Abstract
Background
Angiotensin‐converting enzyme inhibitors (ACEis) and angiotensin receptor blockers (ARBs) are widely used in peritoneal dialysis (PD) patients, yet controversy exists about their impact on residual kidney function.
Objectives
This review aimed to evaluate the benefits and harms of ACEis and ARBs for preserving residual kidney function in PD patients.
Search methods
The Cochrane Renal Group's specialised register, Cochrane Register of Controlled Trials (CENTRAL), MEDLINE, EMBASE (OvidSP interface), Chinese Biomedical Literature Database (CBM), China National Knowledge Infrastructure (CNKI) and other resources were searched by applying a prespecified comprehensive search strategy. Date of last search: 01 May 2014.
Selection criteria
Randomised controlled trials (RCTs) and quasi‐RCTs comparing ACEis or ARBs with placebo, other antihypertensive drugs or each other in PD patients were included.
Data collection and analysis
Screening, selection, data extraction and quality assessments for each retrieved article were carried out by two authors using standardised forms. Authors were contacted when published data were incomplete. Statistical analyses were performed using the random effects model and results expressed as risk ratio (RR) with 95% confidence intervals (CI). Heterogeneity among studies was explored using the Cochran Q statistic and the I² test, subgroup analyses and random effects meta‐regression.
Main results
Six open‐label studies (257 patients) were identified. One study compared ACEi with other antihypertensive drugs, three compared ARBs with other antihypertensive drugs, and two studies compared an ARB with an ACEi. Long‐term use (≥ 12 months) of an ARB showed significantly benefit of preserving residual kidney function in continuous ambulatory PD (CAPD) patients (MD 1.11 mL/min/1.73 m², 95% CI 0.38 to 1.83), although there was no significant benefit when an ARB were used short‐term (≤ six months). One study showed that compared with other antihypertensive drugs, long‐term use (12 months) of the ACEi ramipril showed a significant reduction in the decline of residual kidney function in patients on CAPD (MD ‐0.93 mL/min/1.73m², 95% CI ‐0.75 to ‐0.11), and delayed the progression to complete anuria (RR 0.64, 95% CI 0.41 to 0.99). There was no significant difference in serum potassium, urinary protein excretion, Kt/V, weekly creatinine clearance and blood pressure for ARBs versus other antihypertensive drugs. Compared with other antihypertensive drugs, ramipril showed no difference in mortality and cardiovascular events. Compared with an ACEi, ARBs did not show any difference in residual kidney function.
The selection bias assessment was low in four studies and unclear in two. Five studies were open‐label; however the primary outcome (residual kidney function) was obtained objectively from laboratory tests, and were not likely to be influenced by the lack of blinding. Reporting bias was unclear in all six studies.
Authors' conclusions
Compared with other antihypertensive drugs, long‐term use (≥ 12 months) of ACEis or ARBs showed additional benefits of preserving residual kidney function in CAPD patients. There was no significant difference on residual kidney function preservation between ARBs and ACEis. However, limited by the small number of RCTs enrolling small number of participants, there is currently insufficient evidence to support the use of an ACEi or an ARB as first line antihypertensive therapy in PD patients.
Plain language summary
Angiotensin‐converting enzyme inhibitors and angiotensin‐II receptor blockers for preserving residual kidney function in peritoneal dialysis patients
Residual kidney function plays a key role in the health and quality of life of patients on peritoneal dialysis (PD). Better preservation of residual kidney function is associated with decreased mortality, even at 1 mL/min of residual glomerular filtration rate (GFR), which is associated with a nearly 50% reduction in mortality rate. Two kinds of antihypertensive drugs, angiotensin‐converting enzyme inhibitors (ACEis) and angiotensin‐II receptor blockers (ARBs), are frequently prescribed for PD patients (primarily to control hypertension or heart failure), and could provide significant cardiovascular benefit for ESKD patients. Nowadays, while ACEis and ARBs use is advocated in PD patients, the supporting evidence is still unclear. However studies have focused on heart protection rather than residual kidney function. The aim of this review was to assess the benefits and harms of ACEis and ARBs therapy for preserving residual kidney function in PD patients. Six studies (257 patients) were included (three ARB studies, one ACEi study and ACEi versus ARB studies). Long‐term use (12 months or more) of an ARB showed a significant benefit in preserving residual kidney function in continuous ambulatory PD (CAPD) patients compared with other antihypertensive drugs, although there was no significant benefit when an ARB were used for less than six months). One study showed that compared with other antihypertensive drugs, long‐term use of the ACEi ramipril showed a significant reduction in the decline of residual kidney function in patients on CAPD as well as anuria rate. While dizziness and cough are the main adverse events when an ACEi is used, only one study comparing an ARB with an ACEi reported this outcome and no significant difference between the two groups were found. While the use of an ARB or an ACEi may both be useful in preserving residual kidney function, the small number of studies and small number of patients enrolled means there is currently insufficient evidence to support the use of an ACEi or an ARB as first line antihypertensive therapy in PD patients.
Summary of findings
Summary of findings for the main comparison. Angiotensin receptor blockers (ARBs) versus conventional therapy for preserving residual kidney function in peritoneal dialysis patients.
| ARBs versus conventional therapy for preserving residual kidney function in peritoneal dialysis patients | ||||||
|
Patient or population: patients receiving PD Settings: outpatient Intervention: ARB Comparison: Conventional therapy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Conventional therapy | ARBs | |||||
| Residual kidney function (3 months) | Mean across control group was 3.06 mL/min/1.73 m² | Mean was on average 0.44 mL/min/1.73 m² lower (95% Cl ‐1.53 to 0.65) in the ARB group | 44 (1) | ⊕⊕⊕⊝ moderate | ||
| Residual kidney function (6 months) | Mean across control group was 2.26 mL/min/1.73 m² | Mean was on average 0.20 mL/min/1.73 m² lower (95% Cl ‐1.01 to 0.61) in the ARB group | 44 (1) | ⊕⊕⊕⊝ moderate | ||
| Residual kidney function (≥ 12 months) | Mean across control groups ranged from 1.04 to 2.8 mL/min/1.73 m² | Mean was on average 1.11 mL/min/1.73 m² lower (95% Cl 0.38 to 1.83) in the ARB groups | 110 (3) | ⊕⊕⊕⊝ moderate | ||
| Residual kidney function (12 months) | Mean across control group was 1.04 mL/min/1.73 m² | Mean was on average 0.64 mL/min/1.73 m² higher (95% Cl 0.19 to 1.19) in the ARB group | 44 (1) | ⊕⊕⊕⊝ moderate | ||
| Residual kidney function (24 months) | Mean across control groups ranged from 2.57 to 2.8 mL/min/1.73 m² | Mean was on average1.49 mL/min/1.73 m² higher (95% Cl 1.12 to 1.86) in the ARB groups | 66 (2) | ⊕⊕⊕⊝ moderate | ||
| Urinary protein excretion | Mean across control groups ranged from 1.12 to 2.97 g/24 h | Mean was on average0.01 g/24 h lower (95% Cl ‐0.09 to 0.06) in the ARB groups | 66 (2) | ⊕⊕⊝⊝ low | ||
| Kt/V | Mean Kt/V across control groups ranged from 1.69 to 1.98 | Mean was on average0.1 higher (95% Cl ‐0.02 to 0.22) in the ARB groups | 76 (2) | ⊕⊕⊕⊝ moderate | ||
| Weekly creatinine clearance | Mean across control groups from 31.4 to 71.5 L/wk/1.73 m² | Mean was on average9.06 L/wk/1.73 m² higher (95% Cl ‐2.77 to 20.90) in the ARB groups | 110 (3) | ⊕⊕⊝⊝ low | ||
| Systolic BP | Mean across control groups ranged from 129 to 137 mm Hg | Mean was on average‐0.67 mm Hg higher (95% Cl ‐2.77 to 1.42) in the ARB groups | 110 (3) | ⊕⊕⊕⊝ moderate | ||
| Diastolic BP | Mean across control groups ranged from 129 to 137 mm Hg | Mean was on average‐0.70 mm Hg higher (95% Cl ‐2.14 to 0.74) in the ARB groups | 110 (3) | ⊕⊕⊕⊝ moderate | ||
| Serum potassium | Mean across control group was 4.06 mmol/L | Mean was on average0.13 mmol/L higher (95% Cl ‐0.12 to 0.38) in the ARB group | 44 (1) | ⊕⊕⊝⊝ low | ||
| Adverse events (episodes of peritonitis) | High risk population | RR 0.67 (0.18 to 2.54) | 34 (1) | ⊕⊕⊝⊝ low | ||
| 250 per 1000 | 167 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk Ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
Summary of findings 2. Angiotensin‐converting enzyme inhibitors (ACEi) versus conventional therapy for preserving residual kidney function in peritoneal dialysis patients.
| ACEi versus conventional therapy for preserving residual kidney function in peritoneal dialysis patients | ||||||
|
Patient or population: patients receiving PD Settings: outpatient Intervention: ACEi Comparison: Conventional therapy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Conventional therapy | ACEi | |||||
| Decline in residual kidney function (12 months) | Mean across the control group was 1.86 mL/min/1.73 m² | Mean was 0.93 mL/min/1.73 m² lower(95% Cl ‐1.75 to ‐0.11) in the ACEi group | 60 (1) | ⊕⊕⊕⊝ moderate | ||
| Anuria |
High risk population 733 per 1000 |
467 per 1000 |
RR 0.32 (0.11 to 0.94) |
60 (1) | ⊕⊕⊕⊝ moderate | |
| Mortality | High risk population |
RR 1.50 (0.27 to 8.34) |
60 (1) | ⊕⊕⊕⊝ moderate | ||
| 67 per 1000 | 100 per 1000 | |||||
| Cardiac events | High risk population |
RR 1.0 (0.37 to 3.21) |
60 (1) | ⊕⊕⊕⊝ moderate | ||
| 83 per 1000 | 83 per 1000 | |||||
| Cardiac events (fatal) | High risk population |
RR 1.0 (0.15 to 6.64) |
60 (1) | ⊕⊕⊕⊝ moderate | ||
| 67 per 1000 | 67 per 1000 | |||||
| Cardiac events (non fatal) | High risk population |
RR 1.0 (0.31 to 3.27) |
60 (1) | ⊕⊕⊕⊝ moderate | ||
| 100 per 1000 | 100 per 1000 | |||||
| Adverse events (episodes of peritonitis) | High risk population |
RR 1.13 (0.47 to 2.71) |
60 (1) | ⊕⊕⊕⊝ moderate | ||
| 133 per 1000 | 150 per 1000 | |||||
| Adverse events (episodes of peritonitis) ‐ treated with an aminoglycoside | High risk population |
RR 1.20 (0.41 to 3.51) |
60 (1) | ⊕⊕⊕⊝ moderate | ||
| 167 per 1000 | 200 per 1000 | |||||
| Adverse events (episodes of peritonitis) ‐ not treated with an aminoglycoside | High risk population |
RR 1.00 (0.22 to 4.56) |
60 (1) | ⊕⊕⊕⊝ moderate | ||
| 100 per 1000 | 100 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk Ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
Summary of findings 3. Angiotensin receptor blockers (ARBs) versus angiotensin‐converting enzyme inhibitors (ACEis) for preserving residual kidney function in peritoneal dialysis patients.
