Abstract
COVID-19, an acute respiratory disease caused by SARS-CoV-2, has rapidly become a pandemic. On the other hand, obesity is also reaching dramatic dimensions and it is a risk factor for morbidity and premature mortality. Obesity has been linked to a high risk of serious-associated complications to COVID-19, due to the increased risk of concomitant chronic diseases, which highlights the health public relevance of the topic. Obese subjects have a pro-inflammatory environment, which can further exacerbate COVID-19-induced inflammation and oxidative stress, explaining the increased risk of serious complications in these patients. Another factor that favors infection in obese patients is the high expression of ACE2 receptors in the adipose tissue. The negative impact of COVID-19 in obesity is also associated with a decrease in respiratory function, the concurrence of multiple comorbidities, a low-degree chronic inflammatory state, immunocompromised situation, and therefore a higher rate of hospitalization, mechanical ventilation, in-hospital complications such as pneumonia, and death. In this review, the link between obesity and COVID-19 was analyzed, exploring the potential common mechanisms in both diseases, with special attention to oxidative stress and inflammation, due to the crucial role of both pathways in the development of the disease.
Keywords: COVID-19, Obesity, Body mass index, Inflammation, Immunity, Oxidative stress, Nutrition
Introduction
COVID-19, an acute respiratory disease caused by the coronavirus SARS-CoV-2, emerged in December 2019 in a market in Wuhan (Hubei, China), which rapidly turned this a pandemic affecting the vast majority of the countries of the world [69]. The available evidence indicates that SARS-CoV-2 had its origin in processes of natural selection [4]. The significant transmissibility of this new coronavirus and the high mortality associated with COVID-19, in addition to the lack of effective pharmacological treatment, have turned this disease into a serious health problem worldwide [1]. As of May 4, 2020, 184 affected countries had been reported, with 396.558.014 confirmed cases and 5.745.032 deaths [82].
Obesity, on the other hand, is reaching pandemic proportions in the world population, and it is a risk factor for morbidity and premature death [35] with numerous and detrimental repercussions for health and quality of life [78]. Obesity is considered a risk factor for numerous chronic conditions such as type 2 diabetes, hypertension, dyslipidemia, cardiovascular diseases, stroke, sleep apnea and cancer [78].
Obesity, age over 65 years, sex (male), smoking, diabetes, respiratory and cardiovascular diseases have been identified as major risk factors for severe complications of COVID-19 [42, 89]. One of the first reports that evaluated the risk factors for severe disease, found a prevalence of 20% diabetes and 30% high blood pressure in patients diagnosed with SARS-CoV infection [90]. Likewise, obesity has been linked to serious complications associated with COVID-19, due to the increased risk of concomitant chronic diseases [41]. Previous studies have shown the close relationship between similar viruses such as influenza and obesity, where patients with body mass index (BMI) > 40 kg/m2 have higher risk of suffering complications from this viral pathology [7, 39, 54]. In this sense, hence during the 2009 H1N1 flu pandemic, obesity was recognized as an independent risk factor [53].
The World Obesity Federation warns that health systems are not prepared to deal with the growing number of obese patients and that the COVID-19 pandemic will further expose their limitations (World Obesity Federation, 2020). Patients with high BMI could present complications at the time of intubation, due to difficulties in diagnostic images. It is possible that the equipment necessary to care for these patients is available only in some hospitals or specialized units to treat these patients. Obese patients may also have difficulties in the prone position necessary during the treatment of acute respiratory syndrome due to COVID-19 [33].
The concomitance of the COVID-19 and obesity pandemics worldwide highlights the health public relevance of the topic. An increasing amount of scientific literature reveals the close link between obesity, clinical symptoms and the pathological evolution of COVID-19. This review explores the link between obesity and COVID-19, exploring the potential common mechanisms in both pandemics, with special attention to oxidative stress and inflammation, due to the crucial role of both pathways in the development of the disease.
Changes in the respiratory system due to the obesity
Obesity (diagnosed by a BMI equal or higher than 30 kg/m2) represents the main risk factor for severe outcomes of COVID-19. However, in a recent prospective study performed in 6.9 million people in England, the authors found that at a BMI of more than 23 kg/m2, there was an increased risk admission to hospital, admission to intensive care units and death [30]. In addition, obesity has a very marked impact on respiratory function and gas exchange and plays a key role in diseases such as asthma, sleep apnea–hypopnea syndrome, obesity-hypoventilation syndrome and pneumonia [60]. In a study of 148.494 adults in the USA with COVID-19, conducted by Kompaniyets et al. [46], discovered a nonlinear relationship between IMC and COVID-19 severity, with lower risks in BMI around the umbral between healthy weight and obesity in the majority of cases, and then increasing with a higher BMI. Overweight and obesity were both risk factors for invasive mechanical ventilation, and obesity was found to be a risk factor for hospitalization and death, particularly among those under the age of 65.
The chronic inflammatory state associated with obesity can be responsible of some of these deleterious changes and can potentiate and aggravate the immune response against viral infection [73]. Obesity has a negative influence on ventilatory mechanics because it affects the elastic resistance of the rib cage, decreases functional residual and total lung capacity which predispose to breathing difficulties. It is known that lung volumes and increased elastic tension in the rib cage decrease the effectiveness or function of the airways [70]. There is a proportional and dependent relationship between the subject's BMI and pulmonary elastic resistance. In this sense, obese patients present a rapid adaptation to shallow breathing to the increase in fatty depots in the chest area [64]. This type of shallow breathing increases ventilatory requirements and oxygen consumption [34]. In addition, obesity can cause muscular hypertrophy secondary to the increased exertion of breathing caused by mechanical overload, which causes muscular dysfunction with increased activity of the diaphragm [57]. Control of respiratory centers in obese subjects is also not homogeneous. In some individuals, increased breathing rate alters the response of the respiratory center to hypercapnia and hypoxemia. There is a high occlusion pressure in obese patients, which reflects the state of the central respiratory impulse, as a consequence of the increase in elastic resistance of the thorax [51].
Additionally, obesity is one of the main risk factors for the development of obstructive sleep apnea syndrome, characterized by recurrent obstruction/collapse of the upper airways, with resulting reduction in airflow, intermittent hypoxia and frequent awakening during sleep [64].
Some studies suggest that obesity could be a very important risk factor in young patients [31]. A study of 3,615 patients reported that obesity is significantly related to intensive care units (ICU) and hospital admissions among patients under 60 years of age [50]. Moreover, another study demonstrated a higher prevalence of obesity among young patients (59% in the 18–49 years group, 49% in the 50–64 years group and 41% in the ≥ 65 years group) on admission [31].
