There is a significant and as yet underexplored area of literature related to the use of mobile devices and their impact on radiology education. This editorial will highlight some of the novel tools and techniques, which are accessible to radiology trainees that may enhance their medical education.
The recent growth in popularity of mobile devices among clinicians and other healthcare professionals since the introduction of the ‘smartphone’ and ‘tablet’ has been exponential. Mobile devices offer multiple functions that allow them to function as an adjunct clinical tool. Many have identified that mobile devices can serve as mobile clinical references, with easy access to the literature which has seen a surge in expansion from printed format to ‘apps’.1–3 Recent data has demonstrated a large utilisation of mobile devices among the medical professionals and students.4–6 Overall, usage by medical professionals has ranged from point-of-care references to clinical and drug references, medical calculators and access to the electronic health record.4–6 Medical students have found mobile devices as a tool to supplement their education, with access to e-textbooks, simulation tools and similar medical references.6
The visual nature of digital radiology makes it highly suitable to modern mobile devices. There is significant potential to use these devices to support day-to-day clinical radiology activities including mobile viewing and assessment of Digital Imaging and Communications in Medicine (DICOM) format images. Mobile devices have greatly improved in the past decade to now support high definition displays that improves image visibility. Accordingly, formal investigation into the utility of these devices has predominantly focused on their suitability for this clinical task including mobile image reporting, mobile diagnosis and comparison of interobserver reliability.7–10 Many of these early studies have been encouraging and there certainly appears to be value to continue this research further as mobile hardware improves. Recent studies of radiology apps identified 8111 and 32112 radiology specific applications in a range of categories including DICOM viewers, decision support applications, clinical reference, interactive radiographic encyclopaedias, patient education and journal reading programmes.
Mobile devices can support independent radiology education
The utility of mobile devices to support medical education has been recognised at a range of undergraduate and postgraduate levels.13–15 Many educators attribute this to the fact that mobile devices offer users enhanced access to learning resources at useful times independently of geographic location. From a general perspective, mobile devices offer a number of features which can assist and facilitate medical education. The portable nature of these devices combined with their ability to store and access e-learning materials is recognised as improving learning efficiency in general medical education and radiology.16 One example is the ability to access the internet and other online radiology learning resources. While in the UK radiology trainees are familiar with the RITI platform, which is accessed across the internet, it is not a dedicated platform. Mobile devices can also access existing online question banks and other self-assessment tools which are useful to practice questions in advance of postgraduate exams. There are also a number of journals that have developed mobile-friendly versions or dedicated apps allowing radiology trainees to access the latest medical literature in their particular field of interest. Interestingly, one survey of radiology trainees highlighted the use of mobile tablet devices noting that 81% felt they would spend more time learning radiology if equipped with a mobile tablet device.17
One of the advantages of mobile devices over traditional learning resources such as textbooks and radiographic atlases is the ability to run specific ‘Apps’. An app is an independent piece of software that can be run on a mobile device to carry out a specific purpose. There are a number of specific advantages of using a mobile app for radiology education. Mobile apps are not bound by the same physical limitations as traditional books and can therefore contain vast imaging databases while remaining truly portable. A number of case-based mobile apps exist which allow trainees to assess their own diagnostic ability in the context of a specific case. There are also other educational resources in a range of media including audio podcasts and video. One of the real strengths of mobile devices is their ability to store hundreds of standard textbooks in electronic format. These offer additional benefits over ‘traditional’ books due to their use of hyperlinking, search functionality and ability to share images and other learning resources via social media and email. Given the educational potential using mobile devices it is therefore perhaps not surprising that the most common radiology app themes are clinical reference and education which include apps focused on guidelines, revision guides, cancer staging, scanning protocols, textbooks, interactive cases, tutorials and question banks.11 12
