Abstract
Background
Anxiety during pregnancy is a common problem. Anxiety and stress could have consequences on the course of the pregnancy and the later development of the child. Anxiety responds well to treatments such as cognitive behavioral therapy and/or medication. Non‐pharmacological interventions such as mind‐body interventions, known to decrease anxiety in several clinical situations, might be offered for treating and preventing anxiety during pregnancy.
Objectives
To assess the benefits of mind‐body interventions during pregnancy in preventing or treating women's anxiety and in influencing perinatal outcomes.
Search methods
We searched the Cochrane Pregnancy and Childbirth Group’s Trials Register (30 November 2010), MEDLINE (1950 to 30 November 2010), EMBASE (1974 to 30 November 2010), the National Center for Complementary and Alternative Medicine (NCCAM) (1 December 2010), ClinicalTrials.gov (December 2010) and Current Controlled Trials (1 December 2010), searched the reference lists of selected studies and contacted professionals and authors in the field.
Selection criteria
Randomized controlled trials, involving pregnant women of any age at any time from conception to one month after birth, comparing mind‐body interventions with a control group. Mind‐body interventions include: autogenic training, biofeedback, hypnotherapy, imagery, meditation, prayer, auto‐suggestion, tai‐chi and yoga. Control group includes: standard care, other pharmacological or non‐pharmacological interventions, other types of mind‐body interventions or no treatment at all.
Data collection and analysis
Three review authors independently assessed trials for inclusion all assessed risk of bias for each included study. We extracted data independently using an agreed form and checked it for accuracy.
Main results
We included eight trials (556 participants), evaluating hypnotherapy (one trial), imagery (five trials), autogenic training (one trial) and yoga (one trial). Due to the small number of studies per intervention and to the diversity of outcome measurements, we performed no meta‐analysis, and have reported results individually for each study. Compared with usual care, in one study (133 women), imagery may have a positive effect on anxiety during labor decreasing anxiety at the early and middle stages of labor (MD ‐1.46; 95% CI ‐2.43 to ‐0.49; one study, 133 women) and (MD ‐1.24; 95% CI ‐2.18 to ‐0.30). Another study showed that imagery had a positive effect on anxiety and depression in the immediate postpartum period. Autogenic training might be effective for decreasing women's anxiety before delivering.
Authors' conclusions
Mind‐body interventions might benefit women’s anxiety during pregnancy. Based on individual studies, there is some but no strong evidence for the effectiveness of mind‐body interventions for the management of anxiety during pregnancy. The main limitations of the studies were the lack of blinding and insufficient details on the methods used for randomization.
Plain language summary
Mind‐body interventions during pregnancy for preventing or treating women's anxiety
Mind‐body interventions like yoga or hypnotherapy may be effective for reducing anxiety. These can be learned to induce mental relaxation and alter negative thinking related to anxiety to change the perception of a stressful event, leading to better adapted behaviour and coping skills. Their effectiveness for treatment or prevention of women’s anxiety during pregnancy needs to be confirmed in clinical trials, as anxiety during the different stages of pregnancy can affect women’s health and have consequences for the child. This review identified few studies that examined this. We included eight randomized controlled studies with 556 women in this review. Based on these studies, there is some not strong evidence for the effectiveness of mind‐body interventions in the management of anxiety during pregnancy, labor, or in the first four weeks after giving birth. Compared with usual care, imagery may have a positive effect on anxiety during labor. Another study showed that imagery had a positive effect on anxiety and depression in the immediate postpartum period. Autogenic training might be effective for decreasing women's anxiety before delivering. No harmful effects were reported for any mind‐body interventions in the studies included in the review. The studies used different mind‐body interventions, sometimes as part of a complex intervention, that they compared with usual care or other potentially active interventions using diverse outcome measures. Several studies were at high risk of bias, had small sample sizes and high dropout rates.
Background
Description of the condition
Being pregnant may cause anxiety (Huizink 2004), which can affect a woman’s health. Anxiety during the antenatal period often remains undetected (Alder 2007; Coleman 2008) and is under‐researched. Subclinical anxiety is prevalent and more frequent than depression at all stages of pregnancy (Lee 2007). Around 54% of women experience anxiety at some point of their pregnancy (versus 37% for depression). Anxiety and depression are more prevalent and severe in the first and third trimesters of pregnancy. Thus, new cases of anxiety emerge at different stages of pregnancy, making it difficult to diagnose such cases from only one antenatal visit (Lee 2007). In an observational study, higher anxiety rates were found in the first (15%) and third pregnancy trimesters (18%), whereas lower rates were reported at the second trimester (12.3%) (Teixeira 2009). In a longitudinal study (N = 8323), around 16% of pregnant women were diagnosed with anxiety at week 32 of gestation and 8.5% at week eight of the postpartum period (Heron 2004).
Anxiety symptoms during pregnancy are reported to be associated with depression and low social support (Gee 2008; Milgrom 2008b). However, internal resources, like low self‐esteem, must also be considered. The relationship between psychosocial determinant factors (e.g. socioeconomic or age considerations) and anxiety during pregnancy is controversial (Littleton 2007). High anxiety levels during pregnancy have also been related to invasive procedures such as in vitro fertilization (IVF), pregnancy termination, amniocentesis, ultrasound scans, genetic counselling and hospitalization (Brisch 2003; Cwikel 2004; Sosa 2004). High‐risk pregnancies (preterm labor, hypertension, diabetes, breech version or fetal abnormality), generate further anxiety (Vendittelli 2002). Several studies suggest that labelling a pregnancy as a risk may intensify women's feelings of loss of control and helplessness (Stahl 2003) and could potentially raise anxiety levels (Hatmaker 1998; Kowalcek 2003).
Anxiety has a negative influence on obstetric, fetal and perinatal outcomes, but conclusions are often limited due to low sample size in these studies, and to methodological weakness (Alder 2007; Littleton 2007). As a result, there is a lack of consensus among researchers on the role of anxiety in perinatal outcomes (Glover 2002; Johnson 2003; Littleton 2007). Women experiencing higher levels of anxiety during pregnancy seem to report more symptoms (nausea and vomiting) and make more medical visits (Andersson 2004; Swallow 2004). In addition, anxiety during pregnancy can influence particular behaviors, such as increase in alcohol or tobacco consumption (Alvik 2006; Goodwin 2007) or unhealthy eating habits (Hurley 2005). Finally, anxious pregnant women are at a greater risk of postpartum depression and mood disorders (Britton 2008; Lee 2007).
Anxiety and stress during pregnancy also affect the course of pregnancy and the health of the child. Conflicting results have been reported on the role of enhanced levels of anxiety in the development of pre‐eclampsia (Andersson 2004; Kurki 2000; Sikkema 2001). Mothers experiencing high levels of psychological or social stress might be at increased risk of preterm birth (Anonymous 2008), but little is known about the mechanism underlying the association between stress (both psychological and social) and prematurity (Gennaro 2003; Goldenberg 2008; Moutquin 2003). Furthermore, maternal anxiety at birth is a prognostic factor in neonatology (Zelkowitz 2005). Anxiety could influence the mother’s immediate attitude towards the infant (e.g. she will be less apt to touch him/her, to speak to him/her) and neonatal care (infant’s appearance, neonatal medical procedure) (Zelkowitz 2000). Anxiety should be considered when developing a program in the early neonatal period to improve mother‐child interactions (massage, touch, skin‐to‐skin care) (DiPietro 2006; Melnyk 2006; O'Connor 2002a; O'Connor 2002b). Besides increasing research on the shared roles of stress, anxiety and depression on adverse pregnancy and neonatal outcomes, there is a need to assess these maternal factors, to document the nature of the anxiety and to develop randomized controlled trials testing interventions aimed at reducing anxiety. Anxiety responds well to treatments such as cognitive behavioral therapy (CBT) or medication. The use of psychotropic medications during pregnancy is controversial (Costei 2002). Given the risk of adverse effects associated with pharmacological treatments, non‐pharmacological interventions like mind‐body interventions might be preferable.
Description of the intervention
Mind‐body interventions are used in different clinical situations such as managing pain (Smith 2006; Uman 2006), depression (Shiha 2009), smoking cessation (Carmodi 2008) and in paediatric care (Galantino 2008). According to the definition of the National Center for Complementary and Alternative Medicine (NCCAM 2008): "mind‐body medicine focuses on the interactions among the brain, mind, body, and behavior, and the powerful ways in which emotional, mental, social, spiritual, and behavioral factors can directly affect health". Mind‐body interventions are intended to enhance the capacity for self‐knowledge and self‐care and provide the opportunity for increasing resilience, personal growth and self‐esteem. They provide tools to improve mood, quality of life and coping. Cerebral activities during mind‐body interventions are complex, but different techniques for such interventions seem to share a common specific modulation of cerebral activity (Grant 2005). Mind‐body interventions constitute a major portion of the overall use of complementary and alternative medicine by the public (Eisenberg 1998). In the adult US population in 2002, almost one in five adults reported having used one or more mind‐body therapies during the previous 12 months (Wolsko 2004). Meditation, imagery, hypnosis and yoga were used by more than 17% of those surveyed, to treat a specific medical condition or to prevent illness. Among the 40% of US women who had used any complementary and alternative medicine, 21% reported the use of mind‐body therapies (Upchurch 2006).
Why it is important to do this review
Anxiety is prevalent during pregnancy and affects both mother and child health. There is increasing evidence for positive effects of mind‐body interventions. Such interventions might be particularly helpful for patients for increasing confidence to develop self‐knowledge, self‐care and ability to cope with chronic conditions (Montgomery 2000; Patterson 2003). These interventions are used in pregnant women to manage anxiety.
To our knowledge, there has been no comprehensive systematic review of mind‐body interventions for managing anxiety during the perinatal period. In this review, we will evaluate the effects of mind‐body interventions during pregnancy.
Objectives
To assess the benefits of mind‐body interventions during pregnancy in preventing or treating women's anxiety and in influencing perinatal outcomes.
Methods
Criteria for considering studies for this review
Types of studies
We have included randomized controlled trials in the review if they took place in any of the following clinical settings: hospital, community, complementary and alternative medicine practice, primary care, family practice or extended care facility. Quasi‐randomised controlled trials are not eligible for inclusion in this review or future updates of the review.
Types of participants
Pregnant women of any age at any time of the antenatal period from conception until one month after birth.
Types of interventions
Mind body interventions
Studies testing mind‐body interventions that, with or without the help of a professional or a supportive relative, can be taught/learned by pregnant women to induce mental relaxation, in order to:
alter negative thinking related to anxiety;
modify the perception of the stressful event;
lead to a better adapted behavior and coping.
CBT and support groups classified as psychological or psychosocial interventions that involve ongoing interactions between people will be the focus of another, Cochrane review ('Psychosocial, psychological and pharmacological interventions for treating antenatal anxiety' ‐ protocol in progress) and we have excluded these interventions from this review.
We divide mind‐body interventions into 10 subcategories. To choose and define each of the subcategories, we based our method on: 1 ‐ The National Center Complementary Alternative Medicine (NCCAM 2008); 2 ‐ The Desktop Guide to Complementary and Alternative Medicine (Ernst 2006); 3 ‐ The National Library of Medicine MeSH definitions (NLM 2008); 4 ‐ Natural Standard (Natural Standard 2008); and 5 ‐ other Cochrane reviews.
Mind‐body interventions sub‐categories and definitions
Autogenic training
Refers to a particular technique of mental exercises involving relaxation and autosuggestion practised regularly, which aims to teach relaxation and body awareness techniques. This approach can then be used lifelong to promote a healthier lifestyle, allowing people to call on their own capacity for self‐healing and stress reduction (Ernst 2006; Natural Standard 2008).
Biofeedback
Biofeedback encompasses a therapeutic technique by which individuals receive training to improve their health and well‐being through signals coming from their own body. The underlying principle is that changes in thoughts and emotions may result in changes in body functioning (Barragan Loayza 2006).
Hypnotherapy
The induction of a trance‐like state to facilitate relaxation and make use of enhanced suggestibility to treat psychological and medical conditions and affect behavioral changes (Ernst 2006).
Imagery
A cognitive technique used to encourage the person to cope with the pain and distress of a given procedure by having him/her imagine a pleasant object or experience (Uman 2006).
Meditation
A diverse range of techniques based on focusing on a physical sensation (such as breathing), repeating a mantra, detaching oneself from the thought process or other self‐directed mental practices which focus the attention and bring about a state of self‐awareness and inner calm (Ernst 2006; Natural Standard 2008).
Prayer
Prayer may be practiced by individuals within the framework of an organized religion, or without ascribing to a particular faith or belief system. Prayers can focus on a specific desired outcome, or be undirected and without a definite objective in mind (Natural Standard 2008).
Relaxation therapy
Numerous relaxation therapies exist. We decided to include this type of intervention only if there was evidence that the therapeutic goal is to facilitate mental relaxation. If the relaxation is part of a pre‐described subcategory (e.g. yoga, autogenic training, meditation, etc.) we have classified the intervention under the respective subcategory. (We have not included Jacobson's relaxation technique.)
Auto‐suggestion
A form of verbal therapy where the patient repeats affirmations or suggestions until he/she body and mind begin to act accordingly (Natural Standard 2008).
Tai chi
A meditative exercise using slow circular stretching movements and positions of body balance (NLM 2008).
Yoga
A practice of gentle exercises for breathing and mental control. It includes a system of exercises for attaining bodily or mental control and well‐being with liberation of the self and union with a universal spirit (Ernst 2006; NLM 2008).
Control conditions
Any form of standard care, other pharmacological or non‐pharmacological interventions, other types of mind‐body interventions or no treatment at all.
Types of outcome measures
Primary outcomes
Maternal anxiety
Maternal anxiety could be self‐reported or observed and assessed using a range of scales, questionnaires, interviews or physiological measurements. If no measures of anxiety were reported, we sent a request to the original authors to ask whether unpublished data on women's anxiety are available. After a first contact and one reminder, we classified a "no answer" as "no data available" and excluded the study.
Secondary outcomes
Maternal
Self‐esteem
Depression
Perceived stress
Pain experience
Sleep
Blood pressure
Quality of life
Mode of delivery
Use of medication (for anxiety or depression, preterm labor)
Hospitalization days
Use of analgesia during labor
Length of labor
Breastfeeding
Biochemical assessment of stress hormones
Treatment discontinuation
Neonatal
Apgar score
Fetal heart rate
Gestational age
Admission to neonatal intensive care unit
Birthweight
intrauterine growth retardation
Other
Cost effectiveness
Father's anxiety
Search methods for identification of studies
Electronic searches
We searched the Cochrane Pregnancy and Childbirth Group’s Trials Register by contacting the Trials Search Co‐ordinator (30 November 2010).
The Cochrane Pregnancy and Childbirth Group’s Trials Register is maintained by the Trials Search Co‐ordinator and contains trials identified from:
quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
weekly searches of MEDLINE;
weekly searches of EMBASE;
handsearches of 30 journals and the proceedings of major conferences;
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Details of the search strategies for CENTRAL, MEDLINE and EMBASE, the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service can be found in the ‘Specialized Register’ section within the editorial information about the Cochrane Pregnancy and Childbirth Group.
Trials identified through the searching activities described above are each assigned to a review topic (or topics). The Trials Search Co‐ordinator searches the register for each review using the topic list rather than keywords.
In addition, we searched MEDLINE (1950 to 30 November 2010), EMBASE (1974 to 30 November 2010), the National Center for Complementary and Alternative Medicine (NCCAM) (1 December 2010), ClinicalTrials.gov (1 December 2010) and Current Controlled Trials (1 December 2010). SeeAppendix 1 for details.
We also initially searched CINAHL (1982 to November 2008), PsycINFO (1840 to November 2008), AMED (The Allied and Complementary Medicine Database) (1985 to November 2008) and British Nursing Index (1994 to November 2008). We were not able to update these searches. SeeAppendix 2 for details.
Searching other resources
We searched the reference lists of selected studies and contacted professionals and authors in the field.
We did not apply any restrictions of language or date.
Data collection and analysis
Selection of studies
Three review authors ‐ Isabelle Marc (IM), Narimane Toureche (NT) and Claudine Blanchet (CB) ‐ independently assessed for inclusion all the potential studies we identified as a result of our search strategy. We resolved disagreements by discussion or, if required, we consulted another author Sylvie Dodin (SD).
Data extraction and management
We designed a form to extract data. For eligible studies, two review authors (NT and IM) extracted the data using the agreed form. We resolved discrepancies through discussion or, if required, we consulted CB. For each included trial, we collected information regarding the location of the study, methodology of the study (randomization, allocation concealment, blinding, loss to follow‐up, etc.), the participants characteristics (age range, eligibility criteria, etc.), the nature of the interventions, and data related to the outcomes specified above. We entered data into the Review Manager software (RevMan 2011) and checked it for accuracy. When information regarding any of the above was unclear, we attempted to contact authors of the original reports to provide further details.
