Abstract
The susceptibilities of Streptococcus pneumoniae (1,476 strains) and untypeable Haemophilus influenzae (1,676 strains) to various oral β-lactam, macrolide-azalide, and fluoroquinolone antimicrobial agents were determined by broth microdilution. Organisms were isolated from specimens obtained from outpatients in six geographic regions of the United States. MIC data were interpreted according to pharmacodynamically derived breakpoints applicable to the oral agents tested. Among H. influenzae strains, 41.6% were β-lactamase positive. Virtually all H. influenzae strains were susceptible to amoxicillin-clavulanate (98%), cefixime (100%), and ciprofloxacin (100%), while 78% were susceptible to cefuroxime, 57% were susceptible to amoxicillin, 14% were susceptible to cefprozil, 9% were susceptible to loracarbef, 2% were susceptible to cefaclor, and 0% were susceptible to azithromycin and clarithromycin. Among S. pneumoniae isolates, 49.6% were penicillin susceptible, 17.9% were intermediate, and 32.5% were penicillin resistant, with penicillin MICs for 50 and 90% of the isolates tested of 0.12 and 4 μg/ml, respectively. Overall, 94% of S. pneumoniae isolates were susceptible to amoxicillin and amoxicillin-clavulanate, 69% were susceptible to azithromycin and clarithromycin, 63% were susceptible to cefprozil and cefuroxime, 52% were susceptible to cefixime, 22% were susceptible to cefaclor, and 11% were susceptible to loracarbef. Although ciprofloxacin has marginal activity against S. pneumoniae, no high-level fluoroquinolone-resistant strains were found. Significant cross-resistance was found between penicillin and macrolides-azalides among S. pneumoniae isolates, with 5% of the penicillin-susceptible strains being macrolide-azalide resistant, compared with 37% of the intermediate isolates and 66% of the resistant isolates. Resistance was highest in S. pneumoniae isolates from patients younger than 10 years of age, middle ear and paranasal sinus specimens, and the southern half of the United States. With the continuing rise in resistance, judicious use of oral antimicrobial agents is necessary in all age groups.
The ubiquitous pathogens Streptococcus pneumoniae and Haemophilus influenzae cause a wide spectrum of pediatric and adult infections, including acute otitis media, sinusitis, acute exacerbations of chronic bronchitis, pneumonia, bacteremia, and meningitis. The advent and widespread use of the protein-conjugated type b capsular polysaccharide H. influenzae vaccine has largely eliminated the risk of life-threatening infections due to encapsulated type b strains (5), but localized infections caused by nonencapsulated H. influenzae strains remain common. Antimicrobial resistance has emerged in both H. influenzae and S. pneumoniae, and effective patient management requires physicians to be aware of the patterns and clinical significance of antibiotic resistance in these pathogens. This knowledge is gained, in large measure, from periodic systematic epidemiological surveillance studies.
β-Lactamase-mediated ampicillin resistance in H. influenzae, which first emerged in the United States in 1974 (26, 41), has evolved into an obstacle to effective treatment with older β-lactams. Its prevalence has risen steadily, from 16% in 1986 (14) to 33% in 1993 (33) and 36% in 1994 and 1995 (25). Notably, the highest frequency of β-lactamase production—45.8%—has been documented in children aged younger than 5 years, the same patient population that experiences the peak incidence of H. influenzae infection, primarily otitis media (25). Additionally, investigators have shown higher MICs of ampicillin, amoxicillin, cefaclor, loracarbef, and cefprozil for β-lactamase-producing strains (12, 25, 40). Far less common is non-β-lactamase-mediated ampicillin resistance (24). β-Lactamase-negative, ampicillin-resistant strains are thought to possess altered penicillin-binding proteins that have decreased affinity for many β-lactam agents. However, spheroplast-producing strains also appear resistant to ampicillin and other β-lactams as a result of the high osmolality of media which currently are used routinely, but there is no evidence that spheroplast-producing strains are resistant in vivo (24, 34, 39).
Antibiotic-resistant strains of S. pneumoniae have been reported on all continents in the 2 decades since resistant pneumococcal strains were identified in the United States (23). In some regions, drug-resistant S. pneumoniae strains predominate, with numerous strains resistant to multiple agents (23, 40). Changes in the affinity of penicillin-binding proteins, which is chromosomally mediated, result in β-lactam resistance. Penicillin-resistant strains (penicillin MICs of ≥2 μg/ml) are common in France, Spain, Romania, Japan, Korea, and Taiwan and are being identified with increasing frequency in the United States (23). Early in this decade, clinical failure of treatment for patients with meningitis led to the detection of S. pneumoniae strains highly resistant to expanded-spectrum cephalosporins (6, 38). The MICs of these cephalosporins exceeded those of penicillin, in contrast to previous experience, which showed the MICs of these cephalosporins to be 1 to 2 doubling dilutions lower than that of penicillin.
Current clinical practice generally involves treating community-acquired respiratory tract infections empirically. In 1997, over 130 million courses of antibiotics were prescribed for outpatient treatment of such infections (including pharyngitis), with almost 90 million courses being for adults and almost 42 million being for children (31). Twenty-one million antibiotic prescriptions were issued for otitis media in children. As empiric antibiotics should be active against both S. pneumoniae and H. influenzae for respiratory tract infections other than pharyngitis, periodic surveillance of respiratory tract isolates for changes in the susceptibility patterns of these pathogens is therefore essential to the effective management of community-acquired S. pneumoniae and H. influenzae infections (17, 20). Accordingly, the present study sought to characterize current levels of resistance in S. pneumoniae and H. influenzae to 10 oral antimicrobial agents by evaluating the susceptibility of isolates from outpatients with community-acquired infections in the United States.
As current susceptibility breakpoints for many oral antimicrobial agents no longer correspond to more recent clinical, microbiological, pharmacokinetic, and investigational experience (8–11), investigators have proposed a new approach based on pharmacokinetic-pharmacodynamic (PK/PD) modeling and on clinical studies that have measured bacteriologic outcome and evaluated this in relation to drug susceptibilities (7, 9, 11, 18, 19). The activity of β-lactams and macrolides has been shown to depend on the time the drug concentration in serum exceeds the MIC of the agent, with clinical success occurring in more than 80% of the cases in which the concentration of the agent exceeds the MIC for an infecting strain for more than 40 to 50% of the dosing interval (8). Using standard dosing regimens and the serum pharmacokinetics of these agents, the concentrations in serum that are maintained for at least 40 to 50% of the dosing interval can be determined and used as PK/PD breakpoints. Different PK/PD parameters correlate with clinical outcome with fluoroquinolones and with azalides such as azithromycin, and breakpoints can be derived from one of two ratios—the ratio of the peak concentration in serum to the MIC or the ratio of the area under the 24-h serum concentration-time curve (AUC) to the MIC (8, 29). Clinical cure correlates best when the AUC/MIC ratio exceeds 25 for these agents in immunocompetent-animal models (8), and MIC breakpoints for susceptibility can therefore be derived from the formula AUC/25.
MATERIALS AND METHODS
Study centers.
