Abstract
Introduction
Hearing impairment is a common condition that can have a significant impact on an individual. Ineffective communication between such individuals and doctors remains an important barrier. There is a need to provide medical students with a deeper understanding of such challenges. Increasingly, simulation is being used to develop empathy skills. In this study, we aimed to seek a deep understanding of medical students’ experiences of being placed in the role of a hearing-impaired patient by means of a virtual reality (VR) simulation.
Methods
A multidisciplinary group developed a 360° VR video-learning experience. This experience portrayed a consultation with a doctor from a hearing-impaired individual’s perspective. A qualitative study approach, using hermeneutic phenomenology, was conducted. Following the VR experience, students were interviewed, and transcripts of interviews were analysed using a Template Analysis approach.
Results
Analysis yielded four main themes: (1) ‘much more than just watching a video’: a VR experience of hearing impairment; (2) ‘hearing through their ears’: experiencing a person’s world with hearing impairment; (3) ‘not just what you can’t hear…but how it makes you feel’: reactions evoked by a VR hearing impairment experience and (4) redirecting my future professional self?
Discussion
This study provides an insight into medical students’ experiences of a novel VR hearing impairment simulation. VR simulation has the potential to provide a novel complementary training method for medical students. By providing an immersive learning experience, VR can offer an empathic stepping into the ears of those that live with hearing impairment.
Keywords: Virtual Reality, Simulation
INTRODUCTION
Hearing loss: much more than a sensory deficit
Over 466 million of the world’s population live with disabling hearing loss. 1 By the year 2050, the WHO estimates that over 900 million people will have hearing loss (ie, 1 in 10 people). 1 The inability to either totally, or partially, hear sounds can have a significant impact on an individual’s life and well-being. 2–4 Hearing impairment, or loss, is more than merely a ‘sensory deficit’. Living with hearing impairment is a personal and individual experience. Not only having an impact on an individual’s physical and mental health, but also on their emotional and psychological well-being. People with hearing loss are more likely to suffer from depression, cardiovascular disease, diabetes and cognitive impairment. 2 In addition, hearing loss can also impact on a person’s social functioning, contributing to social isolation and loneliness. 3 4
Given this additional burden, effectively engaging with and accessing healthcare is of paramount importance. However, despite legislation, such as the Disability Discrimination Act (1995) 5 and the Disability Discrimination Order (2006) 6 (which outlines a hearing-impaired person’s rights with regard to accessing healthcare)—individuals with hearing loss continue to report having difficulty in accessing healthcare. 7 Ineffective communication between such individuals and healthcare professionals (HCPs) remains an important barrier and is a central issue in providing equitable healthcare for such individuals. 2
Just under half of people with hearing loss report difficultly in effectively communicating with healthcare staff. 8 In one study, over a third of patients with hearing loss struggled to understand their diagnosis and treatment as a result of ineffective communication with HCPs. 8 Accessing healthcare and accessing information about health are also issues for such individuals. For example, many patients with hearing loss report difficulty in booking appointments over the phone in general practice, and a lack of induction loops in general practice surgeries. 7 With increasing number of people living with hearing loss and a global ageing population, never has there been a better time to ensure that HCPs can effectively communicate with such patients.
Central to this process is skilful communication by HCPs. 9 There is a duty for HCPs to ensure that they communicate effectively with patients, regardless of their condition or sensory impairments. For example, in the UK, the medical regulator—the General Medical Council—have mandated that all new graduate doctors should ‘communicate clearly, sensitively and effectively with individuals and groups regardless of their age, social, cultural or ethnic backgrounds or their disabilities’. 10
Many educational advances have been made in preparing medical students to communicate effectively with patients who have hearing impairment. 11 However, training methods often fall short of providing medical students with a deep understanding of the experience of individuals living with hearing loss. 12 There can be a disconnect between what medical students learn and how they behave in practice. 12 Unfortunately, individuals with hearing loss continue to highlight how HCPs can lack awareness of the struggles they face. 9 There is a need to provide medical students with a deeper understanding of such challenges in order to transform their behavioural and empathy skills. 7
Experiential learning and empathy skill development
We are aware that doctors who have experienced illness themselves demonstrate greater empathy towards their patients. 13 Being ‘in the shoes’ of someone experiencing an illness can nurture a deep and personal insight into the many ways that illness can impact on a person’s life. 13 Such experience allows them to reconcile their intellectual understanding of illness and their emotional responses. Not that we want HCPs to experience actual illness, but being afforded opportunities to experience certain aspects of illness has the potential to develop their empathic skills.
