Abstract
Background:
As many patients view conventional antidepressants and anxiolytics negatively, it is not surprising that the willingness to apply these treatments is far from ideal, thus posing a critical barrier in promoting an effective and durable treatment.
Aim:
The present study aimed to explore patients’ attitudes toward conventional and herbal treatments for depression and anxiety, while considering cultural and demographic factors, to further elucidate the antecedes that putatively determine the treatment’s outcome.
Methods:
During June 2017, a cross-sectional survey was conducted using stratified sampling from a large-scale Israeli volunteer online panel. The final sample included 591 Jewish Israeli adults that reported they were suffering from depression or anxiety.
Results:
A heterogeneous range of attitudes toward treatment was found: for example, a large group of patients did not utilize prescription medications (39%), a professional consultation (12.9%), or any form of treatment (17.4%). Interestingly, these patients were significantly more likely to support naturally-derived treatments and were less concerned with scientific proof. Further, adverse effects were demonstrated as a prominent factor in the choice of treatment. A higher incidence of adverse effects was associated with an increased willingness to consider an alternative herbal treatment. Noteworthy attitudes were found in orthodox-Jewish individuals, who showed similar consultation rates, but utilized more psychological, rather than pharmacological treatments.
Conclusions:
It is proposed that patients’ perspectives and cultural backgrounds are needed to be taken into consideration during the clinical assessment and choice of treatment. The findings imply that a particular emphasis should be placed on patients that discard conventional pharmacological options and on distinct cultural aspects. Several recommendations for revising the current policy are advocated to promote more culturally-informed and patient-oriented care.
Keywords: Depression, anxiety, attitudes, survey, antidepressants, anxiolytics, herbal treatment, orthodox-Jews
Introduction
Depression and anxiety disorders are debilitating conditions that lead to considerable emotional and physical impairments (Mykletun et al., 2009; Wittchen et al., 2000) and impose substantial societal and economical costs (Whiteford et al., 2013). The worldwide lifetime prevalence of the disorders has been estimated at 10% to 15% for depression (Lépine & Briley, 2011), and at ~12.9% for any anxiety disorder (Steel et al., 2014). Taken together, the importance of developing efficacious treatments is emphasized. Unfortunately, promoting such treatments does not necessarily ensure convalescence; factors such as accessibility, price, and willingness might preempt a feasible recovery. Indeed, many patients do not adhere or categorically refuse to consume conventional pharmacotherapies for depression and anxiety (Ayalon et al., 2011; Sawada et al., 2009; Shigemura et al., 2010). Further, it has been demonstrated that the initiation of antidepressant treatment is highly dependent on the patient’s agreement with the assigned treatment (Raue et al., 2009). Hence, exploring patients’ attitudes is crucial in pursuance of sustainable interventions. The present research was aimed to yield novel insights on this subject, in pursuing the promotion of patient-oriented and culturally-informed care that can improve adherence and even efficacy. The study aimed to so by expanding the understanding of depression and anxiety patients’ attitudes toward treatment, using a cross-sectional web-survey in the Israeli population.
Drugs from the selective serotonin reuptake inhibitors [(SSRIs); for example, escitalopram, sertraline, fluoxetine], and the serotonin-norepinephrine reuptake inhibitors [(SNRIs); for example, venlafaxine, duloxetine] classes are widely acknowledged as first-line pharmacological treatments for both depression (Lam et al., 2016) and anxiety disorders (Baldwin et al., 2011). Anxiety disorders are highly comorbid with depression (Lamers et al., 2011). A major advantage of SSRIs and SNRIs is that they address both psychopathologies. However, these drugs have also been associated with various and highly frequent adverse effects such as weight gain (only in SSRIs), sexual dysfunction, headaches, and nausea (Cascade et al., 2009; Lam et al., 2016). Adverse effects were specified by patients as one of the leading reasons for treatment discontinuation (Lin et al., 1995; MacGillivray et al., 2003). Moreover, the United States Food and Drug Administration (FDA) has issued a requirement for ‘black-box warnings’ regarding an increased risk for suicidal ideation and behavior on all antidepressants for children, adolescents, and young adults (Lenzer, 2006; Stone et al., 2009). Additionally, more than half of the patients with depression or anxiety do not achieve symptoms remission with these drugs (Baldwin et al., 2011; Rush et al., 2006).
The shortfalls of existing antidepressants and anxiolytics are not the sole factor stimulating recipients’ criticism and disapproval; there is also a sturdy resistance to psychiatric phenomenology and methods, influenced by ideas surging from the 1960s antipsychiatry movement (Rissmiller & Rissmiller, 2006). This agenda is manifested in both views of the general public and patients’ attitudes toward psychiatric treatments (e.g. the common perception that antidepressants and anxiolytics might be harmful) (Britten, 1994; Chakraborty et al., 2009; Jorm et al., 1997). Similarly, several minority- and religious-groups show lower utilization rates of mental health services (Alegría et al., 2008; Koopmans et al., 2013), and in some cases view psychiatric treatments as non-relevant, ineffective or even offensive (Roman et al., 2008; Schraufnagel et al., 2006). Some of the orthodox Jewish groups in Israel maintain similar opposing agendas (Coleman-Brueckheimer & Dein, 2011; Freund & Band-Winterstein, 2017) that should be further explored, for the aim of facilitating effective and culturally-informed care.
Recent in vivo and in vitro studies demonstrated a notable therapeutic potential of several herbal medications for depression and anxiety, with fewer adverse effects (Burstein et al., 2017; Doron et al., 2018, 2019; Russo et al., 2014; Sarris & Kavanagh, 2009; Yeung et al., 2014). Frequent use of such phytotherapies was observed among individuals with depression or anxiety (Kessler et al., 2001; Pan et al., 2013).
It is postulated that patients’ attitudes toward their assigned treatment at least partially explain pursuance, adherence, and efficacy. To the best of our knowledge, patients’ attitudes toward scientifically supported herbal medications for depression and anxiety have not been previously investigated. The Jewish Israeli society with its cultural and demographic heterogeneity presents a unique opportunity for elucidating how different sub-cultures construct attitudes toward treatment. The present study aimed to explore the attitudes and preferences among adult Israeli individuals with depression or anxiety, while primarily probing perceptions vis-à-vis herbal and conventional treatments. Understanding these attitudes will then be considered from both a therapeutic and a cultural stance, in ways that may promote treatment outcomes and patients’ trust.
