Abstract
Most cases of intussusception are thought to be idiopathic, related to viral infections, structural abnormalities, or certain vaccinations. In this report, we present the development of intussusception in a pediatric patient who was coronavirus 2019 (COVID‐19) positive. Although the most common gastrointestinal symptoms of COVID‐19 virus are diarrhea and vomiting, there recently have been rare case reports of intussusception in patients throughout the world who are severe acute respiratory syndrome coronavirus 2 positive. This case is only the second known report in the United States and the second case reported globally that required surgical intervention for definitive management.
Keywords: coronavirus, COVID‐19, currant jelly, doughnut sign, intussusception, rotavirus, target sign
1. INTRODUCTION
Intussusception is a common abdominal emergency in early childhood with a mean age of 6 to 18 months with an incidence in the United States from 0.24 to 2.4 per 1000 live births. 1 It is an idiopathic condition in most instances, with ≈30% of cases having an identifiable cause such as Meckel's diverticulum, polyps, vaccines, or viral infections. 2 It is thought that the associated immune response to viral infections results in mesenteric lymphadenopathy, which serves as a lead point, creating the opportunity for the disease process. 3 The most common subtype is ileocolic intussusception, and this is likely secondary to the ileocecal anatomy as well as the abundance of lymphoid tissue found in the terminal ileum. 4 The understanding of this pathophysiology serves as a mechanism by which the coronavirus 2019 (COVID‐19) virus may precipitate intussusception.
Initial presentation of COVID‐19 in pediatric patients seems to vary widely and can even include intussusception as the initial finding. There have been 6 documented cases worldwide that reported intussusception on presentation of pediatric patients with severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) infection, making this the seventh case. This case is only the second to be reported in the United States. This adds to growing evidence of intussusception being a clinically significant manifestation of the SARS‐CoV‐2 infection. Clinicians should have a high index of suspicion for intussusception in the pediatric population with gastrointestinal (GI) complaints regardless of known exposure to COVID‐19.
2. CASE PRESENTATION
A 4‐month‐old boy with no past medical history and born at term 39 weeks 3 days presented to the pediatric emergency department (ED) accompanied by his mother for the complaint of 2 episodes of blood in stool that began 2–3 hours before presentation. According to the mother, the patient had decreased intake of formula during the preceding 24 hours with only 1 wet diaper in the same timeframe. The mother brought the patient to the ED after first noticing 1 episode of brown, normal‐colored stool mixed with some blood and mucus followed by a second episode of only blood and mucus noted in the diaper. On arrival, there was a third episode of mucus and blood in the diaper that was witnessed by the ED physicians, which appeared to be “currant jelly” stool. Additional history included the patient receiving routine scheduled immunizations 9 days before the ED visit that included inactivated polio vaccine (IPV); pneumococcal conjugate vaccine (PCV13); rotavirus (Rotarix); diphtheria, tetanus, and pertussis; and Haemophilus influenzae type b.
In the ED, initial vital signs were within normal limits, with exception of a heart rate of 153 beats per minute with a normal rhythm. On physical examination, he was awake, alert, and in no acute distress, but he did appear lethargic and was not engaging actively as would be normal for his age. An abdominal examination revealed discomfort to palpation diffusely without distension, rigidity, and no palpable masses. No additional significant findings were noted on examination, and all other systems were grossly normal. During the initial hospital course, he was started on intravenous fluid therapy and was ordered nothing by mouth in anticipation of potential operative intervention.
Laboratory studies revealed an elevated total leukocyte count of 15.08 × 103/mcl (reference range, 7.91–13.41 × 103/mcl) with neutrophil predominance and an elevated platelet count of 649 × 103/mcl (reference range, 215–448 × 103/mcl). Serum chemistry revealed significant hypochloremia of 96 mmol/L (reference range, 98–107 mmol/L), mild metabolic acidosis with bicarbonate level of 21 mmol/L (reference range, 22–29 mmol/L), and anion gap of 19 mEq/L (reference range, 6–18 mEq/L). A nasopharyngeal polymerase chain reaction swab for SARS‐CoV‐2 was positive and procalcitonin elevated to 0.32 ng/ml (reference range, 0.02–0.08 ng/ml). Additional laboratory studies were within the normal reference range.
