Abstract
Background
Convulsive status epilepticus (CSE) prevention is critical for pediatric patients with epilepsy. Immediate intervention before CSE reduce severity. Despite its wide usage as an anticonvulsant, valproic acid (VPA) results in harmful side effects such as dose-dependent hepatotoxicity. Hence, reducing VPA dosage to minimize side effects while maintaining its efficacy is necessary, and transcranial photobiomodulation (tPBM) add-on therapy could facilitate this. We recently demonstrated for the first time that tPBM at a wavelength of 808 nm attenuated CSE in peripubertal rats. However, the effects of VPA with the add-on therapy of tPBM prior to seizures have not yet been explored. This study investigated whether adding tPBM to VPA exerts synergistic effect for CSE prevention in peripubertal rats.
Methods
A gallium-aluminum-arsenide laser (wavelength of 808 nm with an exposure duration of 100 s and irradiance of 1.333 W/cm2 at the target) was applied transcranially 30 min after VPA injection in Sprague Dawley rats. All the rats received 90 mg/kg of pentylenetetrazole (PTZ). Except for the saline (n = 3), tPBM + saline (n = 3), and PTZ group (n = 6), all the rats received a PTZ injection 30 min after VPA injection. The rats received add-on tPBM with PTZ immediately after tPBM. In the VPA + PTZ group, the rats received low-dose (100 mg/kg, n = 6), medium-dose (200 mg/kg, n = 6), and high-dose (400 mg/kg, n = 7) VPA. In the VPA + tPBM + PTZ group, the rats received low (100 mg/kg, n = 5), medium (200 mg/kg, n = 6), and high (400 mg/kg, n = 3) doses of VPA. Seizures were evaluated according to the revised Racine’s scale in a non-blinded manner.
Results
Adding tPBM to low-dose VPA reduced the incidence of severe status epilepticus and significantly delayed the latency to stage 2 seizures. However, adding tPBM to high-dose VPA increased the maximum seizure stage, prolonged the duration of stage 4–7 seizures, and shortened the latency to stage 6 seizures.
Conclusions
Adding tPBM to low-dose VPA exerted a synergistic prevention effect on PTZ-induced seizures, whereas adding tPBM to high-dose VPA offset the attenuation effect.
Keywords: Transcranial photobiomodulation, Add-on therapy, Valproic acid, Pentylenetetrazole, Seizures, Epilepsy, Status epilepticus
Background
Convulsive status epilepticus (CSE) is the most common childhood neurological emergency, with a mortality rate of 1% in the United States, 3–5% in the United Kingdom, and 7% in Taiwan [1–3]. Preventing CSE can reduce the severity and morbidity of pediatric patients. Current strategies for preventing CSE includes the use of closed-loop detection–treatment systems that combine the prediction, detection, and immediate treatment of CSE [4]. The US Food and Drug Administration–approved responsive neurostimulation (RNS) system (NeuroPace), a closed-loop detection treatment system [5, 6], could substantially reduce focal-onset seizures and improve patients’ quality of life [7]. Our previous study [8] suggested that the application of transcranial photobiomodulation (tPBM) prior to a CSE event—determined on the basis of a deep learning model’s prediction of seizures [9]—can alleviate CSE. Neurostimulation is applied to the closed-loop detection–treatment systems by using electricity at present, tPBM can also be used for future neurostimulation after seizure prediction and detection. The regular use of antiepileptic drugs (AEDs) for CSE prevention is crucial. With seizure prediction and the regular use of AEDs established as fundamental for CSE prevention, we evaluated whether tPBM as an add-on to routinely used AEDs would exert a synergistic effect on CSE prevention. Valproic acid (VPA or sodium valproate; trade name: Depakine) is one of the first-choice AEDs for benzodiazepine (BZD)-refractory CSE [10, 11]. Despite its frequent clinical usage, VPA may have side effects such as hyperammonemia [12] and liver toxicity (LiverTox category A) [13]. Hepatotoxicity is the most severe side effect of VPA [14]. VPA enhances hepatotoxicity by inhibiting mitochondrial beta-oxidation and shunting into cytochrome P450–associated pathways [15]. Compared with adults, children are more susceptible to VPA-induced hepatotoxicity [16]. Moreover, VPA-induced hepatotoxicity is more severe in children and infants than in adult and has high mortality following acute liver failure [17]. Furthermore, in vitro [18] and in vivo [19] studies have revealed the hepatotoxicity of VPA is dose-dependent. Although a recent cohort study reported non-dose-dependent changes in the liver enzyme levels of pediatric patients with epilepsy, the dose-dependent hepatoxicity of VPA is observed in daily clinical practice [20]. In addition, VPA-induced hyperammonemia was reported to be dose dependent [21]. Therefore, administered doses of VPA must be reduced to minimize its side effects while maintaining or even enhancing its therapeutic effects for CSE. Such dose reduction would be beneficial for pediatric patients with CSE and may be achieved through an add-on therapy.
Photobiomodulation (PBM) therapy, previously known as low-level laser (light) therapy (LLLT) [22], involves the use of red to near-infrared (NIR) light to cause biological alterations in organisms secondary to the interactions of photons in the visible or infrared spectral region with molecules in cells or tissues [23]. PBM therapy or LLLT with red to NIR light works through the absorption of photons by mitochondrial cytochrome c oxidase (CcO) [24], thus accelerating and increasing ATP synthesis [8, 25] and activating numerous pathways, eventually exerting cellular protective effects including anti-inflammatory effect [26, 27]. tPBM thereby is a non-invasive approach in which NIR light penetrates through the scalp–skull–dura–brain tissue via a quantum optical–induced transparency effect [28] and subsequently exerts PBM on the neurons and glia. tPBM modulates electroencephalographic rhythms [25]; increases cerebral oxidized CcO oxygenated hemoglobin levels [29, 30], cerebral blood flow [31] and brain-derived neurotrophic factor levels; and promotes synaptogenesis [32] while inhibits neuronal apoptosis [33, 34] and reduces the reactive oxygen species level in neurons under oxidative stress [27, 35]. Clinical trials have reported that tPBM exerted therapeutic effects on patients with traumatic brain injury [36], Parkinson’s disease [37], age-related cognitive decline [38], autism spectrum disorder [39], sexual dysfunction [40], anxiety and depression [41], and fear [42]. To date, the effects of tPBM on epilepsy have been investigated only in animal studies [8, 43, 44].
The application of tPBM by using NIR lasers (at wavelengths of 808 nm and 780 nm) exerted antiepileptic effects on rats [8, 44]. Previous in vitro and in vivo PBM studies supported the results and provided insights into the underlying mechanisms. Neurochemically, PBM (810 nm) could suppress the excitotoxicity (induced by kainic acid which is an chemoconvulsant that could also trigger CSE [45]) of primary cortical neurons [35]. In their in vivo study, Ahmed et al. [46] reported that tPBM (830 nm) exerted an inhibitory effect on cortical neurotransmitters in normal rats. Radwan et al. [43] demonstrated that tPBM (830 nm) reduced the CSE-induced increase in pilocarpinized rat cortical and hippocampal amino acid neurotransmitters. Hong [47] reviewed PBM studies relevant to epilepsy. Electrophysiologically, the application of PBM (632.8 nm) induced the hyperpolarization of pyramidal cells in the rat olfactory cortex [48, 49]. Kataoka et al. [50] reported that PBM (830 nm) inhibited the transient excitation of the postsynaptic potentials in rat hippocampal slice and neural activity in the primary auditory cortex in vivo. Furthermore, the application of PBM (850 nm) to the rat visual cortex suppressed visual evoked potentials [51]. Moreover, the application of the PBM (808 nm) to the rat subthalamic nucleus predominantly evoked inhibitory responses [52]. tPBM (808 nm) exerted an antiepileptic effect by promoting the function of inhibitory GABAergic interneurons [8]. The application of PBM with NIR (an sub-division of infrared) might involve properties of the “infrared light stimulation” which enhanced the amplitude, increased the frequency, and reduced the decay time constant of the spontaneous inhibitory postsynaptic currents (sIPSCs) of cultured rat cortical neurons [53]. This indicated that infrared light enhanced presynaptic γ-amino butyric acid (GABA) release, and the modulation of sIPSCs was mediated by postsynaptic GABAA receptors (GABAARs) [53]. A study using an animal model of epilepsy administered pentylenetetrazole (PTZ), a noncompetitive GABAA receptor antagonist, to induce CSE in rats and observed the occurrence of neuronal apoptosis during PTZ-induced CSE [54]. PTZ-induces seizures through the noncompetitive antagonism of the GABAA receptor complex [55]. A study suggested that PTZ-induced seizures indirectly activated glutamate N-methyl-D-aspartate (NMDA) receptors [56], and pretreatment with MK-801, an NMDA receptor antagonist, attenuated PTZ-induced seizures in rats [56, 57]. However, compared with tPBM alone, the combination of MK-801 and tPBM (808 nm) was less effective in increasing cerebral blood flow in mice [31], indicating that the neuroprotective effect of tPBM can be relevant to NMDA receptors. Indeed, PBM (808 nm) blocked NMDA receptors in vitro [58]. In hippocampal GABAergic interneurons, parvalbumin-positive interneurons (PV-INs) –expressed the most cytochrome c, indicating that they contained the most abundant CcO [59] and thus were highly susceptible to tPBM – strongly inhibit principal cells through hippocampal gamma oscillation [60]. However, PV-INs are vulnerable to CSE-induced apoptosis [61]. tPBM (808 nm) attenuated neuronal apoptosis in the hippocampus in neonatal rats [62], and the apoptosis of hippocampal neurons was observed in PTZ-induced seizures in peripubertal rats [63]. Taken together, these findings indicated that tPBM could enhance presynaptic GABAergic interneurons, particularly PV-INs, promote the presynaptic release of GABA and thus enhance sIPSCs while attenuating PTZ’s noncompetitive antagonism toward the GABAA receptor complex, and block the NMDA receptors of postsynaptic principal cells. Thus, tPBM administered at a wavelength of 808 nm could exert an antiepileptic or anticonvulsive effect on an animal model of PTZ-induced seizures or status epilepticus (SE) in peripubertal rats.
Our previous study [8] demonstrated the effects of tPBM monotherapy on seizure behaviors and SE in a rodent model of epilepsy and elucidated the mechanisms underlying these effects. We found that the transcranial application of NIR laser irradiation (at wavelength of 808 nm) applied transcranially attenuated PTZ-induced SE by protecting hippocampal PV-INs from apoptosis based on terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL) assay [8] and preserving the integrity of the perisomatic inhibition network of PV-INs in pyramidal neurons present in the hippocampus of peripubertal rat brains based on the result of immunofluorescences [8]. Furthermore, by performing electroencephalography, Vogel et al. observed that tPBM reduced the epileptiform discharge in rats with epilepsy [44].