| ARBs compared with ACEis for preserving residual kidney function in peritoneal dialysis patients | ||||||
|
Patient or population: patients receiving PD Settings: outpatient Intervention: ARB Comparison: ACEi | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| ACEi | ARB | |||||
| Residual kidney function (4 weeks) | Mean across ACEi group was 2.28 mL/min/1.73 m² | Mean was 0.47 mL/min/1.73 m² lower (95% Cl ‐2.73 to 1.79) in the ARB group | 20 (1) | ⊕⊕⊝⊝ low | ||
| Residual kidney function (12 months) | Mean across ACEi group was 2.36 mL/min/1.73 m² | Mean was 0.18 mL/min/1.73 m² higher (95% Cl ‐0.04 to 0.40) in the ARB group | 60 (1) | ⊕⊕⊕⊝ moderate | ||
| Anuria |
High risk population 367 per 1000 |
400 per 1000 | RR 1.15 (0.41 to 3.26) | 60 (1) | ⊕⊕⊕⊝ moderate | |
| Cardiovascular events (non‐fatal) |
High risk population 100 per 1000 |
133 per 1000 | RR 1.33 (0.33 to 5.45) | 60 (1) | ⊕⊕⊕⊝ moderate | |
| Serum potassium | Mean across ACEi group was 4.42 mmol/L | Mean was 0.05 mmol/L lower (95% Cl ‐2.73 to 1.79) in the ARB group | 42 (1) | ⊕⊕⊕⊝ moderate | ||
| Systolic BP | Mean across ACEi group was 141.95 mm Hg | Mean was 0.48 mm Hg higher (95% Cl ‐7.76 to 8.72) in the ARB group | 42 (1) | ⊕⊕⊕⊝ moderate | ||
| Diastolic BP | Mean across ACEi group was 84.19 mm Hg | Mean was 0.38 mm Hg higher (95% Cl ‐6.76 to 7.52) in the ARB group | 42 (1) | ⊕⊕⊕⊝ moderate | ||
| Cough |
High risk population 67 per 1000 |
100 per 1000 |
RR 1.56 (0.24 to 10.05) |
60 (1) | ⊕⊕⊕⊝ moderate | |
| Hyperkalaemia |
High risk population 69 per 1000 |
83 per 1000 | RR 1.23 (0.35 to 4.40) | 144 (2) | ⊕⊕⊕⊝ moderate | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk Ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
Background
Description of the condition
Peritoneal dialysis (PD) has been established for more than 30 years as a form of renal replacement therapy (RRT). Improvements in continuous ambulatory/cyclic PD (CAPD/CCPD) have resulted in its widespread adoption for treating end‐stage kidney disease (ESKD). Cost comparisons between PD and haemodialysis (HD) show that PD is less expensive than HD (Blake 2001). In the United States, 8% of the ESKD population is on PD (USRDS 2003), but it is more prevalent in other countries: Canada (20% to 30%) (Schaubel 2000); Denmark (33%) (Heaf 2002); Netherlands (39%) (Termorshuizen 2003); Hong Kong (80%) (Li 1999); and Mexico (81%) (Cueto‐Manzano 2003). Some epidemiological studies have shown an adjusted survival advantage for PD compared with HD during the first two years of dialysis (Fenton 1997; Heaf 2002), and several studies have also suggested that CAPD is equivalent to HD or may even be superior for certain subgroups (Gokal 1999; Suzuki 2003a).
Residual kidney function is better preserved with PD than with HD (Cancarini 1986) because HD causes substantial haemodynamic disturbance and activates inflammation, which may accelerate the loss of residual kidney function. Patients treated with PD have been shown to have a 65% lower risk for losing residual kidney function than patients receiving HD (Moist 2000). This better preservation, which has been attributed to an effect of residual function on both total solute clearance and fluid status (Bargman 2001), may be an important factor for choosing PD and an important determinant of mortality and morbidity (Bargman 2001; Szeto 2000). Better preservation is associated with decreased mortality, even at a low level (Blake 2001; Shemin 2000) with some studies showing that each 1 mL/min of residual glomerular filtration rate (GFR) is associated with a nearly 50% reduction in mortality rate (Szeto 2000; Maiorca 1995). It has also been estimated that each 1 mL/min of renal clearance can be translated into a Kt/V of 0.25 to 0.3/wk in a 70 kg man (Li 2001a; Venkataraman 2000). One, 2 L dialysis exchange/d could be spared by preserving 1 mL/min of residual GFR, which could improve quality of life and decrease costs substantially (Li 2001b). However, the initial survival advantage of PD compared with HD may change to a disadvantage after long‐term PD (Termorshuizen 2003) because of the decrease of residual GFR and the development of peritoneal membrane alterations (Williams 2002). As a result, measures to preserve residual kidney function and peritoneal membrane are an important target in the treatment of patients receiving PD.
Description of the intervention
Angiotensin‐converting enzyme inhibitors (ACEis) and angiotensin receptor blockers (ARBs) are frequently prescribed in PD patients, primarily for the control of hypertension or heart failure, which could provide significant cardiovascular benefit in ESKD patients. A double blind randomised controlled study (RCT) (Suzuki 2003b) showed that the ARB valsartan had a beneficial effect on left ventricular hypertrophy in patients on CAPD. Use of an ACEi has also been independently associated with a decreased risk for loss of residual kidney function (Moist 2000).
How the intervention might work
Many studies confirm that both ARBs and ACEis are effective in the prevention of progressive chronic kidney disease and reduction of proteinuria. Recently, some clinical studies have demonstrated positive effects of an ACEi or an ARB on preserving residual kidney function in PD patients (Li 2003; Suzuki 2004; Zhong 2007a). In addition, the results of a recent study show that ACEis and ARBs were likely to have a membrane protective effect by preventing the increase in small solute transport that often occurs in long term PD which is possibly related to a larger number of perfused peritoneal microvessels (Kolesnyk 2007).
Why it is important to do this review
A recent systematic review concluded that ACEis and ARBs slow the loss of residual kidney function based on two RCTs enrolling a total of 94 participants (Akbari 2009). A more comprehensive systematic review is warranted since only studies published in English were included and it did not provide details on other parameters of great clinical significance such as peritoneal function, changes in blood pressure and quality of life.
Objectives
This review aimed to evaluate the benefits and harms of ACEis and ARBs for preserving residual kidney function in PD patients.
Methods
Criteria for considering studies for this review
Types of studies
All RCTs and quasi‐RCTs in which allocation to treatment was obtained by alternation, use of alternate medical records, date of birth or other predictable methods) investigating the benefits and harms of ACEi and ARBs for preserving residual kidney function in PD were considered eligible for inclusion, whether or not residual kidney function was set as the primary outcome. However, studies that did not assess residual kidney function were not included.
Types of participants
Inclusion criteria
ESKD patients with residual kidney function receiving any type of PD regardless of age, primary diseases and clinical medical course. The definition of remaining or losing residual kidney function applied by each study was accepted.
Exclusion criteria
Acute kidney injury: abrupt (within 48 hours) reduction in kidney function, currently defined as an absolute increase in serum creatinine (SCr) (≥ 0.3 mg/dL or ≥ 26.5 μmol/L), a percentage increase in SCr of ≥ 50% (1.5‐fold from baseline) or a reduction in urine output (documented oliguria of < 0.5 mL/kg/h for > 6 hours) despite adequate fluid resuscitation when applicable. Patients receiving both PD and HD.
Types of interventions
Any ACEi or ARB used for ESKD patients receiving PD, regardless of dosage, mode of administration or duration of treatment. The comparisons were as follows:
ACEi or ARB or both + routine treatment versus routine treatment + placebo
ACEi or ARB or both + routine treatment versus routine treatment
ACEi or ARB or both+ routine treatment versus routine treatment + other drugs (antihypertensive drugs).
ACEi + routine treatment versus ARB + routine treatment
Routine treatment: PD and supportive treatment.
Supportive treatment can include approaches to treat underlying kidney or medical diseases and to improve other disorders linked to kidney failure, such as anaemia, calcium and phosphate imbalance, and dyslipidaemia. Supportive treatment should be comparable between study and control groups.
Types of outcome measures
Primary outcomes
Residual kidney function (as measured by GFR or endogenous creatinine clearance (CrCl).
Secondary outcomes
All‐cause mortality
Cardiovascular mortality (deaths caused by heart failure, myocardial infarction, stroke or cardiac arrest)
Non‐fatal cardiovascular events (non‐fatal myocardial infarction, angina pectoris, stroke and arrhythmia)
Urinary albumin/protein excretion rate
Anuria
Peritoneal function: dialysis adequacy (Kt/V, weekly CrCl), peritoneal membrane transport
The number of patients changing from PD to HD or increasing PD dose due to declining of residual kidney function
Blood pressure (mm Hg)
Quality of life (validated scale/s are required)
Adverse events: cough, potassium, hyperkalaemia, hypotension, angioedema and peritonitis.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Renal Group's Specialised Register (to 15 May 2014) through contact with the Trials' Search Co‐ordinator using search terms relevant to this review. The Cochrane Renal Group’s Specialised Register contains studies identified from the following sources.
Monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL)
Weekly searches of MEDLINE OVID SP
Handsearching of renal‐related journals and the proceedings of major renal conferences
Searching of the current year of EMBASE OVID SP
Weekly current awareness alerts for selected renal journals
Searches of the International Clinical Trials Register (ICTRP) Search Portal and ClinicalTrials.gov.
Studies contained in the Specialised Register are identified through search strategies for CENTRAL, MEDLINE, and EMBASE based on the scope of the Cochrane Renal Group. Details of these strategies, as well as a list of handsearched journals, conference proceedings and current awareness alerts, are available in the Specialised Register section of information about the Cochrane Renal Group.
See Appendix 1 for search terms used in strategies for this review.
Searching other resources
Chinese Biomedical Literature Database (CBM)
China National Knowledge Infrastructure (CNKI)
Reference lists of clinical practice guidelines, review articles and relevant studies
Letters seeking information about unpublished or incomplete studies to investigators known to be involved in previous studies.
Data collection and analysis
Selection of studies
The review was undertaken by four authors. The search strategy described was used to obtain titles and abstracts of studies that might be relevant to the review. The titles and abstracts were screened independently by two authors, who discarded studies that were not applicable, however studies and reviews that might include relevant data or information on studies were retained initially. Two authors independently assessed retrieved abstracts (and if necessary the full text) to determine which studies satisfied the inclusion criteria.
Data extraction and management
Data extraction was carried out independently by two authors using standard data extraction forms. Studies reported in non‐English or Non‐Chinese language journals were translated before assessment. Where more than one publication of one study exists, reports were grouped together and the most recent or most complete data set were used. Any discrepancy between published versions were highlighted. Disagreements were resolved in consultation with the other authors.
Assessment of risk of bias in included studies
The following items were assessed using the risk of bias assessment tool (Higgins 2011) (see Appendix 2).
Was there adequate sequence generation (selection bias)?
Was allocation adequately concealed (selection bias)?
-
Was knowledge of the allocated interventions adequately prevented during the study (detection bias)?
Participants and personnel
Outcome assessors
Were incomplete outcome data adequately addressed (attrition bias)?
Are reports of the study free of suggestion of selective outcome reporting (reporting bias)?
Was the study apparently free of other problems that could put it at a risk of bias?
Measures of treatment effect
For dichotomous outcomes (mortality, complications of treatment and cardiovascular events) results were expressed as risk ratios (RR) with 95% confidence intervals (CI). Where continuous scales of measurement was used to assess the effects of treatment (e.g. residual kidney function, peritoneal function, blood pressure, proteinuria and urine volume), the mean difference (MD) were used, or the standardised mean difference (SMD) if different scales had been used.
Dealing with missing data
Any further information required from the original author was requested by written correspondence and any relevant information obtained in this manner was included in the review.
Assessment of heterogeneity
Heterogeneity was analysed using a Chi² test on N‐1 degrees of freedom, with an alpha of 0.05 used for statistical significance and with the I² test (Higgins 2003). I² values of 25%, 50% and 75% correspond to low, medium and high levels of heterogeneity.
Assessment of reporting biases
Although we had planned to create funnel plots to assess for the potential existence of small study bias (Higgins 2011), the small number of included studies meant that this was not possible.
Data synthesis
Data were pooled using the random‐effects model but the fixed‐effect model was also applied to ensure robustness of the model chosen and susceptibility to outliers.
Subgroup analysis and investigation of heterogeneity
We performed subgroup analysis to identify possible sources of heterogeneity. Differences in participants (ethnicity, age and underlying kidney diseases) and disparities related to intervention (i.e. the type and dose of ACEi or ARB or both, modality and dose of PD and duration of therapy) might be attributed to heterogeneity. The following subgroup analyses were planned to investigate any observed heterogeneity.
Different underlying kidney diseases (i.e. diabetic kidney disease or non‐diabetic kidney diseases)
Different type and dose of ACEi and or ARB
Different modalities of PD (i.e. CAPD, CCPD or automated PD)
Different durations of therapy and follow‐up.
Adverse effects were tabulated and assessed with descriptive techniques, as they are likely to be different for the various drugs used. Where possible, the risk difference (RD) with 95% CI was calculated for each adverse effect, either compared to no treatment or to another agent.
Sensitivity analysis
Where possible, we performed sensitivity analyses to evaluate the effect on the overall result of removing studies with low methodological quality. Studies with inadequate allocation concealment; achieving inadequate follow‐up and unblinded outcome assessment, or blinding of outcome assessment uncertain, were considered as being of low methodological quality.
