This cohort study investigates whether Tourette syndrome or chronic tic disorder are associated with an increased risk of experiencing violent assault and criminal convictions.
Key Points
Question
Are Tourette syndrome (TS) and chronic tic disorder (CTD) associated with an increased risk of experiencing violent assault and criminal convictions?
Findings
In this cohort study including 7791 individuals with TS or CTD diagnosed in specialist settings and 13 811 493 unaffected individuals, individuals with TS or CTD had a 2.2-fold increased risk of experiencing violent assault (including sexual assault), a 3.1-fold increased risk of violent crime convictions, and a 1.6-fold increased risk of nonviolent crime convictions.
Meaning
Findings suggest that most individuals with TS or CTD are not assaulted nor are perpetrators of crime; however, individuals with TS or CTD diagnosed in specialist settings were more likely to both experience violent assault and be perpetrators of violence.
Abstract
Importance
Tic disorders are associated with multiple social adversities, but little is known about the experience of violent assault (including sexual assault) and criminality in this group.
Objective
To establish if Tourette syndrome (TS) and chronic tic disorder (CTD) are associated with an increased risk of experiencing violent assault and criminal convictions.
Design, Setting, and Participants
In this cohort study, all individuals living in Sweden at any time between January 1, 1973, and December 31, 2013, were identified from Swedish nationwide health and administrative registers. Cox proportional hazards regression models were used to estimate the risk of violent assault and criminal convictions among people with TS or CTD, compared with the general population and unaffected full siblings. Data analyses were conducted between September 1 and October 22, 2021.
Exposures
The Swedish version of the International Classification of Diseases, Eighth Revision (ICD-8), ICD-9, and ICD-10 diagnoses of TS or CTD in the Swedish National Patient Register.
Main Outcomes and Measures
Records of sexual and nonsexual violent assault and death due to violent assaults were obtained from the National Patient Register and the Cause of Death Register, respectively. Convictions for violent and nonviolent criminal offenses were obtained from the Crime Register. Covariates included sex and birth year.
Results
The study cohort included 13 819 284 individuals living in Sweden between 1973 and 2013. A total of 7791 individuals with TS or CTD were identified (median [IQR] age at first diagnosis, 13.4 [10.0-21.8] years; 5944 [76%] male). Compared with unaffected individuals from the general population, people with TS or CTD had a 2-fold increased risk of experiencing any violent assault (sexual and nonsexual) (adjusted hazard ratio [aHR], 2.21; 95% CI, 2.00-2.43), a 3-fold increased risk of violent convictions (aHR, 3.13; 95% CI, 2.92-3.36), and a 1.6-fold increased risk of nonviolent crime convictions (aHR, 1.62; 95% CI, 1.54-1.71). Among people with TS or CTD, 37.0% (114 of 308; 95% CI, 31.6%-42.4%) of individuals who had experienced violent assault also had a violent crime conviction, compared with 17.9% (16 067 of 89 920; 95% CI, 17.6%-18.1%) in the general population. Exclusion of individuals with attention-deficit/hyperactivity disorder and substance use disorders partially attenuated the associations. Similarly, within-sibling models attenuated but did not eliminate the associations (any violent assault: aHR, 1.32; 95% CI, 1.08-1.61; violent crime: aHR, 2.23; 95% CI, 1.86-2.67; nonviolent crime: aHR, 1.34; 95% CI, 1.20-1.50).
Conclusions and Relevance
Results of this cohort study suggest that most individuals with TS or CTD are not assaulted nor are perpetrators of crime. However, individuals with TS or CTD diagnosed in specialist settings were more likely to both experience violent assault and be perpetrators of violence compared with the general population. The risk was highest in individuals with comorbid attention-deficit/hyperactivity disorder and substance use disorders. The increased risk found in specialty clinics will need to be better understood in the general population.
Introduction
Tourette syndrome (TS) and chronic tic disorder (CTD) often co-occur with other neuropsychiatric conditions, such as attention-deficit/hyperactivity disorder (ADHD),1 and are associated with multiple social adversities, including school failure, stigma, social rejection, difficulty establishing relationships, and suicidality.2,3,4,5,6,7,8 Most of what is known on the topic of bullying in TS or CTD originates from self- or parent-reported data.3,6,9 For example, in the 2016 to 2017 National Survey of Children’s Health, 56.1% of US children (104 of 186) with a parent-reported diagnosis of TS experienced bullying, 20.7% (39 of 186) experienced bullying perpetration, and 15.9% (30 of 186) experienced both.6 After adjusting for age, sex, and co-occurring psychiatric disorders, only the association of bullying remained statistically higher in children with TS compared with unaffected children.6
Much less is known about the experience of assault, such as sexual or other violent assaults causing serious injuries, and criminal offenses (ie, the perpetration of crime) in TS and CTD. Some individuals with highly comorbid TS or CTD experience sudden explosive outbursts,9 which may put them at higher risk to be assaulted or get criminal convictions. Case studies have described individuals with TS or CTD who had trouble with the law, sometimes owing to misunderstanding of the disorder’s symptoms, such as socially inappropriate behavior, obscene gestures, or rage attacks.10,11,12,13 A study of 217 tic disorder cases diagnosed in child and adolescent mental health services in Stockholm, Sweden, found that young people with TS had 2.2-fold higher odds of violent criminality than matched controls.14 Another Swedish study reported a greater than 2-fold higher risk of substance use–related criminal convictions in 7832 individuals with TS or CTD, compared with unaffected individuals from the general population.15 Taken together, the limited available evidence suggests that at least some individuals with TS or CTD may be more likely to both experience violent assault and be perpetrators of crime. Because most people with TS or CTD have psychiatric comorbidities1,16 and psychiatric disorders are robustly associated with both assault experience and perpetration of crime,17 it is important to understand if the associations are independent of psychiatric comorbidities.
