Abstract
Context:
Hemodynamic stability during induction of anesthesia is always a concern for an anesthesiologist. Propofol remains the most popular induction agent with its favorable characteristics and few drawbacks like decrease in heart rate and blood pressure (BP). Although etomidate provides better hemodynamic stability, its use declined due to reports of adrenocortical suppression.
Aims:
We designed a study to compare the effect of anesthetic induction with etomidate versus propofol on serum cortisol levels and hemodynamics.
Settings and Design:
This was a prospective randomized double-blind comparative study.
Subjects and Methods:
Sixty ASA PS classes I and II patients scheduled for laparoscopic inguinal hernia repair under general anesthesia were included in the study. Thirty patients received propofol 2 mg.kg−1 and thirty, etomidate 0.3 mg.kg−1. Blood samples for serum cortisol were withdrawn preoperatively, immediate postoperatively, and 24 h after surgery. Vitals were monitored throughout.
Statistical Analysis Used:
All data are presented as mean ± standard deviation and proportions. Demographic data were analyzed by Student's t-test, and Chi-square test was used to analyze changes over time. The statistical software SPSS version 25.0 was used for data analysis.
Results:
Systolic blood pressure (BP), diastolic BP, and mean BP were more stable in the etomidate group compared to the propofol group. Serum cortisol levels before surgery in both the groups were within normal limits and comparable, followed by a significant decline in the etomidate group and rise in the propofol group in the immediate postoperative period. The levels in the third sample were comparable in both the groups.
Conclusion:
Etomidate offers superior hemodynamic compared to propofol. A decrease in serum cortisol level in the etomidate group was transient returning back to normal within 24 h.
Keywords: Adrenocortical suppression, etomidate, hemodynamic stability, propofol, serum cortisol
INTRODUCTION
Hemodynamic stability during induction of anesthesia is always a concern for an anesthesiologist. Among various induction agents, propofol and etomidate are commonly used. Propofol remains the most popular induction agent with its favorable characteristics of rapid and smooth recovery, potent attenuation of airway reflexes, and few major drawbacks like decrease in heart rate (HR) and blood pressure (BP).[1,2,3] Although etomidate provides better hemodynamic stability due to its lack of effect on the sympathetic nervous system, its use declined due to reports of adrenocortical suppression.[4]
Hence, we aimed to compare the effect of anesthetic induction with single-dose etomidate versus propofol on serum cortisol levels and hemodynamics in patients undergoing laparoscopic surgeries.
SUBJECTS AND METHODS
This prospective randomized double-blind comparative study was conducted after approval from the Institutional Ethics Committee and obtaining written informed consent from the patients which included sixty ASA PS classes I and II male patients in the age group of 20–60 years, nondiabetic and nonhypertensive, who had not received steroids in any form in the last month and were scheduled for laparoscopic inguinal hernia repair under general anesthesia. The study population was divided randomly into two groups of thirty patients each, and randomization was done using a computer-generated random number table. The two groups were Group P receiving propofol 2 mg.kg−1 and Group E receiving etomidate 0.3 mg.kg−1. The syringes containing the drugs were prepared by an independent anesthesiologist, not involved in the study, to ensure a proper blinding procedure.
In the preoperative room, on the day of surgery, blood samples were withdrawn from the patients for preoperative serum cortisol estimation.
In the operation theater, pulse oximeter, noninvasive BP apparatus, and five-lead electrocardiogram were connected to the patient and baseline parameters were noted. Patients in both the groups were administered injection midazolam 0.02 mcg.kg−1 and injection fentanyl 2mcg.kg-1 intravenously 3–5 min before the induction of anesthesia.
The induction of general anesthesia in Group E was done with injection etomidate 0.3 mg.kg−1 and in Group P with injection propofol 2 mg.kg−1 followed by a bolus dose of injection vecuronium 0.1 mg.kg−1 intravenously. Anesthesia was maintained with nitrous oxide: oxygen (50%:50%), isoflurane (1–1.5 vol.%), and vecuronium in maintenance doses. Vitals were monitored throughout the procedure.
At the end of the surgery, the residual effect of vecuronium was reversed with injection neostigmine 0.05 mg.kg−1 and injection glycopyrrolate 0.008 mg.kg−1, and the patient was extubated. The postoperative BP (systolic, diastolic, and mean) and HR were noted.
Postoperative blood sample for serum cortisol was obtained at the end of surgery after reversal of anesthesia and extubation, and a later sample was taken 24 h after the end of surgery.
All data are presented as mean ± standard deviation and proportion. Demographic data were analyzed by Student's t-test, and Chi-square test was used to analyze changes over time. The statistical IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp was used for the analysis of the data.
