Abstract
Based on data from the CORONA-MONITORING lokal (CoMoLo) study conducted in four municipalities particularly affected by the COVID-19 pandemic, this article investigates the non-utilisation of health care services in the population aged 18 years and older (n=9,002) in relation to the period after the introduction of the containment measures in March 2020. The results show that about one third of the respondents (35.5%) gave up at least one of the surveyed health care services. The most frequent cancellations were dental (15.2%) and specialist check-ups (11.8%), followed by postponement of physiotherapy, ergotherapy or speech therapy (6.1%), cancellation of general practitioner (GP) check-ups (5.8%), postponement of psychotherapy (2.0%), postponement of planned hospital treatment (1.8%) and not going to an emergency room (0.7%). Almost 10% of the respondents reported not visiting a physician despite health complaints. Compared to respondents without such a waiver, these respondents were more often female and younger than 35 years, less often rated their health as very good or good, more often had a diagnosis of depression and more often used telemedical contacts as an alternative to visiting the practice during the pandemic. Further analyses of trends in utilisation behaviour and changes in health status over the course of the COVID-19 pandemic are important.
Keywords: UTILISATION, CARE, PHYSICIAN VISIT, TREATMENT, COMPLAINTS, TELEMEDICINE, COVID-19, SARS-COV-2
1. Introduction
Since the emergence of the first series of SARS-CoV-2 cases in China at the end of 2019 [1], the novel corona virus, that can lead to COVID-19 disease with sometimes severe courses [2], has been spreading worldwide. In the last week of January 2020, there was the first laboratory-confirmed COVID-19 case in Germany. The high infection dynamics led to every federal state reporting COVID-19 cases as early as the second week of March 2020 [3, 4]. As a result, comprehensive non-pharmaceutical measures to contain SARS-CoV-2 infection were introduced at the federal and state levels before the end of March 2020. These included population-based measures such as general contact restrictions (e.g. by banning events, closing educational institutions and allowing telephone sick notes) and individual infection hygiene measures such as maintaining a minimum distance and wearing mouth-to-nose coverings [3, 4]. Other measures included strengthening intensive care and ventilation capacity in hospitals for COVID-19 patients by postponing scheduled procedures, which was necessary in some cases [5]. The extent and time limit of these measures depended on the development of the pandemic situation. Thus, from the end of April 2020, the measures were gradually relaxed, and in November 2020 they were strengthened again [4].
So far, initial evaluations of the effects of the COVID-19 pandemic and the introduced containment measures on the health care situation of the population are available for the year 2020 [6, 7]. For example, accounting data from the Associations of Statutory Health Insurance (SHI) Physicians show that the number of medical and psychotherapeutic outpatient services in 2020 fell significantly across almost all specialities from March onwards compared to the corresponding period of the previous year, only returning to normal in May and in some cases falling again in the third and fourth quarters [8]. For inpatient services, based on AOK acounting data, a decline is also described for 2020 in comparison to the previous year, which was more pronounced in terms of numbers in the period from March to May than in the period from October to December and mainly, but not exclusively, applied to postponable treatment events [9, 10]. A decline in the number of emergency department visits was also observed with the start of containment measures in 2020 based on a multi-centre data collection in emergency departments [11]. The reasons for the decline in treatment cases are not exclusively attributed to shifts or changes in the supply of care due to COVID-19 cases requiring priority treatment, but at least partly also to fears of infection with SARS-CoV-2 [6].
The analyses from the point of view of the service providers only allow limited conclusions to be drawn about the need in the population. For example, results from the nationwide, population-based survey German Health Update (GEDA) of the Robert Koch Institute (RKI) also indicate a decline in self-reported utilisation of general and specialist outpatient services during the first phase of the containment measures compared to the previous year [12]. However, an evaluation of the GEDA data focussed on persons with diabetes shows at least no relevant change in general practitioner (GP) utilisation for this group of respondents with regularly required GP visits [13]. Similarly, results from the COVID-19 Snapshot Monitoring (COSMO) online survey indicate that a substantial proportion of participants postponed potentially deferrable preventive care appointments due to the COVID-19 pandemic, but the majority considered a supply of necessary physician visits and medications to be assured during the phases of containment activities in 2020 [14–16].
This analysis uses population-based data from the CORONA-MONITORING lokal (CoMoLo) study conducted by the RKI in the second to fourth quarter of 2020 to explore the following questions: 1) What proportion of respondents was affected by suspended health services in the different health care settings with regard to the period of strict containment measures since March 2020, and 2) How do people who refrained from health care services despite health complaints differ from those who did not?
2. Methodology
2.1 CORONA-MONITORING lokal (CoMoLo) study
CoMoLo is a population-based seroepidemiological study that was conducted in four municipalities in Germany that were particularly affected by the COVID-19 pandemic as cross-sectional surveys in independent samples [17]. Criteria for selecting the study sites were a cumulative SARS-CoV-2 reporting incidence of more than 500 cases per 100,000 persons of the population before the start of the study and a willingness to cooperate on site. The aim was to determine the seroprevalence (i.e. the proportion of the population with previous SARS-CoV-2 infection overall), to differentiate the proportion of undetected or asymptomatic SARS-CoV-2 infections, and to determine the risk factors for infection. A further concern was to record changes in health behaviour, health status and the use of health care services in the context of the pandemic and the containment measures introduced [18].