An abdominal radiograph (Figure 1) revealed multiple dilated loops of bowel in the mid and left abdomen; there was no radiographic evidence of pneumoperitoneum. Ultrasound of the abdomen demonstrated apparent bowel within bowel forming a “doughnut sign” and measuring approximately 6.7 × 2.8 × 3.7 cm in the mid‐pelvic region posterior to the bladder (Figure 2). The area was described as a hyperechoic center and hypoechoic wall that likely represents intussusception with some internal vascularity within the lesion.
FIGURE 1.
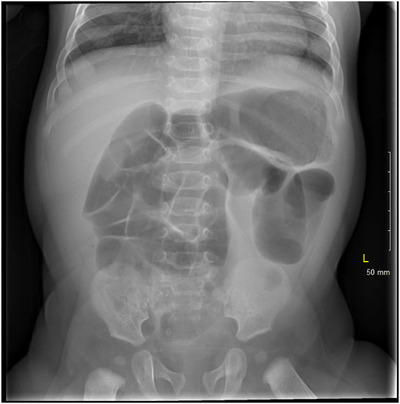
Dilated loops of bowel measuring up to 2.9 cm with a paucity of rectal gas
FIGURE 2.
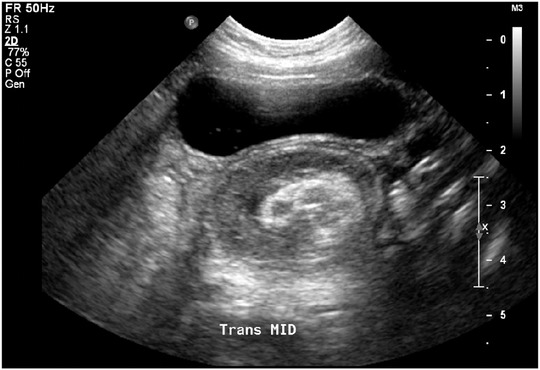
“Doughnut sign” posterior to the bladder likely represents bowel within bowel, which is a classic finding for intussusception
After confirming the diagnosis on ultrasound, a barium enema was performed and demonstrated partial reduction of ileocolic intussusception up to the level of the hepatic flexure without evidence of further reduction beyond the hepatic flexure. At this time the patient was taken for an exploratory laparotomy by the pediatric surgery team. The surgical intervention was successful in locating ileocolic intussusception reaching the hepatic flexure, which was reduced without any areas of compromise requiring resection. After the procedure, the patient was observed as an inpatient for several days and was eventually advanced to a liquid diet and was discharged home on hospital day 5.
3. DISCUSSION
The SARS‐CoV‐2 virus that first appeared in late 2019 has resulted in >96 million confirmed cases and >2 million deaths worldwide according to the World Health Organization (WHO) at the time of this case report in January 2021. There have been many studies attempting to determine the natural course of the SARS‐CoV‐2 infection and possible long‐term effects, but the studies are ongoing. Initially, the pediatric population was thought to be minimally affected by SARS‐CoV‐2; however, multisystem inflammatory syndrome in children first seen in April 2020 has demonstrated the wide range of inflammatory effects the virus can have especially in the pediatric population. SARS‐CoV‐2 has been noted to be associated with GI manifestations with pediatric patients being more affected than adults likely because of their poor attention to hand hygiene. 5 Although viral shedding of SARS‐CoV‐2 is primarily through nasal secretions, a fecal–oral route has been postulated. The possibility of fecal–oral transmission is supported by a study that found that 8 of 10 children who were COVID‐19 positive had positive rectal swabs, even when the nasopharyngeal swabs became negative. 5
It is thought that infections of the GI tract cause lymphoid hyperplasia and hypertrophy of the Peyer's patches. 2 It is this adenopathy that is believed to act as a lead point, called the intussuscipiens, as a result of Peyer's patches acting as an area of traction causing invagination of the distal peristaltic bowel, called the intussusceptum, which forms mechanical obstruction. It is thought that the widespread immune activation seen in COVID‐19 may likely result in such lymphoid hyperplasia and hypertrophy of Peyer's patches, which initiates the suspected pathophysiology of intussusception described previously. 6 Based on the postulated pathogenesis of intussusception and the likelihood that COVID‐19 directly affects the GI tract more in children than adults, it is not surprising that intussusception is a possible presentation or complication of SARS‐CoV‐2 infection.
