Abstract
Background
Effective paediatric basic life support improves survival and outcomes. Current cardiopulmonary resuscitation (CPR) training involves 4-yearly courses plus annual updates. Skills degrade by 3–6 months. No method has been described to motivate frequent and persistent CPR practice. To achieve this, we explored the use of competition and a leaderboard, as a gamification technique, on a CPR training feedback device, to increase CPR usage and performance.
Objective
To assess whether self-motivated CPR training with integrated CPR feedback improves quality of infant CPR over time, in comparison to no refresher CPR training.
Design
Randomised controlled trial (RCT) to assess the effect of self-motivated manikin-based learning on infant CPR skills over time.
Setting
A UK tertiary children's hospital.
Participants
171 healthcare professionals randomly assigned to self-motivated CPR training (n=90) or no refresher CPR training (n=81) and followed for 26 weeks.
Intervention
The intervention comprised 24 h a day access to a CPR training feedback device and anonymous leaderboard. The CPR training feedback device calculated a compression score based on rate, depth, hand position and release and a ventilation score derived from rate and volume.
Main outcome measure
The outcome measure was Infant CPR technical skill performance score as defined by the mean of the cardiac compressions and ventilations scores, provided by the CPR training feedback device software. The primary analysis considered change in score from baseline to 6 months.
Results
Overall, the control group showed little change in their scores (median 0, IQR −7.00–5.00) from baseline to 6 months, while the intervention group had a slight median increase of 0.50, IQR 0.00–33.50. The two groups were highly significantly different in their changes (p<0.001).
Conclusions
A significant effect on CPR performance was demonstrated by access to self-motivated refresher CPR training, a competitive leaderboard and a CPR training feedback device.
Keywords: cardiopulmonary resuscitation, training, self-motivation, game-ification
Introduction
Paediatric arrests occur more frequently than is often appreciated, with low survival rates and significant neurological sequelae.1 2 Provision of high-quality chest compressions for paediatric arrest significantly improves survival outcomes.3–5 A recent meta-analysis of resuscitation studies indicated how significant a determinant high-quality cardiopulmonary resuscitation (CPR) was to survival, showing a strong correlation with appropriate rate and depth of compression.6 However, even among experienced healthcare professionals, high-quality chest compressions do not occur in 36–87% of CPR.7–10
One explanation for poor CPR skill is the current CPR training paradigm of recertification every 2–4 years. Combined with the rarity of paediatric cardiac arrests and rapid decay in resuscitation skills over time,11–14 the provision of more frequent, accessible and user-friendly approaches to CPR training have been explored as an antidote to CPR skill decay. ‘Bedside booster’ CPR sessions with frequent, short bursts of CPR training are more feasible than large-scale, intense courses.15 16 Life support instructor assessment of CPR performance has resource implications and is influenced by inter-instructor variability.17 Use of CPR feedback devices has shown that training with real-time feedback improves learning and skill retention,18 19 as well as performance of CPR delivery on actual patients.20 Such evidence relates to in-hospital and prehospital CPR survival.10 21 22
If increasing use of CPR feedback devices is key, the question arises on whether healthcare professionals would be motivated to practise more frequently given the current paradigm of mandated supervised training. To date, there has been limited exploration of harnessing learner-motivated and learner activated CPR practice. Learner activation is a phenomenon by which learners feel engagement, ownership and even heightened responsibility for the skills to be learnt.23 To date, no specific method has been described to motivate frequent CPR practice among healthcare professionals and no method has been described to motivate persistent self-directed practice to prevent skills decay.
To achieve learner activation in CPR practice, we have explored the use of competition and peer pressure as a gamification technique among healthcare professionals. Gamification is defined as the application of typical elements of game playing (eg, point scoring, competition with others, rules of play) to other areas, typically as an online marketing technique to encourage engagement with a product or service. In this study, we have utilised gamification techniques as positive motivators to increase CPR practice and performance on a self-directed CPR feedback device. Gamification to acquire knowledge and skills has been shown in healthcare and in other fields to improve learner activation and engagement.24 25 Since current CPR simulators provide quantitative feedback, it provided a method to measure skill improvement or decay over time using a scoring system. We postulated that public display of CPR training scores—such as on a leaderboard—would provide learner activation. Leaderboards are one method of motivating competitive behaviour in gamification and in games in general.26 27 We hypothesised that healthcare providers with 24 h access to a self-directed CPR training feedback device with monthly anonymised scores displayed on a leaderboard would both naturally increase frequency of CPR practice and improve their CPR performance.