The cross-sectional surveys were based on randomly drawn population registration office samples in Kupferzell (Baden-Württemberg), Bad Feilnbach (Bavaria), Straubing (Bavaria) and Berlin-Mitte [17]. Adults aged 18 years and older who were registered with their main residence in the respective municipality during the survey period were included. An oropharyngeal swab, a blood sample and an interview based on a short written questionnaire were performed at a temporary study centre with examination buses or during a home visit. Participants were asked for permission to re-contact for a detailed follow-up interview. Approximately one to two weeks after participation in the study, an in-depth follow-up interview was conducted, either webbased or by telephone [18, 19].
More information on reporting incidence, sampling and study methodology as well as results on seroprevalence and magnitude of undetected or asymptomatic cases per study site are given elsewhere [20–25]. Table 1 summarises the timing, local infrastructure and local outbreak events as well as participant numbers, response rates and sociodemographic characteristics for each study site.
Table 1.
Overview of characteristics of CoMoLo study locations and participants
Source: Own table
| Kupferzell | Bad Feilnbach | Straubing | Berlin-Mitte | |
|---|---|---|---|---|
| Chronological order | ||||
| Study period [20–25] | 20.05.–09.06.2020 | 23.06.–04.07.2020 | 08.09.–26.09.2020 | 17.11.–05.12.2020 |
| National COVID-19 pandemic phase [4, 26] | Start of summer plateau 2020 | Summer plateau 2020 | End of summer plateau 2020 | Second COVID-19 wave |
| Characteristics of the study sites | ||||
| Local spatial structure [25] | Rural | Rural | More urban | Urban |
| Local infection history before the start of the study [25] | Main infection event: Mid-March to the end of March | Main infection event: Mid-March to mid-April | Main infection event: Beginning of March to the end of May | Diffuse infection event |
| Trigger: Local events (mainly church concerts, festivals), travellers returning from ski areas in Austria and Italy | Trigger: Local events (mainly events in the context of local elections, festivals), outbreak in nursing home facility | Trigger: Local events (mainly end of February/beginning of March), outbreaks in nursing home facilities and in the meat processing industry | Trigger: Diverse | |
| Characteristics of the participants | ||||
| Number of participants [20–25] | 2,203 | 2,152 | 2,361 | 2,286 |
| Response rate [20–25] | 63% | 59% | 30% | 29% |
| Age range [24] | 18–94 years | 18–98 years | 18–96 years | 18–92 years |
| Mean age | 49 years | 51 years | 50 years | 45 years |
| Proportion of women [25] | 48.5% | 50.8% | 49.9% | 47.4% |
| Education level (ISCED) | ||||
| Low education group | 20.6% | 18.6% | 23.8% | 15.7% |
| Medium education group | 49.8% | 49.3% | 52.6% | 34.8% |
| High education group | 29.6% | 32.0% | 23.6% | 49.5% |
ISCED = International Standard Classification of Education [27]
2.2 Data collection
Health care services
The non-utilisation of health care services, which is the focus of this article, was assessed through the web-based or telephone CoMoLo follow-up interview via the following question: ‘18 March 2020 is a key date that we refer to frequently in this questionnaire. On that day was the Chancellor’s speech in which she recommended the nationwide measures for contact restriction. Now please think about the time after 18 March 2020. Which of the following events have occurred to you? Multiple answers possible’. For the survey of participants in Berlin-Mitte, which had the greatest time gap from the reference date, the following adjustment was made to the above wording: ‘Now please think about the time of strict measures for contact restriction after 18 March 2020’.
The individual events asked about non-utilisation, which could be ticked in each case if they applied, are listed in Figure 1 analogously to their wording and order in the interview. On the one hand, the survey asked about the cancellation of appointments in the various areas of outpatient medical care (GP, specialist, dental care), whereby an explicit distinction was made as to whether appointments were cancelled by the respondent or by the practice. On the other hand, the renunciation of emergency medical care via an ambulance or emergency room as well as the suspension or postponement of a planned hospital treatment, a psychotherapeutic treatment or a therapeutic treatment (ergotherapy, physiotherapy, speech therapy) was queried. In addition, it was asked whether a visit to the physician had been dispensed with despite existing health complaints.
Figure 1.
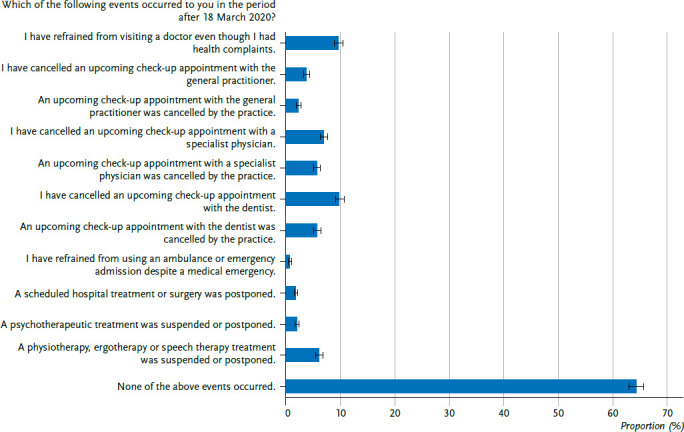
Non-utilisation of health care services (proportions in % with 95% confidence interval, N=7,963)
Source: CoMoLo study
Subsequently, the participants from all four study locations were asked the same question: ‘Have you used telephone or telemedical contact options instead of visiting a medical or psychotherapeutic practice? Multiple answers possible’. The response options were: ‘Yes, by telephone (e.g. telephone consultations)’, ‘Yes, by telemedicine (e.g. video consultations, e-mail contact)’, ‘No’ and ‘No need for examination or treatment’.
