Abstract
Introduction
Current evidence suggests annual training in the management of shoulder dystocia is adequate. The aim of this trial is to test our hypothesis that skills start to decline at 6 months after training and further decline at 12 months.
Methods
In this randomised, single-blinded study, 13 obstetricians and 51 midwives were randomly assigned to attend a 1-hour mixed lecture and simulation session on shoulder dystocia management. Training was conducted on group 2 at month ‘0’ and on group 1 at month ‘6’. Their knowledge scores (primary outcome) were assessed before (pre-training), immediately after the training (at-training) and retested at month ‘12’ (post-training).
Results
Two-way repeated-measures analysis of variance showed a statistically significant interaction between the testing time frame (pre-training, at-training and post-training) on the score (p<0.001), but no significant interaction between the groups on the score (p=0.458).
Compared to pre-training, the score increased after the simulation training (at-training) in both group 1 (8.69 vs 14.34, p<0.001) and group 2 (9.53 vs 14.66, p< 0.001), but decreased at 6 months post- training in group 1 (14.34 vs 11.71, p<0.001) and at 12 months post-training in group 2 (14.66 vs 11.96, p< 0.001). However the score was better than before the training. There was no significant difference in the post –training score (11.71vs 11.96, p=0.684) between both groups.
Conclusions
Our study demonstrated that simulation training results in short-term and long-term improvement in shoulder dystocia management however knowledge degrades over time. Ongoing training is suggested at a minimum of 12 months’ interval for all members of the obstetrics team including midwives and doctors.
Keywords: shouder dystocia, simulation training, Obstetrics
Introduction
Shoulder dystocia is a relatively uncommon but serious obstetrics emergency (0.2%–3% of all deliveries1). This could lead to severe morbidity and mortality to the delivering fetus. Ideally, training of shoulder dystocia management is best through regular real-life encounters; however, due to its infrequent occurrence, real-life training is virtually impossible.2 Simulation training provides opportunities to rehearse and learn from mistakes without risk to patients and resemble to reality as close as possible. Draycott et al3 showed simulation training improves management and neonatal outcomes of births complicated by shoulder dystocia,3–5 while Deering et al6 and Crofts et al7 demonstrated better utilisation of manoeuvres in a timely and correct fashion after using birth simulators as training tools. Multiple studies also showed similar8 9 and other significant benefits such as leadership skills during emergency situations,10 enhanced overall team performance11 12 and increased comfort in managing uncommon events.13 The overall consensus is that regular simulation training, in particular using birth simulator, is the preferred form of training in shoulder dystocia management. Despite the clear benefits of simulation training, knowledge does decline overtime, and regular formal educational activities should be carried out to reinforce knowledge.14
According to the Confidential Enquiries into Maternal Deaths15 and Confidential Enquiries into Stillbirths and Deaths in Infancy,16 substandard care was found to be a major contributor to fetal and neonatal mortality in the labour ward settings. Training for obstetrics emergency is vital to acquire and maintain clinical standards. In England, the Clinical Negligence Scheme of Trusts16 mandated the annual drilling of all obstetrics and midwifery staff in obstetrics emergencies including shoulder dystocia. Meanwhile Crofts et al17 suggested that annual training seems adequate for those who are already proficient before training, but more frequent rehearsals are advisable for those who show insufficient competency initially until they acquire sufficient skill. In Hong Kong, there is no mandatory time frame for regular shoulder dystocia training. At Queen Elizabeth Hospital, taking into account staffing issues and the need to maintain regular hospital service, we conduct shoulder dystocia simulation training at approximately 12–18 months’ intervals.
While most studies suggested annual training is adequate to maintain skills for management of shoulder dystocia, we hypothesised that skills start to decline as early as 6 months after the training and then decline further 12 months after the training. The aim of this trial was to determine whether there was any difference in the level of skill retention between 6 and 12 months after simulation training.
Methods
This was a randomised, controlled, single-blind study on staffs’ ability to deliver a simulated baby encountering a shoulder dystocia scenario. All participants were obstetricians and midwives from Queen Elizabeth Hospital, Hong Kong, who had received their last training more than 12 months ago. Participants were randomly divided into two similar-sized groups.
Interventional group’s (group 1) training was performed at month 6. Their initial abilities were evaluated before the training, immediately after the training and at month 12. Control group’s (group 2) training was performed at month 0. Their initial abilities were evaluated before the training, immediately after the training and also at month 12.
This study was conducted inside the simulation centre of our hospital and was approved by the Kowloon Central/Kowloon East Research and Ethics Committee, Hospital Authority, Hong Kong (Ref number: KC/KE-14-0081/ER-2).