It is widely believed that much of the social adversity experienced by individuals with TS or CTD is at least partially caused by misconceptions about the disorder by parents, teachers, peers, health care professionals, and the wider community.5,18 However, twin and family studies have reported that psychiatric disorders, violent crime, and the experience of violence aggregate in families19,20,21 and may share genetic risk factors.22,23 Therefore, it is critical that familial confounding is taken into account when studying the association between neuropsychiatric disorders, assault experience, and crime.24
We analyzed data from a large specialty cohort of prospectively observed patients with TS or CTD to (1) estimate the risk of different types of violent assault and criminal convictions in individuals with TS or CTD at the population level, (2) establish whether the association between TS or CTD, violent assault experience, and crime is explained by psychiatric comorbidity, and (3) investigate whether the association is explained by familial factors shared by siblings.
Methods
Data Sources
This cohort study used the unique Swedish national identification number25 to link Swedish nationwide health and administrative registers. Data on demographic characteristics, migration, and deaths were extracted from the Total Population Register26 and the Cause of Death Register.27 Information on diagnoses given in both inpatient (from 1969, with nationwide coverage for psychiatric disorders from 1973) and outpatient specialist services (since 2001) were retrieved from the National Patient Register. In this register,28 diagnoses are coded using the Swedish version of the International Classification of Diseases, Eighth Revision (ICD-8), ICD-9, and ICD-10. Medication data were collected from the Prescribed Drug Register, which covers all prescribed medications dispensed in pharmacies in Sweden since July 2005.29 Convictions for criminal offenses were collected from the nationwide Crime Register, with coverage since 1973. The Multigeneration Register allows for linking individuals born in Sweden from 1932 or registered as living in the country since 1961, with their parents, and we used the linkage to identify full siblings within the cohort.30
This study was approved by the Regional Ethical Review Board in Stockholm, and the need for informed consent was waived owing to the use of deidentified patient data. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines.
Study Population and Exposure Variables
The study cohort consisted of all individuals living in Sweden at any time between January 1, 1973, and December 31, 2013. We collected lifetime diagnoses of TS or CTD based on the Swedish versions of the ICD-8 (code 306.2), ICD-9 (code 307C), and ICD-10 (transient tic disorder, code F95.0; chronic motor or vocal tic disorder, code F95.1; Tourette syndrome, code F95.2; other tic disorders, code F95.8; or unspecified tic disorder, code F95.9). In line with prior research,2,31,32 exposure status was ascertained by using an algorithm that minimizes the inclusion of individuals with only transient tics using a minimum age of 3 years for diagnosis to avoid diagnostic misclassification. The Swedish ICD codes for TS or CTD diagnoses have excellent validity and reliability.33
The cohort was followed up from January 1, 1973, immigration to Sweden, or birth (age 15 years for conviction outcomes), whichever occurred last, until the date of the outcome, emigration from Sweden, death, or end of the study period (ie, December 31, 2013), whichever occurred first. People with follow-up ending before age 3 years were excluded. Data on race and ethnicity are not collected in the Swedish registers, and these data were not required by the funders of this study.
Outcomes
We defined violent assault as ICD diagnoses of injuries owing to assaults in the National Patient Register, as well as death resulting from an assault in the Cause of Death Register. Further, we examined sexual assault separately, which was defined as ICD diagnoses of sexual assault and abuse in the National Patient Register.
Criminal conviction outcomes from the Crime Register included violent crimes (eg, assault, robbery, sexual crimes, illegal threats) and nonviolent crimes, further divided into 4 subgroups: (1) alcohol- and drug-related crimes, including driving under the influence of alcohol or drugs and violations of the Narcotic Drugs Act, such as possession, manufacturing, trafficking, or sales of narcotics; (2) traffic-related crimes (eg, reckless driving, hit-and-run offenses, causing death or injury by driving, and moving violations); (3) property crimes (eg, theft, burglary); and (4) other nonviolent crimes. The minimum age for criminal responsibility in Sweden is 15 years. ICD codes are shown in eTable 1 in the Supplement.
Psychiatric Comorbidities
To investigate whether psychiatric comorbidities contributed to the associations under study, we included lifetime diagnoses of the following groups of psychiatric disorders from the National Patient Register: (1) ADHD, (2) anxiety- and stress-related disorders, (3) autism spectrum disorders, (4) conduct disorders, (5) depressive disorders, (6) obsessive-compulsive disorder, (7) psychotic disorders (schizophrenia spectrum disorders and bipolar disorder), and (8) substance use disorders. Individuals were also classified as having ADHD if they had ever been dispensed stimulant medication, which is used almost exclusively for the treatment of ADHD. ICD and medication codes are listed in eTable 2 in the Supplement. Many of these diagnostic codes have been validated with satisfactory results.33,34,35,36,37,38
Statistical Analyses
Primary Analyses
For aim 1, we used Cox proportional hazards regression, with age in years as the underlying time scale, to estimate the association of TS or CTD with assault and criminal conviction outcomes. We compared the risk of any experienced assault and, separately, sexual and nonsexual violent assault, as well as violent and nonviolent criminal convictions, in individuals with TS or CTD with that of unaffected individuals in the general population. We present estimates both for the full sample and separately for men and women. For aim 2, we repeated the main analyses excluding different groups of comorbid psychiatric disorders one at a time to establish whether the association of TS or CTD with the experience of violent assault and convictions for criminal offenses was explained by psychiatric comorbidities.
For aim 3, we investigated the association of TS or CTD with the experience of assault and criminal convictions in a subsample of full siblings within the cohort, identified as individuals who share both biological parents. We used Cox proportional hazards regression models stratified by sibling clusters, which rule out all factors constant within full siblings (ie, on average 50% of genetic factors and all shared environmental influences, eg, parental socioeconomic status). Such stratified models use information from clusters with discordance in the exposure to estimate the associations of TS or CTD with the assault and criminality outcomes within families. We excluded monozygotic twins and twins with unknown zygosity from the analyses.
Additional Analyses
To ensure that the observed associations were not biased owing to lack of data coverage (eg, exposure/outcome occurring before the start of the follow-up), we repeated the analyses for aim 1 in a subcohort of individuals born in Sweden after 1972 (ie, those who had complete follow-up from birth). Within this cohort, we also estimated the cumulative incidence of any assault experience and crime convictions for individuals with and without TS or CTD using Kaplan-Meier survival estimates under the assumption of no competing risks (estimated as 1 minus the Kaplan-Meier estimate of survival function). To investigate the potential overlap in assault experience and violent offenses, we calculated the proportion of those who experienced violent assault (both sexual and nonsexual) with those who also had a violent crime conviction, and vice versa, among people with TS or CTD and in the unaffected general population.