Immune response and obesity during COVID-19
COVID-19 infection presents a great diversity of manifestations, the most serious of which are respiratory symptoms. The key factor in the severity and lethality is the presentation of pneumonia with “cytokine release syndrome” or “cytokine storm.” The main mechanism of this syndrome is the infiltration of inflammatory cells, T cells and macrophages, attracted by the massive release of cytokines [71]. Patients with COVID-19 present a marked increase in interleukin 1β (IL-1β), interferon γ (IFN-γ), protein inducible by interferon 10 (IP-10) and monocyte chemoattractant protein-1 (MCP-1) [52].
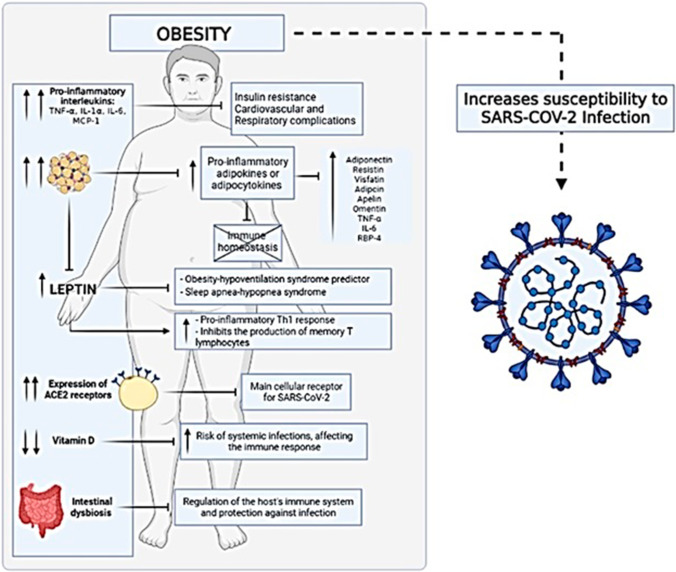
Obesity, on the other hand, is considered a moderate form of chronic inflammation, and interleukins can affect fat cell function in a variety of ways. TNF-, IL-1, IL-6 and MCP-1 are pro-inflammatory interleukins that are elevated in obese people and cause insulin resistance as well as cardiovascular and respiratory issues in patients with obesity [15] (Fig. 1).
Fig. 1.
Obesity induces immune pathophysiologic modifications, increasing susceptibility to SARS-CoV-2 infection. Abbreviation: TNF-α: tumor necrosis factor-alpha; Interleukins: IL; MCP-1: monocyte chemoattractant protein-1; RBP-4: retinol-binding protein 4; ACE2: angiotensin-converting enzyme 2
Additionally, obesity leads to adipose tissue expansion and dysfunction, triggering the release of pro-inflammatory adipokines or adipocytokines [68]. Chronic inflammatory response and the adipose tissue are intricately linked in the immune system [20]. Adipose tissue (AT) performs various functions within the immune system, especially as part of the innate immune response [67]. AT cells population includes not only of adipocytes, but also macrophages, fibroblasts and lymphocytes. Lymphocytes present in AT could be the orchestrators of the inflammatory response of this tissue [26]. Adipocytes are sensitive to various infectious agents through Toll-like lipopolysaccharide receptors (TLRs) [80]. This inflammatory environment, together with the lack of T-helper lymphocytes, causes failure in immune homeostasis, which potentiates the spread of the viral infection.
The adipocyte acts as an endocrine organ and therefore plays an important role in the pathogenesis, evolution and complications of obesity. The adipocyte is known for the production of various adipocytokines such as adiponectin, leptin, resistin, visfatin, adipsin, apelin, omentin, TNF-α, IL-6 and retinol-binding protein 4 (RBP-4) [77]. Serum leptin levels can predict obesity-hypoventilation syndrome better than BMI and are also related to sleep apnea–hypopnea syndrome. Intermittent hypoxemia has been shown to be a potent stimulant of leptin release, regardless of the degree of obesity. Leptin also appears to be connected to the pro-inflammatory T-helper 1 (Th1) response, body composition and energy balance. Leptin promotes the proliferation and activation of peripheral mononuclear cells, as well as the production of Th1-type cytokines like IL-2 and IFN-γ, by lymphocytes, and it is implicated in the production of pro-inflammatory cytokines by circulating monocytes (including IL-6 and TNF-α). Similarly, leptin suppresses memory T lymphocyte development while boosting the amount of B lymphocytes [77]. Patients with obesity exhibit high expression levels of several components for SARS-CoV-2 host cell entry (ACE2, CD147, DPP4 and neuropilin-1) and the spike protein processing enzyme (FURIN) in the visceral adipose tissue [29], and it also has been suggested that AT could serve as a reservoir for the virus [45].
Another commonality between COVID-19, obesity and immunity is vitamin D in the patients. In obese patients, vitamin D deficiency is high, increasing the risk of systemic infections and affecting the immune response [10]. Vitamin D supplementation, on the other hand, can alleviate or prevent respiratory infections by limiting the generation of pro-inflammatory cytokines by the innate immune system, lowering the chance of a cytokine storm that leads to pneumonia [59]. Consequently, studies reported that vitamin D insufficiency may be linked to obesity and increased vulnerability to COVID-19-related morbidity and mortality [36]. Intestinal dysbiosis is another key feature of obesity, and it may play a role in the increased risk of severe COVID-19 infections [3, 23]. Obesity is linked to intestinal dysbiosis, which is necessary for the host's immune system to function properly and to guard against infection. Furthermore, the gut microbiome plays a role in preventing infection-related harm. In fact, certain COVID-19 therapy procedures incorporate the use of probiotics to preserve gut microecology balance and, as a result, indirectly enhance the immune system [78].
Inflammation and oxidative stress
Obesity, persistent low-level inflammation and oxidative stress are all tightly connected. Fat storage causes adipocyte expansion, which results in adipose tissue hypoxia and the release of high quantities of inflammatory cytokines. During SARS-CoV-2 infection, an important mechanism linking the cytokine storm and organ damage is cell death. Several proteins of the SARS-CoV-2 can induce inflammatory cell death, which engages three programmed cell death pathways: pyroptosis, apoptosis and necroptosis [49]. Interestingly, the viral spike protein subunit S1 triggers pyroptosis, apoptosis and necroptosis in human visceral adipocytes. Thus, patients with obesity might increase their COVID-19 susceptibility due to increased adipose tissue expression of SARS-CoV-2 receptors and the amplification of viral protein S1-induced inflammatory cell death in visceral adipocytes [29]. A key aspect of adipose tissue-based inflammation is the reciprocal modulation of pro-inflammatory and anti-inflammatory adipocytokines. [19].
Adipocyte hypoxia promotes cell necrosis, which attracts macrophages and other phagocytic cells [63] and produces an environment that encourages inflammation to persist in the adipose tissue [86]. Increased quantities of visceral adipose tissue cause the portal venous system to transfer more inflammatory adipocytokines and free fatty acids to the liver. These factors may increase the synthesis of C reactive protein (CRP) in the liver. As a result, in the context of obesity, the liver is an important secondary site of inflammation [76].
