Abstract
Background
There have been controversial findings for the effectiveness of rehabilitation before operation after total knee arthroplasty (TKA). This study aimed to conduct an updated, comprehensive systematic review. On that basis, the review was to be combined with meta-analysis to measure the effects of rehabilitation before operation on functions and pain after TKA.
Methods
Articles were searched by using Central Register of Controlled Trials (CENTRAL), Web of Science, EMBASE, Cochrane, Pubmed, CNKI, Wanfang, Weipu and the Chinese Biomedical Database from the beginning to December 10, 2021. The major outcomes included pain, knee flexion and extension, as well as knee range of motion (ROM). Secondary outcomes included timed-up-and-go (TUG), 6-min walk, and patient-reported functional outcome (the Knee Injury and Osteoarthritis Outcome Score (KOOS) or Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC)). Third outcomes included the length of hospital stay.
Results
Nineteen studies recruiting 1008 patients satisfied with the inclusion criteria. Significant difference was identified in knee flexion, TUG, KOOS (knee-associated life quality and functions in sports and recreation), as well as the length of hospital stay (P < 0.05). Insignificant statistical difference was identified in pain, 6-min walk, ROM, knee extension, KOOS (pain, symptoms and function of daily living) after TKA between the two groups. No difference was found between the groups in WOMAC.
Conclusions
Preoperative rehabilitation could significantly shorten hospital stay, whereas there is not any conclusive evidence of the improvement of postoperative functions. Accordingly, in-depth high-quality studies should be conducted to confirm the effectiveness of preoperative rehabilitation in patients having received TKA.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13018-022-03066-9.
Keywords: Rehabilitation, Total knee arthroplasty, Meta-analysis, Randomized controlled trials
Introduction
Osteoarthritis (OA) refers to a commonly used joint degenerative diseases, capable of leading to joint pain and disability. Total knee arthroplasty can effectively treat end-stage knee osteoarthritis, through which knee pain can be significantly effectively relieved, and knee function and quality of life of patients can be improved [1, 2]. 72,100 TKAs were reported in the United States in 2014, and the incidence of TKA was expected to increase from 78 to 182% in the period of 2014 to 2030 [3]. Though the hospitals have optimized many procedures to reduce patients' waiting time for TKA, whereas waiting times remain excessively long for patients with pain and disabilities [4]. Long time waiting may make the patient's muscle strength damage, reduce the range of motion, have negative consequences for postoperative outcome [5].
Appropriate rehabilitation after TKA may certainly affect the course and outcome of the surgery. Rehabilitation program mainly includes supervised rehabilitation and home-based programs. No matter which rehabilitation program can improve the postoperative function of knee surgery, so that patients get the best rehabilitation effect [6]. Preoperative training was reported as an effective and safe method to improve postoperative functional performance and muscle strength for patients having received TKA [7]. According to Calatayud et al. [8] high-intensity preoperative supervised training can reduce postoperative pain, improve lower limb muscle strength, range of motion, and shorten the length of hospital stay in patients with TKA. Moreover, Matassi et al. [9] reported that preoperative home exercise program is more conducive to the recovery of primary TKA patients, as opposed to the control. However, the effectiveness of preoperative rehabilitation is also uncertain. Huber et al. [10] reported that preoperative training programs did not benefit to postoperative functional recovery. Recently, Mat et al. [11] even reported that the 6-week preoperative physiotherapy did not significantly impact the early function and range of motion after TKA. Though existing systematically reviewing studies surveyed the effect of rehabilitation before operation on outcomes after the operation for patients having received TKA, there is still conflicting to whether preoperative rehabilitation improves postoperative outcome [12, 13]. There is a need to conduct a reviewing study the recent articles and assess the impact exerted by rehabilitation before operation on postoperative outcomes for patients having received TKA.
Thus, this study aimed to make a systematic review with an improved and extensive method. On that basis, the meta-analysis was combined to examine the impact of rehabilitation before operation on early functions and pain after TKA.
Materials and methods
Searching strategy and identification of literature
With Pubmed, Cochrane Central Register of Controlled Trials (CENTRAL), Web of Science, EMBASE, CNKI, Wanfang, Weipu and the Chinese Biomedical Database, the search was conducted from their inception to December 10, 2021. In addition, more articles were identified from relevant references. The search used was combined with subject words and free words (e.g., total knee replacement OR total knee arthroplasty OR TKA AND pre-habilitation OR rehabilitation OR resistance Training OR exercise OR training AND before operation). This study has been registered on the Research Registry, registration ID: reviewregistry1139.
Inclusion and exclusion criteria
Inclusion criteria: (1) controlled articles under randomization. (2) Comparison of the preoperative rehabilitation group and the control who lived as usual. (3) Included patients were unilateral TKA with OA. (4) Clinical outcomes: the primary included pain, knee motion range (ROM), knee flexion and extension. Secondary outcomes included TUG, 6-min walk, patient-reported functional performance (KOOS or WOMAC). Third outcomes included the length of hospital stay.
Exclusion criteria: (1) Repeated published literature. (2) Not any outcome of interest suggested. (3) Trials type as “case reports”, “reviews”, “meta-analysis” and “letters”. (4) Animal experiments. (5) Articles without full text. (6) Documents not published in English or Chinese.
Data extraction
All the literatures were imported into Endnote software, and the two investigators independently read abstracts and titles to preliminarily screen the articles under the inclusion and exclusion criteria. The literature that met the inclusion criteria was further read and screened again to determine whether it was included or not. Any objections to the included articles should be resolved on the basis of discussion or arbitration by a third investigator. The extraction contents include authors, publication year, country, patients, age, gander, body mass index (BMI), intervention measures and study type. After data extraction was completed, the two investigators cross-checked the extraction results. If the needed information in the article was missing or ambiguous, we attempt at contacting article authors for more details.
Quality evaluation
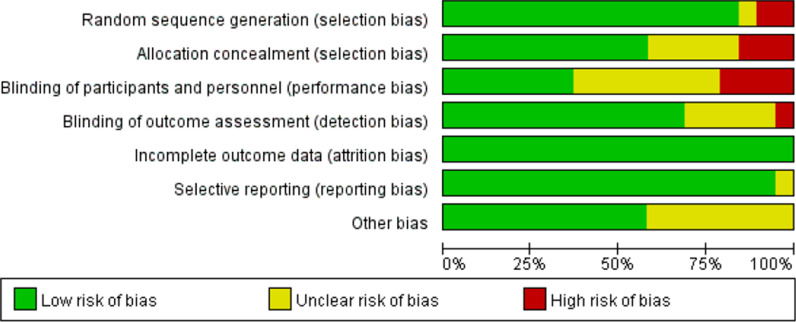
Two investigating staffs conducted the independent evaluation of included trials quality by complying with the Cochrane Handbook for Systematic Reviews of Interventions guideline. Assessment indicators include selective reporting, incomplete outcome data, blinding of outcome assessment, blinding of participants and personnel, allocation concealment, random sequence generation, and other bias. The respective item had the evaluation to be "low risk bias”, “high risk bias" and "unclear". If the two investigators had different opinions in the process of inclusion literature and quality evaluation, they would discuss and resolve or request the third investigator to arbitrate.