Because the National Patient Register does not contain information on TS or CTD severity, we repeated the analyses for aim 1 in a subcohort of individuals who had been diagnosed with TS or CTD at least twice after the age of 18 years, used as a proxy for severity and long-term persistence of TS or CTD into adulthood, and compared them with individuals without a TS or CTD diagnosis. This analysis excluded individuals diagnosed with TS or CTD who were no longer seen by a specialist after age 18 years as well as those who were evaluated only once after age 18 years. All models were adjusted for sex and birth year. Data management and analyses were performed between September 1 and October 22, 2021, using SAS, version 9.4 (SAS Institute) and Stata, version 15.1 (StataCorp), respectively.
Results
Descriptive Statistics
This cohort study included 13 819 284 individuals living in Sweden between 1973 and 2013. A total of 7791 individuals with TS or CTD were identified, of whom 5944 (76%) were male, and 1847 (24%) were female. The median (IQR) age at first TS or CTD diagnosis was 13.4 (10.0-21.8) years in the total cohort and 12.2 (9.5-16.7) years in those with follow-up from birth. Most people with TS or CTD had at least 1 comorbid psychiatric disorder (eTable 2 in the Supplement). The median (IQR) length of follow-up was 29.9 (16.8-41.0) years for violent assault outcomes and 18.4 (6.4-35.1) years for crime conviction outcomes.
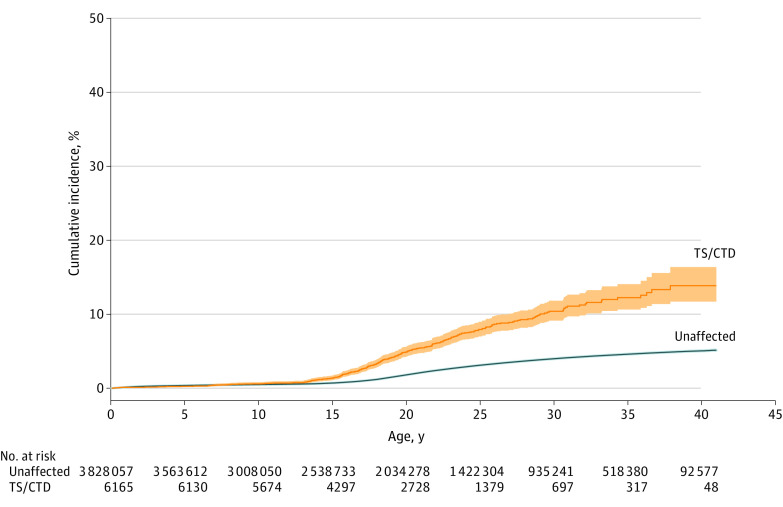
Risk of Violent Assault
People with TS or CTD had a 2-fold increased risk of any violent assault, compared with unaffected individuals from the general population (sex- and birth year–adjusted hazard ratio [aHR], 2.21; 95% CI, 2.00-2.43). Similar estimates were obtained for both sexual and nonsexual assault (Table 1). Based on nonoverlapping CIs, women with TS or CTD had a higher relative risk of experiencing any assault than men. In terms of absolute risks, the cumulative incidence of any violent assault reached 14% by the end of follow-up at age 41 years among people with TS or CTD, compared with 5% in the unaffected general population (Figure 1).
Table 1. Association of Tourette Syndrome or Chronic Tic Disorder With Violent Assault and Criminal Convictions.
| Outcome | People with Tourette syndrome or chronic tic disorder, No. (%)a | Rate per 10 000 person-yearsb | Unaffected general population, No. (%)c | Rate per 10 000 person-yearsb | Sex- and birth year–adjusted HR (95% CI) |
|---|---|---|---|---|---|
| Violent assault | |||||
| Any | 401 (5.2) | 28.3 | 254 805 (1.8) | 8.0 | 2.21 (2.00-2.43) |
| Men | 309 (5.2) | 28.3 | 146 000 (2.1) | 9.2 | 1.90 (1.70-2.12) |
| Women | 92 (5.0) | 28.4 | 108 805 (1.6) | 6.7 | 2.98 (2.43-3.66) |
| Sexual | 59 (0.8) | 4.0 | 45 594 (0.3) | 1.4 | 2.79 (2.16-3.60) |
| Men | 16 (0.3) | 1.4 | 16 206 (0.2) | 1.0 | 3.10 (1.90-5.07) |
| Women | 43 (2.3) | 11.5 | 29 388 (0.4) | 1.7 | 4.40 (3.26-5.94) |
| Nonsexuald | 354 (4.5) | 24.3 | 214 187 (1.6) | 6.6 | 2.14 (1.93-2.38) |
| Men | 296 (5.0) | 26.9 | 131 179 (1.9) | 8.2 | 1.88 (1.68-2.11) |
| Women | 58 (3.1) | 16.9 | 83 008 (1.2) | 5.0 | 2.57 (1.99-3.32) |
| Conviction for criminal offense | |||||
| Violente | 769 (13.1) | 234.5 | 322 720 (2.6) | 21.6 | 3.13 (2.92-3.36) |
| Men | 691 (15.7) | 310.5 | 284 990 (5.0) | 40.2 | 3.04 (2.82-3.28) |
| Women | 78 (5.3) | 64.0 | 37 730 (0.6) | 3.6 | 5.77 (4.62-7.21) |
| Nonviolent | |||||
| Any | 1532 (26.1) | 925.4 | 1 757 905 (14.3) | 178.5 | 1.62 (1.54-1.71) |
| Men | 1305 (29.7) | 1178.1 | 1 341 662 (21.6) | 308.2 | 1.61 (1.53-1.71) |
| Women | 227 (15.4) | 358.9 | 416 243 (6.8) | 53.3 | 2.08 (1.82-2.37) |
| Alcohol- or drug-related | 595 (10.1) | 242.1 | 436 651 (3.5) | 35.2 | 2.10 (1.94-2.27) |
| Men | 532 (12.1) | 310.9 | 381 178 (6.1) | 64.0 | 2.03 (1.86-2.21) |
| Women | 63 (4.3) | 88.1 | 55 473 (0.9) | 7.5 | 3.81 (2.97-4.88) |
| Traffic crime | 557 (9.5) | 176.4 | 769 370 (6.2) | 50.2 | 1.45 (1.34-1.58) |
| Men | 515 (11.7) | 239.2 | 654 386 (10.6) | 91.2 | 1.39 (1.28-1.52) |
| Women | 42 (2.9) | 35.5 | 114 984 (1.9) | 10.6 | 1.88 (1.39-2.54) |
| Property crime | 753 (12.8) | 301.8 | 567 003 (4.6) | 47.8 | 2.06 (1.92-2.21) |
| Men | 613 (13.9) | 364.9 | 381 366 (6.2) | 74.8 | 2.13 (1.97-2.31) |
| Women | 140 (9.5) | 160.3 | 185 637 (3.0) | 21.7 | 2.33 (1.98-2.75) |
| Otherf | 964 (16.4) | 371.7 | 885 987 (7.2) | 65.6 | 2.00 (1.87-2.13) |
| Men | 863 (19.6) | 486.4 | 727 099 (11.7) | 116.5 | 1.96 (1.83-2.10) |
| Women | 101 (6.9) | 114.6 | 158 888 (2.6) | 16.6 | 2.52 (2.07-3.06) |
Abbreviation: HR, hazard ratio.
