Abstract
Background
Obesity can often be a barrier to gender-affirming top surgery in transmasculine patients due to concern for increased surgical site complications.
Study Design
All adult patients (N=948) within an integrated health care system who underwent gender-affirming mastectomy from 2013–2018 were retrospectively reviewed to evaluate the relationship between obesity and surgical site complications or revisions.
Results
One-third of patients (n=295) had obese body mass index (BMI), and those patients were further stratified into obesity class I (BMI 30–34.9, 9.4%), class II (BMI 35–39.9, 8.9%), and class III (BMI ≥40, 2.9%). A majority of patients across BMI categories underwent double incision surgery. There were no significant differences in complications or revisions between patients with obesity versus those with normal BMI, when BMI was treated as a categorical or continuous variable and when evaluating only patients who underwent double incision surgery.
Conclusion
Obesity alone should not be considered a contraindication for gender-affirming mastectomy. Attention should be given to several modifiable risk factors identified in this study, including lesser incision surgical techniques, tobacco use, and testosterone use. Further research is needed to understand risks associated with the highest BMI (≥40) patients and to assess patient satisfaction with surgical outcome.
Keywords: top surgery, transgender surgery, gender affirmation surgery, obesity, surgical complications
Introduction
Obesity is associated with higher risk of surgical site complications in some studies,(1–3) leading some providers to restrict surgical access in obese patients.(4, 5) For overweight transmasculine patients who wish to undergo gender-affirming mastectomy, preoperative weight loss can be challenging.(5) The stigma of being transgender appears to limit opportunities and access, negatively affecting the physical and mental health of transgender people.(6–8) Transgender patients are more likely to be obese and use tobacco, and are less likely to participate in sufficient exercise than their non-transgender counterparts.(5, 9) Transgender patients are less likely to exercise regularly,(10) and report disproportionate rates of unsafe weight management behaviors(11) and depression prior to gender-affirming treatment.(12) Furthermore, transgender patients may be at increased risk of suicide(13) when gender dysphoria is untreated. For the highest BMI patients who tend to have larger breasts, which are not possible to conceal with binding, this stigma can put patients at even greater risk of violence within communities.(14)
Existing literature rarely describes surgical outcomes in transgender patients with obesity,(15) with the average body mass index (BMI) of most cohorts ranging from 22.7 to 28.6.(16–18) We therefore sought to determine the association of BMI with surgical complications and revision in a cohort of almost 1,000 patients, 31% of whom had a BMI of >30, who underwent gender-affirming mastectomy within our integrated health system.
Methods
Kaiser Permanente Northern California (KPNC) is a large, not-for-profit integrated healthcare system that provides comprehensive care to over 4 million members. Health insurance coverage for gender-affirming mastectomy in KPNC members started in April 2013. Patients access the gender-affirming surgery program directly by self-referral or through healthcare provider referral to a centralized clinical hub based in Oakland, California. Prior to surgery, all patients are evaluated by licensed mental health gender specialists, as recommended in the World Professional Association for Transgender Health Standards of Care.(19) Patients ≥18 years who were referred for top surgery between January 1, 2013 and November 1, 2018 were retrospectively identified in our institutional database. Patients identified as either transmasculine or non-binary. We excluded patients with a history of prior breast surgery and patients with <30 days follow-up (days of postoperative clinical records in our electronic health record). Patient demographics and surgical characteristics were collected by manual chart review using a standardized data collection tool. The exposure of interest was BMI at the time of surgery, which was used in our analysis as both a continuous variable and a categorical variable (<25 underweight/normal, 25–29.9 overweight, ≥30 obese). Our outcomes of interest were any complication and any post-operative intervention, including revision. As we did not find any major medical postoperative complications such as deep venous thrombosis, pulmonary embolism, reintubation, or death, we defined complication as having any of the following: infection (suture abscess or cellulitis), dehiscence, hematoma (requiring aspiration or operative evacuation), seroma, and nipple areolar complex (NAC) complications (necrosis or non-take).(17, 18, 20–22) Revisions were defined as any bedside or operative procedure in the post-operative period related to the index surgery, which included NAC hypopigmentation requiring tattoo or excision, hypertrophic scar requiring steroid injection, and revision for aesthetic concerns including NAC, contour, scar, or other. Most of our surgeons wait at least one year before performing any type of major revision, therefore revision analyses were limited to patients with >1-year follow-up. Patients are individually counseled that high BMI can be associated with difficulty creating an optimal chest contour which may only be achieved with surgical revision. Therefore, obese patients with large amounts of skin and fatty excess lateral to the breast mound were advised that two stages of surgery would be required; these patients were categorized as having a revision. All patients who so desired were offered revision provided they had realistic expectations for aesthetic outcome, and requests for surgical revision were initiated by the patient rather than by the surgeon. Given the structure of our integrated healthcare system, revision for any reason is covered by insurance.
