Introduction
Scalp dysesthesia (burning scalp syndrome) is characterized by abnormal sensations of the scalp such as burning, tingling, and pruritus in the absence of objective skin findings.1 Several underlying brain disorders present with dysesthesia, most commonly as neuropathic itch. This type of itch has been described in several neurologic conditions, including stroke, tumors, vascular malformations, demyelinating disease, and radicular compression.2 To date, no cases of localized scalp dysesthesia related to a meningioma have been described. We present a unique case of a patient with scalp dysesthesia related to a left frontal meningioma.
Case report
A 71-year-old woman presented to dermatology with a several-month history of constant 8/10 scalp pruritus, without trichodynia (painful scalp), primarily localized to the right frontal aspect of the scalp. The itch was worse at night. No primary skin changes were found on physical examination. Since there were no cutaneous findings, she was diagnosed with scalp dysesthesia and was started on oral gabapentin 200 mg twice a day without topical medication. Her scalp symptoms improved minimally with this regimen.
Concomitantly, she was seen by her primary care doctor for worsening forgetfulness and imbalance. She was subsequently evaluated by neurology, who noted a 2-year history of progressive decline in memory, cognition, and motor function. She had no history of stroke or major head injury and no family history of dementia of the Alzheimer type, Parkinson disease, or other central nervous system disorders. She was diagnosed with short-term memory loss and bradykinesia. Her neurologic examination was otherwise normal. She was referred for diagnostic testing and imaging to assist in the differential diagnosis and was started on donepezil.
Brain magnetic resonance imaging showed a 6.7 × 4.5 × 4.5-cm durally based mass in the left frontal region causing a significant mass effect on right frontal lobe (Figs 1 and 2). This caused significant brain compression with vasogenic edema surrounding the mass and was suggestive of a meningioma. She immediately underwent craniotomy and tumor debulking. Histology confirmed a meningioma.
Fig 1.
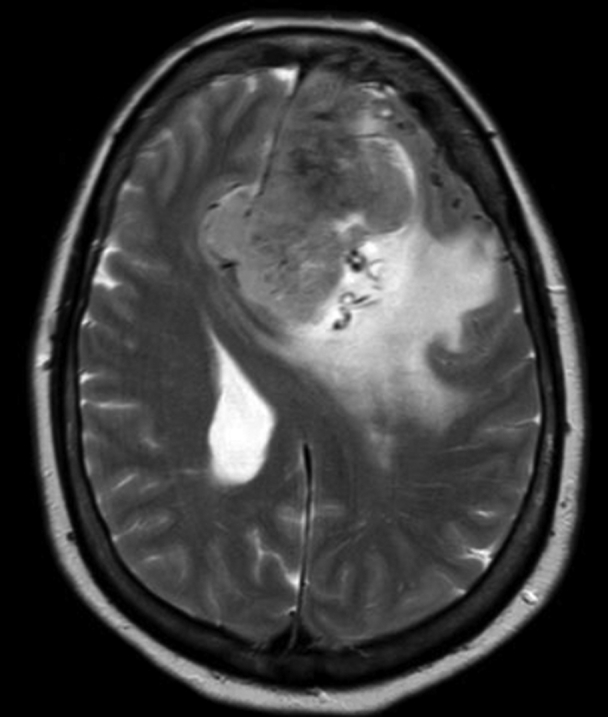
Magnetic resonance imaging of the brain without contrast. Axial view demonstrating a 6.7 × 4.5 × 4.5-cm hypervascular, extraaxial mass in the left front region crossing over the falx and causing a left-midline shift.
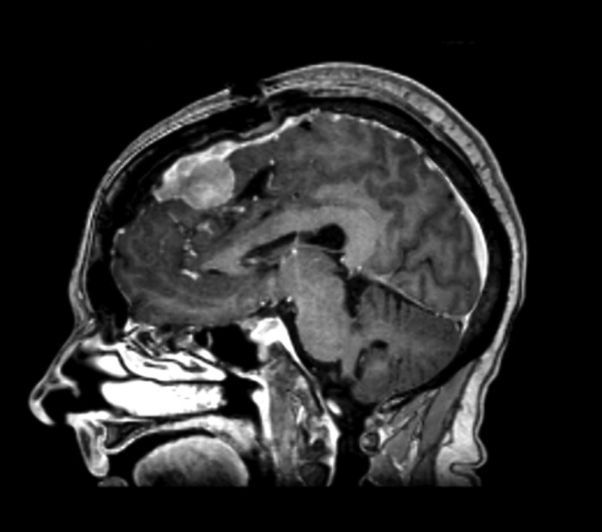
Fig 2.
Magnetic resonance imaging of the brain without contrast. Sagittal view demonstrating a large hypervascular mass in the frontal lobe.
