Abstract
Fracture of the tibial component can be a devastating complication after primary total knee arthroplasty. While fractures of the tibial baseplate have been reported, failure at the junction between the baseplate and stem has not been well-described. We present a 49-year-old male who developed progressively worsening left knee pain and an effusion 7-8 years after an index total knee arthroplasty. Radiographs revealed component subsidence and subtle asymmetry between the baseplate and stem. At the time of revision, the tibial component was found to be fractured at the junction of the baseplate and stem, with complete dissociation between the two pieces. Clinicians should maintain a high index of suspicion for catastrophic failure, as this rare phenomenon can be subtle on radiographs and requires close monitoring for signs of component subsidence.
Keywords: Total knee arthroplasty, Total knee revision, Catastrophic failure, Tibial baseplate, Osteolysis
Introduction
Fracture of the tibial component after total knee arthroplasty (TKA) is a rare and catastrophic complication that requires a challenging revision surgery [1]. The most common reasons for failure and revision surgery include aseptic loosening, instability, and periprosthetic infection [2]. Malpositioned components, limb malalignment, and uneven joint balancing have also been shown to predispose to tibial baseplate fracture [1]. While fractures of the tibial baseplate have been reported previously throughout the literature, a fracture at the stem and baseplate junction has been described far less frequently.
Presented herein is a case of catastrophic failure of the tibial component 7-8 years after the index TKA. The patient had increasing knee pain with an effusion and no obvious signs of implant failure on radiographs except for a subtle asymmetry between the tibial baseplate and stem. Given the absence of any overt mechanical or infectious cause for his knee pain, a TKA revision was performed for presumed aseptic loosening. Intraoperatively, a complete fracture between the tibial baseplate and stem was found, which was not apparent on preoperative radiographs. The patient underwent extraction of all components, and a press-fit condylar Sigma TC3 Knee System (DePuy Synthes/Johnson & Johnson, Warsaw, IN) was implanted. In this report, case details are reviewed, and management of this complication is detailed.
Case history
The patient is a 49-year-old incarcerated male with a body mass index (BMI) of 34 kg/m2 who originally underwent an uncomplicated left primary TKA in January 2012 with a cemented cruciate-retaining tibial implant (Zimmer Biomet, Warsaw, IN). Although full flexion and extension of the knee could be achieved with the prosthesis during the index procedure, he was only able to attain approximately 60° of flexion at his 2-week follow-up visit despite vigorous stretching and physical therapy. In order to prevent this from being a chronic problem, the decision was made to perform a gentle manipulation under anesthesia, and per report, full flexion and extension of the knee were achieved without any undue pressure being applied. At his 2-week clinic follow-up visit, the patient was able to achieve active flexion to 100° and extend to −5°. The patient did well from that point on and had no issues with the prosthesis for about 7-8 years.
He began to notice increasing left knee pain and swelling that progressively worsened over the course of 1 year. He denied any antecedent trauma to the knee. The pain he described was startup pain when he would stand from a seated position, and the pain would typically resolve within the first few steps. He denied any fevers or chills. After the pain acutely worsened and necessitated the use of crutches for ambulation, he presented to the emergency department in July 2020. Physical examination of the knee demonstrated a well-healed midline incision with an effusion present. Left knee range of motion was 0-110° of flexion with tenderness over the medial and lateral aspects of the proximal tibia. He had instability to varus and valgus stress testing in full extension and throughout the range of motion of the left knee. The foot was neurovascularly intact distally. Radiographs of the left knee demonstrated a significant lucency at the bone-cement interface of his proximal tibia medially and laterally concerning for subsidence of the tibial component and subtle asymmetry between the tibial baseplate and stem on the lateral radiograph, but no overt signs of gross catastrophic failure of the tibial prosthesis (Fig. 1). Serology revealed a white blood cell count of 5.7 K/μL (4.0-11.0 K/μL), erythrocyte sedimentation rate of 15 mm/h (0-20 mm/h), and C-reactive protein of 3.1 mg/L (0-5.0 mg/L). Further workup for infection, including sterile aspiration of the prosthetic joint, was negative. The patient consented to a revision left TKA for presumed aseptic loosening.
