Abstract
This review will present developments in simulation-based education (SBE) over the past decade with a focus on activity in the UK’s National Health Service and the role of the national society (the Association for Simulation Practice in Healthcare). The article covers the evolution of strategic changes for the use of SBE in the UK and the operational challenges faced by clinicians and other faculty in SBE. The expansion of the evidence base to support SBE in healthcare both in technical skills and, more broadly, in interprofessional team training is explored. Finally, the wider role of simulation in patient safety and healthcare systems, including testing pathways and the development of cognitive aids and involvement of patients in SBE is considered.
Keywords: simulation based education, simulation faculty, patient safety
Introduction
Isn’t it funny how day by day nothing changes, but when you look back everything is different.
(C.S. Lewis)
Simulation-based education (SBE) is now accepted in the UK and worldwide as an integral part of the armamentarium of an educator in healthcare but it has taken over 50 years since the first publications describing computer-driven manikins1 for it to gain this recognition. The Association for Simulated Practice in Healthcare (ASPiH www.aspih.org.uk) was 10 years old in November 2019 and it seems an appropriate moment to pause and reflect on achievements from the past and consider opportunities for the future.
ASPiH was formed as a union of the National Association of Medical Simulation and the Clinical Skills Network in 2009. This resulted in a properly interdisciplinary organisation based on a fundamental ethos of ASPiH namely, the development of interprofessional SBE. ASPiH’s stated mission is to ‘promote and support simulation based education and technology enhanced learning (TEL) in the pursuit of best practice for our patients, learners and partners’. Underpinning this mission are aims which focus on delivery of effective communication networks; providing a resource for expertise in SBE and TEL; supporting expansion of SBE; sharing resources and encouraging research and innovative practice.
This article will consider strategic and operational developments in SBE in the UK (expanding on a recent conference keynote lecture and editorial2) and present evidence of its value as an educational tool and, more widely, its role in systems analysis and patient safety.
Strategic developments in SBE
National strategies around SBE have followed a similar trajectory to ASPiH in their focus on implementation of experiential training for healthcare professionals through faculty development and interprofessional education. In 2008, Sir Liam Donaldson, England’s Chief Medical Officer (CMO) included a chapter on simulation in his 150th anniversary report. He stated that, ‘…simulation works. Simulation is important to medicine. The NHS must be able to provide the type of simulation that would make a difference to patients like Elaine Bromiley’. Evidence to support the value of SBE in healthcare was probably not as robust as suggested at the time of this report but resonated with the strongly held convictions of educators in SBE which were crystallised by David Gaba’s words in 1992:3 ‘no industry in which human lives depend on the skilled performance of responsible operators has waited for unequivocal proof of the benefits of simulation before embracing it’. SBE is arguably an expensive form of training however, and evidence to support its value in healthcare is vital if funding is to expand in the resource constrained setting of the NHS. Fortunately, research over the past two decades has led to an abundance of such evidence which will be explored below.
Dame Sally Davies succeeded Liam Donaldson as CMO in 2011 and, in the same year, contributed to the new Framework for Technology Enhanced Learning in which she asserted: ‘Simulation in particular allows teams to practise safely and reduces the risk of complications for patients’ and that ‘…this framework clearly states that healthcare professionals, as part of a managed learning process and where appropriate, should learn skills together in a simulation environment and using other technologies before undertaking them in supervised clinical practice’. Subsequent reports and guidance documents have presented similar arguments4–7 and have culminated in Health Education England’s (HEE) publication of a National Framework for Simulation-Based Education in 20188 and the new National Safety Curriculum due to be published in March 2020.
ASPiH’s role during this time has been to work alongside national commissioning bodies (such as HEE) along with other strategic stakeholders, and partners in healthcare, higher education and industry who are involved in SBE to guide its development and implementation across the NHS. ASPiH’s early work on scoping activity in SBE around the UK (the National Simulation Development Project, NDSP9) was a joint project with HEE and the Higher Education Authority and provided vital information on the scale of SBE activity around the country. More importantly, it revealed important barriers to the delivery of simulation training, the most obvious of which is support for faculty in SBE.
