Abstract
Objectives
This study aims to investigate the risk of COVID-19 transmission on aircraft.
Methods
We obtained data on all international flights to Lanzhou, China, from June 1, 2020, to August 1, 2020, through the Gansu Province National Health Information Platform and the official website of the Gansu Provincial Center for Disease Control and Prevention. We then performed the statistical analysis.
Results
Three international flights arrived in Lanzhou. The flights had a total of 700 passengers, of whom 405 (57.9%) were male, and 80 (11.4%) were children under the age of 14 years. Twenty-seven (3.9%) passengers were confirmed to have COVID-19. Confirmed patients were primarily male (17, 65.4%) with a median age of 27.0 years. Most confirmed cases were seated in the middle rows of economy class or near public facility areas such as restrooms and galleys. The prevalence of COVID-19 did not differ between passengers sitting in the window, aisle, or middle seats. However, compared with passengers sitting in the same row up to 2 rows behind a confirmed case, passengers seated in the 2 rows in front of a confirmed case were at a slightly higher risk of being infected.
Conclusions
COVID-19 may be transmitted during a passenger flight, although there is still no direct evidence.
Key Words: Coronavirus Disease 2019 (COVID-19), Aircraft, Transmission, National Health Information Platform
Graphical abstract
Introduction
The transmission routes of SARS-CoV-2, the pathogen of COVID-19, remain still partly unclear (Yang and Duan G, 2020). According to present knowledge (Chinese Thoracic Society and Chinese Association of Chest Physicians, 2021), the main transmission routes of COVID-19 are respiratory droplets from close contacts and aerosols in confined spaces (Rabaan et al., 2021 ; Schijven et al., 2021). However, there is no evidence to exclude the possibility of other routes of transmission, such as gastrointestinal tract transmission (Jiao et al., 2021). In addition, COVID-19 is an emerging infectious disease, and despite the recent vaccination efforts, most of the world's population is still susceptible to infection. As of July 25, 2021, the World Health Organization reports over 194 million cases of COVID-19 causing 4.0 million deaths, which demonstrates the magnitude of the burden of this pandemic (World Health Organization, 2021a).
The global volume of passenger air traffic has rapidly increased over the past years. According to the Statistical Bulletin of Civil Aviation Industry Development, almost 5.0 million passenger flights took off in 2019 in China, an increase of 5.8% compared with 2018 (Civil Aviation Administration of China, 2021a). Although the aviation industry was deeply affected by COVID-19 in 2020, 4.5 million passenger flights were still carried out in 2020 (Civil Aviation Administration of China, 2021b). There have been many outbreaks of airborne diseases, such as tuberculosis, Severe Acute Respiratory Syndrome (SARS), Middle East Respiratory Syndrome (MERS), and Influenza A (H1N1) during flights (Mangili et al., 2016). Pang et al. (Pang et al., 2021) found that the risk of COVID-19 transmission on an aircraft was low, even with infectious persons onboard. Khatib et al. (Khatib et al., 2020) considered that in-flight transmission of SARS-CoV-2 was a real risk. COVID-19 transmission within the aircraft depended on the duration of the flights, contact points, proximity, and movement of passengers. Rosca et al. divided the duration of the flight into short, medium, and long flights, with a low or a high number of secondary cases. The risk of transmission did not necessarily increase with the duration of the flight (Rosca et al., 2021). Hu et al. found that travel time among domestic airplane passengers departing from Wuhan, China, ranged from 1.1 to 4.3 hours. On average, the upper bound of attack rates increased from 0.7% to 1.2% when the co-travel time increased from 2.0 hours to 3.3 hours, whereas the lower bound estimates of attack rates increased from relatively low risk (0.0%) within 1.5 hours to 0.4% for a 3.3 hours co-travel duration. However, there was no significant difference between the estimated upper and lower bounds of attack rates (Hu et al., 2021). The assumption that the risk of transmission increases with the length of flight because of higher exposure needs further investigation. Therefore, we intend to explore the risk of transmission of COVID-19 on aircraft, especially the relation between the risk of transmission and the length of flight, based on the Gansu Province National Health Information Platform.
Methods
Research subjects
We obtained the passenger information data for all international flights to Lanzhou, China, from June 1, 2020, to August 1, 2020, from the Gansu Province National Health Information Platform (Yan et al., 2021). The following variables were extracted for all passengers: age, nationality, gender, native place, flight number, seat number, origin, destination, source city, the duration of the flight, temperature, place of transshipment, nucleic acid test results, the date of entry, the date of diagnosis, the date to release the management of confirmed cases. All passengers were tested for nucleic acid after disembarkation and transferred directly to the hospital if a positive result was found or to the quarantine site in Lanzhou New Area if the result was negative. In most cases, each person was accommodated in a separate quarantine room in cases of passengers who were incapacitated. After arrival, passengers were tested for nucleic acid (once a day) for the first 3 days and on the twelfth and thirteenth days. Additional tests were taken if required by the person's condition. After completing 14 days of quarantine in Lanzhou New Area, the passengers could return to their place of residence for a further 14 days of home quarantine. Nucleic acid testing would be carried out twice during the home quarantine by the local Centers of Disease Control and Prevention staff. During the initial 14-day quarantine period, if symptoms or a positive nucleic acid test result occurred, the person was transferred to a designated hospital (Gansu Provincial Center for Disease Control and Prevention, 2021). The flow chart of the entry process by air is shown in Supplementary Figure 1.