Objective
The objective of our study was to determine the effect of longitudinal, repeated self-motivated CPR refresher training on CPR performance among paediatric practitioners. We compared CPR performance between those who were provided free access to a training simulator and leaderboard scores, compared to those without such access.
Methods
Trial design
This was a randomised controlled trial over 6 months in which a convenience sample of paediatric providers from two distinct practice areas, ranging from senior consultant physicians to junior nurses and support staff, was enrolled. On enrolment, baseline CPR performance data were collected on all participants using the same infant CPR feedback device (Laerdal infant QCPR manikin; Stavanger, Norway). Intervention group subjects with free access to the device were asked to submit their final scores at the end of the study period; control group participants without free access to the device were invited back after 6 months to submit final CPR performance data. The purpose of the study was to determine the effect of open access to a CPR training device and leaderboard on CPR practice and subsequent performance.
Ethical considerations
The local institutional review board approved this study.
Study setting and participants
The study took place at two healthcare delivery settings in a single UK tertiary children's hospital for 6 months starting January 2014. Participants consisted of staff from the postanaesthetic clinical unit in theatres (PACU) and the paediatric intensive care unit (PICU) (table 1). The PACU/theatres and PICU employ approximately 250 full-time staff. Inclusion criteria for enrolment included full-time employment and current certification in basic life support (BLS). Trainees were not excluded from this study.
Table 1.
Demographics of the study participants
| Characteristic | 24 h Access to CPR feedback training device (intervention arm) (n=90) | No access to CPR feedback training device (control arm) (n=81) | Total (overall %) |
|---|---|---|---|
| Role | |||
| Nurse (theatres) | 29 | 24 | 53 (31) |
| Nurse (PICU) | 28 | 21 | 49 (28.7) |
| Doctors (theatres) | 17 | 16 | 33 (19.3) |
| Doctor (PICU) | 2 | 2 | 4 (2.3) |
| Operating department assistant | 10 | 11 | 21 (12.3) |
| Healthcare support worker | 3 | 7 | 10 (5.9) |
| Pharmacist | 1 | 0 | 1 (0.6) |
| Rank | |||
| Junior staff (band 5 nurses & below) | 52 | 54 | 106 (62) |
| Senior staff (band 6 nurses & above) | 19 | 9 | 28 (16.4) |
| Doctors | |||
| Specialist trainees | 4 | 5 | 9 (5.2) |
| Consultants | 15 | 13 | 28 (16.4) |
| Time since last BLS update | |||
| ≤3 months | 20 | 21 | 41 (24) |
| >3–≤6 months | 23 | 20 | 43 (25.2) |
| >6–≤9 months | 20 | 19 | 39 (22.8) |
| >9–≤12 months | 23 | 18 | 41 (24) |
| Expired | 4 | 3 | 7 (4) |
| APLS certified | |||
| Yes | 24 | 12 | 36 (21.1) |
| No | 66 | 69 | 134 (78.4) |
| Last real-life CPR | |||
| ≤6 months | 10 | 11 | 21 (12.3) |
| >6 months–<3 years | 19 | 13 | 32 (18.7) |
| ≥ 3 years | 18 | 11 | 29 (17) |
| Never | 43 | 46 | 89 (52) |
APLS, advanced paediatric life support; BLS, basic life support; CPR, cardiopulmonary resuscitation; PICU, paediatric intensive care unit.
Randomisation
All subjects were randomised to either the intervention or control group for the entire duration of the study on enrolment. Stratified randomisation was accomplished using a random number generator. Stratification took place by healthcare professional role (junior nurse, senior nurse, trainee or consultant physician).