Faculty development
Educators in healthcare have always faced challenges in the delivery of training not least of which is time.10 The NDSP revealed a number of key issues for faculty in SBE across the UK.
Variability in support, either funding or time, leading to limited availability of multidisciplinary faculty in SBE.
Limited and non-standardised training for development of novice and experienced faculty.
Lack of standards and quality assurance in the provision of SBE (the first standards for SBE were published in 2011 by the International Nursing Association of Clinical Simulation and Learning in North America).
Lack of networking opportunities to compare and share good practice in SBE.
Alongside these specific issues in SBE are more generic problems for educators in healthcare. These include the difficulties of delivering training to staff who have limited time allocated for education and delivering training that supports safe care for increasingly complicated patients in highly complex care pathways. Furthermore, the rate of doubling of medical knowledge is set to decrease to just 73 days this year11 presenting a formidable challenge for faculty in staying up to date.
ASPiH has sought to provide answers to some of these problems in the UK by focusing on faculty development through the following:
Enabling access to expert groups and novel research via ASPiH’s website.
Providing free access to an online scenario design platform (iRIS http://irissimulationauthoring.com).
Improving access to communities of practice, commissioners and providers of SBE and industry partners at national and regional events.
Providing support for training of novice and experienced faculty at regional and national events. Most recently, in collaboration with HEE, ASPiH is piloting an entry level faculty development programme in SBE which has already been validated in Australia.12
Designing and publishing national standards for SBE, in collaboration with HEE (https://aspih.org.uk/standards-framework-for-sbe/).
Administering a cost-effective accreditation process for faculty, educational programmes and simulation facilities (https://aspih.org.uk/accreditation/).
Faculty development in SBE will be vital to the success of implementing the new Framework for SBE and the National Safety Curriculum. However, despite obvious progress in the past decade substantial work remains to be done against a backdrop of significant workforce deficits.
Evidence to support the use of SBE in healthcare education
The role of simulation as a tool for educating healthcare professionals has expanded dramatically over the past decade since the advent of ASPiH, along with the evidence to support its value. McGaghie’s 2014 review13 points out that: ‘Medical education research spanning at least four decades demonstrates that simulation technology, used under the right conditions …. can have large and sustained effects on knowledge and skill acquisition and maintenance among medical learners…. Despite their methodological differences, these reviews all conclude that SBME (Simulation Based Medical Education) is highly effective, especially in comparison with no-treatment (placebo) conditions14 and traditional clinical education’.15
Any professional, academic organisation seeking to advance their field of interest and share research and innovative practice benefits from the availability of a peer-reviewed journal as a platform for discussion and debate. ASPiH’s most recent contribution to the evidence base in SBE has been to facilitate publication of research by launching a new journal in 2014 in collaboration with the BMJ group: BMJ Simulation and Technology Enhanced Learning.
Evidence to support the use of SBE for training technical skills
Evidence to support the use of part-task trainers to expedite technical skill acquisition is now plentiful.13 15 16 Core skills, including lumbar puncture, laparoscopy and central venous line insertion, have been studied revealing significant differences in technical skills (including improved sterility and correct use of manometer equipment for lumbar puncture, reduced procedural error rates in laparoscopy and fewer needle passes to correct central venous catheter insertion) as well as a reduction in catheter-related sepsis.17–20
While the value of simulation for training in technical skills has become clear, measuring the value of experiential learning for multidisciplinary team training using SBE is far more challenging. Fortunately, evidence to support this type of training to improve performance for teams in many clinical settings is now available.
