Abstract
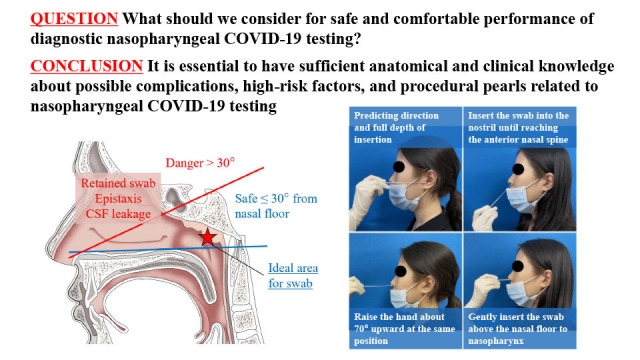
Nasopharyngeal swabs have been widely to prevent the spread of coronavirus disease 2019 (COVID-19). Nasopharyngeal COVID-19 testing is a generally safe and well-tolerated procedure, but numerous complications have been reported in the media. Therefore, the present study aimed to review and document adverse events and suggest procedural references to minimize preventable but often underestimated risks. A total of 27 articles were selected for the review of 842 related documents in PubMed, Embase, and KoreaMed. The complications related to nasopharyngeal COVID-19 testing were reported to be rarely happened, ranging from 0.0012 to 0.026%. Frequently documented adverse events were retained swabs, epistaxis, and cerebrospinal fluid leakage, often associated with high-risk factors, including severe septal deviations, pre-existing skull base defects, and previous sinus or transsphenoidal pituitary surgery. Appropriate techniques based on sufficient anatomical knowledge are mandatory for clinicians to perform nasopharyngeal COVID-19 testing. The nasal floor can be predicted by the line between the nostril and external ear canal. For safe testing, the angle of swab insertion in the nasal passage should remain within 30° of the nasal floor. The swab was gently inserted along the nasal septum just above the nasal floor to the nasopharynx and remained on the nasopharynx for several seconds before removal. Forceful insertion should be attempted, and alternative examinations should be considered, especially in vulnerable patients. In conclusion, patients and clinicians should be aware of rare but possible complications and associated high-risk factors. The suggested procedural pearls enable more comfortable and safe nasopharyngeal COVID-19 testing for both clinicians and patients.
Keywords: Nasopharyngeal Swab, COVID-19 Testing, Complications, Procedural Reference, Risk Factors
Graphical Abstract
INTRODUCTION
The nasopharyngeal swab and rapid antigen detection test or reverse transcription-polymerase chain reaction (RT-PCR) have been performed more than average of 600,000 and 3,000,000 times daily in South Korea1 and USA,2 respectively to detect both symptomatic and asymptomatic patients with coronavirus disease 2019 (COVID-19).3,4,5,6 The initial form of swab, Q-tip, was invented by a Polish-American Leo Gerstenzang to clean his child’s ears in 1923.7,8 The swab gained popularity in the 1950s and is still widely being used in various modified forms from cleaning one’s ear in daily lives to COVID-19 testing in quarantine facilities.
The trans-nasal approach to obtain the respiratory tract secretions in the nasopharynx has been regarded as the gold standard for optimal specimen collection of COVID-19 testing with RT-PCR.3,9 The examination can also be performed on the anterior nares, middle turbinate, and nasopharynx, but the sensitivity resulting from the specimen collected on the anterior nares and middle turbinates was significantly inferior compared with the results of the nasopharynx.3,10 The sensitivity of the rapid antigen detection test using a nasopharyngeal swab was higher than that of the anterior nasal swab often used in the self-performing screening test.6 Therefore, the robust trend to proceed with extensive nasopharyngeal COVID-19 testing is expected to continue considering the diagnostic accuracy and general perception that it is a safe and well-tolerated procedure.3,11,12
However, numerous complications, from minor to even fatal ones, have been repetitively reported in the media13,14 and literatures3,11,12,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36 although complications required further medical evaluation were rarely happened ranging from 0.0012%24 to 0.026%.20 In addition, excessive quarantine burden and stressful condition of the COVID-19 pandemic37,38 occasionally causes uncomfortable testing by the examiner who may not fully understand the nasopharyngeal anatomy or clinically cautious events related to nasopharyngeal swabs.11,39 In this study, a literature review of adverse events related to nasopharyngeal COVID-19 testing was performed to raise attention about rare but existing risks. Moreover, authors suggested the procedural references based on nasopharyngeal anatomy for more comfortable and safe nasopharyngeal COVID-19 testing.
