Abstract
Background
Asthma is the most common chronic disease of childhood and an important preventable cause of mortality in children and young people (CYP). Few studies have brought together CYP and health professionals to understand the patient perspective of routine asthma care. We sought to explore how young people engage with routine asthma care in North West London through sequential simulation.
Method
We designed a sequential simulation focusing on routine asthma management in young people aged 12–18. A 20 min simulation was developed with four young people to depict typical interactions with school nurses and primary care services. This was performed to a mixed audience of young people, general practitioners (GPs), paediatricians, school nurses and commissioners. Young people were invited to attend by their GPs and through social media channels. Attendees participated in audio-recorded, facilitated discussions exploring the themes arising from the simulation. Recordings were transcribed and subjected to thematic analysis.
Results
37 people attended the sequential simulation. Themes arising from postsimulation discussions included recognition of chaotic family lifestyles as a key barrier to accessing care; the importance of strong communication between multidisciplinary team professionals and recognition of the role school nurses can play in delivering routine asthma care.
Conclusion
Sequential simulation allows healthcare providers to understand routine asthma care for CYP from the patient perspective. We propose improved integration of school nurses into routine asthma care and regular multidisciplinary team meetings to reduce fragmentation, promote interprofessional education and address the widespread professional complacency towards this lethal condition.
Keywords: sequential simulation, patient experience, inter-professional education, qualitative research
What is already known on this subject.
Despite effective treatments and clear clinical guidelines, asthma remains an important avoidable cause of morbidity and mortality in young people.
An important contributory factor to poor outcomes in this group is suboptimal engagement with routine asthma care.
Sequential simulation brings patients and professionals together to better understand existing care pathways and codesign service improvements.
What this study adds.
Our work identifies multiple patient-level, systems-level, communication and technological barriers to effective routine asthma care for young people.
School nurses are an important and underused professional group in routine asthma care.
Financial incentives may be insufficient to engage young people in efforts to codesign improvements to existing healthcare services.
Background
Asthma is the most common chronic disease of childhood, with over one million children affected in the UK alone.1 Despite its innocuous reputation, asthma kills; paediatric mortality from asthma in England and Wales is among the worst in Europe.2 The 2014 National Review of Asthma Deaths (NRAD) highlighted widespread failings in the delivery of asthma care in primary and secondary care settings and emphasised the need for an ‘end to the complacency’ surrounding asthma.3 Most deaths occurred in children and young people (CYP) with ‘mild’ or ‘moderate’ asthma, and one or more major avoidable factor was identified in 67% cases. Recommendations from this report included improved patient education, self-management and coordinated multidisciplinary disease management.
Young people bring unique challenges to the management of asthma. The transition to adulthood brings increasing independence and self-reliance, with responsibility for chronic disease management passing from parent to child. However, poor symptom recognition4 and adherence to treatment5 can lead to worse clinical outcomes in this group. Communication barriers can lead to disengagement from services at a time when crucial health behaviours are becoming established.6 Focus group discussions and interviews with adolescents and parents have identified forgetfulness, embarrassment and apathy as key barriers to effective asthma self-management.7
Most paediatric asthma care is routine and reliant on preventive management and self-care.8 In the UK, routine care is usually delivered by general practitioners (GPs). A GP is a local family physician responsible for providing preventive care such as immunisations, managing long-term conditions and acting as a first point of contact for acutely unwell children with non-life-threatening illness. GPs are incentivised to conduct an annual review of children’s symptoms, medications, inhaler technique and personalised asthma action plans (PAAPs).9 A subset of children with moderate to severe asthma may be referred by their GP to secondary care services for further assessment, investigation and treatment under specialist nursing and paediatric teams.
The first stage in improving health services is engagement with those who use, plan and deliver care in order to evaluate the current system. CYP have a right to influence the health services that affect them, and health system codesign can improve engagement of marginalised groups.10 Sequential simulation (SqS) is a novel research tool which places patient experience at the centre of service evaluation and redesign.11–13 Patient and professional input is used to develop a simulation that reflects selected aspects of a given care pathway. The live simulation is then performed to a mixed audience to provoke discussion. We have previously described an SqS which depicted a young person experiencing an acute asthma attack. This highlighted the difficulties in a typical patient journey, such as delayed symptom recognition and access to treatment, and emphasised the importance of integrated and person-centred care.14 Paediatricians who helped to develop this simulation cascaded lessons to colleagues attending monthly multidisciplinary team (MDT) meetings within our regional integrated child health system.15 Subsequent discussions between paediatricians and GPs within this network revealed widespread concerns regarding routine asthma care. Several GPs were worried that young people were not engaging with routine services and were at risk of avoidable asthma attacks. We sought to understand this problem using SqS.