Disease-specific and sociodemographic factors
The analysis includes information on two of the three central indicators of health status (as components of the internationally established Minimal European Health Module, MEHM [28]): the self-assessment of the general state of health (subjective health) and the presence of chronic diseases or long-term health problems. Subjective health was assessed in the short questionnaire with the following question: ‘How is your health in general?’. The five response options were: ‘Very good’, ‘Good’, ‘Fair’, ‘Bad’ or ‘Very bad’. The presence of chronic diseases or long-term health problems was recorded in the follow-up questionnaire via the following question: ‘Do you have any chronic disease or a long-term health problem? This means diseases or health problems that have lasted or are expected to last for at least 6 months’. The response options included ‘Yes’ and ‘No’.
Furthermore, the participants were asked for detailed information about their medical history based on the following question: ‘Have you ever been diagnosed by a physician with any of the following diseases?’ In a subsequent list, specific questions were asked about individual diseases, with ‘Yes’, ‘No’ or ‘Don’t know’ as possible answers. In this article, information was included from the follow-up questionnaire on ‘heart attack’, ‘circulatory disorders of the heart, narrowing of the coronary arteries, angina pectoris (coronary heart disease)’, ‘heart weakness/heart failure’, ‘atrial fibrillation’, ‘stroke’, ‘high blood pressure/hypertension’, ‘diabetes’, ‘dyslipidemia (elevated fat levels: cholesterol or triglycerides)’, ‘bronchial asthma’, ‘chronic bronchitis, chronic obstructive pulmonary disease (COPD), emphysema (chronic overinflation of the lungs)’, ‘chronic liver disease (liver cirrhosis, liver shrinkage, chronic liver inflammation/hepatitis)’, ‘chronic kidney disease (reduced kidney function, renal insufficiency)’, ‘cancer’, ‘depression’, ‘autoimmune disease (e.g. rheumatoid arthritis, lupus erythematosus, Crohn’s disease, ulcerative colitis, celiac disease, sarcoidosis, multiple sclerosis)’ as well as from the short questionnaire on ‘immunodeficiency (e.g. due to a disease, organ transplant, chemotherapy or taking other drugs such as cortisone)’. The information on the individual physical diseases was used together to define a dichotomous yes/no variable ‘pre-existing physician-diagnosed chronic physical disease’ and the information on depression was used separately to define the dichotomous yes/no variable ‘pre-existing physician-diagnosed depression’.
Using the 2011 version of the International Standard Classification of Education (ISCED [27]), which includes information on school and vocational qualifications from the participants’ short and follow-up questionnaires, the education level was divided into a low (ISCED 1–2), medium (ISCED 3–4) and high (ISCED 6–8) education group.
2.3 Study population
The study is based on pooled cross-sectional data from the four study locations (N=9,002). Participants who did not complete a follow-up questionnaire (N=985) and who did not answer the question on non-utilisation of health care services (N=54) were excluded, so that the analysis includes a total of 7,963 participants (N=4,257 women, N=3,706 men). In the further analysis, participants were also excluded who did not answer the question on telemedical contact as an alternative to a visit to a physician’s or psychotherapist’s practice (N=7) or for whom non-plausible information was available (N=83), so that this included a total of 7,873 participants (N=4,205 women, N=3,668 men).
2.4 Statistical analyses
In descriptive analyses, the proportions of suspended health care services were determined with 95% confidence intervals (CI). An additional analysis includes stratification by study location and sex.
For a more detailed characterisation of the particular group of respondents who affirmed that they had refrained from visiting a physician despite health complaints, this group was compared with two other groups with regard to sociodemographic and disease-specific factors: 1) with respondents who, in response to the question ‘Have you used telephone or telemedical contact options instead of visiting a medical or psychotherapeutic practice?’, stated that they had no need for an examination or treatment (hereafter referred to as persons without a need for an examination or treatment) and 2) with respondents who did not affirm that they had not visited a physician despite health complaints and did not state that they had no need for an examination or treatment (hereafter referred to as persons who did not refrain from visiting a physician for health complaints). An additional analysis includes logistic regression models with adjustment (control) for place of study, sex, age and education.
All results were calculated taking into account a weighting factor, whereby the respective sample was adjusted to the population structure of the respective municipality with regard to age, sex and educational distribution (at the district level according to the micro-census). In order to take the weighting appropriately into account when calculating confidence intervals and p-values, all analyses were calculated using the survey procedures of SAS 9.4. A statistically significant difference between groups is assumed if the corresponding p-value in the Rao-Scott-Chi-Square test is smaller than 0.05.
3. Results
3.1 Frequencies of non-utilisation of health care services
Overall, about one-third (35.5%) of respondents reported that they gave up at least one of the surveyed health care services after 18 March 2020 (Figure 1). Among the specialist care services, the most frequent cancellations were of upcoming dental check-up appointments (15.2% in total, 9.8% by the respondents, 5.7% by the practice) and specialist check-up appointments (11.8% in total, 6.9% by the respondents, 5.7% by the practice), followed by the suspension or postponement of physiotherapy, ergotherapy or speech therapy treatment (6.1%) and the cancellation of an upcoming GP checkup appointment (5.8% in total, 3.8% by the respondents, 2.3% by the practice). In comparison, the suspension or postponement of psychotherapeutic treatment (2.0%), the postponement of a planned hospital treatment or operation (1.8%) as well as the renunciation of using an ambulance or emergency room despite a medical emergency (0.7%) were indicated less frequently. The generally formulated question, i.e. not specified according to speciality, about not visiting a physician despite existing health complaints was answered in the affirmative by a total of 9.7%.