Violent assault outcomes: n = 7791; conviction outcomes: n = 5876. People with follow-up ending before age 15 years were excluded from conviction analyses.
Assault outcomes: n = 13 811 493; conviction outcomes: n = 12 333 904. People with follow-up ending before age 15 years were excluded from conviction analyses.
The rate was calculated based on the total number of assaults/convictions for the entire follow-up period (where follow-up ended on emigration, December 31, 2013, or death), ie, accounting for repeated assault/offending for each individual. To avoid double counting the same event, hospital/outpatient visit for assault was included only if the elapsed time between 2 consecutive visits was at least 1 year.
Excluding sexual assault.
Including sexual crime convictions.
Other nonviolent crime, eg, fraud, embezzlement, vandalism, and crimes against public activity or order.
Figure 1. Any Violent Assault in Individuals With Tourette Syndrome (TS) or Chronic Tic Disorder (CTD).
Cumulative incidence under the assumption of no competing risks estimated as 1 minus the Kaplan-Meier estimate of survival function for any violent assault in individuals with TS or CTD and unaffected individuals from the general population in the subsample of 3 834 222 individuals followed up from birth. The shaded areas indicate 95% CIs.
When omitting different groups of individuals with comorbid psychiatric disorders from the cohort, one at a time, we found that exclusion of people with ADHD attenuated, but did not completely eliminate the association between TS or CTD and any violent assault experience (aHR, 1.56; 95% CI, 1.32-1.85) (Table 2). Excluding other comorbidities did not affect the association. As shown in Table 3, the associations were attenuated, but the risks remained significantly elevated in the within-sibling analysis (aHR, 1.32; 95% CI, 1.08-1.61).
Table 2. Association of Tourette Syndrome or Chronic Tic Disorder With Violent Assault and Criminal Convictions When Excluding Psychiatric Comorbidities.
| Outcome | Sex- and birth rate–adjusted HR (95% CI) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Without exclusion | Exclusion | ||||||||
| ADHD | Anxiety disorders | Autism spectrum disorders | Conduct disorders | Depressive disorders | OCD | Psychotic disorders | SUDs | ||
| Any violent assault | 2.21 (2.00-2.43) | 1.56 (1.32-1.85)a | 1.98 (1.73-2.26) | 2.29 (2.04-2.56) | 2.11 (1.90-2.34) | 2.04 (1.81-2.31) | 2.21 (1.98-2.47) | 2.08 (1.86-2.32) | 1.85 (1.63-2.10) |
| Crime conviction | |||||||||
| Violent | 3.13 (2.92-3.36) | 2.20 (1.95-2.48)a | 2.83 (2.57-3.11) | 3.04 (2.80-3.31) | 2.84 (2.63-3.07) | 3.13 (2.88-3.41) | 3.14 (2.90-3.40) | 2.93 (2.71-3.18) | 2.66 (2.42-2.92) |
| Any nonviolent | 1.62 (1.54-1.71) | 1.15 (1.06-1.24)a | 1.40 (1.31-1.50)a | 1.68 (1.59-1.78) | 1.54 (1.46-1.62) | 1.54 (1.45-1.63) | 1.65 (1.56-1.74) | 1.58 (1.50-1.67) | 1.34 (1.26-1.42)a |
| Alcohol- or drug-related | 2.10 (1.94-2.27) | 1.29 (1.12-1.49)a | 1.81 (1.62-2.02) | 2.29 (2.09-2.51) | 1.98 (1.82-2.16) | 1.91 (1.73-2.12) | 2.14 (1.96-2.34) | 2.01 (1.84-2.21) | 1.39 (1.23-1.58)a |
| Traffic | 1.45 (1.34-1.58) | 1.08 (0.96-1.23)a | 1.31 (1.18-1.47) | 1.62 (1.48-1.77) | 1.41 (1.30-1.54) | 1.42 (1.29-1.57) | 1.53 (1.40-1.67) | 1.50 (1.37-1.64) | 1.24 (1.11-1.37) |
| Property | 2.06 (1.92-2.21) | 1.35 (1.20-1.53)a | 1.79 (1.62-1.97) | 2.12 (1.95-2.30) | 1.95 (1.81-2.11) | 2.02 (1.85-2.20) | 2.12 (1.96-2.30) | 1.97 (1.82-2.14) | 1.58 (1.44-1.75)a |
| Other nonviolentb | 2.00 (1.87-2.13) | 1.37 (1.24-1.52)a | 1.72 (1.58-1.88) | 2.03 (1.88-2.18) | 1.88 (1.76-2.01) | 1.92 (1.77-2.07) | 2.06 (1.92-2.21) | 1.91 (1.78-2.05) | 1.57 (1.44-1.70)a |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; HR, hazard ratio; OCD, obsessive-compulsive disorder; SUD, substance use disorder.