Between January and December 1997, strains of H. influenzae and S. pneumoniae isolated from outpatients were collected by eight large regional commercial laboratories from upper and lower respiratory tract sources and other sources such as blood. Patients whose samples were submitted lived in communities representative of six major regions of the United States. Isolates from hospitalized patients, duplicate patient isolates, and isolates referred by other laboratories were excluded. After isolation by the commercial laboratories, strains were frozen at −70°C and transported to reference laboratories at Case Western Reserve University, Cleveland, Ohio (M.R.J.), and the Hershey Medical Center, Hershey, Pa. (P.C.A.). The demographical information submitted for each strain included patient age and gender, specimen collection date, specimen source, and the state and zip code of the submitting physician. The reference laboratories checked the compliance of the isolates with the criteria for inclusion in the study and excluded isolates not meeting these criteria.
Identification of isolates.
The reference laboratories confirmed the identity and purity of every strain. S. pneumoniae isolates were confirmed by inhibition by optochin and positive bile solubility tests. Haemophilus strains were identified by X and V factor requirement and reaction to polyvalent antiserum (Difco Laboratories, Detroit, Mich.), and strains were confirmed as H. influenzae by determination of the requirement for both the X and V factors. Only untypeable or non-type b strains were included in the study.
Susceptibility testing.
The 10 oral antimicrobials tested—amoxicillin, amoxicillin-clavulanate (2:1 ratio), cefaclor, cefixime, cefprozil, cefuroxime, loracarbef, azithromycin, clarithromycin, and ciprofloxacin—were selected to reflect representative current treatment options. Ampicillin was also tested to characterize β-lactamase-negative, ampicillin-resistant strains of H. influenzae. Penicillin was also tested to characterize the penicillin susceptibility of S. pneumoniae, and ceftriaxone was used to characterize strains for which the MICs of this agent are higher than the penicillin MICs. MICs were determined by broth microdilution in accordance with the methods of the National Committee for Clinical Laboratory Standards (NCCLS) (27).
Broth microdilution tests were performed in custom-dried 96-well microdilution trays (Sensititre Division, Accumed International, Westlake, Ohio) in two configurations, one for testing of S. pneumoniae and the other for the testing of H. influenzae. Haemophilus inocula were prepared from chocolate agar plates incubated for a full 24 h by the direct colony suspension method. S. pneumoniae inocula were prepared from blood agar plates incubated for 18 to 20 h, also by direct colony suspension. Growth from these plates was then suspended in tubes of Mueller-Hinton broth (Sensititre) to a density equivalent to a 0.5 McFarland standard. Within 30 min of preparation, 20 μl of a H. influenzae suspension or 200 μl of an S. pneumoniae suspension was added to a 10-ml tube of in-house fresh Haemophilus test medium and Mueller-Hinton broth supplemented with 5% lysed horse blood (Cleveland Scientific, Bath, Ohio). Also within 30 min of preparation, doseheads were placed on the tubes and an autoinoculator (Sensititre) dispensed a 100-μl volume into each well of the Sensititre microdilution trays. The trays were sealed and incubated for 22 to 24 h at 35°C in ambient air, and the lowest drug concentration showing no growth was read as the MIC. Inoculum checks were performed on all isolates by transfer of 10 μl from the Haemophilus test medium or Mueller-Hinton broth–lysed horse blood suspensions into tubes containing 6 ml of saline; after mixing, 100 μl was transferred to a blood or chocolate agar plate and spread over the surface of the plate. Colonies were counted after incubation for 20 to 24 h at 35°C in a 5% CO2 atmosphere; 50 to 120 colonies represented the desired range of 3 × 105 to 7 × 105 CFU/ml, and strains with inocula beyond this range were retested until the inocula were in the correct range. Quality control of MIC testing is detailed below.
H. influenzae isolates were also tested for β-lactamase production by the nitrocefin disk method (Cefinase; Becton Dickinson Laboratories, Sparks, Md.), with positive and negative controls being employed on each day of testing.
Quality control.
Initial quality control assessments included evaluation of the performance characteristics of the Sensitire panels and media used for S. pneumoniae and H. influenzae. Quality control strains specified by the NCCLS, including S. pneumoniae ATCC 49619, H. influenzae ATCC 49247 and 49766, Enterococcus faecalis ATCC 29212, and Escherichia coli ATCC 25922 and 35218, were used (27). Inocula of the nonfastidious strains were prepared as described for S. pneumoniae, except that 50-μl suspension volumes were added to 10-ml tubes of plain Mueller-Hinton broth. MICs for quality control strains were required to fall within NCCLS-specified ranges (28). In addition, a battery of S. pneumoniae and H. influenzae strains for which the MICs are known were tested. The performance characteristics of the Sensititre trays were initially found to be inadequate (data not shown), and this was traced to poor growth properties of the initial Mueller-Hinton–lysed horse blood and Haemophilus test medium broths obtained from Sensititre that were used to rehydrate the trays. Strains were retested by using Mueller-Hinton–lysed horse blood and Haemophilus test medium broths that were freshly prepared in house, and these results showed fully acceptable performance characteristics (data not shown). Consequently, these media were used throughout the study. The Mueller-Hinton–lysed horse blood broth was prepared on the day of testing by adding 1 ml of lysed horse blood to 10 ml of Mueller-Hinton broth (Sensititre). Haemophilus test medium was prepared in accordance with the methods of the NCCLS by using Mueller-Hinton broth base (Difco), 0.5% yeast extract (Difco), 15 μg of NAD per ml, and 15 μg of hematin per ml (Sigma). Haemophilus test medium was prepared in batches and stored at 4°C for use within 2 weeks of preparation (its performance was found to degrade after this time) or stored at −20°C for up to 6 weeks.
After the adequacy of the susceptibility testing materials was confirmed, the relevant quality control strains for each organism were tested on each day of testing and results were accepted only if the MICs for the quality control strains were within specified limits. In addition, at the end of the study, all quality control values were analyzed; this analysis confirmed that modal values for all agents were the same as the modal NCCLS values and that the values from the two testing laboratories were comparable.
Susceptibility interpretation criteria.
MICs were interpreted as indicating susceptible, intermediate, or resistant categories in accordance with NCCLS guidelines (28), where available, and on the basis of PK/PD parameters as well (7, 8, 29). PK/PD breakpoints were based on standard dosing regimens and criteria appropriate to each agent. For β-lactams and clarithromycin, these breakpoints were based on drug concentrations in serum present for 40 to 50% of the dosing interval, while for azithromycin and ciprofloxacin, they were based on 24-h AUC/MIC ratios exceeding 25 (8, 29).
Data collection and analysis.
All pertinent data, including demographical and susceptibility data, were entered into a computerized data base. The MIC ranges and distributions and the MICs that inhibited 50 and 90% of the organisms tested (MIC50 and MIC90, respectively) were determined for each agent. Haemophilus data were analyzed for all strains, β-lactamase-positive strains, and β-lactamase-negative strains. For S. pneumoniae isolates, the analysis included all of the strains, as well as the penicillin-susceptible, intermediate, and penicillin-resistant strains. For all strains of both pathogens, data were also analyzed by geographic region, isolation site, and patient age. Statistical significance was determined by chi-square analysis, and P values of ≤0.05 were regarded as significant.