Participants
All midwives and doctors from the Department of Obstetrics and Gynaecology at Queen Elizabeth Hospital, Hong Kong, were invited to participate in shoulder dystocia drill between August 2014 and September 2015. Every member was questioned regarding their latest participation in shoulder dystocia training. Those who had shoulder dystocia training within the last 12 months were excluded. All participants gave oral informed consent.
Randomisation
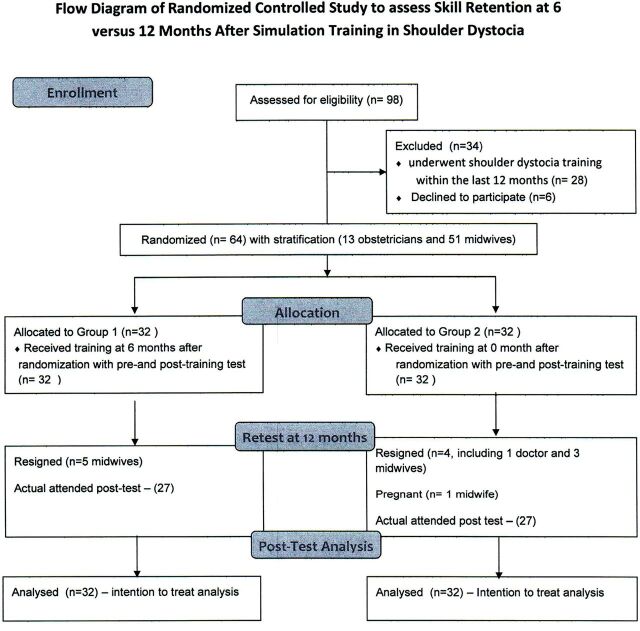
All eligible participants were randomised into either group 1 or group 2 using an online research number randomiser (http://www.randomizer.org/) performed by the principal investigator (figure 1). To achieve similar number of obstetricians and midwives in each group, stratification by staff (obstetricians or midwives) was used.
Figure 1.
Flow diagram of randomised controlled study to assess skill retention at 6 vs 12 months after simulation training in shoulder dystocia.
Group 1 (intervention)
Participants underwent simulation training on shoulder dystocia at 6 months after randomisation. Their shoulder dystocia skills would be tested 1 week before training (pre-training), immediately after training (at-training) and then retested 6 months after training (post-training) (figure 1).
Group 2 (control)
Participants underwent simulation training on shoulder dystocia at month ‘0’ after randomisation. Their shoulder dystocia skills would be tested 1 week before training (pre-training), immediately after training (at-training) and then retested 12 months after training (post-training) (figure 1).
Blinding
All participants were blinded as they were unaware of the need for retesting in future months. At month ‘12’ after randomisation, all participants in both groups 1 and 2 were retested under unexpected conditions (post-training). The idea of having every participant (in both groups 1 and 2) retested at month ‘12’ was to prevent participants being aware of the retesting and to reduce bias (figure 1). The principal investigator who assessed the outcomes performed the randomisation, while the nurse carried out the actual group allocations.
Simulation training session
All participants attended a 60-minutes lecture plus a simulation training session either at month ‘0’ after randomisation (for group 2) or at month 6 (for group 1). During the first 15 minutes, a lecture discussing the risks factors and complications associated with shoulder dystocia delivery was conducted. Via multiple visual aids, the lecture also explained the steps required to perform the manoeuvres and the principles of how these manoeuvres assist in successful shoulder dystocia delivery. In the remaining 45 minutes, the principal investigator demonstrated these manoeuvres through a manikin pelvis and baby. Both lecture and simulation shoulder dystocia training were based on the Advanced Life Support in Obstetrics (ALSO) curriculum. After the demonstration, each participant was given time to practise the manoeuvres under supervision with the manikin provided.
Test and retest
In each of the test (pre-training, at-training or post-training), the participant’s skill to deliver a baby with shoulder dystocia was tested using a birth simulator, which included a manikin pelvis with a manikin baby. The participant was asked to deliver the simulated baby after the baby’s head was delivered, and subsequently showing signs of shoulder dystocia such as turtle sign (during which the fetal head, after it had delivered, retracted back tightly against the maternal perineum) and failure of fetal head to restitute. A 15-mark self-generated marking scheme was used to score the individual’s ability to deliver all steps required for the delivery of a shoulder dystocia scenario. The marking scheme (figure 2) was based on marking schemes derived from internationally recognised courses for obstetrics emergency. These are ALSO18 and Practical Obstetrics Multi-Professional Training19 courses and also from the green-top guideline from the Royal College of Obstetrician and Gynaecologists.20
Figure 2.