The self-motivation-based intervention
The intervention group was given 24 h/day, 7-days-a-week access to an infant CPR feedback training device consisting of a CPR manikin (Laerdal infant QCPR manikin; Stavanger, Norway) and an attached feedback device (Laerdal SkillGuide). Each manikin was located within the PACU or PICU within view of patients and families, accessible to all subjects without leaving their area of clinical practice. Instructions were provided for the intervention group. Each device recorded performance data that were displayed as ventilation and compression scores on the SkillGuide following 2 min of ventilation compression infant CPR on the manikin.28 Subjects were instructed to document their scores using a study identification number and submit the score to a collection device. They were allowed multiple attempts and unlimited submissions throughout the duration of the study. Participant scores were collated and ranked anonymously on leaderboards in the two clinical areas. The leaderboards were updated on a monthly basis. No reminders were sent to the intervention group, which was not proctored, supervised or forced to continue practising on the device. There was no tangible reward for increasing practice, nor a penalty for total avoidance.
Control
The control group participants could see the CPR devices in the workplace at all times but were informed that they could not use the devices. No preventative measures were in place to physically stop the control group from using the devices located within their clinical areas.
Study outcomes and definitions
We defined the outcome variable of CPR performance as the total composite score (TotS) of two measurements: ventilation score (VentS) and compression score (CompS). Both VentS and CompS were expressed as a percentage, ranging from 0 to 100 and were calculated by software within the SkillGuide with real-time data provided by the CPR device.28 VentS is calculated on the basis of the appropriate rate and volume of ventilation required for Paediatric Advanced Life Support for infants (2 breaths for every 15 compressions).29 CompS is amalgamated from the appropriate rate (100–120 compressions/minute), appropriate depth and appropriate full recoil. TotS is a mean score (0–100) of VentS and CompS. In addition to the outcome variables, we collected demographic variables including: Healthcare professional role (junior nurse, senior nurse, trainee, consultant physician), rank as defined by the band of the provider or seniority of the nurse, department, proximity of last BLS, advanced paediatric life support (APLS) training and last actual CPR on a patient.
Sample size
We aimed to detect a 10% difference in CPR performance (TotS) between the intervention and control groups. A sample size of 140 participants (70 in each arm) would provide a detectable effect size of 0.48 with an α of 0.05 and 80% power.
Statistical analyses
Descriptive statistics were used to summarise the subject characteristics of each group, and χ2 tests to check for any significant demographic differences between groups. A Mann–Whitney U test was used to verify that there was no significant difference between baseline scores.
For the primary outcome, we compared change from baseline between the two groups using descriptive statistics and a Mann-Whitney U test. Secondary analysis looked at the 6-month scores via descriptive statistics and paired Wilcoxon signed-rank tests to examine for a significant change.
Analyses were performed in R V.3.1.1.30
Results
Study participants
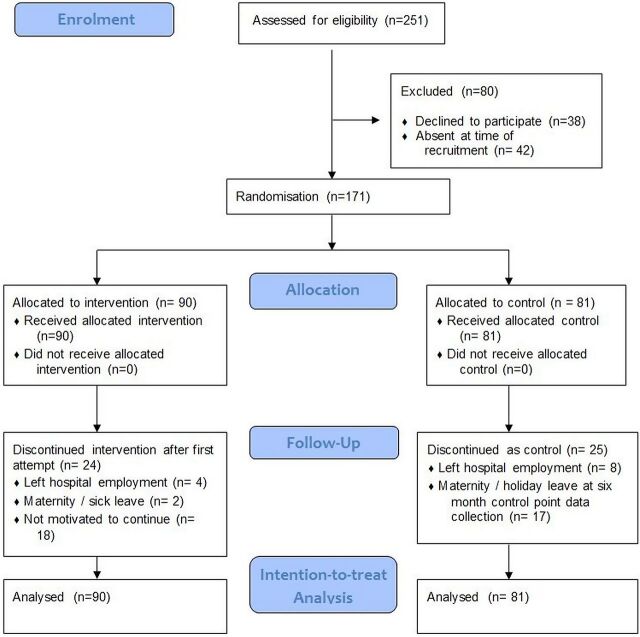
A total of 90 subjects were enrolled in the intervention group and 81 in the control group, shown in table 1. All 171 subjects provided baseline data. Thereafter, 24 (27%) subjects from the intervention group and 25 (31%) subjects from the control group dropped from the study. All dropouts were voluntary (eg, maternity leave, change of job). The apparent imbalance in the dropouts relates to those in the intervention group (n=18) who were not self-motivated to continue on the feedback device after their first baseline score at time zero. In addition, in the control arm, we were unable to track participants at 6 months (n=17) for their 6-month score, as they were on holiday, maternity or sick leave. Figure 1 illustrates the CONSORT diagram for our study.31
Figure 1.