This pattern is evident for every study location, even if the respective proportions of non-utilised care services differ slightly between the locations. Moreover, this pattern exists for both sexes, whereby the respective proportions of non-utilisation of almost all health care services are higher for women than for men.
3.2 Characteristics of people without a physician visit despite the presence of health complaints
In order to characterise the respondents who refrained from visiting a physician despite health complaints, comparisons were made with respondents without a need for an examination or treatment and with respondents who did not refrain from visiting a physician in the case of complaints.
Respondents who had no need for examination or treatment were, as expected, more likely than the other two groups to rate their health as good or very good, less likely to report having had a chronic disease or long-term health problem for at least six months, less likely to report preexisting physician-diagnosed chronic physical diseases and less likely to report pre-existing physician-diagnosed depression. They were also less often low educated and more often male (Table 2). These differences were also observed after adjusting for place of study, age, sex and education in additionally conducted regression models.
Table 2.
Characteristics of the study population overall and subdivided into groups of people according to their indications of refraining from a physician visit despite health complaints and of a need for examination or treatment (N=7,873)
Source: CoMoLo study
| Subdivided into groups of persons | ||||
|---|---|---|---|---|
| Characteristics | Total (N=7,873) |
Persons who refrain from visiting a physician in the event of health complaints (N=708) |
Persons who do not refrain from visiting a physician in the event of health complaints (N=3,480) |
Persons without need for examination or treatment (N=3,685) |
| Sociodemographic factors (proportion in % or mean value, each with 95% CI) | ||||
| Place of study | ||||
| Kupferzell | 24.6 (23.4–25.9) | 24.1 (20.6–28.0) | 25.2 (23.5–27.0) | 24.1 (22.4–25.9) |
| Bad Feilnbach | 24.2 (23.0–25.4) | 21.2 (17.9–25.0) | 23.2 (21.6–24.9) | 25.7 (24.0–27.4) |
| Straubing | 26.2 (25.0–27.5) | 23.9 (20.2–28.0) | 27.1 (25.2–29.0) | 25.9 (24.1–27.7) |
| Berlin–Mitte | 25.0 (23.7–26.3) | 30.8 (26.7–35.2) | 24.5 (22.7–26.5) | 24.3 (22.5–26.3) |
| Female sex | 49.1 (47.9–50.4) | 58.5 (54.1–62.8) | 51.5 (49.5–53.5) | 45.0 (43.2–46.9) |
| Age | ||||
| 18–34 years | 27.7 (26.5–29.0) | 30.4 (26.4–34.7) | 22.8 (21.0–24.6) | 32.2 (30.3–34.1) |
| 35–49 years | 24.7 (23.5–26.0) | 26.0 (22.3–30.1) | 24.7 (22.9–26.6) | 24.5 (22.9–26.3) |
| 50–64 years | 26.5 (25.3–27.6) | 24.0 (20.5–27.9) | 28.9 (27.1–30.7) | 24.5 (22.9–26.2) |
| 65–74 years | 10.7 (10.0–11.4) | 8.7 (6.8–11.1) | 11.9 (10.8–13.1) | 9.8 (8.9–10.9) |
| ≥75 years | 10.4 (9.6–11.3) | 10.9 (8.3–14.2) | 11.7 (10.5–13.1) | 9.0 (7.9–10.2) |
| Mean value (in years) | 48.7 (48.2–49.2) | 47.6 (45.9–49.4) | 50.7 (49.9–51.5) | 46.9 (46.1–47.6) |
| Education level (ISCED)1 | ||||
| Low education group | 12.8 (11.7–13.9) | 16.4 (12.5–21.4) | 15.3 (13.7–17.1) | 9.5 (8.1–11.2) |
| Medium education group | 50.0 (48.6–51.3) | 45.8 (41.5–50.2) | 50.6 (48.6–52.6) | 50.1 (48.1–52.1) |
| High education group | 37.3 (36.0–38.5) | 37.7 (33.9–41.8) | 34.1 (32.3–35.9) | 40.4 (38.5–42.3) |
| Disease-specific factors (proportions in % with 95% CI) | ||||
| Very good/good subjective health2 | 87.8 (86.9–88.7) | 73.6 (69.3–77.5) | 84.5 (83.0–85.9) | 93.7 (92.7–94.6) |
| Chronic disease/long-term health problem for at least six months3 | 34.3 (33.0–35.6) | 47.2 (42.7–51.6) | 41.6 (39.7–43.6) | 24.6 (22.9–26.4) |
| Chronic physician-diagnosed physical disease4 | 45.6 (44.2–46.9) | 54.0 (49.5–58.5) | 51.9 (49.8–54.0) | 37.7 (35.7–39.7) |
| Physician-diagnosed depression5 | 11.2 (10.3–12.1) | 24.1 (20.0–28.7) | 13.3 (11.9–14.8) | 6.8 (5.7–8.0) |
| Telephone/telemedical contact (proportions in % with 95% CI) | ||||
| Telephone | 8.5 (7.8–9.3) | 25.1 (21.6–28.9) | 14.0 (12.7–15.5) | - |
| Telemedical | 2.0 (1.6–2.4) | 6.2 (3.9–9.5) | 3.2 (2.6–4.0) | - |
CI = Confidence interval, ISCED = International Standard Classification of Education [27]
In the individual strata, participants with missing values are excluded: 1N = 9, 2N = 185, 3N = 2, 4N = 523, 5N = 205
Compared to those who did not refrain from visiting a physician for health complaints, respondents who refrained from visiting a physician for complaints were less likely to rate their health as good or very good, more likely to report a chronic disease or health problem for at least six months and more likely to report pre-existing depression diagnosed by a physician. They were also more often female, under 35 years old, and living in Berlin. Furthermore, respondents who refrained from seeing a physician in the event of health complaints reported more frequently the alternative use of a telephone or telemedical contact option (25.1% by telephone, 6.2% by telemedicine, or 29.1% overall (by telephone or telemedicine)) than those who did not refrain from seeing a physician when they had complaints (14.0% by telephone, 3.2% by telemedicine, or 16.5% overall (by telephone or telemedicine)) (Table 2). In the regression models adjusted for place of study, age, sex and education, the differences between the two groups remained except for place of study.