Results
Description of studies
Results of the search
After searching the Cochrane Renal Group's Specialised Register (59 records), CENTRAL (13), EMBASE (22), and Chinese databases (15) we identified 109 records. After duplicate removal and removing irrelevant records 26 reports were retained for full‐text assessment. Full‐text assessment identified revealed six eligible studies (seven reports) (Li 2003; Suzuki 2004; Wang 2005d; Zhong 2007a; Phakdeekitcharoen 2004; Reyes‐Marin 2012) with a total of 257 participants. Two of these studies were published in Chinese (Wang 2005d; Zhong 2007a). Two reports were classified as ongoing studies (NCT00721773; NCT01041963, one conference abstract is awaiting classification (Medcalf 2000), and nine studies (16 reports) were excluded (Cioni 2010; Favazza 1992; Huang 2002; Kolesnyk 2011; Nakamoto 2004; PERFECT Study 1997; Rojas‐Campos 2005; Shigenaga 2009; Suzuki 2003). A flow chart for our study selection procedure is presented as Figure 1.
1.
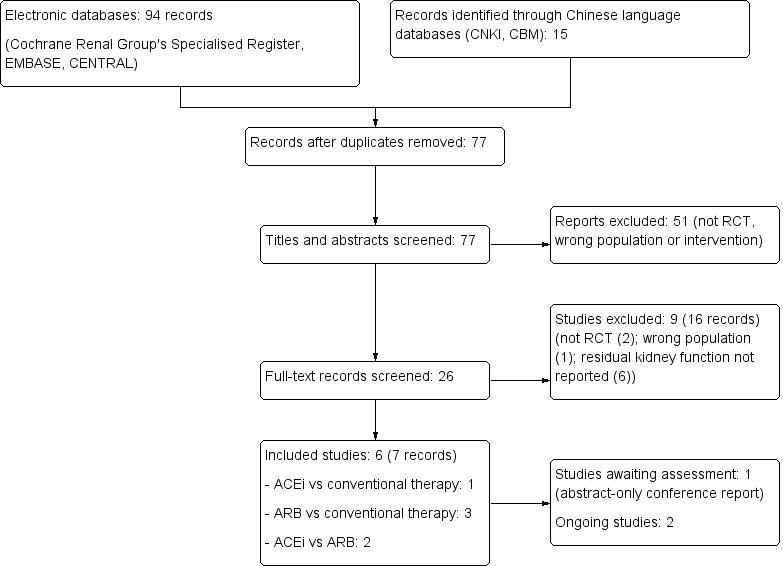
Study flow diagram.
Included studies
Three studies investigated the influence of an ARB on residual kidney function in CAPD patients (Suzuki 2004;Wang 2005d; Zhong 2007a). Based on prospective calculation of sample size, Suzuki 2004 enrolled 34 patients (male/female: 21/13; mean age: 63.5 years) and compared the effects of valsartan (40 to 80 mg/d) with other antihypertensive drugs (except an ACEi or an ARB). An antihypertensive regimen was proposed to achieve the target blood pressure (BP) of 130/80 mm Hg. Patients used 1.5 to 2.5 L of 2.5% dextrose dialysate/exchange for 3 to 5 exchanges/d for CAPD. Zhong 2007a enrolled 48 patients (male/female: 31/17; mean age: 44 years) and compared the effects of irbesartan (300 mg/d) with other antihypertensive drugs (except an ACEi or an ARB). An antihypertensive regimen was proposed to achieve the target BP of 12070 to 135/85 mm Hg. It was reported 1.5% or 2.5% dextrose dialysate was used, but detailed CAPD schedule was not available. In Wang 2005d, valsartan (40 to 80 mg/d) and other antihypertensive drugs were compared in 32 patients (male/female: 21/11; mean age: 42 years). Target BP was set at 130/80 mm Hg. Detailed CAPD schedule was not available.
Li 2003 assessed changes in residual kidney function in CAPD patients treated with the ACEi, ramipril (5 mg/d). On the basis of sample size estimation, 60 patients were included (male/female: 38/22; mean age: 58.6 years). Antihypertensive drugs other than an ACEi were allowed in both study and control groups to maintain target BP of 135/85 mm Hg. CAPD protocol was not provided.
Two studies compared an ARB with an ACEi for preservation of residual kidney function in PD patients (Phakdeekitcharoen 2004; Reyes‐Marin 2012). Phakdeekitcharoen 2004 was a cross‐over study, which enrolled 21 patients (male/female: 14/7; mean age: 44.8 years) and compared the effects of candesartan (8 mg/d) with enalapril (10 mg/d) for four weeks (short‐term use). Reyes‐Marin 2012 enrolled 60 patients (male/female: 36/24) and compared the effects of losartan (50 mg/d) with enalapril (50 mg/d) for 12 months (long‐term use). Target BP was set at 130/85 mm Hg.
Excluded studies
Of the 18 studies (26 reports) identified, nine studies (16 reports) were excluded. One study was not randomised (Kolesnyk 2011); one study enrolled ineligible patients (not all PD patients) (PERFECT Study 1997), and seven studies provided no information about residual kidney function (Cioni 2010; Huang 2002; Nakamoto 2004; Shigenaga 2009; Suzuki 2003; Favazza 1992; Rojas‐Campos 2005). See Characteristics of excluded studies.
Risk of bias in included studies
Details of the assessment of risk of bias of included studies are presented in Figure 2 and Figure 3.
2.
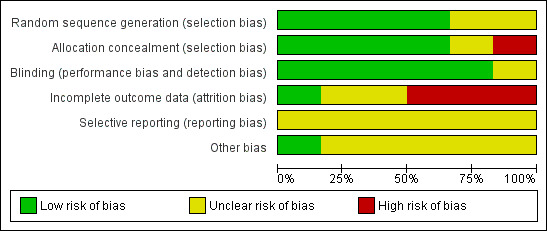
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
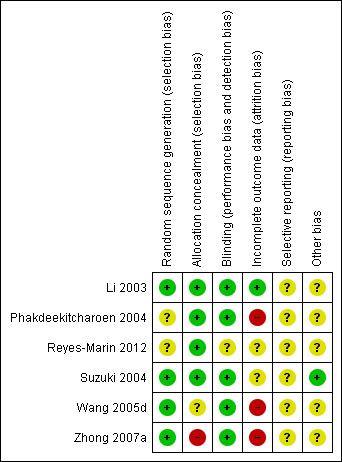
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Two studies provided detailed allocation list generation methods (computer generated) and applied adequate allocation concealment (Li 2003; Suzuki 2004), the remaining four studies did not provide details of allocation (Phakdeekitcharoen 2004; Reyes‐Marin 2012; Wang 2005d; Zhong 2007a). The methods used in the studies by Wang 2005d and Zhong 2007a were obtained through corresponding with the original authors. They used computer software to generate the sequence, but allocation concealment was not used.
Blinding
One study did not provide any information about blinding (Reyes‐Marin 2012), while the other five studies were open‐label. The primary outcome (residual kidney function) assessed in the review was obtained from laboratory tests, and it was judged as unlikely to be influenced by the status of blinding. BP measurements in four studies (Suzuki 2004; Phakdeekitcharoen 2004; Wang 2005d; Zhong 2007a) however might be influenced.
Incomplete outcome data
Suzuki 2004 and Reyes‐Marin 2012 did not report detailed information of patients lost to follow‐up. In Zhong 2007a, two patients withdrew from the study, and two patients were lost to follow‐up with no reason identified. Wang 2005d reported that two patients withdrew from the study but reasons were not provided. In Li 2003, five deaths occurred and 2 patients withdrew due to kidney transplantation; but it was noteworthy that five patients in the ACEi group discontinued ramipril due to persistent dizziness or cough, which are common side effects of ACEis. In Phakdeekitcharoen 2004, eight patients (27.6%) withdraw and reasons were provided.
Selective reporting
None of the included studies reported details of the study protocols or prespecified outcomes. There were insufficient data available to enable an assessment of selective reporting to be made.
Other potential sources of bias
Two studies did not provide detailed antihypertensive protocols (other than ACEis and ARBs) (Wang 2005d; Zhong 2007a), and PD schedules were not provided by four studies (Li 2003; Reyes‐Marin 2012; Wang 2005d; Zhong 2007a).
Effects of interventions
See: Table 1; Table 2; Table 3
Residual kidney function
Three studies reported the effect of ARBs versus other antihypertensive drugs on residual kidney function at various time points. Zhong 2007a reported no significant difference between ARBs and other antihypertensive therapies in reducing the decline of residual kidney function at three months (Analysis 1.1.1 (1 study, 44 participants): MD ‐0.44 mL/min/1.73m², 95% CI ‐1.53 to 0.65) or six months (Analysis 1.1.2 (1 study, 44 participants): MD ‐0.20 mL/min/1.73 m², 95%CI ‐1.01 to 0.61); however ARBs significantly reduced the decline of residual kidney function at 12 months (Analysis 1.1.3 (1 study, 44 participants): MD 0.64 mL/min/1.73 m², 95% CI 0.19 to 1.09). At 24 months ARBs significantly reduced the decline in residual kidney function compared to other antihypertensive regimens (Analysis 1.1.4 (2 studies; 66 participants): MD 1.49 mL/min/1.73 m², 95% CI 1.12 to 1.86; I² = 0%). Long‐term use (≥ 12 months) of ARBs can benefit residual kidney function in PD patients (Analysis 1.3 MD 1.11 mL/min/1.73 m², 95% CI 0.38 to 1.83).
1.1. Analysis.
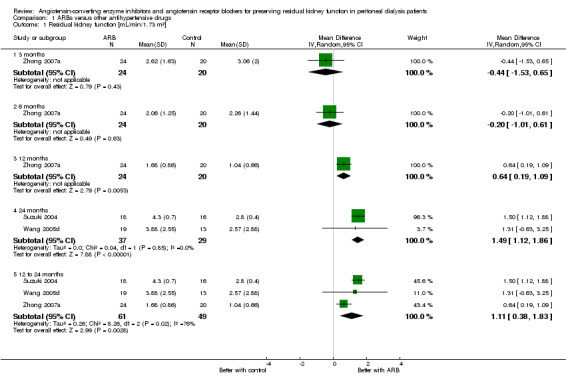
Comparison 1 ARBs versus other antihypertensive drugs, Outcome 1 Residual kidney function [mL/min/1.73 m²].
1.3. Analysis.
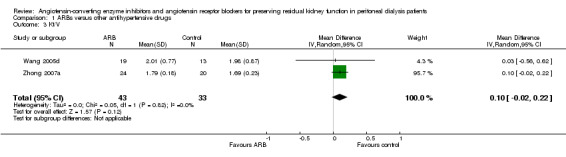
Comparison 1 ARBs versus other antihypertensive drugs, Outcome 3 Kt/V.
Li 2003 reported over 12 months ACEis significantly reduced the decline of residual kidney function compared with other antihypertensive drugs (Analysis 2.1 (1 study, 60 participants): MD ‐0.93 mL/min/1.73 m², 95% CI ‐1.75 to ‐0.11).
2.1. Analysis.
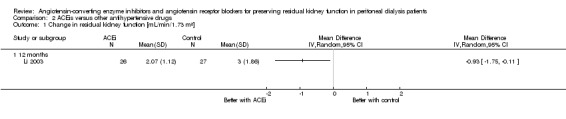
Comparison 2 ACEis versus other antihypertensive drugs, Outcome 1 Change in residual kidney function [mL/min/1.73 m²].
Phakdeekitcharoen 2004 and Reyes‐Marin 2012 reported no significant differences in residual kidney function preservation between ARBs and ACEis in short‐term (four weeks) (Analysis 3.1.1 (1 study, 20 participants): MD ‐0.47 mL/min/1.73 m², 95% CI ‐2.73 to 1.79) or long‐term use (12 months) (Analysis 3.3 (1 study, 60 participants): MD 0.18 mL/min/1.73 m², 95% CI ‐0.04 to 0.40).
3.1. Analysis.
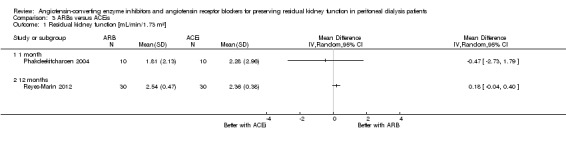
Comparison 3 ARBs versus ACEis, Outcome 1 Residual kidney function [mL/min/1.73 m²].
3.3. Analysis.
Comparison 3 ARBs versus ACEis, Outcome 3 Anuria.
All‐cause mortality
Mortality was not reported in the studies comparing ACEis with other antihypertensive drugs or studies comparing ARBs with ACEis.
Li 2003 reported no significant difference in mortality between patients treated with ACEis compared with other antihypertensive drugs (Analysis 2.2 (1 study, 60 patients): RR 1.50, 95% CI 0.27 to 8.34).