Cellular lipid loading may cause oxidative stress in adipocytes, triggering and perpetuating the inflammatory cascade. It has been claimed that this process is influenced not just by the amount of fat consumed, but also by the type of fat consumed. Given their proximity to inflammatory pathways, lipid mediators, particularly arachidonic acid-derived eicosanoids, are the leading suspects in this process. [44]. Several adult studies have found a possible relationship between food, adipose tissue fatty acid content and obesity. [2, 83]. Clinical studies of obese people have found a link between adipokine levels in the blood and markers of inflammation and/or oxidative stress. [79].
Adiposity, insulin resistance and metabolic syndrome have all been linked to oxidative stress, suggesting that it may be an early event in the pathophysiology of these chronic diseases. Furthermore, a number of studies have linked total body fat and waist circumference to oxidative stress-induced endothelial dysfunction, as well as, more recently, vascular endothelial cell NADPH oxidase activity [9].
The state of inflammation and oxidative stress appear to have a significant impact on obesity. Thus, obesity is associated with the activation of inflammatory cytokines such as TNF-, IL-6 and inflammatory-related molecules such as NF and other transcription factors, either as a cause or as a result of obesity. Overproduction of glucocorticoids in obese people has also been linked to the obesity–inflammation interaction. The involvement of the inflammasome in obesity could explain some of the negative metabolic aspects associated with the increase in adipose tissue and the linkages between pro-inflammatory resources and metabolic stress. Overproduction of glucocorticoids in obese people has also been linked to the obesity–inflammation interaction. The involvement of the inflammasome in obesity could explain some of the negative metabolic aspects associated with the increase in adipose tissue and the linkages between pro-inflammatory resources and metabolic stress. In addition, genetic variants linked to individual vulnerability to obesity, inflammation and oxidative stress have been discovered through gene–environment interactions research. The importance of carrying single-nucleotide polymorphisms (SNPs) on genes that influence both obesity and inflammation, such as PPAR and IL-6, is being investigated in order to confirm the mutual impact of inflammation and oxidative state on obesity [9].
Oxidative stress, obesity and COVID-19
In COVID-19 metabolic obese patients, clinical and biochemical tests revealed that IL-6 was significantly elevated, and CRP was favorably connected with waist-to-hip ratio [17]. Overactivation of the complement system, which is an essential host mediator of virus-induced illnesses and exacerbates inflammation, is also linked to excess adiposity [81]. Furthermore, those with obesity have a higher prevalence of vitamin D deficiency, which has been related to a variety of inflammations, infections and lung disorders, and it can also raise the risk of systemic infections and harm the immune system. Obesity could become a risk factor for cytokine storm if they work together [87]. In this sense, obesity is linked to chronic low-grade inflammation, immunological dysregulation and an increase in free fatty acids and glucose levels in the blood, which leads to an increase in acetyl-CoA concentration, which increases electron donor production (NADH) in the tricarboxylic acid cycle. [55]. When excess NADH cannot be eliminated by oxidative phosphorylation (or other mechanisms), the mitochondrial proton gradient rises and electron transfer to oxygen rises, resulting in the formation of free radicals (especially superoxide anion) and oxidative stress. [56].
In severe cases, when SARS-CoV-2 invades the respiratory epithelium, produces an amplified inflammatory reaction that generates reactive oxygen species (ROS) such as superoxide, hydrogen peroxide and ozone which are highly oxidant molecules potentially capable of damaging cell membrane lipids, cytoplasmic proteins and nuclear DNA, producing cell necrosis and lysis [8]. Patients with moderate and severe COVID-19 frequently experience respiratory distress, which is commonly alleviated by oxygen therapy but can lead to oxidative stress and ARDS. Hyperoxia has been found to cause ROS production in mitochondria, which inhibits oxidative phosphorylation and lowers ATP levels [16]. Monocytes and macrophages are thought to play a key role in the inflammatory processes that precede severe COVID-19 infection [62]. These immune cells produce a lot of pro-inflammatory cytokines (IL-1, IL-6, TNF, IL-8), which is typical of COVID-19 patients who are critically ill [15, 61, 88].
Inside the host cell, its viral replication process begins, the viral RNA is released into the cytoplasm. The new virions are released from the host cell by exocytosis and other cells of the respiratory epithelium will be invaded [74]. As a consequence of this infection, an immune response modulated by the inflammatory process and oxidative stress occurs [43], which is more exacerbated in obese patients [47].
In addition, SARS-CoV-2 induces oxidative stress in the host cell and this mechanism can be used by the virus to increase replication and modify cell biochemistry for its benefit [75]. SARS-CoV-2 infection triggers the production of ROS which induces the stabilization of hypoxia-inducible factor 1α (HIF-1α) and the action of this factor inhibits the T cell response and reduces epithelial cell survival. Likewise, cells infected by SARS-CoV-2 adapt their metabolism after infection and become highly glycolytic, which facilitates the replication of the virus [18].
It has been proposed that in patients with SARS-CoV-2, oxidative stress is associated with coagulopathy and cellular hypoxia [13]. Since oxidative stress is the link of all known mechanisms for viral infection, including SARS-CoV-2, the use of antioxidants, such as glutathione (GSH), can have a positive effect on the recovery of patients with viral infections. Other compounds such as vitamin E, vitamins C, D and selenium, chelating agents that form complexes with iron (deferoxamine), NF-κB inhibitors (NSAIDs, dexamethasone, curcumin, gingerol, etc.), polyphenols, Nuclear factor erythroid 2-related factor 2 (Nrf2) activators (curcumin, resveratrol) and the use of specific pro-inflammatory cytokine inhibitors and anticoagulants [22, 75] can also be used in the management of viral infections. NF-κB inhibitor drugs, such as caffeic acid phenethyl ester (CAPE), that inhibit NF-κB activation have been found to reduce SARS-CoV-2 inflammation in mice [21].
GSH is the most essential antioxidant defense in the lungs and is the principal antioxidant agent in mammals. [12]. When the balance between GSH and GSSG is disrupted by increased ROS, a more oxidative environment oxidizes the proteins that control the activation and localization of transcription factors like Kelch-like ECH-associated protein-1 (KEAP-1), which regulates Nrf2, and IB, which regulates NF-B, activating the anti-inflammatory pathway and inactivating the inflammatory pathway, activating the anti-inflammatory pathway and inactivating the inflammatory pathway [84]. In this way, the cell controls oxidative stress, however, in viral infections, KEAP-1) remains bound to Nrf2, causing its degradation via ubiquitination in the proteasome, or degrading it by non-canonical routes independent of KEAP-1 [65]. Coronavirus infections lead to alterations of the redox balance in infected cells through modulation of NAD + biosynthesis. Therefore, SH group donor molecules, Nrf2 activators and NF-κB inhibitors are potential therapeutic options for infection by RNA viruses, including SARS-CoV-2. This therapeutic approach has been reported to reverse severe symptoms due to different viruses and SARS-CoV-2 [40]. RNA viruses require the active NF-κB pathway within host cells in order to replicate and SARS-CoV-2 is no exception, therefore drugs that inhibit NF-κB activation potentially reduce viral replication. The results obtained in the study of Checconi [14] suggest that reducing oxidative stress is a viable strategy in the management of viral infections. By modulating redox-sensitive pathways, the immune response can be regulated and control viral infection, an aspect that has been studied in the context of a wide variety of viruses, including SARS-CoV-2 [14].