Data analysis and statistical method
The effect sizes of the respective analysis were determined using Review Manager Statistical software (version 5.3). Standardized mean difference (SMD) or weighted mean difference (WMD) acted as effects, the 95% confidence interval represents the effect size. The pooled odds ratio (OR) with 95% confidence intervals (95% CIs) was adopted to assist dichotomous results. Besides, the estimation of the uninterrupted results was made from the WMD or SMD pooled with 95% CIs. The estimation of the statistical heterogeneity between articles was made using the value of P and I2. A fixed-effect model was used when P > 0.1 and I2 < 50%; otherwise, a random-effect model was employed for the analyses. The sensitivity analysis was conducted to examine the likely heterogeneity source. Subsequently, the identified articles causing significant heterogeneity were excluded, and a repeated meta-analysis on the remaining articles was made for the adjustments. The meta-analysis robustness here was demonstrated if no considerable variations were being identified between the regulated and major results. The work has been reported in line with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) and AMSTAR (Assessing the methodological quality of systematic reviews) Guidelines. PRISMA checklist is shown in the Additional file 1.
Results
Study selection and quality assessment
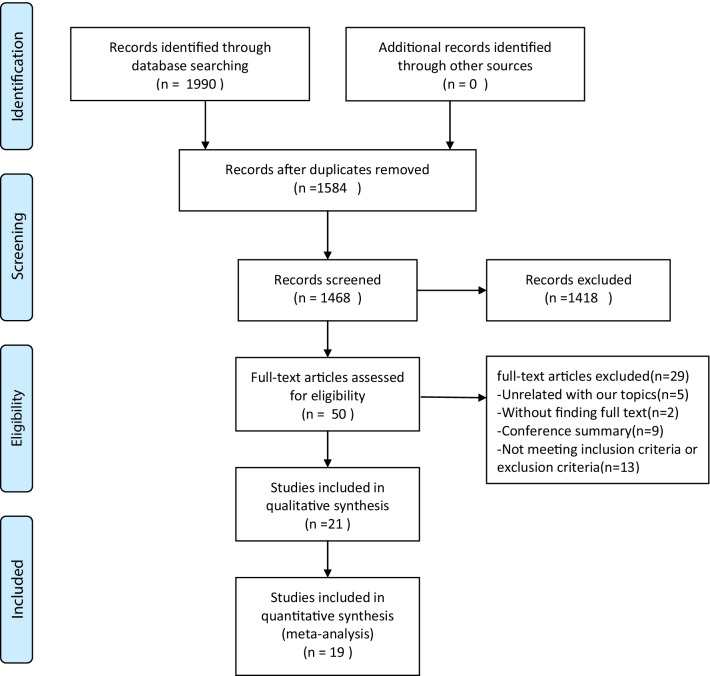
Following the existing searching strategy, 1990 studies originated in the online database from Jan. 1987 to Dec. 10, 2021. When duplicates were removed, 1584 studies were kept. Next, based on the view of titles and abstracts, 1418 articles were removed. Among the rest 50 studies, 31 studies were excluded, which was attributed to several factors. Lastly, 19 full-text articles were applicable to the present meta-analysis [8–11, 14–28] (Fig. 1). Table 1 and Figs. 2, 3 summarize the features, quality assessment and demographics of the articles included (Risk of bias summary).
Fig. 1.
Flow chart of the systematic literature
Table 1.
Characteristics of included studies
| References | Country | Sample sizee, I/C | Age, I/C† (year) | Female sex, I/C (%) | BMI (kg/m2) | Preop. intervention | Study type |
|---|---|---|---|---|---|---|---|
| Calatayud et al. [8] | Spain | 25/25 | 66.8 ± 4.8/66.7 ± 3.1 | 84.1# | 32.0 ± 4.2/31.0 ± 3.8 | Seated leg press, knee extension, leg curl, and hip abduction (5 sets of 10 repetitions for each exercise, with 60 s rest between sets) 3 days per week for 8 weeks | RCT |
| Matassi et al. [9] | Italy | 61/61 | 66 ± 7.2/67 ± 7.7 | 54.1/42.6 | 29.0 ± 4.3/28.0 ± 3.7 | Muscle training: isometric quadriceps, isotonic hamstring, isotonic quadriceps contraction, and dynamic stepping exercise for 6 weeks | RCT |
| Huber et al. [10] | Switzerland | 22/23 | 68.8 ± 8.0/71.9 ± 8.1 | 50.0/43.5 | 30.8 ± 4.9/29.9 ± 5.5 | Neuromuscular training program for 4–12 weeks, depending on their location on the waiting list for surgery | RCT |
| Mat Eil-Ismail et al. [11] | Malaysia | 24/26 | 62.4/64.3 | 91.7/80.8 | – | Physical exercises (stretching, isometric strengthening exercises, mobilising exercises and heat therapy) for 6 weeks | RCT |
| Alghadir et al. [14] | India | 25/25 | 63.3 ± 9.4# | 58.2# | – | Strengthening and mobility exercises, proper techniques of transfers, and gait training, once a day for 30 min | RCT |
| Aytekin et al. [15] | Turkey | 21/23 | 67.8 ± 6.3/69.7 ± 6.4 | 85.7/78.2 | 32.8 ± 5.9/30.2 ± 4.9 | Education and home-based exercise, 2 sets of 10 repetitions of each exercise for five days/week for 12 weeks | RCT |
| Domínguez-Navarro et al. [16] | Spain | 28/26 | 70.8 ± 5.4/70.4 ± 5.6 | 57.1/65.4 | – | Strengthening training and progressive resistance exercise (the sessions lasted 30–40 min) for 5–8 weeks | RCT |
| Huang et al. [17] | Taiwan | 126/117 | 69.8 ± 7.2/70.5 ± 7.4 | 69.8/73.5 | 27.1 ± 4.0/27.2 ± 4.5 | Muscle strength training: knee setting, ankle pumping and hip abduction with resistance for 6 weeks | RCT |
| Saw et al. [18] | South Africa | 35/39 | 60.7 ± 5.5# | 81.1# | 34.5 ± 8.2# | Six physiotherapist-led group-based sessions (two hours/week of education, exercise and relaxation)for 6 weeks | RCT |
| An et al. [19] | Korea | 18/18 | 71.1 ± 3.3/70.4 ± 2.6 | – | 26.5 ± 2.5/26.5 ± 2.9 | Preoperative telerehabilitation program (30 min/session, 2 times/day, 5 days/week for 3 weeks, for a total of 30 sessions) | RCT |
| Cavill et al. [20] | Australia | 21/20 | 66.0 ± 8.4/68.3 ± 9.1 | 52.0/55.0 | – | Prehabilitation included one-hour twice-weekly sessions for at least three and a maximum of 4 weeks prior to surgery | RCT |
| Skoffer et al. [21] | Denmark | 30/29 | 70.7 ± 7.3/70.1 ± 6.4 | 63.3/58.6 | 30/31.8 | Leg press, knee extension, knee flexion, hip extension, hip abduction, and hip adduction in strength training machines 3 training sessions per week for 4 weeks | RCT |
| Skoffer et al. [22] | Denmark | 30/29 | 70.7 ± 7.3/70.1 ± 6.4 | 63.3/58.6 | 30/31.8 | Leg press, knee extension, knee flexion, hip extension, hip abduction, and hip adduction in strength training machines 3 training sessions per week for 4 weeks | RCT |
| Walls et al. [23] | Ireland | 9/5 | 64.4 ± 8.0/63.2 ± 11.4 | 67/80 | 30.7 ± 3.0/32.8 ± 6.3 | 8 weeks of preoperative unsupervised, home-based Neuromuscular electrical stimulation Straining applied unilaterally to the QFM of the affected side | RCT |
| McKay et al. [24] | Canada | 10/12 | 63.5 ± 4.9/60.6 ± 8.1 | 50.0/66.7 | 35.0 ± 6.1/33.8 ± 7.1 | A 10-min aerobic warm-up, followed by a circuit of bilateral lower body exercises (standing calf raise, seated leg press, leg curl, knee extension). 2 sets of 8 repetitions of each exercise | RCT |
| BEAUPRE et al. [25] | Canada | 65/66 | 67.0 ± 7.0/67.0 ± 6.0 | 60.0/50.0 | 32.0 ± 6.0/32.0 ± 5.0 | Crutch walking on level ground and on stairs, bed mobility and transfers, and the postoperative ROM routine, 3 times per week for 4 weeks for a total of 12 treatment sessions | RCT |
| Tungtrongjit et al. [26] | Thailand | 30/30 | 63.0 ± 7.6/65.9 ± 7.2 | 86.7/80.0 | 24.3 ± 2.4/25.3 ± 3.8 | The patients were asked to participate in 3 weeks Home Program (General Quadriceps strengthening exercise) until their TKA | RCT |
| Gstoettner et al. [27] | Austria | 18/20 | 72.8 ± 15.7/66.9 ± 12.6 | 88.9/70 | 27.4/28.2 | Preoperative proprioceptive training programme were taught and supervised for 45 min per setting by the same physical therapist for 6 weeks before TKA | RCT |
| Topp et al. [28] | America | 26/28 | 64.1 ± 7.05/63.5 ± 6.68 | 73.1/64.3 | 32.16 ± 5.87/32.00 ± 6.09 | Resistance, flexibility and step training, 1 supervised and 2 home sessions, 3 days per week for 4 weeks | RCT |
I = intervention group, C = control group
†Values are given as the mean with or without the standard deviation
#Patient demographics were not separated by randomized group
Fig. 2.