2.2. Analysis.
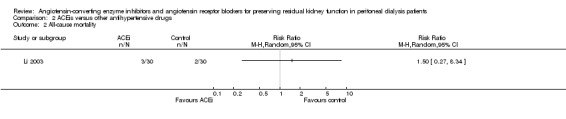
Comparison 2 ACEis versus other antihypertensive drugs, Outcome 2 All‐cause mortality.
Cardiovascular events
ARBs versus other antihypertensive drugs
Cardiovascular events were not reported in the studies comparing an ARB with other antihypertensive drugs.
Li 2003 reported no significant differences between ACEis and other antihypertensive drugs for both fatal (Analysis 2.3.1 (1 study, 60 participants): RR 1.00, 95% CI 0.15 to 6.64) and non‐fatal (Analysis 2.3.2 (1 study, 60 patients): RR 1.00, 95% CI 0.22 to 4.56) cardiovascular events.
2.3. Analysis.
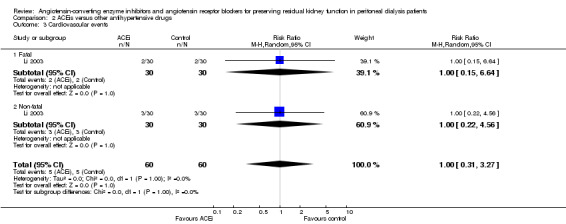
Comparison 2 ACEis versus other antihypertensive drugs, Outcome 3 Cardiovascular events.
Reyes‐Marin 2012 reported no fatal cardiovascular events occurred in either the ARB or ACEi groups, and no significant difference for non‐fatal cardiovascular events (Analysis 3.2 (1 study, 60 participants): RR 1.38, 95% CI 0.28 to 6.80).
3.2. Analysis.
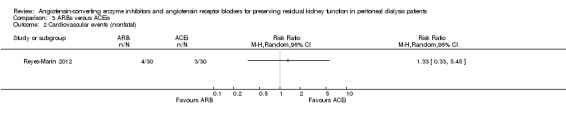
Comparison 3 ARBs versus ACEis, Outcome 2 Cardiovascular events (nonfatal).
Urinary protein excretion
There was no significant difference in urinary protein excretion between patients treated with ARBs and those treated with other antihypertensive drugs (Analysis 1.2 (2 studies, 66 patients): MD ‐0.01 g/d, 95% CI ‐0.09 to 0.06).
1.2. Analysis.

Comparison 1 ARBs versus other antihypertensive drugs, Outcome 2 Urinary protein excretion.
Urinary protein excretion was not reported in the studies comparing an ACEi with other antihypertensive drugs or studies comparing an ARB with an ACEi.
Anuria
Anuria was not reported in the studies comparing an ARB with other antihypertensive drugs.
Li 2003 reported over 12 months ACEis significantly reduced the number progression to complete anuria compared to other antihypertensive drugs (Analysis 2.4 (1 study, 60 participants): RR 0.32, 95% CI 0.11 to 0.94).
2.4. Analysis.
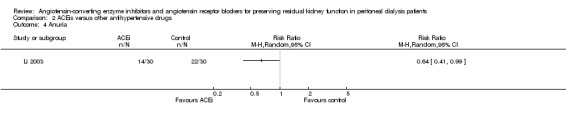
Comparison 2 ACEis versus other antihypertensive drugs, Outcome 4 Anuria.
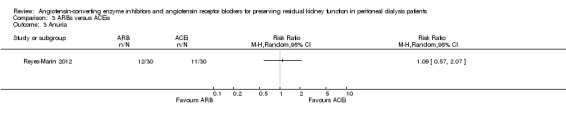
Reyes‐Marin 2012 reported no significant difference in the progression to complete anuria between the ARB and ACEi groups (Analysis 3.3 (1 study, 42 participants): RR 1.15, 95% CI 0.41 to 3.26).
Dialysis adequacy
Dialysis adequacy was measured in studies comparing ARBs with other antihypertensive drugs. There was no significant difference in Kt/V between patients treated with ARBs and those treated with other antihypertensive drugs (Analysis 1.3 (2 studies, 76 participants): MD 0.10, 95% CI ‐0.02 to 0.22). There was no significant difference in weekly creatinine clearance between patients treated with ARBs and those treated with other antihypertensive drugs (Analysis 1.4 (3 studies, 110 participants): MD 9.06 mL/wk/1.73 m², 95% CI ‐2.77 to 20.90; I² = 76%), however significant heterogeneity was identified.
1.4. Analysis.
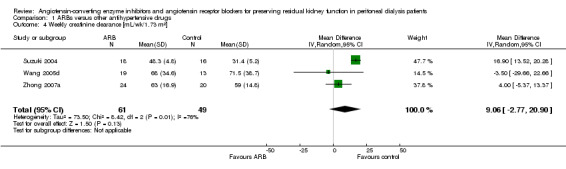
Comparison 1 ARBs versus other antihypertensive drugs, Outcome 4 Weekly creatinine clearance [mL/wk/1.73 m²].
Dialysis adequacy was not reported in studies comparing an ACEi with other antihypertensive drugs or studies comparing an ARB with an ACEi.
Blood pressure
In studies comparing ARBs with other antihypertensive drugs there were no significant differences in either systolic blood pressure (Analysis 1.5 (3 studies, 110 participants): MD ‐0.67 mm Hg, 95% CI ‐2.77 to 1.42; I² = 0%) or diastolic blood pressure (Analysis 1.6 (3 studies, 110 participants): MD ‐0.70 mm Hg, 95% CI ‐2.14 to 0.74; I² = 0%).
1.5. Analysis.
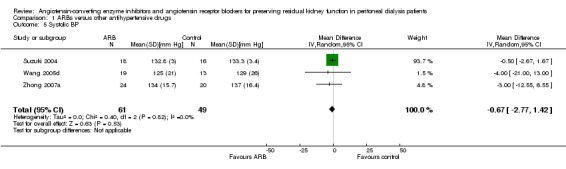
Comparison 1 ARBs versus other antihypertensive drugs, Outcome 5 Systolic BP.
1.6. Analysis.
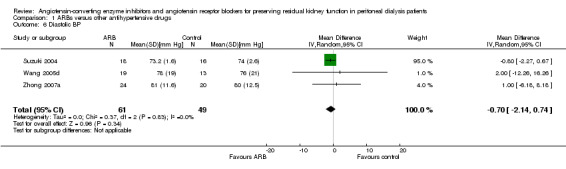
Comparison 1 ARBs versus other antihypertensive drugs, Outcome 6 Diastolic BP.
Reyes‐Marin 2012 reported no significant differences between the ARB and ACEi groups for either systolic blood pressure (Analysis 3.4 (1 study, 42 participants): MD 0.48 mm Hg, 95% CI ‐7.76 to 8.72) or diastolic blood pressure (Analysis 3.5 (1 study, 42 participants): MD ‐0.38 mm Hg, 95% CI ‐6.76 to 7.52).
3.4. Analysis.
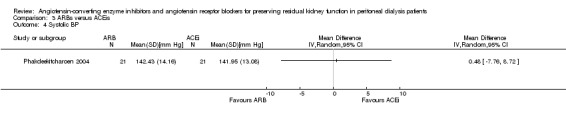
Comparison 3 ARBs versus ACEis, Outcome 4 Systolic BP.
3.5. Analysis.
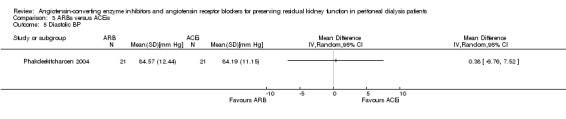
Comparison 3 ARBs versus ACEis, Outcome 5 Diastolic BP.
Blood pressure was not reported in the studies comparing an ACEi with other antihypertensive drugs.
Peritonitis
Suzuki 2004 reported no significant difference in the number of patients experiencing peritonitis between the ARB and other antihypertensive drug groups (Analysis 1.7 (1 study, 34 participants): RR 0.67, 95% CI 0.18 to 2.54).
1.7. Analysis.
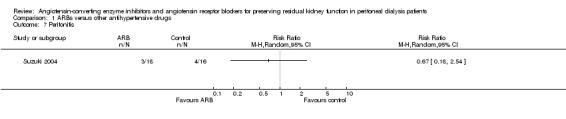
Comparison 1 ARBs versus other antihypertensive drugs, Outcome 7 Peritonitis.
Li 2003 reported no significant difference in the number of patients experiencing peritonitis between the ACEi and control groups (Analysis 2.5.1 (1 study, 60 participants): RR 1.13, 95% CI 0.50 to 2.52). There was no significant difference between the groups for those either treated with an aminoglycoside (Analysis 2.5.2: RR 1.20, 95% CI 0.41 to 3.51) or not treated with an aminoglycoside (Analysis 2.5.3: RR 1.00, 95% CI 0.22 to 4.56).
2.5. Analysis.
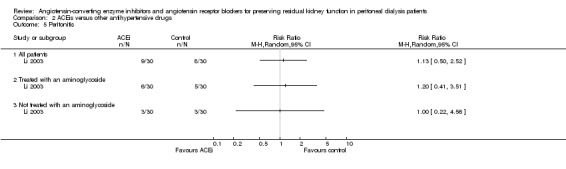
Comparison 2 ACEis versus other antihypertensive drugs, Outcome 5 Peritonitis.
Reyes‐Marin 2012 reported no significant difference in the number of patients experiencing peritonitis between the ARB and ACEi groups (Analysis 3.6 (1 study, 60 patients): RR 1.17, 95% CI 0.44 to 3.06).
3.6. Analysis.
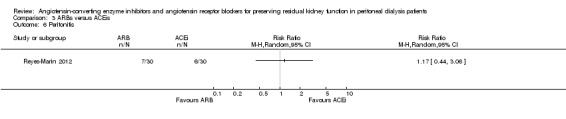
Comparison 3 ARBs versus ACEis, Outcome 6 Peritonitis.
Cough
Cough was not reported in the studies comparing an ARB or an ACEi with other antihypertensive drugs.
Reyes‐Marin 2012 reported no significant difference in the number of patients experiencing cough between the ARB and ACEi groups (Analysis 3.7 (1 study, 60 patients): RR 1.50, 95% CI 0.27 to 8.34).
3.7. Analysis.
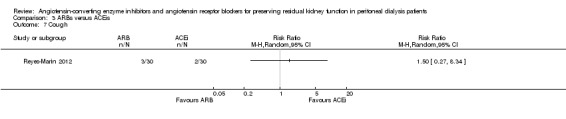
Comparison 3 ARBs versus ACEis, Outcome 7 Cough.
Serum potassium
Zhong 2007a reported no significant difference in serum potassium level between the ARB and other antihypertensive drug groups (Analysis 1.8 (1 study, 44 participants): MD 0.13 mmol/L, 95% CI ‐0.12 to 0.38).
1.8. Analysis.
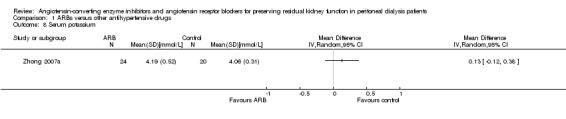
Comparison 1 ARBs versus other antihypertensive drugs, Outcome 8 Serum potassium.
Phakdeekitcharoen 2004 reported no statistical difference was observed in serum potassium between the ARB and ACEi groups (Analysis 3.8 (1 study, 42 participants): MD ‐0.05 mmol/L, 95% CI ‐0.45 to 0.35).
3.8. Analysis.
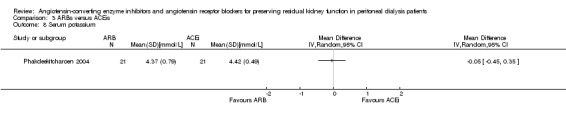
Comparison 3 ARBs versus ACEis, Outcome 8 Serum potassium.
Serum potassium was not reported in any of the studies comparing an ACEi with other antihypertensive drugs.
Hyperkalaemia
Hyperkalaemia was not reported in studies comparing an ARB or an ACEi with other antihypertensive drugs.
There was no significant difference in the number patients experiencing hyperkalaemia between the ARB and ACEi groups (Analysis 3.9 (2 studies, 84 events): RR 1.20, 95% CI 0.40 to 3.63)
3.9. Analysis.
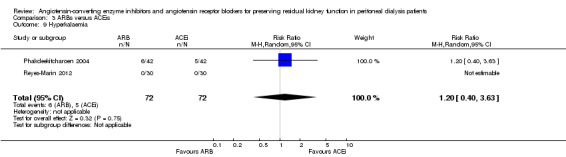
Comparison 3 ARBs versus ACEis, Outcome 9 Hyperkalaemia.