Evidence to support the use of SBE for training non-technical skills
Errors in non-technical skills such as teamwork, communication and decision making are more commonly implicated in critical incidents in healthcare than technical skills.21 A recent review of team training in healthcare highlighted the upsurge in publications on the subject over the past decade. It also found that programmes (incorporating simulated practice) delivered significant improvements in team performance, medication and transfusion error and patient outcomes.22 Not surprisingly, this review also found that the value of SBE for team training was greatly enhanced by providing additional support after the intervention (eg, training in quality improvement methods; leadership training and ongoing assessment of training outcomes in the workplace to reinforce learning). Valid criticisms have been levelled at the design, implementation and analysis of team training interventions in healthcare in the past.23–25 However, evidence from medical centres where standardised programmes of team training (incorporating simulation) were implemented have shown significant benefits in terms of patient outcomes including surgical morbidity and mortality.26–30 One of the significant challenges faced by educators in SBE is the measurement of team performance with non-technical skills assessment tools which are neither straightforward to use nor presented in a standardised format.31 There are currently over 76 tools available for a wide variety of contexts32 from operating theatres to palliative care. Such a bewildering array is unhelpful and off-putting for faculty and does not support educators in improving team performance in healthcare.
No healthcare professional works in isolation but teams are formed on a much more ad hoc basis in clinical settings than was the case before the advent of changes designed, for example, to reduce junior doctors hours of work. These changes have brought home the fact that good teamwork cannot be seen as simply a natural product of working together with familiar colleagues, but must be embedded in the wider healthcare system. Multidisciplinary healthcare professionals are expected to perform efficiently and effectively with very little of the routine, regular training which is provided to support teams in high reliability organisations (HROs). There is unlikely to be a significant impact on avoidable harm in healthcare unless we adopt a similar approach to team training.33
The role of simulation in patient safety
Incident analysis in healthcare
Despite over three decades of increasing focus on patient safety, there has not been widely sustained change or system wide evidence of improvement in the reliability of healthcare systems.34 35 Some of the responsibility for failures to learn from error must be apportioned to the way healthcare incidents are investigated. A Parliamentary Select Committee report in 2015 highlighted that, ‘processes for investigating and learning from incidents, take far too long and are preoccupied with blame or avoiding financial liability’.36 The paradigm shift which has occurred in HROs such that the focus is on the ‘how’ rather than the ‘who’ of an incident has yet to happen in healthcare. It is only by constantly seeking out vulnerabilities in systems of work that we can hope to enact meaningful improvements.37 HROs have spent decades developing robust, standardised systems of investigating incidents including the establishment of truly independent expert investigative bodies (such as the UK’s Air Accident Investigation Branch https://www.gov.uk/government/organisations/air-accidents-investigation-branch). Healthcare has learnt from some of these lessons and in April 2017, the Healthcare Safety Investigation Branch was established in the NHS (https://www.hsib.org.uk) with the stated purpose of ‘improving patient safety through effective and independent investigations that don’t apportion blame or liability’. Their work has only just begun but will draw on existing expertise in the NHS to capture the widely shared ambition of learning from the past to improve the future.
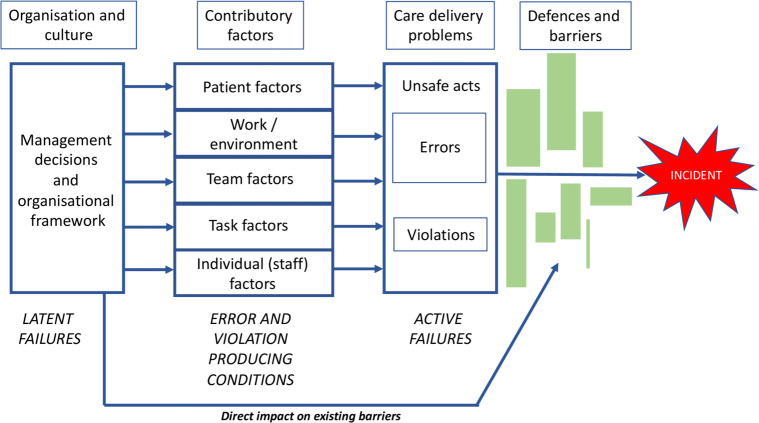
A human factors-based process of incident analysis provides a far richer understanding of the systems, process and behavioural problems that lead to errors. Major incidents almost always evolve over time (sometimes years) and involve multiple team interactions and other environmental and cultural contributory factors. An organisational model of accidents can be very helpful in ‘unpacking’ what went wrong and, more importantly what might be done to prevent a recurrence. Charles Vincent has described such a model (figure 1) where a variety of contributory factors combine, leaving the human at the sharp end of the final catastrophe as ‘the inheritor rather than the instigator’ of the sequence of events.38 His subsequent framework for incident analysis (the London Protocol)39 is a useful scaffold for delivering holistic reports on adverse incidents. Once all the contributory factors from a critical incident are revealed, subsequent intelligent intervention design (including SBE) will be far more likely to lead to improved processes of care and safety.