Coefficients indicate attenuation in the estimate compared with the estimate without exclusion for comorbid conditions.
Other nonviolent crime, eg, fraud, embezzlement, vandalism, and crimes against public activity or order.
Table 3. Association of Tourette Syndrome or Chronic Tic Disorder With Violent Assault and Criminal Convictions Within Siblings.
| Outcomea | Sex- and birth year–adjusted HR (95% CI) | |
|---|---|---|
| Between-individual | Within-siblings | |
| Any assault | 2.21 (2.00-2.43) | 1.32 (1.08-1.61) |
| Crime conviction | ||
| Violent | 3.13 (2.92-3.36) | 2.23 (1.86-2.67) |
| Any nonviolent | 1.62 (1.54-1.71) | 1.34 (1.20-1.50) |
| Alcohol- or drug-related | 2.10 (1.94-2.27) | 1.62 (1.34-1.96) |
| Traffic | 1.45 (1.34-1.58) | 1.46 (1.22-1.75) |
| Property | 2.06 (1.92-2.21) | 1.48 (1.28-1.71) |
| Other nonviolentb | 2.00 (1.87-2.13) | 1.56 (1.35-1.80) |
Abbreviation: HR, hazard ratio.
Assault outcomes: families, n = 2 619 160; individuals with Tourette syndrome or chronic tic disorder, n = 5369; unaffected, n = 6 594 830. Conviction outcomes: families, n = 2 138 574; individuals with Tourette syndrome or chronic tic disorder, n = 3732; unaffected, n = 5 435 939.
Other nonviolent crime, eg, fraud, embezzlement, vandalism, and crimes against public activity or order.
Risk of Crime Convictions
We found TS or CTD to be associated with a 3-fold increased risk of violent crime convictions (aHR, 3.13; 95% CI, 2.92-3.36). Nonoverlapping CIs for the estimates suggest that women with TS or CTD had a higher relative risk of convictions for violent offenses than did men (Table 1). Cumulative incidence showed 22% of individuals with TS or CTD having a violent crime conviction by the age of 41 years, compared with 5% in the unaffected general population (Figure 2A).
Figure 2. Violent and Nonviolent Crime Conviction in Individuals With Tourette Syndrome (TS) or Chronic Tic Disorder (CTD).
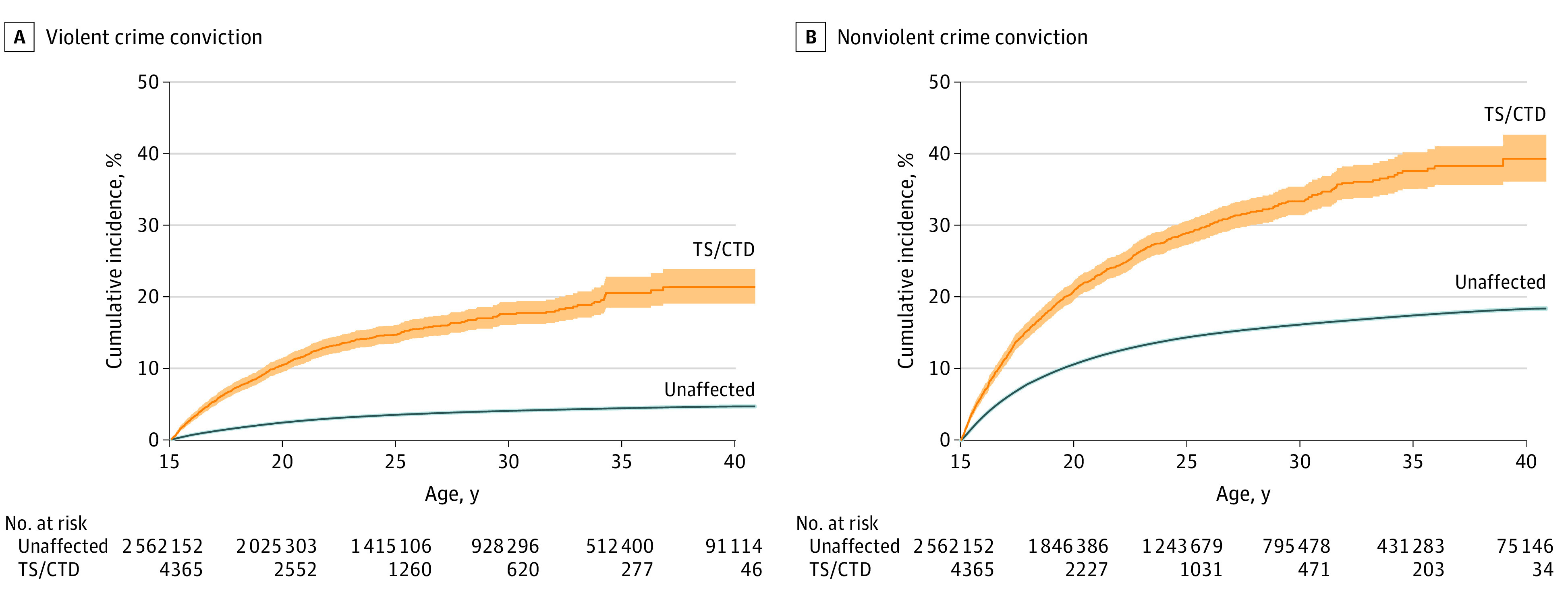
Cumulative incidence under the assumption of no competing risks estimated as 1 minus the Kaplan-Meier estimate of survival function for any violent (A) and nonviolent (B) crime convictions in individuals with TS or CTD and unaffected individuals from the general population in the subsample of 2 566 517 individuals followed up from birth. The shaded areas indicate 95% CIs.
TS or CTD was associated with a 1.6-fold (aHR, 1.62; 95% CI, 1.54-1.71) increased risk of convictions for any nonviolent offenses (Table 1). In absolute terms, the cumulative incidence of any nonviolent crime conviction was 39% in individuals with TS or CTD, compared with 18% in the general population (Figure 2B).