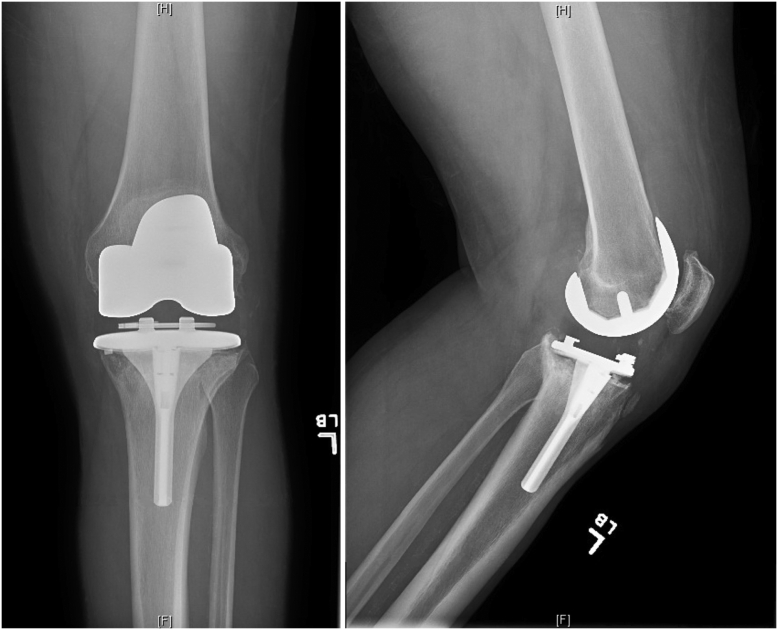
Figure 1.
Preoperative radiographs. Anteroposterior radiograph (a) of the left knee demonstrating lucency at the bone-cement interface of the proximal tibia medially and laterally concerning for loosening of the tibial prosthesis. Lateral radiograph (b) shows subtle asymmetry between the tibial baseplate and stem, but no overt evidence of catastrophic failure of the tibial component.
The patient was taken to the operating room, and a medial parapatellar arthrotomy was performed. There was extensive metal debris and pigmented tissue in the suprapatellar pouch and along the medial and lateral gutters. The tibial component was found to have a clear fracture at the stem and baseplate junction, with disassociation between the tibial baseplate and stem (Fig. 2). The polyethylene was well-fixed and locked into the tibial baseplate, and the baseplate with the locked polyethylene had become loose and separated from the proximal tibia. There was also gross loosening of the femoral component noted intraoperatively as well. Removal of the femoral and tibial components was performed with minimal bone loss. The retained stem portion of the tibial component was extracted using a motorized bur and a combination of rigid and flexible osteotomes. A press-fit condylar Sigma TC3 Knee System (DePuy Synthes/Johnson & Johnson, Warsaw, IN) was implanted, consisting of a size-4 femoral component with a 31-mm sleeve and a 16 × 115-mm stem. The tibial component was a size-3 mobile bearing tibia with a 45-mm sleeve and a 14 × 75-mm stem (DePuy Synthes/Johnson & Johnson). The polyethylene insert was a Gamma Vacuum Foil 10-mm thickness rotating platform TC3 size-4 insert (DePuy Synthes/Johnson & Johnson). The patella was resurfaced with a 38-mm patella button. All components were inserted without complication, and the patient was made weight-bearing as tolerated after the procedure. Immediate postoperative radiographs demonstrated appropriately positioned components (Fig. 3). He was discharged without issue on postoperative day 3 after working with physical therapy.
Figure 2.
Catastrophic failure of the component. Intraoperative photograph demonstrating fracture and catastrophic failure of the tibial component. The tibial baseplate and well-fixed polyethylene were completely dissociated from the stem portion of the tibial component.