Assessment of risk of bias in included studies
Two review authors (NT and IM) independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved any disagreement by discussion or by involving a third assessor (CB).
(1) Sequence generation (checking for possible selection bias)
We described for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We assessed the method as:
low risk of bias (any truly random process, e.g. random number table; computer random number generator);
high risk of bias (any non‐random process, e.g. odd or even date of birth;
hospital or clinic record number) or,unclear risk of bias.
(2) Allocation concealment (checking for possible selection bias)
We described for each included study the method used to conceal the allocation sequence and determined whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as:
low risk of bias (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
high risk of bias (open random allocation;
unsealed or non‐opaque envelopes, alternation; date of birth);unclear risk of bias.
(3) Blinding (checking for possible performance bias)
We described for each included study, the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We considered that studies were at low risk of bias if they were blinded, or if we judged that the lack of blinding could not have affected the results. Blinding was assessed separately for each different outcome or classes of outcomes.
We assessed the methods as:
low, high or unclear risk of bias for participants;
low, high or unclear risk of bias for personnel;
low, high or unclear risk of bias for outcome assessors.
(4) Incomplete outcome data (checking for possible attrition bias through withdrawals, dropouts, protocol deviations)
We described for each included study, and for each outcome or class of outcomes, the completeness of data, including attrition and exclusions from the analysis. We stated whether attrition and exclusion were reported, the numbers included in the analysis at each stage (compared with the total randomized participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported, or was supplied by the trial authors, we re‐included missing data in the analyses which we undertook. We assessed methods as:
low risk of bias (e.g. 20% or less missing outcome data; missing outcome data balanced across groups);
high risk of bias (e.g. numbers or reasons for missing data imbalanced across groups; ‘as treated’ analysis done with substantial departure of intervention received from that assigned at randomization);
unclear risk of bias.
(5) Selective reporting bias
We described for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
We assessed the methods as:
low risk of bias (where it is clear that all of the study’s pre‐specified outcomes and all expected outcomes of interest to the review have been reported);
high risk of bias (where not all the study’s pre‐specified outcomes have been reported; one or more reported primary outcomes were not pre‐specified; outcomes of interest are reported incompletely and so cannot be used; study fails to include results of a key outcome that would have been expected to have been reported);
unclear risk of bias.
(6) Other sources of bias
We described for each included study any important concerns we had about other possible sources of bias.
We assessed whether each study was free of other problems that could put it at risk of bias:
low risk of other bias;
high risk of other bias;
unclear whether there is risk of other bias.
(7) Overall risk of bias
We made explicit judgements about whether studies are at a high risk of bias, according to the criteria given in the Handbook (Higgins 2011). With reference to (1) to (6) above, we assessed the likely magnitude and direction of the bias and whether we considered that it was likely to impact on the findings. We explored the impact of the level of bias through undertaking sensitivity analyses ‐ seeSensitivity analysis.
Measures of treatment effect
Dichotomous data
For dichotomous data, we presented results as summary risk ratio (RR) with 95% confidence intervals (CI).
Continuous data
For continuous data, we used the mean difference (MD) if outcomes were measured in the same way between trials. We used the standardized mean difference (SMD) to combine trials that measured the same outcome, but used different methods.
Unit of analysis issues
Cluster‐randomized trials
We did not identify any cluster‐randomized trials for inclusion in this review. However, if we identify cluster‐randomized trials for inclusion in a subsequent update of this review, we will include them in the analyses along with individually randomized trials.We will adjust their sample sizes using the methods described in the Handbook using an estimate of the intracluster correlation co‐efficient (ICC) derived from the trial (if possible), from a similar trial or from a study of a similar population. If we use ICCs from other sources, we will report this and conduct sensitivity analyses to investigate the effect of variation in the ICC. If we identify both cluster‐randomised trials and individually‐randomised trials, we plan to synthesise the relevant information. We will consider it reasonable to combine the results from both if there is little heterogeneity between the study designs and the interaction between the effect of intervention and the choice of randomisation unit is considered to be unlikely.
We will also acknowledge heterogeneity in the randomisation unit and perform a sensitivity analysis to investigate the effects of the randomisation unit.
Crossover trials
We have not included crossover trials in this review because no washout is possible after a practice of a mind‐body intervention.
Other unit of analysis issues
In cases of repeated measures of anxiety during pregnancy, we have selected the clinically most relevant time point according to other studies in this area. In the event that we would be confronted with cases where such a choice would be difficult, we would calculate an adjusted mean of time‐repeated measures.
For trials with more than two intervention groups, we combined results in meta‐analysis with trials comparing only two interventions. For this, we combined groups to create a single pair‐wise comparison (Section 16.5.4 of the Handbook (Higgins 2011)). That means we combine all relevant experimental intervention groups of the study into a single group, and combined all relevant control intervention groups into a single control group. For dichotomous outcomes, both the sample sizes and the numbers of people with events will be summed across groups. For continuous outcomes, means and standard deviations were combined using methods described in Section 7.7.3.8 of the Handbook (Higgins 2011).
Dealing with missing data
For included studies, we noted levels of attrition. In future updates of this review, if a meta‐analysis is performed, we will explore the impact of including studies with high levels of missing data in the overall assessment of treatment effect by using Sensitivity analysis.
For all outcomes, we carried out analyses, as far as possible, on an intention‐to‐treat basis, i.e. we attempted to include all participants randomized to each group in the analyses, and all participants were analysed in the group to which they were allocated, regardless of whether or not they received the allocated intervention. The denominator for each outcome in each trial was the number randomized minus any participants whose outcomes are known to be missing.
Assessment of heterogeneity
In future updates of this review, if we perform meta‐analysis, we will assess statistical heterogeneity in each meta‐analysis using the T², I² and Chi² statistics. We will regard heterogeneity as substantial if I² is greater than 30% and either T² is greater than zero, or there is a low P value (less than 0.10) in the Chi² test for heterogeneity.
Assessment of reporting biases
If, in future, there are 10 or more studies in the meta‐analysis we will investigate reporting biases (such as publication bias) using funnel plots. We will assess funnel plot asymmetry visually, and use formal tests for funnel plot asymmetry. For continuous outcomes we will use the test proposed by Egger 1997 and for dichotomous outcomes we will use the test proposed by Harbord 2006. If we detect asymmetry in any of these tests or is by a visual assessment, we will perform exploratory analyses to investigate it.
Data synthesis
We carried out statistical analysis according to the type of mind‐body interventions using the Review Manager software (RevMan 2011). Because of the small number of trials per intervention, the clinical heterogeneity, the diversity of outcome measurements and control group interventions, we performed no meta‐analysis and have presented results individually for each study.
If, in future updates of this review it becomes possible to pool data, we will use fixed‐effect meta‐analysis for combining data where it is reasonable to assume that studies are estimating the same underlying treatment effect: i.e. where trials are examining the same intervention, and the trials’ populations and methods are judged sufficiently similar. If there is clinical heterogeneity sufficient to expect that the underlying treatment effects differ between trials, or if we detect substantial statistical heterogeneity, we will use random‐effects meta‐analysis to produce an overall summary if an average treatment effect across trials is considered clinically meaningful. We will treat the random‐effects summary as the average range of possible treatment effects and we will discuss the clinical implications of treatment effects differing between trials.
If we use random‐effects analyses, we will present the results as the average treatment effect with its 95% confidence interval, and the estimates of T² and I².
Subgroup analysis and investigation of heterogeneity
In future updates of this review, if we identify substantial heterogeneity, we will investigate it using subgroup analyses and sensitivity analyses. We will consider whether an overall summary is meaningful, and if it is, use random‐effects analysis to produce it.
For the primary outcome (anxiety), we plan to carry out the following subgroup analyses.
Timing of the intervention during pregnancy (first, second or third trimester)
Duration and frequency of the interventions
Type of intervention for preventing or treating anxiety
Population of pregnant women (low versus high risk of anxiety)
For fixed‐effect inverse variance meta‐analyses, we will assess differences between subgroups by interaction tests. For random‐effects and fixed‐effect meta‐analyses using methods other than inverse variance, we will assess differences between subgroups by inspection of the subgroups’ confidence intervals; non‐overlapping confidence intervals indicate a statistically significant difference in treatment effect between the subgroups.
Sensitivity analysis
In future updates of the review, if data are available, we will carry out sensitivity analysis to explore the effect of trial quality based on the risk of bias item such as sequence generation and allocation concealment. We will exclude studies of poor quality from the analysis (those rated as being at high or unclear risk of bias) in order to assess for any substantive difference to the overall result in their absence.
We will carry out sensitivity analysis to explore the effects of fixed‐effect or random‐effects analyses for outcomes with statistical heterogeneity.
Results
Description of studies
Results of the search
Using our search strategy, we identified 1468 articles. Six studies were published in languages other than English (Mandarin, German, Italian, Farsi and Portuguese) and were evaluated by native speakers. We identified 26 studies reporting a randomized controlled trial and evaluating a mind‐body intervention in the population of interest. After further evaluation, we included six. We undertook an update in collaboration with the Pregnancy and Childbirth Group Trials Search Co‐ordinator that identified eight new relevant studies. Among them, six are either ongoing studies or awaiting classification. We have included a total of eight studies (N = 556) in this review (see Criteria for considering studies for this review).
Included studies
We included eight randomized controlled trials (involving 556 women) in this review (Ip 2009; Korol 1992; Rees 1993; Rees 1995; Teixeira 2005; Urech 2010; Vieten 2008; Zimmermann 1979); see Characteristics of included studies.
All the included studies were published in English between 1979 and 2009 and were carried out in six different countries (USA, Canada, United Kingdom, China, Switzerland and Italy).
These studies compared the effects of mind‐body interventions with various control interventions. Mind‐body interventions under evaluation were hypnotherapy (Teixeira 2005), imagery (Ip 2009; Korol 1992; Rees 1993; Rees 1995; Urech 2010), yoga (Vieten 2008) and respiratory autogenic training (Zimmermann 1979). Control group interventions were: no intervention (Vieten 2008), attention control (Korol 1992), music therapy (Rees 1993; Rees 1995), passive relaxation (Teixeira 2005), usual care (Ip 2009) and a derivation of Lamaze technique (Zimmermann 1979). The Urech 2010 study used two control groups (progressive relaxation and passive relaxation) and for the purposes of this review, we combined the data into a single control group.
Interventions were performed during pregnancy (Ip 2009; Korol 1992; Teixeira 2005; Urech 2010; Vieten 2008; Zimmermann 1979) or during the first four weeks of the postpartum period (Rees 1993; Rees 1995). The number of intervention sessions ranged from one single session (Teixeira 2005; Urech 2010) to multiple sessions (Ip 2009; Korol 1992; Rees 1993; Rees 1995; Vieten 2008; Zimmermann 1979).
The mind‐body interventions focused on the management of maternal anxiety in pregnancy or in the postpartum period (Ip 2009; Korol 1992; Rees 1993; Rees 1995; Teixeira 2005; Urech 2010; Vieten 2008; Zimmermann 1979). Two studies selected participants on their anxiety levels before inclusion (Teixeira 2005; Vieten 2008).
Interventions used in the included studies
SeeCharacteristics of included studies.
1. Hypnotherapy
In one study (Teixeira 2005), one single session of hypnotherapy was compared to passive relaxation for reducing maternal self‐rating anxiety, heart rate, plasma catecholamines, plasma cortisol levels, and uterine artery Doppler resistance index.
2. Imagery
Five studies (N = 352 participants) compared imagery to a control group.
Korol 1992: instructors of antenatal classes were randomly assigned to teach an antenatal course that included or not guided imagery for improving the pregnant women's knowledge and attitude toward pain coping techniques during labor.
Rees 1993: the effectiveness of guided imagery was compared to listening to music for reducing anxiety and depression and increasing self‐esteem in women during the first four postpartum weeks.
Rees 1995: in a subsequent study, Rees 1993 used a similar protocol with the same objectives but outcomes (women's anxiety, depression and self‐esteem) were measured by reliable and validated scales.
Ip 2009: in this trial, the effectiveness of an efficacy‐enhancing educational intervention including imagery to promote women's self‐efficacy for childbirth and coping ability in reducing anxiety and pain during labor was compared to usual care.
Urech 2010: women were randomized into three groups. The aim of this study was to compare the immediate effects of two active and one passive 10‐minute relaxation techniques on perceived and physiological parameters.
3. Yoga
Thirty‐four participants were randomized to receive a complex intervention (mindfulness training that included yoga) or to be on a wait‐list intervention in order to explore the effects of such intervention on the positive affect and anxiety in pregnant women (Vieten 2008).
4. Autogenic training
With a total of 53 primiparous women (Zimmermann 1979), the efficacy of respiratory autogenic training was compared to traditional psychoprophylactic course for reducing muscle tension, anxiety and pain during labor and delivery.
Excluded studies
We excluded 42 studies. We have described reasons for exclusion in the Characteristics of excluded studiestables. We excluded studies because they were not randomized, they did not evaluate a mind‐body intervention or data on the primary outcome (anxiety) were not available, even after contact with the authors.
Risk of bias in included studies
We described the risk of bias of included studies in the 'Risk of bias tables' attached to the Characteristics of included studies tables and the judgements that we made are summarised in Figure 1 and Figure 2.
1.
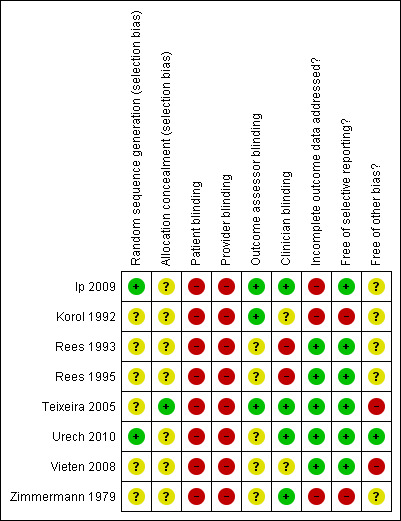
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
2.
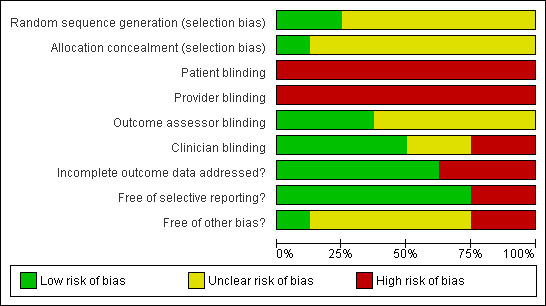
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
Allocation
We judged Teixeira 2005 to have 'adequate' allocation concealment, and although the methods used to generate the allocation sequence were not reported, women were assigned to their groups using closed envelopes. The remaining seven studies had 'unclear' allocation concealment. In five of those studies (Korol 1992; Rees 1993; Rees 1995; Vieten 2008; Zimmermann 1979), the methods used for sequence generate and allocation concealment were not described. Two studies (Ip 2009; Urech 2010) described an adequate method of sequence generation but had 'unclear' allocation concealment. In one study (Korol 1992), instructors but not participants were randomized and allocated to the intervention or control groups; however methods used for allocation generation and/or allocation concealment were not reported.
Blinding
As is often the case in studies evaluating non‐pharmacological interventions, blinding of participant and intervention provider was not feasible. Information on blinding of the clinician and the outcome assessor are included in the 'Risk of bias' tables. The outcome assessor was reported to be blinded in four studies (Ip 2009; Korol 1992; Teixeira 2005; Zimmermann 1979). Nevertheless, three studies reported objective outcomes (Teixeira 2005; Urech 2010; Zimmermann 1979). When the main outcome was self‐reported, we have classified the risk as unclear.
Incomplete outcome data
Four studies were devoid of dropouts (Rees 1993; Rees 1995; Teixeira 2005; Urech 2010). Four studies (Ip 2009; Korol 1992; Vieten 2008; Zimmermann 1979) reported adequate information about how many participants had withdrawn from the studies after having consented to participate. Among them, Zimmermann 1979, Vieten 2008 and Ip 2009 provided details about the reasons for such withdrawals. In all included studies, we have performed analyses on the final number of participants after attrition.
We evaluated each study for the possible risk of incomplete outcome data. Korol 1992 did not report the sample size of each group, but the authors privately provided us the information. Urech 2010 provided us with unpublished data on the primary outcome (anxiety) and physiological data. Rees 1993 did not report a dispersion index for the outcomes measured (e.g. standard deviation). In three studies (Ip 2009; Rees 1993; Rees 1995), data on anxiety at baseline were not reported.