COMPLICATIONS RELATED WITH NASOPHARYNGEAL COVID-19 TESTING
Data searches
The PubMed and Embase databases were searched for articles published between 2019 and 2022. KoreaMed was explored between 2010 and 2022 due to the relative shortage of products in the pilot search. The searched keywords included “nasopharyngeal swab,” “nasopharynx swab,” “nasal swab,” “pernasal swab,” “rhinopharyngeal swab,” “pharyngeal swab,” “nasopharyngeal test,” “swab stick,” “swabbing test,” “complications,” “safe,” “safety,” “COVID,” “severe acute respiratory syndrome,” “coronavirus,” “2019nCoV,” “nCoV2019” or “HCoV-19,” and “NCOVID-19”. The literature search focused on human studies and excluded animal experiments. Articles written in English or Korean were included in the database.
Study selection, data extraction, and assessment
A total of 314, 774, and 29 articles were extracted from the initial search through PubMed, Embase, and KoreaMed databases, respectively. After removing duplicate cases, 842 articles remained. The first author fully screened all abstracts and titles of the results to identify articles related to complications due to nasopharyngeal COVID-19 testing. Finally, 27 articles were selected for review.3,11,12,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,40,41
Documented complications associated with nasopharyngeal COVID-19 testing
All the researched complications due to nasopharyngeal COVID-19 testing were classified, and the related information is shown (Table 1). Retained swabs3,12,16,17,18,20,21,24,26,27,32,35 due to swab fracture during the examination and epistaxis3,12,17,24,28,32 were the frequently reported complications. Cerebrospinal fluid (CSF) leakage3,11,12,15,22,23,28,29,30,33,34,36 was a frequently documented serious adverse event requiring prompt attention and evaluation. Nasal septal abscess,3,12,17,19,25 and ethmoidal silent syndrome31 were also reported as related complications after nasopharyngeal swabbing.
Tables 1. Summary of previously reported adverse events related to coronavirus disease 2019 nasopharyngeal swab testing.
| Complications | References | Article type | No. of cases | Combined medical conditions | Evaluation & management |
|---|---|---|---|---|---|
| Retained swabs | De Luca et al., 202112,16 | Case report | 1 | Swallowed swab in stomach | GI endoscopy |
| Fabbris et al., 20213,12,17 | Letter to editor | 3 | Retained in nasal cavity | Removal under endoscopic view | |
| Farina and Nelson, 202118 | Letter to editor | 1 | Swallowed swab in duodenum | GI endoscopy | |
| Föh et al., 20213,12,20 | Letter to editor | 2 | Retained in nasal cavity, swallowed swab | Nasal endoscopy | |
| Gaffuri et al., 20213,12,21 | Case report | 1 | Retained in choanal cavity | Flexible bronchoscopy | |
| Koskinen et al., 202124 | Research letter | 4 | Retained in nasal cavity | Nasal endoscopy | |
| Molnár et al., 202126 | Case report | 1 | Swallowed swab in stomach | GI endoscopy | |
| Mughal et al., 20203,12,27 | Case report | 1 | Retained in nasal cavity | Nasal endoscopy | |
| Rigante et al., 202132 | Case report | 1 | Retained behind the septal deviation, epistaxis | Nasal endoscopy, mini-septoplasty, removal of septal spur and swab | |
| Tümer and Ardıçlı, 202135 | Letter to editor | 1 | Swallowed swab in duodenum | GI endoscopy | |
| Epistaxis | Fabbris et al., 20213,12,17 | Letter to editor | 4 | Rupture of a small artery of the olfactory area in one case | Nasal packing or surgical cauterization |
| Koskinen et al., 202124 | Research letter | 4 | Local or systemic infection, septum perforation, scarring | Anterior/posterior nasal packing, bipolar coagulation, anterior ethmoidal artery ligation, sphenopalatine artery embolization, local hemostatic, systemic antibiotics | |
| Ovenden et al., 202128 | Case report | 1 | CSF leakage | Nasal endoscopy | |
| Rigante et al., 202132 | Case report | 1 | Retained swab behind the underlying septal deviation | Nasal endoscopy, mini-septoplasty, removal of septal spur and swab | |
| CSF leakage | Agamawi et al., 202111 | Case report | 1 | Sphenoid injury | Endoscopic surgical repair with nasoseptal flap |
| Alberola-Amores et al., 20213,12,15 | Letter to editor | 1 | Cribriform plate injury, meningitis | Systemic antibiotics, corticosteroid | |
| Holmes and Allen, 202122 | Case report | 1 | Pre-existing meningocele, cribriform plate injury, meningitis, ventriculitis | Systemic antibiotics, corticosteroid, endoscopic surgical repair, ventriculo-peritoneal shunt placement | |
| Knížek et al., 202123 | Case report | 1 | Cribriform plate injury | Endoscopic surgical repair, systemic antibiotics | |
| Ovenden et al., 202128 | Case report | 1 | Cribriform plate injury, epistaxis | Nasal endoscopy, conservative management | |
| Paquin et al., 202112,29 | Case report | 1 | Pre-existing encephalocele, cribriform plate injury | Endoscopic surgical repair, bipolar cautery and free mucosal graft | |
| Rajah et al., 20213,12,30 | Case report | 1 | Pre-existing encephalocele, sphenoid injury | Endoscopic skull base repair, excision of encephalocele | |
| Samadian et al., 202133 | Case report | 1 | Cribriform plate injury | Endoscopic surgical repair | |
| Sullivan et al., 20203,12,34 | Case report | 1 | Underlying idiopathic intracranial hypertension, pre-existing encephalocele, cribriform plate injury | Endoscopic surgical repair with acellular human dermal matrix, reduction of the encephalocele | |
| Yilmaz et al., 202136 | Case report | 1 | Past history of minor head trauma, cribriform plate injury | Endoscopic surgical repair with nasoseptal flap | |
| Nasal septal or pharyngeal abscess | Fabbris et al., 20213,12,17 | Letter to editor | 1 | Retained swab, epistaxis | Incision and drainage |
| Fazekas et al., 202119 | Case report | 1 | Preseptal cellulitis, infraorbital abscess | Systemic antibiotics, corticosteroid | |
| Lapeyre et al., 202125 | Case report | 1 | Underlying end stage renal disease, mastoiditis, osteitis, sepsis | Systemic antibiotics | |
| Ethmoidal silent sinus syndrome | Ribeiro et al., 202231 | Case report | 1 | Turbinate fracture | Endoscopic surgical repair with partial resection of the left middle turbinate |
GI = gastrointestinal, CSF = cerebrospinal fluid.