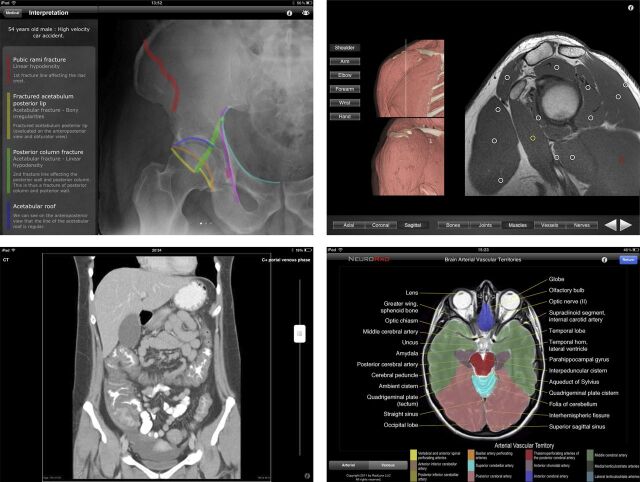
Many of the apps and other e-Learning resources available cover a number of different radiographic modalities highlighting a range of anatomy and pathology. Many apps are aimed at different training levels that enable educators to choose an appropriate resource for the trainee. There is a wide selection of interactive imaging atlases available for mobile devices, with one 2013 study identifying 33 mobile atlases covering a wide range of radiographic modalities and patients, examples of which can be seen in figure 1. Figure 1 highlights features of radiology mobile apps which are of importance to radiology trainees. These apps often provide a short clinical history and the relevant radiographs leaving the user to work out the relevant diagnosis and management as shown in figure 1D. Independent learning using these apps is often easier on a tablet due to the larger screen size and better resolution, however this comes at the cost of portability.11 Certain apps allow the user to access and interact with radiographs including standard adjustment options such as brightness, contrast and zoom features. For more advanced image manipulation such as various radiographic windows, rotation and distance measurement, users would need to load their own DICOM cases into existing mobile apps that can read these files.
Figure 1.
Example screenshots from radiology education mobile apps (clockwise from top left): (A) RealWorld Orthopaedics, (B) Monster Anatomy HD Upper Limb, (C) Neurorad and (D) Radiopaedia.
Another unique feature with great potential in radiology education is the ability to overlay colour and annotations directly onto a specific radiograph. This has been successfully used in a number of radiology apps to highlight relevant pathology and anatomy. As a result, trainees may develop their understanding of complex radiographs without supervision. Figure 1A and C highlights this innovation for the interpretation and recognition of radiographic anatomy and pathology. This technique has also been applied from an anatomical perspective to help trainees develop an understanding of normal radiographic anatomy in a range of modalities such as ultrasound, X-ray, CT and MRI, for example, figure 1B. Simple touch gestures can be used to hide imaging labels allowing trainees to test their own understanding in self-directed learning.
The dark side of mobile radiology education
For all the potential educational advantages that mobile devices can offer radiology, there are some limitations to be aware of. There are no regulatory requirements to ensure that radiology apps contain accurate information. Furthermore, with the barriers to entry to create an app already low and decreasing, it is likely that quality of radiology apps may prove extremely variable, as directly experienced by the authors. Problems that trainees may encounter are poor image quality, missing radiographs, inaccurate content, absent referencing or out of date guidelines among others. These concerns are not strictly limited to radiology apps and work is in in progress to identify an appropriate method of improving the quality of medical apps given the current regulatory oversight of mobile apps.18 19 There are also concerns regarding the ability for clinicians and trainers to identify apps of sufficient quality for educational purposes.3 Many radiology apps do not report any form of authorship with one study identifying that only 36% advertised medical professional involvement in application development.12 There is also very little information given regarding developer conflicts of interest which may bias the content of an app. Current infrastructure limitations such as the need for Internet connectivity, financial concerns and device security also need be taken into account before formal adoption and integration into a training programme. Finally, the lack of formal literature evidence base conclusively proving the utility of mobile devices for education in radiology may act as a deterrent to some.