We extracted data on the confirmed COVID-19 cases from the official website of the Gansu Provincial Center for Disease Control and Prevention, including the following variables: age, nationality, gender, clinical classification, and symptom. Case definition of COVID-19 followed the diagnostic criteria in the “Diagnosis and treatment plan for COVID-19 (Version 7)” issued by the National Health Commission of the People's Republic of China (National Health Commission of the People's Republic of China, 2021). A case was confirmed as COVID-19 if it met at least 1 of the following conditions: (1) positivity for SARS-CoV-2 nucleic acid by real-time fluorescence reverse transcription-polymerase chain reaction; (2) viral gene sequencing results that are highly homologous to the known sequences of SARS-CoV-2; or (3) positivity for serum SARS-CoV-2-specific Immunoglobulin M and Immunoglobulin G antibodies, fourfold or more elevation of serum novel coronavirus-specific Immunoglobulin G antibodies from negative to positive, or in the recovery phase compared with the acute phase. We excluded cases that did not meet the previously mentioned criteria. The clinical classification was also based on the “Diagnosis and treatment plan for COVID-19 (Version 7)” (National Health Commission of the People's Republic of China, 2021), with the following 4 stages: (1) Light: the clinical symptoms were mild, and there was no sign of pneumonia on imaging; (2) Ordinary: the patient had a fever, respiratory tract and other symptoms, and imaging signs of pneumonia; (3) Severe: the patient met at least 1 of the following conditions: ① Shortness of breath with a respiratory rate greater than or equal to 30 breaths/min; ② At rest, means oxygen saturation ≤93%; ③ Partial arterial oxygen concentration/inspired oxygen fraction ≤300 mmHg (1 mmHg = 0.133 kPa); and (4) Critical: the patient met at least 1 of the following conditions: ① Respiratory failure, mechanical ventilation was required; ② Shock; ③ Other organ failure needing intensive care unit monitoring.
Statistical analysis
We used IBM SPSS Statistics for Windows, Version 26.0 (Armonk, New York), to conduct statistical analysis. Variables expected to be normally distributed were expressed as means ± standard deviations and other variables as medians with interquartile ranges (IQR). We used Student's t test for normally distributed variables and Mann-Whitney U test for other variables. Categories variables (e.g., SARS-CoV-2 prevalence, gender, and adults/children) were expressed by rate or composition ratio, and differences between rate or composition ratio were analyzed using Chi-square test or, when not applicable, Fisher's exact probability method. We were unable to distinguish between index cases and secondary cases because the chain of transmission of cases could not be traced. Therefore, the primary outcome indicator was the period prevalence, that is, the number of confirmed cases on a particular flight during the observation period of 14 days divided by the number of all passengers of the same flight.
The World Health Organization declared that passengers seated in the same row or a maximum of 2 rows in front or behind and in the same block (i.e., no aisle in between) of each confirmed patient were considered close contacts (World Health Organization, 2009b). Therefore, to explore the possible transmission risk on the aircraft, we performed an analysis where we divided the seats near each confirmed case into 3 groups: the 2 rows in front, the same row, and the 2 rows behind the case. We considered only seats within the same block, that is, seats not separated by an aisle from the index patient, and calculated the prevalence at each 3-row group (excluding the index patient). We performed this analysis for each confirmed case as an index patient separately and then calculated the overall prevalence of the 3-row groups for each flight (Supplementary Figure 2). To explore the period prevalence of passengers in different seating positions, we divided the seats on the aircraft into 3 categories, namely window seats, middle seats, and aisle seats, and calculated the prevalence for each of these categories. In all prevalence calculations, empty seats were excluded from the denominator.
Results
Three international flights arrived in Lanzhou City, Gansu Province, China, from June 2020 to August 2020: flight MU7792 from Riyadh, flight MU7790 from Jeddah, and flight CA608 from Moscow, including a total of 700 passengers, of whom 27 were confirmed to have COVID-19. We were able to extract the details of all except 1 confirmed case. After treatment, all 27 confirmed cases with the information available were eventually cured and discharged without a single death. Details are listed in Table 1 .
Table 1.
Summary of basic characteristics of 3 flights.
| Flight No. | Date of Flight | Origin | Destination | Duration of the flight (hour) | Total passengers |
Male [N (%)] | Confirmed cases [N (%)] | Children* |
||
|---|---|---|---|---|---|---|---|---|---|---|
| N | M(IQR) | N (%) | M(IQR) | |||||||
| 1 | Jun.15,2020 | Riyadh | Lanzhou | 9 | 253 | 31(24.0-37.0) | 152(60.1%) | 20(7.9%) | 41(16.2%) | 4(2.0-6.0) |
| 2 | Jun.23,2020 | Jeddah | Lanzhou | 9 | 254 | 28(22.0-37.0) | 169(66.5%) | 4(1.6%) | 37(14.6%) | 4(3.0-7.0) |
| 3 | Jul.4,2020 | Moscow | Lanzhou | 7 | 193 | 23(21.0-25.0) | 84(43.5%) | 3(1.6%) | 2(1.0%) | 6(5.5-6.5) |
The age of a child is defined as being under the age of 14 years.