Retained swab
Retained swabs after nasopharyngeal COVID-19 testing have been frequently reported in the literature.3,12,16,17,18,20,21,24,26,27,32,35 Swabs for COVID-19 examination are intrinsically vulnerable to accidental fragmentation due to an inherent breakpoint mechanism for effective transfer to the transport vial, especially in uncooperative or sedated patients.12 Moreover, accidental hard contact with nasal anatomical structures, including septal spurs and inferior and middle turbinates, are other risk factors for swab fracture.12 Therefore, clinicians should remember related anatomical structures and check for the presence of structural anomalies including severe septal deviation before testing. Many cases of the retained swab could be managed with nasal endoscopic removal17,20,24,27 or sometimes retrieved with a bronchoscope.21 In addition, the swab fragments could be found in the gastrointestinal (GI) tract such as the stomach16,26 and duodenum,18,35 which requires GI endoscopy for retrieval. In one case, a fractured swab was found in the upper part of the nose behind the underlying severe septal deviation and was extracted after mini-septoplasty and septal spur removal.32 The possibility of foreign body ingestion or aspiration should be carefully inspected if the retained swab is not found in the endoscopic evaluation.12
Epistaxis
Epistaxis is one of the most common adverse events associated with nasopharyngeal COVID-19 testing. A total of sixteen cases of epistaxis were reported as a result of nasopharyngeal swab.3,12,17,24,28,32 Highly vascular nasal mucosa is prone to mechanical trauma by the swab and bleeding, especially in the circumstances of an inflamed upper respiratory tract in COVID-19 patients, an elderly person who takes anticoagulation medications, or a person with intranasal anatomical variations including septal deviations.3,12 Most of the cases were self-limiting or could be managed with nasal packing.3,12,17 However, potentially life threatening bleeds were also reported and additional procedures including bipolar coagulation, artery ligation, and embolization were required for proper hemostasis.24 The anatomical area of epistaxis often determines the progress because most cases of anterior bleed could be easily managed with firm external nasal pressure; however, posterior bleeds frequently require endoscopic cauterization and packing.3,17,24 Clinicians should remember to screen risk factors, check the more comfortable side during nasal breathing prior to the procedure, and avoid forceful insertion in the presence of any resistance.3,17 In the presence of high-risk factors for bleeding, less invasive evaluation should be considered instead of performing a nasopharyngeal swab.12
CSF leakage
The CSF leakage resulting from iatrogenic skull base damage is a potentially fatal adverse event. It is commonly thought to be rare, but severe cases have been reportedly related to nasopharyngeal COVID-19 testing.11,15,22,23,28,29,30,33,34,36 Traumatic CSF leakage after nasopharyngeal COVID-19 testing is usually manifested as unilateral clear rhinorrhea, persistent headache, or salty or metallic taste postnasal drip within 48 hours after the procedure.11,22,29,30,33,34,36 The amount of rhinorrhea tends to increase with bending forward and Valsalva maneuver.11,22,29,30 The majority of CSF leakage originated from damage in the cribriform plate (Fig. 1A),15,22,23,28,29,33,34,36 and sometimes the sphenoid area.11,30 A beta-2-transferrin assay with the sample of rhinorrhea can confirm the diagnosis of CSF leakage.11,15,22,28,30,33,34 A beta-2-transferrin assay is a sensitive and specific diagnostic tool for CSF leakage because it is only found in CSF, perilymph, and vitreous humor.22 Computed tomography and/or magnetic resonance imaging are required to locate traumatic damage or sometimes pre-existing skull base defects with encephalocele29,30,34 or meningocele.22 Patients who show CSF leakage should remain on strict bed rest, maintain head elevation to 30 degrees, and avoid blowing their nose, coughing, and performing strenuous exercise.22 CSF leakage can be treated with endoscopic surgical repair in most cases, but further management, including systemic antibiotics and corticosteroids, is required when meningitis is complicated.3,12,15,22 Clinicians should check for a history of septal deviations, pre-existing skull base defects, previous sinus or trans-sphenoidal pituitary surgery, and other possible concerns for a skull base injury before testing.3,11,34 After confirmation of the high-risk factors, alternative examinations such as modified nasopharyngeal swab through the trans-oral way or saliva swab should be considered to prevent potentially lethal complications.3,34,42,43 Clinicians should be educated about appropriate angles and depths of swab insertion before nasopharyngeal COVID-19 testing for safe procedures.