Figure 1.
Organisational accident model (adapted with permission from Vincent C; Patient Safety 2010. Wiley-Blackwell). Adverse incidents in healthcare evolve as a result of a combination of organisational, systems, environmental and team problems. Errors and violations are subcategories of unsafe acts. Defences and barriers take many forms (eg, they may be physical or procedural and exist at different points along a patient pathway) and erroneous managerial decisions and existing organisational problems may impact the evolution of an adverse incident directly or indirectly.
Simulation as a tool for analysis of healthcare systems
Simulation is now embedded in healthcare education but its use for analysis of clinical systems and standard operating procedures is in its infancy and continues to focus on the skills and behaviours of healthcare practitioners. There is growing evidence of the benefits of using simulation to analyse patient pathways and novel devices or procedures, although this can be challenging when conducted in busy work environments.40 41 Simple table top exercises or computer simulations (including the use of virtual reality), away from the real clinical environment, can provide a safe solution to such testing in these more complex, dynamic conditions.
The use of simulation either as a tool for training or for analysing procedures or pathways may be recommended after critical incidents in healthcare. However, the Canadian Incident Analysis Framework42 describes a hierarchy of interventions which may cast doubt on the value of training as a useful tool to prevent error. In table 1 training is depicted as a ‘weaker intervention’ but this is largely because training per se would not alter the conditions in which the incident occurred and training interventions in healthcare are not implemented with best evidence in mind.43–45 Multimodal low-dose, high-frequency educational interventions are more likely to lead to skill retention and have been shown to improve outcomes and yet, despite the evidence, use of the least effective techniques (eg, didactic programmes) persists in healthcare. This same hierarchy places cognitive aids, such as checklists, above training as robust interventions to improve safety. However, it must be recognised that the use of checklists is not intuitive46 47 and implementation must be supported by awareness raising and team training (including simulation) in their use.
Table 1.
Examples of potential interventions (from the Canadian Incident Analysis Framework41) graded according to effectiveness in preventing recurrence of a similar incident
| Recommended hierarchy of actions | |
| Stronger actions |
|
| Intermediate actions |
|
| Weaker actions |
|
The is table/figure is freely available at https://www.patientsafetyinstitute.ca for reuse and publication.
A growing academic and professional interest in resilience within organisations is becoming apparent in the current financially challenging circumstances for the delivery of healthcare. We must understand more clearly how healthcare can be delivered in a more efficient and effective manner despite the complexities and constraints that present such challenging conditions. One theme emerging within organisational resilience literature is the concept of ‘Safety 1 vs Safety 2’.48 The traditional approach to patient safety (safety 1) has been to focus on the analysis of factors contributing to the evolution of serious incidents and to share learning across organisations. An alternative (safety 2) approach considers how things ‘go right’ and focuses on the adaptability and flexibility that the system demonstrates to avoid untoward events or their consequences. Reason has referred to the ‘human as hero’ in most workplace activities; we are far more likely to detect a problem and intervene to prevent harm than we are to cause errors.49 Appreciative inquiry is coming to fore as a technique to explore what is going well in a system and extrapolate the learning to other areas. It is a technique widely used in business and industry50 and one that is emerging in healthcare51 52 with obvious implications for simulated practice.