RESULTS
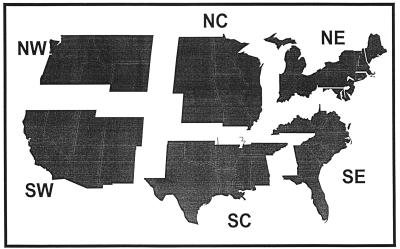
This comprehensive study evaluated 1,476 strains of S. pneumoniae and 1,676 untypeable strains of H. influenzae isolated from specimens submitted from patients in 31 states grouped into six regions (Fig. 1). Tables 1 and 2 show the distribution of strains by region and by specimen source, respectively. S. pneumoniae was isolated more frequently than H. influenzae from children ≤10 years of age, while H. influenzae was more common than S. pneumoniae in specimens from adults older than 30 years (Table 3).
FIG. 1.
Isolates from the six regions shown were analyzed. Abbreviations: NW, northwest; SW, southwest; NC, north central; SC, south central; NE, northeast; and SE, southeast.
TABLE 1.
Distribution of S. pneumoniae and H. influenzae isolates among regions of the United States
| Region | % of strains submitted
|
|
|---|---|---|
| S. pneumoniae | H. influenzae | |
| Northwest | 14.0 | 13.0 |
| Southwest | 7.0 | 9.8 |
| North central | 13.3 | 13.8 |
| South central | 14.2 | 15.7 |
| Northeast | 19.5 | 8.9 |
| Southeast | 31.9 | 38.8 |
TABLE 2.
Distribution of S. pneumoniae and H. influenzae isolates among specimen sources
| Source | % of strains of:
|
||||
|---|---|---|---|---|---|
|
S. pneumoniae
|
H. influenzae
|
||||
| Submitted | Penicillin intermediate | Penicillin resistant | Submitted | β-Lactamase positive | |
| Blood | 7.7 | 21.2 | 17.7 | 0 | NAa |
| Middle ear | 29.8 | 17.3 | 40.9 | 17.6 | 44.1 |
| Eye | 18.9 | 21.9 | 16.1 | 24.1 | 46.3 |
| Nasopharynx | 28.1 | 15.6 | 38.1 | 22.3 | 43.3 |
| Paranasal sinus | 4.7 | 16 | 44.9 | 4.0 | 44.8 |
| Lower respiratory tract | 8.8 | 16.8 | 30.5 | 27.3 | 35.0 |
| Other | 2.0 | 17.2 | 20.7 | 4.7 | 35.1 |
| All strains | 100 | 17.2 | 32.5 | 100 | 41.6 |
NA, not applicable.
TABLE 3.
Distribution of S. pneumoniae and H. influenzae isolates by patient age
| Age group (yr) | % of strains of:
|
||||
|---|---|---|---|---|---|
|
S. pneumoniae
|
H. influenzae
|
||||
| Submitted | Penicillin intermediate | Penicillin resistant | Submitted | β-Lactamase positive | |
| ≤2 | 50.4 | 19.9 | 38.4 | 38.7 | 47 |
| 3–10 | 17.3 | 12.9 | 24.2 | 12.1 | 39.9 |
| 11–20 | 3.1 | 13.0 | 26.1 | 3.8 | 42.2 |
| 21–30 | 4.1 | 19.7 | 21.3 | 3.3 | 30.9 |
| 31–40 | 6.4 | 15.8 | 30.5 | 7.3 | 46.3 |
| 41–50 | 3.7 | 14.8 | 24.1 | 7.8 | 33.8 |
| 51–60 | 2.2 | 24.2 | 27.3 | 5.3 | 37.1 |
| 61–70 | 3.2 | 10.6 | 38.3 | 7.1 | 33.6 |
| >70 | 5.8 | 15.3 | 23.5 | 9.5 | 33.8 |
| Unknown | 3.7 | 29.1 | 32.7 | 5.0 | 46.4 |
In children, isolates of S. pneumoniae and H. influenzae were cultured predominantly from specimens obtained from the eye, blood (S. pneumoniae only), middle ear, and nasopharynx, while in adults, strains were isolated predominantly from specimens obtained from the lower respiratory tract (mainly H. influenzae) and paranasal sinuses. Of S. pneumoniae isolates, 113 were isolated from blood (60% in the ≤2-year age group), 440 were from the middle ear (66%, ≤2 years; 21%, 3 to 10 years), 279 were from the eye (50%, ≤2 years), 415 were from the nasopharynx (76%, ≤10 years), 69 were from the paranasal sinus (28%, 31 to 40 years), and 131 were from sputum (40%, >70 years). Of H. influenzae isolates, 295 were from the middle ear (78%, ≤2 years; 12%, 3 to 10 years), 404 were from the eye (74%, ≤10 years), 374 were from the nasopharynx (67%, <10 years), 67 were from the paranasal sinus (43%, 31 to 50 years), and 374 were from sputum (85%, >30 years); no strains were isolated from blood.
H. influenzae susceptibility.
Of the 1,676 H. influenzae strains tested, 41.6% (697 strains) were β-lactamase positive and 58.4% (979 strains) were β-lactamase negative by the nitrocefin disk method (Tables 2 and 3). The MIC ranges and the MIC50s and MIC90s for all strains and for β-lactamase-positive and -negative strains are shown in Table 4. Only one fluoroquinolone-resistant H. influenzae strain was detected. This strain was additionally highly resistant to azithromycin and clarithromycin (MICs of >64 μg/ml).
TABLE 4.
MICs of 11 antimicrobial agents for H. influenzae isolates
| Antimicrobial agent | Concn (μg/ml) range tested | β-Lactamase-negative isolatesa
|
β-Lactamase-positive isolatesb
|
All isolatesc
|
|||
|---|---|---|---|---|---|---|---|
| MIC range | MIC50/MIC90 | MIC range | MIC50/MIC90 | MIC range | MIC50/MIC90 | ||
| Ampicillin | 0.12–16 | ≤0.12–4 | 0.25/1 | 2–>16 | >16/>16 | ≤0.12–>16 | 0.5/>16 |
| Amoxicillin | 0.12–16 | ≤0.12–4 | 0.5/1 | 2–>16 | >16/>16 | ≤0.12–>16 | 1/>16 |
| Amoxicillin-clavulanate | 0.12–16 | ≤0.12–4 | 0.5/1 | ≤0.12–4 | 0.5/1 | ≤0.12–4 | 0.5/1 |
| Cefaclor | 0.5–64 | ≤0.5–64 | 4/16 | ≤0.5–>64 | 8/32 | ≤0.5–>64 | 4/16 |
| Cefixime | 0.008–1 | ≤0.008–0.5 | 0.03/0.06 | ≤0.008–0.5 | 0.03/0.06 | ≤0.008–0.5 | 0.03/0.06 |
| Cefprozil | 0.5–64 | ≤0.5–32 | 2/8 | ≤0.5–64 | 4/32 | ≤0.5–>64 | 4/16 |
| Cefuroxime | 0.25–32 | ≤0.25–32 | 1/2 | ≤0.25–8 | 1/2 | ≤0.25–32 | 1/2 |
| Loracarbef | 0.5–64 | ≤0.5–>32 | 2/8 | ≤0.5–>64 | 4/32 | ≤0.5–>64 | 2/8 |
| Azithromycin | 0.06–8 | 0.25–4 | 2/2 | 0.25–>8 | 2/2 | 0.25–>8 | 2/2 |
| Clarithromycin | 0.25–32 | ≤0.25–>32 | 8/16 | ≤0.25–>32 | 8/16 | ≤0.25–>32 | 8/16 |
| Ciprofloxacin | 0.03–1 | ≤0.03–>1 | ≤0.03/≤0.03 | ≤0.03–0.06 | ≤0.03/≤0.03 | ≤0.03–>1 | ≤0.03/≤0.03 |
n = 979.
n = 697.
n = 1,676.
