Abstract
Objectives:
To determine (1) the optimal sites for mini-implant placement in the maxilla and the mandible based on dimensional mapping of the interradicular spaces and cortical bone thickness and (2) The effect of age and sex on the studied anatomic measurements.
Material and Methods:
The cone beam computed tomography images of 100 patients (46 males, 54 females) divided into two age groups (13–18 years), and (19–27 years) were used. The following interradicular measurements were performed: (1) Buccolingual bone thickness; (2) Mesiodistal spaces both buccally and palatally/lingually; and (3) Buccal and palatal/lingual cortical thicknesses.
Results:
In the maxilla, the highest buccolingual thickness existed between first and second molars; the highest mesiodistal buccal/palatal distances were between the second premolar and the first molar. The highest buccal cortical thickness was between the first and second premolars. The highest palatal cortical thickness was between central and lateral incisors. In the mandible, the highest buccolingual and buccal cortical thicknesses were between the first and second molars. The highest mesiodistal buccal distance was between the second premolar and the first molar. The highest mesiodistal lingual distance was between the first and second premolars. The highest lingual cortical thickness was between the canine and the first premolar. The males and the older age group had significantly higher buccolingual, buccal, and palatal cortical thicknesses at specific sites and levels in the maxilla and the mandible.
Conclusions:
A clinical guideline for optimal sites for mini-implant placement is suggested. Sex and age affected the anatomic measurements in certain areas in the maxilla and the mandible.
Keywords: Optimal sites, Mini-implants, Interradicular dimensions, Cortical thickness, CBCT
INTRODUCTION
Mini-implants have become a very popular type of orthodontic skeletal anchorage, which is reflected in the escalating number of studies addressing this subject. However, there is still no consensus in these studies about the factors that influence the success of mini-implants. A recent systematic review could not prove an association between the type of mini-implant, patient characteristics, placement site, surgical technique, and orthodontic and implant maintenance factors and the success rates of mini-implants.1
The present study focused on only one of these factors: implant placement site. The most common implant sites appear to be the palate, the palatal aspect of the maxillary alveolar process, the retromolar area in the mandible, and the buccal cortical plate in both the maxilla and the mandible.2–7 Among the important factors that should be considered when choosing mini-implant placement sites are soft-tissue anatomy, interradicular distance, sinus morphology, nerve location, buccolingual bone depth, and buccal and lingual cortical thicknesses.
Several studies provide measurements of the interradicular spaces at the posterior maxilla and mandible. It was reported that the volume of bone in the maxillary interradicular space between the second premolar and the first molar provides the optimal anatomic site for miniscrews in the maxilla.8–10 Poggio et al.11 ranked the safest sites available in interradicular spaces in the posterior maxilla and reported that the safest was between the first molar and the second premolar 2–8 mm from the alveolar crest; for the posterior mandible it was between the first and second molars. Hardly any data are available concerning the interradicular spaces of the anterior maxillary and mandibular areas in spite of the fact that mini-implants can also be useful in the anterior region as anchorage for mesial movement of the posterior dentition or correction of the anterior vertical occlusion.4,6
A limited number of studies have investigated cortical bone thickness in the maxilla and the mandible. Most of these studies have been carried out on a small sample or were limited to the posterior part of the jaws. The buccal cortical bone thickness seems to be greater in the mandible than in the maxilla.12–16 Baumgaertel and Hans15 studied 30 dry skulls and found that the thickness of the buccal cortical bone increases with increasing distance from the alveolar crest in the mandible and in the maxillary anterior area.
The influence of age and sex in success of mini-implants remains controversial. It seems that cortical bone is thinner in females mesial to the maxillary first molar16 However, several articles reported no association between sex and implant success.1 Motoyoshi et al.17 showed less implant success in adolescents when the implants were loaded early, whereas the success rates were similar to that in adults after a 3-month latent period.
The purpose of the present investigation was to determine the optimal sites of mini-implant placement in the anterior and posterior maxilla and mandible based on mapping of the dimensions of the interradicular spaces and cortical bone thickness using cone beam computed tomography (CBCT). In addition, we wanted to elucidate the effect of age and sex on the studied anatomic measurements.