Selective reporting
We evaluated each study for the possible risk of selective reporting bias. Most of the studies (Ip 2009; Rees 1993; Rees 1995; Teixeira 2005; Urech 2010; Vieten 2008) seemed to have a low risk of selective bias. For two studies, the risk of selective reporting bias was apparently high, since some of the outcomes described as to be measured in the study were ultimately not reported in the results (Korol 1992; Zimmermann 1979).
Other potential sources of bias
We assessed other sources of bias frequently reported in non‐pharmacological trials. Details on the care provider experience were not frequently reported: only Vieten 2008 described care provider’s competence but not their degree of experience. None of the studies measured women's expectations toward treatment efficacy before randomization. Six studies used a standardized intervention protocol (Ip 2009; Rees 1993; Rees 1995; Urech 2010; Teixeira 2005; Vieten 2008). None of the studies measured adherence to the protocol.
Effects of interventions
Hypnotherapy
Hypnotherapy versus passive relaxation
Anxiety
Compared to passive relaxation, only one study (Teixeira 2005) reported no significant effect after one session of hypnotherapy on anxiety (Table 1) and on maternal plasma noradrenaline (Table 2), adrenaline (Table 3), cortisol levels (Table 4) and maternal heart rate (Table 5). These data were reported as medians in the article (it was not a normal distribution) and that is why we have presented the data in an additional table.
1. Hypnotherapy versus passive relaxation: Teixeira 2005: post‐treatment anxiety state.
| Study ID | Median: hypnotherapy group | CI 95% | Median: control group | CI 95% |
| Teixeira 2005 | 24.5 | 23 to 27.5 | 27.5 | 25 to 30.5 |
2. Hypnotherapy versus passive relaxation: Teixeira 2005: maternal plasma noradrenaline.
| Study ID | Median: hypnotherapy‐group | CI 95% | Median: control‐group | CI 95% |
| Teixeira 2005 | 1.7 | 1.35 to 2.00 | 1.2 | 1.04 to 1.43 |
3. Hypnotherapy versus passive relaxation: Teixeira 2005: maternal plasma adrenaline.
| Study ID | Median: hypnotherapy‐group | CI 95% | Median: control‐group | CI 95% |
| Teixeira 2005 | 0.76 | 0.61 to 0.98 | 0.72 | 0.56 to 1.00 |
4. Hypnotherapy versus passive relaxation: Teixeira 2005: maternal plasma cortisol.
| Study ID | Median:hypnotherapy‐group | CI 95% | Median:control‐group | CI 95% |
| Teixeira 2005 | 620 | 492 to 707 | 555 | 494 to 608 |
5. Hypnotherapy versus passive relaxation: Teixeira 2005: maternal heart rate.
| Study ID | Median:hypnotherapy group | CI 95% | Median:control group | CI 95% |
| Teixeira 2005 | 78.5 | 73.5 to 82.5 | 81.5 | 75 to 88.5 |
Imagery
Imagery versus usual care
Anxiety
One of the two studies that used imagery during prenatal classes, suggests a borderline significant (P .06) difference in anxiety state during pregnancy (mean difference (MD) ‐3.90; 95% confidence intervals (CI) ‐7.94 to 0.14; Analysis 1.1) as compared to non‐imagery (Korol 1992)
1.1. Analysis.
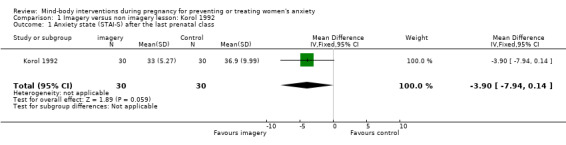
Comparison 1 Imagery versus non imagery lesson: Korol 1992, Outcome 1 Anxiety state (STAI‐S) after the last prenatal class.
However, in Ip 2009, anxiety levels were significantly decreased with imagery at the early and middle stages of labor (MD ‐1.46; 95% CI ‐2.43 to ‐0.49; one study, 133 women; Analysis 2.1; and MD ‐1.24; 95% CI ‐2.18 to ‐0.30; one study, 133 women; Analysis 2.2), but not at the last stage of labor (MD 0.63; 95% CI ‐0.57 to 1.83; one study, 133 women; Analysis 2.3).
2.1. Analysis.
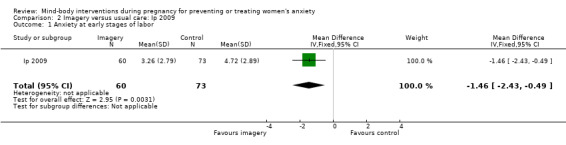
Comparison 2 Imagery versus usual care: Ip 2009, Outcome 1 Anxiety at early stages of labor.
2.2. Analysis.
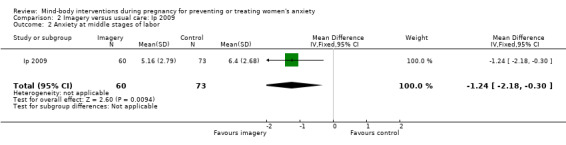
Comparison 2 Imagery versus usual care: Ip 2009, Outcome 2 Anxiety at middle stages of labor.
2.3. Analysis.
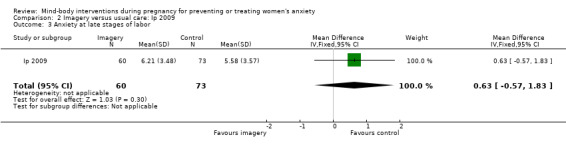
Comparison 2 Imagery versus usual care: Ip 2009, Outcome 3 Anxiety at late stages of labor.
Secondary outcomes
In the Korol 1992 study, women's knowledge on labor and delivery after the last prenatal class changed significantly in favor of the imagery group (MD 3.35; 95% CI 1.06 to 5.64; one study, 60 women; Analysis 1.2).
1.2. Analysis.
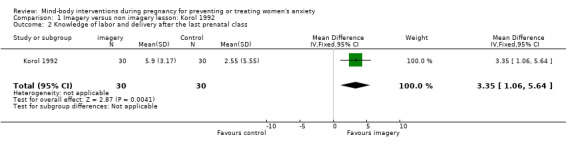
Comparison 1 Imagery versus non imagery lesson: Korol 1992, Outcome 2 Knowledge of labor and delivery after the last prenatal class.
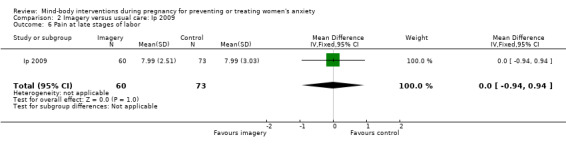
Pain levels in Ip 2009 were significantly decreased with imagery at the early and middle stages of labor ((MD ‐1.49; 95% CI ‐2.28 to ‐0.70; one study, 133 women; Analysis 2.4; and MD ‐0.97; 95% CI ‐1.69 to ‐0.25; one study, 133 women; Analysis 2.5)), but not at the last stage of labor (MD 0.00; 95% CI ‐0.94 to 0.94; one study, 133 women; Analysis 2.6). Furthermore, women in the imagery group reported higher levels of coping (MD 3.95; 95% CI 1.40 to 6.50; one study, 133 women; Analysis 2.7); higher levels of outcomes expectancy (MD 16.77; 95% CI 9.43 to 24.11; one study, 133 women; Analysis 2.8) and efficacy expectancy (MD 20.76; 95% CI 12.73 to 28.79; one study, 133 women; Analysis 2.9).
2.4. Analysis.
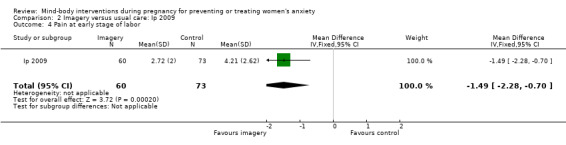
Comparison 2 Imagery versus usual care: Ip 2009, Outcome 4 Pain at early stage of labor.
2.5. Analysis.
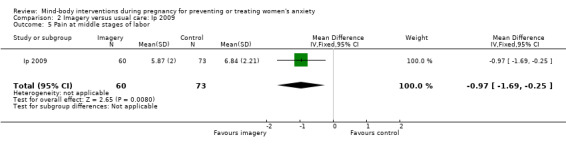
Comparison 2 Imagery versus usual care: Ip 2009, Outcome 5 Pain at middle stages of labor.
2.6. Analysis.
Comparison 2 Imagery versus usual care: Ip 2009, Outcome 6 Pain at late stages of labor.
2.7. Analysis.
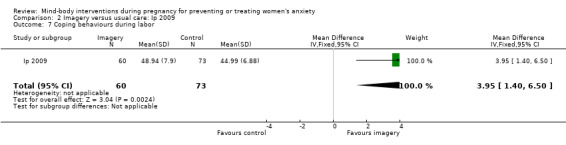
Comparison 2 Imagery versus usual care: Ip 2009, Outcome 7 Coping behaviours during labor.
2.8. Analysis.
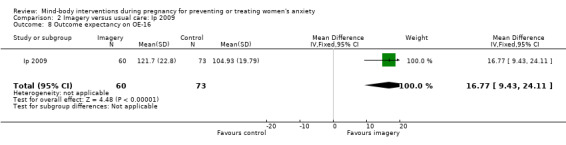
Comparison 2 Imagery versus usual care: Ip 2009, Outcome 8 Outcome expectancy on OE‐16.
2.9. Analysis.
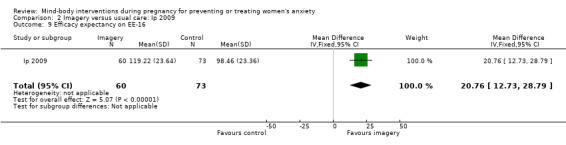
Comparison 2 Imagery versus usual care: Ip 2009, Outcome 9 Efficacy expectancy on EE‐16.
Imagery versus music
Anxiety
Compared with music therapy, a four‐week imagery intervention in women immediately post‐delivery (Rees 1995) was effective in significantly reducing state anxiety (MD ‐0.45; 95% CI ‐0.72 to ‐0.18; Analysis 4.1 ‐ Figure 12).
4.1. Analysis.
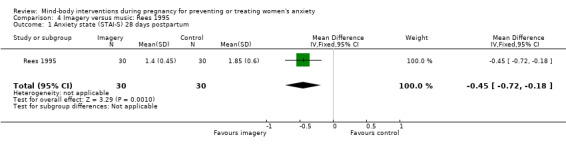
Comparison 4 Imagery versus music: Rees 1995, Outcome 1 Anxiety state (STAI‐S) 28 days postpartum.
In the study by Rees 1993, data on anxiety and depression were incomplete (no standard deviations reported); therefore, this study was not contributive to this review and no further analyses were performed.
Secondary outcomes
In the Rees 1995 study, a four‐week imagery intervention in women immediately post‐delivery was associated with reduced depression (MD ‐0.27; 95% CI ‐0.49 to 0.05; one study, 60 women; Analysis 4.2) and improved self‐esteem (MD 0.39; 95% CI 0.15 to 0.63; one study, 60 women; Analysis 4.3), compared with a music therapy control.
4.2. Analysis.
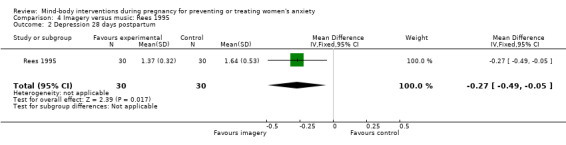
Comparison 4 Imagery versus music: Rees 1995, Outcome 2 Depression 28 days postpartum.
4.3. Analysis.
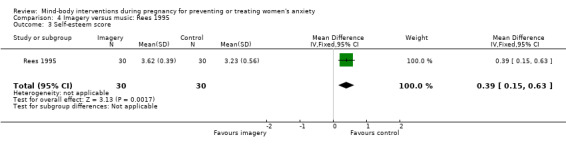
Comparison 4 Imagery versus music: Rees 1995, Outcome 3 Self‐esteem score.
Imagery versus combined group of progressive relaxation and passive relaxation
Anxiety
In one study, involving 39 women, Urech 2010 found that imagery failed to significantly reduce the anxiety immediately after the interventions, compared with a combined control group of progressive relaxation and passive relaxation (MD ‐0.12; 95% CI ‐0.29 to 0.05; Analysis 5.1).
5.1. Analysis.
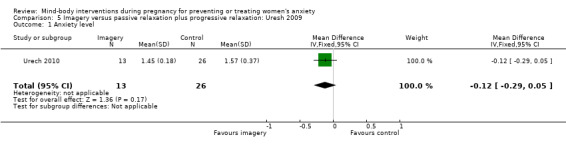
Comparison 5 Imagery versus passive relaxation plus progressive relaxation: Uresh 2009, Outcome 1 Anxiety level.
Secondary outcomes
Most of the physiological outcomes reported in Urech 2010 were not significantly changed by imagery: serum cortisol (MD 0.73; 95% CI ‐8.10 to 9.56; Analysis 5.2); serum ACTH (MD ‐4.96; 95% CI ‐13.91 to 3.99; Analysis 5.3); serum norepinephrine (MD ‐25.58; 95% CI ‐66.06 to 14.90; Analysis 5.4); heart rate (MD ‐2.84; 95% CI ‐8.00 to 2.32; Analysis 5.6); systolic blood pressure (MD 1.37; 95% CI ‐9.21 to 11.95; Analysis 5.7) and diastolic blood pressure (MD ‐1.79; 95% CI ‐7.89 to 4.31; Analysis 5.8). However, a significant effect was observed on the level of relaxation as reported by the women (MD 0.78; 95% CI 0.10 to 1.46; Analysis 5.9) and serum epinephrine (MD ‐9.60; 95% CI ‐17.19 to ‐2.01; Analysis 5.5).
5.2. Analysis.
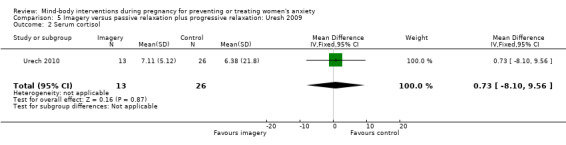
Comparison 5 Imagery versus passive relaxation plus progressive relaxation: Uresh 2009, Outcome 2 Serum cortisol.
5.3. Analysis.
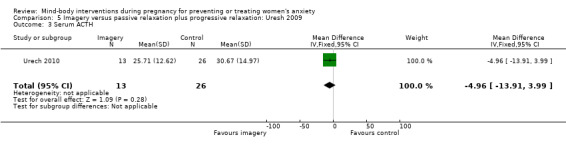
Comparison 5 Imagery versus passive relaxation plus progressive relaxation: Uresh 2009, Outcome 3 Serum ACTH.
5.4. Analysis.
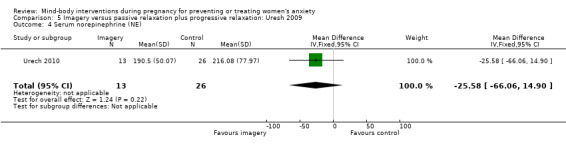
Comparison 5 Imagery versus passive relaxation plus progressive relaxation: Uresh 2009, Outcome 4 Serum norepinephrine (NE).
5.6. Analysis.
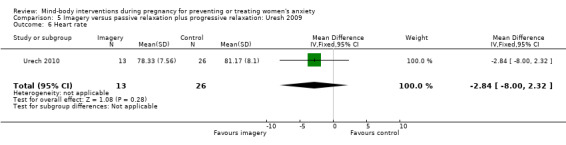
Comparison 5 Imagery versus passive relaxation plus progressive relaxation: Uresh 2009, Outcome 6 Heart rate.
5.7. Analysis.
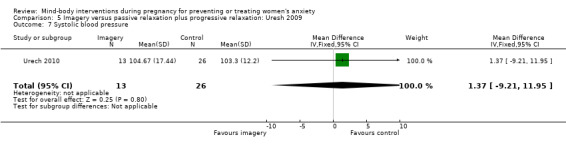
Comparison 5 Imagery versus passive relaxation plus progressive relaxation: Uresh 2009, Outcome 7 Systolic blood pressure.
5.8. Analysis.
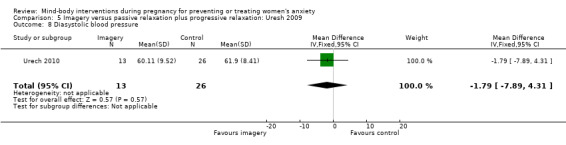
Comparison 5 Imagery versus passive relaxation plus progressive relaxation: Uresh 2009, Outcome 8 Diasystolic blood pressure.
5.9. Analysis.
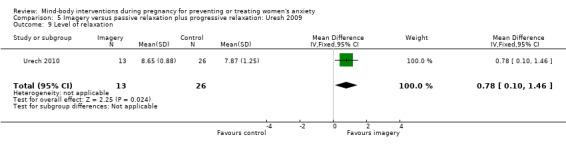
Comparison 5 Imagery versus passive relaxation plus progressive relaxation: Uresh 2009, Outcome 9 Level of relaxation.