Comorbidities associated with obesity and COVID-19
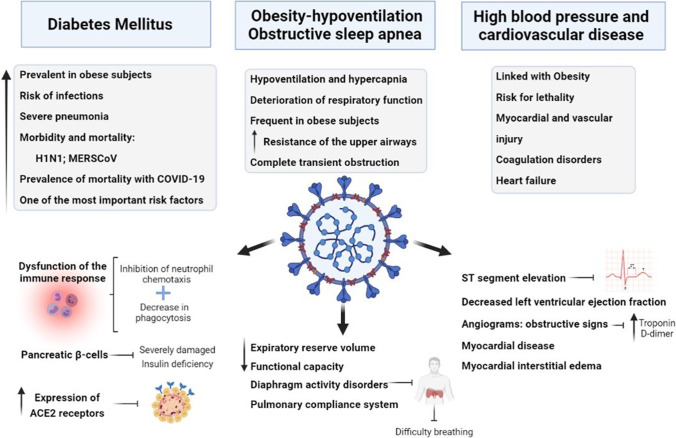
Obesity not only has an impact on mortality, but is also a risk factor for the presentation of severe clinical manifestations such as acute respiratory distress syndrome [11, 38] the need for invasive ventilation [73] or admission to the ICU [50] (Fig. 2). On the other hand, Hajifathalian et al. [38] and Cai et al. [11] reported a higher risk of developing respiratory distress compared to non-obese patients. Another important comorbidity associated with obesity and COVID-19, is nonalcoholic fatty liver disease (NAFLD) [58]. The liver of patients with obesity and biopsy-proven NAFLD or nonalcoholic steatohepatitis (NASH) [28] show increased expression of SARS-CoV-2 receptor ACE2 and spike protein processing enzyme TMPRSS2, which might predispose individuals with obesity to COVID-19. In addition, the alterations in the innate and adaptive immune system in NAFLD might further contribute to severe complications of COVID-19 [48].
Fig. 2.
Comorbidities associated with obesity and COVID-19 and their main clinical manifestations. Abbreviation: ACE2: angiotensin-converting enzyme 2
Diabetes mellitus
Diabetes is highly prevalent in obese subjects and increases the risk of infections and other complications, especially severe pneumonia. The risk decreases with good glycemic control. Diabetes has been described as a risk factor for morbidity and mortality in other respiratory infections caused by viruses such as influenza A (H1N1) or respiratory infection caused by Middle Eastern Coronavirus (MERSCoV) [5]. Data in patients with diabetes infected with SARS-CoV-2 are limited. The study with the largest number of patients collected in China found a higher prevalence of mortality in people with diabetes, being one of the most important risk factors together with arterial hypertension [37]. In several meta-analyses conducted in China with studies with smaller populations, the prevalence of diabetes is estimated to be around 8–10% [25, 27, 85]. The higher incidence and severity of COVID-19 in diabetic patients are explained by several mechanisms. Diabetic patients feature an inhibition of neutrophil chemotaxis, a decrease in phagocytosis and, therefore, a dysfunction of the immune response. On the other hand, in diabetic patients there is also a dysregulation of the inflammatory signaling which is delayed due to the delay in the activation of Th1 cells, however the inflammatory signaling can be exacerbated [32]. A higher rate of Th17 cells and inflammatory cytokines has been described in patients with diabetes infected by SARS-CoV-2, which could explain the exacerbated inflammatory response [37]. In addition, pancreatic β-cells can be severely damaged by SARS-CoV-2, which would lead to insulin deficiency. On the other hand, patients with diabetes mellitus have a higher risk of cardiovascular disease, therefore the presence of other associated comorbidities such as arterial hypertension would justify the increase in mortality in these patients. Furthermore, in the islets of Langerhans there is a high expression of ACE2 receptors, which could suppose the main cellular receptor for SARS-CoV-2, causing an acute inflammatory reaction in β-cells known as insulitis, causing a hyperglycemic state in non-diabetic patients and, on the other, a hyperglycemic decompensation in those previously diabetic patients [85].
High blood pressure and cardiovascular disease
Obesity is linked with high blood pressure and cardiovascular disease constituting a risk for lethality due to the infection and even more so if they are associated with diabetes. These patients suffer myocardial and vascular injury, coagulation disorders with thrombotic and embolic phenomena, cardiac arrhythmias, acute coronary episodes and heart failure with cardiogenic shock. In a recent study, the electrocardiogram and echocardiogram of the patients suffering from COVID-19 revealed ST segment elevation, decreased left ventricular ejection fraction, poor wall mobility, and on angiograms they had obstructive signs with elevation of troponin and D-dimer. Myocardial disease in COVID-19 patients could be due to plaque rupture, cytokine storm, hypoxic injury, coronary spasm, microthrombi, or direct vascular or endothelial injury. Magnetic resonance imaging revealed myocardial interstitial edema in these patients. [6]. In these patients, cerebrovascular episodes have also been reported [6, 90].
Obesity-hypoventilation and obstructive sleep apnea syndromes
The obesity-hypoventilation syndrome is characterized by hypoventilation, hypercapnia and the deterioration of respiratory function is worsened by the decreased ventilatory response to hypercapnia, frequent in obese subjects, which produces a tendency to drowsiness [72]. In some obese subjects, the condition is classified as obstructive sleep apnea syndrome. Generally, they suffer from centripetal or thoraco-abdominal obesity, with the respiratory alterations described, which are associated with an increase in the resistance of the upper airways. In the most serious situation, during sleep, a complete transient obstruction of the respiratory flow can occur with the production of more or less prolonged apneas. This syndrome is characterized by at least 5 apneas lasting 10 s or more for each hour of sleep. This syndrome is due to the narrowing of the airway, due to laryngeal fat accumulation, together with a loss of glossopharyngeal muscle tone, with the result of a reduction in airflow during the inspiratory phases. There is evidence in the literature that reinforces the relationship between leptin [72] and ventilatory deterioration in obesity, such as that the level of leptin is a better predictor of the presence of obstructive hypoventilation syndrome than BMI [66] and this is independent of the presence or absence of apneas during sleep and that the elevated levels of leptin in this syndrome are corrected with non-invasive ventilation. Independently of the sleep apnea syndrome, obesity is associated with a reduction in expiratory reserve volume, functional capacity and the pulmonary compliance system. In addition, in patients with abdominal obesity, lung function is further impaired by diaphragm activity disorders, making breathing even more difficult, which establishes another risk factor for obesity in severe manifestations of COVID-19 infection [24].