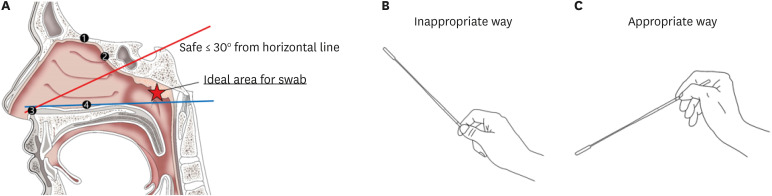
Fig. 1. Basic (A) anatomical and (B, C) procedural background information for a safe nasopharyngeal swab. (A) The blue horizontal line starts from the anterior nasal spine and ends on the external auditory canal. Nasopharyngeal swabs should be performed within 30° from the blue to redline. Clinicians should be cautious not to (B) hold the swab inappropriately and are recommended to (C) grip the swab appropriately. (B) The inappropriate way to hold the swab causes difficulty to enter the safety zone within 30° after passing the anterior nasal spine.
1: cribriform plate; 2: anterior wall of sphenoid sinus; 3: anterior nasal spine; 4: nasal floor.
Reproduced from the article of Mistry et al. (2021).45
Other complications
The nasal septal or pharyngeal abscess could be due to nasopharyngeal COVID-19 testing.3,12,18,19,25 The infectious state could comorbid with cellulitis,19 mastoiditis, osteitis, and even aggravate to sepsis.25 The treatment methods were incision and drainage17 and administration of systemic antibiotics.19,25 A single case of ethmoidal silent sinus syndrome was also documented after nasopharyngeal swab.31 Silent sinus syndrome is manifested as orbital floor depression, enophthalmos, hypoglobus, enlargement of middle nasal meatus, and facial asymmetry due to maxillary sinus atelectasis as a result of chronic obstruction of the sinus drainage.31 The traumatic etiology of silent sinus has been rarely documented.31,44
PROCEDURAL REFERENCES FOR SAFE NASOPHARYNGEAL SWAB
Anatomy
Sufficient orientation or simple reminders of the anatomical background related to the procedure is expected to lower the possibility of adverse events demonstrated in the previous section. The important anatomical landmarks to remember are cribriform plate, anterior wall of the sphenoid sinus, anterior nasal spine, and nasal floor (Fig. 1A).45 The angle of nasopharyngeal swab insertion into the nasal passage should be within 30°, a safe angle, from the nasal floor for safe testing (Fig. 1A). Upward swab insertion with angles greater than 30° not only results in inadequate sample collection but also can damage the skull base, including the cribriform plate and sphenoid, which can lead to CSF leakage.3,12,45 Clinicians could predict the horizontal plane of the nasal floor and full depth of insertion by the line and length between the nostril and the external ear canal, respectively.45 Clinicians need to hold the swab in an appropriate way for safe insertion just above the nasal floor, which requires delicate pressing in the lower direction (Fig. 1B and C).