Other outcomes
The following outcomes were not reported by any of the included studies: hypotension; angioedema; the number of patients changing from PD to HD; increasing PD dose due to declining of residual kidney function; or quality of life.
Due to the small number of studies identified we were unable to perform subgroup analyses to investigate heterogeneity, perform sensitivity analyses, assess publication biases, or tabulate adverse events as stated in our protocol.
Discussion
Summary of main results
This review assessed six small RCTs enrolling 257 participants. Three studies compared an ARB with other antihypertensive drugs (Suzuki 2004; Wang 2005d; Zhong 2007a), one study compared an ACEi with other antihypertensive drugs (Li 2003), and two studies compared an ARB with an ACEi (Phakdeekitcharoen 2004; Reyes‐Marin 2012). Long‐term use (≥ 12 months) of an ARB showed significant benefit in preserving residual kidney function in CAPD patients (MD 1.11 mL/min/1.73 m², 95% CI 0.38 to 1.83), although there was no significant benefit when an ARB were used short‐term (≤ 6 months). One study showed that compared with other antihypertensive drugs, long‐term use (12 months) of the ACEi ramipril, showed a significant reduction in the decline of residual kidney function in patients on CAPD (MD ‐0.93 mL/min/1.73 m², 95% CI ‐1.75 to ‐0.11), as well as slowing of the progression to complete anuria (RR 0.64, 95% CI 0.41 to 0.99). There was no significant difference in serum potassium levels, urinary protein excretion, Kt/V, weekly creatinine clearance and blood pressure for an ARB versus other antihypertensive drugs. Compared with other antihypertensive drugs, ramipril showed no difference in mortality and cardiovascular events. In two studies, there was no significant difference on residual kidney function preservation between an ARB and an ACEi in short‐ or long‐term use (4 weeks: MD ‐0.47 mL/min/1.73 m², 95% CI ‐2.73 to 1.79; 12 months: MD 0.18 mL/min/1.73 m², 95% CI ‐0.04 to 0.40).
Overall completeness and applicability of evidence
This systematic review presents clinical evidence of the application of an ACEi or an ARB for preserving residual kidney function in PD patients. However, the evidence provided in these six small RCTs is limited in their completeness and applicability.
Firstly, the primary outcome we had planned to investigate were not adequately addressed in the included studies. The long‐term effect of an ACEi on residual kidney function was only reported in one study comparing with other antihypertensive drugs (Li 2003). For short‐term effects on residual kidney function, only one study reported an ARB compared with other antihypertensive drugs (Zhong 2007a), and the data of short‐term effect of an ACEi on residual kidney function was lacking. In the two studies comparing an ARB with an ACEi, Phakdeekitcharoen 2004 was a cross‐over study of short‐term use (four weeks), and Reyes‐Marin 2012 did not provide any information about allocation and blinding.
Secondly, no detailed analysis was provided addressing the divergence in age, sex, aetiologic factors and dosage of ACEis and ARBs. As a result, related subgroup analysis was not performed as planned. Adverse events such as hypotension and angioedema were not reported in any of the included studies.
Thirdly, it was also noteworthy that four studies (Li 2003; Suzuki 2004; Wang 2005d; Zhong 2007a), which compared an ARB or an ACEi with other antihypertensive drugs, all included Asian participants, limiting the applicability of the evidence presented by the review to other ethnic or racial groups.
Quality of the evidence
Of the six included RCTs, two provided detailed random sequence generation methods (computer generated) and applied adequate allocation concealment (Li 2003; Suzuki 2004). In the other four studies, the allocation approach used by Wang 2005d and Zhong 2007a were obtained through corresponding with the original authors. They also used computer software to generate the sequence, but allocation concealment was not used. With the exception of Reyes‐Marin 2012 which did not provide any information about blinding, other five included studies were open‐label. However, our primary outcome (residual kidney function) were obtained from laboratory tests, and were not likely to be influenced by the blinding of the participants or investigators; BP measurements in four studies (Suzuki 2004; Wang 2005d; Zhong 2007a; Phakdeekitcharoen 2004) might however be influenced. Suzuki 2004 did not report detailed information of patients lost to follow‐up. In Zhong 2007a, two patients withdrew from the study, and two patients were lost to follow‐up with no reasons reported. In the study by Wang 2005d, two patients withdrew from the study, again with no reasons reported. In Li 2003, five deaths occurred and two patients withdrew due to kidney transplantation; it was noteworthy that five patients in the ACEi group discontinued ramipril due to persistent dizziness or cough, which were common side effects of ACEis. In Phakdeekitcharoen 2004, eight patients (27.6%) withdraw and the reasons were provided. Some parameters listed in the Methods were not further addressed, but all included studies reported the primary outcome. Since study protocols were not available, it was difficult to determine whether there was high risk of selective reporting.
Potential biases in the review process
While we have made efforts to identify clinical studies relevant to our topic in electronic searches and clinical trial registers, we cannot deny the possibility that unpublished studies might exist. Since only four studies were included, we did not construct funnel plots to explore reporting biases. All of these studies did not have protocols available on public clinical trial registers, therefore we couldn't assess selective outcomes reporting.
Agreements and disagreements with other studies or reviews
Akbari 2009 evaluated the effects of ACEis and ARBs in PD, but included only two RCTs (Li 2003; Suzuki 2004) to evaluate the effects of an ACEi and an ARB on residual kidney function. Akbari 2009 reported residual kidney function at 12 months and the weighted MD was 0.91 mL/min/1.73 m² (95% CI 0.14 to 1.68), favouring the use of an ACEi and an ARB, which is similar to our study. However, the result of a recent study by Kolesnyk 2011 is not in line with the results of this review. This study is a large, prospective, multicentre cohort study including 451 Dutch participants, which showed that ACEis and ARBs had no additional benefit in preserving residual kidney function over three years of PD treatment (P = 0.52). However, details of changes of six, 12, 24, 36 months of residual kidney function were lacking. Some bias existed such as non‐randomised design, selection bias and attrition bias, which might influence the results of this study. A recent observational study indicated that the absence of an ACEi or an ARB was one of independent risk factors associated with rapidly declining residual kidney function (Herget‐Rosenthal 2012).
Authors' conclusions
Implications for practice.
Compared with other antihypertensive drugs, long‐term use (≥ 12 months) of an ACEi or an ARB showed additional benefits of preserving residual kidney function in CAPD patients. However, limited by the small number of RCTs enrolling small number of participants, there is currently insufficient evidence to support the use of an ACEi or an ARB as first line antihypertensive therapy in PD patients.
Implications for research.
More high quality RCTs are needed to evaluate the benefits and harms of ACEis and ARBs for preserving residual kidney function in PD patients. We recommend addressing the following issues in future studies.
Register trials before implementation
Describe the process of randomised allocation and allocation concealment in detail
Apply blinding when appropriate
Put restrictions on parameters that might greatly influence the outcomes (i.e. PD schedule and dosage of ACEis or ARBs) when setting up the inclusion and exclusion criteria
Report short‐term and long‐term outcomes of clinical significance, such as mortality, residual kidney function, urine volume and adverse events
There are two ongoing studies that are likely to provide useful information to determine which drug (ACEis or ARBs or both) provides better protection of residual kidney function. NCT00721773 will evaluate the effects of effects of benazepril, valsartan or combination of both on residual kidney function in PD patients; and NCT01041963 will study the effect of enalapril and losartan on peritoneal membrane in CAPD patients.
Feedback
Comment: D Daley, S Hsieh, A Tejani, 9 October 2014
Summary
Comment: While there is emerging evidence that residual renal function (RRF) may be correlated with better survival outcomes in the peritoneal dialysis (PD) population, we question the clinical utility of measuring RRF as the primary outcome of this review. We acknowledge the reviewers attempts to elucidate the appropriateness of RRF as a surrogate marker, by citing a previous systematic review as well as studies by Szeto and Maiorca. However, closer inspection of the literature reveal that evidence supporting an association between RRF and mortality is primarily derived from observational studies with a specific purpose not necessarily related to preserving RRF with drugs and the impact on mortality. For example, both articles that were cited as the source for the following statement, “each 1 mL/min of residual GFR is associated with a nearly 50% reduction in mortality rate”, were prospective observational studies assessing the relationship between dialysis adequacy on mortality, rather than directly assessing the effects of RRF on mortality (1, 2) . Maiorca et al. provided no effect estimate on mortality with RRF and simply states that “mean residual renal function significantly improved survival” (2). Whereas, Szeto et al. reported only a relative mortality risk of 0.65 (95% CI: 0.45‐0.94) with a GFR preservation of 1 mL/min when assessed independently from dialysis adequacy, which is a relative mortality risk that is significantly less than what the review authors have stated (1). Both the aforementioned studies assess the risk of mortality with RRF. In other words, these papers have assessed whether mortality increases with worsening RRF. They have not assessed whether improving RRF with a therapy or intervention is predictably correlated with an reduction in mortality. Therefore, RRF remains an unproven surrogate marker for mortality and it is not clear that improvements in RRF lead to a lower risk of mortality. Given the weak association between RRF and mortality from these two studies, and the issues surrounding the utility of RRF as a surrogate, this Cochrane Review may have overemphasized the clinical utility of measuring RRF as their primary outcome, in its attempt to remedy the paucity of clinical guidance on the maintenance of RRF in PD. Additionally, RRF may also be affected by various patient specific factors such as co‐morbidites (e.g. diabetes mellitus) and frequency of use of aminoglycosides (3). The inclusion of studies that do not control for these variables within a review will undoubtedly impact the utility of the findings. Consequently, we believe that applying RRF as a surrogate marker, given its margin of error and questionable clinical utility, may be unwise, and may not merit a comprehensive review. This is further supported by the Cochrane Handbook, which advises against the use of surrogate markers (4). It states that surrogate markers may not accurately predict clinically important outcomes and may potentially mislead readers. Given that one of the primary goals of therapy for dialysis patients with end‐stage renal disease is to prolong survival, we suggest redirecting the approach of this review to address the impact of ACEi and ARB on these more clinically relevant outcomes. The authors’ conclusion states that “[c]ompared with other antihypertensive drugs, long‐term use (>= 12 months) of ACEi or ARBs showed additional benefits of preserving residual kidney function in CAPD patients”. At best, we believe that the types of interventions included in this review only allow for the comparison of ACEi/ARB to “routine treatment” (i.e. PD and supportive treatment), as other antihypertensive drugs were not included for comparison. Furthermore, in order for the claim that ACEi or ARB are superior to other antihypertensive drugs in preserving RRF to be meaningful, the benefits of ACEi/ARB and other antihypertensive agents over placebo on RRF must first be established. In order to address this concern, we propose the following hierarchical approach to address the revised review objective: ACEi + placebo + routine treatment vs placebo + routine treatment ARB + placebo + routine treatment vs placebo + routine treatment Other antihypertensive medication + placebo + routine treatment vs placebo + routine treatment Only when the above effects have been established, will it be appropriate to compare ACEi/ARB (and routine treatment) with other interventions or with each other. The use of this approach in assessing the literature will prevent misleading the reader and/or prevent authors from falsely implying that the treatment effect is clinically relevant before its effect compared to placebo and routine treatment has been established. In addition to adopting a more hierarchical approach to the assessment of literature, we also noted a deviation from the review authors’ protocol that was not acknowledged in their final review. These include the addition of the comparison between “ACEi + routine treatment versus ARB + routine treatment”. The Cochrane Handbook acknowledges that “changes in a review protocol are sometimes necessary” under unforeseen circumstances, and states that “[c]hanges in the protocol should be documented and reported in the ‘Difference between protocol and review’ section of the completed review, and sensitivity analyses … exploring the impact of deviations from the protocol should be undertaken when possible” (4). The review authors’ expressed that the objective was to evaluate the benefits and harms of ACEis and ARBs for preserving RRF in PD patients. We feel that the review authors can be more comprehensive in the assessment of potential harms of these medications observed in the included studies and present this data in a more organized manner. A closer look at the 6 included trials, revealed that the proportion of subjects experiencing cough in Phakdeekitcharoen 2004 was not mentioned in the review. Although the 7 out of 21 subjects who developed mild cough in this study did not discontinue treatment, we feel that this observation was still important to include within the review to better enable the reader to properly weigh the risks of treatment, especially given that the benefit of preserving RRF is still relatively unclear (5). Another observation of cough and dizziness associated with the use of ramipril in Li et al’s study was noted by the review authors in the “Incomplete outcome data” section but not in the “Cough” section of the review. This could easily be missed by readers who scan relevant sections of the article to read. Cough is a well‐known and frequent adverse effect of ACEis. A meta‐analysis of the pooled incidences of ACEi‐induced cough and its associated withdrawal rates revealed rates of 10.60% and 2.54%, respectively (6). Therefore, exclusion of observations from this section of the review article may cause readers to generate a misleading assessment of the actual incidences of cough induced by ACEi and its associated withdrawal rates. As illustrated above, we question the clinical significance of using RRF to assess the benefits of ACEi or ARB in PD patients. To ensure clinical utility of the review data, we propose revising the objective to assess the benefits and harms of using ACEis and ARBs for reducing mortality in PD patients, and to assess the relevant literature via a hierarchical approach as we described above. In addition, we strongly suggest that a more comprehensive report on cough associated with the use of ACEi/ ARB be included in the review and that these observations be summarized under the “Cough” section, such that it is easier for readers to refer to. We hope that our suggestions will improve the clinical utility of this review in an area where there is little data and allow clinicians to more appropriately assess the risks and benefits of using ACEi/ ARB in PD patients. References 1. Szeto, C C, Wong, T Y, Leung, C B, et al. (2000). Importance of dialysis adequacy in mortality and morbidity of chinese capd patients. Kidney international, 58(1), 400‐407
2. Maiorca, R, Brunori, G, Zubani, R, et al. (1995). Predictive value of dialysis adequacy and nutritional indices for mortality and morbidity in capd and hd patients. a longitudinal study. Nephrology, Dialysis, Transplantation, 10(12), 2295‐2305.chinese capd patients. Kidney international, 58(1), 400‐407.2. 3. Singhal MK, Bhaskaran S, Vidgen E, Bargman JM, Vas SI, Oreopoulos DG. Rate of decline of residual renal function in patients on continuous peritoneal dialysis and factors affecting it. Perit Dial Int. 2000 Jul‐Aug;20(4):429‐38. 4. Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. 5. Phakdeekitcharoen B, Leelasa‐nguan P. Effects of an ACE inhibitor or angiotensin receptor blocker on potassium in CAPD patients. Am J Kidney Dis. 2004 Oct;44(4):738‐46. 6. Bangalore S1, Kumar S, Messerli FH. Angiotensin‐converting enzyme inhibitor associated cough: deceptive information from the Physicians' Desk Reference. Am J Med. 2010 Nov;123(11):1016‐30. We certify that we have no affiliations with or involvement in any organisation or entity with a financial interest in the subject matter of our feedback.
