Abstract
Introduction
Cervical disc replacement (CDR) has become prevalent in the treatment of cervical pathology. CDR is an appealing option for several reasons, including improvement of symptoms, preservation of range of motion, and the absence of risk for nonunion – a complication of an anterior cervical decompression and fusion (ACDF) surgery. In this case series, we explore the use of CDR to treat cervical nonunion.
Methods
Four patients, ages 50 to 64, presented to one surgeon with symptomatic cervical nonunion. Three of the four patients possessed risk factors for further nonunion and were therefore considered especially well-suited to a CDR rather than a revision ACDF. X-ray, MRI, and CT were used to confirm the presence of nonunion and to determine the architectural feasibility of replacing the level with a cervical disc arthroplasty. Six total nonunion levels were present in four patients (two levels in two patients and one level in two patients). Each of the nonunion levels was successfully treated with a revision decompression and CDR.
Results
Postoperatively, all four patients experienced improvement of nonunion symptoms. Neck Disability Index improved on average by 75% (preoperative score 51% to postoperative score 13%). Flexion-extension X-rays were available in three patients, which showed an increase in an average range of motion from 2 degrees to 7 degrees at the revised levels.
Conclusion
The series describing four successful cases expands the current literature and provides support for future investigation into CDR as a treatment for cervical nonunion. We propose CDR as a viable option to treat symptomatic cervical nonunion and restore range of motion in patients without significant arthrosis and with preserved endplate architecture.
Keywords: Cervical disc replacement, Cervical fusion, Nonunion, Spine surgery
Highlights
-
•
Cervical disc replacement as an emerging treatment option for preserving motion
-
•
Four patients with confirmed nonunion successfully received disc replacement.
-
•
All resolved symptoms, measured by NDI, and regained range of motion.
-
•
CDR as viable treatment option for nonunion repair
1. Introduction
Cervical disc replacement (CDR) is growing in popularity for the treatment of cervical spine pathology [1], [2]. Multiple studies over the last 10 years demonstrate that CDR is comparable or superior to anterior cervical discectomy and fusion (ACDF), especially in terms of symptom relief, preserved range of motion, and a lower rate of revision surgery [1], [3], [4]. Additionally, CDR can eliminate the 10% risk of nonunion, a potential complication of ACDF [3]. Repeat fusion as a treatment for cervical nonunion carries the same risks and downsides of ACDF [3]. Accordingly, CDR is proposed as an alternative treatment of cervical nonunion. Herein, we present 4 patients diagnosed with pseudarthrosis following ACDF procedures who received CDR as treatment of the nonunion and clinical follow-up visits. All patients consented to the use of their data and treatment courses for publication. This series has been reported in line with the PROCESS 2020 guideline [5].
2. Methods
Four patients presented to a single surgeon in an outpatient private practice setting 4 to 18 years following their initial fusion to address ongoing symptoms. Nonunion was diagnosed by >3 degrees of motion, lack of connecting bone growth, and lack of synostosis demonstrated on flexion-extension X-rays (3 patients), MRI (4 patients), and CT scan (4 patients), respectively. The CT scans also helped confirm the sufficiency of endplate integrity for the disc arthroplasty and the absence of advanced facet arthrosis.
Six nonunions were present in the four patients. All were between C5 and T1. One patient also had a symptomatic adjacent level requiring surgical intervention. For each patient, appropriate non-operative measures were considered, including physical therapy, epidural steroid injection, and lifestyle modification. However, due to worsening symptoms and quality of life, the four patients received surgical interventions. A CDR was used to treat each nonunion and the symptomatic adjacent level.
In all cases, a standard left-sided Smith-Robinson approach was used, and pseudarthrosis was surgically confirmed at each suspected level. After removal of nonunion fibrocartilage, unincorporated allograft, and PEEK interbody cages, a thorough revision decompression of the spinal canal and foramen was performed in all patients. The intervertebral space was reconstructed with Prestige-LP (Medtronic, Memphis, TN) CDR implant sized to maximize endplate coverage. There were no intraoperative or postoperative complications. The surgical procedure time averaged 130 min (107 to 148 min). Follow-up ranged from 8 to 19 months, 13.5 months on average. Neck Disability Index (NDI) [7] scores were obtained during the preoperative and follow-up visits. Research registry number was obtained for this series [UIN: researchregistry7685].