Covariates included age at time of surgery, race/ethnicity (Black, Latinx, White, or Other), American Society of Anesthesiologists (ASA) Classification (I,II or III/IV), tobacco use (never or former), preoperative testosterone use (yes or no), and surgical technique (double incision,(18) circumareolar/periareolar,(16, 20) keyhole,(18) or buttonhole,(23); Appendix A).(24) At our institution, all patients who plan to undergo elective plastic surgery are required to stop tobacco and all products containing nicotine for at least three months prior to surgery; extensive counseling on smoking cessation is provided at multiple touchpoints prior to surgery. There is no department standard for confirming smoking cessation and nicotine testing is not routinely performed, thus some patients may have still been active smokers. With this discrepancy in mind, we categorized all patients with history of tobacco use as former smokers.
We compared patient demographics using descriptive statistics. We evaluated the associations between patient demographics and characteristics with our outcomes of interest using chi-square, Fisher’s exact, student’s T-Tests, ANOVA, and univariate logistic regression with a significance level of p<0.05. Regression models evaluated the association between patient BMI (both as a continuous and categorical variable) and any surgical complication or revision. Variables with a p-value ≤0.2 on univariate regression were selected as covariates for our multivariable logistic regression models.
We used Stata version 15 (College Station, TX: Stata Corp LP) for all analyses. The study protocol was reviewed and approved by the Kaiser Permanente Northern California Institutional Review Board, which provided a waiver of informed consent.
Results
We included a total of 948 patients whose mean age was 29.1 years (SD 9.5), and 62.7% (594/948) were white. Mean follow-up was 1.9 ± 1.4 years. Average BMI was 27.2 (SD 5.8) with 295 (31.1%) obese patients (Figure 1). An average 486.9 grams (SD 350.3) of tissue were removed from each breast. Seventy one percent (531/754) of patients were taking preoperative testosterone, and most (88.2%, 836/948) underwent double incision with free nipple graft technique.
Figure 1. Box and whisker plot illustrating the BMI distribution of patients with whiskers to maximum and minimum BMI excluding outliers (dots).

The patient demographics and surgical characteristics are demonstrated in Table 1, stratified by weight category. Obese patients tended to be slightly older (mean 31.5 years, SD 10.2) compared to the overweight patients (28.9 years, SD 9.4) and underweight/normal patients (27.2 years, SD 8.5); p<0.001. The obesity category had a higher proportion of Black (12.5%) and Latinx (19.3%) patients compared to the overweight and underweight/normal groups. Obese patients also had a higher proportion of ASA Class III/IV patients and former tobacco users. While most patients underwent the double incision with free nipple graft technique, the proportion of obese patients who had the double incision technique was significantly higher (97.0% versus 90.3% overweight versus 79.0% underweight/normal; p<0.001).
Table 1.
Patient demographics and surgical characteristics for the study cohort, stratified by obesity status.
| Characteristic | Underweight/Normal BMI<25 N=353 (37.2%) |
Overweight 25≤BMI<30 N=300 (31.7%) |
Class I 30≤BMI<35 N=184 (19.4%) |
Class II 35≤BMI<40 N=84 (8.9%) |
Class III 40≥BMI N=27 (2.9%) |
p-value |
|---|---|---|---|---|---|---|
| Age (years), Mean [SD] | 27.2 [8.5] | 28.9 [9.4] | 31.0 [10.3] | 32.1 [9.8] | 32.9 [10.0] | <0.001 |
| Body Mass Index (BMI, kg/m2), Mean [SD] | 21.7 [1.9] | 26.7 [1.3] | 31.9 [1.4] | 36.7 [1.3] | 43.4 [3.3] | <0.001 |
| Race/Ethnicity, N (%) | 0.02 | |||||
| White | 243 (68.8) | 178 (59.3) | 110 (59.8) | 48 (57.1) | 15 (55.6) | |
| Black | 24 (6.8) | 32 (10.7) | 19 (10.3) | 12 (14.3) | 6 (22.2) | |
| Latinx | 44 (12.5) | 48 (16.0) | 34 (18.5) | 17 (20.2) | 6 (22.2) | |
| Other | 42 (11.9) | 42 (14.0) | 21 (11.4) | 7 (8.3) | 0 | |
| ASA Class, N (%) | <0.001 | |||||
| I | 165 (46.7) | 142 (47.3) | 41 (22.3) | 6 (7.1) | 0 | |
| II | 185 (52.4) | 156 (52.0) | 136 (73.9) | 71 (84.52) | 15 (55.6) | |
| III/IV | 3 (0.9) | 2 (0.7) | 7 (3.8) | 7 (8.3) | 12 (44.4) | |
| Former Tobacco Use, N (%) | 109 (30.9) | 97 (32.3) | 74 (40.2) | 34 (40.5) | 11 (40.7) | 0.13 |
| Preoperative Testosterone, N (%) | 247 (70.0) | 207 (69.0) | 134 (72.8) | 60 (71.4) | 22 (81.5) | 0.65 |
| Surgical Technique, N (%) | <0.001 | |||||
| Buttonhole | 21 (6.0) | 10 (3.3) | 4 (2.2) | 2 (2.4) | 0 | |
| Circumareolar/Periareolar | 36 (10.2) | 11 (3.7) | 3 (1.6) | 0 | 0 | |
| Double Incision | 279 (79.0) | 271 (90.3) | 177 (96.2) | 82 (97.6) | 27 (100) | |
| Keyhole | 17 (4.8) | 8 (2.7) | 0 | 0 | 0 | |
| Average Tissue Removed (g), Mean [SD] | 258.7 [167.2] | 457.6 [255.4] | 707.3 [331.5] | 870.0 [372.2] | 1100.9 [447.4] | <0.001 |
| Drain Use, N (%) | 183 (51.8) | 155 (51.7) | 98 (53.3) | 51 (60.7) | 8 (29.6) | 0.09 |
Abbreviations: Body Mass Index (BMI), Standard Deviation (SD), American Society of Anesthesiologists (ASA).