Danika Daley, Stephanie Hsieh, Dr Aaron M Tejani
Reply
We would like to thank Danika and her co‐authors for their interest in our review.
We agree that our review had limitations. We found only six small RCTs (all with fewer than 70 subjects) that were eligible for inclusion. Overall, study quality was modest. Although we found some evidence indicating a benefit in residual kidney function resulting associated with long‐term use of ACEi or ARB, we do not believe that these results constitute a reason to change clinical practice, but rather support the need for further research.
We agree that mortality is a more powerful outcome than residual kidney function to evaluate ACEi or ARB efficacy for people receiving peritoneal dialysis. However, we found only one small RCT that reported mortality with only one year follow‐up between ACEi and control group. Therefore, in the absence of robust data, it was not meaningful to evaluate survival benefits of ACEi or ARB for people undergoing peritoneal dialysis.
Preserving residual kidney function is the primary clinical goal for nephrologists who care for people with chronic kidney disease and dialysis patients. Better residual kidney function is associated with enhanced volume balance, phosphorus control and removal of middle molecular uraemic toxins among people on dialysis. There is no doubt that loss of residual kidney function is an independent mortality risk factor among both peritoneal dialysis and haemodialysis patients (Bargman 2001; Shafi 2010). Residual kidney function is a very valuable asset for people on dialysis, and more attention should be focused on how this can be preserved.
Whether residual kidney function is protective or merely a marker for better health remains uncertain. The mechanisms affecting decline of residual kidney function are poorly understood and few studies have examined its preservation using with medical therapy. The best documented factors that play a role in preserving residual kidney function are related to the RAAS (renin‐angiotensin‐aldosterone system) blockade (Patel 2014). Our review showed that ACEi or ARB is associated with better residual kidney function protection than control. Among the studies included in our review all control group participants received antihypertensive drugs other than ACEi or ARB for blood pressure control. Because of widespread need for antihypertensive drugs among people on peritoneal dialysis, it is difficult to observe effects of ACEi or ARB on residual kidney function using a placebo‐control design.
We also agree that residual kidney function could be affected by patient‐specific factors, making it difficult to balance the baseline between ACEi/ARB and control groups in such small sample‐size RCTs, and pointing to the desirability for large sample‐size RCTs. Although an observational cohort study showed survival benefit of ACEi or ARB for people on peritoneal dialysis (Fang 2008), we found insufficient evidence to enable definitive conclusions about benefits.
We excluded Phakdeekitcharoen 2004 from our analysis of cough as an adverse event because no data were reported for the study's ARB group. However, we agree that cough is a significant problem for people receiving ACEi or ARB therapy.
We believe that further large scale, high‐quality RCTs focusing on residual kidney function and mortality relating to long‐term ACEi or ARB therapy are necessary to fully understand their effects on people undergoing peritoneal dialysis.
Contributors
Comments: Danika Daley, Stephanie Hsieh, Dr Aaron M Tejani
Authors: Ling Zhang, Xiaoxi Zeng, Ping Fu
What's new
| Date | Event | Description |
|---|---|---|
| 1 November 2014 | Feedback has been incorporated | Response |
Acknowledgements
We wish to thank:
The Cochrane Renal Group for their help with the search strategy and development of this review.
The referees for their comments and feedback during the preparation of this review.
Appendices
Appendix 1. Electronic search strategies
| Database | Search terms |
| CENTRAL |
|
| MEDLINE |
|
| EMBASE |
|
Appendix 2. Risk of bias assessment tool
| Potential source of bias | Assessment criteria |
|
Random sequence generation Selection bias (biased allocation to interventions) due to inadequate generation of a randomised sequence |
Low risk of bias: Random number table; computer random number generator; coin tossing; shuffling cards or envelopes; throwing dice; drawing of lots; minimization (minimization may be implemented without a random element, and this is considered to be equivalent to being random). |
| High risk of bias: Sequence generated by odd or even date of birth; date (or day) of admission; sequence generated by hospital or clinic record number; allocation by judgement of the clinician; by preference of the participant; based on the results of a laboratory test or a series of tests; by availability of the intervention. | |
| Unclear: Insufficient information about the sequence generation process to permit judgement. | |
|
Allocation concealment Selection bias (biased allocation to interventions) due to inadequate concealment of allocations prior to assignment |
Low risk of bias: Randomisation method described that would not allow investigator/participant to know or influence intervention group before eligible participant entered in the study (e.g. central allocation, including telephone, web‐based, and pharmacy‐controlled, randomisation; sequentially numbered drug containers of identical appearance; sequentially numbered, opaque, sealed envelopes). |
| High risk of bias: Using an open random allocation schedule (e.g. a list of random numbers); assignment envelopes were used without appropriate safeguards (e.g. if envelopes were unsealed or non‐opaque or not sequentially numbered); alternation or rotation; date of birth; case record number; any other explicitly unconcealed procedure. | |
| Unclear: Randomisation stated but no information on method used is available. | |
|
Blinding of participants and personnel Performance bias due to knowledge of the allocated interventions by participants and personnel during the study |
Low risk of bias: No blinding or incomplete blinding, but the review authors judge that the outcome is not likely to be influenced by lack of blinding; blinding of participants and key study personnel ensured, and unlikely that the blinding could have been broken. |
| High risk of bias: No blinding or incomplete blinding, and the outcome is likely to be influenced by lack of blinding; blinding of key study participants and personnel attempted, but likely that the blinding could have been broken, and the outcome is likely to be influenced by lack of blinding. | |
| Unclear: Insufficient information to permit judgement | |
|
Blinding of outcome assessment Detection bias due to knowledge of the allocated interventions by outcome assessors. |
Low risk of bias: No blinding of outcome assessment, but the review authors judge that the outcome measurement is not likely to be influenced by lack of blinding; blinding of outcome assessment ensured, and unlikely that the blinding could have been broken. |
| High risk of bias: No blinding of outcome assessment, and the outcome measurement is likely to be influenced by lack of blinding; blinding of outcome assessment, but likely that the blinding could have been broken, and the outcome measurement is likely to be influenced by lack of blinding. | |
| Unclear: Insufficient information to permit judgement | |
|
Incomplete outcome data Attrition bias due to amount, nature or handling of incomplete outcome data. |
Low risk of bias: No missing outcome data; reasons for missing outcome data unlikely to be related to true outcome (for survival data, censoring unlikely to be introducing bias); missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups; for dichotomous outcome data, the proportion of missing outcomes compared with observed event risk not enough to have a clinically relevant impact on the intervention effect estimate; for continuous outcome data, plausible effect size (difference in means or standardized difference in means) among missing outcomes not enough to have a clinically relevant impact on observed effect size; missing data have been imputed using appropriate methods. |
| High risk of bias: Reason for missing outcome data likely to be related to true outcome, with either imbalance in numbers or reasons for missing data across intervention groups; for dichotomous outcome data, the proportion of missing outcomes compared with observed event risk enough to induce clinically relevant bias in intervention effect estimate; for continuous outcome data, plausible effect size (difference in means or standardized difference in means) among missing outcomes enough to induce clinically relevant bias in observed effect size; ‘as‐treated’ analysis done with substantial departure of the intervention received from that assigned at randomisation; potentially inappropriate application of simple imputation. | |
| Unclear: Insufficient information to permit judgement | |
|
Selective reporting Reporting bias due to selective outcome reporting |
Low risk of bias: The study protocol is available and all of the study’s pre‐specified (primary and secondary) outcomes that are of interest in the review have been reported in the pre‐specified way; the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified (convincing text of this nature may be uncommon). |
| High risk of bias: Not all of the study’s pre‐specified primary outcomes have been reported; one or more primary outcomes is reported using measurements, analysis methods or subsets of the data (e.g. subscales) that were not pre‐specified; one or more reported primary outcomes were not pre‐specified (unless clear justification for their reporting is provided, such as an unexpected adverse effect); one or more outcomes of interest in the review are reported incompletely so that they cannot be entered in a meta‐analysis; the study report fails to include results for a key outcome that would be expected to have been reported for such a study. | |
| Unclear: Insufficient information to permit judgement | |
|
Other bias Bias due to problems not covered elsewhere in the table |
Low risk of bias: The study appears to be free of other sources of bias. |
| High risk of bias: Had a potential source of bias related to the specific study design used; stopped early due to some data‐dependent process (including a formal‐stopping rule); had extreme baseline imbalance; has been claimed to have been fraudulent; had some other problem. | |
| Unclear: Insufficient information to assess whether an important risk of bias exists; insufficient rationale or evidence that an identified problem will introduce bias. |
Data and analyses
Comparison 1. ARBs versus other antihypertensive drugs.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Residual kidney function [mL/min/1.73 m²] | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 3 months | 1 | 44 | Mean Difference (IV, Random, 95% CI) | ‐0.44 [‐1.53, 0.65] |
| 1.2 6 months | 1 | 44 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐1.01, 0.61] |
| 1.3 12 months | 1 | 44 | Mean Difference (IV, Random, 95% CI) | 0.64 [0.19, 1.09] |
| 1.4 24 months | 2 | 66 | Mean Difference (IV, Random, 95% CI) | 1.49 [1.12, 1.86] |
| 1.5 12 to 24 months | 3 | 110 | Mean Difference (IV, Random, 95% CI) | 1.11 [0.38, 1.83] |
| 2 Urinary protein excretion | 2 | 66 | Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.09, 0.06] |
| 3 Kt/V | 2 | 76 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.02, 0.22] |
| 4 Weekly creatinine clearance [mL/wk/1.73 m²] | 3 | 110 | Mean Difference (IV, Random, 95% CI) | 9.06 [‐2.77, 20.90] |
| 5 Systolic BP | 3 | 110 | Mean Difference (IV, Random, 95% CI) | ‐0.67 [‐2.77, 1.42] |
| 6 Diastolic BP | 3 | 110 | Mean Difference (IV, Random, 95% CI) | ‐0.70 [‐2.14, 0.74] |
| 7 Peritonitis | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 8 Serum potassium | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 2. ACEis versus other antihypertensive drugs.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in residual kidney function [mL/min/1.73 m²] | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 12 months | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 All‐cause mortality | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Cardiovascular events | 1 | 120 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.31, 3.27] |
| 3.1 Fatal | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.15, 6.64] |
| 3.2 Non‐fatal | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.22, 4.56] |