Our primary aim was to understand how young people aged 12–18 years engage with routine asthma services in North West London (NWL). Secondary objectives included identification of barriers to adolescent engagement with routine asthma services; potential solutions for local GP practices; and strengths and weaknesses in current patient pathways of interest to healthcare commissioners.
Methods
Simulation storyboard development
EM and AI conducted semistructured interviews with four young people with asthma who lived and used health services within NWL. All interviews were conducted in the presence of a school nurse. Each young person was asked to reflect on their perceptions of their condition; how they engaged with their GP and other health professionals; and the factors which promoted or hindered their engagement with routine asthma services. To encourage openness, discussions were not audio recorded. However, both interviewers made contemporaneous written notes.
Recurring concepts from these interviews, such as the role of the school nurse in symptom surveillance and tension between young people and their parents, formed the basis of simulation storyboard. The storyboard was developed by a team of junior doctors and a dedicated SqS researcher, and refined by a local GP and Consultant Paediatrician. Disagreements arising during storyboard design were resolved through group discussion and reference to notes taken during semistructured interviews with young people. The SqS researcher (AI) had previously conducted several SqS. MF, CC and EM had no formal training in qualitative research but were involved in system-wide quality improvement with a focus on childhood wheeze and asthma at their National Health Service (NHS) Hospital Trust.
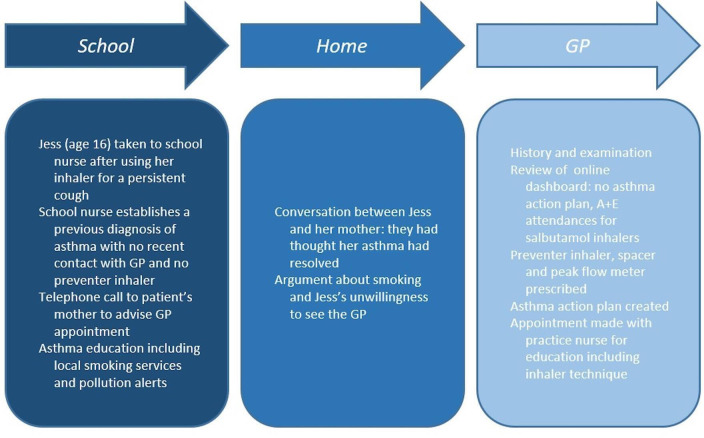
The characters in the simulation were Jess (a 16-year-old girl with asthma), her mother, a school nurse and a GP. These composite characters were not actual patients or relatives and any resemblance to living or deceased people would be coincidental. The simulation structure is shown in figure 1.
Figure 1.
Structure of sequential simulation. GP, general practitioner.
Simulation workshop delivery
The simulation lasted 20 min. Professional actors were employed to portray Jess and her mother. GP and school nurse roles were played by healthcare professionals acting in their usual capacity. The simulation was semiscripted. Actors and healthcare professionals were provided with a storyboard to follow. A scripted narrator linked different scenes together. The workshop took place in the Imperial College London Invention Rooms in White City, North West London. This venue was selected as it is close to three secondary schools and has good transport links. The simulation was performed in a function room. We used stage props including a desk, chairs, inhaler, peak flow metre and stethoscope to enhance realism.
We invited stakeholders in local children’s asthma services to the simulation workshop. These included patients, parents, GPs, school nurses, specialist nurses, paediatricians, youth workers, commissioners, pharmacists, academics and representatives from organisations such as the Healthy London Partnership. GPs issued short message service (SMS) and written invitations to patients with asthma and secondary care providers issued opportunistic invitations over several months. Other stakeholders were invited by email or in person. The event was publicised via social media.