RESULTS
Demographic parameters in both the groups were comparable with respect to age and weight. While comparing hemodynamics in the two groups, mean HR increased at intubation and 5 min after intubation in Group E as etomidate lacks sympathetic blocking property in response to laryngoscopy and intubation compared to the propofol group where HR decreased at intubation and returned to baseline at 5 min. In the rest of the study period, HR was comparable in the two groups. Systolic BP and diastolic BP were more stable in the etomidate group compared to the propofol group, where fall in systolic and diastolic BP was seen. Similarly, deviation in mean arterial pressure was more in the propofol group than the etomidate group where it remained stable throughout [Graph 1 a-d].
Graph 1.
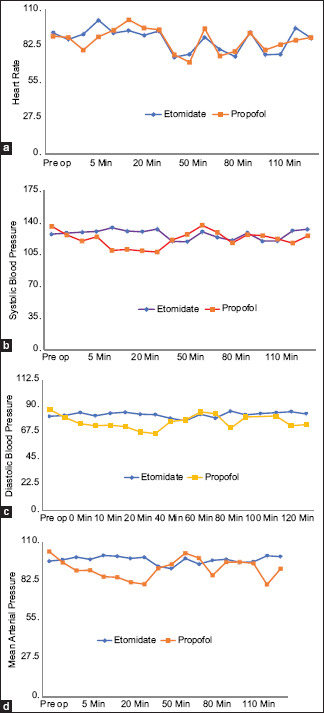
Line graphs showing mean heart rate (a), systolic blood pressure (b), diastolic blood pressure (c), and mean blood pressure (d) in the etomidate and propofol groups
Serum cortisol levels in blood sample taken before surgery in both the groups were within normal limits and comparable. The normal adult serum cortisol levels are 5 mcg.dL-1.
However, a significant decline in serum cortisol level was observed in the etomidate group in the second blood sample, taken in the immediate postoperative period, and the propofol group showed a rise in serum cortisol level as compared to their respective baseline values. The serum cortisol levels in the third sample, taken 24 h after the end of surgery, were comparable in both the groups [Tables 1 and 2].
Table 1.
Mean serum cortisol level in the propofol group
| Time intervals | n | Mean (mcg/dl)±SD | F-test | P |
|---|---|---|---|---|
| Preoperative | 30 | 11.499±2.7740093 | 15.42 | <0.001** |
| Postoperative | 30 | 13.243±1.0751528 | ||
| After 24 h | 30 | 13.39033±2.6091895 |
**P<0.001 highly significant at 5% level of significance. SD=Standard deviation
Table 2.
Mean serum cortisol level in the etomidate group
| Time intervals | n | Mean (mcg/dl)±SD | F-test | P |
|---|---|---|---|---|
| Preoperative | 30 | 11.355±2.5742879 | 374.43 | <0.001** |
| Immediate postoperative | 30 | 3.421333±0.9632189 | ||
| 24 h after surgery | 30 | 13.58833±3.3247178 |
**P<0.001 highly significant at 1% level of significance. SD=Standard deviation
DISCUSSION
Induction of anesthesia is associated with hemodynamic perturbation because of peripheral vasodilatation, reduction in preload, decrease in venous return, and myocardial depression whereas laryngoscopy and tracheal intubation lead to stress response leading to tachycardia, hypertension, arrhythmias, and myocardial ischemia due to a surge in plasma catecholamine levels. This can prove detrimental for patient safety in intraoperative as well as in postoperative period.[5] Hence, it remains challenging for an anesthesiologist to decide an appropriate induction agent.
Etomidate, a nonbarbiturate, imidazole hypnotic, has a short-lasting and rapid onset of action along with minimum respiratory depression and has a safe cardiovascular risk profile preserving hemodynamics.[6,7] Therefore, it is an ideal induction agent for hemodynamically unstable patients. It does not have any effect on the sympathetic nervous system as well as it preserves baroreceptor function.[8,9]
When used as an induction agent in patients with cardiac disease, it provides stable hemodynamics with minimal or no variation in mean BP, HR, mean pulmonary artery pressure, pulmonary capillary wedge pressure, central venous pressure, stroke volume, cardiac index, or pulmonary and systemic vascular resistance. Despite these properties of etomidate, propofol is still widely for induction. At induction dose, propofol decreases preload,[10] afterload,[11] and myocardial contractility,[12,13] and this can be attributed to its arterial and venous dilating properties of direct vascular smooth muscle relaxation.[14] In contrast to etomidate, propofol decreases the baroreceptor reflex causing BP changes.[15]
Although etomidate has fewer hemodynamic effects, its use is reduced possibly due to its adverse effects on adrenal cortex. Etomidate, by reversibly inhibiting the enzyme 11-β hydroxylase and to a lesser extent 17-α hydroxylase, prevents the conversion of cholesterol to cortisol.[16] This effect after single dose can last up to 24 h starting from 30 min of intravenous injection. This can be more hazardous in patients who have received a continuous infusion in intensive care unit for sedation.[17] Furthermore, iatrogenic inhibition of adrenal cortex can prove more detrimental in few patients where steroids can be lifesaving as in cases of sepsis.[18]
In our study, we included patients who were neither emergency cases nor in sepsis nor on steroids. After a single bolus dose of etomidate, there was a significant reduction in serum cortisol level at the end of surgery which was transient and returned toward baseline in 24 h. This reduction was also near-normal physiological cortisol levels. Our results were consistent with that of the study conducted by Srivastava et al.[19] They conducted a similar study on sixty controlled hypertensive patients, undergoing major laparoscopic gynecological surgery, where serum cortisol levels were comparable at preinduction levels in both the groups. At the end of operation, there was a definite fall in serum cortisol levels in the etomidate group, and the difference between the two groups was significant although cortisol levels remained within the physiological range, though toward the lower side and returned to baseline level in the etomidate group at the end of 24 h.