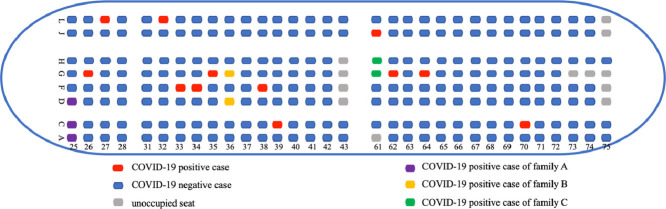
Flight 1
On June 15, 2020, 253 Chinese passengers entered from Riyadh, Saudi Arabia, to Lanzhou, China. The duration of the flight was 9 hours. Of the passengers, 152 (60.1%) were male; 41 (16.2%) were children under the age of 14 years; and the median age was 31 years (IQR, 24.0-37.0). A total of 20 passengers were intermittently diagnosed to be infected with SARS-CoV-2, but for 1 of the cases, detailed information could not be obtained. The seating positions of all passengers are shown in Figure 1 . There were 3 family clusters of infection, meaning confirmed cases from the same household seated close together. Aside from this, most of the confirmed patients were located in the middle: there were 3 confirmed cases in rows 35 and 36, and 4 cases in rows 61 and 62. The remaining confirmed patients were scattered in rows 26, 27, 32, 33, 34, 38, 39, 64, and 70. The prevalence rates were 4.8% (95% confidence interval [CI] [0.7%, 10.3%]) among passengers seated in the window seats (seats with suffixes A and L), 15.5% (95% CI [5.9%, 25.1%]) in the middle seats (seats with suffixes F and G), and 5.6% (95% CI [1.5%, 9.8%]) in the aisle seats (seats with suffixes C, D, H and J) (P=0.054). The prevalence rates were 16.7% (95% CI [9.5%, 27.2%]) in the 2 rows in front each confirmed case, 14.0% (95% CI [5.8%, 28.6%]) in the same row as a confirmed case, and 10.7% (95% CI [6.0%, 17.9%]) in the 2 rows behind each confirmed case (P=0.465).
Figure 1.
Passenger seating diagram on Flight 1.
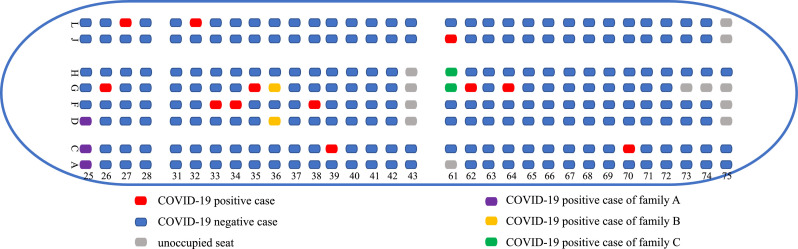
Flight 2
On June 23, 2020, a plane with 254 passengers flew from Jeddah, Saudi Arabia, to Lanzhou, China. The duration of the flight was 9 hours. The median age of passengers was 28 years (IQR, 22.0-37.0), most (n=169, 66.5%) were male, and 37 (14.6%) passengers were children below age 14. There were 4 confirmed cases, all from different households. The prevalence in the window seats (seats with suffixes A and L) was 0, in the middle seats (seats with suffixes F and G) 3.4% (95% CI [1.4%, 8.1%]), and the in the aisle seats (seats with suffixes C, D, H, and J) 1.6% (95% CI [0.6%, 3.8%]) (P=0.268). In the 2 rows in front of each confirmed case, the prevalence was 4.5% (95% CI [0.2%, 24.9%]), in the same row 0, and in the 2 rows behind 4.2% (95% CI [0.2%, 23.1%]) (P=1.000).
Flight 3
On July 4, 2020, 193 passengers arrived on the flight from Moscow, Russia, to Lanzhou, China. The duration of the flight was 7 hours. A total of 84 (43.5%) passengers were male, and the median age was 23 years (IQR, 21.0-25.0). Two (1.0%) were children below age 14. There were 3 confirmed cases, all from separate households. The prevalence rates were 2.3% (95% CI [2.3%, 6.9%]) in the window seats (seats with suffixes A and L), 1.6% (95% CI [1.6%, 4.8%]) in the middle group (seats with suffixes B, E, and K), and 1.1% (95% CI [1.1%, 3.4%]) in the aisle group (seats with suffixes C, D, H, and J) (P=1.000). There were no other confirmed cases around the seats of the 3 confirmed patients.
Characteristics of confirmed cases
The 26 confirmed cases with full data available had a median age of 27.0 years, and most (n=17, 65.4%) were male (Table 2 ). The symptoms of patients were mild, and the main symptoms were throat discomfort (n=12, 46.2%), followed by fatigue (n=6, 23.1%), low fever (n=5, 19.2%), and cough (n=5, 19.2%). Some uncommon symptoms, such as high fever, nasal congestion, runny nose, and headache, were also observed. Twelve patients (46.2%) had no fever, and 5 patients (19.2%) were asymptomatic. Fourteen cases were classified as light and 12 cases as ordinary.
Table 2.