Postsimulation discussions
All workshop participants watched the simulation. Attendees were then split into four small groups, each with a broad range of professionals and comprising 8–9 individuals. Small group discussions were facilitated by RK, MW, Bob Klaber (consultant paediatrician and cofounder of Connecting Care for Children) and David Mummery, an academic GP working in NWL. All facilitators had prior experience of data collection in SqS. MW, Bob Klaber and David Mummery have an interest in asthma quality improvement and integrated care.
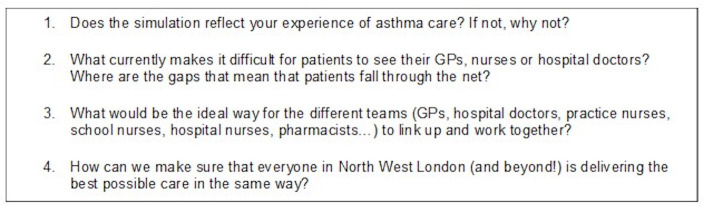
Participants were asked to reflect on the situation presented in the simulation, their own experiences and possible improvements to the current pathway, in small-group discussions lasting 40 min (figure 2). Small groups were then dissolved and discussions continued among a single large group containing all attendees. All discussions were audio recorded.
Figure 2.
Questions for sequential simulation participants. GP, general practitioner.
Data analysis
Following the workshop, MF supervised two medical students who transcribed, encoded and deidentified all excerpts of the discussion. These data were stored in encrypted spreadsheets. The transcribed recordings were subjected to thematic analysis. Data were analysed using an inductive approach, allowing codes and themes to emerge rather than imposing a structured analytical framework. MF and CC independently analysed the transcribed recordings. Written notes made by facilitators during the discussion were cross-checked against the final themes.
Results
Attendance
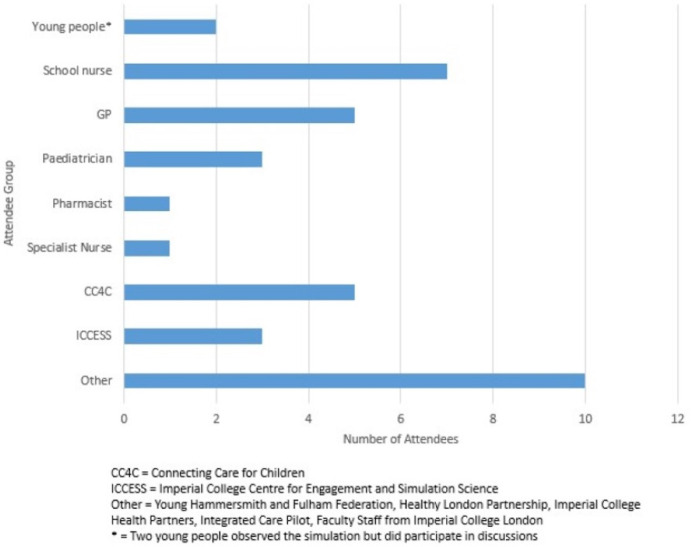
Thirty-seven people attended the workshop (figure 3). Despite recruitment efforts, only two young people attended the workshop and both left prior to small group discussions.
Figure 3.
Attendee breakdown at sequential simulation. GP, general practitioner.
Thematic analysis results
Seven themes were identified from the data (table 1).
Table 1.
Themes and subthemes arising from postsimulation discussions
| Theme | Subthemes |
| Patient factors that imperil high-quality routine asthma care | Chaotic family lifestyles Default use of unscheduled care Language barriers |
| System factors that imperil high-quality routine asthma care | Fragmentation of care leading to an over-reliance on patients, families and professionals going above and beyond to fill gaps Delays in accessing GP appointments |
| Multidisciplinary team (MDT) communication and integrated care | Delays in GPs receiving discharge summaries after a young person is discharged from hospital following an asthma attack Regular face-to-face meetings as a conduit to improved communication between MDT professionals Duplication of work and record keeping in a siloed health system |
| School as a key site for asthma management | School first aiders are often the first group to recognise deteriorating asthma control in young people School nurses have the skills and social capital to perform routine asthma reviews in a convenient setting for young people School nurses are poorly integrated into the wider MDT |
| Technology in routine asthma care | Existing and future tools could be used to promote self-care Risk of personal and regional variation in uptake of technologies entrenching health inequality |
| Consistent communication with young people and carers | Variable completion of written personalised asthma action plans Need to dispel myths around asthma that underpin complacency |
| Change ideas—improving services | Asthma group consultations MDT meetings to facilitate registry reviews, share best practice, and identify young people requiring specialist review Patient records to include contact details for school nurse |
GP, general practitioner; MDT, multidisciplinary team.