MATERIALS AND METHODS
The sample consisted of three-dimensional (3D) images of 100 patients (46 males and 54 females; mean age, 20 years) in whom there were 66 maxillae and 34 mandibles divided into two age groups (13–18 years and 18–27 years) selected from an already available larger sample of images at the Radiology Unit, Clinic of Oral Surgery and Stomatology, University of Bern, Switzerland. Patient data were treated according to the recommendations of the declaration of Helsinki. Images were taken with the 3D Accuitomo (J Morita Manufacturing Corp, Kyoto, Japan). Of the 920 images screened, 780 were rejected according to the following exclusion criteria:
—Overlapping of crowns or roots of adjacent teeth
—Periodontal disease (determined from radiographic signs of alveolar bone resorption)
—Severe ectopic eruption (ie, buccally blocked out canines)
—Missing teeth (excluding third molars)
—Mixed dentition (in the first age group) or incomplete crown eruption
—Blurred or unclear images
The 3D images were generated by the 3DX Accuitomo XYZ Tomograph and I-Dexil software (Morita, Tokyo, Japan). Orthogonal tomographic images were constructed using the I-Dexil. After 2 months of training and trial measurements with 15 cases, the investigator made all the measurements. Four weeks later, the same investigator remeasured 10 randomly selected cases to test for intraobserver reliability.
To minimize measurement errors produced from nonstandardized head postures, all images were oriented using a standardized protocol in which the palatal plane was aligned parallel to the horizontal axis supplied by the software, and the nasal septum was aligned parallel to the vertical axis. The slicing angle would be adjusted accordingly.
Measurements
For each interradicular space in the maxilla and the mandible, from the second molar on one side to the second molar on the opposite side, the following measurements were done at three different depths from the cementoenamel junction, that is, at 2 mm, 4 mm, and 6 mm.
—Mesiodistal distance: These measurements were taken both buccally and palatally/lingually at the widest distance between each two adjacent teeth.
—Buccolingual thickness: The thickness was measured from the outermost point on the buccal side to the outermost point on the palatal/lingual side at the middle of the distance between each two adjacent teeth.
—Cortical bone thickness: Buccally and lingually/palatally, the distance between the internal and external aspects of the cortex in the middle of the interradicular distance between each two adjacent teeth was measured.
For each patient about 195 distances were measured. These distances were measured using the millimetric ruler provided by the I-Dexil (Figures 1 through 4).
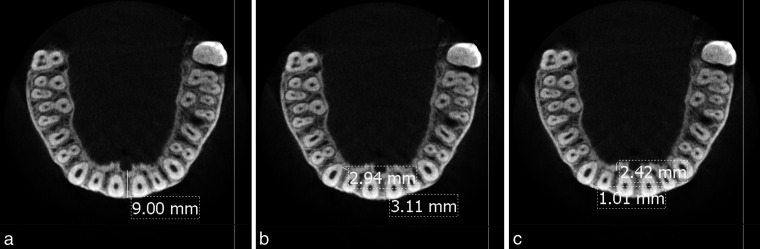
Figure 1.
Maxillary anterior region. (A) Measurement of the buccolingual thickness. (B) Measurement of the mesiodistal buccal and palatal distances. (C) Measurement of the buccal and palatal cortical thicknesses.
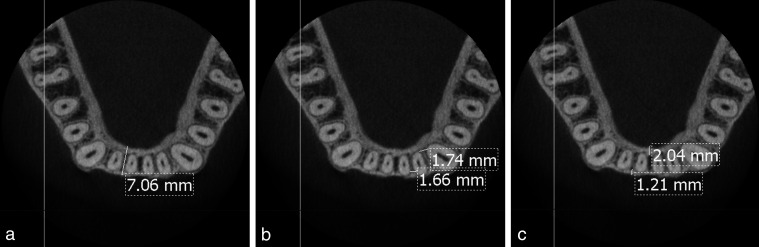
Figure 4.
Mandibular posterior region. (A) Measurement of the buccolingual thickness and the mesiodistal buccal and lingual distances. (B) Measurement of the buccal and lingual cortical thicknesses.
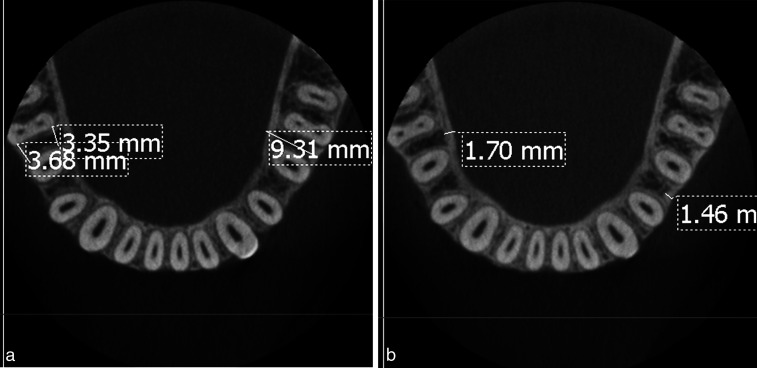
Figure 2.