Experiential forms of learning have been shown to develop empathy skills in HCPs and students. 14 Simulation is one form of experiential learning that can give learners an opportunity to experience aspects of illness in a safe and guided fashion. From wearing body suits that mimic the challenges faced by older patients to adhering to a diabetic diet or wearing a highly realistic malignant melanoma transfer tattoo—all have provided HCPs vicarious insights into illness experiences. 15–17 Such forms of experiential learning permit HCPs to project themselves into the lived experience of such patients, triggering a critical reflection of how best to empathise and treat such people in the future. 15–17
Simulation creates guided learning opportunities. Within the domain of simulation, there are many modalities capable of providing such constructed forms of learning experiences—for example, manikin-based simulation, role-play with simulated patients and computer-based simulations using augmented reality and virtual reality (VR). Recently, there has been increasing interest in the use of VR in medical education. 18 19 VR provides a computer-generated sensory experience using visual images and sound to immerse an individual in a three-dimensional imagined context. 18 19 It could be hypothesised that a VR immersive experience of hearing impairment from a patient’s perspective could provide an experiential learning opportunity for medical students. Exploring such experiences could provide insights into how this affects the learners’ empathy skills.
Therefore, this study aims to provide a deep understanding of medical students’ experiences of being placed in the role of a hearing-impaired patient by means of a VR simulation.
METHODS
‘Virtually hearing through a patient’s ears’: develop a hearing impairment VR experience
A multidisciplinary group at Queen’s University Belfast (QUB) designed and developed a 360° VR video-learning experience. The project group consisted of key stakeholders and experts including medical students, clinicians, a VR media producer and a person who lives with hearing impairment. The aim of this VR learning tool was to provide medical students with an immersive experience of what it is like to have hearing impairment from a patient’s perspective, when interacting with a HCP. The design process initially consisted of a needs assessment from a patient perspective and from a medical practitioner’s perspective. A storyboard and script were drafted to generate simulated scenarios. The scenarios were set in a general practice context, where a general practitioner (GP) was consulting with a patient who presented with a cough. The patient had a viral upper respiratory tract infection. From the patient’s perspective, they were keen to receive an oral antibiotic; however, from the GP’s perspective, an oral antibiotic was not clinically indicated. Therefore, effective communication and dialogue were required to develop a shared understanding of the diagnosis and management plan between patient and GP.
Following refinement of the storyboard and script, the simulated consultations were enacted with actors in a ‘script read through’ rehearsal. The first scenario portrayed a GP who did not communicate well with the patient. Their poor communication skills were based on prior evidence and personal experience of individuals with hearing impairment. Examples of poor communication included the GP covering their mouth while speaking, looking away from the patient while speaking, not acknowledging the patient’s hearing impairment and not inviting opportunities for the patient to clarify what they have said. In contrast, a second scenario was developed to reinforce good communication skills. In this scenario, the GP demonstrated more effective communication skills for a patient with hearing impairment (eg, acknowledging that the individual has hearing impairment, inviting the patient to choose their preferred method of communicating, inviting opportunities for the patient to clarify what has been said, maintaining good face-to-face contact in order to lip-read, adjusting their speech level and pace in an appropriate way).
A general practice setting was created to record these scenarios (figure 1). The enacted simulations were recorded in spherical video with a Go Pro Fusion 360 video camera and a Zoom H3N ambisonics microphone. Two mono lapel microphones were also used to record voices at close proximity. The recordings from these sources were edited and prepared for spherical video and audio for viewing in VR headsets (figure 2). Crucial to the postproduction process was careful manipulation of the recorded sounds to simulate a realistic auditory recreation of hearing impairment. Typical symptoms of sensorineural hearing loss were simulated with processing in the audio frequency domain (eg, attenuation of high-frequency sounds) and in the dynamic domain (eg, attenuation of quieter sounds). Tinnitus, a condition commonly accompanying hearing impairment, was simulated with the addition of two synthesised sounds: a ringing high-frequency pure tone and a hissing white noise with high frequencies attenuated. Finally, a user briefing was devised in order to orientate learners to the VR experience.
Figure 1.
Set-up of filming of the hearing impairment virtual reality simulation.
Figure 2.
Image of virtual reality video footage from the perspective of a patient consulting with a general practitioner.
Conceptual orientation of study
The aim of our study was to gain a nuanced understanding of medical students’ lived experiences of this VR activity. There are a number of qualitative methodologies that can explore individuals’ experiences, for example, narrative-based research or autoethnography. For the purposes of our study, we used a phenomenological conceptual orientation to explore participants lived experiences—specifically hermeneutic phenomenology.