Flow diagram of study design and participant enrolment modified from Consort Transparent. Reporting of Trials.31
Study outcomes
Within the intervention group, 66 (73%) used the CPR feedback device more than once during the study period.
Primary outcome
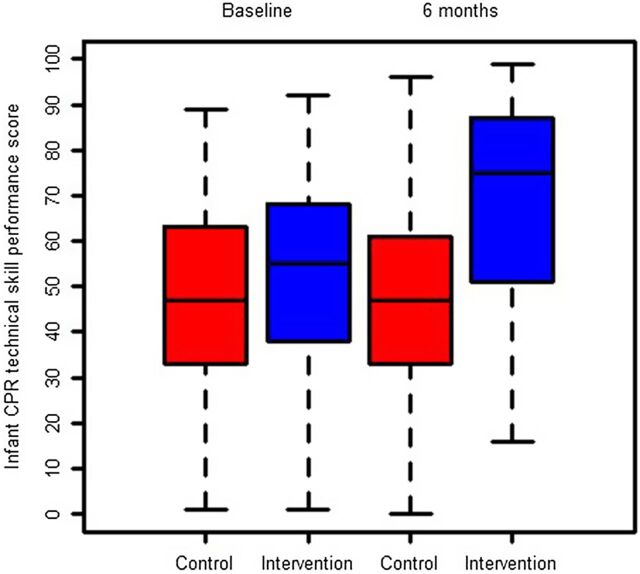
Overall, the control group tended to show little change in their scores (median 0, IQR −7.00–5.00) from baseline to 6 months, while the intervention group had a slight median increase of 0.50, IQR 0.00–33.50. The two groups were highly significantly different in their changes (p<0.001) figure 2.
Figure 2.
Box plot to show changes between control and intervention groups at baseline and 6 months.
Secondary analysis
There was no difference in baseline CPR performance between the intervention group and control group (intervention median 55.00, IQR 38.25–67.50, control median 47.00, IQR 33.00–63.00, p=0.186)). The change from baseline to 6 months was significant in the intervention group (p<0.001), while the control group did not show a significant change (p=0.475).
Discussion
Our study is one of the first to describe the effects of self-motivation on infant CPR practice using a CPR feedback device, in conjunction with a leaderboard. We demonstrate that overall infant CPR performance on the simulator improves with increased practice despite a lack of any observer, instructor or supervisor, and without an external reward or punishment. This is a novel method of motivation that is capable only because of the technologies allowing for an objective, measurable feedback of CPR quality. Cheng et al10 32 noted that even with trained supervision and observation, the reliability of human observation on CPR quality is inferior to CPR simulators that provide this level of feedback, and that the presence of neutral feedback does improve CPR quality. The leaderboard then provides a different level of feedback that provides a more longitudinal performance metric in the form of learner activation.
Gamification techniques to improve social competition—termed points, badges, leaderboards33—have been present in digital education, particularly with schoolchildren, but have also been described in the medical education literature among adult healthcare providers. Leaderboards in particular were reported as the most important motivators for cognitive learning among U.S. internal medicine residents.26 These are examples of learner activation, and gamification can increase the perceived value of the knowledge or skill to be gained.
Despite the life-saving potential of CPR, the inherent task-value of the CPR training is still undervalued among healthcare providers who perceive CPR as a certification to complete.34 CPR training improves confidence and often knowledge, but not always proportionately to performance,35–37 and this incongruence creates a barrier to motivating frequent practice. Providing a leaderboard and concrete, objective feedback also generates further incentive, as providers consistently overestimate the quality of CPR being provided during cardiac arrest.32 Our data support the assertion that gamification techniques can incentivise CPR training36 and also facilitate self-guided or self-directed practice.38 The literature demonstrates that these features allow for successful learning and skills retention.34 38–40 We demonstrate the association between increased practice and improved CPR performance, consistent with other studies that increase CPR practice frequency15 16; however, we showed this improvement in simulated CPR performance without the active supervision or proctoring with instructors or research assistants.
The strengths of this study include the feasibility of our leaderboard technique, as well as its generalisability to almost any unit or in-hospital or in-clinic setting, be it neonatal, paediatric or adult medicine.