A total of 82/948 (8.6%) patients had at least one complication (Figure 2), and there were a total of 89 complications. Of the complications, hematoma requiring operative evacuation was the most prevalent (27/89, 30% of all complications and 27/948, 2.8% of all patients) and only complication requiring urgent return to the operating room, followed by hematoma requiring aspiration (17/89, 19%), seroma (16/89, 18%), and cellulitis (12/89, 13%). In univariate and adjusted analyses (Table 3) for the outcome of any complication, overweight and obese patients did not have significantly higher odds of complications compared to those with normal BMI (Overweight aOR 1.02 [95% CI 0.58–1.78]; Obesity Class I aOR 0.93 [0.48–1.78]; Obesity Class II aOR 0.99 [0.43–2.29]; Obesity Class III aOR 1.17 [0.32–4.26]). Additionally, when the analysis was repeated including only patients who underwent double incision surgery, there was no difference in odds of complication between patients with obese and non-obese BMI. There was no predominant complication type among patients with obese BMI. History of tobacco use (aOR 1.60 [1.00–2.55]) and preoperative testosterone (aOR 1.77 [1.00–3.12]) were associated with higher odds of complications. In a sensitivity analysis, we also treated BMI as a continuous variable, and again found no meaningful effect with regard to postoperative complications (OR 1.02 [0.97–1.06].
Figure 2.
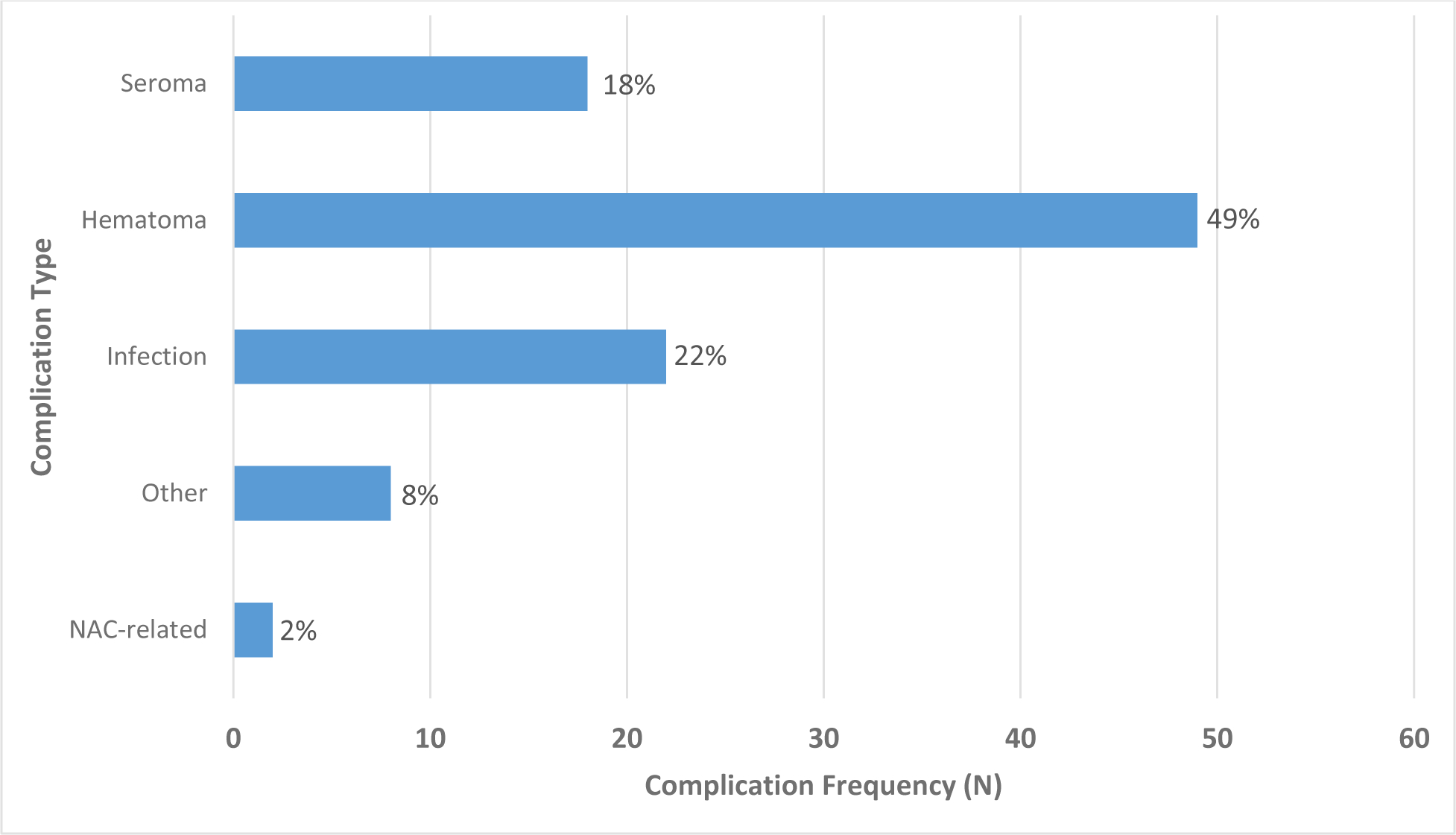
Frequency of surgical complication types following top surgery. A total of 82 patients experienced 89 complications.