Epistemologically, a distinction between descriptive and interpretative phenomenological approaches in qualitative research is often made. In the more descriptive traditions of phenomenology, such as Husserlian descriptive phenomenology, they aim to describe how a phenomenon appears in the consciousness of an individual—separate from the context and the lifeworld that it exists in. 20 However, in the more interpretative traditions of phenomenology, such as hermeneutic phenomenology, they acknowledge that to understand a lived experience of a phenomenon, we also need to interpret the meaning of this described phenomenon. 21–23 Moreover, there is a need to consider the contextual influences that shape the lived experience of this phenomenon, that is, the interconnectedness of the experienced phenomenon and context of the individual’s lifeworld. Such a conceptual orientation considers how lived experiences are constructed and interpreted, while acknowledging that researchers bring their own experiences, assumptions and subjectivity to the analytic process. 21–23 Therefore, through a dynamic reflexive process, researchers need to consider their preconceptions and experiences in the interpretative process—in order to gain an understanding of participants’ lived experiences. 21–23 For the purposes of our study, we aimed to explore medical students’ lived experiences of this VR activity and the contextual influences that shaped the meaning of this experience. Therefore, hermeneutic phenomenology was a conceptual fit for our study.
Setting and context
The study was carried out in the Centre for Medical Education, QUB. The QUB medical degree programme follows a 5-year integrated undergraduate curricular model. Students in their first 2 years undertake an Introductory Clinical Skills Programme (ICSP) where they develop their communication, consultation and physical examination skills.
Recruitment and sampling
All medical students enrolled in the ICSP were invited by email to participate in the study. A convenience sampling strategy was used to sample participants for the study. Phenomenological-based research typically recruits small numbers compared to other research methodologies. 21 Sampling in phenomenological-based research aims to achieve a balance between the deep understanding of participants’ experiences and the broader insights gained by sampling a larger number of participants. Therefore, sample sizes are generally smaller—allowing for more in-depth analysis without being overwhelmed by the volume of data. Therefore, we aimed to recruit 10 participants for this study.
VR experience
Recruited participants underwent the simulated VR experience described above (figure 3). An Oculus Go VR headset was used for the purposes of this study. Given that the auditory experience was crucial in this VR activity, headphones with enhanced sound isolation were used. Following written consent, participants were orientated to the VR headset and headphones. After applying a disposal hygienic face mask, participants placed the VR headset and headphones on and experienced the two simulated VR scenarios. Following the scenarios, the headset and headphones were removed.
Figure 3.

Illustration of a medical student using the hearing impairment virtual reality simulation.
Data capture
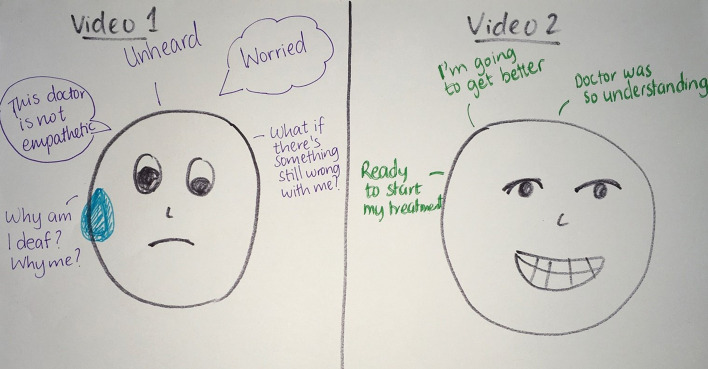
Following the VR exercise, participants took part in one-to-one qualitative interviews conducted by NMcL (who had no relationship to the participants and also received training in qualitative research interview skills). In keeping with our phenomenological methodology, interviews were exploratory and minimally structured, to allow discussions to remain as true as possible to participants’ experiences. In order to enrichen the data obtained a technique known as Rich Pictures (RP) was used. Founded by Checkland in the 1970s, RP is an interview elicitation tool that can enrich participants’ verbal interview data. 24 25 In this study, participants were asked to draw a picture that symbolised their experience of the VR activity (figure 4). These pictures were used to elicit the research interview. Such an interview elicitation method affords interviewers with deeper insights, as they can empathise more with what a subject experiences during the VR activity. 24 25
Figure 4.
Illustration of a qualitative interview elicitation Rich Picture from participant ‘Megan’.
All interviews were transcribed verbatim, checked for accuracy and anonymised using pseudonyms.