Public and patient involvement in SBE
This final section will consider public and patient involvement in SBE, an area that has been a strategic objective of ASPiH’s for the past 5 years. For the first time in 2019, ASPiH’s national conference was accredited as ‘Patients Included’(the charter can be found at: https://patientsincluded.org/conferences/). While we celebrated the achievement, we also recognised the challenges of ensuring meaningful involvement of patients and carers in our work. Policies aimed at improving public engagement in the NHS can be traced back to 1990 at the point of introduction of the internal market and patient choice. However, it is widely recognised that implementation of effective and sustained patient involvement in healthcare policy at any level is patchy and ill-formed.53 54 This is as true in healthcare education (including SBE) as it is for clinical contexts although it may be hoped that fewer barriers to engagement might exist in the training arena. Ocloo and Matthews described a continuum of engagement from more peripheral consultation of patients to partnership and shared leadership roles.54 Patients and carers have spoken at ASPiH’s conferences, led workshops, engaged with and advised our executive committee and judged research in SBE. The organisation has moved away from more tokenistic approaches to patient engagement; the next step will be formal patient representation on the executive committee with close involvement in strategic decisions, a clear goal for the coming years.
Conclusion
This article has presented several key developments in SBE in the UK over the past decade and highlighted some challenges for the future. The role of ASPiH has been integral in embedding innovative educational practices incorporating simulation more widely in the NHS. The importance of providing experiential learning opportunities for healthcare staff and supporting the faculty who provide them has been highlighted. However, challenges persist in both levels of staffing and, as a corollary, availability of simulation faculty. A recent review of the healthcare workforce by the Health Foundation, the King’s Fund and the Nuffield Trust55 revealed that ‘the workforce challenges in the NHS in England now present a greater threat to health services than the funding challenges’ and this view was reinforced in Lord Darzi’s report, ‘Better Health and Care for All’ in which he highlights that 11% of nursing posts, 12% of GP posts and 5% of medical consultant posts are unfilled.56 Against this backdrop of inadequate staffing and the recognition that the NHS has been subject to repeated cycles of feast and famine in funding, the report recommends that funding to the NHS should be increased but that it should be provided more efficiently such that long-term investments, rather than short-term fixes, are possible.
The past two decades of increasingly obvious research and public scrutiny into patient safety provide the impetus, despite funding constraints, for the development of sustainable simulation-based interventions in training or system testing as an essential requirement for safer healthcare. The challenge for our community in SBE will be to ensure the tools we use routinely in our simulation centres are more widely employed across healthcare systems. This review of the past decade would suggest that, despite formidable barriers, we can achieve this goal.
Acknowledgments
This article was written prior to the COVID-19 pandemic and revised when it was reaching its peak in the UK. I have never been more impressed and awed by my colleagues and friends in healthcare than during this time. COVID-19 has presented unparalleled challenges for all of us but never has the importance of the use of simulation to support staff in dealing with uncertainty and pressure been more obvious. All of the educational materials we have developed since the beginning of the pandemic are free to access at: www.oxstar.ox.ac.uk/covid-19. The author wishes to acknowledge and thank the ASPiH executive and the wider SBE community in the UK and internationally for 10 incredibly rewarding years working to promote simulation in healthcare.
Footnotes
Twitter: @HelenEHigham
Contributors: Dr Higham was solely responsible for the content, revisions, final approval and accountability for this review article.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: The author is the immediate Past President of the Association for Simulated Practice in Healthcare and remained a member of the executive committee until January 2020.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data sharing not applicable as no data sets generated and/or analysed for this study. N/A.
Ethics statements
Patient consent for publication
Not required.