History taking and preparation for examination
Past or current medical history should be thoroughly investigated to avoid a preventable high-risk adverse event. The cautious medical history includes recent nasal trauma, surgery, significant septal deviation, chronic obstruction of the nasal passage, known skull base defects with or without encephalocele or meningocele, idiopathic intracranial hypertension, and severe coagulopathy.3,12,45,46
Strict adherence to the respiratory and contact precautions, recommended by the Centers for Disease Control and Prevention (CDC), during the wearing of personal protective equipment (PPE) including a gown, gloves, a qualified respirator, and a face shield is essential.46 All personal items and jewelry should be removed before testing.47 First, clinicians should wear a protective gown and wash their hands. The next steps are putting on non-sterile gloves and a respirator with a grading of N95 or higher. Finally, the equipment of a face shield is followed for face and eye protection.46,47
Procedure
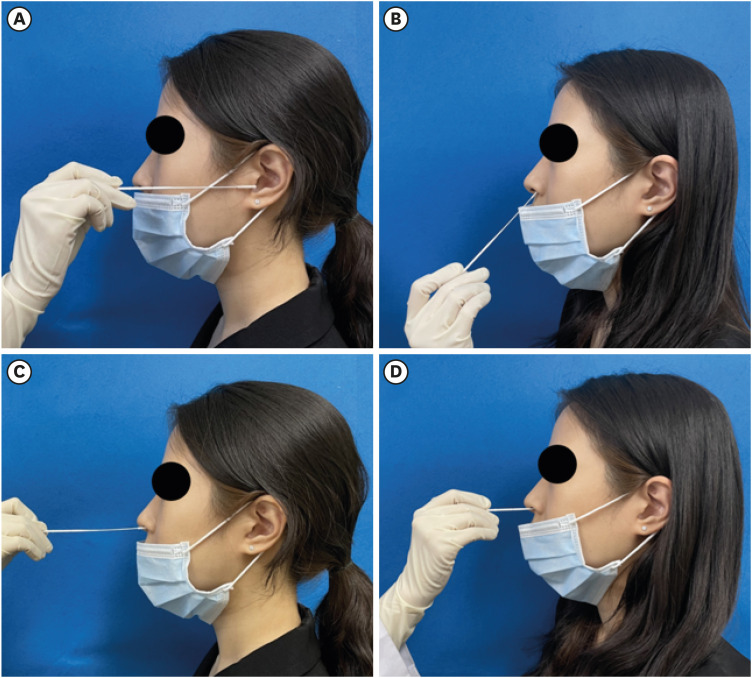
Clinicians are recommended to ask their patients to take off their face masks and blow their nose to clear possible secretions that hinder effective swab insertion.46 Tilting the head slightly backward has been recommended in some studies for a more accessible nasal passage30,46 but a safe and effective approach of nasopharyngeal swab does not seem to be significantly related to head extension.45 Moreover, a head extension exposes the skull base to trauma if the clinician incorrectly performs the procedure.45 Therefore, the recommended procedural steps start from requesting patients to gaze forward with the head positioned on a horizontal plane parallel to the floor.47 Clinicians can predict the full depth of swab insertion by measuring the length between the nostril and the external ear canal (Fig. 2A). It is more ideal if the patient is comfortably seated with the back of their head against the headrest.47,48 Second, the swab is appropriately held (Fig. 1B and C) and inserted into the nostril 2 to 3 cm parallel to the nasal bridge until it reaches the anterior nasal spine (Fig. 2B). Raise the hand that holds the swab approximately 70° upward at the same position and gently insert the swab along the nasal septum just above the nasal floor to the target area, nasopharynx, considering the anatomical structures of the nasal cavity and its surroundings (Fig. 2C).24,45,46,47,48 The swab should be kept on the nasopharynx for several seconds and gently pulled back while rotating it within fingers (Fig. 2D).46,47,48 Forceful movement should be attempted, especially in patients at a high risk of possible complications.24
Fig. 2. The ideal procedural steps to obtain a nasopharyngeal swab specimen for coronavirus disease 2019 testing. (A) Before testing, the clinician can predict the full depth of insertion by measuring the length between the nostril and the external ear canal. (B) Insert the swab into the nostril no more than 3 cm parallel to the nasal bridge until reaching the anterior nasal spine. After passing the anterior nasal spine, (C) raise the hand that holds the swab about 70° upward and (D) delicately insert the swab along the nasal septum just above the nasal floor to the target area, nasopharynx. The swab should be stayed on the target area for several seconds and gently pull back the swab while rotating it within fingers, not making big circles with entire hands, to avoid excessive irritation (The pictures were demonstrated by the authors, Moon JW and Chae S with full agreement for publication).
Handling of the specimen and undressing step
Samples collected on nasopharyngeal swabs were moved to collection tubes by breaking the swab at the groove. Sealed state and labeling should be checked, and surface disinfection should be performed.46,48 Taking off PPE is recommended to be observed by other personnel, if possible, to lower the possible risk of contamination.46 The first step is to remove the gown and gloves, followed by cleansing hands with decontaminating agents, including alcohol-based solutions. Second, new gloves are worn, and the face shield is removed. Third, we put on another pair of new gloves and remove the respirator. Finally, the gloves are removed, and hands are re-washed using decontaminating agents.46
CONCLUSIONS
Our study reviewed the literature on possible complications and recommended procedural references for nasopharyngeal COVID-19 testing. Systemic education regarding high-risk factors and nasopharyngeal anatomical structures is expected to lower the incidence of adverse events. Nasopharyngeal swabs have been regarded as a safe and reliable screening tool for COVID-193,48; however, it is essential to have sufficient anatomical and clinical knowledge for not only accurate examination to minimize the virus spread, but also to protect patients from preventable but often underestimated risks.