Analysis
A template analysis approach was used to analyse the interview data in this study. 26 This method of analysis was an epistemologically good fit with the hermeneutic phenomenological approach used in this study 26 and provides a structured approach to the researcher’s interpretation of participants’ lived experience during the VR exercise and bring light to their meanings. The interview transcripts provided the focus for analysis. The RP were not analysed directly but instead were used to support analysis. Throughout the analytical process, researchers kept a strong orientation and commitment to the phenomenon under investigation. 21–23 Prior to conducting the analysis, the researchers brought to the surface their assumptions about the VR experience. Tentative a priori codes were then created and applied to four initial transcripts. These a priori codes were modified in response to analysing the transcripts. Emergent codes were clustered to identify preliminary themes and used to develop an initial research template. This initial template was then applied to the remaining transcripts and iteratively refined. Finally, all transcripts were coded against the definitive template in order to illuminate the interpretation and meaning of the entire dataset as an emergent whole—that is, the hermeneutic circle. 21–23 Following our analysis, a summary of our findings will be sent to participants for comment (ie, member checking). Analysis ended when all the researchers agreed that a thick and rich description had been achieved. Member checking of the results was conducted to seek respondent validation. Hermeneutic phenomenology requires researchers to acknowledge their own experiences in the interpretative process. 21–23 Therefore, the research team met regularly and were continually reflexive through a thoughtful dynamic process of dialogue, reflexion and writing.
Ethics and quality assurance
Ethical approval was given by Faculty of Medicines Health and Life Sciences Research Ethics Committee (MHLS 20_02). Written informed consent was obtained from all participants. We adhered to the Consolidated criteria for Reporting Qualitative research checklist for our study (see online appendix 1). 27
bmjstel-2020-000683supp001.pdf (482KB, pdf)
RESULTS
Ten participants took part in the study, generating over 303 min of interview data. Analysis yielded four main themes: (1) ‘much more than just watching a video’: a VR experience of hearing impairment; (2) ‘hearing through their ears’: experiencing a person’s world with hearing impairment; (3) ‘not just what you can’t hear…but how it makes you feel’: reactions evoked by a VR hearing impairment experience and (4) redirecting my future professional self?
‘Much more than just watching a video’: a VR experience of hearing impairment
The VR activity provided participants with a distinctive simulation experience. Important to this experience was the multisensory nature of VR. First, the visual stimulus enhanced the immersive properties of the VR experience—particularly the 360° nature of the moving images. The fact that participants could move their head and body, in relation to the VR footage, added to the richness of this experience providing a sense of space and a bodily experience.
“I liked that you could even turn around, move and see the doctor behind you… I think that was really good” (Sophie)
The auditory stimulus provided by the VR activity was an integral part of participants’ experiences. Creating the aural experience of hearing impairment was an important mediator on their degree of immersion. Of note, participants experienced an interesting phenomenon in relation to the soundscape—namely, as they began the VR exercise, they often reached for the volume controls of the VR headset considering there to be a fault with the sound.
“You were constantly straining to hear, it’s like as if the microphone or something wasn’t plugged in properly” (Ciara)
However, given that the soundscape was designed to recreate aspects of what it was like to have hearing impairment, such inaudibility was intentional. When participants realised this intentionality, and not just a fault with the equipment, it marked an important experience for participants. This often disrupted their sense of the VR experience as being a novelty and created a greater sense of what it might be like to have hearing impairment, from pretending to being.
“When I realised…that’s the first time I’ve ever had that experience of you know not being able to hear someone who’s talking to me, properly. Umm it’s nearly scary thinking that this is how people live their lives every day” (Christopher)
Beyond the sensory stimuli, participants also perceived a deeper, more visceral experience. Rather than experiencing the sensory stimuli individually, they perceived the experience as an emergent whole. This was often an embodied experience, with participants ‘feeling’ the VR activity.
“it makes it much more personal… like you feel like you’re in the scenario…you’re there” (Grace)
‘Hearing through their ears’: experiencing a person’s world with hearing impairment
Given the immersive nature of the VR activity, this afforded participants an opportunity to experience what it was like to have hearing impairment, from a patient’s perspective. Participants transitioned from the sense of being a learner to the imagined experience of being a patient with hearing impairment. In so doing they were willing to suspend their disbelief and tentatively ‘walk in the shoes’ of being a patient.
“It’s that element of like total immersion because you’re not watching a video about people with hearing impairment… you are a person with hearing impairment” (Christopher)
For many participants, this phenomenon was the first time they had experienced what it would be like to have hearing impairment. This was often perceived as a privileged experience.
The experience by participants went beyond the aural experience of hearing impairment. Participants expressed a greater holistic sense of what it is to be a person with hearing impairment. Given the context of a GP consultation, communication between the GP and the participants was an important dimension of this more holistic experience. Participants gained a sense of the challenges involved in communicating effectively—both in understanding what others are saying and in being understood by others. A prominent experience for participants was wanting to have a shared understanding of a consultation with a GP. Not only for the GP to understand their clinical history and concerns, but also to gain a clear understanding of their diagnosis and proposed management plan.