Identifying high-quality radiology apps
Given the wide variety and quality of mobile apps available, it is important that educators understand the key qualities to look for when critically appraising a mobile app. There are a number of methods to identify high-quality apps including word of mouth, social media, App stores, physician peer review, journal articles and more however the interested reader is directed to Aungst et al3 for a general overview of how to identify relevant mobile apps. There are a number of considerations users should consider when assessing radiology apps identified in table 1.20 Users should assess each app with regards to each of the considerations and then decide for themselves whether or not the app is suitable for the desired task.
Table 1.
A table highlighting some of the key considerations when assessing the utility of a medical app for radiology education
| Essential considerations | Content considerations | Educational considerations | Other considerations |
|---|---|---|---|
|
|
Range of imaging modalities eg, CT, X-ray, ultrasound, MRI Radiological slices:
|
Background of developer:
Infrastructure
|
A note on regulation of mobile medical apps
The wide range in utility, quality and safety of many mobile apps available has led national regulatory bodies to release guidance governing the use of apps in clinical situations. According to current MHRA and FDA guidelines, mobile apps that diagnose, support diagnosis or clinical decisions, make calculations to determine diagnosis or treatment or are used for any medical purpose are classed as ‘medical devices’ and therefore require formal assessment for a CE mark.21 A CE mark is an assurance that an app meets essential safety criteria and should be clinically safe to use. Under current guidelines, educational apps such as those described above are unlikely to be classed as medical apps and therefore do not require a CE mark. The medical app ecosystem is evolving rapidly and this regulatory system is likely to reflect any change therefore users of medical apps for clinical or educational purposes should remain mindful of the current regulatory position and modify their usage accordingly.16 18 19 21
What does the future hold?
Whatever your personal opinion of mobile devices and medical applications, one fact is clear: these devices are here to stay and thus the real question is; how can the radiological community ensure trainees have access to high-quality educational resources on mobile devices. Formal recognition by trainers, trainees and educational bodies will raise awareness of the advantages and limitations of mobile devices for education. Further investigation of the quality of existing radiology apps alongside development of key criteria and guidance will enable users to assess and identify a useful radiology app at the point of care. Validation and recognition of these key quality standards by appropriate educational bodies will further confirm mobile devices as a formal radiology education tool. Given the fast pace of development and subsequent evolution in this dynamic and turbulent field, it is likely that many of the limitations described here will be mitigated or overcome in due course. In particular, increasing resolution and technological hardware development is likely to result in improved mobile image quality in the future. Recognition of the advantages and limitations of mobile devices and medical apps will enable trainees to appropriately structure and complement their education thus developing their own individual learning by incorporation of mobile learning resources with traditional education programmes.
Acknowledgments
The authors acknowledge helpful comments from the peer reviewers to update this manuscript.
Footnotes
Twitter: Follow Thomas Lewis at @thomasllewis and Timothy Aungst at @tdaungst
Competing interests: TLL and TDA are writers and editors for iMedicalApps.com, a website dedicated towards providing news on the integration of mobile technology into medical care and the reviewing of medical apps for mobile devices. They do not consult nor receive reimbursement from app developers or creators.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Ozdalga E, Ozdalga A, Ahuja N. The smartphone in medicine: a review of current and potential use among physicians and students. J Med Internet Res 2012;14:e128. 10.2196/jmir.1994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mosa AS, Yoo I, Sheets L. A systematic review of healthcare applications for smartphones. BMC Med Inform Decis Mak 2012;12:67. 10.1186/1472-6947-12-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aungst TD, Clauson KA, Misra S, et al. How to identify, assess and utilise mobile medical applications in clinical practice. Int J Clin Pract 2014;68:155–62. 10.1111/ijcp.12375 [DOI] [PubMed] [Google Scholar]