4. Discussion
The present results based on the population-based CoMoLo study show that almost two-thirds of the participating adults from four municipalities in Germany particularly affected by the COVID-19 pandemic did not forego any of the surveyed health care services after the introduction of the containment measures in March 2020. Among the one-third of respondents who forwent at least one of the health care services surveyed, the most frequently reported cancellations of dental and specialist check-up appointments were more than 10% each and almost 10% reported forgoing a visit to the physician despite health complaints. The respondents who refrained from visiting a physician despite health complaints were more often under 35 years of age and female compared to those who did not, and were less likely to rate their health as very good or good, more likely to have a pre-existing diagnosis of depression, and more likely to use a telephone or telemedical contact option.
4.1 Classification of the results in comparison to other studies
Studies based on population-based survey data
To date, only a few population-based studies have investigated the utilisation of health care services in the context of the COVID-19 pandemic, and each of these studies has focused on different questions and time periods [6, 7].
Results from the online COSMO study, conducted on the basis of repeated and independent cross-sectional samples, indicate that the majority of respondents considered their supply of necessary physician’s visits and medication to be guaranteed during the first pandemic phase. The proportion of people who considered necessary visits at a physician as possible was slightly lower at the beginning of April 2020 in the time frame of strict containment measures (87%) than at the end of July 2020 in the time frame of relaxed measures (94%) [14]. Further results of the COSMO study indicate that the majority of respondents at the end of April 2020 ‘rather not’ to ‘not at all’ agreed to have experienced problems with regard to their medical care in the last four weeks (60%) or to have experienced deteriorations in health due to limitations in medical care (73%) [15]. In contrast, the proportion of respondents who reported in July 2020 that they had postponed cancer screening [29], health check-up [30] or dental appointments [31] due to the COVID-19 pandemic was over 40% each among those with a pending appointment [14], with the majority of postponed dental appointments being checkups [31]. The present study accordingly shows that the majority of respondents reported no cancellations of physician or treatment appointments since the beginning of the pandemic (64%) and that the most frequent cancellations relate to check-up appointments.
A further analysis of the COSMO data shows that the majority of respondents considered their supply of necessary physician’s appointments to be guaranteed also in relation to different care services, whereby the information from the beginning of December 2020 already refers to the second phase of the containment measures. For example, of the 51.7% of respondents with necessary GP or specialist check-up appointments, a total of 3.5% stated that necessary physician’s appointments are currently not possible; of the 9.9% with necessary psychotherapeutic treatment, the figure was 2.0%. It should be noted that the relative proportion of respondents without access to an appointment in relation to those with a required appointment varied for the different care services. The relative proportion was lowest for GP or specialist check-ups and for dental check-ups, each at 6.3%, and highest for psychotherapeutic treatments at 16.5% [16]. Interestingly, in the present study, a pre-existing physician-diagnosis of depression was shown to be an associated factor with the group of people who refrained from visiting a physician despite having health complaints. Overall, this may indicate that people with current or previous mental health problems were most likely to have been affected by not being served by needed health services in the context of the containment measures.
Results from the nationwide GEDA 2019/2020-EHIS study on self-reported utilisation of outpatient GP and specialist services in the last four weeks before the interview indicate a temporary decline during the period of the first phase of containment measures. The proportion of people using a GP in the period from the beginning of April to the end of June 2020 was 30% compared to 38% in the same period of the previous year; the corresponding proportion of people using a specialist was 18% compared to 30% [12]. Another GEDA 2019/2020-EHIS analysis, which included only people with diabetes, also showed a decline in specialist utilisation (24% vs. 43%) but no relevant change in GP utilisation (62% vs. 60%). Possible explanations discussed for this observation were the need for regular GP visits by people with diabetes to care for their condition and adaptations in care provision through telephone consultations [13]. A parallel to the present study can be seen in the fact that the proportion of people who cancelled a specialist check-up appointment (12%) is higher than the proportion of people who cancelled a GP check-up appointment (6%). In addition, the present study also indicates a role for the alternative telemedical contact option among persons who refrained from visiting a physician despite health complaints.
Studies based on accounting data
The association of the containment measures with the non-utilisation of health care services can also be seen on the basis of accounting and service data.