The benefits of polytherapy (combination or add-on therapy) using tPBM and AEDs, such as VPA, remained unknown. Combination therapy for seizures that administered AEDs and other electromagnetic waves was first demonstrated by Lotfy et al. who reported that VPA combined with whole-body low-dose gamma irradiation (LDR) exerted synergistic effects on PTZ-induced seizures in rats [64]. However, the adverse side effects of LDR, such as DNA mutation, are concerning, particularly in the context of treating children [65].
Human [29] and animal [66] studies have demonstrated that tPBM enhanced CcO activities. Li et al. reported that VPA dose-dependently increased CcO activities [67]. Thus, the enhancement of CcO activity by both tPBM and VPA suggests synergistic effects may be realized through an add-on therapy that make use of tPBM and VPA. Furthermore, VPA ameliorated neuronal apoptosis [68] and preserved the number of PV-INs [69] in the hippocampus of epileptic rats, including in SE models. Our previous study [8] reported that tPBM inhibited the apoptosis of hippocampal neurons particularly PV-INs. Epigenetically, VPA downregulated of Scn3a promoter activity, thus exerting an anticonvulsant effect in vitro [70] and blocked seizure-induced aberrant neurogenesis by inhibiting histone deacetylases at the epileptic dentate gyrus in vivo [71]. Additionally, PBM could modulate epigenetic events [72, 73].
The similar mechanisms of tPBM and VPA and their anticonvulsant effects suggest the possibility of using a synergistic polytherapy approach to attenuate SE. Here, we hypothesized that combination therapy with both tPBM and VPA for pretreatment prior to an acute seizure event would exert synergistic effects to prevent CSE. We investigated the effects of add-on therapy using a combination of VPA and tPBM on PTZ-induced seizures or SE in peripubertal rats based on the premise that such add-on therapy would reduce hepatotoxicity due to reduced dosage of VPA needed.
Methods
Animals
All animal experiments were performed in accordance with the Animal Protection Act of the Council of Agriculture, Executive Yuan, Taiwan, and complied with the ARRIVE (Animal Research: Reporting of In Vivo Experiments) guidelines and the Basel Declaration, and the 3R concept. Moreover, the animal experiments performed in this study were approved by the Laboratory Animal Center of Taipei Medical University (approval No. LAC-2019-0237) as were those performed in our previous study [8]. A total of 45 male Sprague-Dawley rats (aged 35–41 days) purchased from BioLASCO (BioLASCO Taiwan Co., Ltd., Taipei, Taiwan) were used in the study. The grouping assignment for the 45 rats was as follows: saline (n = 3), tPBM + saline (n = 3), PTZ (n = 6), VPA100 + PTZ (n = 6), VPA200 + PTZ (n = 6), VPA400 + PTZ (n = 7), VPA100 + tPBM + PTZ (n = 5), VPA200 + tPBM + PTZ (n = 6), and VPA400 + tPBM + PTZ (n = 3). Because our previous study indicated that tPBM could attenuate seizures and SE [8], we did not include “tPBM + PBM” as an individual group in this study. In addition, one rat assigned to the PTZ group was excluded from data analysis because of a technical error in PTZ injection. Five rats, including three rats in the PTZ group, one rat in the VPA100 + PTZ group, and one rat in the VPA100 + tPBM + PTZ group, that died due to severe SE received transcardial perfusion immediately after death [8, 74]. The brains of these five rats were harvested and immersed in 4% paraformaldehyde, followed by serial dehydration in 20% sucrose at 4 °C overnight and subsequent preservation in 30% sucrose at 4 °C for future use. The remaining 40 rats survived after seizures or SE were kept in cages for days and were finally euthanized with 60% CO2. After the rats became unconscious following 60% CO2 inhalation, they were considered dead once their heart beats stopped; this was confirmed by palpation of the chests. The rats were exposed to CO2 for at least 5–6 min according to the guideline of the Laboratory Animal Center of Taipei Medical University.
Experimental protocol
All the rats received an intraperitoneal injection of VPA and then were observed and recorded on video for 30 min. Thirty minutes after VPA injection, the rats received tPBM for 100 s. Immediately after tPBM, the rats were subcutaneously injected with PTZ and then observed for seizure behavioral analysis through both direct observation and video recording for 1 h. The experimental sequence arrangement that rats received PTZ immediately after tPBM was in consideration of the bioavailability of tPBM and PTZ. PBM could change neural activity of the central nervous system in rats with time scale of 250 ms [51]. Even if to examine the onset of PBM in the time scale of “minutes”, the PBM took action as at least within “10 min” after laser irradiation on the peripheral nervous system of rats [49, 75, 76]. As for PTZ, the blood oxygen level-dependent signal intensities increased within 2–4 s with peak at 15 s after PTZ injection [77]. The latency to PTZ (90 mg/kg)-induced 1st generalized tonic-clinic (GTC) seizures in rats was in the time scale of 1–5 min [78, 79]). Considering that the instant action of PBM on neural activity in time scale of milliseconds to minutes and that PTZ works on brains within seconds and the latency of 1st GTC seizures is in time scale of minutes, the PTZ was thus arranged immediately after tPBM for the most appropriate therapeutic windows of tPBM against PTZ-induced seizures.
VPA pretreatment
VPA sodium salt (CAS number 1069-66-5, Sigma-Aldrich, USA) was freshly dissolved in saline and prepared in dose of 50, 100, and 200 mg/mL for low, medium, and high subgroups, respectively. VPA doses of 100, 200, and 400 mg/kg were considered low, medium, and high, respectively [80]. The low and medium doses of VPA do not cause hepatotoxicity, whereas a high-dose of VPA (> 300 mg/kg) can cause hepatotoxicity [19]. VPA was injected into the rats intraperitoneally 30 min before PTZ injection [81] because a total of 30 min are required to reach the maximum serum concentration of VPA (110 mg/kg, which is close to the VPA dose of 100 mg/kg) [82].
tPBM
The settings and parameters of tPBM used in the current study were similar to those used in our previous studies [8, 83]. Briefly, a gallium–aluminum–arsenide diode laser apparatus (Transverse Industries, Taiwan) with a center wavelength of 808 nm and an average radiant power of 110 mW per laser was used in the continuous operating mode. Laser beams were collimated using collimating lenses with a lens hood height of 11 mm. The beam shape was elliptical, and the major and minor axes of the laser beam at the horizontal plane of the front of the lens hood were 3.5 and 3.0 mm, respectively. Thus, the beam spot size and irradiance at the target (scalp surface) were 0.0825 cm2 and approximately 1.333 W/cm2, respectively. The exposure duration was 100 s, which yielded a radiant exposure of approximately 133.3 J/cm2 and a total radiant energy of 11 J/animal. The hair on the rats’ scalps was removed on the day of the experiment by using a depilatory cream. After marking the scalp by using an Eppendorf tube (internal diameter of 12 mm) with the center located on the skin corresponding to lambda, we gently wrapped the rats’ bodies in towels and used the mark on the scalp to line the inner edge of the lens hood. We irradiated each rat in the “VPA + tPBM + PTZ” group in only one treatment session with an exposure duration of 100 s (total radiant energy of 11.00 J). To minimize handling stress, the control animals in the VPA + PTZ groups were exposed to the same handling conditions, specifically concerning hair removal, body wrapping, and restraint, as those receiving tPBM, and their scalps were also attached to the laser apparatus for 100 s but with the power switched off.
Acute seizure induction
Acute seizures were induced by administering a subcutaneous injection of PTZ, as described in our previous study [8]. In brief, PTZ powder (Sigma-Aldrich, USA) was dissolved in saline to a concentration of 25 mg/mL and injected subcutaneously into the loose skin on the rats’ backs in a single dose of 90 mg/kg [84].
Seizure behavioral analysis
The rats were individually held in a transparent cage (42 × 42 × 21 cm) without animal bedding. The observation and video recording period for each rat lasted for 1 h, beginning 32–35 min after VPA injection and ending 1 h after PTZ injection. The time of seizure onset was instantly recorded by the observer during experiments. Seizure behavioral analysis was carried out with a 1 h post PTZ injection. Seizure behaviors were evaluated using the method reported by Lüttjohann et al. [85] with minor modifications as described in our previous study [8]. The intensity of seizures was as follows 1, sudden behavioral arrest and/or motionless staring; 2, facial jerking with the muzzle or muzzle and eye; 3, neck jerks; 4, clonic seizures in a sitting position; 5, convulsions including clonic and/or tonic–clonic seizures while lying on the belly and/or pure tonic seizures; and 6, convulsions including clonic and/or tonic–clonic seizures while lying on the side and/or wild jumping. A generalized tonic-clonic seizure (GTCS) refers to stage 5–6 seizures. Minor modifications were made as follows: we defined animal death as stage 7, mild seizures as stages 1–2, moderate seizures as stages 3–4, and severe seizures as stages 5–7. C. M. Tsai conducted the observations (one individual, once for each rat, with immediate recording of results in the laboratory notebook; camera recording was performed simultaneously) and scored seizure events. Thus, the scoring was conducted in a non-blinded manner.
We used the definition of SE reported by Sato and Woolley [86] and adjusted it according to the aforementioned seizure staging system. The onset of SE was recognized as stage 4–7 seizures [8] persisting for at least 30 s and continuing for no more than 2 min between seizures [8, 86].
During the 60 min of seizure behavioral observation, latencies to the onset of stage 1–6 seizures were evaluated during the 30-min period after PTZ injection [87]. If the latency to the seizure stage was absent, then the latency was considered to be 30 min (1800s) [88]. For stage 7 (death), the evaluation period was extended to 75 min for a rat in the PTZ group that died at 73 min. Therefore, if latencies to stage 7 were absent in all the rats alive 60 min after PTZ injection, then the latency was considered to be 75 min (5400 s).
Statistical analysis
Data are expressed as the mean ± standard error of mean (SEM). An unpaired Student’s t test was used to examine the differences between the maximum seizure stages, the total duration of stage 4–7 seizures, and the latency to the onset of stage 1–7 seizures between any two groups of interest. A p value of < 0.05 was considered statistically significant. All statistical analyses were performed using GraphPad Prism software (GraphPad, version 6).
Results
Wet-dog shaking was observed in all the rats after VPA injection
Wet-dog shaking (WDS) is a typical behavioral manifestation observed after VPA treatment [89]. All 33 rats exhibited WDS after VPA injection, indicating the effect of VPA on all rats.