Conclusion
The increase in the prevalence of obesity in recent years may be related to a greater number of people who may have serious complications with COVID-19 infection. Obese subjects have a pre-established pro-inflammatory environment, which can further exacerbate COVID-19-induced inflammation and oxidative stress, explaining the increased risk of serious complications in these patients. The data also suggest that obesity could be a very important factor in younger people. Obesity is considered a mild chronic inflammation situation, and, in this sense, several pro-inflammatory interleukins that are increased in obese people, such as TNF-α, IL-1α, IL-6 and MCP-1, induce undesirable effects during the COVID-19 infection. Leptin also appears to link the pro-inflammatory Th1 response, body composition and energy balance, stimulating the proliferation and activation of peripheral mononuclear cells, and the production of pro-inflammatory cytokines. Another factor that favors infection in obese patients is the high expression of ACE2 receptors in the adipose tissue, the main cellular receptor for SARS-CoV-2, suggesting that could serve as a reservoir for the virus. In patients with SARS-CoV-2, oxidative stress is associated with the amplification of the cytokine storm, coagulopathy and cellular hypoxia. By modulating redox-sensitive pathways, the immune response can be regulated and control viral infection, which can have a positive effect on the recovery of patients. The negative impact of COVID-19 during obesity is also associated with a decrease in expiratory reserve volume and functional capacity, ventilation difficulties due to the decrease in diaphragmatic excursion, the concurrence of multiple comorbidities, a chronic inflammatory state of low degree, immunocompromised situations, and therefore a higher rate of hospitalization, mechanical ventilation, in-hospital complications such as pneumonia, and death.
Acknowledgements
Jorge Moreno-Fernandez was funded by a Postdoctoral “Margarita Salas” contract through the NextGenerationEU Programme of the European Union and is grateful to the Spanish Ministry of Universities and the University of Granada for the concession of the contract. Figures have been created with BioRender.com tool.
Author contributions
J.D.-C. designed the study; J.M.-F. and J.D.-C. performed the literature search; J.D.-C., J.M.-F. and J.J.O. screened the articles; L.O.M., F.N. and O.C. validated the screened articles; J.D.-C., J.M.-F. and J.J.O. wrote original review; L.O.M., F.N. and O.C. reviewed and edited the manuscript. All authors interpreted the data, wrote the paper and have read and approved the final manuscript. The authors declare that all data were generated in-house and that no paper mill was used.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Footnotes
Julio Ochoa and Javier Díaz-Castro are both co-senior authors.
Key points
• Recent findings reveal a high risk of COVID-19 in obese subjects.
• Obesity could exacerbate COVID-19-induced inflammation and oxidative stress.
• Obesity has been associated with a higher risk of significant COVID-19-related consequences.
• Obesity and COVID-19 share some comorbidities and that predispose to high morbidity and mortality.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Jorge Moreno-Fernandez, Email: jorgemf@ugr.es.
Julio Ochoa, Email: jjoh@ugr.es.
References
- 1.Adhikari SP, Meng S, Wu YJ, Mao YP, Ye RX, Wang QZ, Sun C, Sylvia S, Rozelle S, Raat H, et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect Dis Poverty. 2020;9:29. doi: 10.1186/s40249-020-00646-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ailhaud G, Guesnet P, Cunnane SC. An emerging risk factor for obesity: does disequilibrium of polyunsaturated fatty acid metabolism contribute to excessive adipose tissue development? Br J Nutr. 2008;100:461–470. doi: 10.1017/S0007114508911569. [DOI] [PubMed] [Google Scholar]
- 3.Aktas B, Aslim B. Gut-lung axis and dysbiosis in COVID-19. Turkish journal of biology = Turk biyoloji dergisi. 2020;44:265–272. doi: 10.3906/biy-2005-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Andersen KG, Rambaut A, Lipkin WI, Holmes EC, Garry RF. The proximal origin of SARS-CoV-2. Nat Med. 2020;26:450–452. doi: 10.1038/s41591-020-0820-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Badawi A, Ryoo SG. Prevalence of comorbidities in the Middle East respiratory syndrome coronavirus (MERS-CoV): a systematic review and meta-analysis. International journal of infectious diseases : IJID : official publication of the International Society for Infectious Diseases. 2016;49:129–133. doi: 10.1016/j.ijid.2016.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bangalore S, Sharma A, Slotwiner A, Yatskar L, Harari R, Shah B, Ibrahim H, Friedman GH, Thompson C, Alviar CL, et al. ST-Segment Elevation in Patients with Covid-19 - A Case Series. N Engl J Med. 2020;382:2478–2480. doi: 10.1056/NEJMc2009020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bhattacharya I, Ghayor C, Pérez Dominguez A, Weber FE. From Influenza Virus to Novel Corona Virus (SARS-CoV-2)-The Contribution of Obesity. Frontiers in endocrinology. 2020;11:556962. doi: 10.3389/fendo.2020.556962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Biswas S, Das R, Ray Banerjee E. Role of free radicals in human inflammatory diseases. AIMS Biophysics. 2017;4:596–614. doi: 10.3934/biophy.2017.4.596. [DOI] [Google Scholar]
- 9.Bondia-Pons I, Ryan L, Martinez JA. Oxidative stress and inflammation interactions in human obesity. J Physiol Biochem. 2012;68:701–711. doi: 10.1007/s13105-012-0154-2. [DOI] [PubMed] [Google Scholar]
- 10.Bouillon R, Marcocci C, Carmeliet G, Bikle D, White JH, Dawson-Hughes B, Lips P, Munns CF, Lazaretti-Castro M, Giustina A, et al. Skeletal and Extraskeletal Actions of Vitamin D: Current Evidence and Outstanding Questions. Endocr Rev. 2019;40:1109–1151. doi: 10.1210/er.2018-00126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cai Q, Chen F, Wang T, Luo F, Liu X, Wu Q, He Q, Wang Z, Liu Y, Liu L, et al. Obesity and COVID-19 Severity in a Designated Hospital in Shenzhen, China. Diabetes Care. 2020;43:1392–1398. doi: 10.2337/dc20-0576. [DOI] [PubMed] [Google Scholar]
- 12.Cantin AM, North SL, Hubbard RC, Crystal RG. Normal alveolar epithelial lining fluid contains high levels of glutathione. Journal of applied physiology (Bethesda, Md; 1985) 1987;63:152–157. doi: 10.1152/jappl.1987.63.1.152. [DOI] [PubMed] [Google Scholar]