“it’s like a puzzle… she can’t put all the pieces together if she doesn’t have half the information, you know” (Laura)
Participants also experienced the extra effort that it took for an individual to have a normal dialogue in a GP consultation. Barriers and enablers to effective communication with a HCP were brought to surface awareness for participants. They gained insights into measures that enabled more effective communication with a person with hearing impairment. Not just the more practical measures, such as facing the patient while talking, not holding their hand over their mouth and adjusting their vocal levels, but also more facilitatory methods such as clarification with the patient about their preferred method of communicating, signposting their actions (eg, ‘now let’s discuss your treatment’) and inviting the patient to indicate if they failed to hear properly any part of the consultation.
“straight away he addressed you’ve got a hearing impairment, what style of communication do you want me to like do with you? And then when she said lip-reading he was very clear, he didn’t look at the computer as much, he was very direct, face to face umm so she could lip-read… because he was speaking clearly and then he was also making me feel more comfortable and more listened to” (Laura)
Conversely, participants were provided with deeper insights into barriers to effective communication with a person who has hearing impairment. Examples included a GP orientating their face to the computer screen while speaking to a patient, not acknowledging the patient had a hearing impairment nor adjusting their speech in order to optimise what the patient can hear.
“there was a total communication barrier, and nobody seemed to recognise that there was like a wall in front of you because they didn’t recognise like how you were feeling or that you could not understand what they were saying” (Eleanor)
‘Not just what you can’t hear…but how it makes you feel’: reactions evoked by a VR hearing impairment experience
The overall VR immersive activity could evoke a range of experiences and emotions in participants. Such experiences could either be negative or be more positive depending on the context at that time during the immersive VR consultation. For example, if participants felt that the consultation was going well, this could induce emotions of gratitude, joy and serenity.
“you’re like immediately put at ease, content and felt reassured…” (Kate)
Equally, if participants felt that they were not being understood in the VR consultation, this could evoke more negative emotions such as disappointment, annoyance, fear and anger. Such emotions could generate a sense of isolation and the sense of being different.
“She felt unheard, she felt worried like is there something so wrong with her and she felt that the doctor was not empathetic enough towards her, he kept looking at the screen. Umm and like she probably felt like why am I deaf why was I chosen to be deaf…it wasn’t nice” (Megan)
Given the healthcare context of this immersive VR experience, such emotional reactions provided participants with a sense of acknowledgement and respect, or not, with the GP. Participants experienced how good communication could instil trust and empowerment, and equally, how poor communication could evoke a sense of mistrust and isolation.
“she probably feels like she wants to go see another GP or you know go somewhere where she feels listened to and she actually feels like their skills as a clinician are better, even though they’re probably the same skills it’s just like the communications differs” (Laura)
Beyond the sense of trust experienced by participants, the VR activity could also promote a sense of wanting to consult with this GP again, or not.
“I was thinking you know this would make me never want to go near a GP again, or a healthcare professional of any sort” (Christopher)
Redirecting my future professional self?
Participants recounted that the entire VR experience triggered them to reflect critically on their professional development. There was a greater appreciation of how previously perceived ‘minor’ modifications to their communication skills can have a significant impact on patients’ understanding. Furthermore, participants experienced a greater appreciation of how effective communication can have a more holistic impact on patients and their well-being.
“Even just simple things like that sort of made it better, he turned like to face her and was very clear with what he said” (Jack)
As HCPs of the future, the VR experience provided a stimulus for them to consider seek methods of how best to communicate with patients with hearing impairment. They voiced a desire to make greater adaptations in their communication skills in order for patients to be able to understand them in consultations and in other interactions.
“…. I never knew this is what people went through during consultations…and in general as well in life imagining being in that person’s shoes for the whole day for every conversation you’re in is quite distressing. So…I think it makes me much more empathetic towards hearing impaired people and wanting to make a change as a doctor” (Megan)
Interestingly, this not only related to their future professional lives, but participants also acknowledged that this experience aided them in communicating more effectively with others who had hearing impairment—for example, family members.
“My Granny has hearing aids in….so it just makes me more mindful like maybe if I just spoke slightly slower and looking at the person” (Ciara)
DISCUSSION
This study provides a unique insight into medical students’ experiences of a novel VR hearing impairment simulation. The uniqueness of this multisensory simulation affords students an enhanced sense of what it is like to have hearing impairment as a patient. While we cannot recreate true hearing impairment, VR can provide an imagined and broad perspective of what it would be like to be a patient living with hearing impairment. Beyond the aural and visual experience, VR offers an opportunity for medical students to explore the more holistic impact that hearing impairment can have and foster a drive to be more empathic towards such individuals.