Methods
Participants
Data was collected by Geocartography Knowledge Group from members of an Israeli general population pre-recruited volunteer online panel, consisting of 153,533 individuals. Panel members granted written informed consent to participate in online surveys for a modest monetary reward. Participants registered individually to an online platform. The platform authenticated their identity and ensured each participant can respond to each survey once. The sample frame was obtained by randomly sampling 13,200 individuals from the panel. Stratified sampling was utilized to ensure proportionate representation of each sub-group of the adult (age ⩾ 18) Jewish Israeli population (classified by gender, age, geographical region, income, education, and religiosity). Subsequently, screening was conducted to identify participants with depression or anxiety; 7,068 responders initiated the screening, and 6,918 completed it, from which 616 were identified as suffering from depression or an anxiety disorder and qualified for the attitudes survey. From the final sample of 616 responders, 591 completed the entire survey. Only participants that responded to all items were included in the analysis (see Figure 1 for a flow-chart depicting the sample’s derivation). The survey was conducted in the first week of June 2017. Here we present the main findings from the survey.
Figure 1.
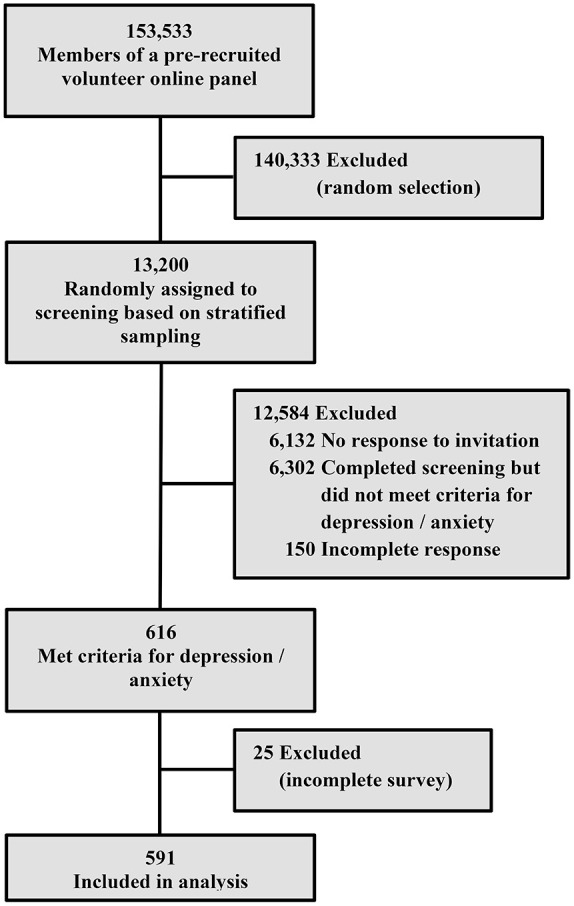
A flow-chart depicting the sample’s derivation.
This study has been approved by the ethics committee of The Academic College Tel-Aviv-Yaffo and has been performed according to the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Response metrics
Following the recommendations for the report of online surveys, the relevant response metrics were calculated (The American Association for Public Opinion Research, 2016). The participation rate, ‘defined as the number of respondents who have provided a usable response divided by the total number of initial personal invitations requesting participation’ (p. 49), was 52.4% for the screening phase (6,918 completed screening/13,200 received the initial invitation) and 96% for the survey phase (591 completed the survey/616 eligible survey participants). The study-specific eligibility rate, representing the proportion of responders that completed the screening and qualified from the total responders that completed the screening (Callegaro & Disogra, 2008), was 8.9% (616 completed the screening and qualified/[6,302 completed the screening and did not qualify + 616 completed the screening and qualified]). In this case, the study-specific eligibility rate serves as an estimate of the point prevalence for depression or an anxiety disorder in the sample.
Questionnaires
Self-report structured questionnaires were designed ad hoc for this study. They were written in Hebrew and accommodated for an online application. Members of the online panel received an e-mail with an invitation to answer the survey through the online platform. In the screening phase responders were required to report whether they were currently suffering from depression or an anxiety disorder. The diagnoses were validated using a DSM-5-based symptoms questionnaire for major depressive disorder (American Psychiatric Association, 2013) and the 7-item Generalized Anxiety Disorder Scale (GAD-7) (Spitzer et al., 2006). Responders who declared they suffer from depression and stated the presence of at least four out of the nine symptoms of major depressive disorder during the same two-week period; and responders who declared they suffer from anxiety and had a GAD-7 score of at least five (representing a cutoff score of mild symptoms or worse) (Spitzer et al., 2006), were eligible for the attitudes questionnaire.
The attitudes questionnaire consisted of 27 items pertaining to socio-demographic characteristics, attitudes toward conventional and herbal treatments for depression/anxiety, the current treatment for depression/anxiety, and the perceived outcomes of the treatment.
Statistical analysis
Results are expressed as percentages and frequencies for nominal variables, or as means and standard errors for continuous variables. For statistical analyses, chi-squared tests and independent samples t-tests were applied as indicated. Significance was assumed as p < .05. Post-hoc analyses were conducted using the Bonferroni correction.
Results
Sample characteristics
In the final sample of 591 Jewish Israeli participants there were 215 males (36.4%) and 376 females (63.6%). Most of the participants were aged 25 to 44 (n = 301, 51%). Participants were geographically dispersed: 129 (21.8%) were from the North, 214 (36.2%) were from the Center (Gush Dan area) and others were from the Jerusalem area (n = 76, 12.9%), the South (n = 98, 16.6%), and the Sharon plain (n = 74, 12.5%). Most of the participants had one college degree or more (n = 280; 47.4%); 107 participants (24.9%) had an associate’s degree, 153 (25.9%) had high school education or less, and the others studied at a Talmudic college (n = 11, 1.9%). The majority was secular (n = 366, 61.9%), and others were traditional (n = 144, 24.4%), religious (n = 52, 8.8%) or orthodox (n = 29, 4.9%). Regarding socioeconomic status, most of the participants reported their income was below average (n = 257, 43.5%). The rest reported on average income (n = 158, 26.7%), above average income (n = 146, 24.7%), and 30 participants (5.1%) declined to respond.