Summary of the details of individual cases in a flight-associated outbreak of COVID-19.
| Number | Flight | Gender | Age (year) | Clinical Classification | Symptom | Family Cluster | Seat Number | Source City | Time from the Date of Entry to the Date of Diagnosis (day) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 1 | Male | 4 | Light | a | A | 25C | Riyadh, Saudi Arabia | 1 |
| 2 | Female | 5 | Light | b | C | 61G | Riyadh, Saudi Arabia | 7 | |
| 3 | Female | 8 | Light | d | B | 36G | Riyadh, Saudi Arabia | 2 | |
| 4 | Female | 9 | Light | a | A | 25D | Riyadh, Saudi Arabia | 1 | |
| 5 | Male | 24 | Ordinary | a e f | / | 64G | Riyadh, Saudi Arabia | 7 | |
| 6 | Male | 24 | Ordinary | b f | / | 70C | Riyadh, Saudi Arabia | 1 | |
| 7 | Male | 25 | Ordinary | a g h | / | 34F | Riyadh, Saudi Arabia | 1 | |
| 8 | Male | 27 | Light | b e | / | 27L | Riyadh, Saudi Arabia | 1 | |
| 9 | Male | 27 | Ordinary | b f | / | 35G | Riyadh, Saudi Arabia | 7 | |
| 10 | Male | 28 | Ordinary | i | / | 62G | Riyadh, Saudi Arabia | 1 | |
| 11 | Male | 29 | Light | b | / | 33F | Riyadh, Saudi Arabia | 7 | |
| 12 | Male | 29 | Ordinary | a | / | 38F | Riyadh, Saudi Arabia | 7 | |
| 13 | Female | 31 | Light | d | C | 61H | Riyadh, Saudi Arabia | 7 | |
| 14 | Male | 32 | Ordinary | c e | / | 39C | Riyadh, Saudi Arabia | 13 | |
| 15 | Female | 36 | Ordinary | a e | A | 25A | Riyadh, Saudi Arabia | 1 | |
| 16 | Female | 37 | Ordinary | a | B | 36D | Riyadh, Saudi Arabia | 1 | |
| 17 | Female | 39 | Ordinary | a | / | 26G | Riyadh, Saudi Arabia | 1 | |
| 18 | Male | 51 | Ordinary | a e | / | 61J | Riyadh, Saudi Arabia | 1 | |
| 19 | Female | 52 | Ordinary | c | / | 32L | Riyadh, Saudi Arabia | 7 | |
| 20 | 2 | Male | 23 | Light | d e | / | 33G | Jeddah, Saudi Arabia | 3 |
| 21 | Male | 26 | Light | e | / | 35F | Jeddah, Saudi Arabia | 3 | |
| 22 | Male | 34 | Light | d e | / | 32J | Jeddah, Saudi Arabia | 3 | |
| 23 | Male | 49 | Light | d e | / | 35C | Jeddah, Saudi Arabia | 3 | |
| 24 | 3 | Male | 18 | Light | a e f | / | 51E | Moscow, Russia | 0 |
| 25 | Female | 19 | Light | a d e | / | 39J | Moscow, Russia | 0 | |
| 26 | Male | 22 | Light | a e f | / | 43L | Moscow, Russia | 0 |
Notes: a. Body temperature is less than 37.3°C; b. Body temperature is between 37.3°C and 37.9°C; c. Body temperature is greater than or equal to 38°C; d. Fatigue; e. Throat discomfort; f. Cough; g. Stuffed nose; h. Runny nose; i. Headache; /: No report.
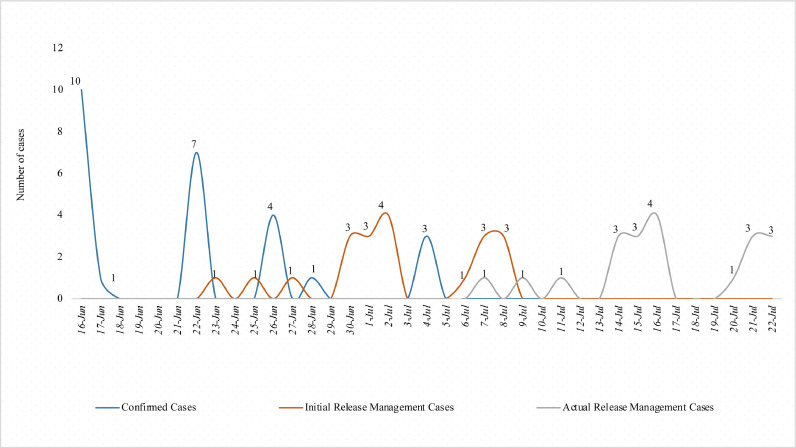
Most of the confirmed cases were seated in the middle of the economy class, and they were in the wing position (rows 32-35). Enclosed public facility areas were the focus areas of infection, such as rows 61 and 62 of Flight 1 (close to the restroom). Furthermore, there were 3 family clusters. The median interval time between the date of arrival in Lanzhou, China, and the date of diagnosis was 1.5 days (IQR, 1.0-7.0). The median interval between the beginning date of physical release management (ending hospital isolation management) and the date of diagnosis was 12.5 days (IQR, 6.5-15.0), and the median interval time from the formal deisolation management (ending home isolation management) to the date of diagnosis was 26.5 days (IQR, 20.5-29.0). The distribution of the time to release the management of confirmed cases is shown in Figure 2 . The information about the management of 6 patients was missing.
Figure 2.
Numbers of COVID-19 cases over time.