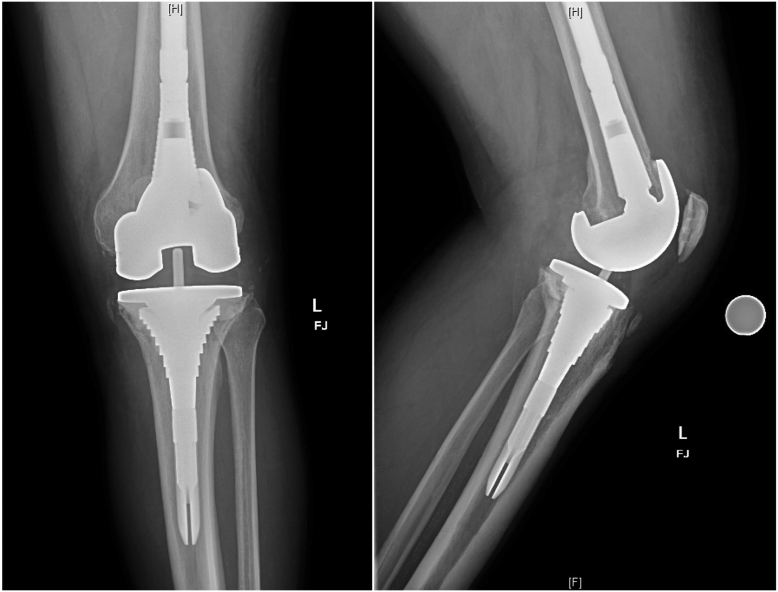
Figure 3.
Immediate postoperative radiographs. Postoperative anteroposterior (a) and lateral (b) radiographs.
The patient was seen in clinic 2 weeks after the revision surgery for staple removal, at which time he reported substantial relief from his pain and no difficulty with ambulation. At the time of his final follow-up appointment at 18 months, examination revealed a well-healed incision with active knee range of motion from 0 to 120° without pain. Radiographs revealed well-fixed components in appropriate alignment (Fig. 4).
Figure 4.
Radiographs at follow-up. Anteroposterior (a) and lateral (b) radiographs demonstrating well-fixed components in appropriate alignment.
The patient was made aware of our intentions to publish this case report detailing his condition and gave his verbal and written consent to proceed.
Discussion
Aseptic tibial component failure resulting from either subsidence of the tibial baseplate or insert wear accounts for approximately 2% of revisions after mechanically aligned TKA [3]. Factors such as varus alignment of the tibial component, elevated BMI, short-keeled tibial baseplates, and young age of the patient have all been cited as reasons for catastrophic failure [3]. Early fractures of the tibial baseplate were historically attributed to poor surgical technique, implant manufacturing issues, or poor bone quality [4]. Through improvements in implant design and metallurgy, and the addition of highly cross-linked ultra-high-molecular-weight polyethylene inserts, case reports detailing fractures of the tibial component have become increasingly less frequent in recent years [1]. Proposed mechanisms leading to late baseplate fractures include malalignment and fatigue failure, bone loss due to osteolysis, undersizing of the tibial component, and elevated patient weight [4]. A common mechanism of failure of the tibial component is varus subsidence of the tibial baseplate, which results from high medial loads that subsequently cause medial bone collapse [3]. Eccentric joint contact forces seen in malalignment are further amplified in the setting of an elevated BMI, as any varus deviation of the tibial component from being perpendicular to the mechanical axis of the tibia increases the risk of tibial component failure [3]. Obesity has been described as a separate risk factor for aseptic loosening, varus collapse, and baseplate failure even without the presence of malalignment [5]. Abdel et al. reported the incidence of aseptic loosening in TKA patients with BMI ≥ 35 kg/m2 to be nearly double that of those with BMI < 35 kg/m2, independent of the coronal alignment of the components [5].
