Abstract
Traumatic ulcerative granuloma with stromal eosinophilia (TUGSE) is a rare, benign, and self-limiting ulcerative lesion, with the tongue being the most common site of occurrence and traumatic inflictions being the common etiology. Case report: A 45-year-old female reported to the dental operatory with a complaint of pain on the left side of her tongue for the past 8 months. Her history revealed that a small ulcer had gradually grown to be 2 cm x 1.5 cm on presentation. She indicated that the ulcer often interfered with her maxillary left canine while occluding. She also gave a history of a tobacco chewing habit for 15 years which she stopped 6 years ago. Clinically she had a single erythematous ulcer with irregular borders and raised margins. The client was treated with surgical excision of the lesion. The excised lesion was confirmed histologically to have eosinophil rich cells and was diagnosed as TUGSE. Conclusion: TUGSE should be recognized and not neglected as it closely resembles malignancies of the oral cavity. It also has a good prognosis and heals rapidly after the surgical excision or on its own with time, which may range from a few weeks to a year.
Keywords: squamous cell carcinoma, tongue, TUGSE
Abstract
Le granulome ulcératif traumatique avec éosinophilie stromale (TUGSE) est une lésion ulcérative rare, bénigne et spontanément résolutive, la langue étant la zone d'occurrence la plus fréquente et les inflictions traumatiques étant l'étiologie la plus courante. Rapport de cas : Une femme de 45 ans s'est présentée à la salle de traitement dentaire en se plaignant d'une douleur du côté gauche de sa langue depuis les 8 derniers mois. Ses antécédents ont révélé qu'un petit ulcère avait progressivement grossi jusqu'à présenter une taille de 2 cm x 1,5 cm. Elle a signalé que l'ulcère entravait souvent sa canine maxillaire gauche lorsque ses dents étaient en occlusion. Elle a aussi fait état d'une habitude de mastication de tabac pendant 15 ans, ce qu'elle a abandonné il y a 6 ans. Elle présentait cliniquement un seul ulcère érythémateux aux contours irréguliers et des marges surélevées. La cliente a été traitée par excision chirurgicale de la lésion. Une analyse histologique de la lésion excisée a confirmé la présence de cellules riches en éosinophiles et a été diagnostiquée comme étant un TUGSE. Conclusion : Le TUGSE doit être constaté et ne pas être négligé, puisqu'il ressemble de près aux tumeurs malignes de la cavité buccale. De plus, son pronostic est bon et il guérit rapidement après l'excision chirurgicale ou par lui-même avec le temps, qui peut varier de quelques semaines à une année.
PRACTICAL IMPLICATIONS OF THIS RESEARCH.
TUGSE resembles squamous cell carcinoma and is often misdiagnosed by clinicians who are unfamiliar with these ulcers.
TUGSE is often caused by trauma and occurs most frequently on the tongue.
Clients presenting with these ulcers have a good prognosis once diagnosed; the oral cavity heals rapidly after surgical excision.
INTRODUCTION
Traumatic ulcerative granuloma with stromal eosinophilia (TUGSE) is a rare, benign, reactive, and self-limiting ulcerative lesion usually affecting the tongue. Clinically, TUGSE presents as a slow-healing ulcer persisting from 1 week to 1 year 1 and is characterized by rolled borders that closely resemble squamous cell carcinoma. 2 The etiology of TUGSE remains questionable, although trauma is considered the most frequent cause. 2 TUGSE typically regresses on its own following excision of the lesion. Histologically it manifests as a surface ulceration along with dense, mixed inflammatory cell infiltrate in the connective tissue, which has a reasonable number of eosinophils. 3 Prognosis remains favourable with rapid healing of the surgical site; the lesion typically does not recur. 4
CASE REPORT
This case presents a 45-year-old female who reported to the Department of Oral and Maxillofacial Surgery with a chief complaint of pain on the left side of her tongue that she claimed had been present for 8 months. Her history revealed she first had a small ulcer that often became irritated by the teeth adjacent to it. The ulcer gradually increased in size over the 8-month period to reach its observed size. She also gave a history of having a tobacco chewing habit for 15 years, which she stopped 6 years ago. On examination, a single erythematous ulcer was seen on the left border of the tongue, measuring about 2 cm x 1.5 cm with irregular borders and everted margins, which was provisionally diagnosed as squamous cell carcinoma (Figure 1). The lesion was surgically excised under local anesthesia and sent for histopathological investigation. Gross examination showed a single soft-tissue specimen measuring 1.7 cm x 0.6 cm. Histologically, a hematoxylin and eosin (H&E) stained soft-tissue section revealed an ulcerated, parakeratinized, stratified squamous surface epithelium with associated fibrovascular connective tissue that had areas of ulcerations infiltrated with chronic inflammatory cells (Figure 2). This inflammatory cell infiltrate was chiefly composed of eosinophils and lymphocytes and the deeper parts of the section showed muscle fibres (Figure 3).