Discussion
As far as we know, this is the first comprehensive analysis of aircraft seats during the outbreak of COVID-19. We found that most of the confirmed cases were in the middle of the economy class, around the wing position of the aircraft. Infections were also clustered around restrooms, galleys, and other public facilities, such as rows 61 and 62 of Flight 1. The prevalence did not seem to differ between window, middle, and aisle seats. The prevalence was higher for passengers seated in the 2 rows in front of the confirmed case than those seated in the same row or 2 rows behind.
Aircraft and transmission
Most of the studies so far have shown that the main routes of transmission of COVID-19 are respiratory droplets, aerosols, and close contact transmission (Expert Group on Prevention and Control of Coronavirus Disease 2019 Chinese Preventive Medicine Association, 2020 ; Pombal et al., 2020 ; Sommerstein et al., 2020). The risk of respiratory transmission is heightened when people move around each other, especially in cases when they are in frequent contact with other people, such as in public transport. However, some studies have claimed that on airplanes, the air quality of the cabin is good (Walkinshaw et al., 2020), and the risk of transmitting respiratory viruses on the aircraft is extremely low (Pombal et al., 2020 ; Mangili and Gendreau, 2005). Studies show that SARS (Olsen et al., 2003), H1N1 (Kim et al., 2010 ; Baker et al., 2010), MERS (Regan et al., 2016 ; Gardner et al., 2016), and other respiratory viruses have been spread during flights. The basic reproduction number (R0) of SARS-CoV-2 has been estimated to be between 1.8 and 3.6, which is higher than that of SARS, MERS, and influenza viruses. This indicates that COVID-19 seemed more likely to cause transmission (Petersen et al., 2020).
In the 3 flights of our study, 7.5%, 1.6%, and 1.5% of the patients were found to be infected, respectively. In other studies, Chen et al. (Chen et al., 2020a) found the prevalence of 4.8% among passengers of a flight from Singapore to Hangzhou, China, and Fan et al. (Fan et al., 2020) found a prevalence of 11.9% among 311 Chinese located overseas evacuated from Iran to Gansu Province, China. Khanh et al. (Khanh et al., 2020) found a 7.4% prevalence of COVID-19 on a direct flight from London, the United Kingdom, to Hanoi, Vietnam. In our study, the prevalence of COVID-19 was lower. There may be several reasons: (1) The incidence of COVID-19 in the original location (Saudi Arabia and Russia) at the time of the flight was not high. In Saudi Arabia, the number of new confirmed cases was 121.5 per 100,000 over 14 days on June 15, 2020, and 160.1 per 100,000 over 14 days on June 23, 2020. In the Russian Federation, the number of new confirmed cases was 66.7 per 100,000 over 14 days on July 4, 2020; (2) In the flights included in our study, passengers were required to wear masks during the flight (Chu et al., 2020); (3) The destination of the flight was Lanzhou, China. Since February 18, 2020, there have been no new confirmed cases of indigenous COVID-19 in Gansu Province, located in northwest China, and has positively managed to control the epidemic; (4) The strictness of the quarantine could have an impact on the prevention and control of diseases. The passengers of all 3 flights were Chinese nationals who were repatriated by flights chartered by the Chinese government and were not screened for symptoms or nucleic acid before boarding. However, the higher prevalence in Flight 1 may be the high number of family clusters in Flight 1. Regarding the duration of the flight, Flight 1 and Flight 2 were both 9 hours. The country of departure was Saudi Arabia. Their total passengers were almost the same (253 vs 254). The epidemic situation of Flight 2 was even more critical than the epidemic situation of Flight 1. However, Flight 1 had a higher prevalence rate than Flight 2 (7.5% vs 1.6%). Therefore, we presume that there was (were) the index case(s) on Flight 1, which caused the spread of the disease. The high number of family clusters has exacerbated the rapid spread of the disease. This could provide indirect evidence that the transmission of COVID-19 occurred during Flight 1.
Seating and transmission
This study found no evidence of an association between the prevalence of infection and being seated on the window, aisle, or middle seats. This agrees with the results of Foxwell et al. (Foxwell et al., 2011). However, both Flight 1 and Flight 2 showed that the period prevalence rate of passengers seated in the middle was relatively high, whereas Foxwell et al. found that the risk of infection in the aisle location was higher through the investigation of the spread of H1N1 on international flights in May 2009 (Foxwell et al., 2011). There are several possible reasons for the different results. In the flights of our study, most of the family clusters appear in the middle position (such as family B and family C in Flight 1); the middle seats are densely distributed, which may increase the risk of infection (4 seats side-by-side in the middle seats of Flights 1 and 2); and the location close to the aisle has more chances of contact with passengers, so the risk of infection may be higher. In addition, it may also be related to the infectivity of different viruses, aircraft types, and protective measures for passengers.
We also found that public facility areas, such as restrooms and galleys, were focal areas of infection. For example, rows 61 and 62 near restrooms in Flight 1 showed a relatively high number of cases, which was consistent with the findings of Chen et al. (Chen et al., 2020a). In addition, infected individuals were also common in the seats around the position of the wings, such as rows 32 to 35 in Flight 1, which may be related to the operation of the aircraft engine, air filtration system, or conditioning system, but there is no evidence for this so far. We further explored the differences in the prevalence of infection of sitting in the 2 rows in front, the same row, and 2 rows behind a confirmed case. The results showed that the prevalence of infection was higher for passengers seated 2 rows in front. This can probably be explained by cabin air entering from the top and exiting the cabin near the floor. In addition, air enters and leaves the cabin mainly in or near the same row of seats, with a low probability of flow in the front and rear rows (Pombal et al., 2020). However, when people move around in the cabin, the airflow changes accordingly. The airflow in the cabin can also have different effects based on the navigation route of the aircraft, especially in nonsmooth conditions such as take-off, landing, and turbulence. Therefore, we suggest recording the flight process in detail to provide a basis for research on transmission dynamics.