Revision TKA related to fracture of the tibial component itself is typically multifactorial, with factors such as implant material, design, surgical technique, and alignment having important contributing roles [6]. While many mechanisms for these fractures have been proposed, most have been related to implant design or wear of the components. Chatterji et al. sought to determine the etiology of tibial baseplate fracture after TKA by reviewing all the fractured knee prostheses in the retrieval laboratories at their institutions [7]. They analyzed 25 metal tibial baseplates that were found to be fractured upon revision TKA, and clinical records and components were reviewed to determine if any relationship existed between patient-related factors, implant design, and fracture type [7]. In their study, 25 fractured tibial baseplates were analyzed with a mean time to fracture of 7.8 years and a mean duration of symptoms before fracture of 10.8 months [7]. They found a relationship between proximal tibial bone loss and fracture location, with the baseplate always fracturing on the same side as the tibial bone loss [7]. The authors concluded that the most important feature predisposing to baseplate fracture was the loss of proximal tibial bone support, as there was a 100% correlation between the site of the fracture on the tibial baseplate and the region of bone loss [7]. They suggested that the lack of subprosthetic proximal tibial bone support predisposes to baseplate fracture, as the repetitive bending forces on the unsupported part of the baseplate can lead to metal fatigue [7].
Preoperative varus deformity and male gender have also been cited as possible risk factors for tibial baseplate fracture [6]. Abernethy et al. identified 16 patients who underwent revision for fracture of the metal tibial tray among 1567 elective TKAs [8]. Fracture of the tibial baseplate occurred at a mean of 54 months after the primary operation, with 11 of the 16 patients developing mild aching discomfort with progressive instability and recurrence of varus deformity [8]. Preoperative radiographs revealed that all the affected knees had varus angulation since the fractures always occurred on the medial side [8]. They found that preoperative varus deformity (hazard ratio [HR] = 8.6), failure to correct such deformity beyond neutral (HR = 5.2), and the use of a bone graft to correct varus deformity (HR = 11.3) were all statistically significant risk factors for tibial baseplate fracture [8]. Male gender was also identified as a risk factor, as there was a higher proportion of male patients (HR = 1.9) who were found to have a fracture of the prosthesis; however, this was not found to be statistically significant [8].
Although TKA implants have undergone numerous advances in design and materials to improve their durability, longevity, and survivorship, fracture of a modern TKA prosthesis is a rare complication that can still occur [1]. Callaghan et al. presented the findings from a retrieval analysis of a modern tibial tray that had fractured in a 67-year-old female who underwent revision TKA [2]. The patient in their case report underwent an uneventful TKA for primary osteoarthritis with a cemented PFC Sigma design with a polished, chrome cobalt tibial tray [2]. She developed medial-sided knee pain at approximately 17 months postoperatively, and radiographs revealed her knee to be in 15° of varus and demonstrated the presence of a fracture of the tibial tray [2]. At the time of revision surgery, there was necrotic bone within the posteromedial aspect of the tibial plateau, and she was revised with a DePuy PFC Sigma revision tibial component [2]. Implant analysis suggested fatigue fracture to be the most likely mechanism of failure, as multiple fatigue striations were observed over the majority of the fracture surface [2]. The authors postulated that the loss of proximal tibial bone support under the fractured area likely led to failure of the implant, and the deficient bony support under a portion of the tibial plate resulted in the loose portion acting as a cantilever [2]. As a result, this created an increased amount of stress at the junction between the supported and nonsupported segments of the prosthesis eventually leading to failure of the device [2]. Additionally, the patient had a BMI of 34.1 kg/m2, so it is possible her weight could have played an important role in the catastrophic failure of the implant.
The etiology of tibial component failure in our patient is likely multifactorial, which is consistent with the modes of failure suggested throughout the literature. Our patient was obese with a BMI of 34 kg/m2, which placed increased contact forces through the prosthesis and may have contributed to subsidence at the bone-cement interface between the tibial baseplate and his native bone. This subsidence, when combined with a relatively well-fixed stem component, likely led to fatigue wear at the baseplate and stem junction, thus propagating the eventual implant’s catastrophic failure.