3. Results
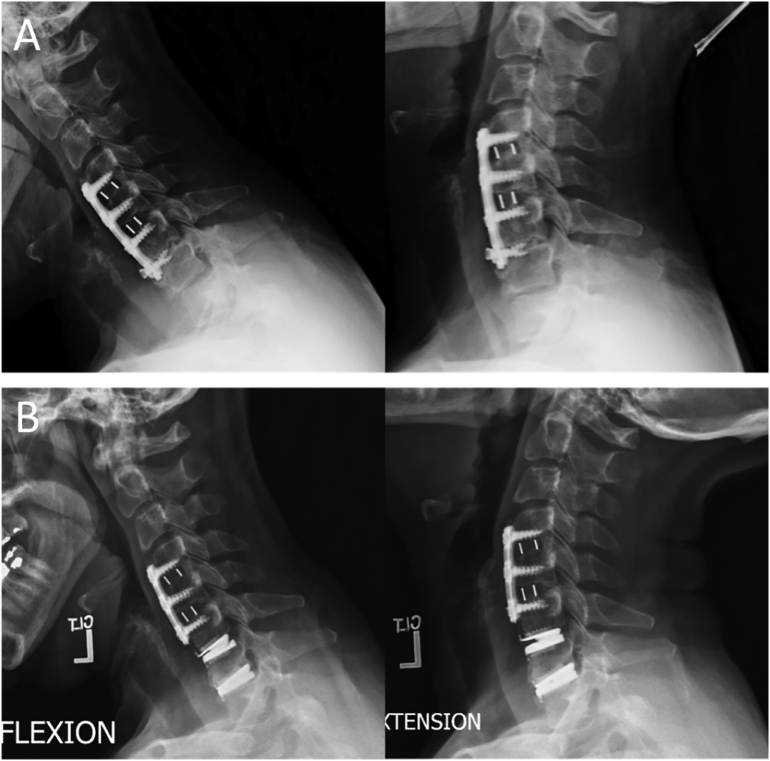
The nonunion treatment with CDR was successful in all 4 patients with no intraoperative or postoperative complications. All four patients experienced improvement of their preoperative axial and radicular symptoms, and no patients required further revision surgeries. Neck Disability Index (NDI) [7] scores obtained during the preoperative and follow-up visits improved on average by 75% (range: 45% to 100%). The preoperative NDI score average was 51% and the postoperative NDI score average was 13%. Postoperative X-rays for the four patients demonstrated well-positioned and functional implants. Preoperative and postoperative flexion-extension X-rays were available in three patients. They demonstrated an average increase in motion at the nonunion level from 2 deg to 7 deg. Fig. 1 shows X-rays for one of the patients studied in this case series.
Fig. 1.
Flexion and extension X-rays of a patient who underwent a pseudarthrosis revision CDR surgery at the C6-C7 level. The flexion and extension X-ray films prior to the operation showed a range of motion at the revised level of 2 degrees (A). 9-month follow-up X-rays demonstrated a range of motion of 9 degrees (B), indicating a 7 degree increase in range of motion. A CDR was also performed at the C7-T1 level due to symptomatic foraminal stenosis at that level.
4. Discussion
Pseudarthrosis rates vary vastly in the literature; 7 to 60% of patients who undergo an ACDF develop a nonunion [3], [6], [8]. Common nonunion side effects include recurrent neck pain, return of radiculopathy, and the need for additional surgery [1], [3], [4], [6]. Revision surgical approaches are revision fusion through ACDF, posterior fusion, or a combined approach [3].
Four reports exist in the literature documenting the reversal of fusions with CDRs [9], [10], [11], [12]. Revision surgeries to reverse the fusions were due to inadequate decompression, recurrence of osteophytes, and/or a suspected pseudarthrosis [9], [10], [11], [12]. Of these case studies, one case series documents the outcomes of CDR in the treatment of pseudarthrosis in five patients with a previous ACDF [9]. In the series, there were no complications, and symptom improvement was experienced in all patients. In all four reports, restoration of motion has been achieved, and in two of these cases, post-operative symptom improvement was noted. To the author's knowledge, there are no other reports in literature documenting the use and outcomes of CDR in the treatment of cervical pseudarthrosis.