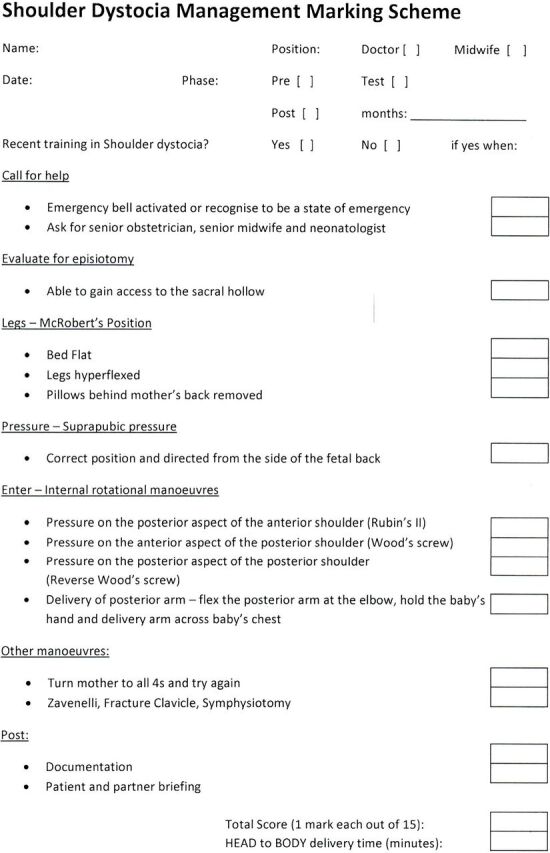
Shoulder dystocia management marking scheme.
Each of the 15 marks included some verbal answer components and some demonstrative components. No mark was awarded if the individual failed to mention any of the required content. Half mark was awarded if the answer was partially complete or if the individual named a shoulder dystocia managing manoeuvre but failed to demonstrate in the correct manner. Full marks were only awarded if all the required content for each component were mentioned and manoeuvres correctly demonstrated.
The time required to complete the scenario was also assessed. Delivery of the manikin baby was deemed achieved when all the required steps were taken. These steps include the demonstration of all four internal manoeuvres (Rubin’s II, wood screw, reverse wood screw and posterior arm) irrespective of the order it was performed. The scenario was deemed complete when the manikin baby was delivered; maternal all four position or Gaskin Maneuver (Rolling the patient onto her hands and knees) was mentioned; demonstrated knowledge of the required actions if all the manoeuvres above has completed but yet failed to deliver the baby (such as Zavanelli manoeuvre, symphysiotomy and so on); and the need for correct documentation and debriefing of the patient. The test was timed and automatically stopped at a maximum of 480 seconds. This was based on 30 seconds for each testing component and 30 seconds of briefing to the scenario.
The testing, the timing and the documentation of the results were all performed by the principal investigator to prevent potential interobserver bias. This principal investigator is a specialist obstetrician with qualifications including membership of the Royal College of Obstetrician and Gynaecology, fellowship of the Hong Kong College of Obstetricians and Gynaecologist and is an instructor for the ALSO course in Hong Kong.
Outcomes
The primary outcome was the drill score. The secondary outcome was the time required to complete the scenario. The differences in the score and time between (1) pre-training and at-training, (2) at-training and post-training, and (3) pre-training and post-training were also determined. Both primary and secondary outcomes were further reviewed after dividing the outcomes to doctors only and midwives only.
Statistical calculation and sample size
We used SPSS V.19 to perform statistical analysis. Analysis of variance (ANOVA) and t-tests were used as appropriate. Intention-to-treat analyses were used in all calculations. Statistical significance was taken with p<0.05. We also performed subgroup analysis by further dividing into doctors and midwives.
From a previous study,8 the SD for score points in dystocia training was 6.6. Assuming that after our simulating training the assessment score at 6 months would be 5 points (out of 100) higher than the score at 12 months, one side difference, and with a power of 0.8, we calculated that the minimal required samples size would be 23 per arm or a total of 46 participants.
Results
A total of 64 participants consisting of 13 obstetricians and 51 midwives were eligible to participate in the study. After randomisation, 32 participants (6 doctors and 26 midwives) were randomly allocated to group 1 (retested at 6 months) and another 32 participants (7 doctors and 25 midwives) to group 2 (retested at 12 months) (figure 1). Their characteristics are shown in table 1.