Difficulties patients and families face in accessing care
There was recognition that children with the greatest need for asthma care were often unlikely to access it, in part due to chaotic family lifestyles. One participant commented: ‘They’ve [the patient and their family] got so much going on…their child having asthma is going to be the least of their worries’. Children within the same family may also share inhalers and thus avoid medical reviews usually prompted by increasing salbutamol prescriptions.
Language barriers within NWL were also identified as a key factor impeding access to care, with parents struggling to book review appointments and conduct consultations in their second language. In conjunction with prolonged waiting times in primary care, this may lead parents to seek help in secondary care or from private providers in their own language. Other patient difficulties identified in the discussion included psychosocial factors—notably the stigma surrounding chronic conditions and peer pressure to engage in risky behaviours such as smoking.
System factors
Participants reported that current services were overstretched, with long-waiting times in general practice and increased emergency department attendances across the region. GPs reported that insufficient time and resources often led to red flags being overlooked, such as frequent prescription requests for salbutamol inhalers. They also said that ‘there’s no prompt in the system to notice if (patients) don’t come (to appointments)’.
Participants felt that care processes were failing young people in the period after their discharge from hospital following an asthma attack. GPs reported long delays in receiving discharge summaries, leading to an over-reliance on patients and parents to ‘connect the dots’. One GP commented ‘If someone’s been in hospital, it’s very unlikely they’ll have a 48-hour review, because no-one will know about it. Families end up being the glue…which I feel is wrong.’
Professionals also felt unsure about who held clinical responsibility for follow-up and creating PAAPs for patients. GPs felt reluctant to ‘undiagnose’ asthma due to medicolegal concerns: ‘The easiest thing is to keep saying that a child has asthma and keep repeating the prescription’.
Enhancing multidisciplinary team working
Effective communication between MDT members was deemed to be important for high quality care. Face-to-face meetings were especially valued to reinforce links within the MDT. ‘If you understand the system as a professional and you know who all the different players are…you’re more likely to reach out to that person…and let them know and share your care plan’.
Participants identified training for non-healthcare professionals (such as youth workers, teachers and sport coaches) as a key priority as they may be the first groups to recognise signs of acute and worsening chronic asthma. ‘School nurses—because there’s not very many of them…rely quite heavily on first aiders.’
Discussions repeatedly focused on children receiving care from the right professional at the right time. It was felt that up-skilled MDT members—such as school and specialist nurses and pharmacists—could perform effective asthma reviews and thereby relieve pressure on an overburdened primary care system. ‘Seeing the nurse, who has done lots of courses in asthma…is probably a better place to go.’
School as a site for improving asthma management
Several participants had never met a school nurse before, symbolising the poor integration of this key group within the wider MDT. One school nurse commented: ‘There’s definitely a lack of communication between parents and us and GPs…who don’t love talking to us, in my experience.’ Many professionals left the workshop with a new appreciation of the role played by school nurses in chronic disease management. ‘(The) school nurse interface with the whole system is part of the solution.’
Schools were also recognised as a key site where external healthcare professionals could engage young people. One school nurse had previously attended Parents’ Evenings in order to provide parents with their child’s PAAP and discuss their symptom burden. Several participants expressed a desire to deliver education and consultations within schools. A consultant paediatrician commented ‘supporting an activity at Parents’ Evening…would message ‘this is serious’ and not ‘just asthma’. Sports days were identified as another potential time at which healthcare professionals could meet with parents and children and deliver targeted asthma education.
Technology
Participants felt that technology had the potential to transform asthma self-care for this digitally literate patient group. Discussions focused on mobile applications capable of providing live pollution updates and monitoring symptom burden; digital inhalers providing feedback to patients and clinicians; and democratising access to test results.
Technology was generally seen as a positive means of engaging and empowering patients and parents. However, participants were uncertain about the benefits of technological innovations and the risk of overloading patients with unhelpful information: ‘This increases anxiety. ‘I have got [asthma] and am getting these text alerts [about pollution] but what should I do?’. They also expressed concerns that those who could not afford smartphones or lacked digital skills could become disadvantaged.