Maxillary posterior region. (A) Measurement of the buccolingual thickness. (B) Measurement of the mesiodistal buccal and palatal distances. (C) Measurement of the buccal and palatal cortical thicknesses.
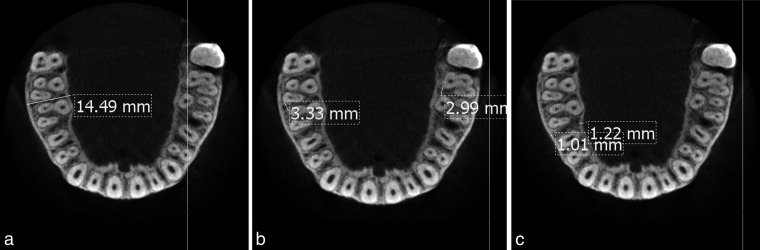
Figure 3.
Mandibular anterior region. (A) Measurement of the buccolingual thickness. (B) Measurement of the mesiodistal buccal and lingual distances. (C) Measurement of the buccal and lingual cortical thicknesses.
Statistical Analysis
Descriptive analysis was used to obtain the mean and standard deviation (SD) of all the studied measurements. Student's t-test was used to determine the intraobserver reliability. To simplify the comparative analysis, the data were divided into two regions: anterior (from canine to canine) and posterior (from the first premolar to the second molar bilaterally). Student's t-test was used for comparisons between sexes and age groups; P < .05 was considered significant, and P < .01 was considered highly significant.
RESULTS
Intraobserver Reliability
There was no significant difference (P > .05) between the repeated measurements of the 10 patients.
Interradicular Dimensions Measured
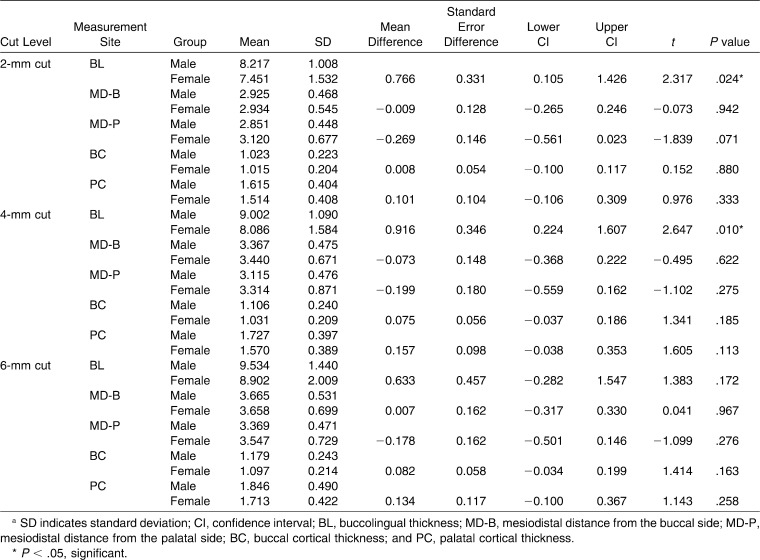
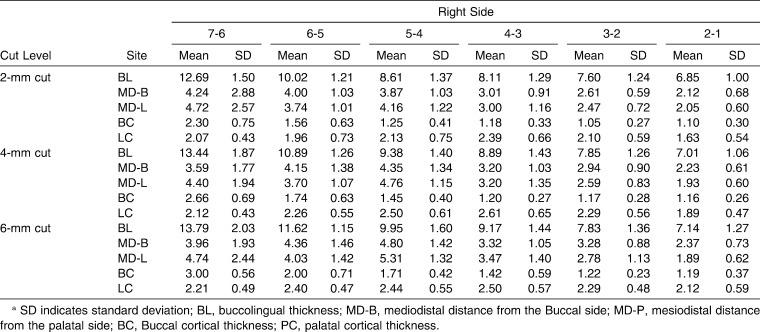
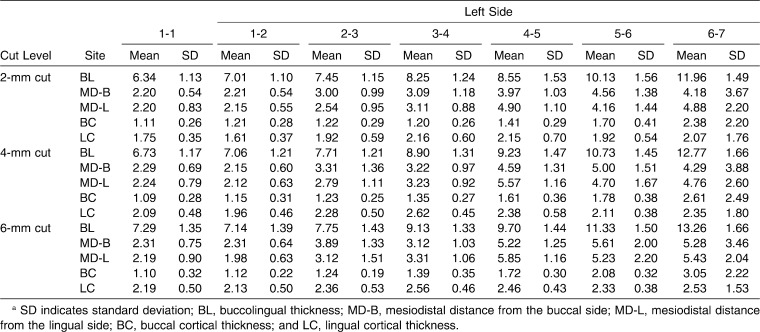
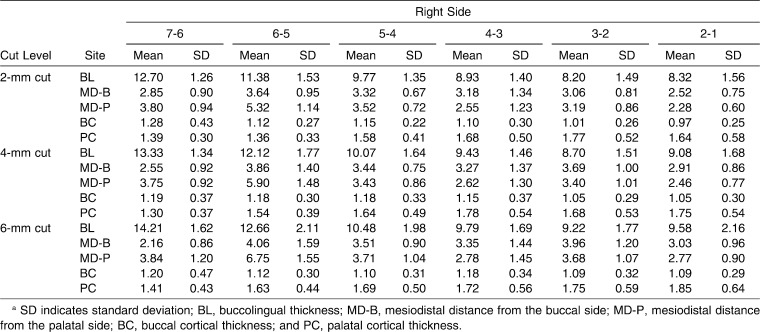
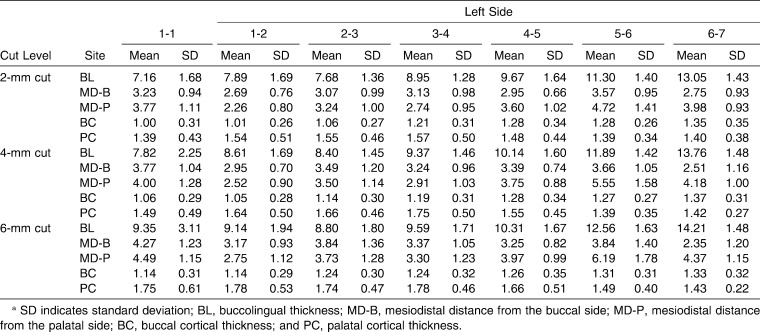
Interradicular dimensions are reported in Tables 1 and 2: (all expressed in millimeters at the 2-mm, 4-mm, and 6-mm levels from CEJ). Generally, all the dimensions measured increased upon moving apically and posteriorly except for the mesiodistal distances between the first and second molars.
Table 1A.
Means and Standard Deviations of Measurements of the Right Side of the Maxillaa