There are many potential benefits to ACDF nonunion conversion to CDR including augmented neck range of motion, avoidance of postoperative non-union risk, reduced stress on adjacent levels, and an accelerated return to function post-operatively. In the current series, 4 patients underwent revision surgery to convert a previous ACDF to a CDR to alleviate symptoms associated with their cervical nonunion. All four patients experienced relief from their symptoms related to their nonunion. There was a 75% decrease on average in the NDI scores, demonstrating the increase in patients' functionality after the procedure. All patients reported having a better range of motion in their neck after this motion restoring procedure – range of motion in four levels (3 patients) for which we obtained flexion and extension X-rays showed a 5 (range 3 to 7) degree increase. In particular, one patient regained motion after 18 years of fusion; the longest reported fusion time before being converted to a CDR in past studies was 9 years.
This series adds to the current literature by expanding the number of successful cases, demonstrated by the significantly improved NDI scores and increased range of motion. Additionally, the treatment of nonunion with a CDR in our case series, in addition to past reported case studies, demonstrates increased validity of the treatment across multiple centers.
The treatment of nonunion by a CDR can especially be advantageous with patients presenting with ongoing nonunion risk factors of a repeated ACDF or patients who are non-compliant. Nonunion risk factors for ACDF include smoking status and diabetes mellitus [13], [14]. Two of the four patients studied in this case series are current everyday smokers, and one patient is diabetic. For these patients, a CDR was additionally preferable to a revision ACDF due to the increased risk of another nonunion.
The conversion of a cervical nonunion to a CDR may not be for everyone, and multiple factors should be accounted for before proceeding. The integrity of the bone endplates at the nonunion level must be assessed and is key in deciding whether to proceed with a CDR. The facet joints must be nonfused and without significant arthrosis [9]. It must also be considered whether the anterior plate and interbody spacer can be removed safely without compromising the endplate of the vertebrae [9]. Finally, patients with osteopenia/osteoporosis may not be good candidates due to the added potential for implant subsidence. In cases where these parameters are met and there is a possibility to restore motion to these levels, CDR is a viable option to treat cervical nonunions.
5. Conclusion
The short-term result of the current series supports the potential role of CDR as a viable treatment option for cervical nonunion. The preliminary results of the current series and the other published reports warrant further study with more patients and a longer follow-up period or a randomized prospective trial.
Consent
Each patient consented to the use of their data and treatment course for publication.
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Ethical approval
This case report is exempt from ethical approval by the Mercy Medical Center IRB.
Funding
The authors received no funding in the creation of this manuscript.
Guarantor
Hyun Song, B.A.
Charles C. Edwards II, M.D.
Research registration number
Research Registry, researchregistry7685, https://www.researchregistry.com/browse-the-registry#user-researchregistry/registerresearchdetails/62195d7ff39169001ecc00d6/.
CRediT authorship contribution statement
Sarah Kujala: Data collection, Investigation, Formal analysis, Writing-Original draft. Hyun Song: Data collection, Investigation, Writing – Review & editing, Formal analysis. Ryan Curto: Conceptualization, Writing – Review & editing. Charles Edwards II: Conceptualization, Methodology, Supervision, Project administration, Writing – Reviewing & editing.
Declaration of competing interest
The authors do not have any proprietary interests in the materials described in this article. The authors have not received grant support or research funding related to this manuscript.