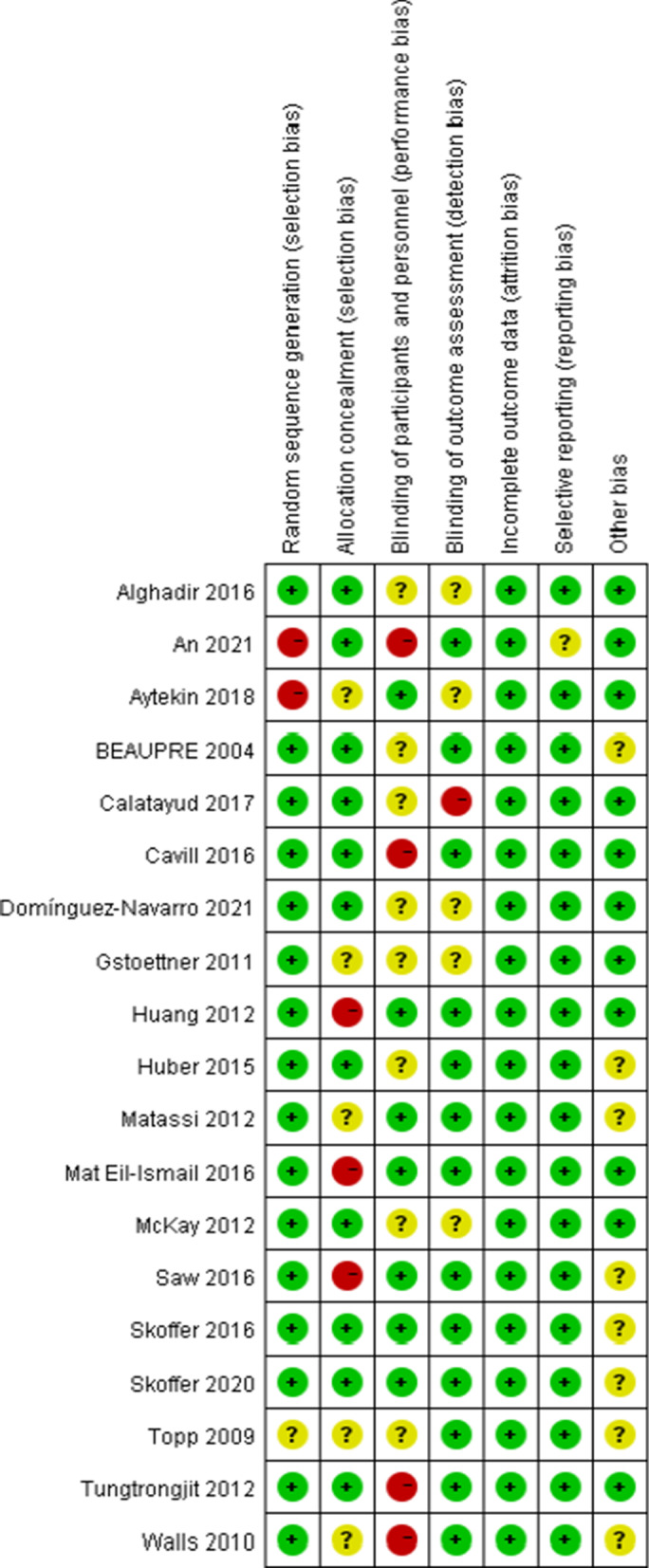
The risk of bias summary of the included studies
Fig. 3.
The risk of bias graph of the included studies
Meta-analysis results
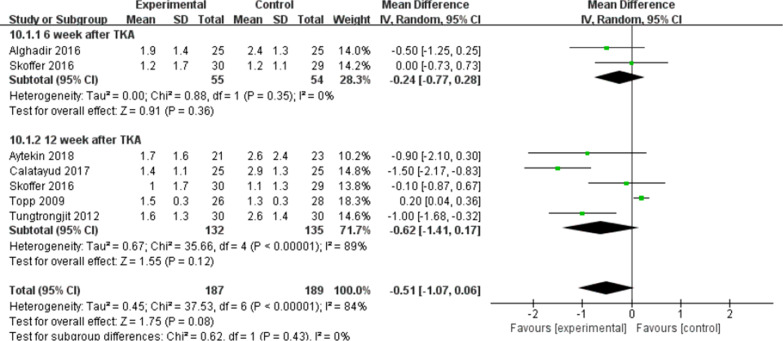
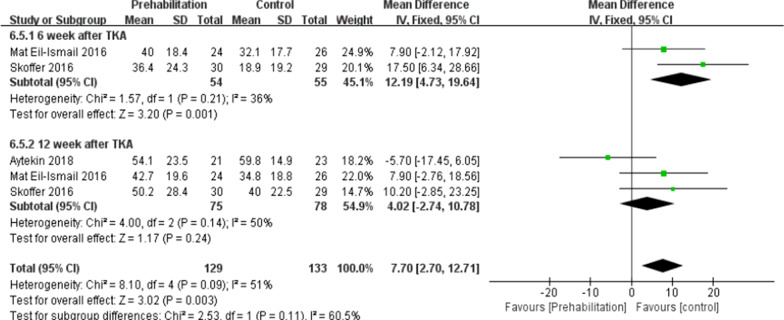
Visual analog scale (VAS)
Pain was measured by VAS scores. Six studies [8, 14, 15, 21, 26, 28] (317 patients) reported the effects of pre-habilitation on postoperative pain. In this study, data were extracted twice. Subgroup analysis was conducted at the 6th and 12th weeks after TKA. As impacted by the heterogeneity of the subgroups (I2 = 84%, P = 0.08), the random response model was adopted. No significant difference received the identification between the two group [MD = − 0.51, 95% CI (− 1.07, 0.06), P = 0.08] (Fig. 4).