Lower incidence rate of severe SE was observed in the rats treated with tPBM add-on therapy than untreated rats with low-dose VPA
Severe SE, which eventually led to death, was noted in three of the six rats (incidence rate: 50%) in the PTZ group. Although two of the six rats (incidence rate: 33%) in the VPA100 + PTZ group developed severe SE, one of them survived. Only one of the five rats in the VPA100 + tPBM + PTZ group developed severe SE (incidence rate: 20%); this incidence rate was lower than that in the VPA100 + PTZ group. This difference was attributable to only one rat. No rats that received medium- or high-dose VPA developed severe SE (Table 1).
Table 1.
Incidence of severe SE in each group
| Dose of VPA | Saline | tPBM + Saline | PTZ | VPA + PTZ | VPA + tPBM + PTZ |
|---|---|---|---|---|---|
| Low (100 mg/kg) | 0 | 0 | 50% (3/6) | 33% (2/6) | 20% (1/5) |
| Medium (200 mg/kg) | 0 | 0 | |||
| High (400 mg/kg) | 0 | 0 |
Data are presented as the percentage (rat numbers with severe SE/total rat numbers in the groups)
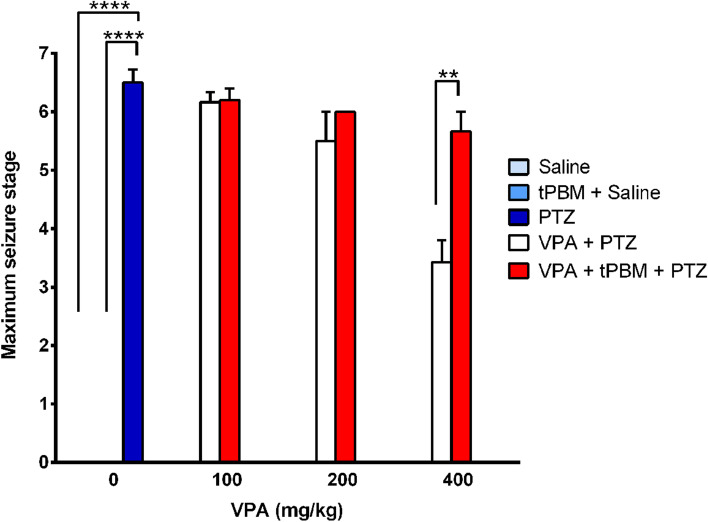
tPBM adding to high dose VPA significantly increased the maximum seizure stage
The maximum seizure stage in the PTZ group was 6.5 ± 0.2, which was significantly higher than that in the Saline group (stage 0, p < 0.0001) and tPBM + saline group (stage 0, p < 0.0001). When pretreated with a low-dose of VPA (100 mg/kg), the maximum seizure stages in both the VPA100 + PTZ and VPA100 + tPBM + PTZ groups were 6.2 ± 0.2. No significant difference in the maximum seizure stage was observed between the PTZ group and the rats treated with low-dose VPA. When pretreated with a medium-dose of VPA (200 mg/kg), the maximum seizure stages in the VPA200 + PTZ and VPA200 + tPBM + PTZ groups were 5.5 ± 0.5 and 6.0 ± 0, respectively. Thus, no significant difference between these two groups and between the low-dose VPA and medium-dose VPA groups with or without tPBM treatment. The maximum seizure stage that occurred in the VPA400 + PTZ group (3.4 ± 0.4) was significantly lower than that in the PTZ (6.5 ± 0.2, p < 0.0001) and VPA200 + PTZ groups (5.5 ± 0.5, p = 0.0060). However, the maximum seizure stage in the VPA400 + tPBM + PTZ group was 5.7 ± 0.3, and no significant differences in the maximum seizure stage were noted between the high-dose VPA and medium- or low-dose VPA groups among the rats receiving add-on therapy with tPBM. Furthermore, the maximum seizure stage in the VPA400 + tPBM + PTZ group was significantly higher than that in the VPA400 + PTZ group (p = 0.0067; Table 2 and Fig. 1). These findings indicated that add-on therapy with tPBM offsets the attenuation effect of a high dose of VPA on PTZ-induced seizures in terms of the maximum seizure stage.
Table 2.
Maximum seizure stage and total durations of stage 4–7 seizures
| Saline | tPBM + Saline | PTZ | VPA + PTZ | VPA + tPBM + PTZ | |||||
|---|---|---|---|---|---|---|---|---|---|
| VPA dosage (mg/kg) | 0 | 0 | 0 | 100 | 200 | 400 | 100 | 200 | 400 |
| Maximum seizure stages | 0a | 0a | 6.5 ± 0.2 | 6.2 ± 0.2 | 5.5 ± 0.5 | 3.4 ± 0.4 | 6.2 ± 0.2 | 6 ± 0 | 5.7 ± 0.3b |
| Total duration of stage 4–7 seizures (s) | 0 | 0 | 951.3 ± 394.7 | 676.8 ± 417.4 | 29 ± 7.1 | 2.6 ± 1.8 | 566.2 ± 526.2 | 57.4 ± 28 | 35.3 ± 11.1c |
Data are expressed as the mean ± SEM. The maximum seizure stage “0” in the tPBM + saline group indicated no seizures events
asignificant difference (p < 0.0001) in respect to the maximum seizure stage in the PTZ group
bsignificant difference (p < 0.01) in respect to the maximum seizure stage in the high-dose VPA (400 mg/kg) + PTZ group
csignificant difference (p < 0.01) in respect to the total duration of stage 4–7 seizures in the high-dose VPA (400 mg/kg) + PTZ group
Fig. 1.
Maximum seizure stages. The maximum seizure stages in the PTZ group are shown with blue bars. The maximum seizure stages in the low-dose, medium-dose, and high-dose VPA groups are depicted as white bars. The maximum seizure stages in the rats receiving VPA and tPBM are shown in red bars. **p < 0.01; ****p < 0.0001
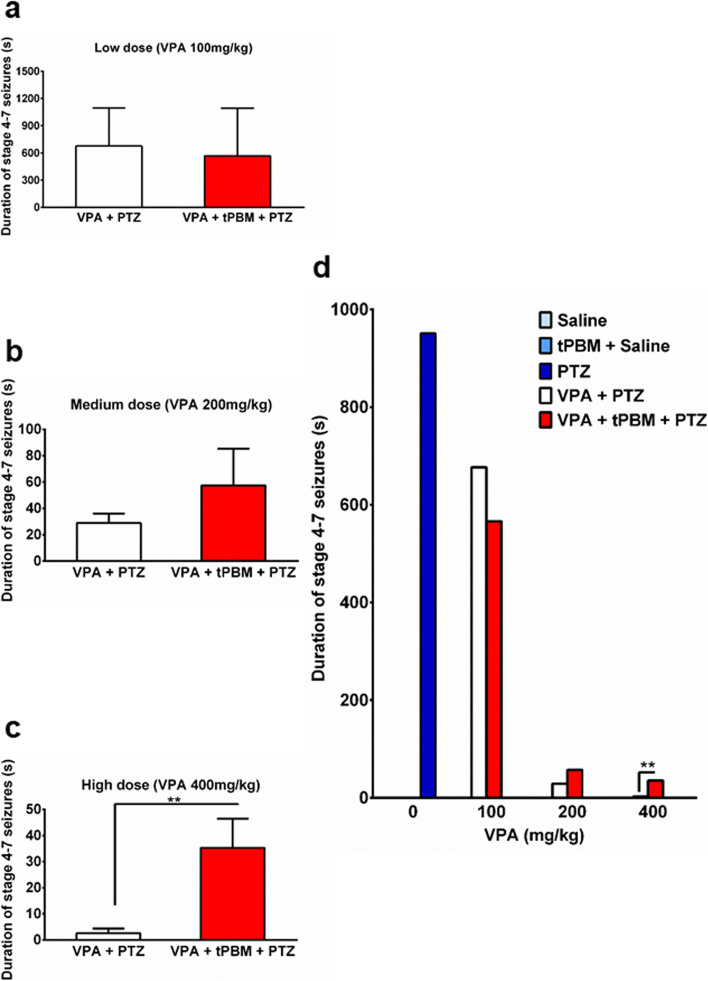
Add-on therapy of tPBM increased the total duration of stage 4–7 seizures in the high-dose VPA group
The total durations of stage 4–7 seizures were 951.3 ± 394.7 s, 676.8 ± 417.4 s, and 566.2 ± 526.2 s in the PTZ, VPA100 + PTZ, and VPA100 + tPBM + PTZ groups, respectively (Table 2, Fig. 2d). Although the mean total duration of stage 4–7 seizures with add-on tPBM was shorter than that without add-on tPBM among the rats receiving a low-dose of VPA, the differences was not significant (Table 2, Fig. 2a and d). At a medium dose of VPA, the total duration of stage 4–7 seizures in the VPA200 + tPBM + PTZ group was 29 ± 7.1 s, which was significantly shorter than that in the PTZ group (p = 0.0416). However, the total duration of stage 4–7 seizures in the rats receiving a medium dose of VPA with add-on tPBM (57.4 ± 28 s) was nonsignificantly longer than that in the rats receiving a medium dose of VPA without tPBM (Table 2, Fig. 2a and d). The total duration of stage 4–7 seizures in the VPA400 + PTZ group was 2.6 ± 1.8 s, which was significantly lower than that in the PTZ group (p = 0.0240) and VPA200 + PTZ (p = 0.0025) groups, respectively, and lower (but not significantly) than in the VPA100 + PTZ group (p = 0.1065). However, among the rats pretreated with a high dose of VPA, the total duration of stage 4–7 seizures with add-on tPBM therapy (35.3 ± 11.1 s) was significantly longer than that without add-on tPBM therapy (**p < 0.01 [p = 0.0018]; Table 2, Fig. 2c and d).
Fig. 2.