Three days after the operation, the patient’s gabapentin was discontinued. Two weeks post-surgery, the patient’s symptoms of scalp dysesthesia completely resolved. Brain magnetic resonance imaging showed significant improvement of the left-right midline shift and a residual small right-sided meningioma. One year later, her symptoms of scalp dysesthesia recurred, again localized to the right frontal aspect of the scalp. Brain magnetic resonance imaging showed an increase in the size of the residual right falcine meningioma, now measuring 4.6 × 2.6 × 2.6 cm.
Discussion
Scalp dysesthesia was first described by Hoss and Segal in 1998 and was reported in the setting of psychiatric disorders.1 In 2013, a limited retrospective review of patients with scalp dysesthesia found a strong association with cervical spine disease. The authors hypothesized that the symptoms were secondary to chronic muscle tension placed on the pericranial muscles and scalp aponeurosis, but the true etiology remains unknown.3
Scalp dysesthesia has been described as secondary to a number of neurologic disorders, including brain tumors. Meningioma is the most common primary central nervous system tumor, with an overall incidence of 7.8/100,000.4 Many meningiomas are asymptomatic or minimally symptomatic, leading to difficulty and delay in diagnosis. Common symptoms include seizures, visual changes, anosmia, headaches, auditory changes, weakness, cognitive and behavioral deficits, aphasia, and mental status changes.5 In previous case reports, patients with meningiomas associated with the trigeminal nerve have presented with dysesthesia of the eye, orbit, and upper portion of the face, while patients with foramen-magnum meningiomas have presented with pruritus of the arm and hand.
In our case, the patient presented with unusual focal scalp dysesthesia likely related to a frontal lobe meningioma. This is supported by the resolution of scalp symptoms following surgical debulking and subsequent recurrence of her scalp symptoms with growth of the frontal meningioma. The right focal nature of her symptoms could be attributed to the significant mass effect and right-sided meningioma. Meningiomas are tumors of the meninges, which have sensory innervation, primarily through the meningeal branches of the trigeminal and vagus nerves, as well as a small component of the upper cervical spinal nerves.6 The associated symptoms of scalp dysesthesia may be related to the shared innervation of the scalp and meninges via the trigeminal nerve.7
To our knowledge, this is the first published case of localized scalp pruritus and dysesthesia associated with meningioma. Many asymptomatic or mildly symptomatic meningiomas go undiagnosed,8 though they are the most common primary central nervous system tumor. This case demonstrates that focal refractory scalp dysesthesia is another useful symptom in the setting of other neurologic findings that can be associated with meningiomas. Physicians should consider referral to neurology when scalp dysesthesia is focal, refractory, and found in combination with other neurologic symptoms.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.Hoss D., Segal S. Scalp dysesthesia. Arch Dermatol. 1998;134(3):327–330. doi: 10.1001/archderm.134.3.327. [DOI] [PubMed] [Google Scholar]
- 2.Oaklander A.L. Neuropathic itch. Semin Cutan Med Surg. 2011;30(2):87–92. doi: 10.1016/j.sder.2011.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thornsberry L.A., English J.C., 3rd Scalp dysesthesia related to cervical spine disease. JAMA Dermatol. 2013;149(2):200–203. doi: 10.1001/jamadermatol.2013.914. [DOI] [PubMed] [Google Scholar]
- 4.Baldi I., Engelhardt J., Bonnet C., et al. Epidemiology of meningiomas. Neurochirurgie. 2018;64(1):5–14. doi: 10.1016/j.neuchi.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 5.Wu A., Garcia M.A., Magill S.T., et al. Presenting symptoms and prognostic factors for symptomatic outcomes following resection of meningioma. World Neurosurg. 2018;111:e149–e159. doi: 10.1016/j.wneu.2017.12.012. [DOI] [PubMed] [Google Scholar]
- 6.Moore K., Daley A., Agur A. 7th ed. Lippincott Williams & Wilkins; Philadelphia: 2013. Moore Clinically Oriented Anatomy; pp. 701–703. [Google Scholar]
- 7.Kemp W.J., 3rd, Tubbs R.S., Cohen-Gadol A.A. The innervation of the scalp: a comprehensive review including anatomy, pathology, and neurosurgical correlates. Surg Neurol Int. 2011;2:178. doi: 10.4103/2152-7806.90699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Radhakrishnan K., Mokri B., Parisi J.E., O'Fallon W.M., Sunku J., Kurland L.T. The trends in incidence of primary brain tumors in the population of Rochester, Minnesota. Ann Neurol. 1995;37(1):67–73. doi: 10.1002/ana.410370113. [DOI] [PubMed] [Google Scholar]