Our study does have several limitations. We relied on self-reported scores; this meant scores could have been fabricated or not reported. However, we believe that this was relatively minimised because no actual reward beyond a higher leaderboard position was provided for a higher score. Ultimately, we measured only performance on the CPR simulator and did not report patient-based outcomes in this study. We would expect those who practised on the simulator to perform better than peers less familiar with it—essentially a null comparator study.41 However, our innovation was spurring spontaneous practice on the CPR feedback device using a leaderboard, the latter of which was the primary intervention in this study, not the manikin. Furthermore, we observed that the motivation gradually waned over the 6-month period, and the study did not assess skill improvement or decay past the 6-month period. It is also possible that the relatively high dropout rate, though similar in both arms, affected the results. Finally, the control group was not actively prevented from practising on the CPR feedback device throughout this study. Such a control group practice would have increased the performance of the control group arm at 6 months. Only one control group member reported scores.
In conclusion, evidence generated by our randomised controlled trial indicates that overall infant CPR performance on the simulator improves with increased practice spurred by a simple leaderboard in the intervention group over the 6-month period (p<0.001), compared with the control group. Our data suggest that longitudinal, self-motivated, rolling refresher CPR training with integrated CPR feedback can improve the quality of CPR over time. This study adds further evidence that interactive CPR manikins providing quantifiable scores can promote self-directed learning in motivated individuals.
Footnotes
Twitter: Follow Ralph MacKinnon at @MacKinnonSIM and Todd Chang at @drtoddchang
Contributors: RJMK conceptualised the research question and study design, co-performed the study, contributed intellectual content, drafted the initial manuscript, reviewed and revised the manuscript. RS and CD co-performed the study, contributed intellectual content, reviewed and revised the manuscript. CF contributed to the study design, statistical analysis and reviewed the manuscript. TPC, TS-H, AC and VN contributed intellectual content and reviewed and revised the manuscript. All authors approved the final manuscript as submitted.
Competing interests: RJMK, TPC AC and VN are members of the INSPIRE network, which receives infrastructure support from the Laerdal. Foundation for Acute Medicine, project funding from Rbaby. Foundation, and funding for biannual meetings from the Society for Simulation in Healthcare and the International Pediatric Simulation Society.
Ethics approval: Ethics opinion was sought from the research host organisation. In the UK, in accordance with current governance guidelines for health research, studies on NHS staff and service provision, this research project does not require NHS Research Ethics Approval. All participating individuals consent to do so and are provided with a participant information document.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The authors will respond to reasonable requests.
References
- 1.Nadkarni VM, Larkin GL, Peberdy MA, et al. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA 2006;295:50–7. 10.1001/jama.295.1.50 [DOI] [PubMed] [Google Scholar]
- 2.Merchant RM, Berg RA, Yang L, et al. Hospital variation in survival after in-hospital cardiac arrest. J Am Heart Assoc 2014;3:400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abella BS, Sandbo N, Vassilatos P, et al. Chest compression rates during cardiopulmonary resuscitation are suboptimal: a prospective study during in-hospital cardiac arrest. Circulation 2005;111:428–34. 10.1161/01.CIR.0000153811.84257.59 [DOI] [PubMed] [Google Scholar]
- 4.Edelson DP, Abella BS, Kramer-Johansen J, et al. Effects of compression depth and pre-shock pauses predict defibrillation failure during cardiac arrest. Resuscitation 2006;71:137–45. 10.1016/j.resuscitation.2006.04.008 [DOI] [PubMed] [Google Scholar]