Total duration of stage 4–7 seizures. The total duration of stage 4–7 seizures in the (a) low-dose (100 mg/kg) VPA group (white bar) and low-dose VPA with tPBM add-on therapy (red bar); (b) medium-dose (200 mg/kg) VPA group (white bar) and medium-dose VPA with tPBM add-on therapy (red bar), and (c) high-dose VPA (400 mg/kg, white bar) and high-dose VPA with tPBM add-on therapy (red bar), **p < 0.01. d The total duration of stage 4–7 seizures for all the groups on the same scale (with unit of seconds). **p < 0.01
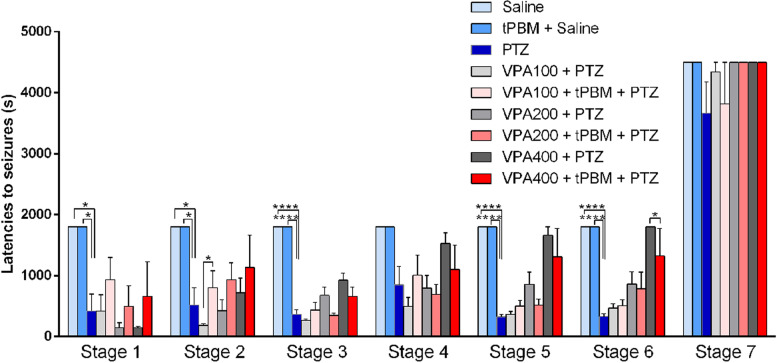
Adding tPBM to low-dose VPA significantly delayed the latency to stage 2 seizures, whereas adding tPBM to high-dose VPA significantly shortened the latency to stage 6 seizures
The latencies to stage 1–3 and 5–6 seizures were significantly shorter in the PTZ group than in the saline and tPBM + saline groups, respectively (p < 0.05 in the analysis of stage 1 and 2 seizures and p < 0.0001 in the analysis of stage 3, 5, and 6 seizures, Table 3 and Fig. 3). However, no significant difference in the latencies to stage 4 seizures and death (stage 7) was noted between these two groups. For the rats receiving a low dose of VPA, the latency to stage 2 seizures in the VPA100 + tPBM + PTZ group (799.2 ± 281.3 s) was significantly longer than the latency to stage 2 seizures in the VPA100 + PTZ group (185.7 ± 30.93 s, p = 0.0402, Table 3 and Fig. 3). In terms of the latencies to stage 1 and 3–7 seizures, no significant difference was observed between these two groups. For the rats receiving a medium dose of VPA, no significant difference was observed in all the stages between the tPBM treated and untreated groups. For the rats receiving a high dose of VPA, no significant difference in stage 1–5 seizures was noted between the tPBM-treated and untreated groups. However, the latency to stage 6 seizures was significantly shorter in the VPA400 + tPBM + PTZ group (1923 ± 922.1 s) than in the VPA400 + PTZ group (3600 ± 0 s, i.e., no occurrence of stage 6 seizures, p = 0.0160, Table 3 and Fig. 3).
Table 3.
Latencies to the onset of stage 1–7 seizures
| Saline | tPBM + Saline | PTZ | VPA + PTZ | VPA + tPBM + PTZ | |||||
|---|---|---|---|---|---|---|---|---|---|
| VPA dosage (mg/kg) | 0 | 0 | 0 | 100 | 200 | 400 | 100 | 200 | 400 |
| Stage 1 | 1800 ± 0a | 1800 ± 0a | 419.0 ± 280.2 | 415.8 ± 272.8 | 146.8 ± 80.17 | 147.9 ± 21.78 | 932.6 ± 366.7 | 495.6 ± 333.5 | 659.3 ± 570.4 |
| Stage 2 | 1800 ± 0b | 1800 ± 0b | 520.5 ± 280.4 | 185.7 ± 30.93 | 424.7 ± 180.3 | 716.1 ± 244.0 | 799.2 ± 281.3c | 931.8 ± 282.4 | 1136 ± 523.0 |
| Stage 3 | 1800 ± 0d | 1800 ± 0d | 369 ± 66.93 | 263.3 ± 28.31 | 676.2 ± 135.8 | 925.7 ± 121.3 | 433.6 ± 126.8 | 349.0 ± 36.93 | 659.3 ± 151.2 |
| Stage 4 | 1800 ± 0 | 1800 ± 0 | 851.2 ± 301.1 | 496.5 ± 146.0 | 795.5 ± 208.7 | 1527 ± 176.5 | 1009 ± 326.0 | 691.2 ± 164.0 | 1102 ± 397.9 |
| Stage 5 | 1800 ± 0e | 1800 ± 0e | 324.7 ± 41.53 | 367.2 ± 46.44 | 856.5 ± 205.3 | 1660 ± 140.0 | 498.4 ± 95.08 | 514.6 ± 101.0 | 1311 ± 463.1 |
| Stage 6 | 1800 ± 0f | 1800 ± 0f | 330.2 ± 41.77 | 466.5 ± 71.5 | 1161 ± 494.3 | 3600 ± 0 | 505.6 ± 93.93 | 1145 ± 621.8 | 1923 ± 922.1g |
| Stage 7 | 5400 ± 0 | 5400 ± 0 | 3667 ± 511.1 | 4340 ± 160.0 | 5400 ± 0 | 5400 ± 0 | 3816 ± 684.0 | 5400 ± 0 | 5400 ± 0 |
Data are expressed as the mean ± SEM
asignificant difference (p < 0.05) in respect to the latency to stage 1 seizures in the PTZ group
bsignificant difference (p < 0.05) in respect to the latency to stage 2 seizures in the PTZ group
csignificant difference (p < 0.05) in respect to the latency to stage 2 seizures in the low-dose VPA (100 mg/kg) + PTZ group
dsignificant difference (p < 0.0001) in respect to the latency to stage 3 seizures in the PTZ group
esignificant difference (p < 0.0001) in respect to the latency to stage 5 seizures in the PTZ group
fsignificant difference (p < 0.0001) in respect to the latency to stage 6 seizures in the PTZ group
gsignificant difference (p < 0.05) in respect to the latency to stage 6 seizures in the high-dose VPA (400 mg/kg) + PTZ group
Fig. 3.
Latencies to the onset of stage 1–7 seizures. The latency to the onset of stage 1–7 seizures in the tPBM + saline group (white bar), PTZ group (blue bar), low-dose (100 mg/kg) VPA group (light-gray bar), low-dose VPA with tPBM add-on therapy (pink bar), medium-dose (200 mg/kg) VPA group (gray bar), medium-dose VPA with tPBM add-on therapy (salmon pink bar), high-dose VPA (400 mg/kg, darkslategray bar), and high-dose VPA with tPBM add-on therapy (red bar), *p < 0.05; ****p < 0.0001
Discussion
The results of the present study demonstrated that the adding tPBM to low-dose VPA resulted in a beneficial synergistic effect on PTZ-induced seizures in the peripubertal rats. In addition, add-on therapy with tPBM could offset attenuation effect of a high dose of VPA on PTZ-induced seizures. A lower incidence rate of severe SE was observed in rats receiving tPBM add-on therapy than in those without tPBM treatment receiving a low dose of VPA. The add-on tPBM therapy and low-dose VPA significantly delayed the latency to stage 2 seizures. Moreover, the results revealed that add-on therapy of tPBM to high-dose VPA increased the maximum seizure stage, prolonged the total duration of stage 4–7 seizures, and shortened the latency to stage 6 seizures.
Adding tPBM to low-dose VPA significantly delayed the latency to stage 2 seizures. In view of clinical applications, reducing the dosage of VPA while maintaining or even increasing the therapeutic effect on seizures or CSE can be beneficial to patients with epilepsy because the adverse effects of VPA, such as hepatotoxicity and hyperammonemia, have been reported to be dose-dependent [20, 21]. In particular, patients with epilepsy with the mutated genotypes of the cytochrome P450 isozymes CYP2C9 and CYP2A6 are more vulnerable to VPA-induced hepatotoxicity [90]. Similarly, pediatric patients with epilepsy and who harbor the mutant alleles of CYP2C9 and CYP2A6 have a higher risk of VPA-induced hyperammonemia [91]. These patients, who presented a particularly problematic clinical scenario, may benefit from adding tPBM to low-dose VPA. Based on our results, reducing the dosage of VPA in pediatric patients with epilepsy and adding tPBM therapy can minimize VPA-induced hepatotoxicity and hyperammonemia, with the anticonvulsant efficacy maintained to a certain extent; however, additional basic and clinical studies are necessary to confirm these findings.
Adding tPBM to high-dose VPA exerted adverse effects on PTZ-induced seizures in terms of the maximum seizure stage, the total duration of stage 4–7 seizures, and the latency to stage 6 seizures. Thus according to these results, a low dose of or even a reduction in the VPA dosage should be considered when applying tPBM as an add-on therapy, but the combined use of tPBM with a high dose of VPA directly, without reducing the VPA dosage, should be avoided.
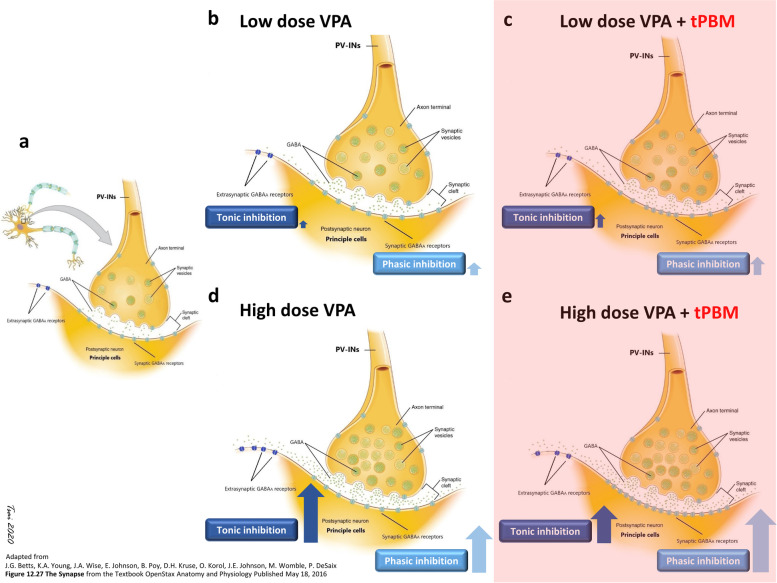
We observed that tPBM could offset the anticonvulsant effect of high-dose VPA; however, its underlying mechanisms remain to be elucidated. The transcranial administration of PBM preserved the perisomatic inhibition of PV-INs in rats with PTZ-induced SE [8]. After the absorption of NIR light by the CcO of PV-INs, CcO enhances ATP production, which increases the synthesis of GABA by PV-INs. Thus, the PV-INs preserved by tPBM release GABA in the postsynaptic GABAARs, a Cl−- selective ion channel, of principal cells. Hence, tPBM might indirectly act as a positive modulator of GABAARs by enhancing the presynaptic synthesis of GABA and the postsynaptic binding of GABA to GABAARs in principal cells. Radwan et al. [43] suggested that tPBM mimics the effects of AEDs such as BZD, barbiturates, and baclofen in their blocking effect on GABAB receptors (referring to the effect of tPBM as a positive modulator of GABAB receptors). The chemical convulsant used in this study, PTZ, is a GABAA receptor antagonist [92]. We previously demonstrated that tPBM attenuated PTZ-induced seizures [8]. Therefore, we speculated that tPBM could also act as a positive modulator of the GABAARs of hippocampal principal cells, thus offsetting the negative modulation of PTZ on GABAARs and consequently optimizing the binding of GABA released from PV-INs.