References
- 1. Cooper JB, Taqueti VR. A brief history of the development of mannequin simulators for clinical education and training. Qual Saf Heal Care 2004;13:563–70. 10.1136/qshc.2004.009886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Higham H, Morrow M, Laws-Chapman C, et al. The role of ASPiH in simulation-based education. Bmj Stel 2019;5:A3–4. 10.1136/bmjstel-2019-000535 [DOI] [Google Scholar]
- 3. Gaba DM. Improving anesthesiologists' performance by simulating reality. Anesthesiology 1992;76:491–4. [PubMed] [Google Scholar]
- 4. Health Education England . Delivering patient safety through education, training and development, 2016. Available: https://www.hee.nhs.uk/sites/default/files/documents/Improvingsafetythrougheducationandtraining.pdf
- 5. Commission on Education and Training for Patient Safety . Improving safety through education and training, 2016. Available: www.hee.nhs.uk/the-commission-on-education-and-training-for-patient-safety
- 6. Yu A, Flott K, Chainani N, et al. Patient Safety 2030.. Available: www.imperial.ac.uk/patient-safety-translational-research-centre
- 7. NHS England, NHS Improvement . The NHS patient safety strategy safer culture, safer systems, safer patients., 2019. Available: https://improvement.nhs.uk/documents/5472/190708_Patient_Safety_Strategy_for_website_v4.pdf
- 8. Health Education England . National Framework for Simulation Based Education (SBE) [Internet], 2018. Available: https://www.hee.nhs.uk/sites/default/files/documents/Nationalframeworkforsimulationbasededucation.pdf
- 9. Anderson A, Baxendale B, Scott L, et al. The National simulation development project: summary report. Available: http://aspih.org.uk/wp-content/uploads/2017/07/national-scoping-project-summary-report.pdf
- 10. Moonesinghe SR, Lowery J, Shahi N, et al. Impact of reduction in working hours for doctors in training on postgraduate medical education and patients' outcomes: systematic review. BMJ 2011;342:d1580. 10.1136/bmj.d1580 [DOI] [PubMed] [Google Scholar]
- 11. Densen P. Challenges and opportunities facing medical education. Trans Am Clin Climatol Assoc 2011;122:48–58. [PMC free article] [PubMed] [Google Scholar]
- 12. Nestel D, Bearman M, Brooks P, et al. A national training program for simulation educators and technicians: evaluation strategy and outcomes. BMC Med Educ 2016;16:25. 10.1186/s12909-016-0548-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. McGaghie WC, Issenberg SB, Barsuk JH, et al. A critical review of simulation-based mastery learning with translational outcomes. Med Educ 2014;48:375–85. 10.1111/medu.12391 [DOI] [PubMed] [Google Scholar]
- 14. Cook DA, Hatala R, Brydges R, et al. Technology-Enhanced simulation for health professions education. JAMA 2011;306:978–88. 10.1001/jama.2011.1234 [DOI] [PubMed] [Google Scholar]
- 15. McGaghie WC, Issenberg SB, Cohen ER, et al. Does simulation-based medical education with deliberate practice yield better results than traditional clinical education? A meta-analytic comparative review of the evidence. Acad Med 2011;86:706–11. 10.1097/ACM.0b013e318217e119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Scalese RJ, Obeso VT, Issenberg SB. Simulation technology for skills training and competency assessment in medical education. J Gen Intern Med 2008;23:46–9. 10.1007/s11606-007-0283-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Barsuk JH, Cohen ER, Feinglass J, et al. Use of simulation-based education to reduce catheter-related bloodstream infections. Arch Intern Med 2009;169:1420. 10.1001/archinternmed.2009.215 [DOI] [PubMed] [Google Scholar]
- 18. Barsuk JH, McGaghie WC, Cohen ER, et al. Use of simulation-based mastery learning to improve the quality of central venous catheter placement in a medical intensive care unit. J Hosp Med 2009;4:397–403. 10.1002/jhm.468 [DOI] [PubMed] [Google Scholar]