Table 2A.
Means and Standard Deviations of Measurements of the Right Side of the Mandiblea
Table 2B.
Means and Standard Deviations of Measurements of the Left Side of the Mandiblea
In the Anterior Maxilla
The highest buccolingual thickness was found between the right central and lateral incisor at the 6-mm level (9.6 ± 2.16), which decreased the more cervical the measurements were taken. The lowest buccolingual thickness was between the central incisors at the 2-mm and 4-mm level. The highest mesiodistal distance from the buccal side between the central incisors at the 6-mm level was 4.27 ± 1.23, and the lowest was between the left central and lateral incisor. The highest mesiodistal distance from the palatal side and buccal cortical thickness was between the lateral incisor and canine at the 6-mm level (3.73 ± 1.28), and (1.24 ± 0.53), respectively. The greatest palatal cortical thickness was at the 6-mm level between the central and lateral incisor (1.85 ± 0.64) and the lateral incisor and canine (1.75 ± 0.59) and was greater in the anterior region than in the posterior region.
In the Posterior Maxilla
The highest buccolingual thickness was found at the 6-mm level between the first and second molars (14.21 ± 1.48). The highest mesiodistal distances, both buccally and palatally, were found between the second premolar and the first molar (4.05 ± 1.6 and 6.75 ± 1.55, respectively). A certain pattern was found in the thickness of the buccal cortex: at the 2-mm level, the thickness was 1.35 ± 0.35 between first and second molars, but it increased to 1.36 ± 0.31 at 4 mm and then decreased to 1.32 ± 0.3214 at 6 mm. The highest palatal cortical bone thickness was found between the canine and the first premolar at the 6-mm level (1.78 ± 0.46).