Symptoms
Most studies showed that fever, cough, and fatigue were the main symptoms of COVID-19 (Zhang et al., 2020 ; Chen et al., 2020b). The main symptoms of SARS were fever, cough, and shortness of breath in flight (Vogt et al., 2006); whereas, for H1N1, they were cough, fever, headache, runny nose, and diarrhea (Foxwell et al., 2011 ; Baker et al., 2010). It was known that asymptomatic SARS-CoV-2-infected individuals could transmit the virus, and nucleic acid detection of patients is essential. Our study showed that symptoms were mild, with only 19.2% of patients with COVID-19 presenting a low fever. However, 46.2% of patients had a body temperature below 37.7°C, and a few patients had no symptoms despite having positive nucleic acid test results. For COVID-19 transmission in asymptomatic infected individuals in flight, Bae et al. (Bae et al., 2020) suggested that temperature testing and symptom screening alone before air travel will not completely block the possibility of coronavirus transmission. We recommended that passengers should be tested for nucleic acid before a flight. Testing could be offered before take-off to reduce the likelihood of cross-infection by passengers.
Limitations and Strengths
Our study has several advantages. First, the data were obtained from the National Health Information Platform of Gansu Province, and we conducted a comprehensive analysis of the seating arrangements during the flight, which is the first study to do this. Second, we analyzed some potential factors related to transmission risk and conditions of COVID-19 in flight to provide a scientific basis for mitigating the risk of infectious disease transmission during transportation.
Our study also has some limitations. First, we were unable to obtain information on passengers’ activities before and during the flight, including whether they had contact with suspected or confirmed patients; whether they drank, ate, or talked (Wang et al., 2022) during the flight; whether they used the restroom; or whether they wore masks all times during the flight. Second, we conducted the relevant analysis through retrospective data collection, so no surface swab sampling, molecular tests, or air sampling were performed in the aircraft cabins or passenger seats. Thus, there is no direct evidence that transmission occurred during the flight. Third, the data on flights were so limited that it was impossible to analyze the relation between the risk of transmission and the length of flight. Our next step will be to collect more data to conduct the relevant analysis. Finally, it was not possible to interview the passengers concerned to determine whether they were index cases, so we were unable to distinguish between index cases and secondary cases because the chain of transmission of cases could not be traced. The passengers who became positive for COVID-19 during the quarantine period could be in the incubation period and got the infection in their country of departure or may have been infected by the COVID-19 positive cases in the aircraft, which was also the problem with previous studies (Yang et al., 2020 ; Chen et al., 2020 ; Khanh et al., 2020). Therefore, the main indicator we used, the period prevalence, can only give insights about the risk of transmission but not confirm whether onward transmission happened during the flight.
Suggestions
According to the results, we make the following suggestions for flights during a pandemic: (1) Before taking flight, passengers must provide a certificate of a negative nucleic acid test result or a vaccination or a recovery certificate and do not have symptoms, to further avoid the risk of the spread of infectious diseases on the plane; (2) Airlines should try not to arrange seats near public facilities, and at least 1 empty seat should be left between groups if possible; (3) Passengers should minimize their activities before and during the flight, and always take protective measures such as wearing masks (especially those near to public facilities or in the middle positions). In addition, it is recommended to adopt this scheme for epidemic prevention and control in other confined spaces such as movie theaters, restaurants, and other public vehicles such as buses, trains, and metros.
Conclusion
In conclusion, this study can provide indirect evidence of SARS-CoV-2 transmission occurring during a flight, and explore the relation between passengers’ seats and prevalence in detail. There are few evidence-based guidelines for COVID-19 air travel, so it is recommended to conduct more relevant studies (especially performing the molecular tests or genomic sequencing for environmental samples of airplanes or passenger seats) and develop reasonable and feasible health policies or guidelines to reduce the risk of the spread of COVID-19 and other airborne infectious diseases on airplanes in the pandemic and to respond to future pandemics.
Conflict of Interest Disclosures
There are no conflicts of interest to declare.
Acknowledgments
Funding
This study was supported by the 2021 Gansu Provincial Health Industry Research Project, called “Research on the Application of Evidence-based Health Decision-making Based on Big Data - the Practice of Precise Control of Inbound Persons under the Background of Epidemic Normalization” (grant number GSWSKY2021-046 to the Health Commission of Gansu Province). The project aimed to develop the scientific, efficient, and rapid mechanism for the centralized isolation and screening of inbound personnel and related systems and processes based on data from multiple departments such as health, customs, and airlines and guided by the principles and methods of evidence-based decision-making. However, it did not affect the design, data collection, analysis, interpretation, and writing of this study.
Acknowledgments
Not applicable.
Authors’ contributions
QG and JW contributed equally to this work. QG, JW, XY, YC designed the study. XY and JY collected the data. QG, HL, JZ, and SW analyzed the data. QG and JW contributed to writing and editing. QG, JW, JE, and YC contributed to modifying and reviewing. All authors have read and approved the manuscript.