Consistent communication
Many clinicians attending the workshop had created PAAPs for their patients but felt that this was inconsistent across the health system. Several participants commented that turning asthma plans into online tick-box exercises could be demotivating and unnecessarily long-winded. ‘The (online) care plan our template generates does not work, so people code values in the wrong boxes.’ Participants were concerned that young people and carers can become confused and overwhelmed by inconsistent educational materials and the mixed messages they receive from the varied asthma action plans issued by different healthcare providers.
Participants felt that education should be used to dispel misconceptions around asthma—notably the widespread belief that adolescents will ‘grow out’ of the condition—and address inhaler technique. ‘I remember this one child who showed me how to use the inhaler and his mother squirted it into the nose. The next time they come back, they are doing something more interesting. I think inhaler technique is key’
Change ideas
Participants felt that many basic elements of routine asthma care ‘were still missing’. Change ideas included:
Timely notification of relevant professionals when a patient’s asthma control is deteriorating. This may require senior clinicians in secondary care to liaise directly with GP receptionists to arrange urgent 48 hours follow-up appointments after discharge. Participants called for more flexibility in allowing school nurses to directly book GP appointments.
Collaboration across NWL to agree on consistent educational materials and a standardised PAAP that could be freely shared between all MDT members.
Asthma group consultations—shared appointments for adolescents with asthma, delivered by several MDT members (such as a GP and specialist nurse). These sessions would incorporate education, individual reviews of asthma control and completion of PAAPs.
MDT Hubs to facilitate regular face-to-face meetings of healthcare professionals and share best practice. The MDT could also review a practice’s asthma registry to ‘de-list’ adolescents without convincing evidence of asthma.
Improved school outreach to help hard-to-reach adolescents with asthma. This may involve clinicians delivering education and consultations in schools through Parents’ Evenings and Sports Days.
Patient records to include clear documentation of their school nurse’s contact details.
‘Asthma friendly school’ certification to include a minimum level of staff training and other asthma standards. More generally, prioritising training for non-healthcare professionals to recognise signs of worsening asthma control.
Increasing use of linked datasets to track signs of poor asthma control, such as multiple salbutamol prescriptions, integrated from multiple primary and secondary care data sources, to allow early identification of high risk patients.
Discussion
We developed an SqS to explore how young people experience routine asthma care in NWL, and to facilitate the codesign of improved services for this hard-to-reach group. This exploratory exercise was informed by discussions with four young people with asthma, and various healthcare professionals including GPs, paediatricians and school nurses. Unfortunately, young people did not contribute to workshop discussions, However, the professionals present recognised the simulation as an effective representation of authentic everyday encounters and endorsed its use as a tool to stimulate debate and facilitate service evaluation. The simulation addressed factors that impede effective self-care, including poor symptom recognition and emphasised the importance of MDT communication in routine clinical care.
Although postsimulation discussions generated tractable change ideas, true codesign of improved healthcare services was not possible as no young people were present. Eligible young people received SMS and written invitations from their GPs; secondary care specialists also issued opportunistic verbal invitations over a period of several weeks. The event was promoted via social media and attendees were offered financial rewards for their participation. Drama appears to be an effective means of engaging young people in discussions around asthma.16 Nonetheless, we were unable to effectively engage young people in this one-off event. Previous codesign workshops involving young people have relied on prior cultivation of strong relationships between researchers and young people10 or have been performed in a school setting.14 Unfortunately, we lacked the human and financial resources to support intense contact between members of our team and young people before the workshop date.
Our paediatric population is ethnically diverse and the region is notable for significant income inequalities.17 These social factors influence health literacy18 and in turn, engagement with health services.19 Our findings may not be generalisable to rural areas with more homogeneous patient populations.
Despite these limitations, this study adds weight to the observation that the current system is fragmented.8 Patients are placed at risk of becoming caught in cycles of asthma exacerbations while missing out on proactive care. Workshop participants identified chaotic family lifestyles as an important barrier impeding access to care. Disruptive family life is associated with poor asthma control in ethnic minority children living in urban areas.20 The current system—reliant on young people and their parents proactively seeking attention if asthma control deteriorates—may disadvantage vulnerable children with limited support.