Figure 1.

Clinical image showing ulceration in the left lateral border of the tongue
Figure 2.
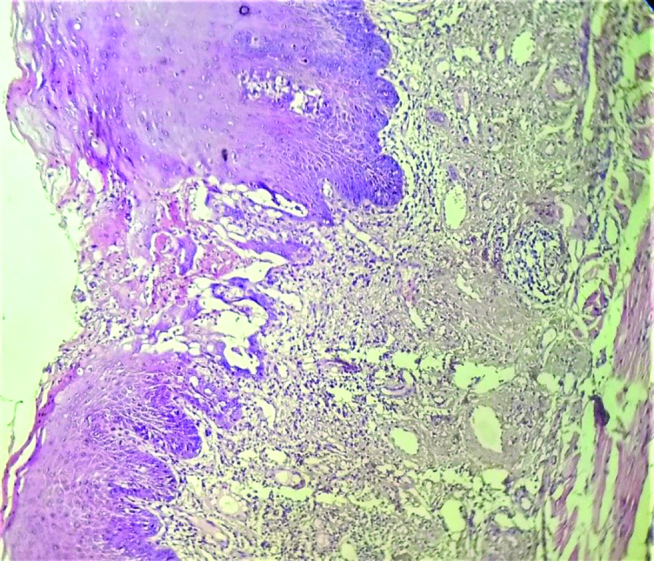
Section showing ulcerated epithelium and dense inflammatory cell infiltrate in connective tissue (standard magnification 10x)
Figure 3.
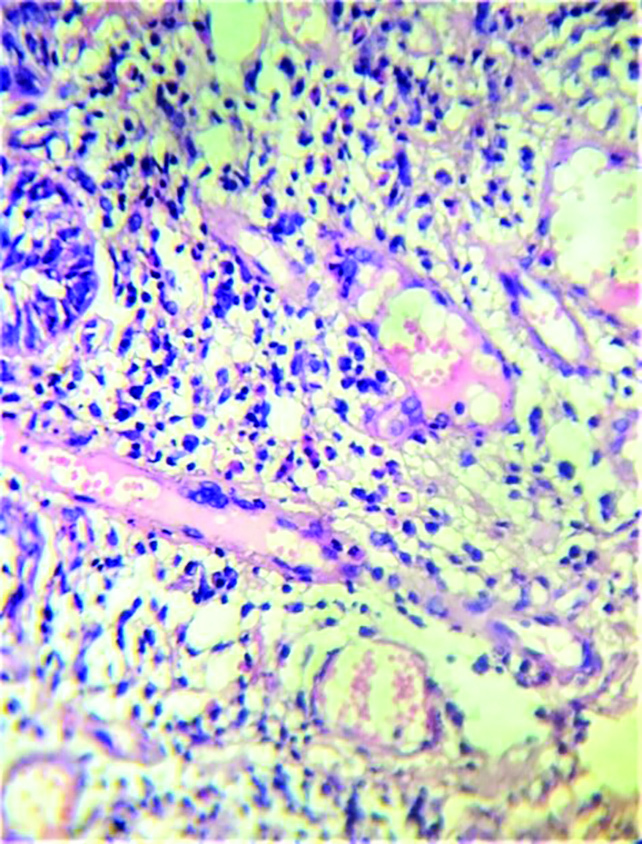
Section showing chronic inflammatory cells such as lymphocytes, plasma cells, and eosinophils (standard magnification 40x)
Postoperative outcome
The postoperative recovery was uneventful, and the client was reviewed after 10 days. On this first review, the healing of the surgical site was satisfactory. After 3 months, on the second review, the surgical site was completely healed and there was no recurrence.