Type of treatment
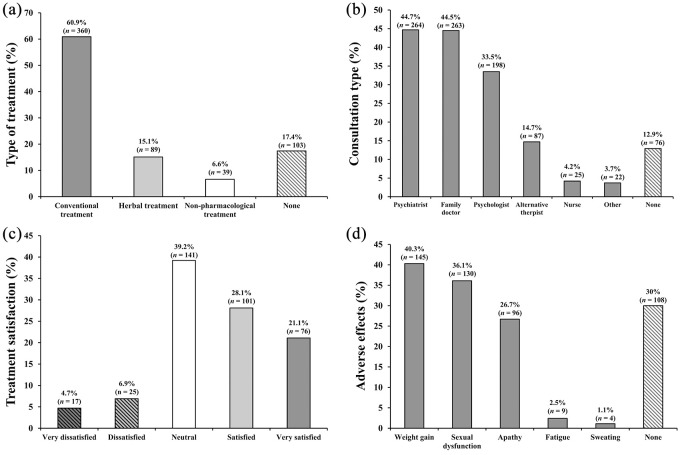
The most common current type of treatment for depression or anxiety among the responders of this survey was a conventional prescription medication (60.9%). 15.1% reported on treatment with an herbal substance (without a prescription medication), while 6.6% of the responders applied a non-pharmacological treatment (i.e., cognitive-behavioral therapy [CBT], psychotherapy, etc.) as a sole intervention. 17.4% of the responders reported they did not receive any treatment (see Figure 2(a)). Among the responders receiving a conventional treatment, 13.1% (n = 47) also reported using an herbal treatment, 11.9% (n = 43) combined the conventional treatment with a non-pharmacological one, and 8.1% (n = 29) utilized a concurrent conventional, herbal, and non-pharmacological polytherapy.
Figure 2.
Treatment-related characteristics among responders suffering from depression or anxiety: (a) treatments distribution. N = 591 (b) responders commonly consulted with a psychiatrist, a family doctor, and a psychologist (respectively); 12.9% did not seek any consultation. Multiple responses were allowed; hence, cumulative percentage precedes 100%. N = 591 (c) treatment satisfaction among responders receiving prescription medication. n = 360 (d) Prevalence rates of adverse effects due to an antidepressant/anxiolytic treatment. Multiple responses were allowed; hence, cumulative percentage precedes 100%. n = 360.
For further analyses responders were classified into four treatment groups: (1) conventional treatment (CT); (2) herbal treatment without conventional one (HT); (3) non-pharmacological treatment only (NPT); and (4) no treatment (NT).
Professional consultation
Of the 591 responders, 87.1% reported they have consulted with a professional regarding their condition. The distribution of consultation types is presented in Figure 2(b).
A significant difference was found in consultation rates (χ2(3) = 150.4, p < .0001) between patients from the different treatment groups (see Table 1), suggesting that the HT and NPT groups tended to seek less consultation compared to the CT group and that the NT group was much less likely to seek consultation compared to all the other groups.
Table 1.
Comparisons between treatment groups.
| Item | Conventional treatment (n = 360) | Herbal treatment (n = 89) | Non-pharmacological treatment (n = 39) | No treatment (n = 103) | p | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| Consultation rate # | 356 | 98.9a | 69 | 77.5b | 34 | 87.2b | 56 | 54.4c | <.0001 |
| Prominent factor for treatment | <.0001 | ||||||||
| Less adverse effect | 181 | 50.3a | 29 | 32.6b | 16 | 41a,b | 41 | 39.8a,b | |
| Scientifically proven as effective | 115 | 31.9a | 13 | 14.6b | 6 | 15.4a,b | 19 | 18.4b | |
| Natural compound | 33 | 9.2a | 31 | 34.8b | 12 | 30.8b | 23 | 22.3b | |
| Reasonable price | 17 | 4.7 | 7 | 7.9 | 0 | 0 | 7 | 6.8 | ns |
| Other | 14 | 3.9 | 9 | 10.1 | 4 | 10.3 | 8 | 7.8 | ns |
| I don’t know | 0 | 0a | 0 | 0a,b | 1 | 2.6b | 5 | 4.9b | |
| Consider herbal treatment ^ | =.002 | ||||||||
| Certainly yes | 115 | 31.9a | 24 | 27.0a,b | 8 | 20.5a,b | 14 | 13.6b | |
| Probably yes | 181 | 50.3 | 47 | 52.8 | 18 | 46.2 | 55 | 53.4 | ns |
| Probably not | 34 | 9.4 | 8 | 9.0 | 4 | 10.3 | 10 | 9.7 | ns |
| Certainly not | 5 | 1.4 | 1 | 1.1 | 2 | 5.1 | 3 | 2.9 | ns |
| I don’t know | 25 | 6.9a | 9 | 10.1a,b | 7 | 17.9a,b | 21 | 20.4b | |
Note. Different superscript letters denote significant differences between the groups at p < .05 following a Bonferroni correction. ns = Not significant. N = 591.
Consultation rate refers to the frequency of responders that received any kind of professional consultation for depression or anxiety.
Item: ‘To what extend would you consider purchasing an herbal treatment that was scientifically proven as effective for the treatment of depression/anxiety, and is natural and without adverse effects?’.
Satisfaction with conventional treatment
Among the 360 responders treated with a conventional medication for their depression or anxiety, 49.2% reported they were satisfied or very satisfied, 39.2% were neutral and 11.6% were dissatisfied or very dissatisfied with the assigned treatment (see Figure 2(c)). Among neutral and dissatisfied responders, the focal reasons for dissatisfaction were ineffectiveness (neutral: 48.9%, n = 69; dissatisfied: 69%, n = 29) and adverse effects (neutral: 28.4%, n = 40; dissatisfied: 23.8%, n = 10).
The prevalence rates of adverse effects attributed to antidepressants and anxiolytics, in the CT group are presented in Figure 2(d).
Attitudes toward treatment
A chi-squared test revealed a significant difference between the groups in the attitude toward the most important factor when considering treatment for depression or anxiety (χ2(15) = 86.85, p < .0001; see Table 1). Responders receiving a conventional treatment were significantly less probable to support ‘natural compound’ as the most important factor compared to all the other groups. Moreover, they were more likely to support ‘scientifically proven as effective’ as the most important factor compared to the HT and NT groups, and more likely to support ‘less adverse effects’ compared to the HT group.
A chi-squared test revealed a significant difference between the groups in the attitude toward purchasing an effective herbal treatment for depression / anxiety without adverse effects (χ2(12) = 30.61, p = .002; see Table 1). The CT group was significantly more likely to respond ‘certainly yes’ compared to the NT group, but not compared to the HT and NPT groups. The NT group was significantly more likely to respond ‘I don’t know’ compared to the CT group.
Further inquiry revealed that in the CT group, 41.7% (n = 150) of the responders replied ‘certainly yes’ and 37.5% (n = 135) replied ‘probably yes’ as to whether they would consider switching the current prescription medication to the abovementioned herbal treatment. The degree of satisfaction with the current prescription medication had no association with the willingness to switch treatment (χ2(16) = 21.8, p = .15, ns). However, a significantly higher rate of adverse effects was found in responders who answered they will certainly be willing to switch treatment (t(358) = 2.99, p = .003; see Figure 3); thus, suggesting that patients suffering from more adverse effects are more likely to consider alternatives.