- 13.Cecchini R, Cecchini AL. SARS-CoV-2 infection pathogenesis is related to oxidative stress as a response to aggression. Med Hypotheses. 2020;143:110102–110102. doi: 10.1016/j.mehy.2020.110102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Checconi P, De Angelis M, Marcocci ME, Fraternale A, Magnani M, Palamara AT, Nencioni L. Redox-Modulating Agents in the Treatment of Viral Infections. Int J Mol Sci. 2020;21:4084. doi: 10.3390/ijms21114084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen G, Wu D, Guo W, Cao Y, Huang D, Wang H, Wang T, Zhang X, Chen H, Yu H, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Investig. 2020;130:2620–2629. doi: 10.1172/JCI137244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chernyak BV, Popova EN, Prikhodko AS, Grebenchikov OA, Zinovkina LA, Zinovkin RA. COVID-19 and Oxidative Stress. Biochemistry Biokhimiia. 2020;85:1543–1553. doi: 10.1134/S0006297920120068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chiappetta S, Sharma AM, Bottino V, Stier C. COVID-19 and the role of chronic inflammation in patients with obesity. Int J Obes. 2020;44:1790–1792. doi: 10.1038/s41366-020-0597-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Codo AC, Davanzo GG, Monteiro LB, de Souza GF, Muraro SP, Virgilio-da-Silva JV, Prodonoff JS, Carregari VC, de Biagi Junior CAO, Crunfli F, et al. Elevated Glucose Levels Favor SARS-CoV-2 Infection and Monocyte Response through a HIF-1α/Glycolysis-Dependent Axis. Cell Metab. 2020;32:437–446.e435. doi: 10.1016/j.cmet.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Codoñer-Franch P, Valls-Bellés V, Arilla-Codoñer A, Alonso-Iglesias E. Oxidant mechanisms in childhood obesity: the link between inflammation and oxidative stress. Translational research : the journal of laboratory and clinical medicine. 2011;158:369–384. doi: 10.1016/j.trsl.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 20.de Heredia FP, Gómez-Martínez S, Marcos A. Obesity, inflammation and the immune system. Proc Nutr Soc. 2012;71:332–338. doi: 10.1017/S0029665112000092. [DOI] [PubMed] [Google Scholar]
- 21.DeDiego ML, Nieto-Torres JL, Regla-Nava JA, Jimenez-Guardeño JM, Fernandez-Delgado R, Fett C, Castaño-Rodriguez C, Perlman S, Enjuanes L. Inhibition of NF-κB-mediated inflammation in severe acute respiratory syndrome coronavirus-infected mice increases survival. J Virol. 2014;88:913–924. doi: 10.1128/JVI.02576-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Delgado-Roche L, Mesta F. Oxidative Stress as Key Player in Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV) Infection. Arch Med Res. 2020;51:384–387. doi: 10.1016/j.arcmed.2020.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dhar D, Mohanty A. Gut microbiota and Covid-19- possible link and implications. Virus research. 2020;285:198018. doi: 10.1016/j.virusres.2020.198018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dietz W, Santos-Burgoa C. Obesity and its Implications for COVID-19 Mortality. Obesity (Silver Spring, Md) 2020;28:1005. doi: 10.1002/oby.22818. [DOI] [PubMed] [Google Scholar]
- 25.Emami A, Javanmardi F, Pirbonyeh N, Akbari A. Prevalence of Underlying Diseases in Hospitalized Patients with COVID-19: a Systematic Review and Meta-Analysis. Arch Acad Emerg Med. 2020;8:e35–e35. [PMC free article] [PubMed] [Google Scholar]
- 26.Exley MA, Hand L, O'Shea D, Lynch L. Interplay between the immune system and adipose tissue in obesity. J Endocrinol. 2014;223:R41–48. doi: 10.1530/JOE-13-0516. [DOI] [PubMed] [Google Scholar]
- 27.Fadini GP, Morieri ML, Longato E, Avogaro A. Prevalence and impact of diabetes among people infected with SARS-CoV-2. J Endocrinol Invest. 2020;43:867–869. doi: 10.1007/s40618-020-01236-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fondevila MF, Mercado-Gómez M, Rodríguez A, Gonzalez-Rellan MJ, Iruzubieta P, Valentí V, Escalada J, Schwaninger M, Prevot V, Dieguez C, et al. Obese patients with NASH have increased hepatic expression of SARS-CoV-2 critical entry points. J Hepatol. 2021;74:469–471. doi: 10.1016/j.jhep.2020.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Frühbeck G, Catalán V, Valentí V, Moncada R, Gómez-Ambrosi J, Becerril S, Silva C, Portincasa P, Escalada J, Rodríguez A. FNDC4 and FNDC5 reduce SARS-CoV-2 entry points and spike glycoprotein S1-induced pyroptosis, apoptosis, and necroptosis in human adipocytes. Cell Mol Immunol. 2021;18:2457–2459. doi: 10.1038/s41423-021-00762-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gao M, Piernas C, Astbury NM, Hippisley-Cox J, O'Rahilly S, Aveyard P, Jebb SA. Associations between body-mass index and COVID-19 severity in 6·9 million people in England: a prospective, community-based, cohort study. Lancet Diabetes Endocrinol. 2021;9:350–359. doi: 10.1016/S2213-8587(21)00089-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Garg S. Hospitalization Rates and Characteristics of Patients Hospitalized with Laboratory-Confirmed Coronavirus Disease 2019 — COVID-NET. MMWR Morb Mortal Wkly Rep. 2020;69:458–464. doi: 10.15585/mmwr.mm6915e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Geerlings SE, Hoepelman AI. Immune dysfunction in patients with diabetes mellitus (DM) FEMS Immunol Med Microbiol. 1999;26:259–265. doi: 10.1111/j.1574-695X.1999.tb01397.x. [DOI] [PubMed] [Google Scholar]
- 33.Ghelichkhani P, Esmaeili M. Prone Position in Management of COVID-19 Patients; a Commentary. Arch Acad Emerg Med. 2020;8:e48–e48. [PMC free article] [PubMed] [Google Scholar]
- 34.Gibson GJ. Obesity, respiratory function and breathlessness. Thorax. 2000;55(Suppl 1):S41–S44. doi: 10.1136/thorax.55.suppl_1.S41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Global BMIMC, Di Angelantonio E, Bhupathiraju ShN, Wormser D, Gao P, Kaptoge S, Berrington de Gonzalez A, Cairns BJ, Huxley R, Jackson ChL, et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet (London, England) 2016;388:776–786. doi: 10.1016/S0140-6736(16)30175-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Grant WB, Lahore H, McDonnell SL, Baggerly CA, French CB, Aliano JL, Bhattoa HP (2020) Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths. Nutrients 12 [DOI] [PMC free article] [PubMed]