Fig. 4.
A forest plot diagram showing the VAS score
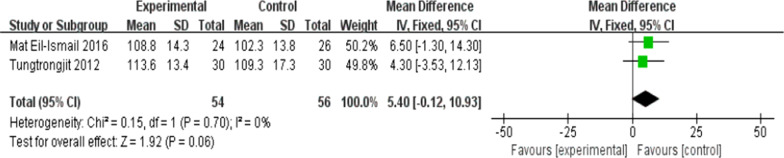
Knee motion range (ROM), knee flexion and extension
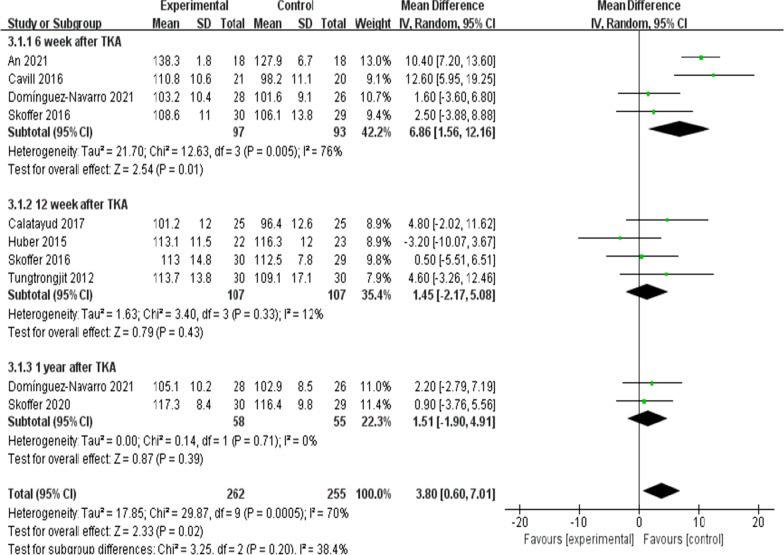
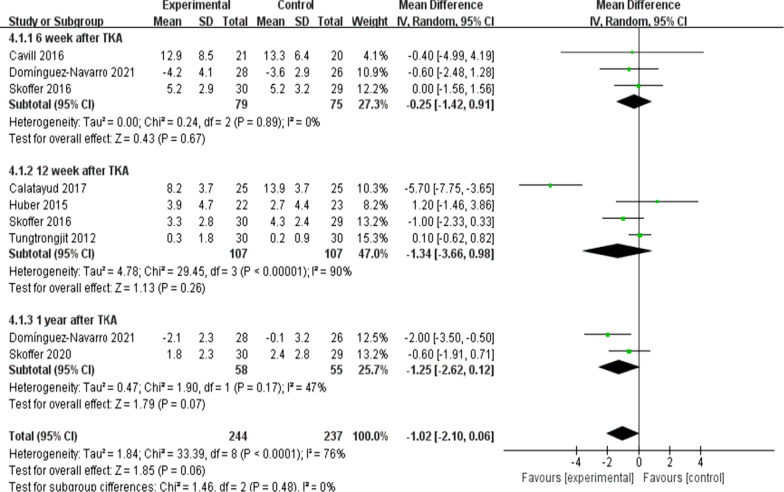
On the whole, two trials [11, 26] (110 patients) presented information regarding knee ROM and eight trials [8, 10, 16, 19–22, 26] (404patients) presented the information regarding knee extension and seven trials [8, 10, 16, 20–22, 26] (368patients) presented the information regarding knee flexion. No significant difference received the identification between the two group for ROM at the 6th week after TKA [I2 = 0%, MD = 5.4, 95% CI (− 0.12, 10.93), P = 0.06)] (Fig. 5). For flexion and extension, data were extracted three times, Subgroup analysis was conducted data extraction was conducted at the 6th week, the 12th week and the 1 year after TKA. Statistical distinction was found between the two groups [I2 = 70%, MD = 3.8, 95% CI (0.6, 7.01), P = 0.02] (Fig. 6). Not any obvious distinction was reported for knee extension between the two groups [I2 = 76%, MD = − 1.02, 95% CI (− 2.10, 0.06), P = 0.06] (Fig. 7).
Fig. 5.
A forest plot diagram showing the ROM
Fig. 6.
A forest plot diagram showing the knee flexion
Fig. 7.
A forest plot diagram showing the knee extension
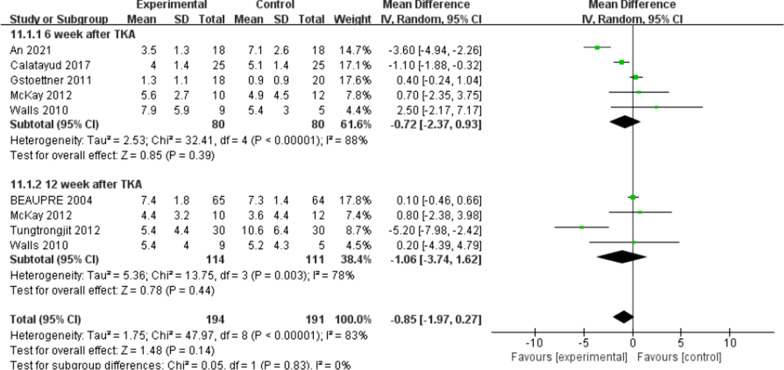
Timed-up-and-go (TUG) and 6-min walk
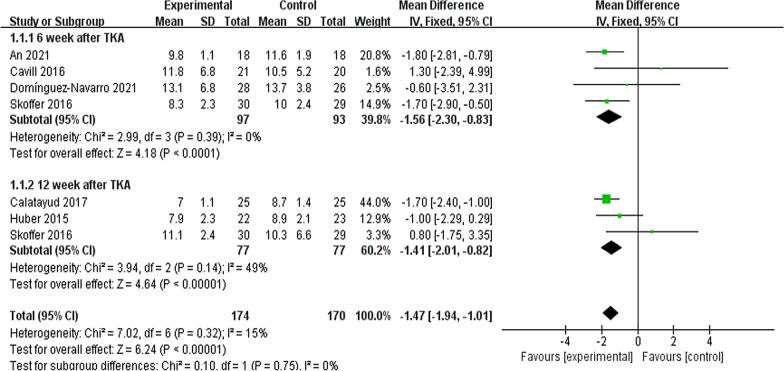
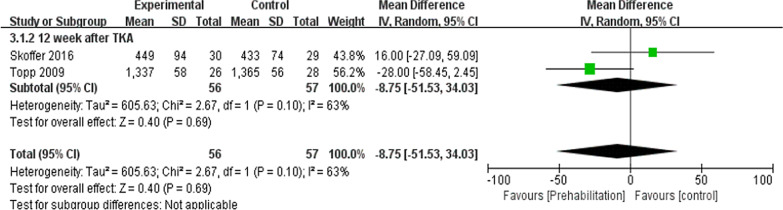
Six trials here [8, 10, 16, 19–21] (285 participants) provided data of TUG. In this study, data were extracted twice. Subgroup analysis was conducted at the 6th week and the 12th week after TKA. Noticeable difference was reported between two groups for TUG [I2 = 15%, MD = − 1.47, 95% CI (− 1.94, − 1.01), P < 0.01] (Fig. 8). Two trials [21, 28] (113 patients) presented the information of 6-min walk at the 12th week after TKA. No significant difference was reported between the two group in 6-min walk test [I2 = 63%, MD = − 8.75, 95% Cl (− 51.53to 34.03), P = 0.69] (Fig. 9).