Table 3.
Univariate logistic regression results (first set of columns) and multivariable logistic regression results (second set of columns) for the outcome of any revision. Only patients with >1-year follow-up time were included in this analysis. A total of 121/615 patients (19.7%) experienced at least one revision after surgery. Body mass index (BMI) category was not associated with increased odds for revision in either univariate or multivariable logistic regression.
| Characteristic | OR | 95% CI | p-value | aOR | 95% CI | p-value |
|---|---|---|---|---|---|---|
| Age (Years), Mean [SD] | 1.05 | 1.03–1.07 | <0.001 | 1.05 | 1.03–1.07 | <0.001 |
| BMI (kg/m2) | ||||||
| Underweight/Normal (<25) | Ref | Ref | Ref | Ref | Ref | Ref |
| Overweight (25–29.9) | 1.28 | 0.80–2.04 | 0.31 | 1.15 | 0.70–1.91 | 0.58 |
| Class I Obesity (30–34.9) | 0.82 | 0.45–1.49 | 0.52 | 0.64 | 0.33–1.21 | 0.17 |
| Class II Obesity (35–39.9) | 0.78 | 0.37–1.64 | 0.51 | 0.69 | 0.31–1.53 | 0.36 |
| Class III Obesity (≥40) | 0.62 | 0.18–2.17 | 0.45 | 0.46 | 0.12–1.74 | 0.26 |
| Race/Ethnicity, N (%) | ||||||
| White | Ref | Ref | Ref | Ref | Ref | Ref |
| Black | 2.19 | 1.24–3.87 | 0.01 | 2.23 | 1.23–4.07 | 0.009 |
| Latinx | 1.06 | 0.59–1.91 | 0.85 | 1.32 | 0.71–2.43 | 0.38 |
| Other | 1.99 | 1.08–3.67 | 0.03 | 2.11 | 1.12–4.00 | 0.02 |
| ASA Class, N (%) | ||||||
| I | Ref | Ref | Ref | -- | -- | -- |
| II | 0.81 | 0.53–1.22 | 0.31 | -- | -- | -- |
| III/IV | 0.62 | 0.20–1.86 | 0.39 | -- | -- | -- |
| Former Tobacco Use, N (%) | 0.81 | 0.53–1.23 | 0.32 | -- | -- | -- |
| Preoperative Testosterone, N (%) | 0.65 | 0.43–0.98 | 0.04 | 0.74 | 0.47–1.14 | 0.17 |
| Surgical Technique, N (%) | ||||||
| Double Incision | Ref | Ref | Ref | Ref | Ref | Ref |
| Buttonhole | 0.63 | 0.18–2.15 | 0.46 | 0.77 | 0.22–2.72 | 0.68 |
| Circumareolar/Periareolar | 1.05 | 0.42–2.63 | 0.92 | 1.24 | 0.47–3.29 | 0.67 |
| Keyhole | 2.93 | 1.09–7.89 | 0.03 | 3.51 | 1.23–10.06 | 0.02 |
| Average Tissue Removed (g), Mean [SD] | 1.00 | 0.99–1.00 | 0.97 | -- | -- | -- |
| Drain Use, N (%) | 1.14 | 0.75–1.73 | 0.54 | -- | -- | -- |
Abbreviations: Body Mass Index (BMI), Standard Deviation (SD), American Society of Anesthesiologists (ASA).
A total of 615 patients were eligible for revision analysis given a minimum of one-year follow-up, of whom, 121/615 (19.7%) had at least one revision (Table 3). Because some patients had more than one revision, there were 185 revisions overall: the majority were scar revisions (62/121, 51%), followed by contour revisions (44/121, 36%), and steroid injections for hypertrophic scarring (28/121, 23%); Figure 3. In univariate and adjusted analyses for the outcome of any revision, (Table 3), older age (aOR 1.05 [1.03–1.07]), Black patients (compared to White patients; aOR 2.20 [1.21–4.01]), and the use of the keyhole technique (compared to double incision; aOR 3.5 [1.23–10.06]) were significantly associated with higher odds of revision. We found no association between BMI category and need for revision (Overweight aOR 1.15 [0.70–1.91]; Obesity Class I aOR 0.64 [0.33–1.78]; Obesity Class II aOR 0.69 [0.31–1.53]; Obesity Class III aOR 0.46 [0.12–1.74]) when treated as a categorical variable or as a continuous variable (OR 0.99 [0.95–1.02]). Again, evaluation of only patients who underwent double incision surgery demonstrated no difference in odds of revision.