References
- 1.Gornet M.F., Lanman T.H., Burkus J.K., et al. Two-level cervical disc arthroplasty versus anterior cervical discectomy and fusion: 10-year outcomes of a prospective, randomized investigational device exemption clinical trial [published online ahead of print, 2019 Jun 21] J. Neurosurg. Spine. 2019:1–11. doi: 10.3171/2019.4.SPINE19157. [DOI] [PubMed] [Google Scholar]
- 2.Phillips F.M., Garfin S.R. Cervical disc replacement. Spine. 2005;30(17 Suppl):S27–S33. doi: 10.1097/01.brs.0000175192.55139.69. [DOI] [PubMed] [Google Scholar]
- 3.Koerner J.D., Kepler C.K., Albert T.J. Revision surgery for failed cervical spine reconstruction: review article. HSS J. 2015;11(1):2–8. doi: 10.1007/s11420-014-9394-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Eck C.F., Regan C., Donaldson W.F., Kang J.D., Lee J.Y. The revision rate and occurrence of adjacent segment disease after anterior cervical discectomy and fusion: a study of 672 consecutive patients. Spine. 2014;39(26):2143–2147. doi: 10.1097/BRS.0000000000000636. [DOI] [PubMed] [Google Scholar]
- 5.Agha R.A., Sohrabi C., Mathew G., Franchi T., Kerwan A., O'Neill N., PROCESS Group The PROCESS 2020 guideline: updating consensus preferred reporting of case series in surgery (PROCESS) guidelines. Int. J. Surg. 2020 Dec;84:231–235. doi: 10.1016/j.ijsu.2020.11.005. [DOI] [PubMed] [Google Scholar]
- 6.Shriver M.F., Lewis D.J., Kshettry V.R., Rosenbaum B.P., Benzel E.C., Mroz T.E. Pseudarthrosis rates in anterior cervical discectomy and fusion: a meta-analysis. Spine J. 2015;15(9):2016–2027. doi: 10.1016/j.spinee.2015.05.010. [DOI] [PubMed] [Google Scholar]
- 7.Vernon H., Mior S. The Neck Disability Index: a study of reliability and validity [published correction appears in J Manipulative Physiol Ther 1992 Jan;15(1):followi] J. Manipulative Physiol. Ther. 1991;14(7):409–415. [PubMed] [Google Scholar]
- 8.McAnany S.J., Baird E.O., Overley S.C., Kim J.S., Qureshi S.A., Anderson P.A. A meta-analysis of the clinical and fusion results following treatment of symptomatic cervical pseudarthrosis. Global Spine J. 2015;5(2):148–155. doi: 10.1055/s-0035-1544176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lanman T.H., CuÉllar J.M. Restoration of spinal motion: conversion of anterior cervical fusion with pseudarthrosis to artificial disc replacement. Int. J. Spine Surg. 2020;14(4):483–487. doi: 10.14444/7063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sekhon L.H. Reversal of anterior cervical fusion with a cervical arthroplasty prosthesis. J. Spinal Disord. Tech. 2005 Feb;18(Suppl):S125–S128. doi: 10.1097/01.bsd.0000117545.88865.b9. PMID: 15699798. [DOI] [PubMed] [Google Scholar]
- 11.Tian W., Han X., Li Z.Y., Mao J.P., Sun Y.Q., James Albert T. Reversal of anterior cervical discectomy and fusion with cervical artificial disc replacement: regain motion after 9 years fusion. J. Spinal Disord. Tech. 2013;26(1):55–59. doi: 10.1097/BSD.0b013e3182337275. [DOI] [PubMed] [Google Scholar]
- 12.Spinelli J., Neal C.J., Rosner M.K. Performance of cervical arthroplasty at a pseudarthrosed level of a MultiLevel anterior cervical discectomy and fusion: case report. Mil. Med. 2016;181(6):e621–e624. doi: 10.7205/MILMED-D-15-00322. [DOI] [PubMed] [Google Scholar]
- 13.Browne J.A., Cook C., Pietrobon R., Bethel M.A., Richardson W.J. Diabetes and early postoperative outcomes following lumbar fusion. Spine. 2007;32(20):2214–2219. doi: 10.1097/BRS.0b013e31814b1bc0. PMID: 17873813. [DOI] [PubMed] [Google Scholar]
- 14.Berman D., Oren J.H., Bendo J., Spivak J. The effect of smoking on spinal fusion. Int. J. Spine Surg. 2017;11(4):29. doi: 10.14444/4029. [DOI] [PMC free article] [PubMed] [Google Scholar]