Adding tPBM therapy to VPA might indirectly modulate the GABAARs of principal cells. VPA increases GABA concentration by increasing presynaptic GABA synthesis and inhibiting GABA metabolism [93]. Most of the GABA released after VPA induction release of GABA binds to GABAARs rather than GABAB or GABAC receptors. Two forms of GABAARs exit with different subunit compositions and locations on the cell membrane of principal cells: synaptic GABAARs and extrasynaptic GABAARs. Synaptic GABAARs mediate phasic inhibition by responding to GABA released across the synaptic cleft. Binding to these low-affinity receptors results in a transient and rapidly desensitizing post-synaptic response on the order of milliseconds [94]. By contrast, extrasynaptic GABAARs have a high affinity to GABA and exhibit persistent tonic inhibition [95], which is a long-term inhibition [94]. A homeostatic competition might exist between phasic and tonic inhibition [96].
VPA increases GABA release from the axonal terminal of PV-INs and inhibits the reuptake of GABA. Most of the released GABA binds to synaptic GABAARs, and some GABA that escapes presynaptic reuptake [97] binds to the extrasynaptic GABAARs of principal cells. Along with the homeostatic competition between the phasic and tonic inhibition of GABAARs, the following hypothesis is proposed to explain the offsetting effects of adding tPBM to high-dose VPA (Fig. 4). Add-on tPBM might increase the release of GABA rom the axonal terminal of PV-INs at perisomatic inhibitory networks; this speculation is supported by our previous study [8]. In our experimental protocol, tPBM was added 30 min after VPA injection. Thus, in the low-dose VPA scenario (Fig. 4b), the phasic inhibition of synaptic GABAARs could be rapidly desensitized before the addition of tPBM. Therefore, synaptic GABAARs could once again be sensitized through binding with GABA released due to the addition of tPBM (Fig. 4c), with the result being a synergistic anticonvulsant effect facilitating by Cl− influx. However, only a limited amount of GABA that escaped from presynaptic reuptake through the GABA transporter reaches extrasynaptic GABAARs; hence, tonic inhibition was limited. Consequently, the rats receiving tPBM added to low-dose VPA still presented prominent SE. However, medium- and high-dose VPA may induce PV-INs to synthesize a large amount of GABA and cause the universal binding of GABA to its binding sites (GABA site) of both synaptic and extrasynaptic GABAARs, thus resulting in phasic and tonic inhibition, respectively. Long-term tonic inhibition effectively offsets the opposite action of PTZ on the picrotoxin site of GABAARs and eventually suppresses SE. Compared with the rats treated with a low dose of VPA, the rats treated with a high dose of VPA (Fig. 4d) had more extrasynaptic GABAARs that were bound to ambient GABA that strongly suppressed SE. However, compared with adding tPBM to low-dose VPA, tPBM added to high-dose VPA increased the synthesis and release of presynaptic GABA and its bindings to synaptic GABAARs were more than those in synaptic GABAARs with low-dose VPA added-on with tPBM. When increased phasic inhibition occurs in principal cells after treatment with add-on tPBM and high-dose VPA, phasic inhibition might have competed with tonic inhibition [96]. Therefore, low tonic inhibition exacerbates SE compared with high-dose VPA without tPBM (Fig. 4e, the schematic diagram is shown in Fig. 4). The aforementioned hypothesis was based on the findings of this study. Additional studies are required to confirm the hypothesis.
Fig. 4.
Schematic of the proposed conjecture of GABAA receptors in low-dose VPA with and without add-on tPBM therapy. Dynamic changes in phasic inhibition generated by the binding of GABA (green dots) to synaptic GABAARs (depicted as light blue) and tonic inhibition caused by the binding of GABA to extrasynaptic GABAARs (dark blue) on the postsynaptic neurons of principal cells are shown. The scenarios with add-on tPBM are depicted with a light red background. a Without VPA or tPBM treatment, only PTZ was injected, and a baseline amount of GABA was released at the synaptic cleft, with some binding to synaptic GABAARs. b When parvalbumin-positive interneurons (PV-INs), the presynaptic neurons, received low-dose VPA, only a limited amount of GABA was bound to synaptic and extrasynaptic GABAARs, thus resulting in limited phasic inhibition (light blue arrow) and tonic inhibition (dark blue arrow). However, phasic inhibition only lasted for milliseconds and was already desensitized upon PTZ injection. c In the scenario of low-dose VPA with add-on tPBM, slightly more GABAs was bound to synaptic and extrasynaptic GABAARs after add-on tPBM compared with low-dose VPA without add-on tPBM. Therefore, new phasic inhibition and more tonic inhibition might contribute to the increased attenuation of SE relative to low-dose VPA without add-on tPBM. d In the high-dose VPA group, a large amount of GABA was produced and released from the axons of PV-INs. The abundant amount of GABA was not only bound to synaptic GABAARs and caused transient phasic inhibition but also effectively diffused to extrasynaptic GABAARs, thus resulting in considerable tonic inhibition after VPA injection; this long-term inhibition could last after PTZ injection, thus resulting in the longest suppression of SE. e Adding tPBM to high-dose VPA increased the preexisting large amount of presynaptic GABA production and release that were stimulated by high-dose VPA injection. A large amount of GABA was bound to synaptic GABAARs, thus resulting in high phasic inhibition, which competes with tonic inhibition and subsequently reduces phasic inhibition. Therefore, the suppression of PTZ-induced SE was inhibited. The use of the material in Fig. 4 was permitted under the Creative Commons Attribution 4.0 International license (https://creativecommons.org/licenses/by/4.0/deed.en) of the “File:1225 Chemical Synapse.jpg” from Wikimedia Commons (the free media repository [https://commons.wikimedia.org/wiki/File:1225_Chemical_Synapse.jpg]). Changes were made, and the original artwork is credited to J.G. Betts, K.A. Young, J.A. Wise, E. Johnson, B. Poe, D.H. Kruse, O. Korol, J.E. Johnson, M. Womble, P. Desaix for their “Figure 12.27 Synapse” from the Textbook OpenStax Anatomy and Physiology, published on May 18, 2016 (source: https://openstax.org/books/anatomy-and-physiology/pages/12-5-communication-between-neurons)
Add-on tPBM might directly modulate GABAARs. Visible and ultraviolet light directly modulate GABAARs [98] and the GABAAR-mediated currents of cortical neurons [99]. We assumed that tPBM with a wavelength of 808 nm directly modulates GABAARs through an unknown mechanism and acts as a positive modulator. Likewise, adding tPBM to low-dose VPA might directly and positively modulate the GABAAR-induced current and enhance phasic inhibition and a portion of tonic inhibition; the addition of tPBM to high-dose VPA might considerably enhance phasic inhibition and suppress tonic inhibition due to homeostatic competition between phasic and tonic inhibition [96].
Limitations and future work
This study has some limitations. Because this study was performed in a non-blinded manner, it lacked interobserver and intraobserver reliability. A small sample size was included in this study. Therefore, the lower incidence rate of severe SE in the VPA100 + tPBM + PTZ group than in the VPA100 + PTZ group was attributable to only one rat, and this finding was not sufficient to infer that the lower incidence was due to add-on tPBM therapy. Regarding the tPBM protocol, the single irradiation administered in this study may be a limitation because it did not mimic regular tPBM maintenance treatment for CSE prevention. For better bench-to-bed translation of regular tPBM add-on to VPA for CSE prevention, experimental designs involving repetitive tPBM, such as irradiation once daily, should be considered in future studies. Moreover, irradiance at the target in this study was higher than 1 W/cm2, which might generate heat over the scalp [100]. Additionally, the thermal effect was not evaluated in this study. However, the photothermal effects of tPBM are less likely to occur in the brain tissue due to poor heat penetration deep into the brain [101], and the superficial heat of the skin and scalp did not affect the therapeutic effect of tPBM due to CcO and cerebral hemodynamics [100]. However, future studies should examine the calibration of thermal effect. Furthermore, the optimal conditions should be determined for use of tPBM as an add-on therapy to VPA or even other AEDs. More convulsive doses for single injection of PTZ model and PTZ kindling model with more time-points of sub-convulsive dose PTZ injection should be also considered to verify the synergistic anticonvulsive effects of tPBM add-on to AEDs in future works. As for VPA, synergistic effect of tPBM was shown when added-up to low-dose VPA. VPA with lower doses than 100 mg/kg should be designed in future works. In this study, we didn’t check safety indicators of add-on therapy of tPBM to VPA including the hepatic and renal function, hemograms including white blood cells and platelets, and these should be included in future works. Future studies should perform histopathological examinations of rat brains, especially the hippocampus; such examinations should include hematoxylin and eosin staining for neuronal damage, TUNEL assay for apoptosis, and propidium iodide staining for necrosis, and electron pathology study for examining mitochondrial morphology. Finally, more future experiments are needed to be designed to demonstrate the synergistic effects of tPBM add-on to AEDs on seizures. To enable the application of tPBM add-on therapy in patients, studies in human cells are warranted. In view of the current progress of epilepsy patient–derived induced pluripotent stem cells platforms for seizure studies [102], additional experiments applying tPBM as an added-on to AEDs in these models should be performed.
Conclusions
In this study, we demonstrated that VPA pretreatment with tPBM add-on therapy (combination therapy and polytherapy) exerted a significant statistical synergistic effect that delayed the latency to stage 2 seizures. However, tPBM add-on therapy to medium- and high-dose VPA increased the maximum seizure stage and prolonged the total duration of stage 4–7 seizures. In terms of future CSE prevention strategies, the application of tPBM add-on therapy to low-dose rather than medium- or high-dose VPA for pediatric patients, especially pubertal patients with CSE, could allow for a reduction in the VPA dosage, thus minimizing its side effects such as hepatotoxicity while maintaining therapeutic efficacy once an optimal protocol is established.