Figure 3.

Frequency of revision procedures performed among patients after top surgery. A total of 121 patients experienced 185 revisions.
Discussion
In this retrospective study, we investigated whether BMI was associated with surgical complications and revisions after gender-affirming mastectomy. We found no statistically significant differences in complications or revisions between patients with obese versus normal BMI; therefore, elevated BMI alone should not be a barrier to undergoing gender-affirming mastectomy. Instead, independent risk factors for complications including minimal incision techniques, history of tobacco use, and testosterone use should be considered when risk-stratifying.(25, 26)
Gender-affirming mastectomy involves a variety of operations designed to remove breast tissue and flatten the chest, generally removing less tissue than mastectomy for cancer, and a greater volume of tissue compared to standard reduction mammaplasty. Mastectomy for cancer must be performed in a timely manner, which often does not allow for preoperative smoking cessation. Furthermore, the surgical technique relies on thinner skin flaps which are more sensitive to ischemia and necrosis. In contrast, the flaps for the obese transgender patient are often thick and undermining is less extensive in order to match the thick subcutaneous fat layer of the adjacent abdominal wall and avoid contour depression (Supplemental Digital Content). The double-incision technique most commonly used for gender-affirming mastectomy is considerably simpler than for reduction mammaplasty, as the procedure is typically performed with a free NAC graft rather than by retaining the NAC on a pedicle. The differences between these procedures and their clinical context invalidate comparisons. (20, 27, 28) While there is some overlap with gynecomastia surgical techniques for cis-male patients, there are several differences. For example, testosterone use is unique to the transmasculine patient population, and may be associated with breast deflation and skin laxity. In this study, we found that testosterone use was associated with increased complication rates, particularly involving hematoma (33/65 testosterone users with complication, 51%). Overall, the decision to discontinue testosterone use for a period before top surgery is surgeon-specific, and no standard of care exists.(29, 30)
The relationship between obesity and complication rate after reduction mammaplasty has been studied in a large American College of Surgeons-National Surgical Quality Improvement Program review and meta-analyses, which report that for reduction mammaplasty, obesity is associated with a greater risk of surgical site complications including infection and necrosis.(1, 2) A second NSQIP study comparing outcomes after transmasculine top surgery versus prophylactic mastectomy in cisgender females reported lower overall complication rates in transmasculine patients, and a positive correlation between obesity and wound and overall complication rate.(28) These findings parallel studies demonstrating a positive correlation between surgical site complication rate and obesity for a variety of operations including cardiothoracic, joint replacement, breast, and intra-abdominal surgeries.(3) However, key differences between the NSQIP study population and our own may contribute to differences in outcome. For example, almost 15% of surgeons who performed transgender top surgery were general surgeons (27) while in our study, only plastic surgeons performed top surgery. In addition to this difference in surgeon training, surgical volume, surgical techniques, potential adjunctive operations such as liposuction and lateral chest roll excision, and familiarity with high BMI patients may contribute to disparate outcomes. Notably, the anesthesiologists at our institution are experienced treating patients with high BMI as they are part of a high-volume bariatric surgery program, and approximately 1/3 of our cohort underwent surgery with these anesthesia teams.
Our encouraging findings among patients undergoing gender-affirming mastectomy may be related to surgical volume, surgical technique, and familiarity with operating on patients with obese BMI as these factors may affect surgical site complication rate for obese patients.(31, 32) Furthermore, thicker skin flaps and lesser degree of undermining in obese patients may contribute to fewer complications. In our study, nearly all patients with obese BMI underwent double incision surgery, the technique associated with the lowest complication or revision risk across BMI categories, while 9.7% and 21% of patients with normal or overweight BMI, respectively, underwent surgery by other less reliable lesser incision techniques. This may have contributed to an equalization of complication and revision rate between the groups. However, a subgroup analysis that included only patients who underwent double incision surgery also demonstrated no difference in complication or revision across BMI categories (Appendix B).
Studies evaluating risk factors for surgical site complications after top surgery are variable with regards to surgical techniques and terminology. The surgeons in our integrated healthcare system use the following four techniques: double incision, circumareolar/periareolar, keyhole, and buttonhole.(24) Our results agree with the consensus in the literature, which reports higher complication rates when using minimally visible incision techniques, such as circumareolar/periareolar or keyhole surgery, which allow lesser access to control bleeding and perform precise tissue contouring.(20, 33, 34) The double incision technique, with NAC graft and a long transverse scar across the chest, is the usual approach for patients with large breasts, and is consistently reported to have the lowest complication rate, in agreement with our findings.(20, 34) Since obesity is correlated with larger breast size, obese patients tend to undergo top surgery via a double incision technique, which is the lowest-risk approach. Nearly all of our patients with an overweight or obese BMI underwent surgery via a double incision technique and had the lowest postoperative complication rate among our patient population. However, selection of patients with obesity for top surgery who were otherwise healthy may have produced an enriched cohort of healthy patients, thereby producing an overall lower risk of postoperative complications.