Table 1.
Demographics among group 1 (retest at 6 months) and group 2 (retest at 12 months)
| Group 1 (retest at 6 months) | Group 2 (retest at 12 months) | |
| Total number of participants | 32 | 32 |
| Total number of doctors | 7 | 6 |
| Total number of midwives | 25 | 26 |
| Total defaulters at post-test | 5 (1 doctor and 4 midwives) | 5 (all midwives) |
| Average years of working experience | 14.05±7.15 | 14.67±5.21 |
| Number of participants regularly working in the labour ward settings (ie, excluding those who only work in antenatal or postnatal wards) | 17 | 19 |
There were five missing participants in each group at the post-testing stage. In order to fulfil the criteria for intention-to-treat analysis, the average score and average time needed to complete the scenario among those who attended the post-training stage were used as the missing data within their respective groups. These missing data hence remained constant throughout.
A two-way repeated-measures ANOVA was conducted that examined the effect of group and the testing time frame (ie, pre-training, at-training and post-training) on the overall score. There was a statistically significant interaction between the effects of testing time frame on the score (p<0.001), but there was no significant interaction between the groups on the score (p=0.458). Similar statistical test was conducted against the overall time needed to complete the scenario. There was a similar significant interaction between the effects of testing time frame on the time needed to complete the scenario (p<0.001) and significant interaction between the groups on the time required to complete the scenario (p=0.018) (table 2).
Table 2.
Two-way repeated-measures analysis of variance: examined effects of group and testing time frame (pretraining, at-training, post-training) on overall score and time required to complete the scenario
| p Values | Interaction between testing time frame and group on score | Interaction between Testing time frame on score | Interaction between group on score | Interaction between testing time frame and group on time to complete scenario | Interaction between testing time frame on time to complete scenario | Interaction between group and time to complete scenario |
|---|---|---|---|---|---|---|
| All | 0.679 | <0.001* | 0.458 | 0.002* | <0.001* | 0.018* |
| Doctors | 0.581 | <0.001* | 0.847 | 0.307 | 0.008* | 0.360 |
| Midwives | 0.641 | <0.001* | 0.386 | 0.004* | <0.001* | 0.025* |
*Demonstrates statistical significance.
When the data were analysed in further details, when compared with pre-training, the drill score increased and the time required to complete the scenario decreased immediately after the simulation training (at-training) in group 1 (8.69 vs 14.34, p<0.001; 265.00 vs 140.94 s, p<0.001) and group 2 (9.53 vs 14.66, p< 0.001; 323.38 vs 183.09 s, p<0.001), respectively (table 3).
Table 3.
Participants’ scores and time to complete the scenario before (pre-training), immediately after (at-training) and retested at 6 months (for group 1) or 12 months (groups 2) after (post-training) simulation training on shoulder dystocia, compared within and between individual groups
| Data comparison within individual group | Mean time or score (±SD) | p Value (paired t-test) | Mean time or score (±SD) | p Value (paired t-test) | |
| Group 1 (retest at 6 months) | Group 2 (retest at 12 months) | ||||
| Overall score (out of 15) | Pre-training versus at-training |
8.69 (±3.58) vs 14.34 (±1.45) | <0.001* | 9.53 (±3.46) vs 14.66 (±0.65) | <0.001* |
| At-training versus post-training | 14.34 (±1.45) vs 11.71 (±2.34) | <0.001* | 14.66 (±0.65) vs 11.96 (±2.55) | <0.001* | |
| Pre-training versus post-training | 8.69 (±3.58) vs 11.71 (±2.34) | <0.001* | 9.53 (±3.46) vs 11.96 (±2.55) | <0.001* | |
| Time (s) | Pre-training versus at-training | 265.00 (±80.65) vs 140.94 (±45.96) | <0.001* | 323.38 (±105.84) vs 183.09 (±45.97) | <0.001* |
| At-training versus post-training | 140.94 (±45.96) vs 208.72 (±56.67) | <0.001* | 183.09 (±45.97) vs 196.52 (±41.98) | 0.168 | |
| Pre-training versus post-training | 265.00 (±80.65) vs 208.72 (±56.67) | <0.001* | 323.38 (±105.84) vs 196.52 (±41.98) | <0.001* | |
| Compare between groups | Mean time or score (±SD) – group 1 | Mean time or score (±SD) – group 2 | p Value (analysis of variance) | ||
| Score | Pre-training | 8.69 (±3.58) | 9.53 (±3.46) | 0.341 | |
| At-training | 14.34 (±1.45) | 14.66 (±0.65) | 0.271 | ||
| Post-training | 11.71 (±2.34) | 11.96 (±2.55) | 0.684 | ||
| Pre-training versus at- training | 5.59 (±3.08) | 5.13 (±3.17) | 0.564 | ||
| At-training vs post-training | −2.63 (±2.34) | −2.53 (±2.83) | 0.879 | ||
| Pre-training vs post- training | 2.97 (±2.87) | 2.41 (±2.83) | 0.469 | ||
| Time | Pre-training | 265.00 (±80.65) | 323.38 (±105.84) | 0.016* | |
| At-training | 140.94 (±45.96) | 183.09 (±45.97) | 0.001* | ||
| Post-training | 208.72 (±56.67) | 196.52 (±41.98) | 0.332 | ||
| Pre-training versus at- training | −120.94 (±65.72) | −127.72 (±96.19) | 0.773 | ||
| At-training versus post-training | 67.65 (±65.63) | 13.39 (±47.27) | <0.001* | ||
| Pre-training versus post-training | −56.35 (±68.73) | −136.01 (±89.65) | 0.003* | ||
*Demonstrates statistical significance.