- 5.Edelson DP, Litzinger B, Arora V, et al. Improving in-hospital cardiac arrest process and outcomes with performance debriefing. Arch Intern Med 2008;168:1063–9. 10.1001/archinte.168.10.1063 [DOI] [PubMed] [Google Scholar]
- 6.Wallace SK, Abella BS, Becker LB. Quantifying the effect of cardiopulmonary resuscitation quality on cardiac arrest outcome: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes 2013;6:148–56. 10.1161/CIRCOUTCOMES.111.000041 [DOI] [PubMed] [Google Scholar]
- 7.Sutton RM, Wolfe H, Nishisaki A, et al. Pushing harder, pushing faster, minimizing interruptions…but falling short of 2010 cardiopulmonary resuscitation targets during in-hospital pediatric and adolescent resuscitation. Resuscitation 2013;84:1680–4. 10.1016/j.resuscitation.2013.07.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sutton RM, Niles D, Nysaether J, et al. Quantitative analysis of CPR quality during in-hospital resuscitation of older children and adolescents. Pediatrics 2009;124:494–9. 10.1542/peds.2008-1930 [DOI] [PubMed] [Google Scholar]
- 9.Sutton RM, Maltese MR, Niles D, et al. Quantitative analysis of chest compression interruptions during in-hospital resuscitation of older children and adolescents. Resuscitation 2009;80:1259–63. 10.1016/j.resuscitation.2009.08.009 [DOI] [PubMed] [Google Scholar]
- 10.Cheng A, Brown LL, Duff JP, et al. Improving cardiopulmonary resuscitation with a CPR feedback device and refresher simulations (CPR CARES study): a randomized controlled trial. JAMA Pediatr 2015;169:137–44. 10.1001/jamapediatrics.2014.2616 [DOI] [PubMed] [Google Scholar]
- 11.Na JU, Sim MS, Jo IJ, et al. Basic life support skill retention of medical interns and the effect of clinical experience of cardiopulmonary resuscitation. Emerg Med J 2012;29:833–7. 10.1136/emermed-2011-200633 [DOI] [PubMed] [Google Scholar]
- 12.Kaye W, Mancini ME. Retention of cardiopulmonary resuscitation skills by physicians, registered nurses, and the general public. Crit Care Med 1986;14:620–2. 10.1097/00003246-198607000-00007 [DOI] [PubMed] [Google Scholar]
- 13.Berden HJ, Willems FF, Hendrick JM, et al. How frequently should basic cardiopulmonary resuscitation training be repeated to maintain adequate skills? BMJ 1993;306:1576–7. 10.1136/bmj.306.6892.1576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hamilton R. Nurses’ knowledge and skill retention following cardiopulmonary resuscitation training: a review of the literature. J Adv Nurs 2005;51:288–97. 10.1111/j.1365-2648.2005.03491.x [DOI] [PubMed] [Google Scholar]
- 15.Sutton RM, Niles D, Meaney PA, et al. Low-dose, high-frequency CPR training improves skill retention of in-hospital pediatric providers. Pediatrics 2011;128:e145–51. 10.1542/peds.2010-2105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sutton RM, Niles D, Meaney PA, et al. “Booster” training: evaluation of instructor-led bedside cardiopulmonary resuscitation skill training and automated corrective feedback to improve cardiopulmonary resuscitation compliance of Pediatric Basic Life Support providers during simulated cardiac arrest. Pediatr Crit Care Med 2011;12:e116–21. 10.1097/PCC.0b013e3181e91271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Soar J, Mancini ME, Bhanji F, et al., Education, implementation, and Teams Chapter Collaborators. Part 12: education, implementation, and teams: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation 2010;81(Suppl 1):e288–330. 10.1016/j.resuscitation.2010.08.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brett-Fleegler MB, Vinci RJ, Weiner DL, et al. A simulator-based tool that assesses pediatric resident resuscitation competency. Pediatrics 2008;121:e597–603. 10.1542/peds.2005-1259 [DOI] [PubMed] [Google Scholar]
- 19.Mpotos N, De Wever B, Valcke MA, et al. Assessing basic life support skills without an instructor: is it possible? BMC Med Educ 2012;12:58. 10.1186/1472-6920-12-58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yeung J, Meeks R, Edelson D, et al. The use of CPR feedback/prompt devices during training and CPR performance: a systematic review. Resuscitation 2009;80:743–51. 10.1016/j.resuscitation.2009.04.012 [DOI] [PubMed] [Google Scholar]
