates. Second, a response bias likely existed in that those who never use mindfulness practices or do not perceive them as important did not begin the survey, and this would also have a negative effect on our response and completion rates. Third, our study was a cross-sectional design and did not reflect athletic trainers' mindfulness use and perceptions over time. Fourth, we did not ask participants about their regional identity nor area of residence, so we could not compare these data with the NHIS data.
Future Research
Now that we have knowledge of athletic trainers' perceptions and use of mindfulness practices for self-care and patient or client care, we must better understand the disconnect between athletic trainers' perceived importance of mindfulness and their inconsistent use personally and professionally. Future directions for research should include mixed-methods investigations into reasons for mindfulness use and potential barriers to its use in self-care and patient or client care among athletic trainers and in their workplaces. Researchers should include future participants' regional identities and current areas of residence, educational backgrounds including those with exposure to or specific training on complementary health, and availability of mindfulness programs in the workplace to gain a better understanding of athletic trainers' geographic and educational backgrounds and life exposure to mindfulness practices. Greater efforts must be made to include athletic trainers who are Black, Indigenous, and people of color in mindfulness-based intervention research. The larger gap observed between perceived benefits and use among this group of athletic trainers compared with others suggests they could strongly benefit from additional access, support, and training related to implementation of mindfulness-based practices in both self-care and patient or client care, particularly given that they are disproportionately affected by social injustices and health disparities that influence mental and physical wellbeing.37 Furthermore, as our profession continues to grow and advance, a substantial need exists for longitudinal studies that investigate the effectiveness of mindfulness-based interventions in 3 populations: (1) athletic training students, (2) practicing athletic trainers, and (3) the patients or clients we serve. Incorporating and investigating mindfulness-based programs in athletic training curricula that facilitate students' emotional resilience, empathy, and coping strategies can act as a catalyst for improved work-life balance and wellbeing for future athletic trainers and potentially improve their patients' or clients' outcomes. Administrators and supervisors should incorporate and assess the impact of workplace-based mindfulness education programs for athletic trainers that are practical and cost and time efficient. Overall, further investigation and implementation of mindfulness-based practices are necessary to understand and overcome challenges related to transferring positive perceptions into higher rates of use for both self-care and patient or client care. Such efforts may result in improved wellbeing and quality of life for both athletic trainers and their patients.
Recommendations for Practice
Time, resources, and knowledge or confidence are commonly cited barriers to mindfulness practice and implementation.9,15 The time barrier is supported by our observations of lower rates of mindfulness use among those in committed relationships, with children in the home, and working in secondary school settings. Therefore, brief mindfulness practices, such as smartphone apps with 5- to 10-minute meditation sessions (many of which have free options), brief yoga, tai chi, and qigong sessions found on YouTube channels, 30- to 60-second metacognition moments (eg, thinking about your thinking, awareness and management of your own thoughts1), breathing (eg, 4-8 breathing: inhale for 4 seconds, exhale for 8 seconds, repeat for a total of 3 times) and body-scanning techniques are more feasible for overworked, stressed health care professionals and students and can be effective in improving their wellbeing. Incorporating brief mindfulness programs into the workplace has been observed to promote the health and wellbeing of employees in various occupational settings,39 yet additional work is required to incorporate them more consistently into health care settings. Workplace-based programs focused on brief mindfulness practices represent a potential intervention strategy for increasing mindfulness use among athletic trainers, particularly those with limited time due to family or relationship commitments. Furthermore, these brief techniques may be more easily integrated into clinical practice once athletic trainers become familiar with the techniques and more comfortable teaching them to their patients or clients.
Athletic trainers should explore resources within their institutions' counseling and human resource centers to assist with self and patient or client mindfulness-based programs, including the feasibility of involving qualified mindfulness instructors in implementing programs, such as MBSR options,12 the Mindfulness-Acceptance and Commitment Approach, and the Mindfulness Meditation for Sport Training.7 Authors9 have stated that the most important component of successful and consistent mindfulness implementation is educating the stakeholders (eg, patients or clients, athletes, coaches, administrators) on what being mindful entails and its benefits to performance and wellbeing. Therefore, continuing education opportunities involving mindfulness-based training would be beneficial in expanding the athletic trainer's knowledge and confidence in successfully implementing mindfulness into clinical practice.
CONCLUSIONS
Mindfulness-based practices are an established intervention for combatting stress, burnout, and anxiety; fostering empathy, compassion, and emotional regulation; and strengthening coping strategies. Therefore, mindfulness may be an effective intervention for enhancing work-life balance and wellbeing among athletic trainers. Although most of our participants reported engaging in mindfulness occasionally or less frequently and rarely to never in patient or client care, strong agreement existed that mindfulness practices were important, particularly for self-care. These results suggest that effective interventions to increase the frequency of mindfulness use among athletic training students and athletic trainers for self-care may be well received and have both direct and indirect benefits for patient or client outcomes and safety. Given the personal and professional demands on athletic trainers, brief and workplace mindfulness-based interventions may be one strategy to increase the use of mindfulness practices among athletic trainers and patients or clients. Also, strategies to increase the use of mindfulness-based programs and techniques in athletic training education curricula should be explored.