5.5. Analysis.
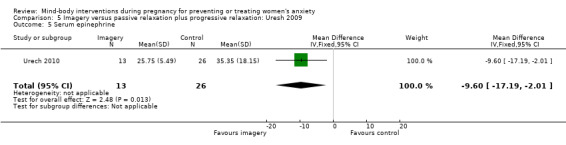
Comparison 5 Imagery versus passive relaxation plus progressive relaxation: Uresh 2009, Outcome 5 Serum epinephrine.
Yoga versus wait list
Anxiety
In the Vieten 2008 study, 31 women followed an eight‐week intervention including yoga. There was no significant reduction in anxiety state (MD ‐0.20; 95% CI ‐6.49 to 6.09; Analysis 6.1); however, taking into account pregnant women's anxiety levels at baseline, the authors reported a positive effect of yoga on anxiety.
6.1. Analysis.
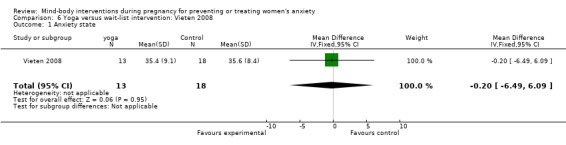
Comparison 6 Yoga versus wait‐list intervention: Vieten 2008, Outcome 1 Anxiety state.
Secondary outcomes
There were no significant differences observed for the following outcomes reported in the Vieten 2008 study: depression (MD 2.00; 95% CI ‐2.69 to 6.69; Analysis 6.2); perceived stress (MD ‐1.00; 95% CI ‐4.76 to 2.76; Analysis 6.3); negative affect (MD ‐1.70; 95% CI ‐5.22 to 1.82; Analysis 6.4); positive affect (MD 2.90; 95% CI ‐1.88 to 7.68; Analysis 6.5) and affect regulation (MD 9.20; 95% CI ‐7.39 to 25.79; Analysis 6.6).
6.2. Analysis.
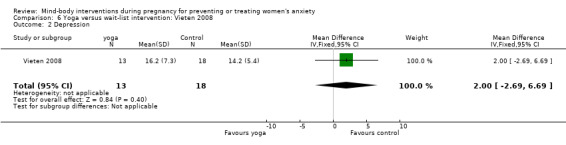
Comparison 6 Yoga versus wait‐list intervention: Vieten 2008, Outcome 2 Depression.
6.3. Analysis.
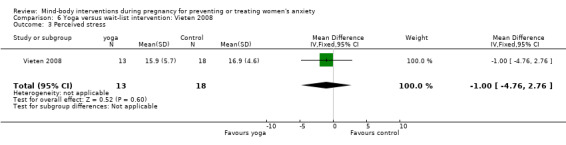
Comparison 6 Yoga versus wait‐list intervention: Vieten 2008, Outcome 3 Perceived stress.
6.4. Analysis.
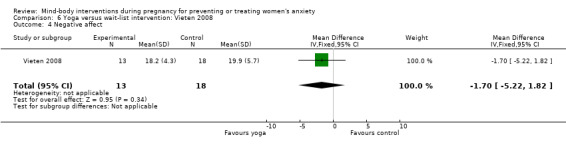
Comparison 6 Yoga versus wait‐list intervention: Vieten 2008, Outcome 4 Negative affect.
6.5. Analysis.
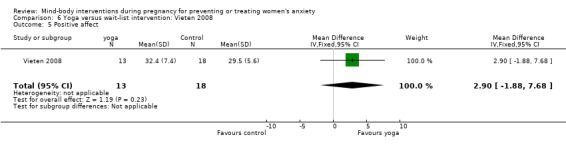
Comparison 6 Yoga versus wait‐list intervention: Vieten 2008, Outcome 5 Positive affect.
6.6. Analysis.
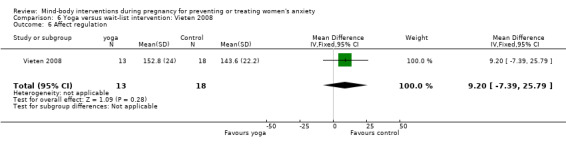
Comparison 6 Yoga versus wait‐list intervention: Vieten 2008, Outcome 6 Affect regulation.
Autogenic training
Autogenic training versus traditional psychoprophylaxis
Anxiety
Compared to traditional psychoprophylaxis, participants receiving autogenic training reported less anxiety before entering the labor room, but this difference was not statistically significant (MD ‐13.90; 95% CI ‐27.84 to 0.04; Analysis 7.1) (Zimmermann 1979).
7.1. Analysis.
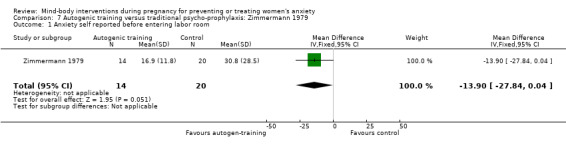
Comparison 7 Autogenic training versus traditional psycho‐prophylaxis: Zimmermann 1979, Outcome 1 Anxiety self reported before entering labor room.
Secondary outcomes
Autogenic training failed to reduce medication use: spasmolytic (RR 1.14; 95% CI 0.37 to 3.51; Analysis 7.2) or oxytocin (RR 1.14; 95% CI 0.82 to 1.59; Analysis 7.3).
7.2. Analysis.
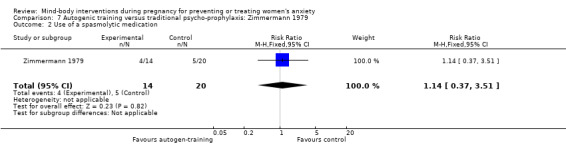
Comparison 7 Autogenic training versus traditional psycho‐prophylaxis: Zimmermann 1979, Outcome 2 Use of a spasmolytic medication.
7.3. Analysis.
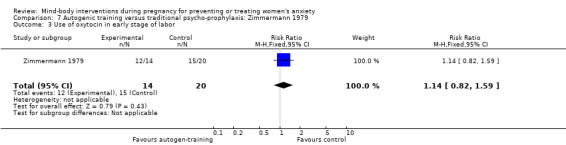
Comparison 7 Autogenic training versus traditional psycho‐prophylaxis: Zimmermann 1979, Outcome 3 Use of oxytocin in early stage of labor.
Discussion
Mind‐body interventions have been showed to be effective for decreasing anxiety levels in several clinical situations (Smith 2006; Uman 2006). Although anxiety may exert adverse perinatal outcomes, few studies have examined the effects of mind‐body interventions on women's anxiety during pregnancy. The primary objective of this review was to evaluate the effectiveness of mind‐body interventions for the management of women's anxiety during pregnancy. To date, eight randomized controlled trials with 556 participants are available for evaluation.
Considering the often poor quality of the included studies, there is some evidence for the effectiveness of mind‐body interventions on anxiety during pregnancy. Compared with usual care, imagery may have a positive effect on anxiety during labor (Ip 2009). Another study showed that imagery had a positive effect on anxiety and depression in the immediate postpartum period (Rees 1995). Autogenic training might be effective for decreasing women's anxiety before delivering (Zimmermann 1979). No harmful effects were reported for any mind‐body interventions in the studies included in the review. None of the included studies reported any of the neonatal secondary outcomes.
Studies that evaluated different forms of mind‐body interventions cannot be combined. Interventions were often well‐described but the adherence to a standardized protocol during the interventions was rarely measured, limiting the applicability. Due to the small number of studies per intervention and to the diversity of outcome measurements, we have performed no meta‐analysis, and reported results individually for each study. Some of the included mind‐body interventions were part of a complex intervention that made it difficult to isolate and evaluate their own specific effects on anxiety.
Several studies were at a high risk of bias. Assessment of randomization quality was difficult in the majority of studies, as the quality of reporting was frequently poor. Providers' and participants' blinding is not an option for mind‐body interventions. This could have introduced bias in favour of these interventions. Blinding of the clinicians in charge of co‐interventions and the outcome assessors are recommended, but was often not implemented or not reported. In addition, only few studies reported objective outcomes that might have compensated for the positive expectations of patients and providers. Moreover, small sample sizes and high dropout rates reduced the chances of detecting small effects.
In contrast to other clinical situations, there is insufficient evidence to assess the effectiveness of mind‐body interventions on anxiety and related outcomes in pregnant women. This is surprising since interventions such as hypnobirth and prenatal yoga are popular. There is an urgent need for more research in this area.
Authors' conclusions
Implications for practice.
Based on a small number of RCTs (with small sample sizes), mind‐body interventions might be useful for preventing anxiety during pregnancy. No evidence is available to draw conclusions about the value of mind‐body interventions for chronic anxiety. When delivered by certified providers, no adverse events are expected.
Implications for research.
Women's anxiety during pregnancy might adversely impact both mother and child health. Women at risk of anxiety might be targeted with specific interventions. Further high‐quality research is required to investigate whether mind‐body interventions are effective tools in managing or preventing women's anxiety during pregnancy and to measure its impact on perinatal outcomes. RCTs with standardized protocols, validated measurements and adequate sample sizes are required.
What's new
| Date | Event | Description |
|---|---|---|
| 3 October 2011 | Amended | Added citation of full paper for Urech 2010. |
Acknowledgements
The search strategies were designed by Isabelle Marc and Carole Thiebaut (Laval University) with significant help from Lynn Hampson (Trials Search Coordinator).
As part of the pre‐publication editorial process, this review has been commented on by three peers (an editor and two referees who are external to the editorial team), a member of the Pregnancy and Childbirth Group's international panel of consumers and the Group's Statistical Adviser.
We thank Bryan Stephenson for his translation of Almeida 2005 and Elizabeth Whiteley for her translation of Gatelli 2000.
Appendices
Appendix 1. Search strategies
MEDLINE
1. prenatal AND development
2. pregnancy
3. #1 OR #2
4. "autogenic training"[MeSH Terms]
5. Tai Chi
6. "suggestion"[MeSH Terms]
7. suggestion AND auto
8. "yoga"[MeSH Terms]
9. "hypnosis"[MeSH Terms]
10. hypnotherapy
11. "meditation"[MeSH Terms]
12. "biofeedback, psychology"[MeSH Terms]
13. mind‐body
14. "relaxation"[MeSH Terms]
15. #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14
16. #15 AND #3
17. #16 AND "humans"[MeSH Terms]
EMBASE
Prenatal‐Development#.DE.
Pregnancy#.W..DE.
1 OR 2
Autogenic‐Training.DE.
Guided‐Imagery.DE.
Relaxation‐Training.DE.
Tai‐Chi.DE.
Suggestion.W..DE.
Yoga.W..DE.
Hypnosis.W..DE.
Meditation.W..DE.
auto ADJ suggestion
guided ADJ imagery
prayer$.TI,AB.
hypnosis.TI,AB.
hypnotherapy.TI,AB.
(mind ADJ body) .TI,AB.
( tai chi OR yoga).TI,AB.
(relax OR relaxation) AND (therapy OR training OR technique$)
(meditat$ or autosuggestion).TI,AB.
4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14 OR 15 OR 16 OR 17 OR 18 OR 19 OR 20
3 AND 21
HUMAN=YES
ClinicalTrials.gov (December 2010) and Current Controlled Trials (December 2010) We searched by combining terms for each of the therapies with the term pregnan*
National Center for Complementary and Alternative Medicine (NCCAM) (December 2010) We browsed the alphabetical list of clinical trials for any relevant trials.
Appendix 2. Searches carried out up to November 2008
Authors searched the following:
CINAHL (1982 to November 2008), PsycINFO (1840 to November 2008), AMED (The Allied and Complementary Medicine Database) (1985 to November 2008), and the British Nursing Index (1994 to November 2008) using the following search strategies:
CINAHL (EBSCO)
"Mind‐Body‐Techniques#.DE.
autosuggestion
auto ADJ suggestion
(autogenic AND (training OR therapy))
mind ADJ body
( hypnosis OR hypnotherapy).TI,AB.
( guided ADJ imagery ).TI,AB.
prayer$.TI,AB.
meditat$.TI,AB.
tai chi OR yoga).TI,AB.
((relax OR relaxation) .TI,AB. AND ( therapy OR training OR techniques$ ) .TI,AB.
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11
Pregnancy#.W..DE.
Pregnan$.TI,AB.
Obstetric‐Care#.DE.
13 or 14 or 15
16 and 12
PsycINFO (OVID)
exp Autogenic Training/
exp RELAXATION THERAPY/
exp Guided Imagery/
exp HYPNOTHERAPy
exp MEDITATION/
exp YOGA/
autosuggestion.mp.
auto‐suggestion.mp.
exp HYPNOSIS/
exp PRAYER/
(Tai adj chi).mp.
(mind adj body).mp.
(hypnosis or hypnotherapy).ti,ab.
(guided adj imagery).mp.
((relax$ or relaxation) and (training or therapy or technique$)).ti,ab.
exp pregnancy/
exp prenatal care/
exp Prenatal Development/
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 14 or 15
16 or 17 or 18
19 and 20
AMED (Allied and Complementary Medicine) (OVID)
exp YOGA/
autosuggestion.mp.
auto‐suggestion.mp.
(Tai adj chi).mp.
(mind adj body).mp.
(hypnosis or hypnotherapy).ti,ab.
(guided adj imagery).mp.
((relax$ or relaxation) and (training or therapy or technique$)).ti,ab.
mind body relations/
exp Psychosomatic therapies/
pregnancy/
pregnan$.mp.
exp obstetrical care/
exp pregnancy complications/
yoga.mp.
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 15
11 or 12 or 13 or 14
16 and 17
BNI (British Nursing Index) (OVID)
exp YOGA/
autosuggestion.mp.
auto‐suggestion.mp.
(Tai adj chi).mp.
(mind adj body).mp.
(hypnosis or hypnotherapy).ti,ab.
(guided adj imagery).mp.
((relax$ or relaxation) and (training or therapy or technique$)).ti,ab.
yoga.mp.
meditation.mp.
autogenic.mp.
suggestion.mp.
exp HYPNOSIS/
prayer.mp.
pregnancy/
pregnan$.mp.
