Abstract
The COVID-19 pandemic is posing new challenges for medical education and simulation practice given local social distancing requirements.
This report describes the use of an online platform for rapid cycle deliberate practice simulation training that can be used and tailored to local COVID-19 pandemic restrictions as it allows for participants, facilitators and simulation equipment to be apart.
Keywords: simulation, screen based (virtual patient), emergency paediatrics, computer simulation, e-learning
Introduction
The COVID-19 pandemic has changed how simulation-based training can be delivered providing learners with a safe learning environment. Telesimulation is an established modality of simulation-training delivery and has been evolving over the past years to accommodate local challenges.1 Traditionally, telesimulation has been conducted with learners and facilitators in separate locations while the simulation equipment is physically present in the same location as the learners.2 3 During rapid cycle deliberate practice (RCDP) simulation, learners receive direct feedback at defined stopping points in the scenario, at which the scenario rewound and then restarted with increased level of difficulty.4 This report describes the use of RCDP for remote simulation training that allows for participants, facilitators and simulation equipment to be apart.
Design objectives
The objectives of this innovation were (1) to provide simulation-based training during times of social distancing and (2) to explore the feasibility of RCDP during remote simulation.
Equipment
Teleconference platform Zoom (Zoom Video Communications, San Jose, California, USA) was used for the communication and Laerdal SimNewB (Laerdal Medical, Stavanger, Norway) served as the manikin.
Implementation/execution
We organised two sessions with a total of 21 third-year anaesthesia residents. All participants, two local and one remote facilitator met on a video conference call. The simulation case was adapted from Hunt et al 4 and involved a presentation of a 3-month-old infant presenting in respiratory distress that subsequently worsened requiring intubation, cardiopulmonary resuscitation and defibrillation. Five RCDP cycles were conducted with increasing level of difficulty at each round: (i) simple bag-mask ventilation (BMV), (ii) difficult BMV, (iii) bradycardia, (iv) refractory pulseless electrical activity, (v) ventricular fibrillation. All participants were at separate locations (at home). Local instructor 1 was in charge of running the case on the computer, local instructor 2 was giving visual hints about the procedures taking place and medications being given. The remote instructor was leading the discussion (figure 1). In each RCDP round, six participants were assigned active roles and the name was changed in Zoom accordingly—Team Leader, Airway, Compressor, Monitor/Defibrillator, Meds, Code Recorder. Other participants remained passive until the discussion at the end of the round, following which the roles were changed. Participants were given role specific cues (eg, ‘chest is not rising’ for the Airway person) in the ‘chat’ window by copying and pasting from a list made in advance. At all times the participants were able to see the manikin and the equipment being used as well as the patient monitor (online supplementary file 1).
Figure 1.
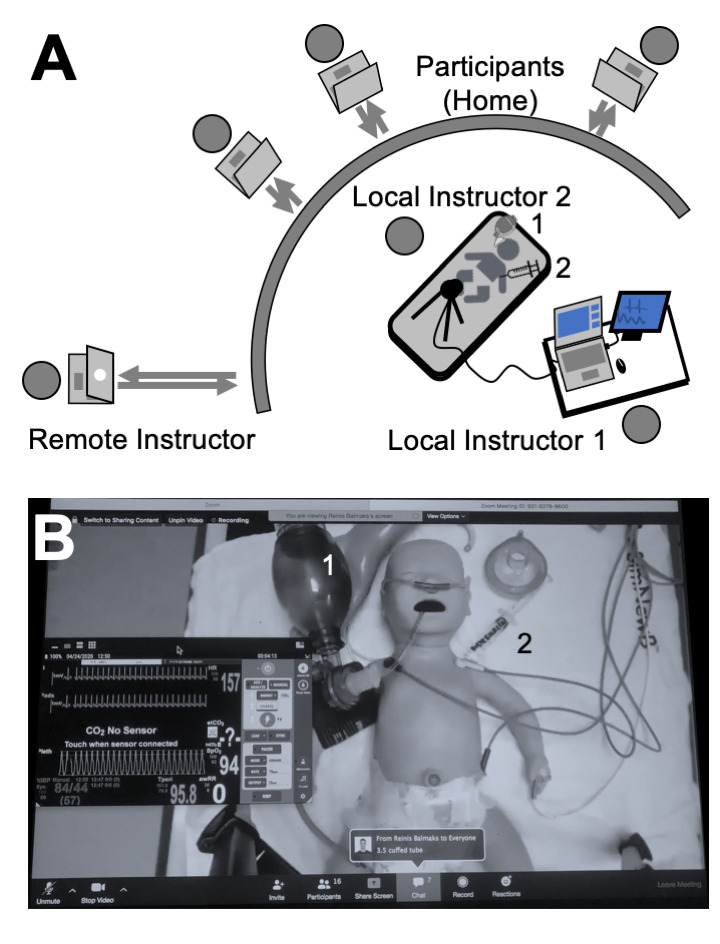
Simulation set-up (panel A) and participant screen view (panel B). The manikin is being hand-bag ventilated (1) and received epinephrine (2). Panel (A) designed by author RB for this publication.