Figure 3.
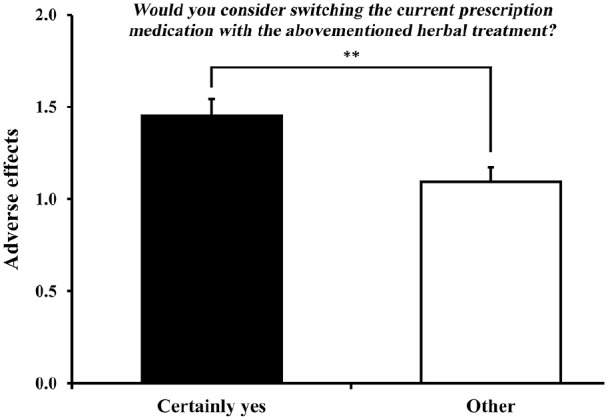
The difference in adverse effects rate between the sub-groups of responders receiving conventional treatment. Responders who answered ‘certainly yes’ as to considering switching to the posited herbal treatment suffered from a significantly higher rate of adverse effects. n = 360. **p < .01.
Implications of socio-demographic factors
The associations between several cardinal background factors and attitudes toward treatment were assessed. These analyses allow us to better understand whether distinct sub-cultures in the Israeli population might maintain different approaches.
Chi-squared tests revealed that females were significantly more likely to receive a prescription medication (χ2(1) = 5.99, p = .014), and tended to seek slightly more professional consultation (χ2(1) = 3.53, p = .06; a trend toward significance) compared to males (64.6% vs. 54.4%, and 89.1% vs. 83.7%, respectively). Gender had no additional associations with the attitudes toward treatment.
Religiosity was found to have significant implications on the treatment’s characteristics. More specifically, the data suggest that although responders from the orthodox-Jewish community were not different in their tendency to seek professional consultation (χ2(3) = 3.18, p = .36, ns), they were slightly less prone to use a prescription medication (χ2(3) = 9.13, p = .028), and significantly more likely to utilize a non-pharmacological treatment such as CBT or psychotherapy (χ2(3) = 11.45, p = .01) compared to the other religious groups (see Table 2). No additional associations were found between religiosity and attitudes toward treatment.
Table 2.
Comparisons between religious groups.
| Item | Secular (n = 366) | Traditional (n = 144) | Religious (n = 52) | Orthodox (n = 29) | p | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| Consultation rate | 325 | 88.8 | 123 | 85.4 | 42 | 80.8 | 25 | 86.2 | ns |
| Prescription medication | 240 | 65.6a | 78 | 54.2 # | 28 | 53.8a | 14 | 48.3 # | .028 |
| Herbal medication | 109 | 29.8 | 39 | 27.1 | 11 | 21.2 | 6 | 20.7 | ns |
| Non-pharmacological treatment | 86 | 23.5a,b | 26 | 18.1a | 6 | 11.5a | 12 | 41.4b | .01 |
Note. Different superscript letters denote a significant difference between the groups at p < .05 following a Bonferroni correction. ns = Not significant. N = 591.
A trend toward significance, p ⩽ .06.
Discussion
In this cross-sectional Israeli survey, a non-negligible group of individuals suffering from depression or anxiety reported they did not receive any conventional treatment (39%), did not consult with a professional (12.9%), or were neutral or not satisfied with their current conventional antidepressants and anxiolytics (50.8%). Furthermore, responders conveyed different attitudes regarding the prominent factor for them in their treatment. Specifically, patients who did not receive conventional treatments were significantly more supportive of natural medications and less concerned with scientific proof.
Similar to our results, studies have indicated that many individuals with psychiatric disorders do not seek or receive evidence-based treatments (Narrow et al., 1993; Wang et al., 2005). Several reports have demonstrated that psychiatric patients and the general public are more likely to favor psychotherapy over antidepressants or other conventional pharmacotherapies (Dahlberg et al., 2008; Ozmen et al., 2005; Van Schaik et al., 2004). In line with our results, it could be conjectured that a sub-group of patients, which deems conventional drugs more negatively, esteems distinctive attributes when considering treatment options. Putatively, proposing an alternative naturally-derived medication or a non-pharmacological treatment will compel this sub-group even more than a scientifically-ratified medication.
The use of herbal medications for depression and anxiety is a widespread phenomenon (Kessler et al., 2001). Astin (1998) reported that the main reason underlying the use of alternative formulas was not dissatisfaction with conventional ones, but rather a strong yoke between one’s personal belief and the allotted treatment. Accumulating findings from randomized controlled trials illustrated the efficacy of several herbal medications in treating depression (Russo et al., 2014; Yeung et al., 2014) and anxiety (Sarris & Kavanagh, 2009; Witte et al., 2005). However, healthcare professionals generally prefer conventional over alternative treatments (Keshet, 2009; Lovell, 2009). Cultivating evidence-based herbal treatments for depression and anxiety disorders might offer a durable solution to patients that usually reject conventional drugs. This calls for a major broadening of the research, to promote effective herbal antidepressants and anxiolytics.
Notwithstanding, the resistance to psychiatric medications is rife with misconceptions (e.g. ‘addictive’, ‘ineffective’, ‘sedation without curing’) (Sartorius et al., 2010). These views are ought to be addressed via psycho-education on the macro-level, in a strive for amending the public discourse. We suggest that a focalized health policy should be generated for conveying knowledge regarding the accurate merits and shortfalls of current antidepressants and anxiolytics. However, such policy will probably not suffice without paying close attention to alternative ideals for treatment and healing.
Accordingly, the current survey suggests that special sensitivity should be placed on cultural aspects when devising a treatment plan. Interestingly, responders suffering from depression or anxiety from the orthodox Jewish community were not different in their tendency to seek professional consultation. However, they were much more likely to utilize psychological interventions rather than pharmacological ones, when compared to other religious groups in Israel. Previous studies have illustrated the complex stance of several orthodox Jewish communities regarding the application of mental healthcare services (Coleman-Brueckheimer & Dein, 2011; Freund & Band-Winterstein, 2017). Despite some positive changes in recent decades (Schnall et al., 2014), an association with mental health services might still lead to stigmatization, and even hinder the prospect of marriage in these communities (Feinberg, 2005). In some instances, pharmacological treatments might be rejected entirely due to a fear that they will excel the stigma and signify a more severe illness (Paradis et al., 1996). In a recent study by Stolovy and colleagues (Stolovy et al., 2013) that investigated perspectives of orthodox Jewish psychiatric patients in Israel, the clinician’s acquaintance and sensitivity for the recipients’ religious views were found to predict better outcomes. Taken together, it is suggested that increased attention should be placed on culturally-related preferences of orthodox Jewish patients, while weighing whether a non-pharmacological strategy would be a more viable one.