exp pregnancy complications/
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14
15 or 16 or 17
18 and 19
Data and analyses
Comparison 1. Imagery versus non imagery lesson: Korol 1992.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Anxiety state (STAI‐S) after the last prenatal class | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐3.90 [‐7.94, 0.14] |
| 2 Knowledge of labor and delivery after the last prenatal class | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 3.35 [1.06, 5.64] |
Comparison 2. Imagery versus usual care: Ip 2009.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Anxiety at early stages of labor | 1 | 133 | Mean Difference (IV, Fixed, 95% CI) | ‐1.46 [‐2.43, ‐0.49] |
| 2 Anxiety at middle stages of labor | 1 | 133 | Mean Difference (IV, Fixed, 95% CI) | ‐1.24 [‐2.18, ‐0.30] |
| 3 Anxiety at late stages of labor | 1 | 133 | Mean Difference (IV, Fixed, 95% CI) | 0.63 [‐0.57, 1.83] |
| 4 Pain at early stage of labor | 1 | 133 | Mean Difference (IV, Fixed, 95% CI) | ‐1.49 [‐2.28, ‐0.70] |
| 5 Pain at middle stages of labor | 1 | 133 | Mean Difference (IV, Fixed, 95% CI) | ‐0.97 [‐1.69, ‐0.25] |
| 6 Pain at late stages of labor | 1 | 133 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.94, 0.94] |
| 7 Coping behaviours during labor | 1 | 133 | Mean Difference (IV, Fixed, 95% CI) | 3.95 [1.40, 6.50] |
| 8 Outcome expectancy on OE‐16 | 1 | 133 | Mean Difference (IV, Fixed, 95% CI) | 16.77 [9.43, 24.11] |
| 9 Efficacy expectancy on EE‐16 | 1 | 133 | Mean Difference (IV, Fixed, 95% CI) | 20.76 [12.73, 28.79] |
Comparison 4. Imagery versus music: Rees 1995.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Anxiety state (STAI‐S) 28 days postpartum | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐0.45 [‐0.72, ‐0.18] |
| 2 Depression 28 days postpartum | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐0.27 [‐0.49, ‐0.05] |
| 3 Self‐esteem score | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.39 [0.15, 0.63] |
Comparison 5. Imagery versus passive relaxation plus progressive relaxation: Uresh 2009.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Anxiety level | 1 | 39 | Mean Difference (IV, Fixed, 95% CI) | ‐0.12 [‐0.29, 0.05] |
| 2 Serum cortisol | 1 | 39 | Mean Difference (IV, Fixed, 95% CI) | 0.73 [‐8.10, 9.56] |
| 3 Serum ACTH | 1 | 39 | Mean Difference (IV, Fixed, 95% CI) | ‐4.96 [‐13.91, 3.99] |
| 4 Serum norepinephrine (NE) | 1 | 39 | Mean Difference (IV, Fixed, 95% CI) | ‐25.58 [‐66.06, 14.90] |
| 5 Serum epinephrine | 1 | 39 | Mean Difference (IV, Fixed, 95% CI) | ‐9.60 [‐17.19, ‐2.01] |
| 6 Heart rate | 1 | 39 | Mean Difference (IV, Fixed, 95% CI) | ‐2.84 [‐6.00, 2.32] |
| 7 Systolic blood pressure | 1 | 39 | Mean Difference (IV, Fixed, 95% CI) | 1.37 [‐9.21, 11.95] |
| 8 Diasystolic blood pressure | 1 | 39 | Mean Difference (IV, Fixed, 95% CI) | ‐1.79 [‐7.89, 4.31] |
| 9 Level of relaxation | 1 | 39 | Mean Difference (IV, Fixed, 95% CI) | 0.78 [0.10, 1.46] |
Comparison 6. Yoga versus wait‐list intervention: Vieten 2008.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Anxiety state | 1 | 31 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐6.49, 6.09] |
| 2 Depression | 1 | 31 | Mean Difference (IV, Fixed, 95% CI) | 2.0 [‐2.69, 6.69] |
| 3 Perceived stress | 1 | 31 | Mean Difference (IV, Fixed, 95% CI) | 1.00 [‐4.76, 2.76] |
| 4 Negative affect | 1 | 31 | Mean Difference (IV, Fixed, 95% CI) | ‐1.70 [‐5.22, 1.82] |
| 5 Positive affect | 1 | 31 | Mean Difference (IV, Fixed, 95% CI) | 2.90 [‐1.88, 7.68] |
| 6 Affect regulation | 1 | 31 | Mean Difference (IV, Fixed, 95% CI) | 9.20 [‐7.39, 25.79] |
Comparison 7. Autogenic training versus traditional psycho‐prophylaxis: Zimmermann 1979.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Anxiety self reported before entering labor room | 1 | 34 | Mean Difference (IV, Fixed, 95% CI) | ‐13.90 [‐27.84, 0.04] |
| 2 Use of a spasmolytic medication | 1 | 34 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.37, 3.51] |
| 3 Use of oxytocin in early stage of labor | 1 | 34 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.82, 1.59] |
| 4 Length of dilatation period | 1 | 34 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Expulsion time | 1 | 34 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
7.4. Analysis.
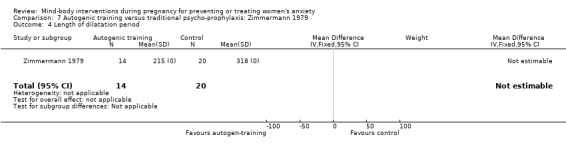
Comparison 7 Autogenic training versus traditional psycho‐prophylaxis: Zimmermann 1979, Outcome 4 Length of dilatation period.
7.5. Analysis.
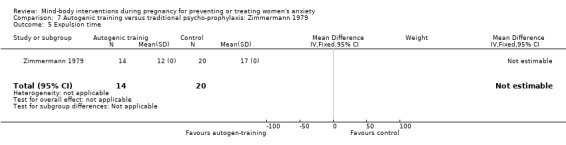
Comparison 7 Autogenic training versus traditional psycho‐prophylaxis: Zimmermann 1979, Outcome 5 Expulsion time.
Characteristics of studies
Characteristics of included studies [author‐defined order]
Teixeira 2005.
| Methods | Randomized controlled trial. | |
| Participants | N = 58 women (30 women scoring high and 28 women scoring low on the state index of the STAI at baseline). Inclusion criteria: non‐smoking women between 28 and 32 weeks of gestation, with singleton pregnancies and without medical complications. Exclusion criteria: not reported. Setting: participants were recruited in the antenatal clinic at the Chelsea and Westminster Hospital, London, UK. |
|
| Interventions |
Intervention group: 1 session of active relaxation based on hypnotherapy induced by a stress management expert. Control group: 1 session of passive relaxation (seating quietly for 45 min, reading a magazine). |
|
| Outcomes | Anxiety (STAI) Spielberger 1983); uterine resistance index (by Doppler); maternal heart rate; maternal plasma noradrenaline; maternal plasma adrenaline; maternal plasma cortisol. Times of assessment of the main outcomes: at baseline and after the relaxation period. |
|
| Notes | At baseline, groups were similar regarding anxiety levels and other outcomes of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported. |
| Allocation concealment (selection bias) | Low risk | Subjects were randomly assigned using closed envelopes. |
| Patient blinding | High risk | Not feasible. |
| Provider blinding | High risk | Not feasible. |
| Outcome assessor blinding | Low risk | Outcomes were objective. Doppler studies were performed by assessor blinding to subject group. |
| Clinician blinding | Low risk | Co‐interventions are the same in both groups. |
| Incomplete outcome data addressed? | Low risk | No attrition. |
| Free of selective reporting? | Low risk | All prespecified outcomes seem to be reported. |
| Free of other bias? | High risk | Interventions were standardized. |
Korol 1992.
| Methods | Randomized controlled trial. | |
| Participants | N = 60 women participating to antenatal classes, 30 participants per group. Inclusion criteria: not reported. Exclusion criteria: not reported. Setting: patients were recruited from the community in antenatal classes in a western Canadian city, at the University of Ottawa, ON, Canada. |
|
| Interventions | 6 imagery classes and 8 non‐imagery classes. Intervention group: imagery visualization (birth visualization, information on labor and delivery) and relaxation. Control group: a non‐imagery lesson (information on labor and delivery) and relaxation. |
|
| Outcomes |
For participants: anxiety (STAI); absorption level (Tellegen absorption scale); knowledge about labor and delivery and the accompanying emotions and physical sensations (Childbirth Education Review); satisfaction with the relaxation techniques and imagery; expectation of pain and perceived ability to control pain during childbirth (VAS). For instructors: attitudes toward the use of imagery in childbirth education by interview. Times of assessment of the main outcomes: at baseline, after the final prenatal class, and at follow‐up in the 2 weeks before the expected delivery date. |
|
| Notes | At baseline, no statistically significant difference was found between groups regarding anxiety level and the other outcomes of interest. Before randomization, all instructors attended a workshop on the use of imagery. A significant effect on "knowledge about labor and delivery" was observed when data post‐intervention were not adjusted for baseline data. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported. |
| Allocation concealment (selection bias) | Unclear risk | Instructors were randomly assigned to the imagery or the non‐imagery group. |
| Patient blinding | High risk | Not feasible. |
| Provider blinding | High risk | Not feasible. |
| Outcome assessor blinding | Low risk | Measures were scored by a nurse who was blind to group assignment. Questionnaires were completed at home and sent back to the center. No objectives outcomes. |
| Clinician blinding | Unclear risk | No data collected by a clinician. |
| Incomplete outcome data addressed? | High risk | Data collected after the final prenatal class were available for all participants. At follow‐up, data are reported for only 37 of the 60 participants. No details given on the attrition rate per group. |
| Free of selective reporting? | High risk | Many prespecified outcomes were not reported in results. |
| Free of other bias? | Unclear risk | Risk of contamination. Instructors were the same to give the intervention to both groups. |
Ip 2009.
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: a Hong Kong Chinese resident; aged 18 or above; at the 32nd and 34th weeks’ gestation; planning to have a singleton by vaginal delivery; able to read and understand Chinese. Exclusion criteria: would not stay in Hong Kong after discharge; had a planned caesarean section. |
|
| Interventions | N = 192 participants were recruited, 96 in each group. However, only 133 participants were analysed (60 in the intervention group and 73 in the control group). Intervention group: self‐efficacy enhancing educational programme (SEEEP): complex educational and motivational intervention including imagery by groups of 6 people or fewer for an optimal interaction and discussion. Control group: usual care which included regular physical check‐up and attending childbirth classes on a voluntary basis. |
|
| Outcomes | Self‐reported anxiety (VAS); self‐reported pain (VAS); coping behaviours during labor (Childbirth coping behaviour scale); women's coping ability for childbirth including Outcome expectancy and Efficacy expectancy measured by the short form of the Chinese Childbirth Self‐Efficacy Inventory. Time of assessment of the main outcomes: at baseline, 37th of gestation and 48 h post delivery. |
|
| Notes | Based on description of the intervention in the manuscript, it was difficult for us to classify this intervention. More details were provided from the authors and allowed us to consider the intervention as a complex intervention which included some imagery. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Women were randomly assigned to either the experimental or the control group by a computer‐generated random‐number table. |
| Allocation concealment (selection bias) | Unclear risk | Not specified. |
| Patient blinding | High risk | Not feasible. |
| Provider blinding | High risk | Not feasible. |
| Outcome assessor blinding | Low risk | The outcome assessor was blind for the following outcomes: anxiety, pain and coping behaviours during labor. |
| Clinician blinding | Low risk | Co‐interventions seemed to be the same in both groups. |
| Incomplete outcome data addressed? | High risk | Hight dropout level. Above 20% in each group. Reasons for were reported and were different in both groups. |
| Free of selective reporting? | Low risk | All prespecified outcomes seemed to be included. |
| Free of other bias? | Unclear risk | Anxiety at baseline were not specified or measured. |
Rees 1995.
| Methods | Randomized controlled trial. | |
| Participants | N = 60 women, 30 in each group. Inclusion criteria: postpartum primiparous without major complication during antenatal, intra‐natal and postpartum periods, with full‐term infant. Exclusion criteria: not reported. Setting: postpartum units of hospitals in southwestern USA communities, University of New Mexico, NM, USA. |
|
| Interventions |
Intervention group: relaxation with guided imagery by listening to an audiotape for 15 min each morning for 4 weeks. The protocol included physical relaxation and focused on the formation of mental images. Control group: listening to music for 15 min each morning for 4 weeks. |
|
| Outcomes | Anxiety (STAI‐form Y); depression (Center of Epidemiologic Studies Depression Scale (CES‐D)) and self‐esteem (Rosenberg Self‐esteem Scale). Times of assessment of the main outcomes: at baseline and 4 weeks later (end of the study). |
|
| Notes | Scores on the STAI reported seems to be lower than the published range of STAI scores (20 to 80). No numerical data were reported on anxiety, depression and self‐esteem for the experimental and control groups at baseline. Authors reported that groups were similar. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported. |
| Allocation concealment (selection bias) | Unclear risk | Participants were randomly assigned to one of the 2 groups. |
| Patient blinding | High risk | Not feasible. |
| Provider blinding | High risk | Not feasible. |
| Outcome assessor blinding | Unclear risk | Outcomes were self‐reported. No objective outcomes. |
| Clinician blinding | High risk | Not applicable. |
| Incomplete outcome data addressed? | Low risk | No attrition. |
| Free of selective reporting? | Low risk | All prespecified outcomes were included. |
| Free of other bias? | Unclear risk | No numerical data were reported on anxiety, depression and self‐esteem for the experimental and control groups at baseline. |
Rees 1993.
| Methods | Randomized controlled trial. | |
| Participants | N = 60 women, 30 per group. Inclusion criteria: healthy primiparous postpartum women. Exclusion criteria: not reported. Setting: participants were recruited in postpartum units in 2 hospitals, University of New Mexico, NM, USA. |
|
| Interventions |
Intervention group: relaxation with guided imagery by listening to an audiotape for 15 min each morning for 4 weeks. The protocol included physical relaxation and focused on the formation of mental images. Control group: listening to music tape ("The Planets" by Gustav Holst), 15 min each morning for 4 weeks. |
|
| Outcomes | Anxiety (self‐rated on a scale of 1 to 7); depression (self‐rated on a scale of 1 to 7); self‐esteem (self‐rated on a scale of 1 to 7) in a daily log each evening. Times of assessment of the main outcomes: at baseline and every day, from day 1 of the study to day 28 (end of the study). |
|
| Notes | No numerical data were reported on anxiety, depression and self‐esteem for the experimental and control groups at baseline. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported. |
| Allocation concealment (selection bias) | Unclear risk | Participants were randomly assigned to one of the 2 groups. |
| Patient blinding | High risk | Not feasible. |
| Provider blinding | High risk | Not feasible. |
| Outcome assessor blinding | Unclear risk | Self‐reported outcome. |
| Clinician blinding | High risk | Not applicable. |
| Incomplete outcome data addressed? | Low risk | No attrition, all participants recruited were analyzed. Did not report SDs for the outcome means. |
| Free of selective reporting? | Low risk | All prespecified outcomes were included. No reported data on anxiety, depression and self‐esteem at baseline. |
| Free of other bias? | Unclear risk | Unknown reliability and validity of scales. |
Urech 2010.
| Methods | Randomized controlled trial. | |
| Participants | N = 39 participants were recruited, 13 in each group. Inclusion criteria: pregnant women aged > 18 years with a single, healthy fetus; between the 32nd and 34th week of gestation; German‐speaking. Exclusion criteria: intake of glucocorticoids; preexisting cardiovascular, nephrological, neurological or metabolic diseases; bad obstetric history as well as intra uterine growth restricted (IUGR) fetuses; fetal malformations; preterm uterine contractions; pregnancy‐induced hypertension and/or pre‐eclampsia. |
|
| Interventions | One intervention group and 2 control groups were evaluated in this study. Group guided imagery (GI): the exercise was delivered by headphones. Participants were instructed to imagine a safe place and invite a person to accompany them who could promote their feeling of security and wellbeing. After the procedure, participants were encouraged to practice at home. Progressive muscle relaxation (PMR): the relaxation exercise was also delivered by headphones. The PMR exercise was adapted from Jacobson and adjusted to pregnancy by leaving out the abdominal musculature in the exercise. After the procedure, participants were encouraged to practice at home. Group passive relaxation control condition: participants were instructed to sit quietly in a semi‐recumbent position for a time equivalent to the intervention in the other groups. |
|
| Outcomes | Anxiety (STAI‐S); level of relaxation (VAS); cortisol; ACTH; norepinephrine (NE); epinephrine (E); women satisfaction (score of 5‐point); blood pressure (systolic and diastolic); heart rate; compliance. Time of assessment of the main outcomes: at 4 time points before and after the relaxation exercise. |
|
| Notes | Author was contacted and provided us with detailed numerical data on all outcomes. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomly assigned using a randomized number table. |
| Allocation concealment (selection bias) | Unclear risk | Participants were not told about group allocation until 1 min prior to the relaxation intervention. |
| Patient blinding | High risk | Not feasible. |
| Provider blinding | High risk | Not feasible. |
| Outcome assessor blinding | Unclear risk | Not reported. Anxiety was self‐reported. Physiological measurements are objective outcomes. |
| Clinician blinding | Low risk | No co‐intervention. |
| Incomplete outcome data addressed? | Low risk | No dropout. |
| Free of selective reporting? | Low risk | Data were presented on graphs in the publication but numerical were provided by the authors. |
| Free of other bias? | Low risk | Reporting was clear |
Vieten 2008.
| Methods | Randomized controlled trial. | |
| Participants | N = 34 women. 14 in intervention group and 20 in control group. Inclusion criteria: pregnant women between 12 and 30 weeks of gestation, who reported to have a history of mood concerns for which they sought some form of treatment, such as psychotherapy, counseling, or medication and were English‐speaking. Exclusion criteria: history of mental disorder, inability to attend each of the classes or participate in the assessments or unable to speak English. Setting: participants were recruited through physicians' offices, childbirth education classes, and in the community. The study took place at a large private non‐profit hospital in San Francisco, CA, USA. |
|
| Interventions |
Intervention group: 8 sessions (120 min per session) of mindfulness intervention including approximately equal parts of education, discussion and experiential exercises. It is a complex intervention which includes awareness of the developing fetus and belly during the body scan meditation; explanatory examples and exercises relating to pregnancy and early parenting regarding pain or sleep issues during pregnancy, anxiety about labor, or dealing with a difficult‐to‐console infant; walking and moving mindfulness practices such a prenatal yoga. Daily home practice using a compact disc and reading was encouraged. Group control: wait‐list intervention (standard care). This group received the intervention at the end of the study after the post‐natal follow‐up. |
|
| Outcomes | Perceived stress (The Perceived Stress Scale); depression (Center for Epidemiologic Studies Depression Scale); anxiety (STAI); positive and negative affect (The Positive and Negative Affect Schedule ‐ Extended); affect regulation (the Affect Regulation Measure); mindfulness (The Mindful Attention Awareness Scale); adherence to the intervention. Times of assessment of the main outcomes: a baseline (during the two weeks prior to the start of the intervention). Second assessment occurred in the week following the end of the experimental group intervention (8 to 10 weeks after baseline assessment) and postnatal follow‐up occurred 3 months after the second assessment. |
|
| Notes | At baseline, groups were similar regarding anxiety level and other outcomes of interest. Providers were trained and certified psychologists and prenatal yoga instructors. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported. |
| Allocation concealment (selection bias) | Unclear risk | Women were randomized to the experimental group or to the wait‐list control group. |
| Patient blinding | High risk | Not feasible. |
| Provider blinding | High risk | Not feasible. |
| Outcome assessor blinding | Unclear risk | Not reported. Primary outcome and most of other outcomes were self‐reported. No objective outcome. |
| Clinician blinding | Unclear risk | No information on the co‐interventions. |
| Incomplete outcome data addressed? | Low risk | Attrition: 13% (2/15) in experimental group; 5% (1/19) in control group. Reasons for drop out were reported. |
| Free of selective reporting? | Low risk | All prespecified outcomes seemed to be included. |
| Free of other bias? | High risk | No control for time and attention in control group. Participants' expectations toward intervention were not assessed at baseline. No monitoring of the adherence to the protocol of the intervention. |
Zimmermann 1979.