Simulating hearing impairment: ‘suspending disbelief’ and stepping into the shoes of patients
VR is an emerging technology and is increasingly being integrated into medical curricula. 28 While largely being used for developing clinical reasoning skills, this study signals an extended role for VR in promoting medical students’ empathetic skills. 19 As with other forms of simulation in health profession education, simulation aims to recreate clinical scenarios which can permit a guided learning experience. In order to optimise the learning experience, learner buy-in is crucial—shifting the student’s sense of pretending to one of believing that the scenario is ‘real’, that is, suspending disbelief. Our findings would suggest that such a VR experience can promote students’ ability to suspend their disbelief. In addition to the narrative content, which was grounded in patient experiences, VR provided an embodied experience. Embodiment can be defined as how one’s own body navigates and mediates everyday life experiences. 29 30 In addition to the visual and auditory sensory experience, participants had a much deeper, bodily experience—they ‘felt’ in the position of a being patient. Being able to move their own body during the exercise, while wearing the VR headset and reacting to the VR content, deepened their sense of realism. It was interesting to note that students often considered there to be a ‘technical fault’ with the VR audio - rather than actually experiencing the world as an individual living with hearing impairment. This ‘disruption’ was a key trigger point for learners to experience the ‘disruption’ that hearing impairment can have on actual patients.
This realism provided learners with a platform to gain a wider sense of the impact that hearing impairment can have on a patient. Beyond the sensory impairment, the VR experience generated a more holistic understanding of what it is to be a patient, living with hearing impairment, to consult with a HCP. It is not just about what cannot be heard or understood, but also about some of the emotional responses that this triggers, especially with the vulnerability of also having an illness.
We are aware that living with hearing impairment can be a stigmatising experience. 3 Such individuals can often feel ‘different’ and make efforts to conceal their differentness. 30 It was interesting to note that students also gained a sense of differentness during the VR simulation and how this can promote a feeling of isolation.
Doctors in the making and empathetic skills
During the VR simulation, students would toggle between being an individual living with hearing impairment and considering their future role as a doctor. Viewing the doctor–patient relationship from these perspectives caused students to reflect critically on how best to communicate with people living with hearing impairment. What was brought to students’ surface attention were things that might be considered trivial in communication with patients but that can mean a lot to such individuals. ‘Small things’ like facing a patient or signposting their conversation can make a huge positive impact on patients’ well-being and understanding of their care. 31–33
Medical education aims to transform medical students’ professional skills. Not only in gaining their clinical competencies, but also promoting their self-awareness and reflective practice. Evident from our findings, this VR simulation appears to be a useful learning tool to trigger medical students’ critical reflective and empathic skills. In so doing, this mediated their desire to modify their attitudes and behaviours in considering how best to work with such patients in the future. Many have argued that empathy is not just an intellectual phenomenon—it is also an embodied and subjective experience—similar to what was found in this study. 34–36 Empathy is the English translation of the German term Einfühlung (‘feeling into’)—‘entering another’s world’—and is in keeping with the findings of our study. This also resonates with other research that explores how simulation can be used to develop medical students’ empathetic skills. 15–17
Pedagogical implications
VR simulation of hearing impairment has the potential to provide a meaningful learning experience for medical students. Not only does it allow students to experience the impact that hearing impairment can have on an individual but it also promotes a holistic focus of how best to communicate with such people in the future. In addition to other teaching methods, VR simulation has the potential to complement other learning experiences in a person-centred approach.
Strengths and limitations
The findings in this study would indicate that VR can provide a novel and meaningful learning experience. However, these findings must be considered within certain limitations. Given the theoretical orientation in this study, generalisability was not an intended objective. Moreover, this study was exploratory and aimed to gain fine-grained insights into the experiences of VR hearing impairment simulation for medical students. The findings of this study may not be transferable to other HCPs although this would be worthy of future research. Lastly, we did not set out to determine the long-term impact of this VR simulation experience on medical students’ empathic skills although such research would be worthwhile to consider.
CONCLUSION
Effective communication skills are important to the success of patient–doctor relationships. This is particularly important for patients who live with hearing impairments. In best preparing medical students to communicate effectively with such individuals, it is important that we focus on more than just the technical aspects of verbal skills. They need to focus on the non-verbal skills and modify their behaviours in order to optimise effective communication. In a person-centred and holistic fashion, VR simulation has the potential to provide a novel complementary training method for medical students. By providing an immersive and memorable learning experience, VR can offer an empathic stepping into the ears of those that live with hearing impairment.
What is already known on this subject.
Hearing impairment is a common condition and there is a duty for all healthcare professionals to ensure that they communicate effectively with such individuals.
However, ineffective communication between such individuals and healthcare professionals remains an important barrier and many have called for enhanced training opportunities.