Compared with at-training, the drill score decreased and the time required to complete the scenario increased 6 months after the training in group 1 (14.34 vs 11.71, p<0.001; 140.94 vs 208.72 s, p<0.001) and 12 months after the training in group 2 (14.66 vs 11.96, p< 0.001; 183.09 vs 196.52 s, p=0.168), respectively (table 3).
However, compared with pre-training, the drill score increased and the time required to complete the scenario decreased at 6 months after the training in group 1 (8.69 vs 11.71, p< 0.001; 265.00 vs 208.72 s, p< 0.001) and 12 months after the training in group 2 (9.53s 11.96, p <0.001; 323.38 vs 196.52 s, p< 0.001), respectively (table 3).
There was no significant difference in the pre-training score (8.69 vs 9.53, p=0.341), at-training score (14.34 vs 14.66, p=0.271), post training score (11.71 vs 11.96, p=0.684) and post-training time needed to complete the scenario (208.72 vs 196.52, p=0.332) between group 1 and group 2. There was also no significant change in score from at-training to post-training between group 1 (retested at 6 months) and group 2 (retested at 12 months) (−2.63 vs −2.53, p=0.879). However, the change in the time required to complete the scenario was longer for group 1 than group 2 (67.65 vs 13.39 s, p=<0.001) (table 3).
Subgroup analysis was performed separately for obstetricians and midwives, and similar trends were found (tables 4 and 5). Interaction between group and time to complete scenario was similarly significant for midwives but not significant for doctors (table 2).
Table 4.
Participants’ scores and time to complete the scenario before (pre-training), immediately after (at-training) and retested at 6 months (for group 1) or 12 months (groups 2) after (post-training) simulation training on shoulder dystocia (doctors only)
| Data comparison within individual group | |||||
| Doctors only | Mean time or score (±SD) | p Value (paired t-test) |
Mean time or score (±SD) | p Value (paired t-test) |
|
| Group 1 (retest at 6 months) | Group 2 (retest at 12 months) | ||||
| Overall score (out of 15) | Pre-training versus at-training | 10.00 (±3.46) vs 14.86 (±0.38) | 0.011* | 11.17 (±2.14) vs 15.00 (±0) | 0.007* |
| At-training versus post-training | 14.86 (±0.38) vs 12.71 (±1.11) | 0.007* | 15.00 (±0) vs 14.17 (±0.75) | 0.042* | |
| Pre-training versus post-training | 10.00 (±3.46) vs 12.71 (±1.11) | 0.159 | 11.17 (±2.14) vs 14.17 (±0.75) | 0.009* | |
| Time (s) | Pre-training versus at-training | 219.00 (±74.76) vs 116.86 (±32.55) | 0.028* | 241.17 (±87.69) vs 166.83 (±53.80) | 0.160 |
| At-training versus post-training | 116.86 (±32.55) vs 185.20 (±11.96) | 0.011* | 166.83 (±53.80) vs 160.50 (±30.09) | 0.717 | |
| Pre-training versus post-training | 219.00 (±74.76) vs 185.20 (±11.96) | 0.485 | 241.17 (±87.69) vs 160.50 (±30.09) | 0.101 | |
| Comparison between group 1 and group 2 | |||||
| Group 1 | Group 2 | p Values (between groups 1 and 2) analysis of variance | |||
| Score (out of 15) | Pre-training | 10.00 (±3.46) | 11.17 (±2.14) | 0.430 | |
| At-training | 14.86 (±0.38) | 15.00 (±0) | 0.297 | ||
| Post-training | 12.71 (±1.11) | 14.17 (±0.75) | 0.084 | ||
| Pre-training versus at- training | 4.86 (±2.58) | 3.83 (±2.14) | 0.543 | ||
| At-training versus post-training | −2.14 (±1.06) | −0.83 (±0.75) | 0.117 | ||
| Pre-training versus post- training | 2.17 (±2.68) | 2.83 (±1.47) | 0.971 | ||
| Time (s) | Pre-training | 219.00 (±74.76) | 241.17 (±87.69) | 0.577 | |
| At-training | 116.86 (±32.55) | 166.83 (±53.86) | 0.107 | ||
| Post-training | 185.20 (±11.96) | 160.50 (±30.09) | 0.118 | ||
| Pre-training versus at- training | −102.14 (±91.37) | −74.33 (±110.42) | 0.724 | ||
| At-training versus post-training | 68.34 (±36.32) | −6.33 (±40.51) | 0.012* | ||
| Pre-training versus post training | −33.80 (±71.02) | −80.67 (±98.28) | 0.347 | ||
Table 5.