DISCUSSION
TUGSE was first described by Popoff in 1956; the first case of TUGSE was reported in 1960. However, it was not considered a distinct entity until 1970 following the publication of research by Shapiro and Juhlin. 5 Although various etiological factors have been proposed, such as sharp tooth margins and ill-fitting dentures, trauma has been identified as the chief etiology of TUGSE. 5 Some studies have reported males to be more prone to present with such a rare phenomenon, giving a male to female ratio of 3:1. 1,2 However, Elzay et al. 6 , after examining 41 clients, concluded there was no gender predilection and reported that females were as equally affected as males. Conversely, Salisburg et al. 3 studied this lesion in 37 clients and reported a slight female predilection, with a ratio of 1:1.85. In terms of age, TUGSE has often been reported in clients between the ages of 30 years and 50 years, which is consistent with the present case. Interestingly, it has also been observed frequently in infants and, in those cases, is known as “Riga-fede disease of infants.” 7
Sharma et al. 8 reported that TUGSE frequently occurs on the left posterolateral surface of the tongue while Soyele et al. 5 proclaimed the dorsum and ventero-lateral surface of the tongue to be the common site of occurrence. Although various sites, such as the lips, buccal mucosa, palate, gingiva, and floor of the mouth, have also been reported, the tongue appears to be the most common site.
TUGSE manifests as a self-limiting ulcer with rolled borders and everted margins that mimic squamous cell carcinoma. 4,9 This traumatic ulceration on the tongue is subsequently invaded by micro-organisms and often by viral and toxic agents. These toxic agents induce an exaggerated inflammatory response that attracts mast cells and eosinophils to the site. Further, the mast cell degranulation recruits more eosinophils by the release of eosinophilic chemotactic factors of anaphylaxis. These eosinophils release histamines and aryl sulfates that prevent the degranulation of mast cells, suppress basophils, and limit the release of other inflammatory mediators. 5
Histologically, in this case report, the TUGSE presented as a surface ulceration with parakeratinized, stratified squamous surface epithelium in association with fibrovascular connective tissue which exhibited a dense, mixed inflammatory cell infiltrate chiefly composed of eosinophils. Shen et al. 2 reported that, typically in such lesions, there is a uniform distribution of eosinophils among the muscle fibres. However, deeper muscle fibres rarely show presence of any eosinophils. The present case report has similar findings to those of Shen et al. 2
Immunohistochemical studies show positivity for CD30, a transmembrane protein that has an extracellular domain homologous to tumour necrosis factor. These CD30 proteins are abundantly expressed in neoplastic lesions. 5 They are also expressed on the activated B and T cells, while the expression of this protein in TUGSE is generally inconsistent and scanty. Hirshberg et al. 9 reported CD30 proteins in 40% of cases; Salisbury et al. 3 showed CD30 proteins in 70% of TUGSE lesions. Chatzistamou et al. 10 reported that large, mononuclear cells were evident in the inflammatory cell infiltrate that expressed positivity for CD30. These findings suggest that this lesion may originate from B cells of an atypical lymphoproliferative disorder with the presence of monoclonal B cells. 10,11
The recommended management of TUGSE is to treat the underlying cause of the lesion. 7,11,12 However, other modalities include use of a 0.1% triamcinolone acetonide mouthwash (typically used to treat erosive lichen planus), electrocoagulation, and liquid nitrogen. Sharma et al. 8 reported that surgical excision is the preferred treatment for TUGSE, and rapid healing has been observed after excision of the lesion. 5 Although TUGSE has a favourable prognosis post-treatment, a minimum of 2 years of follow-up is mandatory. 7 Shen et al. 2 observed 34 cases and recorded recurrence in 1 case. They emphasized that the reason for recurrence may have been a failure to eliminate the causative factors such as sharp tooth margins and ill-fitting prostheses.