An evaluation of the use of outpatient service offered by SHI-accredited physicians and psychotherapists for the months of 2020 in comparison to the corresponding months of the previous year shows a dependence of the observed changes on the measures for contact restriction. Thus, treatment cases declined across all service areas from the beginning of March 2020 (April: -22.7%, May: -15.5%). At the end of May 2020, the number of treatment cases normalised and in June 2020 increases were observed (June: +2.6%), which varied depending on the service area. For most service areas, repeated decreases or approximations of treatment cases to those of the previous year were observed in the third quarter of 2020 (July: -1.3%, August: -0.2%, September: +0.7%) and in the fourth quarter of 2020, after initial increases, declines were again recorded (October: +6.3%, November: -4.5%, December: -3.0%). The outpatient service data show that the declines are particularly pronounced for services that can potentially be postponed, such as screening examinations and training within the framework of the disease management programmes, but are not limited to these. From mid-March onwards, for example, significant decreases in the number of cases were also observed for outpatient emergency and on-call services [8]. A decrease in the number of emergency department visits compared to the previous year – for both outpatient and inpatient stays – is also evident after the introduction of contact restriction measures based on data from 36 university and non-university emergency departments in Germany. Potential reasons discussed were a less frequent occurrence of injuries and accidents as well as infectious diseases, but also a higher inhibition threshold for utilisation (e.g. due to concern about infection with SARS-CoV-2) and a less frequent availability of relatives (who often initiate emergency care, e.g. especially for the elderly) [11]. Here, too, the parallel to the present study can be seen in the fact that decline in utilisation largely, but not exclusively, concerned potentially postponable services. According to the CoMoLo results, 9.7% of the respondents stated that they had not visited a physician despite health complaints and 0.7% that they had not used emergency medical services.
The decrease in treatment cases with direct contact to a physician is offset by a considerable increase in case numbers with telephone counselling (March to December 2020 compared to the corresponding period of the previous year: 6.3 million vs. 3.6 million) and with video consultation (2.5 million vs. around 3,000). This is interpreted as an adjustment of medical and psychotherapeutic services to the necessary care of patients [8]. In line with this, the present study shows that a part of the respondents with examination or treatment needs used telemedical contact options as an alternative and that, as expected, the corresponding proportion among persons who refrained from visiting a physician despite existing health complaints was higher than among persons who did not refrain from visiting a physician in case of complaints (29% vs. 17%).
For inpatient services, according to an evaluation of all hospital stays of AOK-insured persons, there were also decreases, which, compared to the corresponding period of the previous year, were strongest from March to May 2020 (March: -20.9%, April: -35.2%, May: -24.0%), less pronounced in the summer months (June: -6.5%, July: -10.1%, August: -7,8%, September: -6.9%) and stronger again from October to December 2020 (October: -11.4%, November: -16.9%, December: -20.2%) and – similar to the observations based on the population-based data and outpatient accounting data – applied predominantly, but not exclusively, to postponable treatment occasions. In addition to the factors already mentioned in the above paragraph, cited possible influencing factors were regulatory requirements and political recommendations for keeping intensive care capacities available and for postponing hospital stays that can be planned as well as a change in referral behaviour due to reduced consultation times in outpatient practices [9, 10]. In the present study, the postponement of a planned hospital treatment or operation also played a role in a proportion of 1.8% of the respondents.
4.2 Strengths and limitations
Overall, the data collected in the CoMoLo study allow a more differentiated view of the utilisation of health care services from a population perspective than was possible in previous population-based studies. With regard to the observations of cancelling in particular – but not exclusively – potentially deferrable services and the relevance of alternative telemedical contact options, results of the present study are in line with results of other studies. In addition, the CoMoLo study integrates further questions, such as on not visiting a physician despite health complaints as well as on sociodemographic and disease-specific factors, which enabled further analyses by linking them.
Nevertheless, when interpreting the results, it should be noted that there were differences between the study sites in terms of infrastructural and sociodemographic characteristics as well as in terms of local outbreak occurrence, which may have resulted in different implemented local containment measures. In addition, the data collection took place at different times in the study locations, so that the time interval to the reference date of 18 March 2020 varies. For the survey in the study location Berlin-Mitte, which had the largest time gap to the reference date, it was therefore additionally specified to think of ‘the time of strict measures for contact restriction’ when answering. The results from additional analyses adjusted or stratified for study location also indicate agreement with the main findings of the analysis with the pooled data from the four study locations. However, the utilisation behaviour in other municipalities, for example in those with less pronounced infection incidence, could have been different, so that the results cannot be directly generalised to the overall adult population of Germany.
Furthermore, the questions integrated in CoMoLo also only allow limited insights into the care needs of the population. For example, in the case of respondents who did not waive health care services, it was not possible to differentiate which proportion used such services or did not plan to use them or did not need them. Further, it was not possible to ask respondents who had cancelled at least one of the requested health care services which specific services they had cancelled (e.g. cancer screening, health check-ups, prenatal care) and why (e.g. fear of contracting SARS-CoV-2, overload in the family). Another limitation for classifying the results is that ‘complaints’ in the question about refraining from visiting a physician despite health complaints, which almost 10% of the respondents affirmed, cannot be characterised in more detail in terms of their type or severity. This is due to the circumstance that the health complaints cannot be clearly assigned to another answer due to the possibility of multiple entries and that no additional free text entries were possible.
4.3 Conclusion
In summary, 64% of adults did not forego physician and treatment appointments even under strict contact restrictions in place. However, this was not the case for 36%. Every tenth person even refrained from visiting a physician, although health complaints were present. Compared to persons without such a waiver, these persons were, among other determinants, less often characterised by a good or very good state of health and more often by depression in the past, but more often used telemedical contact options as an alternative to visiting a medical or psychotherapeutic practice.
Longitudinal analyses of possible health effects due to a changed health care situation are still largely lacking for Germany. The experiences of the present and previous studies show how important it is to also analyse changes in care provision and utilisation behaviour caused by external conditions from the perspective of those affected. Only in this way, in combination with results from routine data, conclusions can be drawn as to how care must be designed with regard to crisis situations in order to protect vulnerable groups from care bottlenecks.
Key statements
About one third of all respondents refrained from at least one of the health care services surveyed after containment measures began in March 2020.