For β-lactamase-positive strains of H. influenzae, the MIC90 of ampicillin and amoxicillin was >16 μg/ml, that of clarithromycin was 16 μg/ml, and that of cefaclor, cefprozil, and loracarbef was 32 μg/ml (Table 4). Only one β-lactamase-negative strain demonstrated the features of a β-lactamase-negative, ampicillin-resistant strain, with an ampicillin MIC of 4 μg/ml, 1 dilution above the susceptibility breakpoint. It is of note, however, that more than 97% of the H. influenzae strains were susceptible to amoxicillin-clavulanate, cefixime, and ciprofloxacin by both the NCCLS and PK/PD breakpoints (Table 5). For cefuroxime, 99% of the strains were susceptible at the NCCLS breakpoint of 4 μg/ml, compared to 78% at the PK/PD breakpoint of 1 μg/ml. The susceptibility values for cefaclor, cefprozil, and loracarbef were 79, 86, and 91%, respectively, at the NCCLS breakpoint of 8 μg/ml for these agents but were 2, 14, and 9%, respectively, at the PK/PD breakpoints of 0.5, 1, and 0.5 μg/ml, respectively. These three agents were more active against β-lactamase-negative strains than against β-lactamase-positive strains; nonetheless, only 21% of the β-lactamase-negative strains were susceptible to cefprozil, the most active of these three agents. By NCCLS breakpoints, 99.7% of the H. influenzae isolates were susceptible to azithromycin and 76.6% were susceptible to clarithromycin; using PK/PD breakpoints, however, no strains were susceptible to these agents.
TABLE 5.
Percentages of H. influenzae isolates susceptible to 11 antimicrobial agents on the basis of NCCLS and PK/PD breakpoints
| Antimicrobial agent | Susceptibility breakpoint (μg/ml)
|
% of strains susceptible
|
||||||
|---|---|---|---|---|---|---|---|---|
| β-Lactamase-negative isolatesa
|
β-Lactamase-positive isolatesb
|
All isolatesc
|
||||||
| NCCLS | PK/PD | NCCLS | PK/PD | NCCLS | PK/PD | NCCLS | PK/PD | |
| Ampicillin | 1.0 | NAc | 98.1 | NA | 0.0 | NA | 57.3 | NA |
| Amoxicillin | 4.0 | 2.0 | 100.0 | 96.6 | 1.2 | 0.3 | 58.8 | 56.5 |
| Amoxicillin-clavulanate | 4.0 | 2.0 | 100.0 | 97.2 | 100.0 | 97.9 | 100.0 | 97.5 |
| Cefaclor | 8.0 | 0.5 | 89.1 | 2.6 | 64.4 | 0.4 | 78.9 | 1.7 |
| Cefixime | 1.0 | 1.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Cefprozil | 8.0 | 1.0 | 92.4 | 21.2 | 74.4 | 4.9 | 85.5 | 14.4 |
| Cefuroxime | 4.0 | 1.0 | 98.5 | 77.4 | 99.4 | 79.1 | 98.8 | 78.1 |
| Loracarbef | 8.0 | 0.5 | 97.4 | 14.1 | 80.7 | 2.7 | 90.5 | 9.4 |
| Azithromycin | 4.0 | 0.12 | 99.6 | 0 | 99.8 | 0 | 99.7 | 0 |
| Clarithromycin | 8.0 | 0.25 | 79.4 | 0.2 | 72.7 | 0 | 76.6 | 0.1 |
| Ciprofloxacin | 1.0 | 1.0 | 99.9 | 99.9 | 100.0 | 100.0 | 99.9 | 99.9 |
n = 979.
n = 697.
n = 1,676.
NA, not applicable.
S. pneumoniae susceptibility.
The MIC susceptibility data for the 1,476 strains of S. pneumoniae tested are summarized in Tables 2, 3, 6, and 7. Penicillin-susceptible strains accounted for 49.6% of the isolates, while 17.2% were penicillin intermediate and 32.5% were penicillin resistant (Table 2). Only one strain with a ceftriaxone MIC higher than that of penicillin was detected. No strain with a ciprofloxacin MIC of >4 μg/ml was found.
TABLE 6.
MICs of 12 antimicrobial agents for S. pneumoniae isolates
| Antimicrobial agent | Concn (μg/ml) range tested | Penicillin-susceptible isolatesa
|
Penicillin-intermediate isolatesb
|
Penicillin-resistant isolatesc
|
All isolatesd
|
||||
|---|---|---|---|---|---|---|---|---|---|
| MICe range | MIC50/MIC90 | MIC range | MIC50/MIC90 | MIC range | MIC50/MIC90 | MIC range | MIC50/MIC90 | ||
| Penicillin | 0.015–32 | ≤0.015–0.06 | 0.03/0.06 | 0.12–1 | 0.25/1 | 2.0–8.0 | 2/4 | ≤0.015–8 | 0.12/4 |
| Amoxicillin | 0.015–32 | ≤0.015–0.12 | ≤0.015/0.03 | ≤0.015–2 | 0.25/1 | 0.5–16 | 2/4 | ≤0.015–16 | 0.06/2 |
| Amoxicillin-clavulanate | 0.015–32 | ≤0.015–0.25 | 0.03/0.03 | ≤0.015–2 | 0.25/1 | 0.25–16 | 2/4 | ≤0.015–8 | 0.06/2 |
| Ceftriaxone | 0.015–32 | ≤0.015–0.5 | 0.03/0.06 | ≤0.015–4 | 0.25/0.5 | 0.25–8 | 1/2 | ≤0.015–16 | 0.06/2 |
| Cefaclor | 0.5–64 | ≤0.5–4 | 1/1 | ≤0.5–>64 | 4/32 | 1–>64 | 64/>64 | ≤0.5–>64 | 2/>64 |
| Cefixime | 0.5–64 | ≤0.5–16 | ≤0.5/≤0.5 | ≤0.5–>64 | 4/16 | 4–>64 | 32/64 | ≤0.5–>64 | 1/32 |
| Cefprozil | 0.5–64 | ≤0.5–1 | ≤0.5/≤0.5 | ≤0.5–32 | 1/4 | 0.5–>64 | 8/16 | ≤0.5–>64 | ≤0.5/16 |
| Cefuroxime | 0.03–16 | ≤0.03–2 | ≤0.03/0.12 | 0.06–8 | 0.5/4 | 0.25–8 | 4/8 | ≤0.03–8 | 0.25/8 |
| Loracarbef | 0.5–64 | ≤0.5–4 | 1/2 | ≤0.5–>64 | 4/64 | 2–>64 | >64/>64 | ≤0.5–>64 | 2/>64 |
| Azithromycin | 0.03–4 | ≤0.03–>4 | 0.12/0.12 | ≤0.03–>4 | 0.12/>4 | ≤0.03–>4 | 4/>4 | ≤0.03–>4 | 0.12/>4 |
| Clarithromycin | 0.015–2 | ≤0.015–>2 | 0.03/0.06 | ≤0.015–>4 | 0.06/>2 | ≤0.015–>4 | 2/>2 | ≤0.015–>2 | 0.03/>2 |
| Ciprofloxacin | 0.12–4 | ≤0.12–4 | 1/2 | 0.12–4 | 1/2 | 0.5–4 | 1/2 | ≤0.12–4 | 1/2 |
n = 732.
n = 254.
n = 480.
n = 1,476.