Fig. 8.
A forest plot diagram showing the time up and go
Fig. 9.
A forest plot diagram showing the 6-min walk
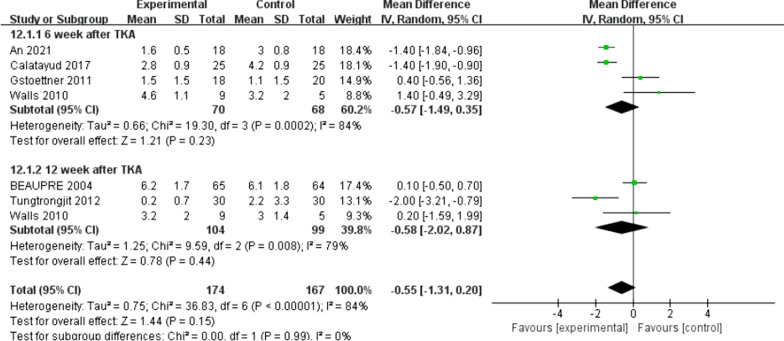
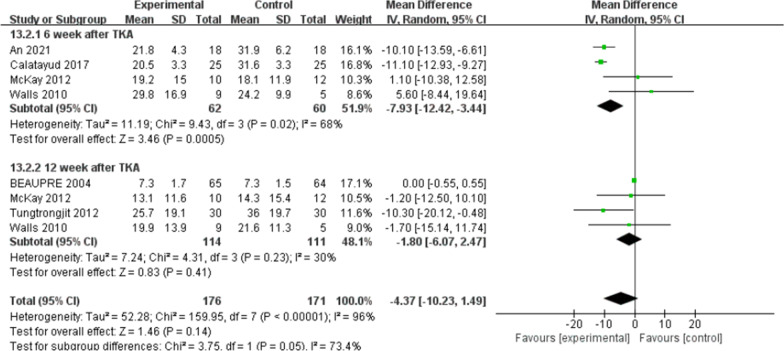
Patient-reported functional outcomes
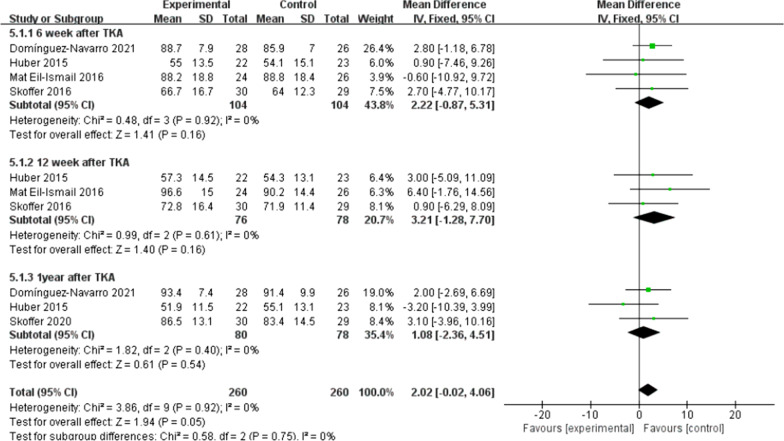
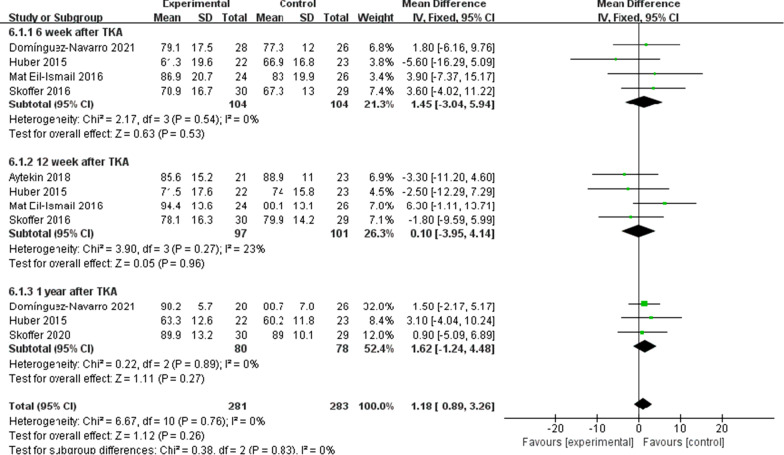
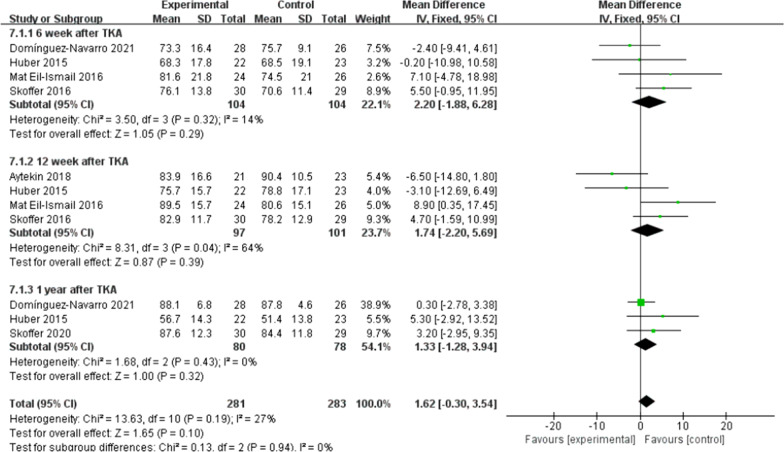
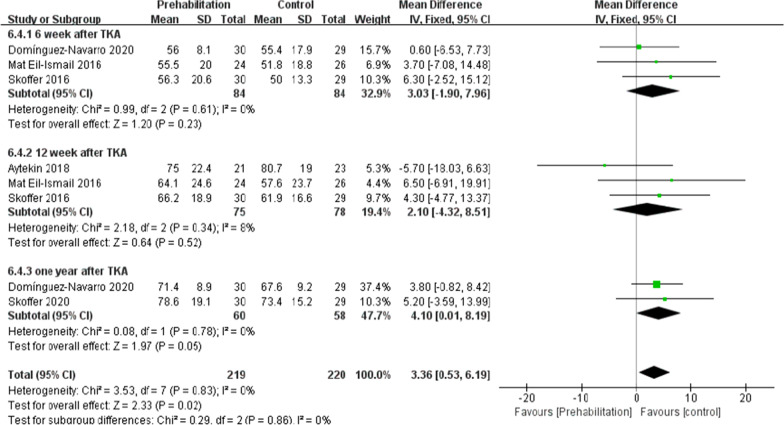
There were five trials [10, 11, 16, 21, 22] (267 patients) reported the data of KOOS symptoms, six trials [10, 11, 15, 16, 21, 22] (311 patients) reported the data of KOOS (knee-associated life quality, daily living function, pain), and four trials [10, 11, 15, 21] (198 patients) reported the data of KOOS functions in sports and recreation. Data were extracted three times, the subgroup analysis was conducted at the 6th week and the 12th week and one year after TKA during KOOS symptoms, pain, function of daily living, knee-related quality of life. There was no statistical difference between the two groups for KOOS symptoms [I2 = 0%, MD = 2.02, 95% CI (− 0.02, 4.06), P = 0.05] (Fig. 10). No statistical difference was identified between the two groups for KOOS pain [I2 = 0%, MD = 1.18, 95% CI (− 0.89, 3.26), P = 0.26] (Fig. 11). There was no statistical difference between the two groups for KOOS function of daily living [I2 = 27%, MD = 1.62, 95% CI (− 0.30, 3.54), P = 0.10] (Fig. 12). A statistical difference was found between the two groups for KOOS knee-related quality of life [I2 = 0%, MD = 2.87, 95% CI (0.23, 5.52), P = 0.03] (Fig. 13). For KOOS functions in sports and recreation, data were extracted twice. The subgroup analysis was conducted at the 6th week and the 12th week after TKA. A statistical difference was found between the two groups [I2 = 42%, MD = 7.51, 95% CI (3.37, 11.65), P < 0.01] (Fig. 14). There were seven trials [8, 19, 23–27] (349 patients) reported the data of WOMAC pain, six trials [8, 19, 23, 25–27] (311 patients) reported the data of WOMAC stiffness, six trials [8, 19, 23–26] (301 patients) reported the data of WOMAC function. The subgroup analysis was conducted at the 6th week and the 12th week after TKA. No statistical difference was identified between the two groups for WOMAC (pain, stiffness, function) (Figs. 15, 16, 17).