REFERENCES
- 1.Kabat-Zinn J. Delacorte Press; 1990. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. [Google Scholar]
- 2.Kaufman KG, Glass CR, Pineau TR. Mindful Sport Performance Enhancement: Mental Training for Athletes and Coaches. American Psychological Association. 2018.
- 3.Raski MP. Mindfulness: what it is and how it is impacting healthcare. UBCMJ . 2015;7(1):56–59. [Google Scholar]
- 4.Simonsson O, Martin M, Fisher S. Sociodemographic characteristics and health status of mindfulness users in the United States. Mindfulness . 2020;11:2725–2729. doi: 10.1007/s12671-020-01486-4. [DOI] [Google Scholar]
- 5.National health interview survey. National Center for Health Statistics. Centers for Disease Control and Prevention. Published 2020. Accessed November 20, 2020. https://www.cdc.gov/visionhealth/vehss/data/national-surveys/national-health-interview-survey.html.
- 6.Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits: a meta-analysis. J Psychosom Res . 2004;57(1):35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- 7.Bühlmayer L, Birrer D, Rothlin P, Faude O, Donath L. Effects of mindfulness practice on performance-relevant parameters and performance outcomes in sports: a meta-analytical review. Sports Med . 2017;47(11):2309–2321. doi: 10.1007/s40279-017-0752-9. [DOI] [PubMed] [Google Scholar]
- 8.Moen F, Federici RA, Abrahamsen F. Examining possible relationships between mindfulness, stress, school and sport performances and athlete burnout. Int J Coach Sci . 2015;9(1):3–19. [Google Scholar]
- 9.Petterson H, Olson BL. Effects of mindfulness-based interventions in high school and college athletes for reducing stress and injury, and improving quality of life. J Sport Rehabil . 2017;26(6):578–587. doi: 10.1123/jsr.2016-0047. [DOI] [PubMed] [Google Scholar]
- 10.Ivarsson A, Johnson U, Anderson MB, Fallby J, Altemyr M. It pays to pay attention: a mindfulness-based program for injury prevention with soccer players. J Appl Sport Psychol . 2015;27(3):319–334. doi: 10.1080/10413200.2015.1008072. [DOI] [Google Scholar]
- 11.Naderi A, Shaabani F, Gharayagh Zandi H, Calmeiro L, Brewer BW. The effects of a mindfulness-based program on the incidence of injuries in young male soccer players. J Sport Exerc Psychol . 2020;42(2):161–171. doi: 10.1123/jsep.2019-0003. [DOI] [PubMed] [Google Scholar]
- 12.Mohammed WA, Pappous A, Sharma D. Effect of mindfulness based stress reduction (MBSR) in increasing pain tolerance and improving the mental health of injured athletes. Front Psychol . 2018;9:722. doi: 10.3389/fpsyg.2018.00722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lomas T, Medina JC, Ivtzan I, Rupprecht S, Eiroa-Orosa FJ. A systematic review of the impact of mindfulness on the well-being of healthcare professionals. J Clin Psychol . 2018;74(3):319–355. doi: 10.1002/jclp.22515. [DOI] [PubMed] [Google Scholar]
- 14.Klein A, Taieba O, Xavier S, Baubet T, Reyre A. The benefits of mindfulness-based interventions on burnout among health professionals: a systematic review. Explore (NY) . 2020;16(1):35–43. doi: 10.1016/j.explore.2019.09.002. [DOI] [PubMed] [Google Scholar]
- 15.Gilmartin H, Goyal A, Hamati MC, Mann J, Saint S, Chopra V. Brief mindfulness practices for healthcare providers – a systematic literature review. Am J Med . 2017;130(10):1219.e1–1219.e17. doi: 10.1016/j.amjmed.2017.05.041. [DOI] [PubMed] [Google Scholar]
- 16.Burton A, Burgess C, Dean S, Koutsopoulou GZ, Hugh-Jones S. How effective are mindfulness-based interventions for reducing stress among healthcare professionals? A systematic review and meta-analysis. Stress Health . 2017;33(1):3–13. doi: 10.1002/smi.2673. [DOI] [PubMed] [Google Scholar]
- 17.Chiappetta M, D'Egidio V, Sestili C, Cocchiara RA, La Torre G. Stress management interventions among healthcare workers using mindfulness: a systematic review. Senses Sci . 2018;5(2):517–549. doi: 10.14616/sands-2018-5-517549. [DOI] [Google Scholar]
- 18.Willgens AM, Craig S, DeLuca M, et al. Physical therapists' perceptions of mindfulness for stress reduction: an exploratory study. J Phys Ther Educ . 2016;30(2):45–51. doi: 10.1097/00001416-201630020-00009. [DOI] [Google Scholar]
- 19.Braun SE, Kinser PA, Rybarczyk B. Can mindfulness in health care professionals improve patient care? An integrative review and proposed model. Transl Behav Med . 2019;9(2):187–201. doi: 10.1093/tbm/iby059. [DOI] [PubMed] [Google Scholar]