| Methods | Randomized controlled trial. | |
| Participants | N = 53 participants were recruited. Only 34 were analyzed, 14 in the respiratory autogenic training group and 20 in the traditional psychoprophylactic course group. Inclusion criteria: married primipara (20 and 35 years), in the 7th month of pregnancy, no physical abnormalities, who had already participated in no less than five preparation courses for childbirth. Exclusion criteria: not reported. Setting: participants were recruited through childbirth course at the Obstetrics Clinic of the University of Verona (Verona, Italy). |
|
| Interventions | 9 weekly sessions in each group. Intervention group: respiratory autogenic training, derives from the autogenous training in the Schultz and Jacobson's progressive relaxation method. 7 exercises in which the woman, by concentrating on her body, learns sensations in order to diminish her muscle tonus by deep relaxation. Every session includes theoretical lectures about the physiology of pregnancy and delivery and group discussions about the medical and psychological problems connected with them. Control group: traditional psychoprophylactic course, derived from Lamaze and consisting in the combination of lectures and group discussions regarding the problems of pregnancy and delivery with specific gymnastics exercises. |
|
| Outcomes | Anxiety (Morbid Anxiety Inventory); anxiety self‐rating; relaxation self‐rating; use of medication during labor; pain assessment; length of the dilatation period; expulsion time; baby weight; Apgar score; women's views on their delivery and attendance to the course. Times of assessment of the main outcomes: at baseline, after admission for delivery, during labor and after delivery. |
|
| Notes | At baseline, groups were similar regarding anxiety level and other outcomes of interest. Theoretical lectures were performed by the same lecturers in both groups and courses were conducted by the same obstetrical team of physiotherapists, midwives, doctors and psychologists. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Participants were randomly assigned to their groups. |
| Patient blinding | High risk | Not feasible. |
| Provider blinding | High risk | Not feasible. |
| Outcome assessor blinding | Unclear risk | Some outcomes were self‐reported. |
| Clinician blinding | Low risk | Doctors who made the clinical evaluations were unaware of which training course the subject had attended. Some of the co‐interventions (medication use) were considered as outcomes. |
| Incomplete outcome data addressed? | High risk | High dropout rate. N = 53 participants were recruited. Only 34 out of 53 eligible participants were analyzed; details about the drop out are given. |
| Free of selective reporting? | High risk | Outcomes defined in the methods were not all reported in the results. |
| Free of other bias? | Unclear risk | Risk of contamination between groups |
min: minutes SD: standard deviation STAI: State Trait Anxiety Inventory VAS: visual analogue scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Almeida 2005 | Not a RCT. This study aimed to evaluate the effect of respiration and relaxation techniques on pain and anxiety during labor. Does not evaluate a mind‐body intervention. |
| Astbury 1980 | RCT, N = 90 investigated the effectiveness of childbirth education intervention in pregnancy and during labor in reducing maternal anxiety. This study was excluded because it does not evaluate a mind‐body intervention. |
| Bastani 2006 | RCT, N = 110. Does relaxation education in anxious primigravid Iranian women influence adverse pregnancy outcomes? The aim of the study was to evaluate the effect of relaxation in anxious pregnant Iranian women on anxiety, perceived stress and neonatal outcomes. It does not evaluate a mind‐body intervention. |
| Bauer 2010 | A randomized controlled trial of music and recreation therapy to alleviate distress during antepartum hospitalization. It does not evaluate a mind‐body intervention. |
| Beck 1980 | This study evaluated a standard Lamaze training in pregnant women on maternal preparation and anxiety. It was excluded because it does not evaluate a mind‐body intervention. |
| Bosco 2007 | Acupuncture for mild to moderate emotional complaints in pregnancy‐‐a prospective, quasi‐randomized, controlled study. Does not evaluate a mind‐body intervention. |
| Brown 1999 | RCT (pilot study), N = 4. The objectives of the study were to assess the feasibility of a RCT evaluating effectiveness of medical hypnosis in prolonging pregnancy for patients in preterm labor. Control group was usual care. No data on anxiety are available. |
| Casko 2002 | Thesis. Theses are excluded unless they are published. |
| Cha 2001 | RCT, N = 199. The aim of the study was to assess the potential effect of intercessory prayer on pregnancy rates in women being treated with IVF‐ET. Control group was no intervention. No published data on anxiety. Information was asked to authors without a response. |
| Chambers 2007 | Thesis. Theses are excluded unless they are published. |
| Chang 2008 | RCT, N = 236. Effects of music therapy on psychological health of women during pregnancy. Not a mind‐body intervention (music). |
| Chuntharapat 2008 | RCT, N = 74. The aim of the study was to examine the effects of a yoga program during pregnancy on maternal comfort, labor pain, and birth outcomes. Control group was routine care, discussion sessions and weekly telephone calls. Maternal trait anxiety was assessed at baseline but anxiety was not an outcome. Author was contacted for additional information on anxiety (no response). |
| Dasari 2007 | RCT, N = 50. The aims of the study were to compare the effect of tocolysis along with a psychotherapeutic intervention including relaxation and meditation on the prolongation of pregnancy and on neonatal outcomes in pregnant women with preterm labor. Control group was tocolysis alone. No anxiety data. Authors were contacted for any unpublished data on anxiety (no response). |
| Duchene 1989 | RCT, N = 55. The aim of the study was to evaluate the effects of biofeedback on childbirth pain. Control group intervention was a Lamaze technique. No data on anxiety were available. Originals authors contacted without response. |
| Feher 1989 | RCT, N = 71. The objective of the study was to evaluate an intervention for increasing breast milk production in mothers of premature infants admitted at the neonatal unit. Guided imagery techniques were compared with routine supportive care. This study was excluded because anxiety was not reported as an outcome. We contacted author for additional data but without a response. |
| Field 1997 | RCT, N = 28. 28 women were recruited from prenatal classes and randomly assigned to receive massage in addition to coaching in breathing from their partners during labor, or to receive coaching in breathing alone. We excluded the study because it does not evaluate a mind‐body intervention. |
| Field 1999 | RCT, N = 26 pregnant women were assigned to a massage therapy or a relaxation therapy group for 5 weeks. We excluded the study because it does not evaluate a mind‐body intervention. |
| Field 2004 | RCT, N = 84. Depressed pregnant women were recruited during the second trimester of pregnancy and randomly assigned to a massage therapy group, a progressive muscle relaxation group or a control group that received standard prenatal care alone. Does not evaluate a mind‐body intervention. |
| Field 2009 | RCT, N = 113. Depressed women were randomly assigned to a group of Interpersonal psychotherapy or interpersonal psychotherapy plus massage therapy. Not a mind‐body intervention. |
| Freeman 1986 | RCT, N = 82. The aim of the study was to evaluate the effectiveness of self‐hypnosis on pain relief, satisfaction, and analgesic requirements in pregnant primigravidas willing to avoid epidural anesthesia. Control group was not specified. No published data on anxiety. Authors contacted but without response. |
| Gatelli 2000 | Excluded because it does not evaluate a mind‐body intervention. In the aim to evaluate the experience in labor and delivery, participants were assigned to an obstetric psychoprophylaxis course (OPP) plus individual guided relaxation sessions, to OPP plus individual psychological counselling sessions, or only to OPP. |
| Guse 2006 | RCT, N = 46. The aim of the study was to evaluate the effect of a prenatal hypnotherapy program on the postnatal psychological well‐being of first‐time mothers. No data on anxiety (as confirmed by the author). |
| Harmon 1990 | RCT, N = 45. The aim of the study was to assess the effectiveness of a bio‐behavioral intervention (relaxation and biofeedback, bed rest and compliance enhancement training) in addition to the treatment of mild pregnancy‐induced hypertension in hypertensive women between 30‐36 weeks of gestation. Control condition was bed rest alone and bed rest with compliance enhancement training. No data on anxiety as an outcome (as confirmed by authors). |
| Holt 2008 | RCT, intervention group is allocated to a CBT group program. The trial is still open to recruitment. Does not evaluate a mind‐body intervention. |
| Janke 1999 | RCT, N = 107. To examine the effect of relaxation on preterm labor outcomes. 2 groups, daily relaxation exercise or control group. A third group was added to the study: women who were originally assigned to the relaxation group but were unable to adhere to the daily practice. We excluded the study because it does not evaluate a mind‐body intervention. |
| Larden 2004 | RCT, N = 54. Participants were randomly assigned to receive either therapeutic touch, shared activity with a registered nurse or standard ward care. Does not evaluate a mind‐body intervention. |
| Lee 2006 | Not a RCT: effects of a Qigong prenatal education program on anxiety, depression and physical symptoms in pregnant women. Not a mind‐body intervention. |
| Liebman 1989 | Thesis. Theses are excluded unless they are published. |
| Little 1984 | RCT, N = 60. The aim of the study was to determine whether relaxation therapy alone or combined with biofeedback training reduces blood pressure and prevents hospital admissions in hypertensive pregnant women. Control group was usual care. Women's anxiety was measured at baseline but was not an outcome. |
| Lukesch 1980 | 2 groups of primiparae were subjected to 2 different forms of basically behavior therapeutic treatments which aimed to reduce birth anxiety. In comparison with an untreated control group a significant reduction of birth anxieties was found. Not a RCT. |
| Marcus 1995 | RCT, N = 31. The aim of the study was to compare the efficacy of a combined non‐pharmacological treatment (relaxation, skin‐warming biofeedback, and physical therapy) with attention (headache education and skin‐cooling biofeedback) on the management of headache during pregnancy. Control group received headache education and skin‐cooling biofeedback. This study was excluded because anxiety was not reported as an outcome. The author was contacted and confirmed that no anxiety data were available. |
| Martin 2001 | RCT, N = 47. The aim of the study was to evaluate how childbirth preparation incorporating hypnotic techniques affect the labor processes and birth outcomes in pregnant adolescents. Control group was supportive counseling. Women's anxiety was not an outcome (as confirmed by the author). |
| Mehl‐Madrona 2004 | RCT, N = 720. The aim of the study was to determine if a program of prenatal hypnosis could reduce birth complications. Comparison group was supportive psychotherapy and a reference group without any intervention. Anxiety was measured at baseline but was not an outcome. Author was contacted for data on anxiety (no response). |
| Rock 1969 | RCT, N = 40. The aims of the study were to evaluate hypnotic techniques as an aid to labor management. Control group was standard care. No anxiety data were reported as an outcome. No contact with the author was possible to retrieve unpublished data on anxiety. |
| Satyapriya 2009 | RCT, N = 122 patients. The aim of the study was to evaluate the effect of integrated yoga practice and guided yogic relaxation on both perceived stress and measured autonomic response in healthy pregnant women. No data on anxiety. Authors have been contacted (no response). |
| Schorn 2009 | RCT, N = 60. The aim of this RCT was to test the effects of guided imagery on blood loss during third stage of labor. No anxiety data. |
| Shaw 1993 | Thesis. Theses are excluded unless they are published. |
| Somers 1989 | RCT, N = 45. The aim of the study was to assess the effectiveness of a bio‐behavioral intervention (relaxation and biofeedback, bed rest and compliance enhancement training) in adjunct to treatment of mild pregnancy‐induced hypertension in women between 30‐36 weeks of gestation. Control condition was bed rest alone and bed rest with compliance enhancement training. No data on anxiety were collected (as confirmed by the authors). |
| St‐James Robert 1982 | RCT, N = 39. The aim of this study was to evaluate the adjunct of biofeedback relaxation procedures to conventional antenatal training and childbirth. Aims were to compare autonomic (skin conductance level) and voluntary‐muscle (electro‐myographic) relaxation training procedures, and to determine whether either or both procedures facilitated the labor and delivery of women receiving the training. Control group received relaxation and education classes. We excluded this study after the author was contacted and confirmed that no anxiety data were available. |
| Valbo 1996 | RCT, N = 130. The aim of the study was to evaluate a hypnotic intervention for smoking cessation and smoking reduction among women who were smoking in pregnancy. Control group intervention was routine care. We excluded the study because the author was contacted and confirmed that no anxiety data were available. |
| Yang 2009 | Music therapy to relieve anxiety in pregnant women on bedrest. RCT but does not evaluate a mind‐body intervention. |
| Yim 2005 | Thesis. Theses are excluded unless they are published. |
RCT: randomized controlled trial
Characteristics of studies awaiting assessment [ordered by study ID]
Ahmadian 2009.
| Methods | Randomized controlled trial. |
| Participants | 280 uncomplicated pregnant women (140 experimental group and 140 control group). |
| Interventions | Antenatal educational interventions. |
| Outcomes | Anxiety measured by the Spielberger state‐trait anxiety inventory during latent and active phase of labor. |
| Notes | Abstract published in International Journal of Gynecology & Obstetrics. No details on the intervention used in this trial are given in the abstract. Further details on the publication and data were requested from the authors (waiting for response). |
Fisher 2009.
| Methods | Randomized controlled trial. |
| Participants | 38 women were randomized and completed the study. |
| Interventions | Hypnobirthing versus standard childbirth preparation course. |
| Outcomes | Patient attitudes toward coping mechanisms; role of her partner and nurse; anxiety level. |
| Notes | Abstract published in the American Journal of Obstetrics and Gynecology 2009. Further details on the publication and data were requested from the authors (waiting for response). |
Jallo 2008.
| Methods | Prospective, longitudinal study using controlled randomized experimental design. |
| Participants | N = 59 women. |
| Interventions | The intervention was a set of 3 R‐GI (imagery) CDs developed and sequenced to influence study outcomes. |
| Outcomes | Perceived Stress Scale (PSS), anxiety (STAI‐state) and plasma CRH levels were collected at 3 times. |
| Notes | We are waiting for the full version of the paper (not available) to complete the evaluation of this study. |
Taghavi 2009.
| Methods | Randomized controlled trial. |
| Participants | 280 pregnant women (140 experimental and 140 control). |
| Interventions | Antenatal education intervention. |
| Outcomes | Pain; delivery process. |
| Notes | This study seems to be the same as Ahmadian 2009 reporting different outcomes. Abstract published in International Journal of Gynecology & Obstetrics. No details on the intervention used in this trial are given in the abstract. Further details on the publication and data were requested from the authors (waiting for response). |
STAI: State Trait Anxiety Inventory
Characteristics of ongoing studies [ordered by study ID]
Cyna 2006.
| Trial name or title | Hypnosis Antenatal Training for Childbirth (HATCh): a randomized controlled trial. |
| Methods | A single centre, randomized controlled trial using a 3‐arm parallel group design in the largest tertiary maternity unit in South Australia. |
| Participants | Women > 34 and < 39 weeks' gestation, planning a vaginal birth, not in active labor, with a singleton, viable fetus of vertex presentation, are eligible to participate. |
| Interventions |
Group 1: participants receive antenatal hypnosis training in preparation for childbirth administered by a qualified hypnotherapist with the use of an audio compact disc on hypnosis for re‐enforcement. Group 2: consists of antenatal hypnosis training in preparation for childbirth using an audio compact disc on hypnosis administered by a nurse with no training in hypnotherapy; Group 3: participants continue with their usual preparation for childbirth with no additional intervention. |
| Outcomes | The use of pharmacological analgesia during labor and childbirth; use of oxytocics, the mode of delivery, neonatal Apgar score at 5 minutes < 7 and maternal admission to the high dependency unit or the ICU. Maternal side effects such as: postpartum hemorrhage => 600 ml; blood transfusion; death; ICU admission, meconium‐stained liquor; babies admitted to neonatal unit. |
| Starting date | December 2005. |
| Contact information | Cyna A: allan.cyna@cywhs.sa.gov.au |
| Notes | The recruitment is completed, confirmed by authors. |
Milgrom 2008a.
| Trial name or title | Toward parenthood: delivering an antenatal self‐help intervention with telephone support for depression, anxiety and parenting difficulties ‐ facilitating the perinatal health journey. |
| Methods | Randomized controlled trial. |
| Participants | Women, 20 to 30 weeks of gestation. |
| Interventions | Intervention group receives self‐help guidebooks (for participants and their partners), 8 weekly telephone support sessions from therapists until 6 weeks postpartum and networking with health professionals. |
| Outcomes | Depression Anxiety Stress Scales; Information about birth and services used. |
| Starting date | 30/06/2006. |
| Contact information | jeannette.milgrom@austin.org.au |
| Notes | Trial is closed: follow‐up continuing (based on "Australian New Zealand Clinical Trials Registry" on December 2010). To classify this study, more details on intervention are needed. Authors have been contacted about date of publication (no response). |
ICU: intensive care unit
Differences between protocol and review
We have performed additional searching of the following resources up to November 2008 using the strategy described in Appendix 2 (seeAppendix 2 for details): CINAHL; PsycINFO; AMED (The Allied and Complementary Medicine Database); and the British Nursing Index. However, we were not able to run these searches after November 2008.