Ethical consideration
Our data were obtained with the consent of the Health Commission of Gansu Province. To protect privacy, no personal information of the passengers involved was disclosed to the researchers.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ijid.2022.03.024.
Appendix. Supplementary materials
References
- Bae S H, Shin H, Koo H Y, Lee SW, Yang JM, Yon DK. Asymptomatic transmission of SARS-CoV-2 on evacuation flight. Emerging infectious diseases, 2020, 26(11): 2705-2708. doi: 10.3201/eid2611.203353. [DOI] [PMC free article] [PubMed]
- Baker M G, Thornley C N, Mills C, Roberts S, Perera S, Peters J, et al. Transmission of pandemic A/H1N1 2009 influenza on passenger aircraft: retrospective cohort study. BMJ. 2010:340. doi: 10.1136/bmj.c2424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J, He H, Cheng W, Liu Y, Sun Z, Chai C, et al. Potential transmission of SARS-CoV-2 on a flight from Singapore to Hangzhou, China: an epidemiological investigation. Travel medicine and infectious disease, 2020a, 36: 101816. doi: 10.1016/j.tmaid.2020.101816. [DOI] [PMC free article] [PubMed]
- Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. The Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinese Thoracic Society Chinese Association of Chest Physicians. Guidelines for the diagnosis, treatment and prevention and control of Coronavirus Disease 2019 in Chinese adults. National Medical Journal of China. 2021;101(18):1293–1356. doi: 10.3760/cma.j.cn112137-20210112-00090. [DOI] [Google Scholar]
- Chu D K, Akl E A, Duda S, Solo K, Yaacoub S, Schünemann HJ, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. The Lancet. 2020;395(10242):1973–1987. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Civil Aviation Administration of China. Statistical bulletin on the development of the civil aviation industry in 2019. [cited 2021 Jul 29]. http://www.caac.gov.cn/XXGK/XXGK/TJSJ/202006/P020200605630677965649.pdf.
- Civil Aviation Administration of China. China Civil Aviation December 2020 Key Production Indicators Statistics. [cited 2021 Jul 29]. http://www.caac.gov.cn/XXGK/XXGK/TJSJ/202102/P020210220503535940242.pdf.
- Expert Group on Prevention and Control of Coronavirus Disease 2019 Chinese Preventive Medicine Association An update on the epidemiological characteristics of novel coronavirus pneumonia (COVID-19) Chinese Journal of Epidemiology. 2020;41(2):139–144. doi: 10.3760/cma.j.issn.0254-6450.2020.02.002. [DOI] [PubMed] [Google Scholar]
- Fan J, Liu X, Shao G, Qi J, Li Y, Pan W, et al. The epidemiology of reverse transmission of COVID-19 in Gansu Province, China. Travel medicine and infectious disease, 2020, 37: 101741. doi: 10.1016/j.tmaid.2020.101741. [DOI] [PMC free article] [PubMed]
- Foxwell A R, Roberts L, Lokuge K, Kelly P M. Transmission of influenza on international flights, May 2009. Emerging infectious diseases. 2011;17(7):1188–1194. doi: 10.3201/eid1707.101135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gansu Provincial Centre for Disease Control and Prevention. Closed-loop management of epidemic prevention for people entering Gansu from abroad "a clear picture". [cited 2021 Jul 29]. http://www.gscdc.net/index.php?s=news&c=show&id=1775.
- Gardner L M, Chughtai A A, MacIntyre C R. Risk of global spread of Middle East respiratory syndrome coronavirus (MERS-CoV) via the air transport network. Journal of travel medicine. 2016;23(6):taw063. doi: 10.1093/jtm/taw063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu M, Wang J, Lin H, Ruktanonchai CW, Xu C, Meng B, et al. Risk of SARS-CoV-2 Transmission among Air Passengers in China. Clinical infectious diseases. 2021:ciab836. doi: 10.1093/cid/ciab836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiao L, Li H, Xu J, Yang M, Ma C, Li J, et al. The gastrointestinal tract is an alternative route for SARS-CoV-2 infection in a nonhuman primate model. Gastroenterology. 2021;160(5):1647–1661. doi: 10.1053/j.gastro.2020.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khanh N C, Thai P Q, Quach H L, Thi N A H, Dinh P C, Duong T N, et al. Transmission of SARS-CoV 2 during long-haul flight. Emerging infectious diseases, 2020, 26(11): 2617-2624. doi: 10.3201/eid2611.203299. [DOI] [PMC free article] [PubMed]
- Khatib AN, Carvalho AM, Primavesi R, To K, Poirier V. Navigating the risks of flying during COVID-19: a review for safe air travel. Journal of travel medicine. 2020;27(8):taaa212. doi: 10.1093/jtm/taaa212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J H, Lee D H, Shin S S, Kang C, Kim J S, Jun B Y, et al. In-flight transmission of novel influenza A (H1N1) Epidemiology and health. 2010:32. doi: 10.4178/epih/e2010006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mangili A, Gendreau M A. Transmission of infectious diseases during commercial air travel. The Lancet. 2005;365(9463):989–996. doi: 10.1016/S0140-6736(05)71089-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mangili A, Vindenes T, Gendreau M. Infectious risks of air travel. Infections of Leisure. 2016:333–344. doi: 10.1128/9781555819231.ch17. [DOI] [PubMed] [Google Scholar]
- National Health Commission of the People's Republic of China. Diagnosis and treatment plan for COVID-19 (Version 7). [cited 2021 Jul 29]. http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989/files/ce3e6945832a438eaae415350a8ce964.pdf.