- 20.Amutio-Kareaga A, García-Campayo J, Delgado LC, Hermosilla D, Martínez-Taboada C. Improving communication between physicians and their patients through mindfulness and compassion-based strategies: a narrative review. J Clin Med . 2017;6(3):33. doi: 10.3390/jcm6030033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sibinga EMS, Wu AW. Clinician mindfulness and patient safety. JAMA . 2010;304(22):2532–2533. doi: 10.1001/jama.2010.1817. [DOI] [PubMed] [Google Scholar]
- 22.Geigle PR, Galatino ML. Complementary and alternative medicine inclusion in physical therapist education in the United States. Physiother Res Int . 2009;14(4):224–233. doi: 10.1002/pri.437. [DOI] [PubMed] [Google Scholar]
- 23.Barnes N, Hattan P, Black D, Shuman-Oliver Z. An examination of mindfulness-based programs in US medical schools. Mindfulness . 2017;8:489–494. doi: 10.1007/s12671-016-0623-8. [DOI] [Google Scholar]
- 24.Demarzo MMP, Cebolla A, Garcia-Campayo J. The implementation of mindfulness in healthcare systems: a theoretical analysis. Gen Hosp Psychiatry . 2015;37(2):166–171. doi: 10.1016/j.genhosppsych.2014.11.013. [DOI] [PubMed] [Google Scholar]
- 25.Calabrese LH. Why mindfulness/meditation is a “no-brainer” for health-care professionals. J Patient Exp . 2019;6(1):21–23. doi: 10.1177/2374373518774390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Clarke TC, Barnes PM, Black LI, Stussman BJ, Nahin RL. Use of yoga, meditation, and chiropractors among U.S. adults aged 18 and over. NCHS Data Brief No 325 National Center for Health Statistics Published 2018 Accessed November 20 2020. https://translatereality.com/wp-content/uploads/2019/09/CDC-Study-on-Mindfulness-Yoga.pdf . [PubMed]
- 27.Kachan D, Olano H, Tannenbaum SL, et al. Prevalence of mindfulness practices in the US workforce: National Health Interview Survey. Prev Chronic Dis . 2017;14:E01. doi: 10.5888/pcd14.160034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schoenberger NE, Matheis RJ, Shiflett SC, Cotter AC. Opinions and practices of medical rehabilitation professionals regarding prayer and meditation. J Altern Complement Med . 2002;8(1):59–69. doi: 10.1089/107555302753507186. [DOI] [PubMed] [Google Scholar]
- 29.Reid D, Farragher J, Ok C. Exploring mindfulness with occupational therapists practicing in mental health contexts. Occup Ther Ment Health . 2013;29(3):279–292. doi: 10.1080/0164212X.2013.819727. [DOI] [Google Scholar]
- 30.Mazerolle SM, Pitney WA, Goodman A, et al. National Athletic Trainers' Association position statement: facilitating work-life balance in athletic training practice settings. J Athl Train . 2018;53(8):796–811. doi: 10.4085/1062-6050-51.11.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.DeFreese JD, Mihalik JP. Work-based social interactions, perceived stress, and workload incongruence as antecedents of athletic trainer burnout. J Athl Train . 2016;51(1):28–34. doi: 10.4085/1062-6050-51.2.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Directory NCAA. National Collegiate Athletics Association. Published 2019. Accessed February 11, 2019. https://web3.ncaa.org/directory/
- 33.Athletic Training Locations and Services (ATLAS) Korey Stringer Institute: Published 2019. Accessed February 1, 2019. https://ksi.uconn.edu/atlas/ [Google Scholar]
- 34.Explore census data United States Census Bureau. Published 2020. Accessed November 30, 2020. https://data.census.gov/cedsci/
- 35.Upchurch DM, Johnson PJ. Gender differences in prevalence, patterns, purposes, and perceived benefits of meditation practices in the United States. J Womens Health (Larchmt) . 2019;28(2):135–142. doi: 10.1089/jwh.2018.7178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ethnicity demographic data National Athletic Trainers' Association Web site. Published 2018. Accessed November 30, 2020. https://www.nata.org/sites/default/files/ethnicity-demographic-data-sept-2018.pdf.
- 37.Stolberg SG. ‘Pandemic within a pandemic' fuels unrest. The New York Times . 2020. June 8. A20.
- 38.Renshaw TL, Cook CR. Introduction to the special issue: Mindfulness in the schools-historical roots, current status, and future directions. Psychol Sch . 2017;54(1):5–12. doi: 10.1002/pits.21978. [DOI] [Google Scholar]
- 39.Bartlett L, Martin A, Neil A, et al. A systematic review and meta-analysis of workplace mindfulness training randomized controlled trials. J Occup Health Psychol . 2019;24(1):108–112. doi: 10.1037/ocp0000146. [DOI] [PubMed] [Google Scholar]