Fig. 10.
A forest plot diagram showing the KOOS symptoms
Fig. 11.
A forest plot diagram showing the KOOS pain
Fig. 12.
A forest plot diagram showing the KOOS function of daily living
Fig. 13.
A forest plot diagram showing the KOOS knee-related quality of life
Fig. 14.
A forest plot diagram showing the KOOS function in sport and recreation
Fig. 15.
A forest plot diagram showing the WOMAC pain
Fig. 16.
A forest plot diagram showing the WOMAC stiffness
Fig. 17.
A forest plot diagram showing the WOMAC function
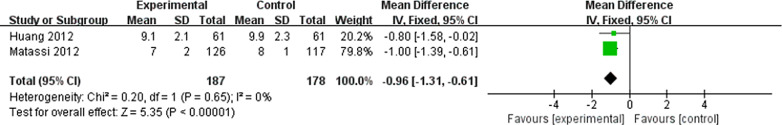
The length of hospital stay
Of the 19 trials, two trials [9, 17] (365 patients) reported the data of length of hospital stay. The pre-habilitation group showed a shorter length of hospital stay when compared with the control [I2 = 0%, MD = − 0.96, 95% Cl (− 1.31, − 0.61), P < 0.001] (Fig. 18).
Fig. 18.
A forest plot diagram showing the length of hospital stay
Discussion
The efficacy of preoperative rehabilitation on functional recovery for patients having received TKA remains controversial [17, 29]. Previous systematic reviews [12] reported that compared with the control, preoperative rehabilitation had a consistent functional recovery effect in patients having received TKA. Recently, preoperative rehabilitation has still aroused huge attention, and considerable studies were conducted on the effect of preoperative rehabilitation for functional recovery after TKA [8, 15, 16, 21]. Accordingly, the meta-analysis of the present study updated the literature to further assess the effect of preoperative rehabilitation on postoperative functions for patients having received TKA. This study made a summary of evidence from 19 randomized controlled trials which provided a clearer pole of preoperative rehabilitation for patients with TKA. According to the results of this study, preoperative rehabilitation was effective in reducing the length of hospital stay. It could be effective in improving knee flexion, TUG, KOOS (knee-related quality of life and functions in sports and recreation). However, it did not alter among pain, 6-min walk, ROM, knee extension, KOOS (symptoms, pain, function of daily living), WOMAC (pain, stiffness, function) following TKA. There was a certain heterogeneity among the included studies, which may be due to the different evaluation scales held by different researchers.
Pain was the primary outcome in the meta-analysis here. As it was uncovered from this study, preoperative rehabilitation did not increase postoperative pain following TKA in terms of the VAS scores either at the 6th week or the 12th week postoperatively, which was consistent with precedent studies [30]. Pain acts as the main symptom of knee OA and a key determinant of knee extension and flexion in knee OA. Thus, it has become one of the main problems to be solved by TKA. Such a study further showed that OA who had never exercised thought exercise might damage joints. However, preoperative rehabilitation is capable of reducing this fear, helping find ways to cope with pain, and maintaining exercise levels after surgery to improve their quality of life in depth [8].
Moreover, the knee range of motion is a vital indicator of postoperative functional recovery. As illustrated by Skoffer et al. [21] as opposed to the control, the 4-week preoperative progressive resistance training failed to significantly mitigate the knee flexion and extension at the 6th week and the 12th week postoperatively. As reported by Mat et al. [11] no significant difference in ROM was identified in the two groups. However, An [19] indicated that preoperative tele-rehabilitation yielded improvement in the knee flexion at the 6th week postoperatively. In the meta-analysis here, the subgroup analysis was conducted at the 6th week and the 12th week after the surgery, and the results complied with the mentioned findings. The meta-analysis of the present study showed that compared with the control, the preoperative rehabilitation group has no improvement in knee ROM and knee extension. Statistical difference was found between the two groups in the knee flexion. Many factors are found to affect knee ROM (e.g., implant design, the surgical technique used, preoperative ROM, knee kinematics, associated perioperative complications and postoperative rehabilitation compliance), which all impact knee flexion after TKA [31]. However, a single factor (e.g., preoperative rehabilitation) has little impact on postoperative knee ROM [11]. Therefore, large sample and high-quality randomized controlled trial should be carried out to verify the effect of preoperative rehabilitation on knee range of motion in the future.
According to the meta-analysis here, the subgroup analysis was conducted at the 6th week and the 12th week after TKA, indicating that compared with the control, the rehabilitation group was preoperatively better in TUG. Skoffer et al. [21]showed that the TUG was better in the preoperative rehabilitation group than the control at the 6th week and the 12th week postoperatively. Calatayud et al. [8] also demonstrated that the 8-week preoperative high-intensity strength training improved TUG after TKA. The ability to walk refers to a basic ability in daily life, as well as a predictor of mobility and functional ability. The mentioned result further supports the conclusion that the Timed Up and Go test complied with the theory of preoperative rehabilitation [28]. The 6-min walk test measured the maximum walking distance covered in 6 min. As indicated from the result of the meta-analysis here, the preoperative rehabilitation group had consistent results on the 6-min walk compared with the control. Topp et al. [28] and Skoffer et al. [21] reported that no significant difference in 6-min walk was reported between the preoperative rehabilitation group and the control for patients following TKA. This result may be attributed to the strength of the quadriceps, indicating that the stronger the quadriceps, the longer the 6-min walk will be [28].