Schenarts et al.[20] also found in their study that fall in serum cortisol level caused by etomidate was significant though it remained near lower limits and returned to normal at the end of 24 h. Further, they found that there was a reduction in cosyntropin stimulation response test for up to 3 h of induction which came back to normal at 12 h after etomidate induction. This inhibition of steroidogenesis had no significant effect on biochemical parameters such as blood sugar level, lactates, and fatty acids as shown by Lacoumenta et al.[21] Furthermore, hemodynamics were comparable between the two groups as seen in our study as well as in previous studies. There was no obvious adverse effect on patients due to this transient inhibition of steroidogenesis.
Myoclonus was found to be a disturbing side effect apart from pain on injection in the etomidate group. Incidence of myoclonus is significantly reduced with the use of medium-chain triglyceride etomidate as compared to propylene glycol preparation and with the use of benzodiazepines and opioids as premedication.[22,23]
Propofol use is also associated with pain on injection which can be reduced with i.v. lignocaine or prior use of opioids.
CONCLUSION
Etomidate is found to be a better induction agent as it offers superior hemodynamic stability during induction of general anesthesia as compared to propofol although it does not block sympathetic responses to laryngoscopy and intubation. A decrease in serum cortisol level in the etomidate group was transient returning back to normal within 24 h and does not adversely affect the patient.
Limitation
The sample size was very small, and the study needs to be conducted on a larger population to extrapolate these data to general population.
Financial support and sponsorship
This was a self-funded study.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Maruyama K, Nishikawa Y, Nakagawa H, Ariyama J, Kitamura A, Hayashida M. Can intravenous atropine prevent bradycardia and hypotension during induction of total intravenous anesthesia with propofol and remifentanil? J Anesth. 2010;24:293–6. doi: 10.1007/s00540-009-0860-2. [DOI] [PubMed] [Google Scholar]
- 2.Frazee BW, Park RS, Lowery D, Baire M. Propofol for deep procedural sedation in the ED. Am J Emerg Med. 2005;23:190–5. doi: 10.1016/j.ajem.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 3.Ozgul U, Begec Z, Erdogan MA, Aydogan MS, Sanli M, Colak C. Effect of alkalinisation of lignocaine for propofol injection pain: A prospective, randomised, double-blind study. Anaesth Intensive Care. 2013;41:501–4. doi: 10.1177/0310057X1304100411. [DOI] [PubMed] [Google Scholar]
- 4.Mackenzie N, Grant IS. Comparison of the new emulsion formulation of propofol with methohexitone and thiopentone for induction of anaesthesia in day cases. Br J Anaesth. 1985;57:725–31. doi: 10.1093/bja/57.8.725. [DOI] [PubMed] [Google Scholar]
- 5.Kayhan Z, Aldemir D, Mutlu H, Oğüş E. Which is responsible for the haemodynamic response due to laryngoscopy and endotracheal intubation.Catecholamines, vasopressin or angiotensin? Eur J Anaesthesiol. 2005;22:780–5. doi: 10.1017/s0265021505001298. [DOI] [PubMed] [Google Scholar]
- 6.Saricaoglu F, Uzun S, Arun O, Arun F, Aypar U. A clinical comparison of etomidate-lipuro, propofol and admixture at induction. Saudi J Anaesth. 2011;5:62–6. doi: 10.4103/1658-354X.76509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sarkar M, Laussen PC, Zurakowski D, Shukla A, Kussman B, Odegard KC. Hemodynamic responses to etomidate on induction of anesthesia in pediatric patients. Anesth Analg. 2005;101:645–50. doi: 10.1213/01.ane.0000166764.99863.b4. [DOI] [PubMed] [Google Scholar]