In micrograms per milliliter.
TABLE 7.
Percentages of S. pneumoniae isolates susceptible to antimicrobial agents on the basis of NCCLS and PK/PD breakpoints
| Antimicrobial agent | Susceptibility breakpoint (μg/ml)
|
% of isolates susceptible
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Penicillin-susceptible isolatesa
|
Penicillin-intermediate isolatesb
|
Penicillin-resistant isolatesc
|
All isolatesd
|
|||||||
| NCCLS | PK/PD | NCCLS | PK/PD | NCCLS | PK/PD | NCCLS | PK/PD | NCCLS | PK/PD | |
| Penicillin | 0.06, 1e | NAf | 100, 0 | 0, 100 | 0, 0 | 49.6, 67.5 | ||||
| Amoxicillin | 0.5 | 2 | 100 | 100 | 83.0 | 100 | 3.3 | 80.2 | 63.5 | 93.5 |
| Amoxicillin-clavulanate | 0.5 | 2 | 100 | 100 | 83.0 | 100 | 4 | 80.8 | 65.8 | 93.9 |
| Ceftriaxone | 0.5g | NA | 100 | 90.5 | 6.7 | 68.0 | ||||
| Cefaclor | 0.5 | 43.7 | 3.8 | 0 | 22.4 | |||||
| Cefixime | 1 | 95.2 | 21.7 | 0 | 52.1 | |||||
| Cefprozil | 1 | 100 | 72.0 | 0.4 | 62.6 | |||||
| Cefuroxime | 0.5 | 1 | 98.9 | 99.7 | 61.7 | 71.2 | 0.2 | 0.4 | 60.7 | 62.9 |
| Loracarbef | 0.5 | 20.4 | 3.4 | 0 | 10.7 | |||||
| Azithromycin | 0.5 | 0.12 | 95.2 | 94.7 | 65.5 | 64.8 | 33.3 | 32.9 | 69.8 | 69.2 |
| Clarithromycin | 0.25 | 0.25 | 95.2 | 95.2 | 65.5 | 65.5 | 33.3 | 33.3 | 69.8 | 69.8 |
| Ciprofloxacin | 1 | 85.7 | 80.3 | 82.9 | 83.8 | |||||
n = 732.
n = 264.
n = 480.
n = 1,476.
Penicillin susceptibility and intermediate penicillin susceptibility breakpoints.
NA, not applicable.
Meningitis breakpoint (see text).
It is of note that the MIC90s for all strains of cefaclor (>64 μg/ml), cefixime (32 μg/ml), and loracarbef (>64 μg/ml) were very high (Table 6), and susceptibility values at PK/PD breakpoints (Table 7) were low for these antimicrobial agents (22.4% for cefaclor, 52.1% for cefixime, and 10.7% for loracarbef); these agents do not currently have NCCLS breakpoints for S. pneumoniae. The overall susceptibility values by NCCLS breakpoints for the other antimicrobial agents tested were 60.7% for cefuroxime, 63.5% for amoxicillin, 65.8% for amoxicillin-clavulanate, 68% for ceftriaxone, and 69.8% for azithromycin and clarithromycin (Table 7). The overall susceptibility values by PK/PD breakpoints were the highest for amoxicillin (93.5%) and amoxicillin-clavulanate (93.9%), followed by cefuroxime at 62.9% and cefprozil at 62.6%; the values for azithromycin and clarithromycin were unchanged.
Analysis of the macrolide-azalide and penicillin cross-resistance of S. pneumoniae strains showed that 5.1% of the penicillin-susceptible strains were resistant to macrolides-azalides while 36.7% of the penicillin-intermediate strains and 65.6% of the penicillin-resistant strains were macrolide-azalide resistant (Table 8). All differences between penicillin and macrolide susceptibility categories were statistically significant (P < 0.001).
TABLE 8.
S. pneumoniae penicillin–macrolide-azalide cross-resistance
| Macrolide-azalide susceptibility | % of strains among:
|
||
|---|---|---|---|
| Penicillin-susceptible isolates | Penicillin-intermediate isolates | Penicillin-resistant isolates | |
| Susceptible | 94.9 | 60.8 | 32.6 |
| Intermediate | 0 | 2.5 | 1.8 |
| Resistant | 5.1 | 36.7 | 65.6 |
Susceptibility variations by region, age, and specimen source.
Susceptibility patterns were determined for each of six regions of the United States (Table 9). The highest proportions of penicillin-intermediate and penicillin-resistant strains of S. pneumoniae were from the south central region (62.4%) (P < 0.001 compared to the overall proportion) and the southeastern region (60.7%) (P < 0.001), while the northwestern region (39.3%) (P = 0.003) and northeastern region (35.8%) (P < 0.001) had the lowest. In all regions, but particularly in the south central and southeastern regions, more strains of S. pneumoniae were resistant than intermediately susceptible (Table 9). Overall, the proportion of penicillin-intermediate and penicillin-resistant strains in the three southern regions (60.7%) was significantly higher than in the three northern regions (39.2%) (P < 0.001). Similarly, the proportion of macrolide-azalide-resistant strains in the southern regions (39.5%) was higher than in the northern regions (22.7%) (P < 0.001).
TABLE 9.
Regional variation in β-lactam susceptibility of S. pneumoniae and H. influenzae isolates
| Region | % of strains of:
|
|||
|---|---|---|---|---|
|
S. pneumoniae
|
β-Lactamase-positive H. influenzae | |||
| Penicillin-intermediate | Penicillin- resistant | Penicillin- resistant or intermediate | ||
| Northwest | 16.0 | 23.3 | 39.3a | 36.7 |
| Southwest | 20.2 | 33.7 | 53.9 | 35.4 |
| North central | 18.8 | 25.4 | 44.2 | 48.3 |
| South central | 16.2 | 46.2 | 62.4b | 44.5 |
| Northeast | 14.6 | 21.2 | 35.8c | 50.3d |
| Southeast | 20.6 | 40.1 | 60.7e | 39.2 |
| Overall susceptibility | 17.9 | 32.5 | 50.4 | 41.6 |
P = 0.003.
P < 0.001.
P < 0.001.
P = 0.047.
P < 0.001.
The highest proportions of β-lactamase-positive strains of H. influenzae were from the northeastern (50.3%) (P = 0.047 compared to the overall proportion) and north central (48.3%) regions, while the lowest were from the northwestern (36.7%) and southwestern (35.4%) regions, although the differences for the last three regions did not reach statistical significance. Overall, however, the proportion of β-lactamase-positive strains from the three northern regions (44.6%) compared with the three southern regions (39.9%) just reached statistical significance (P = 0.05).