- 21.Abella BS, Edelson DP, Kim S, et al. CPR quality improvement during in-hospital cardiac arrest using a real-time audiovisual feedback system. Resuscitation 2007;73:54–61. 10.1016/j.resuscitation.2006.10.027 [DOI] [PubMed] [Google Scholar]
- 22.Kramer-Johansen J, Myklebust H, Wik L, et al. Quality of out-of-hospital cardiopulmonary resuscitation with real time automated feedback: a prospective interventional study. Resuscitation 2006;71:283–92. 10.1016/j.resuscitation.2006.05.011 [DOI] [PubMed] [Google Scholar]
- 23.Boman J. Facilitating student involvement in large classroom settings. J Nurs Educ 1986;25:226–9. [DOI] [PubMed] [Google Scholar]
- 24.Garris R, Ahlers R, Driskell JE. Games, motivation, and learning: a research and practice model. Simulation Gaming 2002;33:441–67. 10.1177/1046878102238607 [DOI] [Google Scholar]
- 25.Bedwell WL, Pavlas D, Heyne K, et al. Toward a taxonomy linking game attributes to learning: An empirical study. Simulation Gaming 2012;43:729–60. 10.1177/1046878112439444 [DOI] [Google Scholar]
- 26.Nevin CR, Westfall AO, Rodriguez JM, et al. Gamification as a tool for enhancing graduate medical education. Postgrad Med J 2014;90:685–93. 10.1136/postgradmedj-2013-132486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Christy KR, Fox J. Leaderboards in a virtual classroom: a test of stereotype threat and social comparison explanations for women's math performance. Comput Educ 2014;78:66–77. 10.1016/j.compedu.2014.05.005 [DOI] [Google Scholar]
- 28.Laerdal Inc. CPR scoring explained, 2013. http://www.laerdal.com/downloads/f2729/Scoring_CPR_November_v2.pdf (accessed 10 Sept 2014).
- 29.Berg MD, Schexnayder SM, Chameides L, et al. Part 13: pediatric basic life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010;122(Suppl 3):P862–75. 10.1161/CIRCULATIONAHA.110.971085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing, 2014. (accessed Jan 2015). [Google Scholar]
- 31.Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomized trials. Ann Intern Med 2001;134:657–62. 10.7326/0003-4819-134-8-200104170-00011 [DOI] [PubMed] [Google Scholar]
- 32.Cheng A, Overly K, Kessler D, et al. Perception of CPR quality: influence of CPR feedback, just-in-time CPR training and provider role. Resuscitation 2015;87:44–50. 10.1016/j.resuscitation.2014.11.015 [DOI] [PubMed] [Google Scholar]
- 33.Gibson D, Ostashewski N, Flintoff K, et al. Digital badges in education. Educ Info Technol 2015;20:403–10. 10.1007/s10639-013-9291-7 [DOI] [Google Scholar]
- 34.Hopstock LA. Motivation and adult learning: a survey among hospital personnel attending a CPR course. Resuscitation 2008;76:425–30. 10.1016/j.resuscitation.2007.09.011 [DOI] [PubMed] [Google Scholar]
- 35.Kurosawa H, Ikeyama T, Achuff P, et al. A randomized, controlled trial of in situ pediatric advanced life support recertification (“pediatric advanced life support reconstructed)” compared with standard pediatric advanced life support recertification for icu frontline providers. Crit Care Med 2014;42:610–18. 10.1097/CCM.0000000000000024 [DOI] [PubMed] [Google Scholar]
- 36.Dwyer T, Williams LM. Nurses’ behaviour regarding CPR and the theories of reasoned action and planned behaviour. Resuscitation 2002;52:85–90. 10.1016/S0300-9572(01)00445-2 [DOI] [PubMed] [Google Scholar]
- 37.Schlessel JS, Rappa HA, Lesser M, et al. CPR knowledge, self-efficacy, and anticipated anxiety as functions of infant/child CPR training. Ann Emerg Med 1995;25:618–23. 10.1016/S0196-0644(95)70174-5 [DOI] [PubMed] [Google Scholar]
- 38.Flint LS Jr, Billi JE, Kelly K, et al. Education in adult basic life support training programs. Ann Emerg Med 1993;22:468–74. 10.1016/S0196-0644(05)80479-2 [DOI] [PubMed] [Google Scholar]
- 39.Knowles MS. Andragogy in action: applying modern principles of adult education. San Francisco, CA: Jossey Bass, 1984. [Google Scholar]
- 40.Issenberg SB, McGaghie WC, Petrusa ER, et al. Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Med Teach 2005;27:10–28. 10.1080/01421590500046924 [DOI] [PubMed] [Google Scholar]
- 41.Cheng A, Auerbach M, Hunt EA, et al. Designing and conducting simulation-based research. Pediatrics 2014;133:1091–101. 10.1542/peds.2013-3267 [DOI] [PubMed] [Google Scholar]