Footnotes
Funding: This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF), funded by the Korean Ministry of Science and ICT (MSIT) (grant No. 2020R1F1A1077244).
Disclosure: All authors have no potential conflicts of interest to disclose.
- Conceptualization: Rhyu IJ.
- Data curation: Rhyu IJ, Kim DH.
- Formal analysis: Rhyu IJ, Kim D.
- Funding acquisition: Rhyu IJ.
- Investigation: Kim DH, Kim D, Moon JW.
- Methodology: Rhyu IJ, Chae S, Kim DH.
- Validation: Rhyu IJ, Chae S, Kim DH.
- Visualization: Chae S, Moon JW.
- Writing - original draft: Kim DH.
- Writing - review & editing: Rhyu IJ, Chae S.
References
- 1.Korea Disease Control and Prevention Agency (KDCA) COVID-19 vaccination and domestic outbreak status (as of 00:00 am, Feb 20, 2022) [Updated February 20, 2022]. [Accessed February 20, 2022]. http://ncov.mohw.go.kr/tcmBoardView.do?brdId=3&brdGubun=31&dataGubun=&ncvContSeq=6406&contSeq=6406&board_id=312&gubun=ALL .
- 2.Centers for Disease Control and Prevention (CDC) United States COVID-19 Cases, Deaths, and Laboratory Testing (NAATs) by State, Territory, and Jurisdiction. [Updated February 19, 2022]. [Accessed February 19, 2022]. https://covid.cdc.gov/covid-data-tracker/#cases_tests30day .
- 3.Clark JH, Pang S, Naclerio RM, Kashima M. Complications of nasal SARS-CoV-2 testing: a review. J Investig Med. 2021;69(8):1399–1403. doi: 10.1136/jim-2021-001962. [DOI] [PubMed] [Google Scholar]
- 4.Liu R, Han H, Liu F, Lv Z, Wu K, Liu Y, et al. Positive rate of RT-PCR detection of SARS-CoV-2 infection in 4880 cases from one hospital in Wuhan, China, from Jan to Feb 2020. Clin Chim Acta. 2020;505:172–175. doi: 10.1016/j.cca.2020.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Okoye GA, Kamara HI, Strobeck M, Mellman TA, Kwagyan J, Sullivan A, et al. Diagnostic accuracy of a rapid diagnostic test for the early detection of COVID-19. J Clin Virol. 2022;147:105023. doi: 10.1016/j.jcv.2021.105023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wölfl-Duchek M, Bergmann F, Jorda A, Weber M, Müller M, Seitz T, et al. Sensitivity and specificity of SARS-CoV-2 rapid antigen detection tests using oral, anterior nasal, and nasopharyngeal swabs: a diagnostic accuracy study. Microbiol Spectr. 2022;10(1):e0202921. doi: 10.1128/spectrum.02029-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barton RT. Q-tip otalgia. JAMA. 1972;220(12):1619. [PubMed] [Google Scholar]
- 8.Smith M, Darrat I, Seidman M. Otologic complications of cotton swab use: one institution’s experience. Laryngoscope. 2012;122(2):409–411. doi: 10.1002/lary.22437. [DOI] [PubMed] [Google Scholar]
- 9.Bwire GM, Majigo MV, Njiro BJ, Mawazo A. Detection profile of SARS-CoV-2 using RT-PCR in different types of clinical specimens: a systematic review and meta-analysis. J Med Virol. 2021;93(2):719–725. doi: 10.1002/jmv.26349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee RA, Herigon JC, Benedetti A, Pollock NR, Denkinger CM. Performance of saliva, oropharyngeal swabs, and nasal swabs for SARS-CoV-2 molecular detection: a systematic review and meta-analysis. J Clin Microbiol. 2021;59(5):e02881-20. doi: 10.1128/JCM.02881-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Agamawi YM, Namin A, Ducic Y. Cerebrospinal fluid leak from COVID-19 swab. OTO Open. 2021;5(4):2473974X211059104. doi: 10.1177/2473974X211059104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hakimi AA, Goshtasbi K, Kuan EC. Complications associated with nasopharyngeal COVID-19 testing: an analysis of the MAUDE database and literature review. Am J Rhinol Allergy. 2022;36(2):281–284. doi: 10.1177/19458924211046725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Forbes. Can painful complications arise after a Covid-19 nasal swab test? [Updated February 14, 2022]. [Accessed February 15, 2022]. https://www.forbes.com/sites/anuradhavaranasi/2021/04/29/can-painful-complications-arise-after-a-covid-19-nasal-swab-test/?sh=7574e69f2e49 .
- 14.The New York Times. Must this swab go that far up your nose to test for Covid? [Updated November 25, 2021]. [Accessed February 15, 2022]. https://www.nytimes.com/2021/11/18/world/swab-test-covid.html .