For S. pneumoniae isolates, the overall intermediate penicillin intermediate and penicillin resistance values were 17.9 and 32.5%, respectively. The prevalence of penicillin resistance in S. pneumoniae was the highest in isolates from the middle ear (40.9%) (P < 0.001 versus non-ear isolates) and sinus (44.9%) (P = 0.03 versus non-sinus isolates) specimens (Table 2). The proportion of strains nonsusceptible (intermediate and resistant) to penicillin was also the highest in the < 2-year-old age group (58.3% versus 42.1%) (P < 0.001 compared with the >2-year-old age group) (Table 3). In the youngest age groups, the prevalence of penicillin-resistant strains from middle ear specimens (49.7%) was higher than that of penicillin-intermediate strains (19.5%) in the <2-year-old age group (P < 0.001). The prevalence of penicillin-intermediate strains (21.2%) was similar to that of penicillin-resistant strains (17.7%) (no statistically significant difference) in blood specimens. The prevalence of penicillin-intermediate and penicillin-resistant strains was also high (resistant > intermediate) in nasopharyngeal specimens from all age groups.
Overall, 41.6% of the H. influenzae isolates were β-lactamase positive; the highest occurrence of β-lactamase-positive strains was in children younger than 2 years of age (47.0 versus 37.4% for >2-year-olds; P < 0.001), while the lowest was in nasopharyngeal (35.0%) and other (35.4%) specimen sources (Tables 2 and 3). In an analysis of H. influenzae resistance by both age and specimen source, the prevalence of β-lactamase-positive strains was higher in the following groups: (i) ear specimens from children <2 years of age (45.0%), compared with those from children ≥2 years old (37.3%); (ii) nasopharyngeal specimens from children <10 years of age (44.9%), compared with those from children ≥10 years of age (37.6%); and (iii) sinus specimens in adults 31 to 50 years of age (58.6%). However, none of these differences were statistically significant.
DISCUSSION
The recent increase in the resistance of the major respiratory pathogens H. influenzae and S. pneumoniae to oral antimicrobial agents has produced a need to re-evaluate treatment options for respiratory tract infections (16, 20). This is particularly important for the established oral agents, many of which have decreased activity against contemporary isolates, and also for newer agents like the fluoroquinolones, which currently have broader spectra of activity against these and other respiratory tract pathogens. Recent studies have shown that up to 33% of the strains of S. pneumoniae are penicillin intermediate or penicillin resistant in many parts of the country (13, 40). Furthermore, over 30% of the strains of H. influenzae and 90% of the strains of Moraxella catarrhalis now produce β-lactamases (12, 40). This severely limits the activity of many oral antimicrobial agents, particularly for pediatric use (1–4, 20, 23, 30).
Applying PK/PD breakpoints to the results of this study has identified amoxicillin-clavulanate and the fluoroquinolones as active against more than 90% of the strains of both S. pneumoniae and H. influenzae. Although ciprofloxacin itself has marginal activity against S. pneumoniae, no strains for which the ciprofloxacin MIC was >4 μg/ml were found and the newer fluoroquinolones, such as levofloxacin, sparfloxacin, grepafloxacin, and trovafloxacin, are active against pneumococci (23). Cefuroxime is the next most active agent against both species, with 78% of H. influenzae and 63% of S. pneumoniae strains being susceptible at PK/PD breakpoints. While 100% of H. influenzae strains are susceptible to cefixime, only 52% of S. pneumoniae strains are susceptible. In contrast, while 94% of S. pneumoniae strains are susceptible to amoxicillin, only 59% of H. influenzae strains are susceptible. Cefprozil has activity similar to that of cefuroxime against S. pneumoniae (63% susceptible) but poor activity against H. influenzae (14% susceptible). Cefaclor and loracarbef have poor activity against both species, with only 22 and 11% of S. pneumoniae and 2 and 9% of H. influenzae isolates, respectively, being susceptible. Although 69% of S. pneumoniae strains were susceptible to azithromycin and clarithromycin, no H. influenzae strains were susceptible based on serum PK/PD parameters. However, a human volunteer study on the intrapulmonary distribution of clarithromycin and azithromycin demonstrated much higher concentrations of these agents in epithelial lining fluid (ELF) than in serum (35). Drug concentrations present in ELF for ≥50% of the dosing interval were 15 to 30 μg/ml (mean of five values, 26.1 μg/ml) for clarithromycin and <0.1 to 1 μg/ml (mean of five values [excluding one value of <0.1 μg/ml], 0.95 μg/ml). These concentrations exceed the MICs of clarithromycin for most strains of H. influenzae and some strains of macrolide-resistant S. pneumoniae and the MICs of azithromycin for some strains of H. influenzae. However, the importance of these drug concentrations in ELF for the clinical outcome of pulmonary infections is unclear.
Analysis of the pathogen distribution obtained in this study by patient age, specimen source, and geographic area shows some interesting patterns. The number of strains isolated from middle ear specimens is alarming, since such specimens can only be obtained by tympanocentesis or after the tympanic membrane ruptures spontaneously. Thus, these isolates likely represent treatment failures, which is supported by the resistant nature of many of the S. pneumoniae isolates from ear specimens compared to other sites. Similarly, paranasal sinus specimens were presumably obtained by sinus puncture and may well also represent treatment failures. The majority of S. pneumoniae (68%) and H. influenzae (51%) strains were isolated from children <10 years of age, although many of these strains were recovered from eye and nasopharyngeal specimens. The significance of these strains in eye specimens, predominantly from conjunctival exudates, is questionable. Their significance in nasopharyngeal specimens is unknown but presumably results from practitioners wanting to know whether patients are carrying resistant strains to guide the therapy of treatment failures or complications.
This study documents the dramatic and alarming increase in β-lactam and macrolide-azalide resistance in S. pneumoniae, particularly the alarming increase in strains both fully penicillin resistant and also resistant to macrolides-azalides. A few case reports have documented the clinical failure of macrolides-azalides (21, 32), and the clinical value of these agents remains controversial (4, 42). Amoxicillin and amoxicillin-clavulanate still retain their activity, however, with 94% of the S. pneumoniae strains being susceptible in our study. In addition, ceftriaxone-resistant strains with lower penicillin MICs remain rare (only one strain being found in this study) and most strains causing nonmeningeal infections should respond to this agent administered intravenously or intramuscularly. An appropriate PK/PD breakpoint for this agent in nonmeningeal infections is 2 μg/ml (8), with 97.7% of the strains being susceptible at this concentration in our study. Treating meningitis with ceftriaxone may be a problem, however, since only 68% of the strains were susceptible at the meningitis breakpoint of 0.5 μg/ml and for a further 9.4% of the strains the MIC was 1 μg/ml, the current intermediate value in meningitis. Although no fluoroquinolone-resistant strains were found in this study, such strains have been identified (19, 40) and the indiscriminate use of these agents to treat respiratory tract infections could lead to the development and spread of resistance.