| 4 Anuria | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5 Peritonitis | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5.1 All patients | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Treated with an aminoglycoside | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 Not treated with an aminoglycoside | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 3. ARBs versus ACEis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Residual kidney function [mL/min/1.73 m²] | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 1 month | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 12 months | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Cardiovascular events (nonfatal) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Anuria | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Systolic BP | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5 Diastolic BP | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6 Peritonitis | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7 Cough | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 8 Serum potassium | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 9 Hyperkalaemia | 2 | 144 | Risk Ratio (M‐H, Random, 95% CI) | 1.2 [0.40, 3.63] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Li 2003.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A computer‐generated list that was maintained by a third party not involved in the conduct of the study was used for randomization" |
| Allocation concealment (selection bias) | Low risk | Quote: "Investigators were unaware of the randomization schedule when recruiting patients, and both investigators and patients were not blinded during the follow‐up period" |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "open‐label" but the primary outcome (residual kidney function) was not likely to be influenced by the status of blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Analyses were done on an intention‐to‐treat basis". In study group and control group, 4 (death: 3, kidney transplantation: 1) and 3 patients (death: 2, kidney transplantation: 1) withdrew from study respectively. But 5 patients in the ramipril group discontinued drugs due to persistent dizziness or cough |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | CAPD schedules were not provided |
Phakdeekitcharoen 2004.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group 1
Treatment group 2
|
|
| Outcomes |
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information about details of randomisation |
| Allocation concealment (selection bias) | Low risk | Cross‐over study with a 2‐week washout period |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "open‐label" but the primary outcome (residual kidney function) was not likely to be influenced by the status of blinding |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 8 patients (27.6%) withdrew: unwilling to continue the study (2); symptomatic ischaemic heart disease (2); anorexic (2); severe peptic ulcer and sepsis (2) |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Reyes‐Marin 2012.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group 1
Treatment group 2
|
|
| Outcomes |
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information about details of randomisation |
| Allocation concealment (selection bias) | Low risk | Quote: "The participating patients were recruited from the Hospital General ISSEMYM" |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information about blinding |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information about incomplete outcome data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | APD schedules were not provided |
Suzuki 2004.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was performed by using a computer‐generated list maintained by a third party not involved in the conduct of the study" |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomization was performed by using a computer‐generated list maintained by a third party not involved in the conduct of the study" |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "open‐label" but the primary outcome (residual kidney function) was not likely to be influenced by the status of blinding |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The number of patients for analysis was equal to that of participants being allocated. However, no information on patients that withdrew or were lost to follow‐up was provided |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | Free of other bias |
Wang 2005d.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The method for random sequence generation was not reported in the study; but after contacting the original author, we learnt that the random sequence was generated through computer software |
| Allocation concealment (selection bias) | Unclear risk | NS |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "open‐label" but the primary outcome (residual kidney function) was not likely to be influenced by the status of blinding |
| Incomplete outcome data (attrition bias) All outcomes | High risk | In study group, 2 patients withdrew from study, but the reasons for lost‐to‐follow‐up were not known |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | The detailed antihypertensive protocols (other than ACEi and ARB) and CAPD schedules were not provided |
Zhong 2007a.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The method for random sequence generation was not reported in the study; but after contacting the original author, we learnt that the random sequence was generated through computer software |
| Allocation concealment (selection bias) | High risk | Allocation concealment was not applied |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "open‐label" but the primary outcome (residual kidney function) was not likely to be influenced by the status of blinding |
| Incomplete outcome data (attrition bias) All outcomes | High risk | In study group and control group, 2 (lost to follow‐up: 1, kidney transplantation: 1) and 2 patients (lost to follow‐up: 1, changing to HD due to ultrafiltration failure: 1) withdrew from study respectively. But the reasons for lost‐to‐follow‐up were not known |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | The detailed antihypertensive protocols (other than ACEi and ARBs) and CAPD schedules were not provided |
ACEi ‐ angiotensin‐converting enzyme inhibitors; ARB ‐ angiotensin receptor blockers; APD ‐ automated peritoneal dialysis; BP ‐ blood pressure; CAPD ‐ continuous ambulatory peritoneal dialysis; GFR ‐ glomerular filtration rate; NS ‐ not stated; RCT ‐ randomised controlled trial; RRT ‐ renal replacement therapy
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Cioni 2010 | No information about residual kidney function |
| Favazza 1992 | No information about residual kidney function |
| Huang 2002 | No information about residual kidney function |
| Kolesnyk 2011 | Not RCT |
| Nakamoto 2004 | No information about residual kidney function |
| PERFECT Study 1997 | Includes haemodialysis patients |
| Rojas‐Campos 2005 | No information about residual kidney function |
| Shigenaga 2009 | No information about residual kidney function |
| Suzuki 2003 | No information about residual kidney function |
RCT ‐ randomised controlled trial
Characteristics of studies awaiting assessment [ordered by study ID]
Medcalf 2000.
| Methods | Not known |
| Participants | Not known |
| Interventions | Not known |
| Outcomes | Not known |
| Notes | Only abstract published in congress |
Characteristics of ongoing studies [ordered by study ID]
NCT00721773.
| Trial name or title | Effects of benazepril, valsartan or combination of both on residual renal function in peritoneal dialysis patients |
| Methods | Open‐label RCT |
| Participants |
|
| Interventions | Benazepril group:10 to 20 mg daily Valsartan group:80 to 160 mg daily Benazepril plus valsartan group:10‐20 mg benazepril plus 80 to 60 mg valsartan daily Control group: antihypertensive drugs except ACEi and ARB |
| Outcomes | Primary outcome: residual kidney function Secondary outcomes: Kt/V; weekly creatinine clearance; peritoneal membrane function; blood pressure; time to anuria; death |
| Starting date | September 2008 |
| Contact information | Xueqing Yu, M.D.& Ph.D. Phone:8620‐87766335 Email: yuxq@mail.sysu.edu.cn Haiping Mao, M.D.& Ph.D. Phone:8620‐87755766 ext 8143 Email: haipingmao@126.com |
| Notes | Target blood pressure: 120‐140/70‐90 mm Hg |
NCT01041963.
| Trial name or title | The effect of enalapril and losartan on peritoneal membrane in continuous ambulatory peritoneal dialysis patients |
| Methods | Open‐label RCT |
| Participants |
|
| Interventions | Enalapril group: 20 to 40 mg daily Enalapril plus losartan group: enalapril 20 to 40 mg plus losartan 25 to 50 mg daily Control group: antihypertensive drugs except ACEi, ARB or spironolactone |
| Outcomes | Primary outcomes: change in dialysate CA‐125; modified peritoneal equilibrium test Secondary outcomes: dialysis adequacy; residual kidney function; hospitalisation; peritonitis episodes; any adverse drug effects; death from any cause |
| Starting date | June 2009 |
| Contact information | Talerngsak Kanjanabuch |
| Notes | Target blood pressure: 130/80 mm Hg |
ACEi ‐ angiotensin‐converting enzyme; ARB ‐ angiotensin receptor blocker; CAPD ‐ continuous ambulatory peritoneal dialysis
Differences between protocol and review
The following outcomes have been added to the review: anuria, potassium levels; peritonitis
Contributions of authors
Draft the protocol: Ling Zhang, Xiaoxi Zeng, Ping Fu, Hong Mei Wu
Study selection: Xiaoxi Zeng, Ling Zhang
Extract data from studies: Xiaoxi Zeng, Ling Zhang
Enter data into RevMan: Xiaoxi Zeng, Ling Zhang
Carry out the analysis: Xiaoxi Zeng, Ling Zhang, Ping Fu
Interpret the analysis: Xiaoxi Zeng, Ling Zhang, Hong Mei Wu
Draft the final review: Xiaoxi Zeng, Ling Zhang, Ping Fu
Disagreement resolution: Ping Fu, Hong Mei Wu
Update the review: Xiaoxi Zeng, Ling Zhang
Declarations of interest
Ling Zhang: none known
Xiaoxi Zeng: none known
Ping Fu: none known
Hong Mei Wu: none known
Edited (no change to conclusions), comment added to review
References
References to studies included in this review
Li 2003 {published data only}
- Li PK, Chow K, Wong TY, Leung C, Szeto CC. Effects of an angiotensin‐converting enzyme inhibitor on residual renal function in patients receiving peritoneal dialysis. A randomized, controlled study. Annals of Internal Medicine 2003;139(2):105‐12. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Li PK, Chow K, Wong TY, Leung C, Szeto CC. Preservation of residual renal function in peritoneal dialysis patients by angiotensin‐converting‐enzyme inhibitor ‐ a prospective study [abstract no: F‐FC004]. Journal of the American Society of Nephrology 2002;13(September, Program & Abstracts):1a. [CENTRAL: CN‐00446373] [Google Scholar]
Phakdeekitcharoen 2004 {published data only}
- Phakdeekitcharoen B, Leelasa‐nguan P. Effects of an ACE inhibitor or angiotensin receptor blocker on potassium in CAPD patients. American Journal of Kidney Diseases 2004;44(4):738‐46. [MEDLINE: ] [PubMed] [Google Scholar]
Reyes‐Marin 2012 {published data only}
- Reyes‐Marin FA, Calzada C, Ballesteros A, Amato D. Comparative study of enalapril vs. losartan on residual renal function preservation in automated peritoneal dialysis. A randomized controlled study. Revista de Investigacion Clinica 2012;64(4):315‐21. [MEDLINE: ] [PubMed] [Google Scholar]
Suzuki 2004 {published data only}
- Suzuki H, Kanno Y, Sugahara S. Effects of an angiotensin II receptor blocker, valsartan, on residual renal function in patients on CAPD. American Journal of Kidney Diseases 2004;43(6):1056‐64. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Wang 2005d {published data only}
- Wang J, Xiao MY. Protective effects of valsartan on residual renal function in patients on CAPD. Chinese Journal of Blood Purification 2005;4(11):605‐6. [Google Scholar]
Zhong 2007a {published data only}
- Zhong H, Sha CH, Sui TL, Qiu HY, Liu F, Qin W, et al. Effects of irbesartan on residual renal function in peritoneal dialysis patients. Chinese Journal of Nephrology 2007;23(7):413‐6. [Google Scholar]
References to studies excluded from this review
Cioni 2010 {published data only}
- Cioni A, Sordini C, Cavallini I, Bigazzi R, Vito M, Campese VM. Angiotensin receptor blocker telmisartan improves insulin sensitivity in peritoneal dialysis patients. Peritoneal Dialysis International 2010;30(1):66‐71. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Favazza 1992 {published data only}
- Favazza A, Motanaro D, Messa P, Antonucci F, Gropuzzo M, Mioni G. Peritoneal clearances in hypertensive CAPD patients after oral administration of clonidine, enalapril, and nifedipine. Peritoneal Dialysis International 1992;12(3):287‐91. [MEDLINE: ] [PubMed] [Google Scholar]
Huang 2002 {published data only}