We will analyze the secondary neonatal outcomes in subgroup analyses depending on the presence or absence of an effect of the interventions on anxiety.
Contributions of authors
Isabelle Marc (IM) wrote the first draft of the protocol. IM and Narimane Toureche (NT) selected and classified the studies to be included with Claudine Blanchet (CB) and Sylvie Dodin (SD) if a consensus is needed. IM and NT extracted the data. NT entered relevant data, carried out the risk of bias assessment and discussed it with IM. M Njoya statistician is the resource person at CHUQ if a meta‐analysis is eventually necessary. NT (as part of her MSc in epidemiology) wrote the first draft of the review under IM supervision. Ellen Hodnett, Edzart Ernst, Claudine Blanchet and Sylvie Dodin commented on the review.
Sources of support
Internal sources
No sources of support supplied
External sources
-
Canadian Institutes of Health Research, Canada.
Scholarship (RCT mentoring program) awarded to Isabelle Marc : grant number MTP85228
Declarations of interest
Isabelle Marc and Sylvie Dodin received a grant from the Canadian Institute of Health Research and conducted a clinical trial to investigate the benefits of hypnosis for pain and anxiety management in pregnancy termination.
Edited (no change to conclusions)
References
References to studies included in this review
Ip 2009 {published data only}
- Ip WY, Tang CS, Goggins WB. An educational intervention to improve women's ability to cope with childbirth. Journal of Clinical Nursing 2009;18(15):2125‐35. [DOI] [PubMed] [Google Scholar]
Korol 1992 {published and unpublished data}
- Korol C, Baeyer C. Effects of brief instruction in imagery and birth visualisation in prenatal education. Journal of Mental Imagery 1992;16(3 & 4):167‐72. [Google Scholar]
Rees 1993 {published data only}
- Rees BL. An exploratory study of the effectiveness of a relaxation with guided imagery protocol. Journal of Holistic Nursing 1993;11(3):271‐6. [DOI] [PubMed] [Google Scholar]
Rees 1995 {published data only}
- Rees BL. Effect of relaxation with guided imagery on anxiety, depression, and self‐esteem in primiparas. Journal of Holistic Nursing 1995;13(3):255‐67. [DOI] [PubMed] [Google Scholar]
Teixeira 2005 {published data only}
- Teixeira J, Martin D, Prendiville O, Glover V. The effects of acute relaxation on indices of anxiety during pregnancy. Journal of Psychosomatic Obstetrics & Gynecology 2005;26(4):271‐6. [DOI] [PubMed] [Google Scholar]
Urech 2010 {published data only}
- Urech C, Alder J, Bitzer J, Hosli I. The effect of relaxation exercises on psychological wellbeing during pregnancy [Entspannungs‐Ubungen wahrend der Schwangerschaft: Der Einfluss auf das psychobiologische Wohlbefinden]. Geburtshilfe und Frauenheilkunde 2009;69:163. [Google Scholar]
- Urech C, Fink NS, Wilhelm FH, Bitzer J, Alder J. Effects of relaxation on psychobiological wellbeing during pregnancy: a randomized controlled trial. Psychoneuroendocrinology 2010;35:1348‐55. [DOI] [PubMed] [Google Scholar]
Vieten 2008 {published data only}
- Vieten C, Astin J. Effects of a mindfulness‐based intervention during pregnancy on prenatal stress and mood: results of a pilot study. Archives of Women's Mental Health 2008;11(1):67‐74. [DOI] [PubMed] [Google Scholar]
Zimmermann 1979 {published data only}
- Zimmermann‐Tansella CH, Dolcetta G, Azziniv V, Zacche G, Bertagni P, Siani R, et al. Preparation courses for childbirth in primipara. A comparison. Journal of Psychosomatic Research 1979;23(4):227‐33. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Almeida 2005 {published data only}
- Almeida NA, Sousa JT, Bachion MM, Silveira NA. The use of respiration and relaxation techniques for pain and anxiety relief in the parturition process [Utilizacao de tecnicas de respiracao e relaxamento para alivio de dor e ansiedade no processo de parturicao]. Revista Latino‐Americana de Enfermagem 2005;13(1):52‐8. [DOI] [PubMed] [Google Scholar]
Astbury 1980 {published data only}
- Astbury J. The crisis of childbirth: can information and childbirth education help?. Journal of Psychosomatic Research 1980;24:9‐13. [DOI] [PubMed] [Google Scholar]
Bastani 2006 {published data only}
- Bastani F, Hidarnia A, Kazemnejad A, Vafaei M, Kashanian M. A randomized controlled trial of the effects of applied relaxation training on reducing anxiety and perceived stress in pregnant women. Journal of Midwifery & Women's Health 2005;50(4):e36‐e40. [DOI] [PubMed] [Google Scholar]
- Bastani F, Hidarnia A, Montgomery KS, Aguilar‐Vafaei ME, Kazemnejad A. Does relaxation education in anxious primigravid Iranian women influence adverse pregnancy outcomes? A randomized controlled trial. Journal of Perinatal & Neonatal Nursing 2006;20(2):138‐46. [DOI] [PubMed] [Google Scholar]
Bauer 2010 {published data only}
- Bauer CL, Victorson D, Rosenbloom S, Barocas J, Silver RK. Alleviating distress during antepartum hospitalization: a randomized controlled trial of music and recreation therapy. Journal of Women's Health 2010;19(3):523‐31. [DOI] [PubMed] [Google Scholar]
Beck 1980 {published data only}
- Beck NC, Siegel LJ, Davidson NP, Kormeier S, Breitenstein A, Hall DG. The prediction of pregnancy outcome: maternal preparation, anxiety and attitudinal sets. Journal of Psychosomatic Research 1980;24:343‐51. [DOI] [PubMed] [Google Scholar]
Bosco 2007 {published data only}
- Bosco Guerreiro da Silva J. Acupuncture for mild to moderate emotional complaints in pregnancy‐‐a prospective, quasi‐randomised, controlled study. Acupuncture in Medicine 2007;25(3):65‐71. [DOI] [PubMed] [Google Scholar]
Brown 1999 {published data only}
- Brown Dc, Murphy M. Medical hypnosis in preterm labor: a randomized clinical trial. Report of two pilot projects. Hypnos 1999;26(2):77‐87. [Google Scholar]
Casko 2002 {published data only}
- Casko RB. An analysis of the effectiveness of relaxation training for preterm labor and of interactions between relaxation exercises, state and trait anxiety, and desire for control in women with preterm labor [thesis]. Iowa: University of Iowa, 2002. [Google Scholar]
Cha 2001 {published data only}
- Cha KY, Wirth DP, Lobo RA. Does prayer influence the success of in vitro fertilization‐embryo transfer? Report of a masked, randomized trial. Journal of Reproductive Medicine 2001;49(9):781‐7. [PubMed] [Google Scholar]
Chambers 2007 {published data only}
- Chambers AS. Relaxation during pregnancy to reduce stress and anxiety and their associated complications [thesis]. Arizona, USA: Univeristy of Arizona, 2007. [Google Scholar]
Chang 2008 {published data only}
- Chang MY, Chen CH, Huang KF. Effects of music therapy on psychological health of women during pregnancy. Journal of Clinical Nursing 2008;17(19):2580‐7. [DOI] [PubMed] [Google Scholar]
Chuntharapat 2008 {published data only}
- Chuntharapat S, Petpichetchian W, Hatthakit U. Yoga during pregnancy: effects on maternal comfort, labor pain and birth outcomes. Complementary Therapies in Clinical Practice 2008;14(2):105‐15. [DOI] [PubMed] [Google Scholar]
Dasari 2007 {published data only}
- Dasari P, Kodenchery MM. Psychological factors in preterm labor and psychotherapeutic intervention. International Journal of Gynecology & Obstetrics 2007;97(3):196‐7. [DOI] [PubMed] [Google Scholar]
Duchene 1989 {published data only}
- Duchene P. Effects of biofeedback on childbirth pain. Journal of Pain & Symptom Management 1989;4(3):117‐23. [DOI] [PubMed] [Google Scholar]
Feher 1989 {published data only}
- Feher SD, Berger LR, Johnson JD, Wilde JB. Increasing breast milk production for premature infants with relaxation and imagery. Pediatrics 1989;83:57‐60. [PubMed] [Google Scholar]
Field 1997 {published data only}
- Field T, Hernandez Reif M, Taylor S, Quintino O, Burman I. Labor pain is reduced by massage therapy. Journal of Psychosomatic Obstetrics and Gynaecology 1997;18(4):286‐91. [DOI] [PubMed] [Google Scholar]
Field 1999 {published data only}
- Field T, Hernandez‐Reif M, Hart S, Theakston H, Schanberg S, Kuhn C. Pregnant women benefit from massage therapy. Journal of Psychosomatic Obstetrics and Gynaecology 1999;20(1):31‐8. [DOI] [PubMed] [Google Scholar]
Field 2004 {published data only}
- Field T, Diego MA, Hernandez‐Reif M, Schanberg S, Kuhn C. Massage therapy effects on depressed pregnant women. Journal of Psychosomatic Obstetrics and Gynaecology 2004;25:115‐22. [DOI] [PubMed] [Google Scholar]
Field 2009 {published data only}
- Field T, Deeds O, Diego M, Hernandez‐Reif M, Gauler A, Sullivan S, et al. Benefits of combining massage therapy with group interpersonal psychotherapy in prenatally depressed women. Journal of Bodywork & Movement Therapies 2009;13(4):297‐303. [DOI] [PMC free article] [PubMed] [Google Scholar]
Freeman 1986 {published data only}
- Freeman RM, Macaulay AJ, Eve L, Chamberlain GV, Bhat AV. Randomised trial of self hypnosis for analgesia in labour. British Medical Journal Clinical Research Ed 1986;292(6521):657‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gatelli 2000 {published data only}
- Gatelli L, Panzeri M, Casadei D, Pagan F. Obstetric psychophysiology and quality of the experience of labour/delivery: application within hospitals. Medicina Psicosomatica 2000;45:89‐100. [Google Scholar]
Guse 2006 {published data only}
- Guse T, Wissing M, Hartman W. The effect of a prenatal hypnotherapeutic programme on postnatal maternal psychological well‐being. Journal of Reproductive & Infant Psychology 2006;24(2):163‐77. [Google Scholar]
Harmon 1990 {published data only}
- Harmon TM, Hynan MT, Tyre TE. Improved obstetric outcomes using hypnotic analgesia and skill mastery combined with childbirth education. Journal of Consulting & Clinical Psychology 1990;58(5):525‐30. [DOI] [PubMed] [Google Scholar]
Holt 2008 {published data only}
- Holt C. Beating the blues before birth: evaluating an antenatal depression treatment model as a public health priority. Australian New Zealand Clinical Trials Registry (www.anzctr.org.au) (accessed 19 February 2008).
Janke 1999 {published data only}
- Janke J. The effect of relaxation therapy on preterm labor outcomes. Journal of Obstetric Gynecologic and Neonatal Nursing 1999;28(3):255‐63. [DOI] [PubMed] [Google Scholar]
Larden 2004 {published data only}
- Larden CN, Palmer ML, Janssen P. Efficacy of therapeutic touch in treating pregnant inpatients who have a chemical dependency. Journal of Holistic Nursing 2004;22(4):320‐32. [DOI] [PubMed] [Google Scholar]
Lee 2006 {published data only}
- Lee KO, Kim KR, Ahn SH. Effects of a Qigong prenatal education program on anxiety, depression and physical symptoms in pregnant women. Korean Journal of Women Health Nursing 2006;12(3):240‐8. [Google Scholar]
Liebman 1989 {published data only}
- Liebman SS. The effects of music and relaxation on third trimester anxiety in adolescent pregnancy [thesis]. Miami, USA: University of Miami, 1989. [Google Scholar]
Little 1984 {published data only}
- Little BC, Hayworth J, Benson P, Hall F, Beard RW, Dewhurst J, Priest RG. Treatment of hypertension in pregnancy by relaxation and biofeedback. Lancet 1984;1(8382):865‐7. [DOI] [PubMed] [Google Scholar]
Lukesch 1980 {published data only}
- Lukesch H, Kochenstein P, Holz C. Therapeutical treatment of primiparae to reduce anxieties in connection with pregnancy and delivery [Therapeutische Interventionen bei Erstgebarenden mit Geburtsangsten.]. Zeitschrift fur Geburtshilfe und Perinatologie 1980;184(4):303‐9. [PubMed] [Google Scholar]
Marcus 1995 {published data only}
- Marcus DA, Scharff L, Turk DC. Nonpharmacological management of headaches during pregnancy. Psychosomatic Medicine 1995;57(6):527‐35. [DOI] [PubMed] [Google Scholar]
Martin 2001 {published data only}
- Martin AA, Schauble PG, Rai SH, Curry Jr. R. The Effects of hypnosis on the labor processes and birth outcomes of pregnant adolescents. Journal of Family Practice 2001;50:441‐3. [PubMed] [Google Scholar]
Mehl‐Madrona 2004 {published data only}
- Mehl‐Madrona Le. Hypnosis to facilitate uncomplicated birth. American Journal of Clinical Hypnosis. 2004;46(4):299‐312. [DOI] [PubMed] [Google Scholar]
Rock 1969 {published data only}
- Rock NL, Shipley TE, Campbell C. Hypnosis with untrained, nonvolunteer patients in labor. International Journal of Clinical and Experimental Hypnosis 1969;17(1):25‐36. [DOI] [PubMed] [Google Scholar]
Satyapriya 2009 {published data only}
- Satyapriya M, Nagendra HR, Nagarathna R, Padmalatha V. Effect of integrated yoga on stress and heart rate variability in pregnant women. International Journal of Gynecology & Obstetrics 2009;104(3):218‐22. [DOI] [PubMed] [Google Scholar]
Schorn 2009 {published data only}
- Schorn, MN. The effect of guided imagery on the third stage of labor: a pilot study. Journal of Alternative and Complementary Medicine 2009;15(8):863‐70. [DOI] [PubMed] [Google Scholar]
Shaw 1993 {published data only}
- Shaw ER. Effect of therapeutic relaxation on anxiety and mood states in primiparous women [thesis]. University of South Carolina, 1993. [Google Scholar]
Somers 1989 {published data only}
- Somers PJ, Gevirtz RN, Jasin SE, Chin HG. The efficacy of biobehavioral and compliance interventions in the adjunctive treatment of mild pregnancy‐induced hypertension. Biofeedback & Self Regulation 1989;14(4):309‐18. [DOI] [PubMed] [Google Scholar]
St‐James Robert 1982 {published data only}
- James‐Roberts I, Chamberlain G, Haran FJ, Hutchinson CM. Use of electromyographic and skin‐conductance biofeedback relaxation training of facilitate childbirth in primiparae. Journal of Psychosomatic Research 1982;26(4):455‐62. [DOI] [PubMed] [Google Scholar]
- James‐Roberts I, Hutchinson CMPA, Haran FJ, Chamberlain G. Can biofeedback‐based relaxation training be used to help women with childbirth?. Journal of Reproductive and Infant Psychology 1983;1:5‐10. [Google Scholar]
Valbo 1996 {published data only}
- Valbo A, Eide T. Smoking cessation in pregnancy: the effect of hypnosis in a randomized study. Addictive Behaviors 1996;21(1):29‐35. [DOI] [PubMed] [Google Scholar]
Yang 2009 {published data only}
- Yang M, Li L, Zhu H, Alexander IM, Liu S, Zhou W, et al. Music therapy to relieve anxiety in pregnant women on bedrest: a randomized, controlled trial. MCN, American Journal of Maternal Child Nursing 2009;34(5):316‐23. [DOI] [PubMed] [Google Scholar]
Yim 2005 {published data only}
- Yim IPW. The effect of a theory‐based intervention on promoting self‐efficacy for childbirth amongst pregnant women in Hong Kong [thesis]. University of Hong Kong, 2005. [Google Scholar]
References to studies awaiting assessment
Ahmadian 2009 {published data only}
- Ahmadian heris S, Taghavi S, Hoseininasab D. The effect of antenatal education interventions on state‐trait anxiety in the parturition process. International Journal of Gynecology & Obstetrics 2009;107(Suppl 2):S548. [Google Scholar]
Fisher 2009 {published data only}
- Fisher B, Esplin S, Stoddard G, Silver R. Randomized controlled trial of hypnobirthing versus standard childbirth classes: patient satisfaction and attitudes towards labor. American Journal of Obstetrics and Gynecology 2009;201(6 Suppl 1):S61‐S62. [Google Scholar]
Jallo 2008 {published data only}
- Jallo N, Bourguignon C, Taylor AG, Ruiz J, Goehler L. The biobehavioral effects of relaxation guided imagery on maternal stress. Advances in Mind‐Body Medicine 2009;24(4):12‐22. [PubMed] [Google Scholar]
Taghavi 2009 {published data only}
- Taghavi S, Hoseininasab D, Ahmadian heris S. The effect of antenatal education on pain intensity and labor. International Journal of Gynecology & Obstetrics 2009;107(Suppl 2):S493. [Google Scholar]
References to ongoing studies
Cyna 2006 {published data only}
- Cyna A. Hypnosis antenatal training for childbirth (HATCh): a randomised controlled trial (ongoing trial). ClinicalTrials.gov (http://clinicaltrials.gov/) (accessed 21 March 2006). [DOI] [PMC free article] [PubMed]
- Cyna AM, Andrew MI, Robinson JS, Crowther CA, Baghurst P, Turnbull D, et al. Hypnosis antenatal training for childbirth (HATCh): a randomised controlled trial. BMC Pregnancy and Childbirth 2006;6:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Milgrom 2008a {published data only}
- Milgrom J. Toward parenthood: delivering an antenatal self‐help intervention with telephone support for depression, anxiety and parenting difficulties ‐ facilitating the perinatal health journey. Australian New Zealand Clinical Trials Registry (www.anzctr.org.au) (accessed 19 February 2008).