Cancellations of dental and specialist check-up appointments were most frequently reported.
Almost one tenth of the respondents stated that they had refrained from seeing a physician after the start of the containment measures despite health complaints.
Those who refrained from visiting a physician despite health complaints were more often younger than 35 years and female, reported less often very good or good health and more often a physician-diagnosed depression than those without such a refrain.
Those who refrained from seeing a physician despite health complaints were more likely to use a telephone or telemedical contact option than those without such a refrain.
Funding Statement
The CORONA-MONITORING lokal study was funded by the German Federal Ministry of Health.
Footnotes
The German version of the article is available at: www.rki.de/journalhealthmonitoring
Data protection and ethics
All of the Robert Koch Institute’s studies are subject to strict compliance with the data protection provisions set out in the EU General Data Protection Regulation (GDPR) and the Federal Data Protection Act (BDSG). The ethics committee of the Berlin Chamber of Physicians assessed the ethics of the CORONA-MONITORING lokal study and provided its approval (Eth-11/20). Participation in the study was voluntary. The participants were informed about the aims and contents of the study and about data protection. Informed consent was obtained in writing.
Conflicts of interest
The authors declared no conflicts of interest.
Acknowledgement
We would like to thank all of our colleagues at the departments 2 and 3 and the Centre for Biological Threats and Special Pathogens (ZBS) at the Robert Koch Institute for their support. We are especially grateful to the colleagues of the survey administration and of the epidemiological central laboratory and the field teams. We also warmly thank all participants for their support of the CORONA MONITORING lokal study. We also thank the local authorities and other local individuals for their support.
Disclaimer
Note: External contributions do not necessarily reflect the opinions of the Robert Koch Institute
References
- 1.Huang C, Wang Y, Li X, et al. (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395(10223):497-506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Potere N, Valeriani E, Candeloro M, et al. (2020) Acute complications and mortality in hospitalized patients with coronavirus disease 2019: a systematic review and meta-analysis. Crit Care 24(1):389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grote U, Arvand M, Brinkwirth S, et al. (2021) Maßnahmen zur Bewältigung der COVID-19-Pandemie in Deutschland: nichtpharmakologische und pharmakologische Ansätze. Bundesgesundheitsbl 64(4):435-445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wieler LH, Rexroth U, Gottschalk R. (2021) Emerging COVID-19 success story: Germany’s push to maintain progress. OurWoldInDataorg. https://ourworldindata.org/covid-exemplar-germany?country= (As at 14.01.2022)
- 5.Osterloh F. (2020) Krankenhäuser verschieben planbare Eingriffe. Dtsch Arztebl Int 117(12):A575-577 [Google Scholar]
- 6.Scheidt-Nave C, Barnes B, Beyer AK, et al. (2020) Care for the chronically ill in Germany – The challenges during the COVID-19 pandemic. Journal of Health Monitoring 5(S10): 2–27. https://edoc.rki.de/handle/176904/7801 (As at 11.05.2021) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Narres M, Linnekamp U, Hochlenert D, et al. (2021) Die Versorgungsituation von Menschen mit Diabetes mellitus in Zeiten der COVID-19-Pandemie. Version 01. Kompetenznetz Public Health COVID-19, Bremen. https://www.public-health-covid19.de/images/2021/Ergebnisse/230310_Hintergundpapier_Nicht-COVID_Diabetes_finaliter.pdf (As at 11.05.2021)
- 8.Mangiapane S, Zhu L, Kretschmann J, et al. (2021) Veränderung der vertragsärztlichen Leistungsinanspruchnahme während der COVID-Krise: Tabellarischer Trendreport für das Jahr 2020. Zentralinstitut für die kassenärztliche Versorgung in Deutschland, Berlin. https://www.zi.de/fileadmin/images/content/Publikationen/Trendreport_4_Leistungsinanspruchnahme_COVID_2021-04-19.pdf (As at 06.09.2021)
- 9.Günster C, Drogan D, Hentschker C, et al. (2020) WIdO-Report: Entwicklung der Krankenhausfallzahlen während des Coronavirus-Lockdowns. Nach ICD-Diagnosekapiteln und ausgewählten Behandlungsanlässen. WIdO, Berlin. https://www.wido.de/fileadmin/Dateien/Bilder/News/2020_06_WIdO-Report_FZ-Entwicklung_Lockdown.pdf (As at 11.05.2021) [Google Scholar]
- 10.Mostert C, Hentschker C, Scheller-Kreinsen D, et al. (2021) Auswirkungen der COVID-19-Pandemie auf die Krankenhausleistungen im Jahr 2020. In: Klauber J, Wasem J, Beivers A, et al. (Eds) Krankenhaus-Report 2021: Versorgungsketten – Der Patient im Mittelpunkt. Springer; Berlin. Heidelberg, Berlin, Heidelberg, P. 277-306 [Google Scholar]