Acknowledgements
We thank Professor Geng-Chang Yeh for initiating and guiding the direction of VPA treatment with tPBM add-on therapy by using PTZ-induced SE. We thank Yu Shan Lin for valuable discussions. We thank Chia-Wei Chiang for assisting in a portion of the experiments. We thank Dr. Sung-Tse Li for sharing the concept of VPA-cytochrome P450 hepatotoxicity. We thank Dr. Min-Lan Tsai for sharing the information on the RNS system. We thank Uni-edit (http://www.uniedit.net) and Wallace Academic Editing (https://www.editing.tw/) for editing and proofreading this manuscript.
Abbreviations
- CSE
Convulsive status epilepticus
- VPA
Valproic acid
- PBM
Photobiomodulation
- NIR
Near-infrared
- CcO
Cytochrome c oxidase
- tPBM
Transcranial photobiomodulation
- PTZ
Pentylenetetrazole
- AEDs
Antiepileptic drugs
- BZD
Benzodiazepine
- SE
Status epilepticus
- sIPSCs
Spontaneous inhibitory postsynaptic currents
- GABA
γ-amino butyric acid
- GABAARs
GABAA receptors
- NMDA
N-methyl-D-aspartate
- PV
Parvalbumin
- INs
Interneurons
- PV-INs
Parvalbumin-positive interneurons
- TUNEL
Terminal deoxynucleotidyl transferase dUTP nick end labeling
- LDR
Low-dose gamma irradiation
- LLLT
Low-level laser (light) therapy
- GTCS
Generalized tonic–clonic seizures
- WDS
Wet-dog shaking
Authors’ contributions
CMT and HC conceived and designed the experiments. CMT performed the experiments and analyzed the data. CMT and HC wrote the manuscript. SFC and HC instructed the manuscript preparation and the submission strategy. All authors have read and approved the final manuscript.
Funding
No funding was received.
Availability of data and materials
The data used and analyzed during the current study are available from the corresponding author.
Declarations
Ethics approval and consent to participate
The study followed the Animal Protection Act, Council of Agriculture, Executive Yuan, Taiwan, complied with the ARRIVE guidelines, the Basel Declaration and the 3R concept, and was approved by the Laboratory Animal Center of Taipei Medical University (Protocol LAC-2019-0237).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Loddenkemper T, Syed TU, Ramgopal S, Gulati D, Thanaviratananich S, Kothare SV, et al. Risk factors associated with death in in-hospital pediatric convulsive status epilepticus. PLoS One. 2012;7(10):e47474. doi: 10.1371/journal.pone.0047474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lin KL, Lin JJ, Hsia SH, Wu CT, Wang HS. Analysis of convulsive status epilepticus in children of Taiwan. Pediatr Neurol. 2009;41(6):413–418. doi: 10.1016/j.pediatrneurol.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 3.Raspall-Chaure M, Chin RF, Neville BG, Scott RC. Outcome of paediatric convulsive status epilepticus: a systematic review. Lancet Neurol. 2006;5(9):769–779. doi: 10.1016/S1474-4422(06)70546-4. [DOI] [PubMed] [Google Scholar]
- 4.Amengual-Gual M, Ulate-Campos A, Loddenkemper T. Status epilepticus prevention, ambulatory monitoring, early seizure detection and prediction in at-risk patients. Seizure. 2019;68:31–37. doi: 10.1016/j.seizure.2018.09.013. [DOI] [PubMed] [Google Scholar]
- 5.Premarket Approval (PMA) 2021. Available from: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfPMA/pma.cfm?id=P100026.
- 6.Iyengar S, Shafer PO. Responsive Neurostimulation (RNS) 2017. Available from: https://www.epilepsy.com/learn/treating-seizures-and-epilepsy/devices/responsive-neurostimulation-rns.
- 7.Nair DR, Laxer KD, Weber PB, Murro AM, Park YD, Barkley GL, et al. Nine-year prospective efficacy and safety of brain-responsive neurostimulation for focal epilepsy. Neurology. 2020;95(9):e1244–e1e56. doi: 10.1212/WNL.0000000000010154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tsai CM, Chang SF, Chang H. Transcranial photobiomodulation attenuates pentylenetetrazole-induced status epilepticus in peripubertal rats. J Biophotonics. 2020;13(8):e202000095. doi: 10.1002/jbio.202000095. [DOI] [PubMed] [Google Scholar]
- 9.Stacey WC. Seizure prediction is possible-now Let's make it practical. EBioMedicine. 2018;27:3–4. doi: 10.1016/j.ebiom.2018.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chamberlain JM, Kapur J, Shinnar S, Elm J, Holsti M, Babcock L, et al. Efficacy of levetiracetam, fosphenytoin, and valproate for established status epilepticus by age group (ESETT): a double-blind, responsive-adaptive, randomised controlled trial. Lancet. 2020;395(10231):1217–1224. doi: 10.1016/S0140-6736(20)30611-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Singh A, Stredny CM, Loddenkemper T. Pharmacotherapy for pediatric convulsive status Epilepticus. CNS Drugs. 2020;34(1):47–63. doi: 10.1007/s40263-019-00690-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tseng YL, Huang CR, Lin CH, Lu YT, Lu CH, Chen NC, et al. Risk factors of hyperammonemia in patients with epilepsy under valproic acid therapy. Medicine (Baltimore) 2014;93(11):e66. doi: 10.1097/MD.0000000000000066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sridharan K, Daylami AA, Ajjawi R, Ajooz H. Drug-induced liver injury in critically ill children taking antiepileptic drugs: a retrospective study. Curr Ther Res Clin Exp. 2020;92:100580. doi: 10.1016/j.curtheres.2020.100580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Powell-Jackson PR, Tredger JM, Williams R. Hepatotoxicity to sodium valproate: a review. Gut. 1984;25(6):673–681. doi: 10.1136/gut.25.6.673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lal A, Bapna JS. Drug-induced hepatotoxicity. Natl Med J India. 1996;9(5):227–230. [PubMed] [Google Scholar]
- 16.Pineiro-Carrero VM, Pineiro EO. Liver. Pediatrics. 2004;113(4 Suppl):1097–1106. [PubMed] [Google Scholar]
- 17.Squires RH, Jr, Shneider BL, Bucuvalas J, Alonso E, Sokol RJ, Narkewicz MR, et al. Acute liver failure in children: the first 348 patients in the pediatric acute liver failure study group. J Pediatr. 2006;148(5):652–658. doi: 10.1016/j.jpeds.2005.12.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jurima-Romet M, Abbott FS, Tang W, Huang HS, Whitehouse LW. Cytotoxicity of unsaturated metabolites of valproic acid and protection by vitamins C and E in glutathione-depleted rat hepatocytes. Toxicology. 1996;112(1):69–85. doi: 10.1016/0300-483x(96)03352-5. [DOI] [PubMed] [Google Scholar]
- 19.Shakya R, Hoque MK, Sapkota AS, Gupta PK. Differential hepatotoxic effects of sodium valproate at different doses in albino rats. Kathmandu Univ Med J (KUMJ) 2018;16(61):78–82. [PubMed] [Google Scholar]
- 20.Sussman NM, McLain LW., Jr A direct hepatotoxic effect of valproic acid. JAMA. 1979;242(11):1173–1174. [PubMed] [Google Scholar]
- 21.Vázquez M, Fagiolino P, Maldonado C, Olmos I, Ibarra M, Alvariza S, et al. Hyperammonemia associated with Valproic acid concentrations. Biomed Res Int. 2014;2014:217269. [DOI] [PMC free article] [PubMed]
- 22.Anders JJ, Lanzafame RJ, Arany PR. Low-level light/laser therapy versus photobiomodulation therapy. Photomed Laser Surg. 2015;33(4):183–184. doi: 10.1089/pho.2015.9848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hamblin F, Huang, de Freitas, Carroll. Low-level light therapy: Photobiomodulation. Bellingham: SPIE; 2018. p. 1. [Google Scholar]
- 24.Karu T. Primary and secondary mechanisms of action of visible to near-IR radiation on cells. J Photochem Photobiol B. 1999;49(1):1–17. doi: 10.1016/S1011-1344(98)00219-X. [DOI] [PubMed] [Google Scholar]
- 25.Wang X, Dmochowski JP, Zeng L, Kallioniemi E, Husain M, Gonzalez-Lima F, et al. Transcranial photobiomodulation with 1064-nm laser modulates brain electroencephalogram rhythms. Neurophotonics. 2019;6(2):025013. doi: 10.1117/1.NPh.6.2.025013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.de Freitas LF, Hamblin MR. Proposed mechanisms of Photobiomodulation or low-level light therapy. IEEE J Sel Top Quantum Electron. 2016;22(3):348–364. doi: 10.1109/JSTQE.2016.2561201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hamblin MR. Mechanisms and applications of the anti-inflammatory effects of photobiomodulation. AIMS Biophys. 2017;4(3):337–361. doi: 10.3934/biophy.2017.3.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shanks S, Leisman G. Perspective on broad-acting clinical physiological effects of Photobiomodulation. Adv Exp Med Biol. 2018;1096:41–52. doi: 10.1007/5584_2018_188. [DOI] [PubMed] [Google Scholar]
- 29.Wang X, Tian F, Reddy DD, Nalawade SS, Barrett DW, Gonzalez-Lima F, et al. Up-regulation of cerebral cytochrome-c-oxidase and hemodynamics by transcranial infrared laser stimulation: a broadband near-infrared spectroscopy study. J Cereb Blood Flow Metab. 2017;37(12):3789–3802. doi: 10.1177/0271678X17691783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang X, Tian F, Soni SS, Gonzalez-Lima F, Liu H. Interplay between up-regulation of cytochrome-c-oxidase and hemoglobin oxygenation induced by near-infrared laser. Sci Rep. 2016;6:30540. doi: 10.1038/srep30540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Uozumi Y, Nawashiro H, Sato S, Kawauchi S, Shima K, Kikuchi M. Targeted increase in cerebral blood flow by transcranial near-infrared laser irradiation. Lasers Surg Med. 2010;42(6):566–576. doi: 10.1002/lsm.20938. [DOI] [PubMed] [Google Scholar]