In contrast to S. pneumoniae, our results showed no major changes in susceptibility in H. influenzae isolates, although the prevalence of β-lactamase positivity continued to increase, with 42% of the strains being positive. The MIC50s and MIC90s were generally unchanged from those of previous studies, however, despite the fact that the proportions of strains susceptible to many agents differ markedly from those in other studies due to our use of PK/PD breakpoints (2, 12, 15, 25, 40). As with S. pneumoniae, fluoroquinolone resistance has not yet emerged in H. influenzae, with only one resistant strain detected. Additionally, no major shift in non-β-lactamase-mediated β-lactam resistance was found, with only one possible β-lactamase-negative, ampicillin-resistant strain being found. No amoxicillin-clavulanate-resistant strains were found, in contrast to a previous study, in which 3.6% of the strains from a comparable patient population were found to be resistant to the NCCLS breakpoint of 4 μg/ml, with MICs mainly 1 dilution above the breakpoint (12). The MIC distributions of several agents in that study, including amoxicillin-clavulanate and cefuroxime, were wider than those most investigators have reported, and the MIC50 and MIC90 of amoxicillin-clavulanate were 1 and 2 μg/ml, rather than the usual 0.5 and 1 μg/ml reported in previous studies (22, 24, 36), as well as in the current study. Problems associated with the methods used to test Haemophilus susceptibility appear to be responsible for these differences (24).
The results of this study should be applied to clinical practice based on the clinical presentation of the patient, the probability of the patient’s having a bacterial rather than a viral infection, the natural history of the disease, the potential of pathogens to be susceptible to various oral antimicrobial agents, the potential for cross-resistance between agents with S. pneumoniae, and the potential of pathogens to develop further resistance (37). Antibiotics should be used judiciously to maintain any remaining activity (16, 17) and chosen carefully based on activity determined by PK/PD-based breakpoints (8).
In summary, this study has highlighted the continued dramatic rise in β-lactam and macrolide-azalide resistance in S. pneumoniae and a modest continued rise in β-lactamase production in untypeable H. influenzae. In addition, pharmacodynamic parameters have been used to interpret susceptibility data in a more clinically meaningful way. Judicious antibiotic use is the key to avoiding the development of further resistance to available agents in these bacteria.
ACKNOWLEDGMENTS
Financial support for this work was provided by SmithKline Beecham Pharmaceuticals, Philadelphia, Pa.
We thank Raymond Kaplan and Linda Miller for coordinating collection of strains, Gwen Kendall for secretarial assistance, and PMSI Scott-Levin, Inc., Newtown, Pa., for permission to use antibiotic prescription data.
REFERENCES
- 1.Barry A L, Fuchs P C. In vitro activities of a streptogramin (RP59500), three macrolides, and an azalide against four respiratory tract pathogens. Antimicrob Agents Chemother. 1995;39:238–240. doi: 10.1128/aac.39.1.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barry A L, Pfaller M A, Fuchs P C, Packer R R. In vitro activities of 12 orally administered antimicrobial agents against four species of bacterial respiratory pathogens from U.S. medical centers in 1992 and 1993. Antimicrob Agents Chemother. 1994;38:2419–2425. doi: 10.1128/aac.38.10.2419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barry A L. Antimicrobial agents for community-acquired respiratory tract infections. Infection. 1995;23(Suppl. 2):S59–S63. doi: 10.1007/BF01742985. . (Discussion, S64.) [DOI] [PubMed] [Google Scholar]
- 4.Bartlett J G. Empirical therapy of community-acquired pneumonia: macrolides are not ideal choices. Semin Respir Infect. 1997;12:329–333. [PubMed] [Google Scholar]
- 5.Black S B, Shinefield H R The Kaiser Permanente Vaccine Study Group. Immunization with oligosaccharide conjugate Haemophilus influenzae type b (HbOC) vaccine on a large HMO population: extended follow-up and impact on Haemophilus influenzae disease epidemiology. Pediatr Infect Dis J. 1992;11:610–613. [PubMed] [Google Scholar]
- 6.Bradley J S, Connor J D. Ceftriaxone failure in meningitis caused by Streptococcus pneumoniae with reduced susceptibility to β-lactam antibiotics. Pediatr Infect Dis J. 1991;10:871–872. [PubMed] [Google Scholar]
- 7.Craig W A, Andes D. Pharmacokinetics and pharmacodynamics of antibiotics in otitis media. Pediatr Infect Dis J. 1996;15:255–259. doi: 10.1097/00006454-199603000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Craig W A. Pharmacokinetic/pharmacodynamic parameters: rationale for antibacterial dosing of mice and men. Clin Infect Dis. 1998;26:1–10. doi: 10.1086/516284. [DOI] [PubMed] [Google Scholar]
- 9.Dagan R, Abramson O, Leibovitz E, Greenberg D, Lang R, Goshen S, Yagupsky P, Leiberman A, Fliss D M. Bacteriologic response to oral cephalosporins: are established susceptibility breakpoints appropriate in the case of acute otitis media? J Infect Dis. 1997;176:1253–1259. doi: 10.1086/514120. [DOI] [PubMed] [Google Scholar]
- 10.Dagan R, Abramson O, Leibovitz E, Lang R, Goshen S, Greenberg D, Yagupsy P, Leiberman A, Fliss D M. Impaired bacteriologic response to oral cephalosporins in acute otitis media caused by pneumococci with intermediate resistance to penicillin. Pediatr Infect Dis J. 1996;15:980–985. doi: 10.1097/00006454-199611000-00010. [DOI] [PubMed] [Google Scholar]
- 11.Dagan R, Piglansky L, Yagupsky P, Fliss D M, Leiberman A, Leibovitz E. Abstracts of the 37th Interscience Conference on Antimicrobial Agents and Chemotherapy. Washington, D.C: American Society for Microbiology; 1997. Bacteriologic response in acute otitis media (AOM): comparison between azithromycin (AOM), (AZ), cefaclor (CEC) and amoxicillin (AMOX), abstr. K-103; p. 346. [Google Scholar]
- 12.Doern G V, Brueggemann A B, Pierce G, Holley H P, Jr, Rauch A. Antibiotic resistance among clinical isolates of Haemophilus influenzae in the United States in 1994 and 1995 and detection of β-lactamase-positive strains resistant to amoxicillin-clavulanate: results of a national multicenter surveillance study. Antimicrob Agents Chemother. 1997;41:292–297. doi: 10.1128/aac.41.2.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Doern G V, Brueggemann A, Holley H P, Jr, Rauch A M. Antimicrobial resistance of Streptococcus pneumoniae recovered from outpatients in the United States during the winter months of 1994 to 1995: results of a 30-center national surveillance study. Antimicrob Agents Chemother. 1996;40:1208–1213. doi: 10.1128/aac.40.5.1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Doern G V, Jorgensen J H, Thornsberry C, Preston D A, Tubert T, Redding J S, Maher L A. National collaborative study of the prevalence of antimicrobial resistance among clinical isolates of Haemophilus influenzae. Antimicrob Agents Chemother. 1988;32:180–185. doi: 10.1128/aac.32.2.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Doern G V. Antimicrobial resistance among lower respiratory tract isolates of Haemophilus influenzae: results of a 1992–93 Western Europe and USA collaborative study. J Antimicrob Chemother. 1996;38(Suppl. A):59–69. doi: 10.1093/jac/38.suppl_a.59. [DOI] [PubMed] [Google Scholar]