Workshop participants also emphasised the importance of improving MDT communication, particularly when clinical responsibility is transferred between teams. The NRAD identified several fatalities in children who were not followed up in primary care after a recent attendance with an acute asthma attack at their local emergency department.3 This underpins the recommendations that every NHS general practice has a named clinical lead for asthma and that all children requiring emergency treatment for an asthma attack are reviewed by their GP within 48 hours of discharge. Many GPs expressed dismay at delays in processing hospital discharge summaries, which prevents them from meeting this important target. We propose that prior to discharge, hospital doctors contact this named GP directly to arrange timely follow-up.
GPs were hesitant to remove patients from their asthma registries due to medicolegal concerns. Participants also expressed a desire to clearly allocate responsibility for a young person’s care to a named GP or paediatrician. We propose that regular MDT meetings involving GPs, paediatricians and specialist nurses would represent an ideal forum interprofessional education and asthma registry reviews. A similar pilot study in adults with chronic diseases has won national acclaim.21 Patients showing signs of deteriorating asthma control at the time of registry review could be referred appropriately to secondary care, and GPs and Paediatricians could develop individualised plans to ease a patient’s transition between children’s and adult services. The development of primary care networks across England—collaborations involving general practices, pharmacists and social care providers, serving 30–50 000 people—offers a unique opportunity to expand this model at scale.
Discussions highlighted the importance of school nurses in routine asthma care. They are often the first health professionals to identify signs of deteriorating asthma control in young people and can facilitate access for clinicians seeking to deliver asthma education and routine care to young people in a school setting. Nonetheless, several GPs attending the workshop had never met a school nurse before, exemplifying the poor integration of this group into the wider MDT. School nurses attending the workshop recognised that they were highly dependent on non-clinically trained first aiders. Measures seeking to address the complacency around asthma might be better targeted at non-healthcare professionals.
Our experience suggests that traditional methods of invitation and financial rewards are not sufficient to engage young people in one-off codesign events. Future coproduction strategies should emphasise regular contact between researchers and young people to build trust and give young people an equal voice. Nonetheless, this qualitative study confirms the value of SqS as a tool for engaging health professionals and generating tractable change ideas for health system improvement.
Acknowledgments
We thank Sharon-Marie Weldon and Camilla March for their help in designing and executing an accurate simulation. We also thank Bob Klaber (REK) and David Mummery (DM) for facilitating group discussions, and Amer Al-Balah and Nour Houbby for their help in transcribing and encoding recorded material.
Footnotes
Contributors: All authors were involved in the development of the simulation and workshop. MF and CC performed independent thematic analyses of the transcribed data. MF wrote the first draft, which was critically revised for important intellectual content by CC, EM and MW. MF, CC and EM contributed equally to this paper. All authors approve the final version of the manuscript.
Funding: CC and EM received small grants worth £800 and £375, respectively, from the National Institute for Health Research, via the Imperial College London Biomedical Research Centre Small Grants Fund. Funds were used to provide expendables on the day and to incentivise CYP to participate in the initial semi-structured interviews and sequential simulation. AI’s position was supported by a grant from the Imperial Health Charity.
Competing interests: MW is cofounder of Connecting Care for Children, an organisation that promotes integrated child health.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
The results of this study are underpinned by transcribed recordings made during post-simulation discussions. Deidentified, encoded transcriptions are available on reasonable request. Data will be made available to researchers who provide a methodologically sound proposal and where data will allow them to achieve their stated aims. Data will be available from immediately after publication to five years after publication. Proposals should be directed to charles.coughlan@nhs.net.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This project was discussed with the Research Ethics Committees at Imperial College London and Imperial College Healthcare NHS Trust. Both committees advised that formal research ethics were not required. After consultation with the Trust’s Caldicott Guardian, approval was granted for a service evaluation.
References
- 1. Asthma UK . Asthma facts and statistics, 2019. Available: https://www.asthma.org.uk/about/media/facts-and-statistics/ [Accessed 23 July 2019].
- 2. Asthma UK . UK asthma death rates among worst in Europe, asthma UK. Available: https://www.asthma.org.uk/about/media/news/press-release-uk-asthma-death-rates-among-worst-in-europe/ [Accessed 8 May 2019].