- 37.Guan W-j, Ni Z-y, Hu Y, Liang W-h, Ou C-q, He J-x, Liu L, Shan H, Lei C-l, Hui DSC, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hajifathalian K, Kumar S, Newberry C, Shah S, Fortune B, Krisko T, Ortiz-Pujols S, Zhou XK, Dannenberg AJ, Kumar R, et al. Obesity is Associated with Worse Outcomes in COVID-19: Analysis of Early Data from New York City. Obesity (Silver Spring, Md) 2020;28:1606–1612. doi: 10.1002/oby.22923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Honce R, Schultz-Cherry S. Impact of Obesity on Influenza A Virus Pathogenesis, Immune Response, and Evolution. Front Immunol. 2019;10:1071. doi: 10.3389/fimmu.2019.01071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Horowitz RI, Freeman PR, Bruzzese J. Efficacy of glutathione therapy in relieving dyspnea associated with COVID-19 pneumonia: A report of 2 cases. Respiratory medicine case reports. 2020;30:101063. doi: 10.1016/j.rmcr.2020.101063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Huang Y, Lu Y, Huang YM, Wang M, Ling W, Sui Y & Zhao HL (2020) Obesity in patients with COVID-19: a systematic review and meta-analysis. Metab: Clin Experiment 113:154378 [DOI] [PMC free article] [PubMed]
- 42.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet (London, England) 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Iddir M, Brito A, Dingeo G, Fernandez Del Campo SS, Samouda H, La Frano MR, Bohn T. Strengthening the Immune System and Reducing Inflammation and Oxidative Stress through Diet and Nutrition: Considerations during the COVID-19 Crisis. Nutrients. 2020;12:1562. doi: 10.3390/nu12061562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Iyer A, Fairlie DP, Prins JB, Hammock BD, Brown L. Inflammatory lipid mediators in adipocyte function and obesity. Nat Rev Endocrinol. 2010;6:71–82. doi: 10.1038/nrendo.2009.264. [DOI] [PubMed] [Google Scholar]
- 45.Kassir R. Risk of COVID-19 for patients with obesity. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2020;21:e13034. doi: 10.1111/obr.13034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kompaniyets L, Goodman AB, Belay B, Freedman DS, Sucosky MS, Lange SJ, Gundlapalli AV, Boehmer TK, Blanck HM. Body Mass Index and Risk for COVID-19-Related Hospitalization, Intensive Care Unit Admission, Invasive Mechanical Ventilation, and Death - United States, March-December 2020. MMWR Morb Mortal Wkly Rep. 2021;70:355–361. doi: 10.15585/mmwr.mm7010e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Korakas E, Ikonomidis I, Kousathana F, Balampanis K, Kountouri A, Raptis A, Palaiodimou L, Kokkinos A, Lambadiari V. Obesity and COVID-19: immune and metabolic derangement as a possible link to adverse clinical outcomes. American Journal of Physiology-Endocrinology and Metabolism. 2020;319:E105–E109. doi: 10.1152/ajpendo.00198.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lamadrid P, Alonso-Peña M, San Segundo D, Arias-Loste M, Crespo J, Lopez-Hoyos M. Innate and Adaptive Immunity Alterations in Metabolic Associated Fatty Liver Disease and Its Implication in COVID-19 Severity. Frontiers in immunology. 2021;12:651728. doi: 10.3389/fimmu.2021.651728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lee S, Channappanavar R, Kanneganti TD. Coronaviruses: Innate Immunity, Inflammasome Activation, Inflammatory Cell Death, and Cytokines. Trends Immunol. 2020;41:1083–1099. doi: 10.1016/j.it.2020.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lighter J, Phillips M, Hochman S, Sterling S, Johnson D, Francois F, Stachel A. Obesity in Patients Younger Than 60 Years Is a Risk Factor for COVID-19 Hospital Admission. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2020;71:896–897. doi: 10.1093/cid/ciaa415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lin CK, Lin CC. Work of breathing and respiratory drive in obesity. Respirology (Carlton, Vic) 2012;17:402–411. doi: 10.1111/j.1440-1843.2011.02124.x. [DOI] [PubMed] [Google Scholar]
- 52.Liu E, Marin D, Banerjee P, Macapinlac HA, Thompson P, Basar R, Nassif Kerbauy L, Overman B, Thall P, Kaplan M, et al. Use of CAR-Transduced Natural Killer Cells in CD19-Positive Lymphoid Tumors. N Engl J Med. 2020;382:545–553. doi: 10.1056/NEJMoa1910607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Louie JK, Acosta M, Winter K, Jean C, Gavali S, Schechter R, Vugia D, Harriman K, Matyas B, Glaser CA, et al. Factors associated with death or hospitalization due to pandemic 2009 influenza A(H1N1) infection in California. JAMA. 2009;302:1896–1902. doi: 10.1001/jama.2009.1583. [DOI] [PubMed] [Google Scholar]
- 54.Luzi L, Radaelli MG. Influenza and obesity: its odd relationship and the lessons for COVID-19 pandemic. Acta Diabetol. 2020;57:759–764. doi: 10.1007/s00592-020-01522-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Maddux BA, See W, Lawrence JC, Jr, Goldfine AL, Goldfine ID, Evans JL. Protection against oxidative stress-induced insulin resistance in rat L6 muscle cells by micromolar concentrations of alpha-lipoic acid. Diabetes. 2001;50:404–410. doi: 10.2337/diabetes.50.2.404. [DOI] [PubMed] [Google Scholar]
- 56.Maechler P, Jornot L, Wollheim CB. Hydrogen peroxide alters mitochondrial activation and insulin secretion in pancreatic beta cells. J Biol Chem. 1999;274:27905–27913. doi: 10.1074/jbc.274.39.27905. [DOI] [PubMed] [Google Scholar]
- 57.Magnani KL, Cataneo AJ. Respiratory muscle strength in obese individuals and influence of upper-body fat distribution. Sao Paulo Medical Journal = Revista paulista de medicina. 2007;125:215–219. doi: 10.1590/S1516-31802007000400004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Marjot T, Webb GJ, Barritt ASt, Moon AM, Stamataki Z, Wong VW, Barnes E. COVID-19 and liver disease: mechanistic and clinical perspectives. Nature reviews Gastroenterology & hepatology. 2021;18:348–364. doi: 10.1038/s41575-021-00426-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Martineau AR, Jolliffe DA, Greenberg L, Aloia JF, Bergman P, Dubnov-Raz G, Esposito S, Ganmaa D, Ginde AA, Goodall EC, et al. Vitamin D supplementation to prevent acute respiratory infections: individual participant data meta-analysis. Health technology assessment (Winchester, England) 2019;23:1–44. doi: 10.3310/hta23020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Masa JF, Pépin JL, Borel JC, Mokhlesi B, Murphy PB, Sánchez-Quiroga M (2019) Obesity hypoventilation syndrome. Eur Respir Rev 28 [DOI] [PMC free article] [PubMed]