- Olsen S J, Chang H L, Cheung T Y Y, Tang A F Y, Fisk T L, Ooi S P L, et al. Transmission of the severe acute respiratory syndrome on aircraft. New England Journal of Medicine. 2003;349(25):2416–2422. doi: 10.1056/NEJMoa031349. [DOI] [PubMed] [Google Scholar]
- Pang JK, Jones SP, Waite LL, Olson NA, Armstrong JW, Atmur RJ, et al. Probability and estimated risk of SARS-CoV-2 transmission in the air travel system. Travel medicine and infectious disease, 2021, 43: 102133. doi: 10.1016/j.tmaid.2021.102133. [DOI] [PMC free article] [PubMed]
- Petersen E, Koopmans M, Go U, Hamer DH, Petrosillo N, Castelli F, et al. Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics. The Lancet infectious diseases. 2020 doi: 10.1016/S1473-3099(20)30484-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pombal R, Hosegood I, Powell D. Risk of COVID-19 during air travel. JAMA. 2020;324(17):1798. doi: 10.1001/jama.2020.19108. [DOI] [PubMed] [Google Scholar]
- Rabaan A A, Al-Ahmed S H, Al-Malkey M K, Alsubki R, Ezzikouri S, Al-Hababi FH, et al. Airborne transmission of SARS-CoV-2 is the dominant route of transmission: droplets and aerosols. Infez Med. 2021;29:10–19. https://infezmed.it/media/journal/Vol_29_1_2021_2.pdf [PubMed] [Google Scholar]
- Regan J J, Jungerman M R, Lippold S A, Washburn F, Roland E, Objio T, et al. Tracing airline travelers for a public health investigation: Middle East respiratory syndrome coronavirus (MERS-CoV) infection in the United States, 2014. Public Health Reports. 2016;131(4):552–559. doi: 10.1177/0033354916662213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosca EC, Heneghan C, Spencer EA, Brassey J, Plüddemann A, Onakpoya IJ, et al. Transmission of SARS-CoV-2 associated with aircraft travel: a systematic review. Journal of travel medicine. 2021;28(7):taab133. doi: 10.1093/jtm/taab133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schijven J, Vermeulen L C, Swart A, Meijer A, Duizer E, de Roda Husman AM. Quantitative microbial risk assessment for airborne transmission of SARS-CoV-2 via breathing, speaking, singing, coughing, and sneezing. Environmental health perspectives. 2021;129(4) doi: 10.1289/EHP7886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sommerstein R, Fux C A, Vuichard-Gysin D, Abbas M, Marschall J, Balmelli C, et al. Risk of SARS-CoV-2 transmission by aerosols, the rational use of masks, and protection of healthcare workers from COVID-19. Antimicrobial Resistance & Infection Control. 2020;9(1):1–8. doi: 10.1186/s13756-020-00763-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogt T M, Guerra M A, Flagg E W, Ksiazek TG, Lowther SA. Arguin PM. Risk of severe acute respiratory syndrome–associated coronavirus transmission aboard commercial aircraft. Journal of travel medicine. 2006;13(5):268–272. doi: 10.1111/j.1708-8305.2006.00048.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walkinshaw D S, ENG P. A Brief Introduction To Passenger Aircraft Cabin Air Quality. Ashrae Journal. 2020:12–16. https://indoorair.ca/echo/pdf/Brief_Intro_To_Passenger_Aircraft_Cabin_Air_Quality-Walkinshaw-web.pdf [Google Scholar]
- Wang W, Wang F, Lai D, Chen Q. Evaluation of SARS-COV-2 transmission and infection in airliner cabins. Indoor Air. 2022;32(1):e12979. doi: 10.1111/ina.12979. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Weekly epidemiological update on COVID-19 - 27 July 2021a. [cited 2021 Jul 29]. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---27-july-2021.
- World Health Organization . The Organization; Geneva: 2009. World Health Organization WHO technical advice for case management of influenza A (H1N1) in air transport. [Google Scholar]
- Yan X, Wang J, Yao J, Estill J, Wu S, Lu J, et al. A cross-sectional study of the epidemic situation on COVID-19 in Gansu Province, China - a big data analysis of the national health information platform. BMC Infectious diseases. 2021;21(1):1–7. doi: 10.1186/s12879-020-05743-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang H, Duan G. Analysis on the epidemic factors for COVID-19. Chinese Journal of Preventive Medicine. 2020;54(6):608–613. doi: 10.3760/cma.j.cn112150-20200227-00196. [DOI] [PubMed] [Google Scholar]
- Yang N, Shen Y, Shi C, Ma AHY, Zhang X, Jian X, et al. In-flight transmission cluster of COVID-19: a retrospective case series. Infectious diseases. 2020, 52(12):891-901. doi: 10.1080/23744235.2020.1800814. [DOI] [PubMed]
- Zhang J, Dong X, Cao Y, Yuan Y, Yang Y, Yan Y, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan. China. Allergy. 2020;75(7):1730–1741. doi: 10.1111/all.14238. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.