Additional references
Alder 2007
- Alder J, Fink N, Bitzer J, Hösli I, Holzgreve W. Depression and anxiety during pregnancy: a risk factor for obstetric, fetal and neonatal outcome? A critical review of the literature. Journal of Maternal‐Fetal and Neonatal Medicine 2007;20(3):189‐209. [DOI] [PubMed] [Google Scholar]
Alvik 2006
- Alvik A, Heyerdahl S, Haldorsen T, Lindemann R. Alcohol use before and during pregnancy: a population‐based study. Acta Obstetricia et Gynecologica Scandinavica 2006;85(11):1292‐8. [DOI] [PubMed] [Google Scholar]
Andersson 2004
- Andersson L, Sundstrom‐Poromaa I, Wulff M, Astrom M, Bixo M. Implications of antenatal depression and anxiety for obstetric outcome. Obstetrics & Gynecology 2004;104(3):467‐76. [DOI] [PubMed] [Google Scholar]
Anonymous 2008
- Anonymous. Preterm birth: what can be done?. Lancet 2008;371(9606):2. [DOI] [PubMed] [Google Scholar]
Barragan Loayza 2006
- Barragán Loayza IM, Gonzales F. Biofeedback for pain during labour. (Protocol). Cochrane Database of Systematic Reviews 2006, Issue 4. [DOI: 10.1002/14651858.CD006168] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brisch 2003
- Brisch KH, Munz D, Bemmerer‐Mayer K, Terinde R, Kreienberg R, Kachele H. Coping styles of pregnant women after prenatal ultrasound screening for fetal malformation. Journal of Psychosomatic Research 2003;55(2):91‐7. [DOI] [PubMed] [Google Scholar]
Britton 2008
- Britton JR. Maternal anxiety: course and antecedents during the early postpartum period. Depression and Anxiety 2008;25(9):793‐800. [DOI] [PubMed] [Google Scholar]
Carmodi 2008
- Carmodya TP, Duncana C, Solkowitz S, Huggins J, Lee S, Delucchi K. Hypnosis for smoking cessation: a randomized trial. Nicotine & Tobacco Research 2008;10(5):811‐8. [DOI] [PubMed] [Google Scholar]
Coleman 2008
- Coleman VH, Carter MM, Morgan MA, Schulkin J. Obstetrician‐gynecologists' screening patterns for anxiety during pregnancy. Depression and Anxiety 2008;25(2):114‐23. [DOI] [PubMed] [Google Scholar]
Costei 2002
- Costei AM, Kozer E, Ho T, Ito S, Koren G. Perinatal outcome following third trimester exposure to paroxetine. Archives of Pediatrics & Adolescent Medicine 2002;156(11):1129‐32. [DOI] [PubMed] [Google Scholar]
Cwikel 2004
- Cwikel J, Gidron Y, Sheiner E. Psychological interactions with infertility among women. European Journal of Obstetrics & Gynecology and Reproductive Biology 2004;117(2):126‐31. [DOI] [PubMed] [Google Scholar]
DiPietro 2006
- DiPietro JA, Novak MF, Costigan KA, Atella LD, Reusing SP. Maternal psychological distress during pregnancy in relation to child development at age two. Child Development 2006;77(3):573‐87. [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315(7109):629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Eisenberg 1998
- Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Rompay M, et al. Trends in alternative medicine use in the United States, 1990‐1997: results of a follow‐up national survey. JAMA 1998;280(18):1569‐75. [DOI] [PubMed] [Google Scholar]
Ernst 2006
- Ernst E, Pittler M, Wider B. The desktop guide to complementary and alternative medicine: an evidence‐based approach. 2nd Edition. Edinburgh: Mosby, 2006:480. [Google Scholar]
Galantino 2008
- Galantino ML, Galbavy R, Lauren Q. Therapeutic effects of yoga for children: a systematic review of the literature. Pediatric Physical Therapy 2008;20(1):66‐80. [DOI] [PubMed] [Google Scholar]
Gee 2008
- Gee CB, Rhodes JE. A social support and social strain measure for minority adolescent mothers: a confirmatory factor analytic study. Child Care, Health and Development 2008;34(1):87‐97. [DOI] [PubMed] [Google Scholar]
Gennaro 2003
- Gennaro S, Hennessy MD. Psychological and physiological stress: impact on preterm birth. Journal of Obstetric, Gynecologic and Neonatal Nursing 2003;32(5):668‐75. [DOI] [PubMed] [Google Scholar]
Glover 2002
- Glover V, O'Connor TG. Effects of antenatal stress and anxiety: implications for development and psychiatry. British Journal of Psychiatry 2002;180:389‐91. [DOI] [PubMed] [Google Scholar]
Goldenberg 2008
- Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet 2008;371(9606):75‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Goodwin 2007
- Goodwin RD, Keyes K, Simuro N. Mental disorders and nicotine dependence among pregnant women in the United States. Obstetrics & Gynecology 2007;109(4):875‐83. [DOI] [PubMed] [Google Scholar]
Grant 2005
- Grant JA, Rainville P. Hypnosis and meditation: similar experiential changes and shared brain mechanisms. Medical Hypotheses 2005;65(3):625‐6. [DOI] [PubMed] [Google Scholar]
Harbord 2006
- Harbord RM, Egger M, Sterne JA. A modified test for small‐study effects in meta‐analyses of controlled trials with binary endpoints. Statistics in Medicine 2006;25(20):3443‐75. [DOI] [PubMed] [Google Scholar]
Hatmaker 1998
- Hatmaker DD, Kemp VH. Perception of threat and subjective well‐being in low‐risk and high‐risk pregnant women. Journal of Perinatal & Neonatal Nursing 1998;12(2):1‐10. [DOI] [PubMed] [Google Scholar]
Heron 2004
- Heron J, O'Connor TG, Evans J, Golding J, Glover V. The course of anxiety and depression through pregnancy and the postpartum in a community sample. Journal of Affective Disorders 2004;80(1):65‐73. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Huizink 2004
- Huizink AC, Mulder EJ, Robles de Medina PG, Visser GH, Buitelaar JK. Is pregnancy anxiety a distinctive syndrome?. Early Human Development 2004;79(2):81‐91. [DOI] [PubMed] [Google Scholar]
Hurley 2005
- Hurley KM, Caulfield LE, Sacco LM, Costigan KA, Dipietro JA. Psychosocial influences in dietary patterns during pregnancy. Journal of the American Dietetic Association 2005;105(6):963‐6. [DOI] [PubMed] [Google Scholar]
Johnson 2003
- Johnson RC, Slade P. Obstetric complications and anxiety during pregnancy: is there a relationship?. Journal of Psychosomatic Obstetrics and Gynaecology 2003;24(1):1‐14. [DOI] [PubMed] [Google Scholar]
Kowalcek 2003
- Kowalcek I, Huber G, Bieniakiewitz I, Lammers C, Brunk I, Gembruch U. The influence of gestational age on depressive reactions, stress and anxiety of pregnant women and their partners in relation to prenatal diagnosis. Journal of Psychosomatic Obstetrics and Gynaecology 2003;24(4):239‐45. [DOI] [PubMed] [Google Scholar]
Kurki 2000
- Kurki T, Hiilesmaa V, Raitasalo R, Mattila H, Ylikorkala O. Depression and anxiety in early pregnancy and risk for preeclampsia. Obstetrics & Gynecology 2000;95(4):487‐90. [DOI] [PubMed] [Google Scholar]
Lee 2007
- Lee AM, Lam SK, Sze Mun Lau SM, Chong CS, Chui HW, Fong DY. Prevalence, course, and risk factors for antenatal anxiety and depression. Obstetrics & Gynecology 2007;110(5):1102‐12. [DOI] [PubMed] [Google Scholar]
Littleton 2007
- Littleton HL, Breitkopf CR, Berenson AB. Correlates of anxiety symptoms during pregnancy and association with perinatal outcomes: a meta‐analysis. American Journal of Obstetrics and Gynecology 2007;196(5):424‐32. [DOI] [PubMed] [Google Scholar]
Melnyk 2006
- Melnyk BM, Feinstein NF, Alpert‐Gillis L, Fairbanks E, Crean HF, Sinkin RA, et al. Reducing premature infants' length of stay and improving parents' mental health outcomes with the Creating Opportunities for Parent Empowerment (COPE) neonatal intensive care unit program: a randomized, controlled trial. Pediatrics 2006;118(5):e1414‐e1427. [DOI] [PubMed] [Google Scholar]
Milgrom 2008b
- Milgrom J, Gemmill AW, Bilszta JL, Hayes B, Barnett B, Brooks J, et al. Antenatal risk factors for postnatal depression: a large prospective study. Journal of Affective Disorders 2008;108(1‐2):147‐57. [DOI] [PubMed] [Google Scholar]
Montgomery 2000
- Montgomery GH, DuHamel KN, Redd WH. A meta‐analysis of hypnotically induced analgesia: how effective is hypnosis?. International Journal of Clinical and Experimental Hypnosis 2000;48(2):138‐53. [DOI] [PubMed] [Google Scholar]
Moutquin 2003
- Moutquin JM. Socio‐economic and psychosocial factors in the management and prevention of preterm labour. BJOG: an international journal of obstetrics and gynaecology 2003;110 Suppl 20:56‐60. [PubMed] [Google Scholar]
Natural Standard 2008
- Anonymous. Natural Standard: the authority on integrative medicine. http://www.naturalstandard.com/ (accessed 2008) 2008.
NCCAM 2008
- Anonymous. Mind‐body medicine: an overview. National Center for Complementary and Alternative Medicine (http://nccam.nhi.gov/health/backgrounds/mindbody.htm#1) (accessed 2008) 2008.
NLM 2008
- National Library of Medicine. MeSH definitions. PubMed MeSH Datababse (http://www.ncbi.nlm.nih.gov/sites/entrez) (accessed 2008) 2008.
O'Connor 2002a
- O'Connor TG, Heron J, Glover V. Antenatal anxiety predicts child behavioral/emotional problems independently of postnatal depression. Journal of the American Academy of Child and Adolescent Psychiatry 2002;41(12):1470‐7. [DOI] [PubMed] [Google Scholar]
O'Connor 2002b
- O'Connor TG, Heron J, Golding J, Beveridge M, Glover V. Maternal antenatal anxiety and children's behavioural/emotional problems at 4 years. Report from the Avon Longitudinal Study of Parents and Children. British Journal of Psychiatry 2002;180:502‐8. [DOI] [PubMed] [Google Scholar]
Patterson 2003
- Patterson DR, Jensen MP. Hypnosis and clinical pain. Psychological Bulletin 2003;129(4):495‐521. [DOI] [PubMed] [Google Scholar]
RevMan 2011 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.1. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2011.
Shiha 2009
- Shiha M, Yang YH, Malcolm K. A meta‐analysis of hypnosis in the treatment of depressive symptoms: a brief communication. International Journal of Clinical and Experimental Hypnosis 2009;57(4):431‐42. [DOI] [PubMed] [Google Scholar]
Sikkema 2001
- Sikkema JM, Robles de Medina PG, Schaad RR, Mulder EJ, Bruinse HW, Buitelaar JK, et al. Salivary cortisol levels and anxiety are not increased in women destined to develop preeclampsia. Journal of Psychosomatic Research 2001;50(1):45‐9. [DOI] [PubMed] [Google Scholar]
Smith 2006
- Smith AC, Collins TC, Cyna AC, Crowther AC. Complementary and alternative therapies for pain management in labour. Cochrane Database of Systematic Reviews 2006, Issue 4. [DOI: 10.1002/14651858.CD003521.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sosa 2004
- Sosa C, Althabe F, Belizan J, Bergel E. Bed rest in singleton pregnancies for preventing preterm birth. Cochrane Database of Systematic Reviews 2004, Issue 1. [DOI: 10.1002/14651858.CD003581.pub2] [DOI] [PubMed] [Google Scholar]
Spielberger 1983
- Spielberger CD, Gorsuch RL, Lushene RE, Vagg PR, Jacobs GA, Alto CAP. Manual for the state‐trait anxiety inventory. Consulting Psychologists, 1983. [Google Scholar]
Stahl 2003
- Stahl K, Hundley V. Risk and risk assessment in pregnancy ‐ do we scare because we care?. Midwifery 2003;19(4):298‐309. [DOI] [PubMed] [Google Scholar]
Swallow 2004
- Swallow BL, Lindow SW, Masson EA, Hay DM. Psychological health in early pregnancy: relationship with nausea and vomiting. Journal of Obstetrics and Gynaecology 2004;24(1):28‐32. [DOI] [PubMed] [Google Scholar]
Teixeira 2009
- Teixeira C, Figueiredo B, Conde A, Pacheco A, Costa R. Anxiety and depression during pregnancy in women and men. Journal of Affective Disorders 2009;119(1‐3):142‐8. [DOI] [PubMed] [Google Scholar]
Uman 2006
- Uman LS, Chambers CT, McGrath PJ, Kisely S. Psychological interventions for needle‐related procedural pain and distress in children and adolescents. Cochrane Database of Systematic Reviews 2006, Issue 4. [DOI: 10.1002/14651858.CD005179.pub2] [DOI] [PubMed] [Google Scholar]
Upchurch 2006
- Upchurch DM, Chyu L, Greendale GA, Utts J, Bair YA, Zhang G, et al. Complementary and alternative medicine use among American women: findings from The National Health Interview Survey, 2002. Journal of Women's Health 2007;16(1):102‐13. [DOI] [PubMed] [Google Scholar]
Vendittelli 2002
- Vendittelli F, Lachcar P. Threat of premature labor, stress, psychosocial support and psychotherapy: a review of the literature. Gynecologie, Obstetrique & Fertilite 2002;30(6):503‐13. [DOI] [PubMed] [Google Scholar]
Wolsko 2004
- Wolsko PM, Eisenberg DM, Davis RB, Phillips RS. Use of mind‐body medical therapies. Journal of General Internal Medicine 2004;19(1):43‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zelkowitz 2000
- Zelkowitz P, Bardin C, Papageorgiou A. Medical and psychological factors related to parental behavior with very low birthweight infants. Pediatric Research 2000;47:36A. [Google Scholar]
Zelkowitz 2005
- Zelkowitz P, Papageorgiou A. Maternal anxiety: an emerging prognostic factor in neonatology. Acta Paediatrica 2005;94(12):1704‐5. [DOI] [PubMed] [Google Scholar]


