Abstract
The increasing use of emerging technologies in healthcare simulation, particularly virtual reality, has caused in increase in both use and misuse. It is the exploration and study of these types of technology that are key to their success—or failure—in simulation learning and teaching. Therefore, this exploratory study evaluated the most common perceived side effect of virtual reality, that of cybersickness. A total of n=60 undergraduate healthcare students participated in one of four identical learning outcome simulation events, using different simulation techniques. This study compared these four common simulation tools, high-fidelity manikin, standardised patient, video case study and 360-degree virtual reality video, and analysed the self-reported cybersickness symptoms. The results show that some virtual reality tools, in this case 360-degree video, are no more likely to provoke cybersickness symptoms than the other simulation methods used in this study. In addition, virtual reality is reported as less fatiguing than other methods of simulation learning. Virtual reality technologies may be a useful addition to the spectrum of simulation tools and techniques currently in use. This study suggests that there is no greater risk of cybersickness symptoms and this potential barrier to use is not borne out by this study.
Keywords: virtual reality, cybersickness, 360-degree video
Introduction
If the goal of virtual reality is immersing a learner, via multiple sense inputs, to create an illusion of being present in a simulated environment, then this surely is the goal of simulation as a pedagogical tool in healthcare. To what degree the learner is immersed depends on a number of factors, but mostly relate to the clarity, and reality, of the virtual environment. As part of this, virtual reality is seemingly the answer to the harassed simulation educator’s prayers. No more manikins or standardised patients. The endless replicability of learning environments and immersive experiences, enjoyed both by students and those who fund new and emerging technologies alike. There are no physical constraints in the virtual reality environment, with the limits of imagination bounding the healthcare simulation of the future. However, in reality, virtual reality may have some impactful physical limitations. As virtual reality has evolved over the last decades, a key negative side effect of its use has been the feeling, similar to motion sickness, called cybersickness.1 Physiological mechanisms that cause cybersickness are poorly understood but the emetic chemoreceptor trigger zone has been shown to be non-essential for motion sickness vomiting and a different mechanism.2
Cybersickness
Cybersickness is a feeling of sickness or a feeling of malaise due to exposure to virtual reality. However, it is often confused with vection; this is the illusion of self-motion when experiencing visual motion information. This is a related but entirely distinct phenomenon.3 The symptoms of cybersickness are varied and subjective in that they are subjective according to the user. The symptoms may include dizziness, nausea, eye strain and/or a feeling of fatigue. There is some evidence that observing virtual reality, rather than actively taking part, is more likely to provoke motion sickness. This phenomenon has been noted in car passengers, who seemed to suffer motion sickness more than drivers.4 However, scant evidence exists to support the ‘watching’ rather than ‘doing’ provocation of cybersickness.
Simulator Sickness Questionnaire
Therefore, the consideration of the impact of cybersickness in healthcare simulation learning and teaching may be to understand its psychological construct rather than its physiological triggers. This is where the Simulator Sickness Questionnaire (SSQ)5 may be useful. This questionnaire is the standard measure of the psychological construct of cybersickness, in other words, the subjective negative psychological effects of using virtual reality. The SSQ was developed to measure feelings of sickness in military pilots when using simulators. A 28-item questionnaire was given both before and after over a thousand simulated flights in 10 different flight simulators.6 Items that had a low frequency response were eliminated from the questionnaire, and principal-factors analysis and normalised varimax rotation were carried out, leaving a three-factor, partially independent solution.
360-Degree video
Omnidirectional video, also called 360-degree video or 360 video or virtual reality video, is the production of a video sphere where the user’s head or point of view is in the centre of that sphere. Users have the ability to look around in 3DOF (three degrees of freedom); this is achieved by capturing all the possible angles in any scene using multiple cameras and then ‘stitching’ the images together to create an equirectangular image or video that can be viewed in virtual reality headsets. The video used for this study was 30 fps (frames per second) and was shown on Samsung S6 and Gear VR (5.1-inch display with a 1440×2560 p Quad HD resolution) along with the Pico Goblin (5.5″ Super-fast TFT LCD Resolution 2560×1440). A screenshot of the environment used for this experiment is shown in figure 1.