- 61.Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet (London, England) 2020;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Merad M, Martin JC. Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages. Nat Rev Immunol. 2020;20:355–362. doi: 10.1038/s41577-020-0331-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.O'Rourke RW, White AE, Metcalf MD, Olivas AS, Mitra P, Larison WG, Cheang EC, Varlamov O, Corless CL, Roberts CT, Jr, et al. Hypoxia-induced inflammatory cytokine secretion in human adipose tissue stromovascular cells. Diabetologia. 2011;54:1480–1490. doi: 10.1007/s00125-011-2103-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Parameswaran K, Todd DC, Soth M. Altered respiratory physiology in obesity. Can Respir J. 2006;13:203–210. doi: 10.1155/2006/834786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Patra U, Mukhopadhyay U, Mukherjee A, Sarkar R, Chawla-Sarkar M. Progressive Rotavirus Infection Downregulates Redox-Sensitive Transcription Factor Nrf2 and Nrf2-Driven Transcription Units. Oxid Med Cell Longev. 2020;2020:7289120. doi: 10.1155/2020/7289120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Phipps PR, Starritt E, Caterson I, Grunstein RR. Association of serum leptin with hypoventilation in human obesity. Thorax. 2002;57:75–76. doi: 10.1136/thorax.57.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pond CM. Adipose tissue and the immune system. Prostaglandins Leukot Essent Fatty Acids. 2005;73:17–30. doi: 10.1016/j.plefa.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 68.Rakotoarivelo V, Variya B, Langlois MF, Ramanathan S. Chemokines in human obesity. Cytokine. 2020;127:154953. doi: 10.1016/j.cyto.2019.154953. [DOI] [PubMed] [Google Scholar]
- 69.Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. Journal of Autoimmunity. 2020;109:102433. doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sant'Anna M, Jr, Carvalhal RF, Oliveira F, Zin WA, Lopes AJ, Lugon JR, Guimarães FS. Respiratory mechanics of patients with morbid obesity. Jornal brasileiro de pneumologia : publicacao oficial da Sociedade Brasileira de Pneumologia e Tisilogia. 2019;45:e20180311. doi: 10.1590/1806-3713/e20180311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Shimabukuro-Vornhagen A, Gödel P, Subklewe M, Stemmler HJ, Schlößer HA, Schlaak M, Kochanek M, Böll B, von Bergwelt-Baildon MS. Cytokine release syndrome. J Immunother Cancer. 2018;6:56. doi: 10.1186/s40425-018-0343-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Shimura R, Tatsumi K, Nakamura A, Kasahara Y, Tanabe N, Takiguchi Y, Kuriyama T. Fat accumulation, leptin, and hypercapnia in obstructive sleep apnea-hypopnea syndrome. Chest. 2005;127:543–549. doi: 10.1378/chest.127.2.543. [DOI] [PubMed] [Google Scholar]
- 73.Simonnet A, Chetboun M, Poissy J, Raverdy V, Noulette J, Duhamel A, Labreuche J, Mathieu D, Pattou F, Jourdain M. High Prevalence of Obesity in Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) Requiring Invasive Mechanical Ventilation. Obesity (Silver Spring, Md) 2020;28:1195–1199. doi: 10.1002/oby.22831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Song Z, Xu Y, Bao L, Zhang L, Yu P, Qu Y, Zhu H, Zhao W, Han Y, Qin C (2019) From SARS to MERS, Thrusting Coronaviruses into the Spotlight. Viruses 11 [DOI] [PMC free article] [PubMed]
- 75.Suhail S, Zajac J, Fossum C, Lowater H, McCracken C, Severson N, Laatsch B, Narkiewicz-Jodko A, Johnson B, Liebau J, et al. Role of Oxidative Stress on SARS-CoV (SARS) and SARS-CoV-2 (COVID-19) Infection: A Review. Protein J. 2020;39:644–656. doi: 10.1007/s10930-020-09935-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Tilg H. Adipocytokines in nonalcoholic fatty liver disease: key players regulating steatosis, inflammation and fibrosis. Curr Pharm Des. 2010;16:1893–1895. doi: 10.2174/138161210791208929. [DOI] [PubMed] [Google Scholar]
- 77.Tilg H, Moschen AR. Adipocytokines: mediators linking adipose tissue, inflammation and immunity. Nat Rev Immunol. 2006;6:772–783. doi: 10.1038/nri1937. [DOI] [PubMed] [Google Scholar]
- 78.Upadhyay J, Farr O, Perakakis N, Ghaly W, Mantzoros C. Obesity as a Disease. Med Clin North Am. 2018;102:13–33. doi: 10.1016/j.mcna.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 79.Vincent HK, Bourguignon CM, Weltman AL, Vincent KR, Barrett E, Innes KE, Taylor AG (2009) Effects of antioxidant supplementation on insulin sensitivity, endothelial adhesion molecules, and oxidative stress in normal-weight and overweight young adults. Metab: Clin Experiment 58:254–262 [DOI] [PMC free article] [PubMed]
- 80.Vitseva OI, Tanriverdi K, Tchkonia TT, Kirkland JL, McDonnell ME, Apovian CM, Freedman J, Gokce N. Inducible Toll-like receptor and NF-kappaB regulatory pathway expression in human adipose tissue. Obesity (Silver Spring, Md) 2008;16:932–937. doi: 10.1038/oby.2008.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Watanabe M, Risi R, Tuccinardi D, Baquero CJ, Manfrini S, Gnessi L (2020) Obesity and SARS-CoV-2: A population to safeguard. Diabetes/Metab Res Rev e3325 [DOI] [PubMed]
- 82.WHO. (2020) Coronavirus disease (COVID-19). Situation Report-105. World Health Organization:1–18
- 83.Williams ES, Baylin A, Campos H. Adipose tissue arachidonic acid and the metabolic syndrome in Costa Rican adults. Clinical nutrition (Edinburgh, Scotland) 2007;26:474–482. doi: 10.1016/j.clnu.2007.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Winterbourn CC, Hampton MB. Thiol chemistry and specificity in redox signaling. Free Radical Biol Med. 2008;45:549–561. doi: 10.1016/j.freeradbiomed.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 85.Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, Ji R, Wang H, Wang Y, Zhou Y. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. International journal of infectious diseases : IJID : official publication of the International Society for Infectious Diseases. 2020;94:91–95. doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ye J. Adipose tissue vascularization: its role in chronic inflammation. Curr DiabRep. 2011;11:203–210. doi: 10.1007/s11892-011-0183-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Yu W, Rohli KE, Yang S, Jia P. Impact of obesity on COVID-19 patients. Journal of Diabetes and its Complications. 2021;35:107817. doi: 10.1016/j.jdiacomp.2020.107817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Zhang W, Zhao Y, Zhang F, Wang Q, Li T, Liu Z, Wang J, Qin Y, Zhang X, Yan X, et al. The use of anti-inflammatory drugs in the treatment of people with severe coronavirus disease 2019 (COVID-19): The Perspectives of clinical immunologists from China. Clinical immunology (Orlando, Fla) 2020;214:108393. doi: 10.1016/j.clim.2020.108393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Zheng Z, Peng F, Xu B, Zhao J, Liu H, Peng J, Li Q, Jiang C, Zhou Y, Liu S, et al. Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. J Infect. 2020;81:e16–e25. doi: 10.1016/j.jinf.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet (London, England) 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]