- 32.Xuan W, Agrawal T, Huang L, Gupta GK, Hamblin MR. Low-level laser therapy for traumatic brain injury in mice increases brain derived neurotrophic factor (BDNF) and synaptogenesis. J Biophotonics. 2015;8(6):502–511. doi: 10.1002/jbio.201400069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liang HL, Whelan HT, Eells JT, Meng H, Buchmann E, Lerch-Gaggl A, et al. Photobiomodulation partially rescues visual cortical neurons from cyanide-induced apoptosis. Neuroscience. 2006;139(2):639–649. doi: 10.1016/j.neuroscience.2005.12.047. [DOI] [PubMed] [Google Scholar]
- 34.Salehpour M, Kamari S-E, Rasta H. Brain Photobiomodulation therapy: a narrative review. Mol Neurobiol. 2018;55(8):6601–6636. doi: 10.1007/s12035-017-0852-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huang YY, Nagata K, Tedford CE, McCarthy T, Hamblin MR. Low-level laser therapy (LLLT) reduces oxidative stress in primary cortical neurons in vitro. J Biophotonics. 2013;6(10):829–838. doi: 10.1002/jbio.201200157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Figueiro Longo MG, Tan CO, Chan ST, Welt J, Avesta A, Ratai E, et al. Effect of Transcranial low-level light therapy vs sham therapy among patients with moderate traumatic brain injury: a randomized clinical trial. JAMA Netw Open. 2020;3(9):e2017337. doi: 10.1001/jamanetworkopen.2020.17337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Santos L, Olmo-Aguado SD, Valenzuela PL, Winge K, Iglesias-Soler E, Arguelles-Luis J, et al. Photobiomodulation in Parkinson's disease: a randomized controlled trial. Brain Stimul. 2019;12(3):810–812. doi: 10.1016/j.brs.2019.02.009. [DOI] [PubMed] [Google Scholar]
- 38.Chan AS, Lee TL, Yeung MK, Hamblin MR. Photobiomodulation improves the frontal cognitive function of older adults. Int J Geriatr Psychiatry. 2019;34(2):369–377. doi: 10.1002/gps.5039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Leisman G, Machado C, Machado Y, Chinchilla-Acosta M. Effects of low-level laser therapy in autism Spectrum disorder. Adv Exp Med Biol. 2018;1116:111–130. doi: 10.1007/5584_2018_234. [DOI] [PubMed] [Google Scholar]
- 40.Cassano P, Dording C, Thomas G, Foster S, Yeung A, Uchida M, et al. Effects of transcranial photobiomodulation with near-infrared light on sexual dysfunction. Lasers Surg Med. 2019;51(2):127–135. doi: 10.1002/lsm.23011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kerppers FK, Dos Santos K, Cordeiro MER, da Silva Pereira MC, Barbosa D, Pezzini AA, et al. Study of transcranial photobiomodulation at 945-nm wavelength: anxiety and depression. Lasers Med Sci. 2020;35(9):1945–1954. doi: 10.1007/s10103-020-02983-7. [DOI] [PubMed] [Google Scholar]
- 42.Zaizar ED, Gonzalez-Lima F, Telch MJ. Singular and combined effects of transcranial infrared laser stimulation and exposure therapy: a randomized clinical trial. Contemp Clin Trials. 2018;72:95–102. doi: 10.1016/j.cct.2018.07.012. [DOI] [PubMed] [Google Scholar]
- 43.Radwan NM, El Hay Ahmed NA, Ibrahim KM, Khedr ME, Aziz MA, Khadrawy YA. Effect of infrared laser irradiation on amino acid neurotransmitters in an epileptic animal model induced by pilocarpine. Photomed Laser Surg. 2009;27(3):401–409. doi: 10.1089/pho.2008.2275. [DOI] [PubMed] [Google Scholar]
- 44.Vogel DDS, Ortiz-Villatoro NN, de Freitas L, Aimbire F, Scorza FA, Albertini R, et al. Repetitive transcranial photobiomodulation but not long-term omega-3 intake reduces epileptiform discharges in rats with stroke-induced epilepsy. J Biophotonics. 2020;14(1):e202000287. [DOI] [PubMed]
- 45.Ben-Ari Y, Tremblay E, Ottersen OP. Injections of kainic acid into the amygdaloid complex of the rat: an electrographic, clinical and histological study in relation to the pathology of epilepsy. Neuroscience. 1980;5(3):515–528. doi: 10.1016/0306-4522(80)90049-4. [DOI] [PubMed] [Google Scholar]
- 46.Ahmed R, Ibrahim K, Aziz E, Khadrawy. Effect of three different intensities of infrared laser energy on the levels of amino acid neurotransmitters in the cortex and hippocampus of rat brain. Photomed Laser Surg. 2008;26(5):479–488. doi: 10.1089/pho.2007.2190. [DOI] [PubMed] [Google Scholar]
- 47.Hong N. Photobiomodulation as a treatment for neurodegenerative disorders: current and future trends. Biomed Eng Lett. 2019;9(3):359–366. doi: 10.1007/s13534-019-00115-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Iwase T, Hori N, Morioka T. Possible mechanisms of the he-ne laser effects on the cell membrane characteristics. Lasers Surg Med. 1988;4:166–171. [Google Scholar]
- 49.Shimoyama M, Fukuda Y, Shimoyama N, Iijima K, Mizuguchi T. Effect of he-ne laser irradiation on synaptic transmission of the superior cervical sympathetic ganglion in the rat. J Clin Laser Med Surg. 1992;10(5):337–342. doi: 10.1089/clm.1992.10.337. [DOI] [PubMed] [Google Scholar]
- 50.Kataoka Y, Cui Y, Maegawa Y, Ito T, Watanabe Y. Direct and suppressive action of photon on brain neurotransmission. Jpn J Physiol. 2000;50:S166. [Google Scholar]
- 51.Wu XY, Mou ZX, Hou WS, Zheng XL, Yao JP, Shang GB, et al. Irradiation of 850-nm laser light changes the neural activities in rat primary visual cortex. Lasers Med Sci. 2013;28(3):791–798. doi: 10.1007/s10103-012-1160-x. [DOI] [PubMed] [Google Scholar]
- 52.Yoo M, Koo H, Kim M, Kim HI, Kim S. Near-infrared stimulation on globus pallidus and subthalamus. J Biomed Opt. 2013;18(12):128005. doi: 10.1117/1.JBO.18.12.128005. [DOI] [PubMed] [Google Scholar]
- 53.Feng HJ, Kao C, Gallagher MJ, Jansen ED, Mahadevan-Jansen A, Konrad PE, et al. Alteration of GABAergic neurotransmission by pulsed infrared laser stimulation. J Neurosci Methods. 2010;192(1):110–114. doi: 10.1016/j.jneumeth.2010.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yis U, Topcu Y, Ozbal S, Tugyan K, Bayram E, Karakaya P, et al. Caffeic acid phenethyl ester prevents apoptotic cell death in the developing rat brain after pentylenetetrazole-induced status epilepticus. Epilepsy Behav. 2013;29(2):275–280. doi: 10.1016/j.yebeh.2013.08.002. [DOI] [PubMed] [Google Scholar]
- 55.Hansen SL, Sperling BB, Sanchez C. Anticonvulsant and antiepileptogenic effects of GABAA receptor ligands in pentylenetetrazole-kindled mice. Prog Neuro-Psychopharmacol Biol Psychiatry. 2004;28(1):105–113. doi: 10.1016/j.pnpbp.2003.09.026. [DOI] [PubMed] [Google Scholar]
- 56.Ahmed A, Chikuma K. Pentylenetetrazol-induced seizures affect the levels of prolyl oligopeptidase, thimet oligopeptidase and glial proteins in rat brain regions, and attenuation by MK-801 pretreatment. Neurochem Int. 2005;47(4):248–259. doi: 10.1016/j.neuint.2005.04.025. [DOI] [PubMed] [Google Scholar]
- 57.Corda MG, Orlandi M, Lecca D, Giorgi O. Decrease in GABAergic function induced by pentylenetetrazol kindling in rats: antagonism by MK-801. J Pharmacol Exp Ther. 1992;262(2):792–800. [PubMed] [Google Scholar]
- 58.Golovynska I, Golovynskyi S, Stepanov YV, Garmanchuk LV, Stepanova LI, Qu J, et al. Red and near-infrared light induces intracellular Ca (2+) flux via the activation of glutamate N-methyl-D-aspartate receptors. J Cell Physiol. 2019;234:15989–16002. doi: 10.1002/jcp.28257. [DOI] [PubMed] [Google Scholar]
- 59.Gulyas AI, Buzsaki G, Freund TF, Hirase H. Populations of hippocampal inhibitory neurons express different levels of cytochrome c. Eur J Neurosci. 2006;23(10):2581–2594. doi: 10.1111/j.1460-9568.2006.04814.x. [DOI] [PubMed] [Google Scholar]
- 60.Hu H, Gan J, Jonas P. Interneurons. Fast-spiking, parvalbumin(+) GABAergic interneurons: from cellular design to microcircuit function. Science. 2014;345(6196):1255263. doi: 10.1126/science.1255263. [DOI] [PubMed] [Google Scholar]
- 61.Kim JE, Kang TC. p47Phox/CDK5/DRP1-mediated mitochondrial fission evokes PV cell degeneration in the rat dentate Gyrus following status Epilepticus. Front Cell Neurosci. 2017;11:267. doi: 10.3389/fncel.2017.00267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tucker LD, Lu Y, Dong Y, Yang L, Li Y, Zhao N, et al. Photobiomodulation therapy attenuates hypoxic-ischemic injury in a neonatal rat model. J Mol Neurosci. 2018;65(4):514–526. doi: 10.1007/s12031-018-1121-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sahin S, Gurgen SG, Yazar U, Ince I, Kamasak T, Acar Arslan E, et al. Vitamin D protects against hippocampal apoptosis related with seizures induced by kainic acid and pentylenetetrazol in rats. Epilepsy Res. 2019;149:107–116. doi: 10.1016/j.eplepsyres.2018.12.005. [DOI] [PubMed] [Google Scholar]
- 64.Lotfy DM, Safar MM, Mohamed SH, Kenawy SA. Effect of valproic acid alone or combined with low dose gamma irradiation in modulating PTZ-induced convulsions in rats involving AKT/m-TOR pathway. Life Sci. 2018;212:261–266. doi: 10.1016/j.lfs.2018.10.007. [DOI] [PubMed] [Google Scholar]
- 65.Fucic A, Brunborg G, Lasan R, Jezek D, Knudsen LE, Merlo DF. Genomic damage in children accidentally exposed to ionizing radiation: a review of the literature. Mutat Res. 2008;658(1–2):111–123. doi: 10.1016/j.mrrev.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 66.Arias JL, Mendez M, Martinez JA, Arias N. Differential effects of photobiomodulation interval schedules on brain cytochrome c-oxidase and proto-oncogene expression. Neurophotonics. 2020;7(4):045011. doi: 10.1117/1.NPh.7.4.045011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Li R, Liu Y, Chen N, Zhang Y, Song G, Zhang Z. Valproate attenuates nitroglycerin-induced Trigeminovascular activation by preserving mitochondrial function in a rat model of migraine. Med Sci Monit. 2016;22:3229–3237. doi: 10.12659/MSM.900185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Li Q, Li QQ, Jia JN, Cao S, Wang ZB, Wang X, et al. Sodium valproate ameliorates neuronal apoptosis in a Kainic acid model of epilepsy via enhancing PKC-dependent GABAAR gamma2 serine 327 phosphorylation. Neurochem Res. 2018;43(12):2343–2352. doi: 10.1007/s11064-018-2659-8. [DOI] [PubMed] [Google Scholar]