Figure 1.
Screenshot of 360-degree pharmacy environment used in this study.
Method
Although the analyses used for this non-parametric test violates the assumptions for the common Cohen’s formula for sample and effect size, other tests are available and well evidenced.7 Therefore, Rosenthal’s calculation for the Wilcoxon matched-pairs signed-rank test was used to calculate sample size.8 This was based on an significance ‘α’ level of 0.05. Based on this sample calculation, participants were purposively sampled from currently enrolled cohorts of all undergraduate health courses at Coventry University, who took part in interprofessional education simulation days or health leadership learning group (n=65), and randomly allocated to either the 360-degree video ‘virtual reality-VR’ learning condition or non-360-degree video simulation ‘non-VR’ learning condition. Therefore, of the total number of students who took part (n=65), n=62 completed the survey, with n=2 online responses discarded, due to duplicated Internet Protocol (IP) address.
The non-VR learning condition had three subconditions: manikin or standardised patient or video case study condition. The simulation learning outcomes were identical in all conditions and all simulations lasted 30 min, including debriefing time. The learning outcomes were based on the 2016 version of the Core Competencies for Interprofessional Collaborative Practice.9
All participants completed the SSQ immediately after participation in one of the four simulation conditions. To ensure response bias was minimised, participants were unaware of the nature of the SSQ or the cybersickness aspect of the study, and the questions were framed as an evaluation of the simulation event as a whole and not as any one tool. The responses were collected via anonymous QR matrix bar code linked to an organisation-supported Bristol Online Survey data collection tool. The Simulator Sickness Survey was converted to a web form, but all items and response options were identical to the hard-copy version.
Results
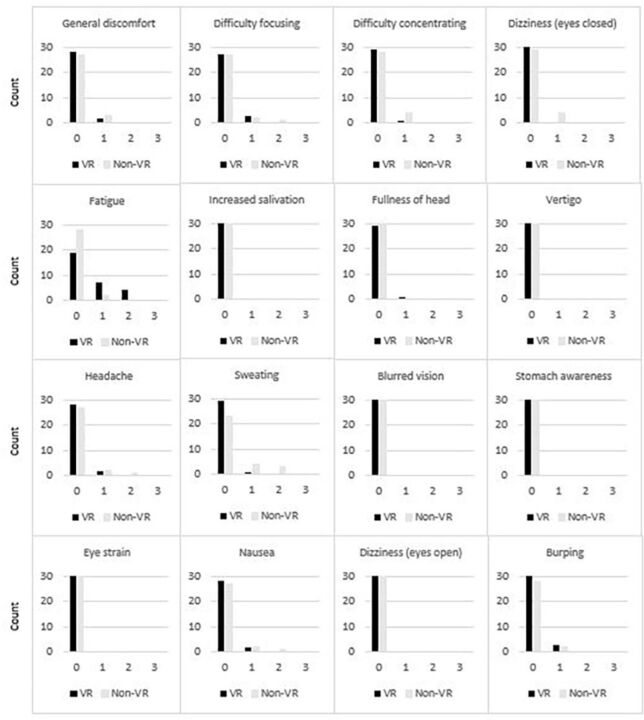
The final number of participants was n=60, randomly allocated to one of four conditions: 360-degree video (n=30), non-360-degree video—manikin (n=10), non-360-degree video—standardised patient (n=10) and non-360-degree video—video case study (n=10). The table grid (figure 2) shows the analysis of cybersickness symptoms, as outlined in the SSQ in the 360-degree video ‘VR’ and non-360-degree video ‘non-VR’ conditions.
Figure 2.
Comparison of VR and non-VR cybersickness symptoms reported.