The majority of the responders receiving prescription antidepressants or anxiolytics reported the occurrence of at least one adverse effect. Further, 45.2% of the responders declared that a minimal risk for adverse effects is the most important factor for them in their choice of treatment. Patients suffering from a higher incidence of adverse effects were also found to be more drawn to the possibility of switching a conventional treatment with an herbal one. As previously shown, adverse effects have a critical role in adherence to antidepressants and anxiolytics (Lin et al., 1995; MacGillivray et al., 2003). As the rate of nonadherence to such drugs is remarkably high in Israel (Ayalon et al., 2011), it seems that assessing the extent of adverse effects and the suffering attributed to them by the patient is an essential requirement in clinical follow-up sessions. Tackling these questions could facilitate a more accurate and sustainable treatment program.
A major limitation of the current study is related to the method for the identification of individuals suffering from depression or anxiety. The standard for psychiatric diagnosis in research includes the utilization of a clinical interview, a semi-structured diagnostic interview (e.g., The Structured Clinical Interview for DSM-5 – Research Version) (First, Williams, Karg, & Spitzer, 2015) and, in addition, self-report measures that have been previously validated (Goldstein et al., 2011). In this survey, diagnoses relied on self-report measures, using both a declaration of the patient that he suffers from one of the disorders and an acknowledged self-report measure, without a direct assessment by a clinician. One could argue that such a method impedes both the sensitivity and discriminability of the diagnoses. Nevertheless, the point prevalence for depression or anxiety found in the current study (8.9%) is comparable to the 12-month prevalence (9.7%) reported in an earlier Israeli study that utilized a clinical interview (Levinson et al., 2007). This supports the notion that the responders’ report was in most cases genuine and approximately reflects their condition.
Conclusions
The traditional psychiatric paradigm (also referred to as the ‘technological paradigm’), dictates that the main task of a clinician is to assert a reliable diagnosis and present a suitable, evidence-based treatment. From a technological-positivist stance, psychiatric disorders are the observed outcomes of neuro-biophysiological disturbances that should be mapped and therapeutically targeted regardless of any rapport or relations with their ‘carriers’. The psychological distress is pasteurized into a mere technical issue, rather than being fathomed as a human challenge. To its extreme, the role of the patient is reduced to mere compliance (Bracken & Thomas, 2005; Bracken et al., 2012). It seems to us that this agenda might devaluate the cardinal role of the patient’s point of view and its important impact on not just promoting an egalitarian moral, but fostering effective therapeutics. Patients’ attitudes impact treatment outcomes through expectancies (Krell et al., 2004; Kuusisto et al., 2011), placebo effect (Kaptchuk & Miller, 2015; McQueen & Smith, 2012), adherence (Lingam & Scott, 2002; Sjölander et al., 2013), and the therapeutic alliance (Meyer et al., 2002; Verhulst et al., 2013). Complying with the empirical evidence an alternative psychiatric paradigm was advocated, emphasizing concordance rather than compliance (Bracken et al., 2012; Foster & Hudson, 1998).
A prominent approach that assimilated these ideas is the personal recovery approach (Slade, 2009), which accentuates values such as hope, personal responsibility, meaning, and identity. Recipients are encouraged to carve their own journey, while actively weighing their unique preferences and concepts of recovery. Such an approach accentuates that patients have a free choice regarding their treatment. Accordingly, clinicians are expected to be receptive to patients’ preferences and also have broad knowledge regarding feasible formal and informal therapeutic options. For that aim, treating clinicians should be acquainted with various epistemologies and methodologies for healing; and, hence, it could be of great benefit to include basic education in alternative, herbal, culturally-informed and complementary treatment strategies in the curriculum of mental healthcare providers. It seems to us that further implementing such personal recovery strategies in mental health systems could prove highly relevant and effective.
Results from the current survey suggest that patients suffering from depression and anxiety are not unanimous in their perspectives toward treatment and that cultural- and personal-ideals for recovery matter. In acquiescence with the concordance paradigm, it is stipulated that these factors should be taken into consideration during clinical assessments and the choice of treatment. For instance, it seems that subscribing an herbal medication to an individual who will only agree to such a form of treatment or embracing an open dialogue with patients from the orthodox Jewish community, while considering evidence-based psychotherapeutic treatments as first-line options, will prove fruitful.
Research Data
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (http://www.creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
Supplemental material, sj-xlsx-1-isp-10.1177_0020764021992385 for Patients’ attitudes toward conventional and herbal treatments for depression and anxiety: A cross-sectional Israeli survey by Or Burstein, Alon Shamir, Nurit Abramovitz and Ravid Doron in International Journal of Social Psychiatry
Acknowledgments
The authors would like to thank Prof. Avi Degani for his support in data collection.
