Background
Emergency laparotomy is one of six index operations for which all higher general surgery trainees (HST) are required to demonstrate both a minimum indicative number and competence level, prior to the award of a certificate of completion of training. It is a high-risk procedure associated with significant morbidity and mortality and has been subject to several contemporary, high profile national initiatives not least the National Emergency Laparotomy Audit (NELA),1 aimed at improving the quality of care for patients. Compounded by out of hours presentations and the high risks associated with the procedure, training opportunities for emergency laparotomy are often challenging and sporadic.2 Here, we describe a novel simulation model for emergency laparotomy (figure 1).
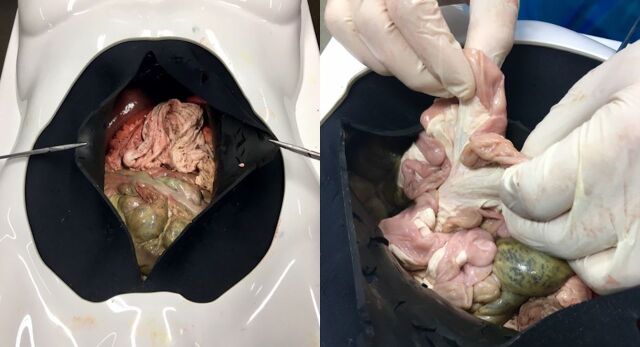
Figure 1.
Emergency laparotomy simulation model.
Technique
The wet lab bench model was designed to recreate a patient undergoing emergency laparotomy. A standard body torso laparoscopic training box covered with a neoprene skin was used to simulate the abdominal cavity. An entire porcine gastrointestinal tract was anatomically orientated, with minimal dissection of the intestinal mesentery, into the typical human orientation and fixed with pins to a large cork board which was placed inside the laparoscopic box trainer. Using artificial blood and bile, three separate models were created to simulate three different clinical scenarios: blunt force liver injury, perforated duodenal ulcer and a splenic laceration. The simulation model was piloted during the Health Education and Improvement Wales HST surgical boot camp during which trainees were given a clinical scenario prior to undertaking the simulated laparotomy. Each trainee was observed by a consultant trainer, who on recognition of the pathological findings by the trainee, asked them to describe the surgical management options as well as demonstrate how they would carry out important interventions such as haemostatic packing for a bleeding liver or splenic laceration or over sewing a perforated duodenal ulcer.
Discussion
To our knowledge, this is the first emergency laparotomy simulation model that provides safe and effective, high-fidelity training in emergency laparotomy. This simple and cost-effective model enables important training opportunities in this index surgical procedure, aiming to accelerate the learning curve of junior trainees with implications for enhanced training time, boosted and more efficient training and most of all a commensurate improvement in patient safety.
Following the success of the initial pilot, this simulation model has now been incorporated as a key component in the annual boot camp which forms part of the formal surgical training programme in the Health Education and Improvement Wales Deanery. Further analysis looking at the corresponding impact of this simulation model on trainee curricula assessment (Procedural-Based Assessments) is ongoing.
Footnotes
Contributors: CB: concept, write-up and submission. DR: concept, write-up. TA, RE, JP: training faculty. SG, NW: design and materials. WL: final review.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; internally peer reviewed.
References
- 1. National Emergency Laparotomy Audit (NELA). Healthcare quality improvement partnership: The Royal College of Anaesthetists. [Google Scholar]
- 2. Egan RJ, Abdelrahman T, Tate S, et al. Wales Deanery Emergency General Surgery Working Group. Modular emergency general surgery training: A pilot study of a novel programme. Ann R Coll Surg Engl 2016;98:475–8. 10.1308/rcsann.2016.0187 [DOI] [PMC free article] [PubMed] [Google Scholar]