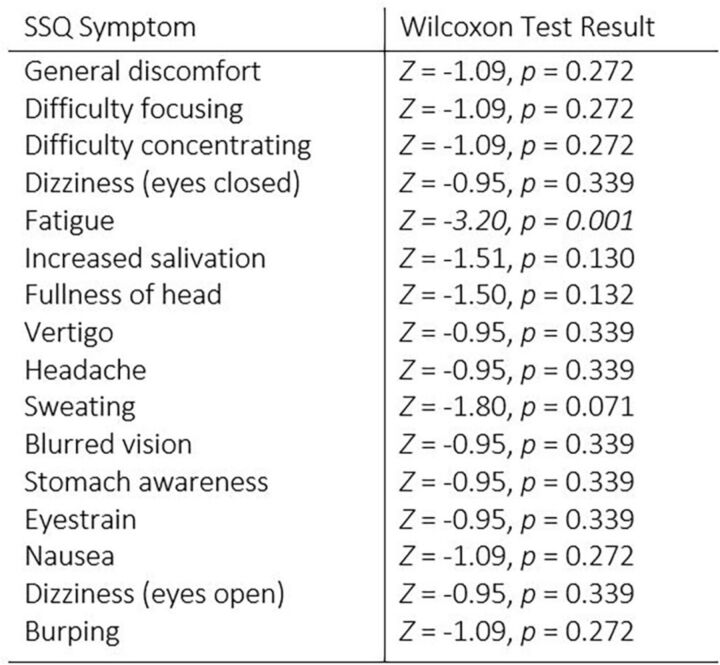
The results of the responses to the SSQ for all four conditions, split equally between the VR and non-VR groups, were analysed using the non-parametric Wilcoxon matched-pairs signed-rank test. This non-parametric test was used as no assumptions were made about the normality of distribution of the data. The results of this analysis can be seen in figure 3. Using the alpha level outlined, the fatigue symptom of participants in the non-VR condition is statistically significantly higher than those in the VR condition (Z=−3.20, p=0.001). No other statistically significant effects between conditions were found (Z=−0.95 to −1.80, p=0.071 to 0.339).
Figure 3.
Wilcoxon matched-pairs signed-rank test results for Simulator Sickness Questionnaire (SSQ) data.
Discussion
This study sought to determine the level of cybersickness symptoms in common simulation learning and teaching tools, specifically 360-degree video, manikin, standardised patient and video case study. The results of this study indicate that there are no greater self-reported symptoms of cybersickness when using a virtual reality tool compared with the other three common simulation tools.
This is contrary to the general acceptance that virtual reality, and in particular, virtual reality used while wearing a headset, provokes negative symptoms.10 11 These negative symptoms, known collectively as cybersickness, can be seen as a barrier to the use of this emerging technology and is generally regarded as its main impactor as a useful tool.12 This is not borne out by the findings in this study and no increase in symptoms was reported by participants in the virtual reality condition. Whether this is due to the photorealism aspect of this tool or the image refresh rate or alteration to field of view13 needs further exploration.
However, the key finding, as seen in this study, in that most of the symptom items, the differences in reported issues were negligible or not statistically significant, meaning that, in this type of photorealistic virtual reality, cybersickness is not a negative impactor on its use. An additional finding was a statistically significant increase in self-reported fatigue reported in those participants in the non-VR group. Meaning that other, non-360-degree video, simulation tools were reported as more fatiguing for participants. This is, therefore, part of the start of a discussion on the use of virtual reality tools in healthcare simulation, and one that will evolve as the technologies evolve.14
Conclusion
In conclusion, this experiment shows that, in this study, participants were no more likely to suffer cybersickness than when using other, well-established, simulation tools. Therefore, this should not be a barrier to its use and evaluation as a healthcare simulation learning and teaching technique. The next phase in this research project, which is ongoing, is an evaluation of cybersickness symptoms in more immersive realities, specifically room-scale virtual reality; results will be disseminated.