Footnotes
Declaration of conflicting interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr. Doron has an approved patent relating to herbal treatment for anxiety disorders (Patent No. US 9,329,772). The authors declare that they have no other competing interests.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by Lobasa. Lobasa had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
ORCID iD: Ravid Doron  https://orcid.org/0000-0003-3601-2356
https://orcid.org/0000-0003-3601-2356
References
- Alegría M., Chatterji P., Wells K., Cao Z., Chen C. N., Takeuchi D., Jackson J., Meng X. L. (2008). Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatric Services, 59(11), 1264–1272. 10.1176/ps.2008.59.11.1264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders – Fifth Edition. 10.1176/appi.books.9780890425596 [DOI]
- Astin J. A. (1998). Why patients use alternative medicine. JAMA, 279(19), 1548. 10.1001/jama.279.19.1548 [DOI] [PubMed] [Google Scholar]
- Ayalon L., Gross R., Yaari A., Feldhamer E., Balicer R. D., Goldfracht M. (2011). Disparities in antidepressant adherence in primary care: Report from Israel. The American Journal of Managed Care, 17(9), e340–e347. http://europepmc.org/abstract/MED/21902441 [PubMed] [Google Scholar]
- Baldwin D. S., Waldman S., Allgulander C. (2011). Evidence-based pharmacological treatment of generalized anxiety disorder. The International Journal of Neuropsychopharmacology, 14(5), 697–710. 10.1017/S1461145710001434 [DOI] [PubMed] [Google Scholar]
- Bracken P., Thomas P. (2005). Democracy, citizenship and the radical possibilities of postpsychiatry. In Critical psychiatry. Palgrave Macmillan. [Google Scholar]
- Bracken P., Thomas P., Timimi S., Asen E., Behr G., Beuster C., Bhunnoo S., Browne I., Chhina N., Double D., Evans C., Fernando S., Garland M. R., Hopkins W., Huws R., Johnson B., Martindale B., Middleton H., Moldavsky D., . . . Yeomans D. (2012). Psychiatry beyond the current paradigm. British Journal of Psychiatry, 201, 430–434. 10.1192/bjp.bp.112.109447 [DOI] [PubMed] [Google Scholar]
- Britten N. (1994). Patients’ ideas about medicines: A qualitative study in a general practice population. British Journal of General Practice, 44(387), 465–468. 10.1186/1471-2296-6-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burstein O., Franko M., Gale E., Handelsman A., Barak S., Motsan S., Shamir A., Toledano R., Simhon O., Hirshler Y., Chen G., Doron R. (2017). Escitalopram and NHT normalized stress-induced anhedonia and molecular neuroadaptations in a mouse model of depression. PLoS ONE, 12(11). 10.1371/journal.pone.0188043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callegaro M., Disogra C. (2008). Computing response metrics for online panels. Public Opinion Quarterly, 72(5), 1008–1032. 10.1093/poq/nfn065 [DOI] [Google Scholar]
- Cascade E., Kalali A. H., Kennedy S. H. (2009). Real-world data on SSRI antidepressant side effects. Psychiatry (Edgemont), 6(2), 16–18. 10.3928/00904481-20120727-02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakraborty K., Avasthi A., Kumar S., Grover S. (2009). Attitudes and beliefs of patients of first episode depression towards antidepressants and their adherence to treatment. Social Psychiatry and Psychiatric Epidemiology, 44(6), 482–488. 10.1007/s00127-008-0468-0 [DOI] [PubMed] [Google Scholar]
- Coleman-Brueckheimer K., Dein S. (2011). Health care behaviours and beliefs in Hasidic Jewish populations: A systematic review of the literature. Journal of Religion and Health, 50(2), 422–436. 10.1007/s10943-010-9448-2 [DOI] [PubMed] [Google Scholar]
- Dahlberg K. M., Waern M., Runeson B. (2008). Mental health literacy and attitudes in a Swedish community sample – Investigating the role of personal experience of mental health care. BMC Public Health, 8, 8. 10.1186/1471-2458-8-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doron R., Sever A., Handelsman A., Toledano R., Franko M., Hirshler Y., Shamir A., Burstein O., Rehavi M. (2018). GABAA receptor density is not altered by a novel herbal anxiolytic treatment. Journal of Molecular Neuroscience, 65(1), 110–117. 10.1007/s12031-018-1078-2 [DOI] [PubMed] [Google Scholar]
- Doron R., Versano Z., Burstein O., Franko M., Shamir A., Toledano R., Handelsman A., Rehavi M. (2019). Cerebral MAO activity is not altered by a novel herbal antidepressant treatment. Journal of Molecular Neuroscience, 69, 371–379. 10.1007/s12031-019-01366-0 [DOI] [PubMed] [Google Scholar]
- Feinberg S. S. (2005). Issues in the psychopharmacologic assessment and treatment of the orthodox Jewish patient. CNS Spectrums, 10(12), 954–965. 10.1017/S109285290001052X [DOI] [PubMed] [Google Scholar]
- First M. B., Williams J. B. W., Karg R. S., Spitzer R. L. (2015). Structured clinical interview for DSM-5—Research version (SCID-5 for DSM-5, research version; SCID-5-RV). Arlington, VA: American Psychiatric Association. [Google Scholar]
- Foster P., Hudson S. (1998). From compliance to concordance: A challenge for contraceptive prescribers. Health Care Analysis, 6(2), 123–130. [DOI] [PubMed] [Google Scholar]
- Freund A., Band-Winterstein T. (2017). Cultural psychiatry: A spotlight on the experience of clinical social workers’ encounter with Jewish ultra-orthodox mental health clients. Community Mental Health Journal, 53(5), 613–625. 10.1007/s10597-016-0056-9 [DOI] [PubMed] [Google Scholar]
- Goldstein J. M., Cherkerzian S., Simpson J. C. (2011). Validity: Definitions and applications to psychiatric research. In Tsuang M. T., Tohen M., Jones P. (Eds.), Textbook in psychiatric epidemiology (3rd ed., pp. 99–116). John Wiley & Sons. [Google Scholar]
- Jorm A. F., Korten A. E., Jacomb P. A., Rodgers B., Pollitt P., Christensen H., Henderson S. (1997). Helpfulness of interventions for mental disorders: beliefs of health professionals compared with the general public. The British Journal of Psychiatry, 171(3), 233–237. 10.1192/bjp.171.3.233 [DOI] [PubMed] [Google Scholar]
- Kaptchuk T. J., Miller F. G. (2015). Placebo effects in medicine. New England Journal of Medicine, 373(1), 8–9. 10.1056/NEJMp1504023 [DOI] [PubMed] [Google Scholar]
- Keshet Y. (2009). The untenable boundaries of biomedical knowledge: Epistemologies and rhetoric strategies in the debate over evaluating complementary and alternative medicine. Health, 13(2), 131–155. 10.1177/1363459308099681 [DOI] [PubMed] [Google Scholar]
- Kessler R. C., Soukup J., Davis R. B., Foster D. F., Wilkey S. A, Van Rompay M. I., Eisenberg D. M. (2001). The use of complementary and alternative therapies to treat anxiety and depression in the United States. The American Psychiatric Association, 158(2), 289–294. 10.1176/appi.ajp.158.2.289 [DOI] [PubMed] [Google Scholar]