- 3. Royal College of Physicians . Why asthma still kills: the National review of asthma deaths (NRAD) Confidential enquiry report. London: RCP, 2014. [Google Scholar]
- 4. Rhee H, Belyea MJ, Halterman JS. Adolescents' perception of asthma symptoms and health care utilization. J Pediatr Health Care 2011;25:105–13. 10.1016/j.pedhc.2009.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Naimi DR, Freedman TG, Ginsburg KR, et al. Adolescents and asthma: why bother with our meds? J Allergy Clin Immunol 2009;123:1335–41. 10.1016/j.jaci.2009.02.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kim B, White K. How can health professionals enhance interpersonal communication with adolescents and young adults to improve health care outcomes?: systematic literature review. Int J Adolesc Youth 2018;23:198–218. 10.1080/02673843.2017.1330696 [DOI] [Google Scholar]
- 7. Holley S, Walker D, Knibb R, et al. Barriers and facilitators to self-management of asthma in adolescents: an interview study to inform development of a novel intervention. Clin Exp Allergy 2018;48:944–56. 10.1111/cea.13141 [DOI] [PubMed] [Google Scholar]
- 8. Levy ML, Fleming L, Warner JO, et al. Paediatric asthma care in the UK: fragmented and fatally fallible. Br J Gen Pract 2019;69:405–6. 10.3399/bjgp19X704933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. National Institute for Health and Care Excellence . Quality and outcomes framework indicators. Available: www.nice.org.uk/standards-and-indicators/qofindicators [Accessed 08 May 2020].
- 10. Hackett CL, Mulvale G, Miatello A. Co-designing for quality: creating a user-driven tool to improve quality in youth mental health services. Health Expect 2018;21:1013–23. 10.1111/hex.12694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Weldon SM, Kelay T, Ako E, et al. Sequential simulation used as a novel educational tool aimed at healthcare managers: a patient-centred approach. BMJ Simulation and Technology Enhanced Learning 2018;4:13–18. 10.1136/bmjstel-2017-000216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Weldon SM, Ralhan R, Paice E, et al. Sequential simulation (SqS): an innovative approach to educating GP receptionists about integrated care via a patient journey. Biomed Central J Fam Pract 2015;16:108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Imran A, Holden B, Weldon SM, et al. ‘How to help your unwell child’: a sequential simulation project. BMJ Simulation and Technology Enhanced Learning 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Powell P, Sorefan Z, Hamilton S, et al. Exploring the potential of sequential simulation. Clin Teach 2016;13:112–8. 10.1111/tct.12391 [DOI] [PubMed] [Google Scholar]
- 15. Montgomery-Taylor S, Watson M, Klaber R. Child health general practice hubs: a service evaluation. Arch Dis Child 2016;101:333–7. 10.1136/archdischild-2015-308910 [DOI] [PubMed] [Google Scholar]
- 16. Mosler G, Euba T. Taking control through drama. Lancet 2018;391:303–4. 10.1016/S0140-6736(17)32283-3 [DOI] [PubMed] [Google Scholar]
- 17. London Borough of Hammersmith and Fulham . Joint strategic needs assessment highlights report 2013-14. available at. Available: https://www.lbhf.gov.uk/sites/default/files/Joint_Strategic_Needs_Assessment_2013-2014.pdf [Accessed 09 May 2020].
- 18. Ferguson LA, Pawlak R, literacy H. The road to improved health outcomes. The Journal for Nurse Practitioners 2011;7:123–9. [Google Scholar]
- 19. Tzeng Y-F, Chiang B-L, Chen Y-H, et al. Health literacy in children with asthma: A systematic review. Pediatr Neonatol 2018;59:429–38. 10.1016/j.pedneo.2017.12.001 [DOI] [PubMed] [Google Scholar]
- 20. Weinstein SM, Pugach O, Rosales G, et al. Family chaos and asthma control. Pediatrics 2019;144. 10.1542/peds.2018-2758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hawkes N. The BMJ awards: education team of the year. BMJ 2018;361:k1519. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The results of this study are underpinned by transcribed recordings made during post-simulation discussions. Deidentified, encoded transcriptions are available on reasonable request. Data will be made available to researchers who provide a methodologically sound proposal and where data will allow them to achieve their stated aims. Data will be available from immediately after publication to five years after publication. Proposals should be directed to charles.coughlan@nhs.net.