The association of TS or CTD with violent crime convictions attenuated when individuals with ADHD were excluded, but a 2-fold increased risk persisted even after exclusion (aHR, 2.20; 95% CI, 1.95-2.48) (Table 2). Excluding other comorbidities did not affect the association. A similar pattern emerged for nonviolent convictions, where removing individuals with ADHD partially attenuated the associations, and in the case of convictions for traffic offenses, eliminated the association entirely. Comorbid substance use disorders contributed significantly to the association of TS or CTD with alcohol- and drug-related crime (aHR, 1.39; 95% CI, 1.23-1.58), property crime (aHR, 1.58; 95% CI, 1.44-1.75), and other nonviolent crimes (aHR, 1.57; 95% CI, 1.44-1.70).
Table 3 shows that, when the association of TS or CTD with violent crime convictions was estimated within siblings, the association was reduced, but remained elevated with a more than 2-fold increased risk (aHR, 2.23; 95% CI, 1.86-2.67). A similar pattern was observed for convictions for nonviolent criminal offenses, although the estimates were not as high as those seen in violent offenses (aHR, 1.34; 95% CI, 1.20-1.50).
Additional Analyses
When the data were restricted to a subsample of individuals with follow-up from birth, the association of TS or CTD with violent assault and conviction outcomes remained similar to the main results (eTable 3 in the Supplement). Among people with TS or CTD, 37.0% (114 of 308; 95% CI, 31.6%-42.4%) of individuals who had experienced any violent assault (sexual and nonsexual) also had a violent crime conviction. The corresponding proportion in the general population was 17.9% (16 067 of 89 920; 95% CI, 17.6%-18.1%). Conversely, 21.3% (114 of 536; 95% CI, 17.8%-24.7%) of those convicted of violent offenses also experienced violence among people with TS or CTD. The corresponding proportion in the general population was 18.6% (16 067 of 86 498; 95% CI, 18.3%-18.8%).
We also estimated the association with an alternative definition for TS or CTD, aiming to capture individuals with a persistent, severe tic disorder. Although some of the point estimates were slightly higher than those observed in the main analysis, the CIs overlapped (eTable 4 in the Supplement).
Discussion
Results of this cohort study suggest that individuals with TS or CTD had a 2-fold increased risk of experiencing any violent assault (sexual and nonsexual), compared with unaffected individuals from the general population. Exclusion of psychiatric comorbidities, including ADHD, and controlling for unmeasured familial confounders attenuated but did not eliminate the risk. The cumulative incidence was 14% in those followed up from birth, compared with 5% in the general population; patient and control groups started to diverge already before age 15 years, indicating early vulnerability to experiencing violent assault. These results expand those of the previous literature on self- or parent-reported bullying3,6,39 by providing new objective data on more serious assault outcomes requiring medical attention.
Results suggest that individuals with TS or CTD had a 3-fold increased risk of violent crime convictions, which decreased to approximately 2-fold after the exclusion of individuals with comorbid ADHD and in the sibling comparison models. These results confirm the results of a previous, much smaller register-based study.14 The risk of nonviolent crime convictions (including alcohol- or drug-related crimes, traffic offenses, property crime, and other nonviolent crimes) was comparatively smaller and was substantially attenuated (no longer significant for traffic convictions) when individuals with comorbid ADHD and substance use disorders were excluded from the cohort. In absolute terms, 22% of people with TS or CTD who were followed up from birth had a violent crime conviction by age 41 years (vs 5% of the general population). Similarly, 39% had a conviction for nonviolent crime (vs 18% in the general population). Thus, although most individuals with TS or CTD were not involved in crime, those with comorbid ADHD and substance use disorders may represent a subgroup at greater risk of being involved in crime.
Results of this study further showed that, in line with the previous literature on psychiatric disorders in general,17 violent assault and perpetration of crime were not independent phenomena. In our study, 37.0% of the individuals with TS or CTD who had experienced any violent assault also had a violent crime conviction. These findings contribute to our understanding of the origin of disruptive behavior and crime in TS and CTDs.
Further, although men had higher absolute risks of experiencing violent assault and crime convictions, our results showed that the relative risks were highest among women with TS or CTD, probably owing to the lower rates of these outcomes among women from the general population. The reasons for these sex differences are unclear and require further study.
These results have important clinical, social, and medicolegal implications. From a clinical perspective, early detection and management of TS and CTD and associated comorbidities are key. It is paramount to improve access to specialist multidisciplinary teams and to evidence-based treatments, particularly behavior therapy, for TS and CTD.40 From a social perspective, more needs to be done to support patient organizations in their efforts to educate the general public about TS and CTD and to reduce the considerable stigma and misunderstanding still associated with these disorders.4,5 From a medicolegal perspective, it is important to increase awareness within the legal community on the nature of TS and CTD and associated comorbidities. When appropriate, legal proceedings should involve medical experts who can advise on diminished legal responsibility issues (ie, to help determine if the person’s behavior was deliberately intended to cause harm). A better understanding of the peculiarities of TS and CTD may prevent unwarranted convictions.10
Strengths and Limitations
The main strengths of this study were the large cohort of individuals with TS and CTD who were followed up for a median of 3 decades, thereby providing ample opportunity to capture the outcomes of interest. We systematically accounted for psychiatric comorbidities and adjusted for unmeasured familial confounding. Surveillance bias was likely to be minimal given the seriousness of the outcomes and the fact that the Crime Register is independent from health care.
The study had some limitations. First, the patients were seen in specialist settings, limiting the generalizability of the findings to milder forms of TS and CTD. Second, the violent assault outcomes were serious events requiring medical care, which means that our study could not detect milder or unreported forms of assault, nor did it capture crimes that did not result in convictions. Third, we did not have detailed information on tic symptom severity. We used a proxy for the chronicity of tics, which did not show stronger associations with the outcomes under study. Finally, the sibling comparisons could only adjust for approximately 50% of the shared genetic risks, leaving room for potential residual genetic confounding.