- 19. Barsuk JH, Cohen ER, Caprio T, et al. Simulation-Based education with mastery learning improves residents' lumbar puncture skills. Neurology 2012;79:132–7. 10.1212/WNL.0b013e31825dd39d [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gallagher AG, Seymour NE, Jordan-Black J-A, et al. Prospective, randomized assessment of transfer of training (TOT) and transfer effectiveness ratio (TER) of virtual reality simulation training for laparoscopic skill acquisition. Ann Surg 2013;257:1025–31. 10.1097/SLA.0b013e318284f658 [DOI] [PubMed] [Google Scholar]
- 21. Flin R, O’Connor P, Crichton M. Chapter 2: Safety at the sharp end: A guide to non-technical skills. In: Safety at the sharp end: a guide to non-technical skills, 2008: 17–40. [Google Scholar]
- 22. Weaver SJ, Dy SM, Rosen MA. Team-training in healthcare: a narrative synthesis of the literature. BMJ Qual Saf 2014;23:359–72. 10.1136/bmjqs-2013-001848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Weaver SJ, Lyons R, DiazGranados D, et al. The anatomy of health care team training and the state of practice: a critical review. Acad Med 2010;85:1746–60. 10.1097/ACM.0b013e3181f2e907 [DOI] [PubMed] [Google Scholar]
- 24. Salas E, Rosen MA. Building high reliability teams: progress and some reflections on teamwork training. BMJ Qual Saf 2013;22:369–73. 10.1136/bmjqs-2013-002015 [DOI] [PubMed] [Google Scholar]
- 25. Grand JA, Pearce M, Rench TA, et al. Going deep: guidelines for building simulation-based team assessments. BMJ Qual Saf 2013;22:436–48. 10.1136/bmjqs-2012-000957 [DOI] [PubMed] [Google Scholar]
- 26. Neily J, Mills PD, Young-Xu Y, et al. Association between implementation of a medical team training program and surgical mortality. JAMA 2010;304:1693. 10.1001/jama.2010.1506 [DOI] [PubMed] [Google Scholar]
- 27. Armour Forse R, Bramble JD, McQuillan R. Team training can improve operating room performance. Surgery 2011;150:771–8. 10.1016/j.surg.2011.07.076 [DOI] [PubMed] [Google Scholar]
- 28. Deering S, Rosen MA, Ludi V, et al. On the front lines of patient safety: implementation and evaluation of team training in Iraq. Jt Comm J Qual Patient Saf 2011;37:350–1. 10.1016/S1553-7250(11)37045-6 [DOI] [PubMed] [Google Scholar]
- 29. Riley W, Davis S, Miller K, et al. Didactic and simulation nontechnical skills team training to improve perinatal patient outcomes in a community hospital. Jt Comm J Qual Patient Saf 2011;37:357–64. 10.1016/S1553-7250(11)37046-8 [DOI] [PubMed] [Google Scholar]
- 30. Young-Xu Y, Neily J, Mills PD, et al. Association between implementation of a medical team training program and surgical morbidity. Arch Surg 2011;146:1368. 10.1001/archsurg.2011.762 [DOI] [PubMed] [Google Scholar]
- 31. Johnson AP, Aggarwal R. Assessment of non-technical skills: why aren't we there yet? BMJ Qual Saf 2019;28:606–8. 10.1136/bmjqs-2018-008712 [DOI] [PubMed] [Google Scholar]
- 32. Higham H, Greig PR, Rutherford J, et al. Observer-based tools for non-technical skills assessment in simulated and real clinical environments in healthcare: a systematic review. BMJ Qual Saf 2019;28:672–86. 10.1136/bmjqs-2018-008565 [DOI] [PubMed] [Google Scholar]
- 33. Higham H, Baxendale B. To err is human: use of simulation to enhance training and patient safety in anaesthesia. Br J Anaesth 2017;119:i106–14. 10.1093/bja/aex302 [DOI] [PubMed] [Google Scholar]
- 34. Vincent C, Amalberti R. Safer healthcare : strategies for the real world. Springer Open 2016:157. [PubMed] [Google Scholar]
- 35. Makary MA, Daniel M. Medical error-the third leading cause of death in the US. BMJ 2016;353:i2139. 10.1136/bmj.i2139 [DOI] [PubMed] [Google Scholar]