For the outcome of self-reported physical function, compared with patients allocated to the control group, no significant improvement was observed except for the KOOS (sport and knee-associated quality of life subscale) on TKA patients who received preoperative rehabilitation. Skoffer et al. [21] reported that no differences were identified between the groups in KOOS, except for the KOOS sport subscale in favor of the preoperative rehabilitation group. According to Mat et al. [11] a noticeable distinction was reported in symptoms and ADL function, but no significant difference was found for other KOOS subscales. Aytekin et al. [15] also declared no significant differences within both groups in KOOS. Calatayud et al. [8] reported that no improvement for WOMAC function score was found in preoperative rehabilitation group. Likewise, Rooks et al. [32] also demonstrated that no significant difference in WOMAC function score between the preoperative rehabilitation group and the control group following TKA. All the included articles indicated that both groups of patients had significant improvement in patient-reported functional outcomes after TKA, not unrelated to whether they underwent preoperative rehabilitation or not. We found that the different programs, intensity and duration of preoperative rehabilitation in across enrolled studies might result in the heterogeneity of our outcomes. An et al. [19] declared that preoperative telerehabilitation could improve WOMAC functional results after TKA. Therefore, the effect of preoperative rehabilitation on postoperative function of TKA patients remains uncertain. In addition, Paravlic et al. [33] reported that home-based motor imagery intervention can improve functional performance after total knee replacement in the short term without increasing patients' pain. Motor imagery refers to the mental representation of body movements without obvious body movements, which can effectively improve the performance of sports [34]. A systematic review shows that motion imagery is effective in the treatment of strength enhancement, pain reduction, and improved physical activity in patients undergoing TKA [35]. The intervention time of preoperative rehabilitation is generally 4–8 weeks. Therefore, whether the preoperative rehabilitation combined with motor imagery has a positive effect on the knee function of TKA patients is worth further exploring. Furthermore, our meta-analysis showed that preoperative rehabilitation could significantly shorten the length of hospital stay, which was in congruity with the results of another meta-analysis by Chen [36]. We know that the length of hospital stay is affected by numerous factors (e.g., the time of postoperative suture removal), so it cannot act as one of the effective indicators to assess the rehabilitation effect.
The systematic review and here meta-analysis of the present study are subject to several limitations. (1) The number of literatures in the subgroup analysis was small in the meta-analysis here, and the sample size of the respective study was small, thereby reducing the statistical ability of our meta-analysis. (2) Only English and Chinese publications were included in our meta-analysis. Accordingly, publication bias is inevitable. (3) Outcomes (e.g., complications, muscle strength and knee society score were not analyzed as impacted by the lack of data. (4) The preoperative rehabilitation protocol varied with the studies. Different preoperative rehabilitation protocol may cause higher statistical heterogeneity on postoperative functional outcomes (e.g., knee extension).
Conclusion
Preoperative rehabilitation could effectively shorten the length of hospital stay. Our meta-analysis showed that preoperative rehabilitation had the similar effect on postoperative functional recovery following TKA compared with the control group. In short, high-quality randomized controlled trials (RCTs) are needed to determine the efficacy of preoperative rehabilitation on postoperative recovery following TKA.
Supplementary Information
Acknowledgements
We would like to show sincere appreciation to the editors and reviewers for their work of this manuscript.
Abbreviations
- AMSTAR
Assessing the methodological quality of systematic reviews
- KOOS
The Knee Injury and Osteoarthritis Outcome Score
- OA
Osteoarthritis
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analysis
- ROM
Knee range of motion
- SMD
Standardized mean difference
- TUG
Timed-up-and-go
- TKA
Total knee arthroplasty
- VAS
Visual Analog Scale
- WOMAC
Western Ontario and McMaster Universities Osteoarthritis Index
- WMD
Weighted mean difference
Authors’ contributions
WS: Conceptualization; Data curation; Formal analysis; Methodology; Software; Writing original draft; Writing review and editing; Translate, YZ: Translate; Validation; Supervision; Writing review and editing, Data curation; Methodology; HQ: Validation; Software; Investigation; HW: Conceptualization; Project administration; Resources; Validation; Supervision; Writing review and editing. All authors read and approved the final manuscript.
Funding
This work was supported by Health Commission of Hunan Province of China (No. 202114021174).
Availability of data and materials
The authors declare that all the data supporting the findings of this study are available within the article and its supplementary information files.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Neuprez A, Neuprez AH, Kurth W, et al. Profile of osteoarthritic patients undergoing hip or knee arthroplasty, a steptoward a definition of the "need for surgery". Aging Clin Exp Res. 2018;30(4):315–321. doi: 10.1007/s40520-017-0780-1. [DOI] [PubMed] [Google Scholar]
- 2.Price AJ, Alvand A, Troelsen A, Katz JN, Hooper G, Gray A, Carr A, Beard D. Knee replacement. Lancet. 2018;392(10158):1672–82. doi: 10.1016/S0140-6736(18)32344-4. [DOI] [PubMed] [Google Scholar]
- 3.Schwartz AM, Farley KX, Guild GN, et al. Projections and epidemiology of revision hip and knee arthroplasty in the United States to 2030. J Arthroplasty. 2020;35(6S):S79–85. doi: 10.1016/j.arth.2020.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bird C. Wait times increasing for hip and knee replacement. CMAJ. 2013;185(8):E325. doi: 10.1503/cmaj.109-4445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schroer WC, Berend KR, Lombardi AV, et al. Why are total knees failing today? Etiology of total knee revision in 2010 and 2011. J Arthroplasty. 2013;28(8 Suppl):116–119. doi: 10.1016/j.arth.2013.04.056. [DOI] [PubMed] [Google Scholar]
- 6.Papalia R, Vasta S, Tecame A, et al. Home-based vs supervised rehabilitation programs following knee surgery: a systematic review. Br Med Bull. 2013;108:55–72. doi: 10.1093/bmb/ldt014. [DOI] [PubMed] [Google Scholar]
- 7.Gränicher P, Stöggl T, Fucentese SF, et al. Preoperative exercise in patients undergoing total knee arthroplasty: a pilot randomized controlled trial. Arch Physiother. 2020;10:13. doi: 10.1186/s40945-020-00085-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Calatayud J, Casaña J, Ezzatvar Y, et al. High-intensity preoperative training improves physical and functional recovery in the early post-operative periods after total knee arthroplasty: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2017;25(9):2864–2872. doi: 10.1007/s00167-016-3985-5. [DOI] [PubMed] [Google Scholar]
- 9.Matassi F, Duerinckx J, Vandenneucker H, et al. Range of motion after total knee arthroplasty: the effect of a preoperative home exercise program. Knee Surg Sports Traumatol Arthrosc. 2014;22(3):703–709. doi: 10.1007/s00167-012-2349-z. [DOI] [PubMed] [Google Scholar]