Conclusions
In this cohort study, results suggest that individuals with TS or CTD diagnosed in specialist settings were more likely to both experience violent assault and be perpetrators of violence. The risk was highest in individuals with comorbid ADHD and substance use disorders. Future studies should focus on understanding the etiology of such serious outcomes in an effort to prevent the experience of assault or criminal convictions in individuals with TS or CTD.
eTable 1. International Classification of Diseases Codes for Violent Assault Outcomes and Types of Criminal Offense Outcomes
eTable 2. International Classification of Diseases Codes and Frequencies for Psychiatric Comorbidities
eTable 3. Association of Tourette Syndrome/Chronic Tic Disorder With Violent Assault and Criminal Convictions Restricted to a Subcohort With Follow-up From Birth
eTable 4. Association of Persistent Tourette Syndrome/Chronic Tic Disorder With Violent Assault and Criminal Convictions
References
- 1.Hirschtritt ME, Lee PC, Pauls DL, et al. ; Tourette Syndrome Association International Consortium for Genetics . Lifetime prevalence, age of risk, and genetic relationships of comorbid psychiatric disorders in Tourette syndrome. JAMA Psychiatry. 2015;72(4):325-333. doi: 10.1001/jamapsychiatry.2014.2650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pérez-Vigil A, Fernández de la Cruz L, Brander G, et al. Association of Tourette syndrome and chronic tic disorders with objective indicators of educational attainment: a population-based sibling comparison study. JAMA Neurol. 2018;75(9):1098-1105. doi: 10.1001/jamaneurol.2018.1194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zinner SH, Conelea CA, Glew GM, Woods DW, Budman CL. Peer victimization in youth with Tourette syndrome and other chronic tic disorders. Child Psychiatry Hum Dev. 2012;43(1):124-136. doi: 10.1007/s10578-011-0249-y [DOI] [PubMed] [Google Scholar]
- 4.Malli MA, Forrester-Jones R, Murphy G. Stigma in youth with Tourette syndrome: a systematic review and synthesis. Eur Child Adolesc Psychiatry. 2016;25(2):127-139. doi: 10.1007/s00787-015-0761-x [DOI] [PubMed] [Google Scholar]
- 5.Cox JH, Nahar A, Termine C, et al. Social stigma and self-perception in adolescents with Tourette syndrome. Adolesc Health Med Ther. 2019;10:75-82. doi: 10.2147/AHMT.S175765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Charania SN, Danielson ML, Claussen AH, Lebrun-Harris LA, Kaminski JW, Bitsko RH. Bullying victimization and perpetration among US children with and without Tourette syndrome. J Dev Behav Pediatr. 2022;43(1):23-31. doi: 10.1097/DBP.0000000000000975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Storch EA, Hanks CE, Mink JW, et al. Suicidal thoughts and behaviors in children and adolescents with chronic tic disorders. Depress Anxiety. 2015;32(10):744-753. doi: 10.1002/da.22357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fernández de la Cruz L, Rydell M, Runeson B, et al. Suicide in Tourette and chronic tic disorders. Biol Psychiatry. 2017;82(2):111-118. doi: 10.1016/j.biopsych.2016.08.023 [DOI] [PubMed] [Google Scholar]
- 9.Budman CL, Bruun RD, Park KS, Lesser M, Olson M. Explosive outbursts in children with Tourette disorder. J Am Acad Child Adolesc Psychiatry. 2000;39(10):1270-1276. doi: 10.1097/00004583-200010000-00014 [DOI] [PubMed] [Google Scholar]
- 10.Jankovic J, Kwak C, Frankoff R. Tourette syndrome and the law. J Neuropsychiatry Clin Neurosci. 2006;18(1):86-95. doi: 10.1176/jnp.18.1.86 [DOI] [PubMed] [Google Scholar]
- 11.Fatih P, Mutluer T, Shabsog M, et al. Sociolegal consequences of Tourette syndrome and its comorbidities: a case study and review of the literature. J Forensic Leg Med. 2020;71:101937. doi: 10.1016/j.jflm.2020.101937 [DOI] [PubMed] [Google Scholar]
- 12.Porta M, Servello D, Dell’Osso B, Dina CZ, Bona A, Alleva GC. Critical aspects in the legal defence of patients with Tourette syndrome: an Italian case series. Int J Law Psychiatry. 2018;61:1-5. doi: 10.1016/j.ijlp.2018.08.003 [DOI] [PubMed] [Google Scholar]
- 13.Nunes FT, Telles LEB. Tourette disorder and sexual offenses: psychiatric-forensic considerations. Br J Psychiatry. 2019;41(4):364-365. doi: 10.1590/1516-4446-2019-0420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lundström S, Forsman M, Larsson H, et al. Childhood neurodevelopmental disorders and violent criminality: a sibling control study. J Autism Dev Disord. 2014;44(11):2707-2716. doi: 10.1007/s10803-013-1873-0 [DOI] [PubMed] [Google Scholar]
- 15.Virtanen S, Sidorchuk A, Fernández de la Cruz L, et al. Association of Tourette syndrome and chronic tic disorder with subsequent risk of alcohol- or drug-related disorders, criminal convictions, and death: a population-based family study. Biol Psychiatry. 2021;89(4):407-414. doi: 10.1016/j.biopsych.2020.09.014 [DOI] [PubMed] [Google Scholar]
- 16.Freeman RD; Tourette Syndrome International Database Consortium . Tic disorders and ADHD: answers from a worldwide clinical dataset on Tourette syndrome. Eur Child Adolesc Psychiatry. 2007;16(suppl 1):15-23. doi: 10.1007/s00787-007-1003-7 [DOI] [PubMed] [Google Scholar]
- 17.Sariaslan A, Arseneault L, Larsson H, Lichtenstein P, Fazel S. Risk of subjection to violence and perpetration of violence in persons with psychiatric disorders in Sweden. JAMA Psychiatry. 2020;77(4):359-367. doi: 10.1001/jamapsychiatry.2019.4275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eapen V, Snedden C, Črnčec R, Pick A, Sachdev P. Tourette syndrome, comorbidities and quality of life. Aust N Z J Psychiatry. 2016;50(1):82-93. doi: 10.1177/0004867415594429 [DOI] [PubMed] [Google Scholar]
- 19.Fisher HL, Caspi A, Moffitt TE, et al. Measuring adolescents’ exposure to victimization: the Environmental Risk (E-Risk) Longitudinal Twin Study. Dev Psychopathol. 2015;27(4 pt 2):1399-1416. doi: 10.1017/S0954579415000838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Frisell T, Lichtenstein P, Långström N. Violent crime runs in families: a total population study of 12.5 million individuals. Psychol Med. 2011;41(1):97-105. doi: 10.1017/S0033291710000462 [DOI] [PubMed] [Google Scholar]