Participants’ scores and time to complete the scenario before (pre-training), immediately after (at-training) and retested at 6 months (for group 1) or 12 months (group 2) after (post-training) simulation training on shoulder dystocia (midwives only)
| Data comparison within individual group | |||||
| Midwives only | Mean time or score (±SD) | p Value (paired t-test) |
Mean time or score (±SD) | p Value (paired t-test) |
|
| Group 1 (retest at 6 months) | Group 2 (retest at 12 months) | ||||
| Overall score (out of 15) | Pre-training versus at-training | 8.32 (±3.59) vs 14.20 (±1.61) | <0.001* | 9.15 (±3.62) vs 14.58 (±0.70) | <0.001* |
| At-training versus post-training | 14.20 (±1.61) vs 11.43 (±2.53) | <0.001* | 14.58 (±0.70) vs 11.45 (±2.55) | <0.001* | |
| Pre-training versus post-training | 8.32 (±3.59) vs 11.43 (±2.53) | <0.001* | 9.15 (±3.62) vs 11.45 (±2.55) | <0.001* | |
| Time (s) | Pre-training versus at-training | 277.88 (±78.83) vs 147.68 (±47.40) | <0.001* | 342.35 (±101.67) vs 186.85 (±44.31) | <0.001* |
| At-training versus post-training | 147.68 (±47.40) vs 215.30 (±62.50) | <0.001* | 186.85 (±44.31) vs 204.83 (±40.26) | 0.115 | |
| Pre-training versus post-training | 277.88 (±78.83) vs 215.30 (±62.50) | <0.001* | 342.35 (±101.76) vs 204.83 (±40.26) | 0.001* | |
| Comparison between group 1 and group 2 | |||||
| Group 1 | Group 2 | p Values (between groups 1 and 2) analysis of variance |
|||
| Score (out of 15) | Pre-training | 8.32 (±3.59) | 9.15 (±3.62) | 0.413 | |
| At-training | 14.20 (±1.61) | 14.58 (±0.70) | 0.280 | ||
| Post-training | 11.43 (±2.53) | 11.45 (±2.55) | 0.975 | ||
| Pre-training versus at- training | 5.80 (±2.98) | 5.42 (±3.51) | 0.685 | ||
| At-training versus post-training | −2.76 (±2.51) | −2.92 (±2.67) | 0.827 | ||
| Pre-training vs post- training | 3.04 (±3.27) | 2.31 (±2.96) | 0.421 | ||
| Time (s) | Pre-training | 277.88 (±78.83) | 342.35 (±101.76) | 0.015* | |
| At-training | 147.68 (±47.40) | 186.85 (±44.31) | 0.040* | ||
| Post-training | 215.30 (±65.50) | 204.83 (±40.26) | 0.479 | ||
| Pre-training versus at- training | −126.20 (±61.62) | −140.04 (±86.76) | 0.590 | ||
| At-training versus post-training | 67.46 (±62.53) | 17.95 (±35.41) | 0.003* | ||
| Pre-training versus post-training | −65.66 (±61.51) | −154.71 (±82.62) | 0.005* | ||
Discussion
In the present study, the participants’ management skills of shoulder dystocia in terms of drill score and time required to complete the scenario improved immediately after the simulation training, and declined at 6 months or 12 months afterwards but to a level better than before the training. Besides, the decline in drill score after 6 months (in group 1) was similar to after 12 months (in group 2), while the lengthening in scenario duration after 12 months was less than after 6 months. Similar findings were found when we separated the groups further, consisting only obstetricians and only midwives.