Among the previously recorded cases of intussusception with SARS‐CoV‐2 infection, all cases presented with “currant jelly” stools in infants <1 year of age. Interestingly, half of the prior cases had no associated respiratory complaints, and half of the cases had no known exposure to individuals who were COVID‐19 positive, similar to our case. The majority of other recorded cases of intussusception with COVID‐19 infection were managed with either pneumatic or hydrostatic enema reduction. A retrospective study at the Children's Hospital of Philadelphia found that 89.6% of intussusception cases were reduced with the use of pneumatic or hydrostatic enema. In this study, enema failed in 13.2% of cases, and surgical intervention was required. Of the failed cases in the study, ≈85.1% were also found to have ileocolic intussusception as was the diagnosis in our patient. 7
This case of intussusception is unique because the patient falls outside the average age, being <6 months of age at presentation. In addition, the patient had received the routine scheduled rotavirus (Rotarix) vaccine in the week before presentation, which has long been thought to be associated with an increased likelihood of developing intussusception. Based on the concomitant presence of the SARS‐CoV‐2 infection, it is not clear which cause superseded in the development of intussusception or if both contributed equally. This case report aims to inform clinicians caring for the pediatric population during the ongoing COVID‐19 pandemic to consider this as a differential diagnosis in presence of vague systemic symptoms or GI symptoms in a pediatric patient with confirmed SARS‐CoV‐2 infection.
4. CONCLUSION
We present a rare case of intussusception in the setting of acute SARS‐CoV‐2 infection in an infant <6 months of age with no known exposure to COVID‐19 and without any respiratory symptoms. After reviewing the 6 other case reports of intussusception in pediatric patients who were SARS‐CoV‐2 positive, it seems plausible that the virus has some direct effect on GI pathology. More studies need to be executed to better understand the mechanism of infectivity of gut epithelial or endothelial cells. Such studies could allow the Centers for Disease Control and Prevention and WHO to better protect the global pediatric and adult patient population throughout the pandemic.
PATIENT CONSENT
Consent was not obtained to publish this case report. The report does not contain personal information that could lead to the identification of the patient.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Swyden S, Damanakis H, Cooper A, Velasquez J, James J. Intussusception in the setting of severe acute respiratory syndrome coronavirus 2 infection following rotavirus vaccination. JACEP Open. 2022;3:e12703. 10.1002/emp2.12703
Supervising Editor: Sing‐Yi Feng, MD.
Funding and Support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
REFERENCES
- 1. Xu Y, Li X, Zhu B, et al. Characteristics of pediatric SARSCoV‐2 infection and potential evidence for persistent fecal viral shedding. Nat Med. 2020;26:502–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Moazzam Z, Salim A, Ashraf A, Jehan F, Arshad M. Intussusception in an infant as a manifestation of COVID‐19. J Pediatr Surg Case Rep. 2020;59:101533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Martínez‐Castaño I, Calabuig‐Barbero E, Gonzálvez‐Piñera J, López‐Ayala JM. COVID‐19 infection is a diagnostic challenge in infants with ileocecal intussusception. Pediatr Emerg Care. 2020;6:e368. [DOI] [PubMed] [Google Scholar]
- 4. Marsicovetere P, Ivatury SJ, White B, Holubar SD. Intestinal intussusception: etiology, diagnosis, and treatment. Clin Colon Rectal Surg. 2017;30(1):30–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. West KW, Stephens B, Vane DW, Grosfeld JL. Intussusception: current management in infants and children. Surgery. 1987;102(4):704–710. [PubMed] [Google Scholar]
- 6. Bazuaye‐Ekwuyasi EA, Camacho AC, Saenz Rios F, et al. Intussusception in a child with COVID‐19 in the USA. Emerg Radiol. 2020;27(6):761–764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ntoulia A, Tharakan SJ, Reid JR, Mahboubi S. Failed intussusception reduction in children: correlation between radiologic, surgical, and pathologic findings. Am J Roentgenol. 2016;207(2):424–433. [DOI] [PubMed] [Google Scholar]