- 15.Alberola-Amores FJ, Valdeolivas-Urbelz E, Torregrosa-Ortiz M, Álvarez-Sauco M, Alom-Poveda J. Meningitis due to cerebrospinal fluid leak after nasal swab testing for COVID-19. Eur J Neurol. 2021;28(11):e91–e92. doi: 10.1111/ene.14736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.De Luca L, Maltoni S. Is naso-pharyngeal swab always safe for SARS-CoV-2 testing? An unusual, accidental foreign body swallowing. Clin J Gastroenterol. 2021;14(1):44–47. doi: 10.1007/s12328-020-01236-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fabbris C, Cestaro W, Menegaldo A, Spinato G, Frezza D, Vijendren A, et al. Is oro/nasopharyngeal swab for SARS-CoV-2 detection a safe procedure? Complications observed among a case series of 4876 consecutive swabs. Am J Otolaryngol. 2021;42(1):102758. doi: 10.1016/j.amjoto.2020.102758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Farina DA, Nelson KK. How deep is too deep? Gastrointestinal complication of COVID-19 deep nasal swab testing. Endosc Int Open. 2021;9(11):E1841–E1842. doi: 10.1055/a-1578-2273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fazekas B, Fazekas B, Darraj E, Jayakumar D. Preseptal cellulitis and infraorbital abscess as a complication of a routine COVID-19 swab. BMJ Case Rep. 2021;14(5):e241963. doi: 10.1136/bcr-2021-241963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Föh B, Borsche M, Balck A, Taube S, Rupp J, Klein C, et al. Complications of nasal and pharyngeal swabs: a relevant challenge of the COVID-19 pandemic? Eur Respir J. 2021;57(4):2004004. doi: 10.1183/13993003.04004-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gaffuri M, Capaccio P, Torretta S, Daga M, Zuccotti GV, Pignataro L. An unusual retained choanal foreign body: a possible complication of COVID-19 testing with nasopharyngeal swab. Ear Nose Throat J. 2021 doi: 10.1177/0145561321993933. Forthcoming. [DOI] [PubMed] [Google Scholar]
- 22.Holmes A, Allen B. Case report: an intracranial complication of COVID-19 nasopharyngeal swab. Clin Pract Cases Emerg Med. 2021;5(3):341–344. doi: 10.5811/cpcem.2021.5.52232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Knížek Z, Michálek R, Vodicka J, Zdobinská P. Cribriform plate injury after nasal swab testing for COVID-19. JAMA Otolaryngol Head Neck Surg. 2021;147(10):915–917. doi: 10.1001/jamaoto.2021.2216. [DOI] [PubMed] [Google Scholar]
- 24.Koskinen A, Tolvi M, Jauhiainen M, Kekäläinen E, Laulajainen-Hongisto A, Lamminmäki S. Complications of COVID-19 nasopharyngeal swab test. JAMA Otolaryngol Head Neck Surg. 2021;147(7):672–674. doi: 10.1001/jamaoto.2021.0715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lapeyre M, Coupez E, Ghelis N, Dupuis C. Pharyngeal abscess: a rare complication of repeated nasopharyngeal swabs. Intensive Care Med. 2021;47(5):612–613. doi: 10.1007/s00134-021-06358-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Molnár D, Zsigmond F, Helfferich F. Safety precautions for self-performed severe acute respiratory syndrome coronavirus 2 tests: a case of a swallowed swab. Cureus. 2021;13(5):e15297. doi: 10.7759/cureus.15297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mughal Z, Luff E, Okonkwo O, Hall CE. Test, test, test - a complication of testing for coronavirus disease 2019 with nasal swabs. J Laryngol Otol. 2020;134(7):646–649. doi: 10.1017/S0022215120001425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ovenden C, Bulshara V, Patel S, Vsykocil E, Valentine R, Psaltis A, et al. COVID-19 nasopharyngeal swab causing a traumatic cerebrospinal fluid leak. ANZ J Surg. 2021;91(5):1021–1022. doi: 10.1111/ans.16910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Paquin R, Ryan L, Vale FL, Rutkowski M, Byrd JK. CSF leak after COVID-19 nasopharyngeal swab: a case report. Laryngoscope. 2021;131(9):1927–1929. doi: 10.1002/lary.29462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rajah J, Lee J. CSF rhinorrhoea post COVID-19 swab: a case report and review of literature. J Clin Neurosci. 2021;86:6–9. doi: 10.1016/j.jocn.2021.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ribeiro SP, Loureiro RM, Gil JM, Dutra DL, Gomes RL, Daniel MM. Ethmoidal silent sinus syndrome after nasal swab test. Neuroradiology. 2022;64(1):205–207. doi: 10.1007/s00234-021-02856-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rigante M, Picciotti PM, Parrilla C. A nasal complication of nasopharyngeal swab for reverse transcription polymerase chain reaction (RT-PCR) detection of SARS-CoV-2 mRNA. Cureus. 