Our study is limited by its retrospective nature as well as variability in postoperative follow-up time, as patients with <30 day follow up were excluded from complication rate and patients with less than one year follow up were excluded from revisions, which may have resulted in lead-time bias. However, the mean follow-up time was 2.2 ± 1.4 years (SD 1.4), and greater than 75% of patients had a follow up time of over one year, which should be adequate for capturing surgical complications. Some patients may also have transitioned their care to outside our system or lost their healthcare access, and therefore may have been misclassified as free of complications. These theoretical shortcomings are minimal given high patient retention rate and an electronic medical record system that allows access to electronic charts from outside hospitals.(35, 36) Our study is also unable to account for possible clustering by surgeon and medical center and, given the low number of outcome events, it is possible that the study was insufficiently powered to detect differences in complications or revisions across BMI categories (underweight, normal, overweight, obesity classes I-III). Notably, there were only 27 patients in the obesity class III category, attributable to pre-operative screening for co-morbidities by surgeons; assessment of a greater number of class III patients may expose differences in outcome that were not identified in this study. Patient satisfaction was also not evaluated, which is a necessary factor to consider when studying surgical outcomes. When considering revisions, it is conceivable that the highest BMI patients have less concern with standing cone (dog ear) deformities compared to patients with low or normal BMI. Finally, our data was collected from a single, integrated healthcare system and all patients are insured; a minority of patients receive care within this type of healthcare system, which may limit generalizability of these data.
Conclusions
Our study suggests that gender affirming mastectomy in otherwise healthy obese patients does not result in greater complications or revisions, which may be attributable, in part, to using the double incision technique in a majority of these patients. Therefore, recommendations for preoperative weight loss, which is unlikely to be successful,(5) may not be warranted if the patient is otherwise healthy enough to undergo surgery with minimal risks. We found that minimal incision techniques, testosterone use, and history of tobacco use were all risk factors for complications, which should be considered during pre-operative planning. A shared decision-making model should be used to select operative technique and manage testosterone use, and plastic surgeons should continue to support preoperative smoking cessation among patients. As surgeon experience with gender-affirming mastectomy in obese BMI increases, it is imperative that research efforts be devoted to characterizing risk factors specific to gender-affirming surgery, and to analyzing patient satisfaction outcomes.
Supplementary Material
Table 2.
Univariate logistic regression results (first set of columns) and multivariable logistic regression results (second set of columns) for the outcome of any complication. A total of 82/948 patients (8.7%) experienced any complication after surgery. Body mass index (BMI) category was not associated with increased odds for complication in either univariate or multivariable logistic regression.
| Characteristic | OR | 95% CI | p-value | aOR | 95% CI | p-value |
|---|---|---|---|---|---|---|
| Age (Years) | 1.02 | 1.00–1.04 | 0.08 | 1.02 | 0.996–1.04 | 0.11 |
| BMI (kg/m2) | ||||||
| Underweight/Normal (<25) | Ref | Ref | Ref | Ref | Ref | Ref |
| Overweight (25–29.9) | 1.06 | 0.61–1.84 | 0.84 | 1.02 | 0.58–1.78 | 0.96 |
| Class I Obesity (30–34.9) | 1.06 | 0.56–2.01 | 0.85 | 0.93 | 0.48–1.78 | 0.83 |
| Class II Obesity (35–39.9) | 1.18 | 0.52–2.67 | 0.70 | 0.99 | 0.43–2.29 | 0.98 |
| Class III Obesity (≥40) | 1.40 | 0.40–4.91 | 0.60 | 1.17 | 0.32–4.26 | 0.81 |
| Race/Ethnicity | ||||||
| White | Ref | Ref | Ref | -- | -- | -- |
| Black | 1.14 | 0.54–2.40 | 0.73 | -- | -- | -- |
| Latinx | 0.93 | 0.48–1.80 | 0.84 | -- | -- | -- |
| Other | 1.04 | 0.51–2.12 | 0.91 | -- | -- | -- |
| ASA Class | ||||||
| I | Ref | Ref | Ref | -- | -- | -- |
| II | 0.95 | 0.59–1.53 | 0.83 | -- | -- | -- |
| III/IV | 1.54 | 0.51–4.70 | 0.45 | -- | -- | -- |
| Former Tobacco Use | 1.74 | 1.10–2.75 | 0.02 | 1.60 | 1.00–2.55 | 0.048 |
| Preoperative Testosterone | 1.65 | 0.95–2.87 | 0.08 | 1.76 | 1.00–3.11 | 0.053 |
| Surgical Technique | ||||||
| Double Incision | Ref | Ref | Ref | -- | -- | -- |
| Buttonhole | 1.68 | 0.64–4.46 | 0.29 | -- | -- | -- |
| Circumareolar/Periareolar | 1.20 | 0.46–3.11 | 0.71 | -- | -- | -- |
| Keyhole | 0.45 | 0.06–3.37 | 0.44 | -- | -- | -- |
| Average Tissue Removed (g) | 1.00 | 0.99–1.00 | 0.25 | -- | -- | -- |
| Drain Use | 1.40 | 0.88–2.22 | 0.15 | 1.27 | 0.80–2.04 | 0.32 |
Abbreviations: Body Mass Index (BMI), Standard Deviation (SD), American Society of Anesthesiologists (ASA).