- 21.Whiting D, Lichtenstein P, Fazel S. Violence and mental disorders: a structured review of associations by individual diagnoses, risk factors, and risk assessment. Lancet Psychiatry. 2021;8(2):150-161. doi: 10.1016/S2215-0366(20)30262-5 [DOI] [PubMed] [Google Scholar]
- 22.Pettersson E, Larsson H, Lichtenstein P. Common psychiatric disorders share the same genetic origin: a multivariate sibling study of the Swedish population. Mol Psychiatry. 2016;21(5):717-721. doi: 10.1038/mp.2015.116 [DOI] [PubMed] [Google Scholar]
- 23.Ghirardi L, Kuja-Halkola R, Pettersson E, et al. Neurodevelopmental disorders and subsequent risk of violent victimization: exploring sex differences and mechanisms. Psychol Med. Published online September 1, 2021. doi: 10.1017/S0033291721003093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fazel S, Sariaslan A. Victimization in people with severe mental health problems: the need to improve research quality, risk stratification and preventive measures. World Psychiatry. 2021;20(3):437-438. doi: 10.1002/wps.20908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ludvigsson JF, Otterblad-Olausson P, Pettersson BU, Ekbom A. The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. Eur J Epidemiol. 2009;24(11):659-667. doi: 10.1007/s10654-009-9350-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ludvigsson JF, Almqvist C, Bonamy AKE, et al. Registers of the Swedish total population and their use in medical research. Eur J Epidemiol. 2016;31(2):125-136. doi: 10.1007/s10654-016-0117-y [DOI] [PubMed] [Google Scholar]
- 27.Brooke HL, Talbäck M, Hörnblad J, et al. The Swedish cause of death register. Eur J Epidemiol. 2017;32(9):765-773. doi: 10.1007/s10654-017-0316-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ludvigsson JF, Andersson E, Ekbom A, et al. External review and validation of the Swedish national inpatient register. BMC Public Health. 2011;11:450. doi: 10.1186/1471-2458-11-450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wettermark B, Hammar N, Fored CM, et al. The new Swedish Prescribed Drug Register—opportunities for pharmacoepidemiological research and experience from the first 6 months. Pharmacoepidemiol Drug Saf. 2007;16(7):726-735. doi: 10.1002/pds.1294 [DOI] [PubMed] [Google Scholar]
- 30.Ekbom A. The Swedish multigeneration register. Methods Mol Biol. 2011;675:215-220. doi: 10.1007/978-1-59745-423-0_10 [DOI] [PubMed] [Google Scholar]
- 31.Brander G, Isomura K, Chang Z, et al. Association of Tourette syndrome and chronic tic disorder with metabolic and cardiovascular disorders. JAMA Neurol. 2019;76(4):454-461. doi: 10.1001/jamaneurol.2018.4279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mataix-Cols D, Brander G, Chang Z, et al. Serious transport accidents in Tourette syndrome or chronic tic disorder. Mov Disord. 2021;36(1):188-195. doi: 10.1002/mds.28301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rück C, Larsson KJ, Lind K, et al. Validity and reliability of chronic tic disorder and obsessive-compulsive disorder diagnoses in the Swedish National Patient Register. BMJ Open. 2015;5(6):e007520. doi: 10.1136/bmjopen-2014-007520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vilaplana-Pérez A, Isung J, Krig S, et al. Validity and reliability of social anxiety disorder diagnoses in the Swedish National Patient Register. BMC Psychiatry. 2020;20(1):242. doi: 10.1186/s12888-020-02644-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hollander AC, Askegård K, Iddon-Escalante C, Holmes EA, Wicks S, Dalman C. Validation study of randomly selected cases of PTSD diagnoses identified in a Swedish regional database compared with medical records: is the validity sufficient for epidemiological research? BMJ Open. 2019;9(12):e031964. doi: 10.1136/bmjopen-2019-031964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Idring S, Rai D, Dal H, et al. Autism spectrum disorders in the Stockholm Youth Cohort: design, prevalence and validity. PLoS One. 2012;7(7):e41280. doi: 10.1371/journal.pone.0041280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dalman Ch, Broms J, Cullberg J, Allebeck P. Young cases of schizophrenia identified in a national inpatient register—are the diagnoses valid? Soc Psychiatry Psychiatr Epidemiol. 2002;37(11):527-531. doi: 10.1007/s00127-002-0582-3 [DOI] [PubMed] [Google Scholar]
- 38.Sellgren C, Landén M, Lichtenstein P, Hultman CM, Långström N. Validity of bipolar disorder hospital discharge diagnoses: file review and multiple register linkage in Sweden. Acta Psychiatr Scand. 2011;124(6):447-453. doi: 10.1111/j.1600-0447.2011.01747.x [DOI] [PubMed] [Google Scholar]
- 39.Storch EA, Murphy TK, Chase RM, et al. Peer victimization in youth with Tourette syndrome and chronic tic disorder: relations with tic severity and internalizing symptoms. J Psychopathol Behav Assess. 2007;29(4):211-219. doi: 10.1007/s10862-007-9050-4 [DOI] [Google Scholar]
- 40.Cuenca J, Glazebrook C, Kendall T, et al. Perceptions of treatment for tics among young people with Tourette syndrome and their parents: a mixed methods study. BMC Psychiatry. 2015;15:46. doi: 10.1186/s12888-015-0430-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. International Classification of Diseases Codes for Violent Assault Outcomes and Types of Criminal Offense Outcomes
eTable 2. International Classification of Diseases Codes and Frequencies for Psychiatric Comorbidities
eTable 3. Association of Tourette Syndrome/Chronic Tic Disorder With Violent Assault and Criminal Convictions Restricted to a Subcohort With Follow-up From Birth
eTable 4. Association of Persistent Tourette Syndrome/Chronic Tic Disorder With Violent Assault and Criminal Convictions