2021;13(7):e16183. doi: 10.7759/cureus.16183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Samadian M, Maroufi SF, Taheri MS, Jafari A. CSF rhinorrhea after nasopharyngeal swab testing for COVID-19: a case report and review of literature. Otolaryngol Case Rep. 2021;21:100370. doi: 10.1016/j.xocr.2021.100370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sullivan CB, Schwalje AT, Jensen M, Li L, Dlouhy BJ, Greenlee JD, et al. Cerebrospinal fluid leak after nasal swab testing for coronavirus disease 2019. JAMA Otolaryngol Head Neck Surg. 2020;146(12):1179–1181. doi: 10.1001/jamaoto.2020.3579. [DOI] [PubMed] [Google Scholar]
- 35.Tümer M, Ardıçlı B. A fractured nasopharyngeal swab in the duodenum of a toddler: an unusual complication of preoperative COVID-19 testing. Can J Anaesth. 2021;68(9):1450–1451. doi: 10.1007/s12630-021-01995-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yılmaz M, Bahadır Z, Madendere B, Yüksel RT, Gökay H, Yiğitbaşı AA. A brief report: cerebrospinal fluid rhinorrhea after repetitive nasal swab testing for coronavirus disease 2019(COVID-19) Otolaryngol Case Rep. 2021;20:100313. doi: 10.1016/j.xocr.2021.100313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cheong HS, Kwon KT, Hwang S, Kim SW, Chang HH, Park SY, et al. Workload of healthcare workers during the COVID-19 outbreak in Korea: a nationwide survey. J Korean Med Sci. 2022;37(6):e49. doi: 10.3346/jkms.2022.37.e49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee HA, Ahn MH, Byun S, Lee HK, Kweon YS, Chung S, et al. How COVID-19 affected healthcare workers in the hospital locked down due to early COVID-19 cases in Korea. J Korean Med Sci. 2021;36(47):e325. doi: 10.3346/jkms.2021.36.e325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li L, Shim T, Zapanta PE. Optimization of COVID-19 testing accuracy with nasal anatomy education. Am J Otolaryngol. 2021;42(1):102777. doi: 10.1016/j.amjoto.2020.102777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.May J, Mason K, Patel P, Madden B. A challenging case of tracheal foreign body retrieval following COVID-19 swabbing. Monaldi Arch Chest Dis. 2021 doi: 10.4081/monaldi.2021.2014. Forthcoming. [DOI] [PubMed] [Google Scholar]
- 41.Roque M, Proudfoot K, Mathys V, Yu S, Krieger N, Gernon T, et al. A review of nasopharyngeal swab and saliva tests for SARS-CoV-2 infection: disease timelines, relative sensitivities, and test optimization. J Surg Oncol. 2021;124(4):465–475. doi: 10.1002/jso.26561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Butler-Laporte G, Lawandi A, Schiller I, Yao M, Dendukuri N, McDonald EG, et al. Comparison of saliva and nasopharyngeal swab nucleic acid amplification testing for detection of SARS-CoV-2: a systematic review and meta-analysis. JAMA Intern Med. 2021;181(3):353–360. doi: 10.1001/jamainternmed.2020.8876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Matti E, Lizzio R, Spinozzi G, Ugolini S, Maiorano E, Benazzo M, et al. An alternative way to perform diagnostic nasopharyngeal swab for SARS-CoV-2 infection. Am J Otolaryngol. 2021;42(2):102828. doi: 10.1016/j.amjoto.2020.102828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Février E, Vandersteen C, Castillo L, Savoldelli C. Silent sinus syndrome: a traumatic case. J Stomatol Oral Maxillofac Surg. 2017;118(3):187–190. doi: 10.1016/j.jormas.2017.04.004. [DOI] [PubMed] [Google Scholar]
- 45.Mistry SG, Walker W, Earnshaw J, Cervin A. COVID-19 swab-related skull base injury. Med J Aust. 2021;214(10):457–459.e1. doi: 10.5694/mja2.51082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Marty FM, Chen K, Verrill KA. How to obtain a nasopharyngeal swab specimen. N Engl J Med. 2020;382(22):e76. doi: 10.1056/NEJMvcm2010260. [DOI] [PubMed] [Google Scholar]
- 47.Di Maio P, Iocca O, Cavallero A, Giudice M. Performing the nasopharyngeal and oropharyngeal swab for 2019-novel coronavirus (SARS-CoV-2) safely: How to dress, undress, and technical notes. Head Neck. 2020;42(7):1548–1551. doi: 10.1002/hed.26230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Petruzzi G, De Virgilio A, Pichi B, Mazzola F, Zocchi J, Mercante G, et al. COVID-19: nasal and oropharyngeal swab. Head Neck. 2020;42(6):1303–1304. doi: 10.1002/hed.26212. [DOI] [PMC free article] [PubMed] [Google Scholar]