- Koopmans G. T., Uiters E., Devillé W., Foets M. (2013). The use of outpatient mental health care services of migrants vis-à-vis Dutch natives: Equal access? International Journal of Social Psychiatry. 10.1177/0020764012437129 [DOI] [PubMed]
- Krell H. V., Leuchter A. F., Morgan M., Cook I. A., Abrams M. (2004). Subject expectations of treatment effectiveness and outcome of treatment with an experimental antidepressant. Journal of Clinical Psychiatry, 65(9), 1174–1179. 10.4088/JCP.v65n0904 [DOI] [PubMed] [Google Scholar]
- Kuusisto K., Knuuttila V., Saarnio P. (2011). Pre-treatment expectations in clients: Impact on retention and effectiveness in outpatient substance abuse treatment. Behavioural and Cognitive Psychotherapy, 39(3), 257–271. 10.1017/S1352465810000846 [DOI] [PubMed] [Google Scholar]
- Lam R. W., McIntosh D., Wang J., Enns M. W., Kolivakis T., Michalak E. E., Sareen J., Song W. Y., Kennedy S. H., MacQueen G. M., Milev R. V., Parikh S. V., Ravindran A. V.; CANMAT Depression Work Group. (2016). Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder. The Canadian Journal of Psychiatry, 61(9), 510–523. 10.1177/0706743716659416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamers F., van Oppen P., Comijs H. C., Smit J. H., Spinhoven P., van Balkom A. J. L. M., Nolen V. A., Zitman F. G., Beekman A. T. F., Penninx B. W. J. H. (2011). Comorbidity patterns of anxiety and depressive disorders in a large cohort study: the Netherlands Study of Depression and Anxiety (NESDA). The Journal of Clinical Psychiatry, 72(3), 341–348. 10.4088/JCP.10m06176blu [DOI] [PubMed] [Google Scholar]
- Lenzer J. (2006). Antidepressants double suicidality in children, says FDA. BMJ, 332(7542), 626.16543316 [Google Scholar]
- Lépine J. P., Briley M. (2011). The increasing burden of depression. Neuropsychiatric Disease and Treatment, 7(Suppl 1), 3–7. 10.2147/NDT.S19617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levinson D., Zilber N., Lerner Y., Grinshpoon A., Levav I. (2007). Prevalence of mood and anxiety disorders in the community: Results from the Israel National Health Survey. The Israel Journal of Psychiatry and Related Sciences, 44(2), 94–103. http://europepmc.org/abstract/MED/18080646 [PubMed] [Google Scholar]
- Lin E. H., Von Korff M., Katon W., Bush T., Simon G. E., Walker E., Robinson P. (1995). The role of the primary care physician in patients’ adherence to antidepressant therapy. Medical Care, 33(1), 67–74. 10.1097/00005650-199501000-00006 [DOI] [PubMed] [Google Scholar]
- Lingam R., Scott J. (2002). Treatment non-adherence in affective disorders. Acta Psychiatrica Scandinavica, 105, 164–172. 10.1034/j.1600-0447.2002.1r084.x [DOI] [PubMed] [Google Scholar]
- Lovell B. (2009). The integration of bio-medicine and culturally based alternative medicine: Implications for health care providers and patients. Global Health Promotion, 16(4), 65–68. 10.1177/1757975909348132 [DOI] [PubMed] [Google Scholar]
- MacGillivray S., Arroll B., Hatcher S., Ogston S., Reid I., Sullivan F., Williams B., Crombie. (2003). Efficacy and tolerability of selective serotonin reuptake inhibitors compared with tricyclic antidepressants in depression treated in primary care: Systematic review and meta-analysis. British Medical Association (Clinical Research Ed.), 326(7397), 1014. 10.1136/bmj.326.7397.1014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McQueen D., Smith P. S. J. (2012). Placebo effects: A new paradigm and relevance to psychiatry. International Psychiatry, 9(1), 1–3. [PMC free article] [PubMed] [Google Scholar]
- Meyer B., Pilkonis P. A., Krupnick J. L., Egan M. K., Simmens S. J., Sotsky S. M. (2002). Treatment expectancies, patient alliance, and outcome: Further analyses from the National Institute of Mental Health Treatment of Depression Collaborative Research Program. Journal of Consulting and Clinical Psychology, 70(4), 1051–1055. 10.1037//0022-006X.70.4.1051 [DOI] [PubMed] [Google Scholar]
- Mykletun A., Bjerkeset O., Øverland S., Prince M., Dewey M., Stewart R. (2009). Levels of anxiety and depression as predictors of mortality: The HUNT study. British Journal of Psychiatry, 195(2), 118–125. 10.1192/bjp.bp.108.054866 [DOI] [PubMed] [Google Scholar]
- Narrow W. E., Regier D. a, Rae D. S., Manderscheid R. W., Locke B. Z. (1993). Use of services by persons with mental and addictive disorders. Findings from the National Institute of Mental Health Epidemiologic Catchment Area Program. Archives of General Psychiatry, 50, 95–107. 10.1001/archpsyc.1993.01820140017002 [DOI] [PubMed] [Google Scholar]
- Ozmen E., Ogel K., Aker T., Sagduyu A., Tamar D., Boratav C. (2005). Public opinions and beliefs about the treatment of depression in urban Turkey. Social Psychiatry and Psychiatric Epidemiology, 40(11), 869–876. 10.1007/s00127-005-0985-x [DOI] [PubMed] [Google Scholar]
- Pan Y.-J., Cheng I.-C., Yeh L.-L., Cho Y.-M., Feng J. (2013). Utilization of traditional Chinese medicine in patients treated for depression: A population-based study in Taiwan. Complementary Therapies in Medicine, 21(3), 215–223. 10.1016/j.ctim.2013.03.003 [DOI] [PubMed] [Google Scholar]
- Paradis C. M., Friedman S., Hatch M. L., Ackerman R. (1996). Cognitive behavioral treatment of anxiety disorders in Orthodox Jews. Cognitive and Behavior Practice, 3(2), 271–288. 10.1016/S1077-7229(96)80018-6 [DOI] [Google Scholar]
- Raue P., Schulberg H., Heo M., Klimstra S., Bruce M. (2009). Patients’ depression treatment preferences and initiation, adherence, and outcome: A randomized primary care study. National Institute of Health, 60(3), 337–343. 10.1176/appi.ps.60.3.337.Patients [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rissmiller D. J., Rissmiller J. H. (2006). Open forum: Evolution of the antipsychiatry movement into mental health consumerism. Psychiatric Services, 57(6), 863–866. 10.1176/ps.2006.57.6.863 [DOI] [PubMed] [Google Scholar]
- Roman J. S., Griswold K. S., Smith S. J., Servoss T. J. (2008). How patients view primary care: Differences by minority status after psychiatric emergency. Journal of Cultural Diversity, 15(2), 56–60. [PubMed] [Google Scholar]
- Rush A. J., Trivedi M. H., Wisniewski S. R., Nierenberg A. A., Stewart J. W., Warden D., Niederehe G., Thase M. E., Lavori P. W., Lebowitz B. D., McGrath P. J., Rosenbaum J. F., Sackeim H. A., Kupfer D. J., Luther J., Fava M. (2006). Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: A STAR*D report. American Journal of Psychiatry, 163(11), 1905–1917. 10.1176/appi.ajp.163.11.1905 [DOI] [PubMed] [Google Scholar]