CONCLUSION
TUGSE seems to be often misdiagnosed by clinicians due to limited knowledge and awareness. This ulcer can be diagnosed with the help of histopathological studies that show the ulceration infiltrated by inflammatory cells, predominantly eosinophils. Thus, clinicians must remember to include TUGSE in their differential diagnosis for such solitary ulcers that have a close resemblance to squamous cell carcinoma.
CONFLICTS OF INTEREST
The authors have declared no conflicts of interest.
Footnotes
CDHA Research Agenda category: risk assessment and management
References
- Farooq S , Hamid R , Kour G , Shah A Traumatic ulcerative granuloma with stromal eosinophilia: a clinical study Int J Applied Dental Sci 2018 ; 4 ( 2 ): 80 - 82 [Google Scholar]
- Shen WR , Chang JY , Yang CW , Cheng SJ , Chen HM , Wang YP Oral traumatic ulcerative granuloma with stromal eosinophilia: a clinicopathological study of 34 cases J Formos Med Assoc 2015 ; 114 : 881 - 885 [DOI] [PubMed] [Google Scholar]
- Salisbury CL , Steven DB , Shiyong L T-cell receptor gene rearrangement and CD30 immunoreactivity in traumatic ulcerative granuloma with stromal eosinophilia of the oral cavity Am J Clin Pathol 2009 ; 132 : 722 - 727 [DOI] [PubMed] [Google Scholar]
- Marszałek A, Neska-długosz I Traumatic ulcerative granuloma with stromal eosinophilia. A case report and short literature review Pol J Pathol 2011;3:172-175 [PubMed] [Google Scholar]
- Shapiro L , Juhlin EA Eosinophilic ulcer of the tongue report of two cases and review of the literature Dermatologica 1970 ; 140 : 242 - 250 [PubMed] [Google Scholar]
- Elzay RP Traumatic ulcerative granuloma with stromal eosinophilia (Riga‑Fede disease and traumatic eosinophilic granuloma) Oral Surg Oral Med Oral Pathol 1983 ; 55 : 497 - 506 [DOI] [PubMed] [Google Scholar]
- Sarangarajan R , Vaishnavi VVK , Sivadas G , Sarangarajan A , Meera S Traumatic ulcerative granuloma with stromal eosinophilia—Mystery of pathogenesis revisited J Pharm Bioallied Sci 2015 ; 7 ( Suppl 2 ): S420 - S423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma B , Koshy G , Kapoor S Traumatic ulcerative granuloma with stromal eosinophila: a case report and review of pathogenesis J Clin Diagn Res 2016 Oct ; 10 ( 10 ): ZD07 - ZD09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirshberg A , Amariglio N , Akrish S , Yahalom R , Rosenbaum H , Okon E , et al. Traumatic ulcerative granuloma with stromal eosinophilia: a reactive lesion of the oral mucosa Am J Clin Pathol 2006 ; 126 : 522 - 529 [DOI] [PubMed] [Google Scholar]
- Chatzistamou I , Ipatia DA , Georgiou G , Gkilas H , Prodromidis G , Maria A , et al. Traumatic ulcerative granuloma with stromal eosinophilia J Oral Maxillofac Surg 2012 ; 70 : 349 - 353 [DOI] [PubMed] [Google Scholar]
- Dhanrajani P , Cropley P Oral eosinophilic or traumatic ulcer: a case report and brief review Natl J Maxillofac Surg 2015 ; 6 ( 2 ): 237 - 240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagaraj T, Okade D, Sinha P, Mahalakshmi IP Traumatic ulcerative granuloma with stromal eosinophilia: a diagnostic dilemma? J Adv Clin Res Insights 2014;3:102-105 [Google Scholar]