The overall results demonstrated a common theme. Regardless of whether the individual is a midwife or doctor, simulation training improves one’s skill in shoulder dystocia management immediately and significantly. Skills declined with time. Despite reasonable performances by our medical staff during the retesting process, the decline was significant at 6 months after training. This finding was shared with those retested at 12 months after training, hence suggesting skill levels declined within 6 months and certainly at 12 months. However, the decline at 6 months was similar to 12 months, suggesting the skills level at 6 months could be maintained at a similar level at 12 months. Despite this, any remaining knowledge score at 12 months post-training remained significantly higher than those at pre-training where an individual lacked training for over 12 months.
While most other researches in obstetrics simulation and certain international governing body suggest annual training in obstetrics emergency including shoulder dystocia, with some deemed mandatory, Vadnais et al8 conducted a similar study that showed simulation training resulted in short-term and long-term improvements in knowledge and comfort level in the management of uncommon but critical obstetrical events including shoulder dystocia. The study showed that among resident physicians, knowledge declined as soon as 4 months after testing, but improvements were retained at both 4 and 12 months compared with the pretest status, hence suggesting annual knowledge reinforcement is necessary. Our study certainly supported the view shared by Vadnais et al. Besides, our study further suggested that the regular annual training should be mandatory, while six monthly intervals would be preferable as the skills at 12-month post-training were significantly better than that at the pre-training period, and the decline in skills was significant at 6-month post-training, although maintained at 12 months. Our study also suggested regular training should benefit both midwives and doctors alike.
Surprisingly, compared with immediately after testing, the increase in time required to complete the scenario at retesting was significantly less among group 2 (retested at 12 months) than group 1 (retested at 6 months), while the decline in drill score was similar between the two groups. This unexpected finding occurred in the entire group, even on the subgroup analysis by doctors and midwives. We did not have a good explanation for this. It was possible that score and time were two different dimensions of skills, and the simulation training started 6 months earlier in group 2 than group 1.
As far as we know, this is one of the first prospective trials on simulation training carried out in Hong Kong. In our study, the two group demographics were comparable after randomisation, with no difference in doctor-to-midwife ratio, years of experience and the number of staff who regularly works in the labour ward setting where real-life exposure to shoulder dystocia is more likely. Initial skills on shoulder dystocia for both groups were suboptimal when more than 12 months have elapsed after last training, hence validating the need for annual training as other studies suggested.16 17
This study was limited by the fact that it was carried out in a single centre and with a limited number of staff. Data involving larger numbers and multiple obstetric centres are preferable. This study also possessed a significant potential for bias as the practitioner testing the participants was not blinded from the study. However, although the assessor also performed the randomisation, the actual allocation process was carried out by the midwives. As the interval between the last and previous assessment was at least 6 months, the assessor could not have remembered to which group the participants were assigned. So the bias was probably not as significant. Other limitations included the inevitability of encountering real-life shoulder dystocia scenario between testing and hence updated participants’ knowledge, which may affect the result validity. And despite the best effort to test all participants in the same period of time, it was impossible to test all individuals simultaneously and on the same day. It was unavoidable that tested participants may inform other participants about the unexpected post-training test and resulting in revision before the post-training test, hence affecting the final results.
Conclusions
Our study demonstrated that simulation training results in short-term and long-term improvement in shoulder dystocia management; however, knowledge degrades over time. Ongoing training is suggested at a minimum of 12 months’ interval for all members of the obstetrics team including midwives and doctors.
Footnotes
Contributors: MMHL: Implemented the trial, designed data collection tools, monitored data collection for the whole trial, wrote the statistical analysis plan, cleaned and analysed the data, and drafted and revised the paper. He is the guarantor and the corresponding author. CCN: Implemented the trial and revised the paper. MATWL: Initiated the project, implemented the trial and revised the paper.