- Russo E., Scicchitano F., Whalley B. J., Mazzitello C., Ciriaco M., Esposito S., Patanè M., Upton R., Pugliese M., Chimirri S., Mammì M., Palleria C., De Sarro G. (2014). Hypericum perforatum: Pharmacokinetic, mechanism of action, tolerability, and clinical drug-drug interactions. Phytotherapy Research, 28, 643–655. 10.1002/ptr.5050 [DOI] [PubMed] [Google Scholar]
- Sarris J., Kavanagh D. J. (2009). Kava and St. John’s Wort: Current evidence for use in mood and anxiety disorders. The Journal of Alternative and Complementary Medicine, 15(8), 827–836. 10.1089/acm.2009.0066 [DOI] [PubMed] [Google Scholar]
- Sartorius N., Gaebel W., Cleveland H. R., Stuart H., Akiyama T., Arboleda-Flórez J., Baumann A. E., Gureje O., Jorge M. R., Kastrup M., Suzuki Y., Tasman A. (2010). WPA guidance on how to combat stigmatization of psychiatry and psychiatrists. World Psychiatry, 9, 131–144. 10.1002/j.2051-5545.2010.tb00296.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawada N., Uchida H., Suzuki T., Watanabe K., Kikuchi T., Handa T., Kashima H. (2009). Persistence and compliance to antidepressant treatment in patients with depression: A chart review. BMC Psychiatry, 9, 38. 10.1186/1471-244X-9-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnall E., Kalkstein S., Gottesman A., Feinberg K., Schaeffer C. B., Feinberg S. S. (2014). Barriers to mental health care: A 25-year follow-up study of the orthodox jewish community. Journal of Multicultural Counseling and Development, 42(3), 161–173. 10.1002/j.2161-1912.2014.00052.x [DOI] [Google Scholar]
- Schraufnagel T. J., Wagner A. W., Miranda J., Roy-Byrne P. P. (2006). Treating minority patients with depression and anxiety: What does the evidence tell us? General Hospital Psychiatry, 28(1), 27–36. 10.1016/j.genhosppsych.2005.07.002 [DOI] [PubMed] [Google Scholar]
- Shigemura J., Ogawa T., Yoshino A., Sato Y., Nomura S. (2010). Predictors of antidepressant adherence: Results of a Japanese Internet-based survey. Psychiatry and Clinical Neurosciences, 64(2), 179–186. 10.1111/j.1440-1819.2009.02058.x [DOI] [PubMed] [Google Scholar]
- Sjölander M., Eriksson M., Glader E. L. (2013). The association between patients’ beliefs about medicines and adherence to drug treatment after stroke: A cross-sectional questionnaire survey. BMJ Open, 3(9), e003551. 10.1136/bmjopen-2013-003551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slade M. (2009). Personal recovery and mental illness: A guide for mental health professionals. In Personal recovery and mental illness: A guide for mental health professionals. Cambridge University Press. 10.1017/CBO9780511581649 [DOI] [Google Scholar]
- Spitzer R. L., Kroenke K., Williams J. B. W., Löwe B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Steel Z., Marnane C., Iranpour C., Chey T., Jackson J. W., Patel V., Silove D. (2014). The global prevalence of common mental disorders: A systematic review and meta-analysis 1980-2013. International Journal of Epidemiology, 43(2), 476–493. 10.1093/ije/dyu038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stolovy T., Levy Y. M., Doron A., Melamed Y. (2013). Culturally sensitive mental health care: A study of contemporary psychiatric treatment for ultra-orthodox Jews in Israel. International Journal of Social Psychiatry. 10.1177/0020764012461206 [DOI] [PubMed]
- Stone M., Laughren T., Jones M. L., Levenson M., Holland P. C., Hughes A., Hammad T. A., Temple R., Rochester G. (2009). Risk of suicidality in clinical trials of antidepressants in adults: Analysis of proprietary data submitted to US Food and Drug Administration. BMJ (Online), 339(7718), 431–434. 10.1136/bmj.b2880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The American Association for Public Opinion Research. (2016). Standard definitions: Final Dispositions of case codes and outcome rates for survey (9th ed.). AAPOR. 10.1038/nsmb.2010 [DOI]
- Van Schaik D. J. F., Klijn A. F. J., Van Hout H. P. J., Van Marwijk H. W. J., Beekman A. T. F., De Haan M., Van Dyck R. (2004). Patients’ preferences in the treatment of depressive disorder in primary care. General Hospital Psychiatry, 26, 184–189. 10.1016/j.genhosppsych.2003.12.001 [DOI] [PubMed] [Google Scholar]
- Verhulst J., Kramer D., Swann A. C., Hale-Richlen B., Beahrs J. (2013). The medical alliance: From placebo response to alliance effect. Journal of Nervous and Mental Disease, 201(7), 546–552. 10.1097/NMD.0b013e31829829e1 [DOI] [PubMed] [Google Scholar]
- Wang P. S., Lane M., Olfson M., Pincus H. A., Wells K. B., Kessler R. C. (2005). Twelve-month use of mental health services in the United States: Results from the National Comorbidity Survey Replication. Archives of General Psychiatry, 62, 629–640. 10.1001/archpsyc.62.6.629 [DOI] [PubMed] [Google Scholar]
- Whiteford H. A., Degenhardt L., Rehm J., Baxter A. J., Ferrari A. J., Erskine H. E., Charlson F. J., Norman R. E., Flaxman A. D., Johns N., Burstein R., Murray C. J. L., Vos T. (2013). Global burden of disease attributable to mental and substance use disorders: Findings from the Global Burden of Disease Study 2010. The Lancet, 382(9904), 1575–1586. 10.1016/S0140-6736(13)61611-6 [DOI] [PubMed] [Google Scholar]
- Wittchen H. U., Carter R. M., Pfister H., Montgomery S. A., Kessler R. C. (2000). Disabilities and quality of life in pure and comorbid generalized anxiety disorder and major depression in a national survey. International Clinical Psychopharmacology, 15, 319–328. 10.1097/00004850-200015060-00002 [DOI] [PubMed] [Google Scholar]
- Witte S., Loew D., Gaus W. (2005). Meta-analysis of the efficacy of the acetonic kava-kava extract WS®1490 in patients with non-psychotic anxiety disorders. Phytotherapy Research, 19, 183–188. 10.1002/ptr.1609 [DOI] [PubMed] [Google Scholar]
- Yeung W.-F., Chung K.-F., Ng K.-Y., Yu Y.-M., Ziea E. T.-C., Ng B. F.-L. (2014). A systematic review on the efficacy, safety and types of Chinese herbal medicine for depression. Journal of Psychiatric Research, 57, 165–175. 10.1016/j.jpsychires.2014.05.016 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (http://www.creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
Supplemental material, sj-xlsx-1-isp-10.1177_0020764021992385 for Patients’ attitudes toward conventional and herbal treatments for depression and anxiety: A cross-sectional Israeli survey by Or Burstein, Alon Shamir, Nurit Abramovitz and Ravid Doron in International Journal of Social Psychiatry