- 11.Slagman A, Behringer W, Greiner F, et al. (2020) Medical Emergencies During the COVID-19 Pandemic. Dtsch Arztebl Int 117(33-34):545-552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Damerow S, Rommel A, Prütz F, et al. (2020) Developments in the health situation in Germany during the initial stage of the COVID-19 pandemic for selected indicators of GEDA 2019/2020-EHIS. Journal of Health Monitoring 5(4):3–20. https://edoc.rki.de/handle/176904/7550.2 (As at 25.4.2021) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Du Y, Baumert J, Damerow S, et al. (2021) Utilisation of outpatient medical services by people with diagnosed diabetes during the COVID-19 pandemic in Germany. Journal of Health Monitoring 6(2): 51–58. https://edoc.rki.de/handle/176904/8404 (As at 14.01.2022) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Heidemann C, Paprott R, Huebl L, et al. (2021) Selbst eingeschätzte medizinsiche Versorgung im Verlauf der SARS-CoV-2-Pandemie in Deutschland: Ergebnisse der COSMO-Studie. Epidemiologisches Bulletin 46:3-10. https://edoc.rki.de/handle/176904/7466.2 (As at 10.03.2021) [Google Scholar]
- 15.Hajek A, De Bock F, Wieler LH, et al. (2020) Perceptions of Health Care Use in Germany during the COVID-19 Pandemic. Int J Environ Res Public Health 17(24):9351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reitzle L, Schmidt C, Farber F, et al. (2021) Perceived Access to Health Care Services and Relevance of Telemedicine during the COVID-19 Pandemic in Germany. Int J Environ Res Public Health 18(14) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Robert Koch-Institut (RKI) (2021) Studie CORONA-MONITORING lokal. www.rki.de/corona-monitoring-lokal (As at 16.09.2021)
- 18.Santos-Hövener C, Busch MA, Koschollek C, et al. (2020) Seroepidemiological study on the spread of SARS-CoV-2 in populations in especially affected areas in Germany – Study protocol of the CORONA-MONITORING lokal study. Journal of Health Monitoring 5(S5): 2–16. https://edoc.rki.de/handle/176904/7490 (As at 12.05.2021) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Santos-Hövener C, Neuhauser HK, Rosario AS, et al. (2020) Serology- and PCR-based cumulative incidence of SARS-CoV-2 infection in adults in a successfully contained early hotspot (CoMoLo study), Germany, May to June 2020. Euro Surveill 25(47) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Corona Monitoring lokal (2021) Eckdaten für Kupferzell (aktualisiert am 15.09.2021). https://www.rki.de/DE/Content/Gesundheitsmonitoring/Studien/cml-studie/Dokumente/Factsheet_Kupferzell.pdf?__blob=-publicationFile (As at 14.01.2022)
- 21.Corona Monitoring lokal (2021) Eckdaten für Bad Feilnbach (aktualisiert am 15.09.2021). https://www.rki.de/DE/Content/Gesundheitsmonitoring/Studien/cml-studie/Factsheet_Bad_Feilnbach.html (As at 14.01.2022)
- 22.Corona Monitoring lokal (2021) Eckdaten für Straubing (aktualisiert am 15.09.2021). https://www.rki.de/DE/Content/Gesundheitsmonitoring/Studien/cml-studie/Factsheet_Straubing.html (As at 14.01.2022)
- 23.Corona Monitoring lokal (2021) Eckdaten für Berlin-Mitte (aktualisiert am 15.09.2021). https://www.rki.de/DE/Content/Gesundheitsmonitoring/Studien/cml-studie/Factsheet_Berlin-Mitte.html (As at 14.01.2022)
- 24.Neuhauser H, Buttmann-Schweiger N, Ellert U, et al. (2021) Seroepidemiologische Studien zu SARS-CoV-2 in Stichproben der Allgemeinbevölkerung und bei Blutspenderinnen und Blutspendern in Deutschland – Ergebnisse bis August 2021. Epidemiologisches Bulletin 37:3-12. https://edoc.rki.de/handle/176904/8743 (As at 14.01.2022) [Google Scholar]
- 25.Robert Koch-Institut (2022) Sachbericht - Seroepidemiologische Studie zur Abschätzung der Verbreitung von SARS-CoV-2 in der Bevölkerung an besonders betroffenen Orten in Deutschland. CORONA-MONITORING lokal. Abschlussbericht 2021. Robert Koch Institute, Berlin. https://www.rki.de/DE/Content/Gesundheitsmonitoring/Studien/cml-studie/Dokumente/Abschlussbericht_2021.pdf?__blob=-publicationFile (As at 07.02.2022) [Google Scholar]
- 26.Schilling J, Buda S, Fischer M, et al. (2021) Retrospektive Phaseneinteilung der COVID-19-Pandemie in Deutschland bis Februar 2021. Epidemiologisches Bulletin 15:8-17. https://edoc.rki.de/handle/176904/7935 (As at 14.01.2022) [Google Scholar]
- 27.Statistisches Amt der Europäischen Union (Eurostat) (2017) Internationale Standardklassifikation für das Bildungswesen (ISCED). https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Glossary:International_standard_classification_of_education_(ISCED)/de (As at 25.05.2021)
- 28.Cox B, van Oyen H, Cambois E, et al. (2009) The reliability of the Minimum European Health Module. Int J Public Health 54(2):55-60 [DOI] [PubMed] [Google Scholar]
- 29.Hajek A, De Bock F, Huebl L, et al. (2021) Determinants of Postponed Cancer Screening During the COVID-19 Pandemic: Evidence from the Nationally Representative COVID-19 Snapshot Monitoring in Germany (COSMO). Risk Manag Healthc Policy 14:3003-3011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hajek A, De Bock F, Kretzler B, et al. (2021) Factors associated with postponed health checkups during the COVID-19 pandemic in Germany. Public Health 194:36-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hajek A, De Bock F, Huebl L, et al. (2021) Postponed Dental Visits during the COVID-19 Pandemic and their Correlates. Evidence from the Nationally Representative COVID-19 Snapshot Monitoring in Germany (COSMO). Healthcare (Basel) 9(1):50. [DOI] [PMC free article] [PubMed] [Google Scholar]