Acknowledgements
The authors would like to acknowledge the UCSF Biostatistics Department for their assistance with data interpretation, as well as Winnie Tong, M.D. and Terri Hupfer, R.N.
Appendix A.
Description of the four primary top surgery techniques and their indications.
Double Incision:
Patients with various degrees of skin excess are candidates for double-incision technique. An upper and lower curvilinear incision, the full length of the inframammary crease, is made to excise an ellipse of excess skin and breast tissue. The NAC is placed as a skin graft in the desired location. The technique provides the most reliable control of both skin envelope and NAC position.
Circumareolar/Periareolar:
Two concentric circular incisions are made around the nipple margin, through which breast tissue is removed. Once the incisions are closed, only a single scar is visible around the nipple margin. This technique is typically used for smaller chest volumes. Candidates may have some skin excess, and both skin and NAC can be downsized with this method.
Keyhole:
A semi-circular incision is made, and a small amount of tissue is preserved deep to the NAC; no skin is removed. Breast tissue is removed through a combination of liposuction plus direct excision, via the limited incision, using a lighted retractor. Candidates should have small breasts and good skin elasticity.
Buttonhole:
Incision design is similar to the double-incision technique, but the NAC complex is maintained on an inferior dermal pedicle. Suitable candidates for this technique should have a pedicle size that is small in relation to overall chest size or be accepting of the excess volume created by the pedicle.
Footnotes
Financial Disclosure Statement: The authors have no financial disclosures.
Presented at the American College of Surgeons Clinical Congress October 2019, San Francisco, California
References
- 1.Gust MJ, Smetona JT, Persing JS, et al. The impact of body mass index on reduction mammaplasty: a multicenter analysis of 2492 patients. Aesthet Surg J 2013;33:1140–1147 [DOI] [PubMed] [Google Scholar]
- 2.Myung Y, Heo CY. Relationship Between Obesity and Surgical Complications After Reduction Mammaplasty: A Systematic Literature Review and Meta-Analysis. Aesthet Surg J 2017;37:308–315 [DOI] [PubMed] [Google Scholar]
- 3.Meijs AP, Koek MBG, Vos MC, et al. The effect of body mass index on the risk of surgical site infection. Infect Control Hosp Epidemiol 2019;40:991–996 [DOI] [PubMed] [Google Scholar]
- 4.The obesity epidemic. Plast Reconstr Surg 2006;117:5S-7S; discussion 82S-83S [DOI] [PubMed] [Google Scholar]
- 5.Martinson TG, Ramachandran S, Lindner R, et al. High Body Mass Index Is a Significant Barrier to Gender-Confirmation Surgery for Transgender and Gender-Nonbinary Individuals. Endocr Pract 2020;26:6–15 [DOI] [PubMed] [Google Scholar]
- 6.White Hughto JM, Reisner SL, Pachankis JE. Transgender stigma and health: A critical review of stigma determinants, mechanisms, and interventions. Soc Sci Med 2015;147:222–231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kcomt L, Gorey KM, Barrett BJ, et al. Healthcare avoidance due to anticipated discrimination among transgender people: A call to create trans-affirmative environments. SSM Popul Health 2020;11:100608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Winter S, Diamond M, Green J, et al. Transgender people: health at the margins of society. Lancet 2016;388:390–400 [DOI] [PubMed] [Google Scholar]
- 9.VanKim NA, Erickson DJ, Eisenberg ME, et al. Weight-related disparities for transgender college students. Health Behav Policy Rev 2014;1:161–171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Downing JM, Przedworski JM. Health of Transgender Adults in the U.S., 2014–2016. Am J Prev Med 2018;55:336–344 [DOI] [PubMed] [Google Scholar]
- 11.Guss CE, Williams DN, Reisner SL, et al. Disordered Weight Management Behaviors, Nonprescription Steroid Use, and Weight Perception in Transgender Youth. J Adolesc Health 2017;60:17–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Witcomb GL, Bouman WP, Claes L, et al. Levels of depression in transgender people and its predictors: Results of a large matched control study with transgender people accessing clinical services. J Affect Disord 2018;235:308–315 [DOI] [PubMed] [Google Scholar]
- 13.Virupaksha HG, Muralidhar D, Ramakrishna J. Suicide and Suicidal Behavior among Transgender Persons. Indian J Psychol Med 2016;38:505–509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johns MM, Lowry R, Andrzejewski J, et al. Transgender Identity and Experiences of Violence Victimization, Substance Use, Suicide Risk, and Sexual Risk Behaviors Among High School Students - 19 States and Large Urban School Districts, 2017. MMWR Morb Mortal Wkly Rep 2019;68:67–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pittelkow EM, Duquette SP, Rhamani F, et al. Female-to-Male Gender-Confirming Drainless Mastectomy May Be Safe in Obese Males. Aesthet Surg J 2020;40:NP85–NP93 [DOI] [PubMed] [Google Scholar]