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: Kowloon Central/Kowloon East Research and Ethics Committee, Hospital Authority, Hong Kong.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Shoulder dystocia. ACOG Practice Bulletin No. 40. American College of Obstetrician and Gynaecologists. Obstet Gynecol 2002;100:1045–50. [DOI] [PubMed] [Google Scholar]
- 2.Ennen CS, Satin AJ. Training and assessment in obstetrics: the role of simulation. best practice & research clinical obstetrics and gynaecology. 24, 2010:747–58. [DOI] [PubMed] [Google Scholar]
- 3.Draycott T, Sibanda T, Owen L, et al. Does training in obstetric emergencies improve neonatal outcome? BJOG 2006;113:177–82. 10.1111/j.1471-0528.2006.00800.x [DOI] [PubMed] [Google Scholar]
- 4.Cass GK, Crofts JF, Draycott TJ. The use of simulation to teach clinical skills in obstetrics. Semin Perinatol 2011;35:68–73. 10.1053/j.semperi.2011.01.005 [DOI] [PubMed] [Google Scholar]
- 5.Draycott TJ, Crofts JF, Ash JP, et al. Improving neonatal outcome through practical shoulder dystocia training. Obstet Gynecol 2008;112:14–20. 10.1097/AOG.0b013e31817bbc61 [DOI] [PubMed] [Google Scholar]
- 6.Deering S, Poggi S, Macedonia C, et al. Improving resident competency in the management of shoulder dystocia with simulation training. Obstet Gynecol 2004;103:1224–8. 10.1097/01.AOG.0000126816.98387.1c [DOI] [PubMed] [Google Scholar]
- 7.Crofts JF, Bartlett C, Ellis D, et al. Training for shoulder dystocia: a trial of simulation using low-fidelity and high-fidelity mannequins. Obstet Gynecol 2006;108:1477–85. 10.1097/01.AOG.0000246801.45977.c8 [DOI] [PubMed] [Google Scholar]
- 8.Vadnais MA, Dodge LE, Awtrey CS, et al. Assessment of long-term knowledge retention following single-day simulation training for uncommon but critical obstetrical events. J Matern Fetal Neonatal Med 2012;25:1640–5. 10.3109/14767058.2011.648971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Buerkle B, Pueth J, Hefler LA, et al. Objective structured assessment of technical skills evaluation of theoretical compared with hands-on training of shoulder dystocia management: a randomized controlled trial. Obstet Gynecol 2012;120:809–14. 10.1097/AOG.0b013e31826af9a9 [DOI] [PubMed] [Google Scholar]
- 10.Gregg SC, Heffernan DS, Connolly MD, et al. Teaching leadership in trauma resuscitation: immediate feedback from a real-time, competency-based evaluation tool shows long-term improvement in resident performance. J Trauma Acute Care Surg 2016;81:729–34. 10.1097/TA.0000000000001186 [DOI] [PubMed] [Google Scholar]
- 11.Smith S. Team training and institutional protocols to prevent shoulder dystocia complications. Clin Obstet Gynecol 2016;59:830–40. 10.1097/GRF.0000000000000231 [DOI] [PubMed] [Google Scholar]
- 12.Grobman WA. Shoulder dystocia: simulation and a team-centered protocol. Semin Perinatol 2014;38:205–9. 10.1053/j.semperi.2014.04.006 [DOI] [PubMed] [Google Scholar]
- 13.Goffman D, Heo H, Pardanani S, et al. Improving shoulder dystocia management among resident and attending physicians using simulations. Am J Obstet Gynecol 2008;199:294.e1–294.e5. 10.1016/j.ajog.2008.05.023 [DOI] [PubMed] [Google Scholar]
- 14.Madani A, Watanabe Y, Vassiliou MC, et al. Long-term knowledge retention following simulation-based training for electrosurgical safety: 1-year follow-up of a randomized controlled trial. Surg Endosc 2016;30:1156–63. 10.1007/s00464-015-4320-9 [DOI] [PubMed] [Google Scholar]
- 15.Cemach LG, Die WM. The Sixth report of the confidential enquiries into maternal deaths in the United Kingdom. 2004: RCOG Press, 2000-2002. [Google Scholar]
- 16.Siassakos D, Crofts J. Winter C and SaFE study group. Education Multiprofessional ‘fire-drill’ training in the labour ward. The Obstetrician and Gynaecologist 2009;11:55–60. [Google Scholar]
- 17.Crofts JF, Bartlett C, Ellis D, et al. Management of shoulder dystocia: skill retention 6 and 12 months after training. Obstet Gynecol 2007;110:1069–74. 10.1097/01.AOG.0000286779.41037.38 [DOI] [PubMed] [Google Scholar]
- 18.ALSO Advanced Life support in Obstetrics, 2016. [Google Scholar]
- 19.Cornthwaite K, Crofts JF, Draycott T, et al. Training for obstetrics emergencies: prompt and shoulder dystocia. PROMPT 2015. [Google Scholar]
- 20.RCOG. Shoulder dystocia. Green Top Guideline. 42, 2012. [Google Scholar]