- 10.Huber EO, Roos EM, Meichtry A, et al. Effect of preoperative neuromuscular training (NEMEX-TJR) on functional outcome after total knee replacement: an assessor-blinded randomized controlled trial. BMC Musculoskelet Disord. 2015;16:101. doi: 10.1186/s12891-015-0556-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mat Eil-Ismail MS, Sharifudin MA, Ahmed Shokri A, et al. Preoperative physiotherapy and short-term functional outcomes of primary total knee arthroplasty. Singap Med J. 2016;57(3):138–143. doi: 10.11622/smedj.2016055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ma JX, Zhang LK, Kuang MJ, et al. The effect of preoperative training on functional recovery in patients undergoing total knee arthroplasty: a systematic review and meta-analysis. Int J Surg. 2018;51:205–212. doi: 10.1016/j.ijsu.2018.01.015. [DOI] [PubMed] [Google Scholar]
- 13.Moyer R, Ikert K, Long K, et al. The value of preoperative exercise and education for patients undergoing total hip and knee arthroplasty: a systematic review and meta-analysis. JBJS Rev. 2017;5(12):e2. doi: 10.2106/JBJS.RVW.17.00015. [DOI] [PubMed] [Google Scholar]
- 14.Alghadir A, Iqbal ZA, Anwer S. Comparison of the effect of pre- and post-operative physical therapy versus post-operative physical therapy alone on pain and recovery of function after total knee arthroplasty. J Phys Ther Sci. 2016;28(10):2754–2758. doi: 10.1589/jpts.28.2754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aytekin E, Sukur E, Oz N, et al. The effect of a 12 week prehabilitation program on pain and function for patients undergoing total knee arthroplasty: a prospective controlled study. J Clin Orthop Trauma. 2019;10(2):345–349. doi: 10.1016/j.jcot.2018.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Domínguez-Navarro F, Silvestre-Muñoz A, Igual-Camacho C, et al. A randomized controlled trial assessing the effects of preoperative strengthening plus balance training on balance and functional outcome up to 1 year following total knee replacement. Knee Surg Sports Traumatol Arthrosc. 2021;29(3):838–848. doi: 10.1007/s00167-020-06029-x. [DOI] [PubMed] [Google Scholar]
- 17.Huang SW, Chen PH, Chou YH. Effects of a preoperative simplified home rehabilitation education program on length of stay of total knee arthroplasty patients. Orthop Traumatol Surg Res. 2012;98(3):259–264. doi: 10.1016/j.otsr.2011.12.004. [DOI] [PubMed] [Google Scholar]
- 18.Saw MM, Kruger-Jakins T, Edries N, et al. Significant improvements in pain after a six-week physiotherapist-led exercise and education intervention, in patients with osteoarthritis awaiting arthroplasty, in South Africa: a randomised controlled trial. BMC Musculoskelet Dis. 2016;17:236. doi: 10.1186/s12891-016-1088-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.An J, Ryu HK, Lyu SJ, et al. Effects of preoperative telerehabilitation on muscle strength, range of motion, and functional outcomes in candidates for total knee arthroplasty: a single-blind randomized controlled trial. Int J Environ Res Public Health. 2021;18(11):6071. doi: 10.3390/ijerph18116071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cavill S, McKenzie K, Munro A, et al. The effect of prehabilitation on the range of motion and functional outcomes in patients following the total knee or hip arthroplasty: a pilot randomized trial. Physiother Theory Pract. 2016;32(4):262–270. doi: 10.3109/09593985.2016.1138174. [DOI] [PubMed] [Google Scholar]
- 21.Skoffer B, Maribo T, Mechlenburg I, et al. Efficacy of preoperative progressive resistance training on postoperative outcomes in patients undergoing total knee arthroplasty. Arthritis Care Res. 2016;68(9):1239–1251. doi: 10.1002/acr.22825. [DOI] [PubMed] [Google Scholar]
- 22.Skoffer B, Maribo T, Mechlenburg I, et al. Efficacy of preoperative progressive resistance training in patients undergoing total knee arthroplasty: 12-month follow-up data from a randomized controlled trial. Clin Rehabil. 2020;34(1):82–90. doi: 10.1177/0269215519883420. [DOI] [PubMed] [Google Scholar]
- 23.Walls RJ, McHugh G, O'Gorman DJ, et al. Effects of preoperative neuromuscular electrical stimulation on quadriceps strength and functional recovery in total knee arthroplasty. A pilot study. BMC Musculoskelet Disord. 2010;11:119. doi: 10.1186/1471-2474-11-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McKay C, Prapavessis H, Doherty T. The effect of a prehabilitation exercise program on quadriceps strength for patients undergoing total knee arthroplasty: a randomized controlled pilot study. PM&R. 2012;4(9):647–656. doi: 10.1016/j.pmrj.2012.04.012. [DOI] [PubMed] [Google Scholar]
- 25.Beaupre LA, Lier D, Davies DM, et al. The effect of a preoperative exercise and education program on functional recovery, health related quality of life, and health service utilization following primary total knee arthroplasty. J Rheumatol. 2004;31(6):1166–1173. [PubMed] [Google Scholar]
- 26.Tungtrongjit Y, Weingkum P, Saunkool P. The effect of preoperative quadriceps exercise on functional outcome after total knee arthroplasty. J Med Assoc Thail. 2012;95(Suppl 10):S58–S66. [PubMed] [Google Scholar]
- 27.Gstoettner M, Raschner C, Dirnberger E, et al. Preoperative proprioceptive training in patients with total knee arthroplasty. Knee. 2011;18(4):265–270. doi: 10.1016/j.knee.2010.05.012. [DOI] [PubMed] [Google Scholar]
- 28.Topp R, Swank AM, Quesada PM, et al. The effect of prehabilitation exercise on strength and functioning after total knee arthroplasty. PM&R. 2009;1(8):729–735. doi: 10.1016/j.pmrj.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 29.Jahic D, Omerovic D, Tanovic A, et al. The effect of prehabilitation on postoperative outcome in patients following primary total knee arthroplasty. Med Arch. 2018;72(6):439. doi: 10.5455/medarh.2018.72.439-443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brown K, Topp R, Brosky JA, et al. Prehabilitation and quality of life three months after total knee arthroplasty: a pilot study. Percept Mot Skills. 2012;115(3):765–774. doi: 10.2466/15.06.10.PMS.115.6.765-774. [DOI] [PubMed] [Google Scholar]
- 31.Kurosaka M, Yoshiya S, Mizuno K, et al. Maximizing flexion after total knee arthroplasty: the need and the pitfalls. J Arthroplasty. 2002;17(4 Suppl 1):59–62. doi: 10.1054/arth.2002.32688. [DOI] [PubMed] [Google Scholar]
- 32.Rooks DS, Huang J, Bierbaum BE, et al. Effect of preoperative exercise on measures of functional status in men and women undergoing total hip and knee arthroplasty. Arthritis Rheum. 2006;55(5):700–708. doi: 10.1002/art.22223. [DOI] [PubMed] [Google Scholar]
- 33.Paravlic AH, Maffulli N, Kovač S, et al. Home-based motor imagery intervention improves functional performance following total knee arthroplasty in the short term: a randomized controlled trial. J Orthop Surg Res. 2020;15(1):451. doi: 10.1186/s13018-020-01964-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Paravlic AH, Slimani M, Tod D, et al. Effects and dose-response relationships of motor imagery practice on strength development in healthy adult populations: a systematic review and meta-analysis. Sports Med. 2018;48(5):1165–1187. doi: 10.1007/s40279-018-0874-8. [DOI] [PubMed] [Google Scholar]
- 35.Li R, Du J, Yang K, et al. Effectiveness of motor imagery for improving functional performance after total knee arthroplasty: a systematic review with meta-analysis. J Orthop Surg Res. 2022;17(1):65. doi: 10.1186/s13018-022-02946-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen H, Li S, Ruan T, et al. Is it necessary to perform prehabilitation exercise for patients undergoing total knee arthroplasty: meta-analysis of randomized controlled trials. Phys Sportsmed. 2018;46(1):36–43. doi: 10.1080/00913847.2018.1403274. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The authors declare that all the data supporting the findings of this study are available within the article and its supplementary information files.