- 4.Boruff JT, Bilodeau E. Creating a mobile subject guide to improve access to point-of-care resources for medical students: a case study. J Med Libr Assoc 2012;100:55–60. 10.3163/1536-5050.100.1.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sclafani J, Tirrell TF, Franko OI. Mobile tablet use among academic physicians and trainees. J Med Syst 2013;37:9903. 10.1007/s10916-012-9903-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Payne KF, Wharrad H, Watts K. Smartphone and medical related App use among medical students and junior doctors in the United Kingdom (UK): a regional survey. BMC Med Inform Decis Mak 2012;12:121. 10.1186/1472-6947-12-121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.John S, Poh AC, Lim TC, et al. The iPad tablet computer for mobile on-call radiology diagnosis? Auditing discrepancy in CT and MRI reporting. J Digit Imaging 2012;25:628–34. 10.1007/s10278-012-9485-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnson PT, Zimmerman SL, Heath D, et al. The iPad as a mobile device for CT display and interpretation: diagnostic accuracy for identification of pulmonary embolism. Emerg Radiol 2012;19:323–7. 10.1007/s10140-012-1037-0 [DOI] [PubMed] [Google Scholar]
- 9.Tennant JN, Shankar V, Dirschl DR. Reliability and validity of a mobile phone for radiographic assessment of ankle injuries: a randomized inter- and intraobserver agreement study. Foot Ankle Int 2013;34:228–33. 10.1177/1071100712466849 [DOI] [PubMed] [Google Scholar]
- 10.De Maio P, White LM, Bleakney R, et al. Diagnostic accuracy of an iPhone DICOM viewer for the interpretation of magnetic resonance imaging of the knee. Clin J Sport Med 2014;24:308–14. 10.1097/JSM.0000000000000005 [DOI] [PubMed] [Google Scholar]
- 11.Székely A, Talanow R, Bágyi P. Smartphones, tablets and mobile applications for radiology. Eur J Radiol 2013;82:829–36. 10.1016/j.ejrad.2012.11.034 [DOI] [PubMed] [Google Scholar]
- 12.Rodrigues MA, Visvanathan A, Murchison JT, et al. Radiology smartphone applications; current provision and cautions. Insights Imaging 2013;4:555–62. 10.1007/s13244-013-0274-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wallace S, Clark M, White J. “It”s on my iPhone’: attitudes to the use of mobile computing devices in medical education, a mixed-methods study. BMJ Open 2012;2:pii:e001099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davies BS, Rafique J, Vincent TR, et al. Mobile Medical Education (MoMEd)—how mobile information resources contribute to learning for undergraduate clinical students—a mixed methods study. BMC Med Educ 2012;12:1. 10.1186/1472-6920-12-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hardyman W, Bullock A, Brown A, et al. Mobile technology supporting trainee doctors’ workplace learning and patient care: an evaluation. BMC Med Educ 2013;13:6. 10.1186/1472-6920-13-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pinto A, Selvaggi S, Sicignano G, et al. E-learning tools for education: regulatory aspects, current applications in radiology and future prospects. Radiol Med 2008;113:144–57. 10.1007/s11547-008-0227-z [DOI] [PubMed] [Google Scholar]
- 17.Korbage AC, Bedi HS. Mobile technology in radiology resident education. J Am Coll Radiol 2012;9:426–9. 10.1016/j.jacr.2012.02.008 [DOI] [PubMed] [Google Scholar]
- 18.Misra S, Lewis TL, Aungst TD. Medical application use and the need for further research and assessment for clinical practice: creation and integration of standards for best practice to alleviate poor application design. JAMA Dermatol 2013;149:661–2. 10.1001/jamadermatol.2013.606 [DOI] [PubMed] [Google Scholar]
- 19.Lewis TL, Wyatt JC. mHealth and mobile medical apps: a framework to assess risk and promote safer use. J Med Internet Research 2014;16:e210. 10.2196/jmir.3133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boissaud-Cooke MA, Lewis TL, Miller G, et al. Development of a checklist to identify neuro-radiology and -anatomy apps in medical education. Oral presentation. British Association of Clinical Anatomists Winter Meeting, Bristol, 8 January 2015. [Google Scholar]
- 21.Royal College of Physicians. Using apps in clinical practice. April 2015. https://www.rcplondon.ac.uk/sites/default/files/apps_guidance_factsheet.pdf (accessed 10 May 2015).