Simulation is increasingly being used to afford healthcare professionals empathic learning opportunities by allowing them to ‘step into the shoes’ of their patients.
What this study adds.
With multistakeholder involvement, including with those living with hearing impairment, a rich immersive VR experience can be created including an aural experience of hearing impairment.
Such an immersive VR experience can provide learners with a profound and embodied experience of what it is like to live with hearing impairment.
Providing this immersive experience can trigger learners to critically reflect on how best to communicate with an individual who has hearing impairment and drive their desire to enact this in actual practice.
Footnotes
Twitter: GerardGormley@DrGerryGl.
Acknowledgements: The authors would like to thank all the students and faculty staff who participated in the study. Thanks also to Professor Jayne Woodside and James Bailey for their guidance and support in this study. Finally, we would like to thank the Clinical Skills Education Centre (CSEC) staff for their help in this study.
Contributors: All authors (NMcL, JR, JDA and GG) contributed to conception and design of the study, analysis of the data and reviewed and approved the final manuscript. NMcL and GG drafted the initial manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
REFERENCES
- 1. Deafness and hearing loss, World Health Organisation. 2019. Available https://www.who.int/news-room/fact-sheets/detail/deafness-and-hearing-loss (last accessed 11th Apr 2020)
- 2. The Deaf Health Charity Sign Health . Deaf health summary. 2019. Available https://www.eclsensoryservice.org/wp-content/uploads/2016/09/THE-HEALTH-OF-DEAF-PEOPLE-IN-THE-UK-.pdf (last accessed 11th Apr 2020).
- 3. Mulrow C, Aguilar C, Endicott J, et al. Association between hearing impairment and the quality of life of elderly individuals. J Am Geriatr Soc 1990;38:45–50. 10.1111/j.1532-5415.1990.tb01595.x [DOI] [PubMed] [Google Scholar]
- 4. Ciorba A, Bianchini C, Pelucchi S, et al. The impact of hearing loss on the quality of life of elderly adults. Clin Interv Aging 2012;7:159–63. 10.2147/CIA.S26059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Disability Discrimination Act (DDA) RNIB. 2019. Available https://www.rnib.org.uk/information-everyday-living-your-rights/disability-discrimination-act-dda (last accessed 11th Apr 2020)
- 6. The disability discrimination (Northern Ireland) order 2006, Legislation.gov.uk. 2019. Available http://www.legislation.gov.uk/nisi/2006/312/contents/made (last accessed 11th Apr 2020)
- 7. Action on Hearing Loss . Is it my turn yet?. 2010. Available http://file:///Q:/Is%20it%20my%20turn%20yet%20report%204.pdf (last accessed 11th Apr 2020)
- 8. A simple cure: a national report into deaf and hard of hearing people’s experiences of the national health service - social care online scie-socialcareonline.org.uk. Available https://www.scie-socialcareonline.org.uk/a-simple-cure-a-national-report-into-deaf-and-hard-of-hearing-peoples-experiences-of-the-national-health-service/r/a11G00000017vcpIAA (last accessed 11th Apr 2020)
- 9. Mackenzie I, Smith A. Deafness: the neglected and hidden disability. Ann Trop Med Parasitol 2009;103:565–71. 10.1179/000349809X12459740922372 [DOI] [PubMed] [Google Scholar]
- 10. Outcomes for graduates, Gmc-uk.org. 2019. Available https://www.gmc-uk.org/education/standards-guidance-and-curricula/standards-and-outcomes/outcomes-for-graduates (last accessed 11th Apr 2020)
- 11. Gilmore M, Sturgeon A, Thomson C. Changing medical students’ attitudes to and knowledge of deafness: a mixed methods study. BMC Med Educ 2019;19:227. 10.1186/s12909-019-1666-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. McGlade K, Saunders E, Thomson C, et al. Deaf awareness training in medical schools. Med Teach 2013;35:789–90. 10.3109/0142159X.2013.786808 [DOI] [PubMed] [Google Scholar]
- 13. Tomlinson J. Lessons from “the other side”: teaching and learning from doctors’ illness narratives. BMJ 2014;g3600. 10.1136/bmj.g3600 [DOI] [Google Scholar]
- 14. Bearman M, Palermo C, Allen L, et al. Learning empathy through simulation. simulation in healthcare. J Soc Simul Healthcare 2015;10:308–19. 10.1097/SIH.0000000000000113 [DOI] [PubMed] [Google Scholar]