- 16.Donato DP, Walzer NK, Rivera A, et al. Female-to-Male Chest Reconstruction: A Review of Technique and Outcomes. Ann Plast Surg 2017;79:259–263 [DOI] [PubMed] [Google Scholar]
- 17.Knox ADC, Ho AL, Leung L, et al. A Review of 101 Consecutive Subcutaneous Mastectomies and Male Chest Contouring Using the Concentric Circular and Free Nipple Graft Techniques in Female-to-Male Transgender Patients. Plast Reconstr Surg 2017;139:1260e-1272e [DOI] [PubMed] [Google Scholar]
- 18.McEvenue G, Xu FZ, Cai R, et al. Female-to-Male Gender Affirming Top Surgery: A Single Surgeon’s 15-Year Retrospective Review and Treatment Algorithm. Aesthet Surg J 2017;38:49–57 [DOI] [PubMed] [Google Scholar]
- 19.World Professional Association for Transgender Health. Standards of Care. 2011; 7th Version [PubMed]
- 20.Bluebond-Langner R, Berli JU, Sabino J, et al. Top Surgery in Transgender Men: How Far Can You Push the Envelope? Plast Reconstr Surg 2017;139:873e-882e [DOI] [PubMed] [Google Scholar]
- 21.Lo Russo G, Tanini S, Innocenti M. Masculine Chest-Wall Contouring in FtM Transgender: a Personal Approach. Aesthetic Plast Surg 2017;41:369–374 [DOI] [PubMed] [Google Scholar]
- 22.Wolter A, Diedrichson J, Scholz T, et al. Sexual reassignment surgery in female-to-male transsexuals: an algorithm for subcutaneous mastectomy. J Plast Reconstr Aesthet Surg 2015;68:184–191 [DOI] [PubMed] [Google Scholar]
- 23.Rothenberg KA, Tong WMY, Yokoo KM. Early Experiences With the Buttonhole Modification of the Double-Incision Technique for Gender-Affirming Mastectomies. Ann Plast Surg 2018;81:642–645 [DOI] [PubMed] [Google Scholar]
- 24.Safa B, Lin WC, Salim AM, et al. Current Concepts in Masculinizing Gender Surgery. Plast Reconstr Surg 2019;143:857e-871e [DOI] [PubMed] [Google Scholar]
- 25.Gabriel A, Sigalove S, Sigalove NM, et al. Effect of Body Mass Index on Outcomes after Prepectoral Breast Reconstruction. Plast Reconstr Surg 2019;144:550–558 [DOI] [PubMed] [Google Scholar]
- 26.Banuelos J, Abu-Ghname A, Vyas K, et al. Should Obesity Be Considered a Contraindication for Prepectoral Breast Reconstruction? Plast Reconstr Surg 2020;145:619–627 [DOI] [PubMed] [Google Scholar]
- 27.Cuccolo NG, Kang CO, Boskey ER, et al. Masculinizing Chest Reconstruction in Transgender and Nonbinary Individuals: An Analysis of Epidemiology, Surgical Technique, and Postoperative Outcomes. Aesthetic Plast Surg 2019 [DOI] [PubMed] [Google Scholar]
- 28.Cuccolo NG, Kang CO, Boskey ER, et al. Mastectomy in Transgender and Cisgender Patients: A Comparative Analysis of Epidemiology and Postoperative Outcomes. Plast Reconstr Surg Glob Open 2019;7:e2316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berry MG, Curtis R, Davies D. Female-to-male transgender chest reconstruction: a large consecutive, single-surgeon experience. J Plast Reconstr Aesthet Surg 2012;65:711–719 [DOI] [PubMed] [Google Scholar]
- 30.Boskey ER, Taghinia AH, Ganor O. Association of Surgical Risk With Exogenous Hormone Use in Transgender Patients: A Systematic Review. JAMA Surg 2019;154:159–169 [DOI] [PubMed] [Google Scholar]
- 31.Moulla Y, Lyros O, Bluher M, et al. Feasibility and Safety of Bariatric Surgery in High-Risk Patients: A Single-Center Experience. J Obes 2018;2018:7498258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pakula A, Skinner R. Do acute care surgeons need bariatric surgical training to ensure optimal outcomes in obese patients with nonbariatric emergencies? Surg Obes Relat Dis 2018;14:339–341 [DOI] [PubMed] [Google Scholar]
- 33.Kaariainen M, Salonen K, Helminen M, et al. Chest-wall contouring surgery in female-to-male transgender patients: A one-center retrospective analysis of applied surgical techniques and results. Scand J Surg 2017;106:74–79 [DOI] [PubMed] [Google Scholar]
- 34.Ammari T, Sluiter EC, Gast K, et al. Female-to-Male Gender-Affirming Chest Reconstruction Surgery. Aesthet Surg J 2019;39:150–163 [DOI] [PubMed] [Google Scholar]
- 35.Winden TJ, Boland LL, Frey NG, et al. Care everywhere, a point-to-point HIE tool: utilization and impact on patient care in the ED. Appl Clin Inform 2014;5:388–401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sadoughi F, Nasiri S, Ahmadi H. The impact of health information exchange on healthcare quality and cost-effectiveness: A systematic literature review. Comput Methods Programs Biomed 2018;161:209–232 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