- Huang YH. Effect of angiotensin‐converting enzyme inhibitors on serum levels of erythropoietin in patients on peritoneal dialysis. Di Yi Junyi Daxue Xuebao 2002;22(1):74‐5. [MEDLINE: ] [PubMed] [Google Scholar]
Kolesnyk 2011 {published data only}
- Kolesnyk I, Noordzij M, Dekker FW, Boeschoten EW, Krediet RT. Treatment with angiotensin II inhibitors and residual renal function in peritoneal dialysis patients. Peritoneal Dialysis International 2011;31(1):53‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Nakamoto 2004 {published data only}
- Nakamoto H, Kanno Y, Okada H, Suzuki H. Erythropoietin resistance in patients on continuous ambulatory peritoneal dialysis. Advances in Peritoneal Dialysis 2004;20:111‐6. [MEDLINE: ] [PubMed] [Google Scholar]
PERFECT Study 1997 {published data only}
- Collins JF, Robson R, MacMahon S, Bailey RR, PERFECT Study Group. Safety and efficacy of enalapril and simvastatin in dialysis patients [abstract]. 6th Asian Pacific Congress of Nephrology; 1995 Dec 5‐9; Hong Kong. 1995:144. [CENTRAL: CN‐00460572]
- Robson R, Collins J, Johnson R, Kitching R, Searle M, Walker R, et al. Effects of simvastatin and enalapril on serum lipoprotein concentrations and left ventricular mass in patients on dialysis. The Perfect Study Collaborative Group. Journal of Nephrology 1997;10(1):33‐40. [MEDLINE: ] [PubMed] [Google Scholar]
- Robson R, Collins J, Kitchings R, Searle M, Walker R, Sharpe N, et al. A randomized controlled trial of simvastatin and enalapril in dialysis patients: effects on serum lipoproteins and left ventricular mass [abstract]. Journal of the American Society of Nephrology 1994;5(3):526. [CENTRAL: CN‐00550525] [Google Scholar]
- Robson RA, Collins J, Walker RJ, MacMahon S. A randomised controlled trial of simvastatin and enalapril in dialysis patients: effects on serum lipoproteins and left ventricular mass [abstract]. ISN XIII International Congress of Nephrology; 1995 Jul 2‐6; Madrid, Spain. 1995:530. [CENTRAL: CN‐00509440]
- Walker RJ, Sutherland WH, Walker H. Simvastatin and cholesteryl ester transfer (CET) activity in renal failure (RF) [abstract]. ISN XIII International Congress of Nephrology; 1995 Jul 2‐6; Madrid, Spain. 1995:529. [CENTRAL: CN‐00509553]
- Walker RJ, Sutherland WH, Walker H, Robson RA, MacMahon SA. The effects of simvastatin and enalapril on plasma cholesteryl ester transfer (CET) activity in renal failure (RF) [abstract]. 6th Asian Pacific Congress of Nephrology; 1995 Dec 5‐9; Hong Kong. 1995:28. [CENTRAL: CN‐00461958]
- Walker RJ, Sutherland WH, Walker HL, MacMahon S, Robson RA. Effect of treatment with simvastatin on serum cholesteryl ester transfer in patients on dialysis. PERFECT Study Collaborative Group. Nephrology Dialysis Transplantation 1997;12(1):87‐92. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Rojas‐Campos 2005 {published data only}
- Rojas‐Campos E, Cortes‐Sanabria L, Martinez‐Ramirez HR, Gonzalez L, Martin‐del‐Campo F, Gonzalez‐Ortiz M, et al. Effect of oral administration of losartan, prazosin, and verapamil on peritoneal solute transport in continuous ambulatory peritoneal dialysis patients. Peritoneal Dialysis International 2005;25(6):576‐82. [MEDLINE: ] [PubMed] [Google Scholar]
- Rojas‐Campos E, Martinez‐Ramirez H, Cortes‐Sanabria L, Camacho R, Martin‐del‐Campo F, Cueto‐Manzano AM. Oral verapamil increases ultrafiltration and peritoneal small solute clearance of CAPD patients [abstract no: SA‐FC130]. Journal of the American Society of Nephrology 2005;16:110A. [CENTRAL: CN‐00583927] [Google Scholar]
Shigenaga 2009 {published data only}
- Shigenaga A, Tamura K, Dejima T, Ozawa M, Wakui H, Masuda S, et al. Effects of angiotensin II type 1 receptor blocker on blood pressure variability and cardiovascular remodeling in hypertensive patients on chronic peritoneal dialysis. Nephron Clinical Practice 2009;112(1):c31–c40. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Suzuki 2003 {published data only}
- Suzuki H, Nakamoto H, Okada H, Sugahara S, Kanno Y. A selective angiotensin receptor antagonist, valsartan, produced regression of left ventricular hypertrophy associated with a reduction of arterial stiffness. Advances in Peritoneal Dialysis 2003;19:59‐66. [MEDLINE: ] [PubMed] [Google Scholar]
References to studies awaiting assessment
Medcalf 2000 {published data only}
- Medcalf JF, Carr S, Walls J, Harris KP. The effect of ACE Inhibitors and AII receptor antagonists on erythrocytosis in patients on CAPD taking EPO [abstract]. 37th Congress. European Renal Association. European Dialysis and Transplantation Association; 2000 Sept 17‐20; Nice, France. 2000:235. [CENTRAL: CN‐00461288]
References to ongoing studies
NCT00721773 {published data only}
- NCT00721773. Effects of benazepril, valsartan or combination of both on residual renal function in peritoneal dialysis patients. http://clinicaltrials.gov/ct2/show/NCT00721773 (accessed 12 June 2014).
NCT01041963 {published data only}
- NCT01041963. The effect of enalapril and losartan on peritoneal membrane in continuous ambulatory peritoneal dialysis patients. http://clinicaltrials.gov/ct2/show/NCT01041963 (accessed 12 June 2014).
Additional references
Akbari 2009
- Akbari A, Knoll G, Ferguson D, McCormick B, Davis A, Biyani M. Angiotensin‐converting enzyme inhibitors and angiotensin receptor blockers in peritoneal dialysis: systematic review and meta‐analysis of randomized controlled trials. Peritoneal Dialysis International 2009;29(5):554–61. [MEDLINE: ] [PubMed] [Google Scholar]
Bargman 2001
- Bargman JM, Thorpe KE, Churchill DN. Relative contribution of residual renal function and peritoneal clearance to adequacy of dialysis: a reanalysis of the CANUSA study. Journal of the American Society of Nephrology 2001;12(10):2158‐62. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Blake 2001
- Blake PG. Integrated end‐stage renal disease care: the role of peritoneal dialysis. Nephrology Dialysis Transplantation 2001;16 Suppl 5:61‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Cancarini 1986
- Cancarini G, Bunori G, Camererini C, Brasa S, Manili L, Maiorca R. Renal function recovery and maintenance of residual diuresis in CAPD and hemodialysis. Peritoneal Dialysis Bulletin 1986;6(2):77‐9. [EMBASE: 1986213696] [Google Scholar]
Cueto‐Manzano 2003
- Cueto‐Manzano AM. Peritoneal dialysis in Mexico. Kidney International 2003;83(Suppl):S90‐2. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Fang 2008
- Fang W, Oreopoulos DG, Bargman JM. Use of ACE inhibitors or angiotensin receptor blockers and survival in patients on peritoneal dialysis. Nephrology Dialysis Transplantation 2008;23(11):3704‐10. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Fenton 1997
- Fenton SS, Schaubel DE, Desmeules M, Morrison HI, Mao Y, Copleston P, et al. Hemodialysis versus peritoneal dialysis: a comparison of adjusted mortality rates. American Journal of Kidney Diseases 1997;30(3):334‐42. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Gokal 1999
- Gokal R, Figueras M, Olle A, Rovira J, Badia X. Outcomes in peritoneal dialysis and haemodialysis‐a comparative assessment of survival and quality of life. Nephrology Dialysis Transplantation 1999;14 Suppl 6:24‐30. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Heaf 2002
- Heaf JG, Lokkegaard H, Madsen M. Initial survival advantage of peritoneal dialysis relative to haemodialysis. Nephrology Dialysis Transplantation 2002;17(1):112‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Herget‐Rosenthal 2012
- Herget‐Rosenthal S, Ostrowski M, Kribben A. Definition and risk factors of rapidly declining residual renal function in peritoneal dialysis: an observational study. Kidney & Blood Pressure Research 2012;35(4):233‐41. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Kolesnyk 2007
- Kolesnyk I, Dekker FW, Noordzij M, Cessie S, Struijk DG, Krediet RT. Impact of ACE inhibitors and AII receptor blockers on peritoneal membrane transport characteristics in long‐term peritoneal dialysis patients. Peritoneal Dialysis International 2007;27(4):446‐53. [MEDLINE: ] [PubMed] [Google Scholar]
Li 1999
- Li PK, Szeto CC, Law MC, Chau KF, Fung KS, Leung CB, et al. Comparison of double‐bag and Y‐set disconnect systems in continuous ambulatory peritoneal dialysis: a randomized prospective multicenter study. American Journal of Kidney Diseases 1999;33(3):535‐40. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Li 2001a
- Li PK, Szeto CC. Adequacy targets of peritoneal dialysis in the Asian population. Peritoneal Dialysis International 2001;21 Suppl 3:S378‐83. [MEDLINE: ] [PubMed] [Google Scholar]
Li 2001b
- Li LP, Chow KM. The cost barrier to peritoneal dialysis in the developing world‐an Asian perspective. Peritoneal Dialysis International 2001;2001(21 Suppl 3):S307‐13. [MEDLINE: ] [PubMed] [Google Scholar]
Maiorca 1995
- Maiorca R, Brunori G, Zubani R, Cancarini GC, Manili L, Camerini C, et al. Predictive value of dialysis adequacy and nutritional indices for mortality and morbidity in CAPD and HD patients. A longitudinal study. Nephrology Dialysis Transplantation 1995;10(12):2295‐305. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Moist 2000
- Moist LM, Port FK, Orzol SM, Young EW, Ostbye T, Wolfe RA, et al. Predictors of loss of residual renal function among new dialysis patients. Journal of the American Society of Nephrology 2000;11(3):556‐64. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Patel 2014
- Patel N, Hu SL. Preserving residual renal function in dialysis: What we know. Seminars in Dialysis 2014;9(18):epub. [DOI: 10.1111/sdi.12302] [DOI] [PubMed] [Google Scholar]
Schaubel 2000
- Schaubel DE, Fenton SS. Trends in mortality on peritoneal dialysis: Canada. Journal of the American Society of Nephrology 2000;11(1):126‐33. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Shafi 2010
- Shafi T, Jaar BG, Plantinga LC, Fink NE, Sadler JH, Parekh RS, et al. Association of residual urine output with mortality, quality of life, and inflammation in incident hemodialysis patients: the Choices for Healthy Outcomes in Caring for End‐Stage Renal Disease (CHOICE) Study. American Journal of Kidney Diseases 2010;56(2):348‐58. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shemin 2000
- Shemin D, Bostom AG, Lambert C, Hill C, Kitsen J, Kliger AS. Residual renal function in a large cohort of peritoneal dialysis patients: change over time, impact on mortality and nutrition. Peritoneal Dialysis International 2000;20(4):439‐44. [MEDLINE: ] [PubMed] [Google Scholar]
Suzuki 2003a
- Suzuki H, Nakamoto H, Okada H, Sugahara S, Kanno Y. A selective angiotensin receptor antagonist, Valsartan, produced regression of left ventricular hypertrophy associated with a reduction of arterial stiffness. Advances in Peritoneal Dialysis 2003;19:59‐66. [MEDLINE: ] [PubMed] [Google Scholar]
Suzuki 2003b
- Suzuki T, Kanno Y, Nakamoto N, Okada H, Sugahara S, Suzuki H. Peritoneal dialysis versus hemodialysis: A five‐year comparison of survival and effects on the cardiovascular system, erythropoiesis, and calcium metabolism. Advances in Peritoneal Dialysis 2003;19:148‐54. [MEDLINE: ] [PubMed] [Google Scholar]
Szeto 2000
- Szeto CC, Wong TY, Leung CB, Wang AY, Law MC, Lui SF, et al. Importance of dialysis adequacy in mortality and morbidity of Chinese CAPD patients. Kidney International 2000;58(1):400‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Termorshuizen 2003
- Termorshuizen F, Korevaar JC, Dekker FW, Manen JG, Boeschoten EW, Krediet RT. Hemodialysis and peritoneal dialysis: comparison of adjusted mortality rates according to the duration of dialysis: analysis of The Netherlands Cooperative Study on the Adequacy of Dialysis. Journal of the American Society of Nephrology 2003;14(11):2851‐60. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
USRDS 2003
- US Renal Data System. USRDS 2003 annual report: atlas of end‐stage renal disease in the United States. Bethesda, MD, 2003. http://www.usrds.org/atlas03.aspx (accessed 12 June 2014):78‐80.
Venkataraman 2000
- Venkataraman V, Nolph KD. Preservation of residual renal function‐an important goal. Peritoneal Dialysis International 2000;20(4):392‐5. [MEDLINE: ] [PubMed] [Google Scholar]
Williams 2002
- Williams JD, Craig KJ, Topley N, Ruhland C, Fallon M, Newman GR, et al. Morphologic changes in the peritoneal membrane of patients with renal disease. Journal of the American Society of Nephrology 2002;13(2):470‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Zhang 2011
- Zhang L, Zeng X, Fu P, Wu HM. Angiotensin converting enzyme inhibitors and angiotensin II receptor blockers for preserving residual kidney function in peritoneal dialysis patients. Cochrane Database of Systematic Reviews 2011, Issue 5. [DOI: 10.1002/14651858.CD009120] [DOI] [PMC free article] [PubMed] [Google Scholar]