- 15. Corr M, Roulston G, King N, et al. Living with ‘melanoma’ … for a day: a phenomenological analysis of medical students’ simulated experiences. Br J Dermatol 2017;177:771–8. 10.1111/bjd.15402 [DOI] [PubMed] [Google Scholar]
- 16. Barry T, Chester L, Fernando M, et al. Improving medical student empathy: initial findings on the use of a book club and an old age simulation suit. Eur Psychiatry 2017;41:S894. ISSN 0924-9338. 10.1016/j.eurpsy.2017.01.1821 [DOI] [Google Scholar]
- 17. Parker D, Fontem A, Ojong E, et al. Impact of diabetes simulation on empathy in pharmacy students. Am J Pharm Educ 2019;83:6432. 10.5688/ajpe6432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pottle J. Virtual reality and the transformation of medical education. Future Healthc J Oct 2019;6:181–5. 10.7861/fhj.2019-0036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Dyer E, Swartzlander BJ, Gugliucci MR. Using virtual reality in medical education to teach empathy. J Med Libr Assoc 2018;106:498–500. 10.5195/jmla.2018.518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Langdridge D. Phenomenological psychology: theory, research and method . Harlow: Pearson Education, 2004. [Google Scholar]
- 21. Laverty SM. Hermeneutic phenomenology and phenomenology: a comparison of historical and methodological considerations. Int J Qual Methods 2003;2:21–35. 10.1177/160940690300200303 [DOI] [Google Scholar]
- 22. Sloan A, Bowe B. Phenomenology and hermeneutic phenomenology: the philosophy, the methodologies, and using hermeneutic phenomenology to investigate lecturers’ experiences of curriculum design. Qual Quant 2014;48:1291–303. 10.1007/s11135-013-9835-3 [DOI] [Google Scholar]
- 23. Bynum W, Varpio L. When I say … hermeneutic phenomenology. Med Educ 2018;52:252–3. 10.1111/medu.13414 [DOI] [PubMed] [Google Scholar]
- 24. Bergvall‐Kåreborn B, Grahn A. Multi‐modal thinking in soft systems methodology’s rich pictures. World Futures 1996;47:79–92. 10.1080/02604027.1996.9972588 [DOI] [Google Scholar]
- 25. Booton CM. Using rich pictures to verify, contradict, or enhance verbal data. Qual Report 2018;23:2835–49. https://nsuworks.nova.edu/tqr/vol23/iss11/13/ [Google Scholar]
- 26. Brooks J, McCluskey S, Turley E, et al. The utility of template analysis in qualitative psychology research. Qual Res Psychol 2015;12:202–22. 10.1080/14780887.2014.955224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Booth A, Hannes K, Harden A, et al. COREQ (Consolidated Criteria for Reporting Qualitative Studies). In: In guidelines for reporting health research . A User’s Manual, 2014. [Google Scholar]
- 28. Samadbeik M, Yaaghobi D, Bastani P, et al. The applications of virtual reality technology in medical groups teaching. J Adv Med Educ Prof 2018;6:123–9. [PMC free article] [PubMed] [Google Scholar]
- 29. Csordas T. Embodiment as a paradigm for anthropology. Ethos 1990;18:5–47. 10.1525/eth.1990.18.1.02a00010 [DOI] [Google Scholar]
- 30. Scheper-Hughes N. Embodied knowledge: thinking with the body in critical medical anthropology. In: Borofsky R, ed. Assessing cultural anthropology . New York: McGraw-Hill, 1994: 229–39. [Google Scholar]
- 31. Hines J. Communication problems of hearing-impaired patients. Nurs Stand 2000;14:33. 10.7748/ns2000.01.14.19.33.c2752 [DOI] [PubMed] [Google Scholar]
- 32. Middleton A, Niruban A, Girling G, et al. Communicating in a healthcare setting with people who have hearing loss. BMJ. 2010;341:c4672–c4672. 10.1136/bmj.c4672 [DOI] [PubMed] [Google Scholar]
- 33. Barnett S. Communication with deaf and hard-of-hearing people: a guide for medical education. Acad Med 2002;77:694–700. 10.1097/00001888-200207000-00009 [DOI] [PubMed] [Google Scholar]
- 34. The importance of empathy in healthcare: advancing humanism. Blog.medicalgps.com. 2019. Available http://blog.medicalgps.com/the-importance-of-empathy-in-healthcare/ (last accessed 11th Apr 2020)
- 35. Neumann M, Edelhäuser F, Tauschel D, et al. Empathy decline and its reasons: a systematic review of studies with medical students and residents. Acad Med 2011;86:996–1009. 10.1097/ACM.0b013e318221e615 [DOI] [PubMed] [Google Scholar]
- 36. Nunes P, Williams S, Sa B, et al. A study of empathy decline in students from five health disciplines during their first year of training. Int J Med Educ 2011;2:12–17. 10.5116/ijme.4d47.ddb0 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjstel-2020-000683supp001.pdf (482KB, pdf)