- 36. House of Commons Public Administration Select Committee . Investigating clinical incidents in the NHS (HC886), 2015. Available: https://publications.parliament.uk/pa/cm201415/cmselect/cmpubadm/886/886.pdf
- 37. Woods DD, Dekker SWA, Cook R, et al. Behind human error. Ashgate, 2010: 271. [Google Scholar]
- 38. Vincent C. Patient safety. 2nd ED. Wiley-Blackwell Publishing Ltd, 2010. [Google Scholar]
- 39. Taylor-Adams S, Vincent C. Systems analysis of clinical incidents: the London protocol. Clin Risk 2004;10:211–20. 10.1258/1356262042368255 [DOI] [Google Scholar]
- 40. Patterson MD, Geis GL, Falcone RA, et al. In situ simulation: detection of safety threats and teamwork training in a high risk emergency department. BMJ Qual Saf 2013;22:468–77. 10.1136/bmjqs-2012-000942 [DOI] [PubMed] [Google Scholar]
- 41. Macrae C, Draycott T. Delivering high reliability in maternity care: in situ simulation as a source of organisational resilience. Saf Sci 2016;117. [Google Scholar]
- 42. Hoffman C, Beard P, Greenall J UD, et al. Canadian root cause analysis framework, 2006. Available: http://www.patientsafetyinstitute.ca/en/toolsResources/IncidentAnalysis/Documents/CanadianIncidentAnalysisFramework.PDF
- 43. Bluestone J, Johnson P, Fullerton J, et al. Effective in-service training design and delivery: evidence from an integrative literature review. Hum Resour Health 2013;11:51. 10.1186/1478-4491-11-51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Bloom BS. Effects of continuing medical education on improving physician clinical care and patient health: a review of systematic reviews. Int J Technol Assess Health Care 2005;21:380–5. 10.1017/S026646230505049X [DOI] [PubMed] [Google Scholar]
- 45. Drake M, Bishanga DR, Temu A, et al. Structured on-the-job training to improve retention of newborn resuscitation skills. BMC Pediatr 2019;19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Catchpole K, Russ S. The problem with checklists. BMJ Qual Saf 2015;24:545–9. 10.1136/bmjqs-2015-004431 [DOI] [PubMed] [Google Scholar]
- 47. Weiser TG, Haynes AB. Ten years of the surgical safety checklist. Br J Surg 2018;105:927–9. 10.1002/bjs.10907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Hollnagel E. Safety-I and safety-II : the past and future of safety management. CRC Press, 2014: 187. [Google Scholar]
- 49. Reason JT. The human contribution : unsafe acts, accidents and heroic recoveries. Ashgate, 2008: 295 [Google Scholar]
- 50. Watkins JM, Mohr BJ, Kelly R. Appreciative inquiry : change at the speed of imagination. Pfeiffer 2011:318.
- 51. Trajkovski S, Schmied V, Vickers M, et al. Using appreciative inquiry to transform health care. Contemp Nurse 2013;45:95–100. 10.5172/conu.2013.45.1.95 [DOI] [PubMed] [Google Scholar]
- 52. Sandars J, Murdoch-Eaton D. Appreciative inquiry in medical education. Med Teach 2017;39:123–7. 10.1080/0142159X.2017.1245852 [DOI] [PubMed] [Google Scholar]
- 53. Florin D, Dixon J. Public involvement in health care. BMJ 2004;328:159–61. 10.1136/bmj.328.7432.159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Ocloo J, Matthews R. From tokenism to empowerment: progressing patient and public involvement in healthcare improvement. BMJ Qual Saf 2016;25:626–32. 10.1136/bmjqs-2015-004839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. The King’s Fund . The healthcare workforce in England. London: The King’s Fund, 2018. https://www.kingsfund.org.uk/publications/health-care-workforce-england [Google Scholar]
- 56. Darzi L. Better health and care for all, 2018. Available: www.ippr.org
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable as no data sets generated and/or analysed for this study. N/A.