While most reports in the literature describe a fracture of the tibial component occurring at or around the baseplate, a fracture at the stem and baseplate junction of the prosthesis has been infrequently described. Although the preoperative radiographs demonstrated findings consistent with osteolysis and a subtle asymmetry between the tibial baseplate and the stem on the lateral radiograph, no overt signs of gross catastrophic failure of the tibial prosthesis were apparent. It was not until the time of revision surgery that the tibial component was found to be fractured, with the tibial baseplate and polyethylene completely dissociated from the intact stem distally. Delayed diagnosis can often be a contributing factor to poor outcomes since bone loss can continue to occur from the altered loading environment of the knee with implant fracture, if it is not readily identified and expeditiously revised [4]. This highlights the importance for clinicians to maintain a high index of suspicion for potential implant failure if there are findings consistent with implant subsidence or asymmetry between the individual components of the prosthesis.
Summary
Fracture of the tibial component after TKA is a rare complication that requires a complex revision surgery, scrutiny of preoperative radiographs, and analysis of the failed implant to determine the likely cause of catastrophic failure. This case highlights the importance of component alignment, optimizing the BMI, and careful monitoring on radiographs for signs of component subsidence and asymmetry of the prosthesis in the postoperative TKA patient.
Conflicts of interest
The authors declare there are no conflicts of interest.
For full disclosure statements refer to https://doi.org/10.1016/j.artd.2022.02.002.
Informed patient consent
The author(s) confirm that informed consent has been obtained from the involved patient(s) or if appropriate from the parent, guardian, power of attorney of the involved patient(s); and, they have given approval for this information to be published in this case report (series).
Footnotes
No author associated with this paper has disclosed any potential or pertinent conflicts which may be perceived to have impending conflict with this work.
Appendix A. Supplementary data
References
- 1.Scully W.F., Deren M.E., Bloomfield M.R. Catastrophic tibial baseplate failure of a modern cementless total knee arthroplasty implant. Arthroplasty Today. 2019;5:446. doi: 10.1016/j.artd.2019.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Callaghan J.J., DeMik D.E., Bedard N.A., Odland A.N., Kane W.M., Kurtz S.M. Tibial tray fracture in a modern prosthesis with retrieval analysis. Arthroplasty Today. 2018;4:143. doi: 10.1016/j.artd.2017.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nedopil A.J., Howell S.M., Hull M.L. What mechanisms are associated with tibial component failure after kinematically-aligned total knee arthroplasty? Int Orthop. 2017;41(8):1561. doi: 10.1007/s00264-017-3490-6. [DOI] [PubMed] [Google Scholar]
- 4.Constantinescu D.S., Ross J.A., Patel N.K., Strong B.M., Giambra L.A., Golladay G.J. Radiographic false evidence of a tibial baseplate fracture after total knee arthroplasty. Arthroplasty Today. 2021;8:114. doi: 10.1016/j.artd.2021.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mesko D.R., Sadauskas A.J., Sporer S.M. Fracture of a cemented modern titanium alloy tibia baseplate: a case report. MOJ Orthop Rheumatol. 2018;10(4):303. [Google Scholar]
- 6.Austin M.S., Sharkey P.F., Hozack W.J., Rothman R.H. Knee failure mechanisms after total knee arthroplasty. Tech Knee Surg. 2004;3(1):55. [Google Scholar]
- 7.Chatterji U., Ashworth M.J., Smith A.L., Brewster N., Lewis P.L. Retrieval study of tibial baseplate fracture after total knee arthroplasty. J Arthroplasty. 2005;20:101. doi: 10.1016/j.arth.2004.09.033. [DOI] [PubMed] [Google Scholar]
- 8.Abernethy P.J., Robinson C.M., Fowler R.M. Fracture of the metal tibial tray after kinematic total knee replacement. A common cause of early aseptic failure. J Bone Joint Surg [Br] 1996;78:220. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.