- 69.Langer M, Brandt C, Zellinger C, Loscher W. Therapeutic window of opportunity for the neuroprotective effect of valproate versus the competitive AMPA receptor antagonist NS1209 following status epilepticus in rats. Neuropharmacology. 2011;61(5–6):1033–1047. doi: 10.1016/j.neuropharm.2011.06.015. [DOI] [PubMed] [Google Scholar]
- 70.Tan NN, Tang HL, Lin GW, Chen YH, Lu P, Li HJ, et al. Epigenetic Downregulation of Scn3a expression by valproate: a possible role in its anticonvulsant activity. Mol Neurobiol. 2017;54(4):2831–2842. doi: 10.1007/s12035-016-9871-9. [DOI] [PubMed] [Google Scholar]
- 71.Jessberger S, Nakashima K, Clemenson GD, Jr, Mejia E, Mathews E, Ure K, et al. Epigenetic modulation of seizure-induced neurogenesis and cognitive decline. J Neurosci. 2007;27(22):5967–5975. doi: 10.1523/JNEUROSCI.0110-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.de Farias GA, Wagner VP, Correa C, Webber LP, Pilar EFS, Curra M, et al. Photobiomodulation therapy modulates epigenetic events and NF-kappaB expression in oral epithelial wound healing. Lasers Med Sci. 2019;34(7):1465–1472. doi: 10.1007/s10103-019-02745-0. [DOI] [PubMed] [Google Scholar]
- 73.Zamani ARN, Saberianpour S, Geranmayeh MH, Bani F, Haghighi L, Rahbarghazi R. Modulatory effect of photobiomodulation on stem cell epigenetic memory: a highlight on differentiation capacity. Lasers Med Sci. 2020;35(2):299–306. doi: 10.1007/s10103-019-02873-7. [DOI] [PubMed] [Google Scholar]
- 74.Gage GJ, Kipke DR, Shain W. Whole animal perfusion fixation for rodents. J Vis Exp. 2012;65:3564. [DOI] [PMC free article] [PubMed]
- 75.Chow R, Yan W, Armati P. Electrophysiological effects of single point transcutaneous 650 and 808 nm laser irradiation of rat sciatic nerve: a study of relevance for low-level laser therapy and laser acupuncture. Photomed Laser Surg. 2012;30(9):530–535. doi: 10.1089/pho.2012.3248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Yan W, Chow R, Armati PJ. Inhibitory effects of visible 650-nm and infrared 808-nm laser irradiation on somatosensory and compound muscle action potentials in rat sciatic nerve: implications for laser-induced analgesia. J Peripher Nerv Syst. 2011;16(2):130–135. doi: 10.1111/j.1529-8027.2011.00337.x. [DOI] [PubMed] [Google Scholar]
- 77.Brevard ME, Kulkarni P, King JA, Ferris CF. Imaging the neural substrates involved in the genesis of pentylenetetrazol-induced seizures. Epilepsia. 2006;47(4):745–754. doi: 10.1111/j.1528-1167.2006.00502.x. [DOI] [PubMed] [Google Scholar]
- 78.Hosseini M, Sadeghnia HR, Salehabadi S, Alavi H, Gorji A. The effect of L-arginine and L-NAME on pentylenetetrazole induced seizures in ovariectomized rats, an in vivo study. Seizure. 2009;18(10):695–698. doi: 10.1016/j.seizure.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 79.Liu LM, Wang N, Lu Y, Wang WP. Edaravone acts as a potential therapeutic drug against pentylenetetrazole-induced epilepsy in male albino rats by downregulating cyclooxygenase-II. Brain Behav. 2019;9(1):e01156. doi: 10.1002/brb3.1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Biggs CS, Pearce BR, Fowler LJ, Whitton PS. The effect of sodium valproate on extracellular GABA and other amino acids in the rat ventral hippocampus: an in vivo microdialysis study. Brain Res. 1992;594(1):138–142. doi: 10.1016/0006-8993(92)91038-g. [DOI] [PubMed] [Google Scholar]
- 81.Sadek B, Saad A, Schwed JS, Weizel L, Walter M, Stark H. Anticonvulsant effects of isomeric nonimidazole histamine H3 receptor antagonists. Drug Des Devel Ther. 2016;10:3633–3651. doi: 10.2147/DDDT.S114147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Coppola G, Arcieri S, D'Aniello A, Messana T, Verrotti A, Signoriello G, et al. Levetiracetam in submaximal subcutaneous pentylentetrazol-induced seizures in rats. Seizure. 2010;19(5):296–299. doi: 10.1016/j.seizure.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 83.Kou YT, Liu HT, Hou CY, Lin CY, Tsai CM, Chang H. A transient protective effect of low-level laser irradiation against disuse-induced atrophy of rats. Lasers Med Sci. 2019;34(9):1829–1839. doi: 10.1007/s10103-019-02778-5. [DOI] [PubMed] [Google Scholar]
- 84.Lian XY, Zhang Z, Stringer JL. Anticonvulsant and neuroprotective effects of ginsenosides in rats. Epilepsy Res. 2006;70(2–3):244–256. doi: 10.1016/j.eplepsyres.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 85.Luttjohann A, Fabene PF, van Luijtelaar G. A revised Racine's scale for PTZ-induced seizures in rats. Physiol Behav. 2009;98(5):579–586. doi: 10.1016/j.physbeh.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 86.Sato SM, Woolley CS. Acute inhibition of neurosteroid estrogen synthesis suppresses status epilepticus in an animal model. Elife. 2016;5:e12917. doi: 10.7554/eLife.12917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Swinyard EA, Kupferberg HJ. Antiepileptic drugs: detection, quantification, and evaluation. Fed Proc. 1985;44(10):2629–2633. [PubMed] [Google Scholar]
- 88.Chen CR, Tan R, Qu WM, Wu Z, Wang Y, Urade Y, et al. Magnolol, a major bioactive constituent of the bark of Magnolia officinalis, exerts antiepileptic effects via the GABA/benzodiazepine receptor complex in mice. Br J Pharmacol. 2011;164(5):1534–1546. doi: 10.1111/j.1476-5381.2011.01456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Loscher W, Fisher JE, Nau H, Honack D. Valproic acid in amygdala-kindled rats: alterations in anticonvulsant efficacy, adverse effects and drug and metabolite levels in various brain regions during chronic treatment. J Pharmacol Exp Ther. 1989;250(3):1067–1078. [PubMed] [Google Scholar]
- 90.Zhao M, Zhang T, Li G, Qiu F, Sun Y, Zhao L. Associations of CYP2C9 and CYP2A6 polymorphisms with the concentrations of valproate and its Hepatotoxin metabolites and valproate-induced hepatotoxicity. Basic Clin Pharmacol Toxicol. 2017;121(12):138–143. doi: 10.1111/bcpt.12776. [DOI] [PubMed] [Google Scholar]
- 91.Zhu X, Li X, Zhang T, Zhao L. Risk factors for Valproic acid-induced Hyperammonaemia in Chinese Paediatric patients with epilepsy. Basic Clin Pharmacol Toxicol. 2018;123(5):628–634. doi: 10.1111/bcpt.13049. [DOI] [PubMed] [Google Scholar]
- 92.Ramanjaneyulu R, Ticku MK. Interactions of pentamethylenetetrazole and tetrazole analogues with the picrotoxinin site of the benzodiazepine-GABA receptor-ionophore complex. Eur J Pharmacol. 1984;98(3–4):337–345. doi: 10.1016/0014-2999(84)90282-6. [DOI] [PubMed] [Google Scholar]
- 93.Owens MJ, Nemeroff CB. Pharmacology of valproate. Psychopharmacol Bull. 2003;37(Suppl 2):17–24. [PubMed] [Google Scholar]
- 94.Sigel E, Steinmann ME. Structure, function, and modulation of GABA(a) receptors. J Biol Chem. 2012;287(48):40224–40231. doi: 10.1074/jbc.R112.386664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Lee V, Maguire J. The impact of tonic GABAA receptor-mediated inhibition on neuronal excitability varies across brain region and cell type. Front Neural Circuits. 2014;8:3. doi: 10.3389/fncir.2014.00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Wu X, Huang L, Wu Z, Zhang C, Jiang D, Bai Y, et al. Homeostatic competition between phasic and tonic inhibition. J Biol Chem. 2013;288(35):25053–25065. doi: 10.1074/jbc.M113.491464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Benarroch EE. GABAA receptor heterogeneity, function, and implications for epilepsy. Neurology. 2007;68(8):612–614. doi: 10.1212/01.wnl.0000255669.83468.dd. [DOI] [PubMed] [Google Scholar]
- 98.Chang Y, Xie Y, Weiss DS. Positive allosteric modulation by ultraviolet irradiation on GABA(a), but not GABA(C), receptors expressed in Xenopus oocytes. J Physiol. 2001;536:471–478. doi: 10.1111/j.1469-7793.2001.0471c.xd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Leszkiewicz DN, Aizenman E. Reversible modulation of GABA(a) receptor-mediated currents by light is dependent on the redox state of the receptor. Eur J Neurosci. 2003;17(10):2077–2083. doi: 10.1046/j.1460-9568.2003.02656.x. [DOI] [PubMed] [Google Scholar]
- 100.Wang X, Reddy DD, Nalawade SS, Pal S, Gonzalez-Lima F, Liu H. Impact of heat on metabolic and hemodynamic changes in transcranial infrared laser stimulation measured by broadband near-infrared spectroscopy. Neurophotonics. 2018;5(1):011004. doi: 10.1117/1.NPh.5.1.011004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Bhattacharya M, Dutta A. Computational modeling of the photon transport, tissue heating, and cytochrome C oxidase absorption during Transcranial near-infrared stimulation. Brain Sci. 2019;9(8):179. doi: 10.3390/brainsci9080179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Adedapo ADA, Demaki WE, Lagunju I. Non-dose-dependent changes in liver enzyme levels of children with epilepsy on treatment with sodium valproate. Dose-Response. 2020;18(2):1559325820918445. doi: 10.1177/1559325820918445. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used and analyzed during the current study are available from the corresponding author.