- 16.Dowell S F, Marcy S M, Phillips W R, Gerber M A, Schwartz B. Principles of judicious use of antimicrobial agents for pediatric upper respiratory tract infections. Pediatrics. 1998;101:163–165. [Google Scholar]
- 17.Dowell S F, Butler J C, Giebink G S, Jacobs M R, Jernigan D, Musher D M, Rakowsky A, Schwartz B. Acute otitis media: management and surveillance in an era of pneumococcal resistance—a report from the Drug-Resistant Streptococcus pneumoniae Therapeutic Working Group. Pediatr Infect Dis J. 1999;18:1–9. [PubMed] [Google Scholar]
- 18.Drusano G L, Craig W A. Relevance of pharmacokinetics and pharmacodynamics in the selection of antibiotics for respiratory tract infections. J Chemother. 1997;9(Suppl. 3):38–44. [PubMed] [Google Scholar]
- 19.Drusano G L, Goldstein F W. Relevance of the Alexander Project: pharmacodynamic considerations. J Antimicrob Chemother. 1996;38(Suppl. A):141–154. doi: 10.1093/jac/38.suppl_a.141. [DOI] [PubMed] [Google Scholar]
- 20.Green M, Wald E R. Emerging resistance to antibiotics: impact on respiratory infections in the out-patient setting. Ann Allergy Asthma Immunol. 1996;77:167–173. doi: 10.1016/S1081-1206(10)63250-4. [DOI] [PubMed] [Google Scholar]
- 21.Jackson M A, Burry V F, Olson L C, Duthie S E, Kearns G L. Breakthrough sepsis in macrolide-resistant pneumococcal infection. Pediatr Infect Dis J. 1996;15:1049–1051. doi: 10.1097/00006454-199611000-00026. [DOI] [PubMed] [Google Scholar]
- 22.Jacobs M R. Assessing the quality of the Alexander Project. J Chemother. 1999;11:26–34. doi: 10.1179/joc.1999.11.Supplement-2.26. [DOI] [PubMed] [Google Scholar]
- 23.Jacobs M R, Appelbaum P C. Antibiotic-resistant pneumococci. Rev Med Microbiol. 1995;6:77–93. [Google Scholar]
- 24.Jacobs M R, Bajaksouzian S. Microbiologic evaluation of contemporary Haemophilus influenzae isolates having elevated MICs to amoxicillin-clavulanic acid. Diagn Microbiol Infect Dis. 1997;28:105–112. doi: 10.1016/s0732-8893(97)00008-4. [DOI] [PubMed] [Google Scholar]
- 25.Jones R N, Jacobs M R, Washington J A, Pfaller M A. A 1994–95 survey of Haemophilus influenzae susceptibility to ten orally administered agents. A 187 clinical laboratory center sample in the United States. Diagn Microbiol Infect Dis. 1997;27:75–83. doi: 10.1016/s0732-8893(96)00219-2. [DOI] [PubMed] [Google Scholar]
- 26.Khan W, Ross S, Rodriguez W, Controni G, Saz A K. Haemophilus influenzae type b resistant to ampicillin: a report of two cases. JAMA. 1974;229:298–301. [PubMed] [Google Scholar]
- 27.National Committee for Clinical Laboratory Standards. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. Approved standard M7-A4. Villanova, Pa: National Committee for Clinical Laboratory Standards; 1997. [Google Scholar]
- 28.National Committee for Clinical Laboratory Standards. Performance standards for antimicrobial susceptibility testing. Sixth information supplement M100-S7. Villanova, Pa: National Committee for Clinical Laboratory Standards; 1997. [Google Scholar]
- 29.Nightingale, C. H. Pharmacokinetics and pharmacodynamics of newer macrolides. Pediatr. Infect. Dis. J. 16:438–443. [DOI] [PubMed]
- 30.Pelton S I. Defining resistance: breakpoints and beyond implications for pediatric respiratory infection. Diagn Microbiol Infect Dis. 1996;25:195–199. doi: 10.1016/s0732-8893(96)00138-1. [DOI] [PubMed] [Google Scholar]
- 31.PMSI Scott-Levin, Inc. Physician drug and diagnosis audit (PDDA). 1997. PMSI Scott-Levin, Inc., Newtown, Pa. [Google Scholar]
- 32.Reid R, Jr, Bradley J S, Hindler J. Pneumococcal meningitis during therapy of otitis media with clarithromycin. Pediatr Infect Dis J. 1995;14:1104–1105. doi: 10.1097/00006454-199512000-00016. [DOI] [PubMed] [Google Scholar]
- 33.Rittenhouse S F, Miller L A, Kaplan R L, Mosely G H, Poupard J A. A survey of β-lactamase-producing Haemophilus influenzae. Diagn Microbiol Infect Dis. 1995;21:223–225. doi: 10.1016/0732-8893(95)00028-9. [DOI] [PubMed] [Google Scholar]
- 34.Roberts D E, Ingold A, Want S V, May J R. Osmotically stable L-forms of Haemophilus influenzae and their significance in testing sensitivity to penicillins. J Clin Pathol. 1974;27:560–564. doi: 10.1136/jcp.27.7.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rodvold K A, Gotfried M H, Danziger L H, Servi R J. Intrapulmonary steady-state concentrations of clarithromycin and azithromycin in healthy adult volunteers. Antimicrob Agents Chemother. 1997;41:1399–1402. doi: 10.1128/aac.41.6.1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rolinson G N. A review of the microbiology of amoxicillin-clavulanic acid over the 15-year period 1978–1993. J Chemother. 1994;6:283–318. doi: 10.1080/1120009x.1994.11741165. [DOI] [PubMed] [Google Scholar]
- 37.Rosenfeld R M. An evidence-based approach to treating otitis media. 1996. Pediatr Clin N Am. 1996;430:1165–1181. doi: 10.1016/s0031-3955(05)70512-5. [DOI] [PubMed] [Google Scholar]
- 38.Sloas M M, Barrett F F, Chesney P J, English B K, Hill B C, Tenover F C, Leggiadro R J. Cephalosporin treatment failure in penicillin- and cephalosporin-resistant Streptococcus pneumoniae meningitis. Pediatr Infect Dis J. 1992;11:662–666. [PubMed] [Google Scholar]
- 39.Sykes R B, Griffiths A, Ryan D M. Comparative activity of ampicillin and cefuroxime against three types of Haemophilus influenzae. Antimicrob Agents Chemother. 1977;11:599–604. doi: 10.1128/aac.11.4.599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Thornsberry C, Oglivie P, Kahn J, Mauritz Y. Surveillance of antimicrobial resistance in Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis in the United States in 1996–1997 respiratory season. Diagn Microbiol Infect Dis. 1997;29:249–257. doi: 10.1016/s0732-8893(97)00195-8. [DOI] [PubMed] [Google Scholar]
- 41.Tomeh M O, Starr S E, McGowan J E, Jr, Terry P M, Nahamias A J. Ampicillin-resistant Haemophilus influenzae type b infection. JAMA. 1974;229:295–297. [PubMed] [Google Scholar]
- 42.Vergis E N, Yu V L. Macrolides are ideal for empiric therapy of community-acquired pneumonia in the immunocompetent host. Semin Respir Infect. 1997;12:322–328. [PubMed] [Google Scholar]