In addition, further study is required to evaluate virtual reality as a useful tool for cognitive change, and it is not merely sufficient that these technologies do not cause negative effects; the next step is to evaluate their positive effects.
Acknowledgments
The authors wish to acknowledge Alex Harvey and Brad Woodward from RiVR: Reality in Virtual Reality (https://www.rivr.uk/) for their technological assistance and support in this study.
Footnotes
Contributors: NT wrote ethical approval, study design and statistical analysis. NT and AL organised the simulation events, collected data and collaborated on the writing of the paper.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Ethics approval: This study is subject to Coventry University ethical approval processes and gained ethical approval, reference number P69909.
Provenance and peer review: Not commissioned; internally peer reviewed.
References
- 1. McCauley ME, Sharkey TJ. Cybersickness: perception of self-motion in virtual environments. Presence 1992;1:311–8. 10.1162/pres.1992.1.3.311 [DOI] [Google Scholar]
- 2. Rebenitsch L, Owen C. Review on cybersickness in applications and visual displays. Virtual Real 2016;20:101–25. 10.1007/s10055-016-0285-9 [DOI] [Google Scholar]
- 3. Keshavarz B, Riecke BE, Hettinger LJ, et al. Vection and visually induced motion sickness: how are they related? Front Psychol 2015;6:472. 10.3389/fpsyg.2015.00472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chen Y-C, Dong X, Hagstrom J, et al. Control of a virtual ambulation influences body movement and motion sickness. BIO Web of Conferences 2011;1:00016. 10.1051/bioconf/20110100016 [DOI] [Google Scholar]
- 5. Kennedy RS, Lane NE, Berbaum KS, et al. Simulator Sickness Questionnaire: an enhanced method for quantifying simulator sickness. Int J Aviat Psychol 1993;3:203–20. 10.1207/s15327108ijap0303_3 [DOI] [Google Scholar]
- 6. Kennedy RS, Lilienthal MG, Berbaum KS, et al. Simulator sickness in U.S. Navy flight simulators. Aviat Space Environ Med 1989;60:10–16. [PubMed] [Google Scholar]
- 7. Fritz CO, Morris PE, Richler JJ. Effect size estimates: current use, calculations, and interpretation. J Exp Psychol Gen 2012;141:2–18. 10.1037/a0024338 [DOI] [PubMed] [Google Scholar]
- 8. Rosenthal R. Parametric measures of effect size. In: Cooper H, Hedges LV, The handbook of research synthesis. edn. New York: Russell Sage Foundation, 1994:231–44. [Google Scholar]
- 9. Interprofessional Education Collaborative Expert Panel. Core competencies for interprofessional collaborative practice: report of an expert panel. 2011. https://www.ipecollaborative.org/resources.html.
- 10. Moss JD, Muth ER. Characteristics of head-mounted displays and their effects on simulator sickness. Hum Factors 2011;53:308–19. 10.1177/0018720811405196 [DOI] [PubMed] [Google Scholar]
- 11. Nalivaiko E, Davis SL, Blackmore KL, et al. Cybersickness provoked by head-mounted display affects cutaneous vascular tone, heart rate and reaction time. Physiol Behav 2015;151:583–90. 10.1016/j.physbeh.2015.08.043 [DOI] [PubMed] [Google Scholar]
- 12. Cobb SVG. Measurement of postural stability before and after immersion in a virtual environment. Appl Ergon 1999;30:47–57. 10.1016/S0003-6870(98)00038-6 [DOI] [PubMed] [Google Scholar]
- 13. Fernandes AS, Feiner SK. Combating VR sickness through subtle dynamic field-of-view modification. 2016:201–10. 10.1109/3DUI.2016.7460053 [DOI]
- 14. LaViola JJ. A discussion of cybersickness in virtual environments. ACM SIGCHI Bulletin 2000;32:47–56. 10.1145/333329.333344 [DOI] [Google Scholar]