bmjstel-2020-000671supp001.mp4 (12MB, mp4)
Lessons learned
We are excited to report that remote RCDP simulations can be executed when facilitators and students are apart. When choosing a scenario, we suggest to choose scenarios that focus on choreography rather than on procedural skills. A confederate could add additional fidelity but we chose not to use one as we were worried about too many different voices talking over each other. We found the use of the chat window helpful especially when assigning a team member to concentrate on the chat. This also decreased the number of voices talking at the same time and the information needed to be not only noticed but also screened for relevance and consequence. For example, when chest compressions were reported to be ongoing at a rate of 150/min, the participant had to decide to both report it and to interpret that it was too fast. We felt that both reality (changes with the manikin) and conceptual (updates in the chat window) cues were important to improve fidelity which is the main challenge in this type of simulation.5
Conducting the simulation using RCDP helped increase the level of difficulty as the session progressed and predefined stopping points were useful to both provide direct feedback and to change roles throughout the simulation scenario.
It was challenging to engage learners who were not assigned a role within the simulation (observers). We used the Simulation Design Scale to assess the objectives, support, problem solving, feedback and fidelity6 and the median scores (with IQR) on Likert Scale were 4 (4–5) 5 (4–5), 4 (4–5), 5 (4–5) and 4.5 (4–5), respectively. In free text comments, residents appreciated that this was a new experience, the opportunity to enhance communication skills and learning from home. They would have liked to be ‘hands on’, it was challenging at times to remember each other’s roles, difficult to communicate non-verbally and sometimes too many people were talking at once.
Conclusion
Remote simulations using an online platform can be used as a flexible and adjustable tool for RCDP simulation-based training during the current COVID-19 pandemic and potentially for other remote simulation training when simulation equipment, facilitators and learners are potentially all in different locations.
Footnotes
Twitter: @reinis_balmaks
Contributors: All authors have made substantial contributions to all of the following: (1) conception and design of the study, or analysis and interpretation of data, and (2) drafting the article or revising it critically for important intellectual content. Each author has consented to take public responsibility for the entire final work as submitted and have acknowledged familiarity with the submission guidelines for BMJ Simulation & Technology Enhanced Learning.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; internally peer reviewed.
References
- 1. von Lubitz DKJE, Carrasco B, Gabbrielli F, et al. Transatlantic medical education: preliminary data on distance-based high-fidelity human patient simulation training. Stud Health Technol Inform 2003;94:379–85. [PubMed] [Google Scholar]
- 2. McCoy CE, Sayegh J, Alrabah R, et al. Telesimulation: an innovative tool for health professions education. AEM Educ Train 2017;1:132–6. 10.1002/aet2.10015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hayden EM, Khatri A, Kelly HR, et al. Mannequin-based Telesimulation: increasing access to simulation-based education. Acad Emerg Med 2018;25:144–7. 10.1111/acem.13299 [DOI] [PubMed] [Google Scholar]
- 4. Hunt EA, Duval-Arnould JM, Nelson-McMillan KL, et al. Pediatric resident resuscitation skills improve after "rapid cycle deliberate practice" training. Resuscitation 2014;85:945–51. 10.1016/j.resuscitation.2014.02.025 [DOI] [PubMed] [Google Scholar]
- 5. Paige JB, Morin KH. Simulation fidelity and cueing: a systematic review of the literature. Clin Simul Nurs 2013;9:e481–9. 10.1016/j.ecns.2013.01.001 [DOI] [Google Scholar]
- 6. National League for Nursing . Simulation design scale (student version). Available: http://www.nln.org/docs/default-source/professional-development-programs/nln-instrument_simulation-design-scale.pdf?sfvrsn=0 [Accessed 6 May 2020].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjstel-2020-000671supp001.mp4 (12MB, mp4)