- 8.Stockham RJ, Stanley TH, Pace NL, Gillmor S, Groen F, Hilkens P. Fentanyl pretreatment modifies anaesthetic induction with etomidate. Anaesth Intensive Care. 1988;16:171–6. doi: 10.1177/0310057X8801600207. [DOI] [PubMed] [Google Scholar]
- 9.Priano LL, Bernards C, Marrone B. Effect of anesthetic induction agents on cardiovascular neuroregulation in dogs. Anesth Analg. 1989;68:344–9. [PubMed] [Google Scholar]
- 10.Lepage JY, Pinaud ML, Helias JH, Cozian AY, Le Normand Y, Souron RJ. Left ventricular performance during propofol or methohexital anesthesia: Isotopic and invasive cardiac monitoring. Anesth Analg. 1991;73:3–9. doi: 10.1213/00000539-199107000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Lowe D, Hettrick DA, Pagel PS, Warltier DC. Propofol alters left ventricular afterload as evaluated by aortic input impedance in dogs. Anesthesiology. 1996;84:368–76. doi: 10.1097/00000542-199602000-00015. [DOI] [PubMed] [Google Scholar]
- 12.Wodey E, Chonow L, Beneux X, Azzis O, Bansard JY, Ecoffey C. Haemodynamic effects of propofol vs thiopental in infants: An echocardiographic study. Br J Anaesth. 1999;82:516–20. doi: 10.1093/bja/82.4.516. [DOI] [PubMed] [Google Scholar]
- 13.Lam CF, Chang PJ, Chen YA, Yeh CY, Tsai YC. Inhibition of ATP-sensitive potassium channels attenuates propofol-induced vasorelaxation. Crit Care Resusc. 2010;12:186–90. [PubMed] [Google Scholar]
- 14.Sato M, Tanaka M, Umehara S, Nishikawa T. Baroreflex control of heart rate during and after propofol infusion in humans. Br J Anaesth. 2005;94:577–81. doi: 10.1093/bja/aei092. [DOI] [PubMed] [Google Scholar]
- 15.de Jong FH, Mallios C, Jansen C, Scheck PA, Lamberts SW. Etomidate suppresses adrenocortical function by inhibition of 11 beta-hydroxylation. J Clin Endocrinol Metab. 1984;59:1143–7. doi: 10.1210/jcem-59-6-1143. [DOI] [PubMed] [Google Scholar]
- 16.Zed PJ, Mabasa VH, Slavik RS, Abu-Laban RB. Etomidate for rapid sequence intubation in the emergency department: Is adrenal suppression a concern? CJEM. 2006;8:347–50. doi: 10.1017/s1481803500014044. [DOI] [PubMed] [Google Scholar]
- 17.Green R, Gorman SK. Safety of etomidate bolus administration in patients with septic shock. CJEM. 2011;13:105–8. doi: 10.2310/8000.2011.110388. [DOI] [PubMed] [Google Scholar]
- 18.Cuthbertson BH, Sprung CL, Annane D, Chevret S, Garfield M, Goodman S, et al. The effects of etomidate on adrenal responsiveness and mortality in patients with septic shock. Intensive Care Med. 2009;35:1868–76. doi: 10.1007/s00134-009-1603-4. [DOI] [PubMed] [Google Scholar]
- 19.Srivastava S, Ghosh S, Bhattacharya D, Nayak SK, Bhattacharya S, Haldar P, et al. Cortisol lowering action and cardiovascular stability of etomidate: A comparison with propofol in controlled hypertensives. J Evol Med Dent Sci. 2015;75:13016–24. [Google Scholar]
- 20.Schenarts CL, Burton JH, Riker RR. Adrenocortical dysfunction following etomidate induction in emergency department patients. Acad Emerg Med. 2001;8:1–7. doi: 10.1111/j.1553-2712.2001.tb00537.x. [DOI] [PubMed] [Google Scholar]
- 21.Lacoumenta S, Paterson JL, Myers MA, Hall GM. Effects of cortisol suppression by etomidate on changes in circulating metabolites associated with pelvic surgery. Acta Anaesthesiol Scand. 1986;30:101–4. doi: 10.1111/j.1399-6576.1986.tb02376.x. [DOI] [PubMed] [Google Scholar]
- 22.Hüter L, Schreiber T, Gugel M, Schwarzkopf K. Low-dose intravenous midazolam reduces etomidate-induced myoclonus: A prospective, randomized study in patients undergoing elective cardioversion. Anesth Analg. 2007;105:1298–302. doi: 10.1213/01.ane.0000287248.25610.c0. [DOI] [PubMed] [Google Scholar]
- 23.Hueter L, Schwarzkopf K, Simon M, Bredle D, Fritz H. Pretreatment with sufentanil reduces myoclonus after etomidate. Acta Anaesthesiol Scand. 2003;47:482–4. doi: 10.1034/j.1399-6576.2003.00081.x. [DOI] [PubMed] [Google Scholar]