In the Anterior Mandible
The highest buccolingual thickness, mesiodistal distances labially and lingually, and cortical thicknesses both labially and lingually were found between the lateral incisor and canine at the 6-mm level (7.83 ± 1.36, 3.89 ± 1.33, 3.12 ± 1.51, 1.24 ± 0.19, and 2.36 ± 0.53, respectively). The lowest measured dimensions were found between the central incisors.
In the Posterior Mandible
The highest buccolingual thickness and buccal cortical thickness were between the first and second molars (13.79 ± 2.03, 3.05 ± 2.22, respectively). The highest mesiodistal distance from the buccal side was found between the second premolar and the first molar (5.61 ± 1.99), and the highest mesiodistal distance from the lingual side was between the first and second premolars (5.85 ± 1.16). The thickest lingual cortex was found between the canine and the first premolar (2.56 ± 0.46).
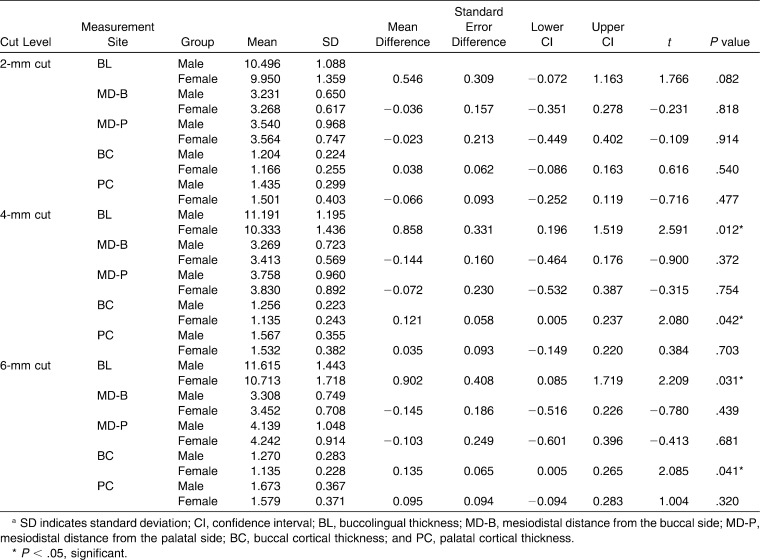
Comparison Between Sexes
Comparison between sexes was significant at P < .05 (Tables 3 through 6).
Table 1B.
Means and Standard Deviations of Measurements of the Left side of the Maxillaa
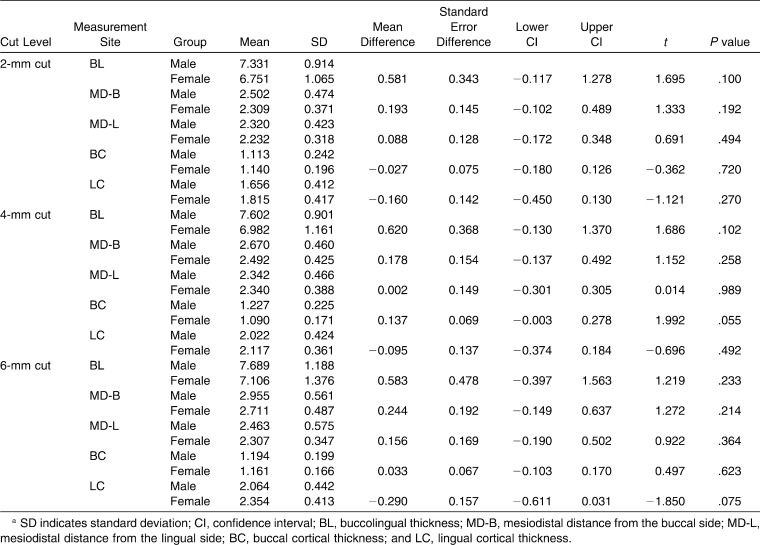
Table 3.
Comparison Between Measurements of Males and Females in the Anterior Maxillary Region (Student's t-test)a
Table 4.
Comparison Between Measurements of Males and Females in the Posterior Maxillary Region (Student's t-test)a
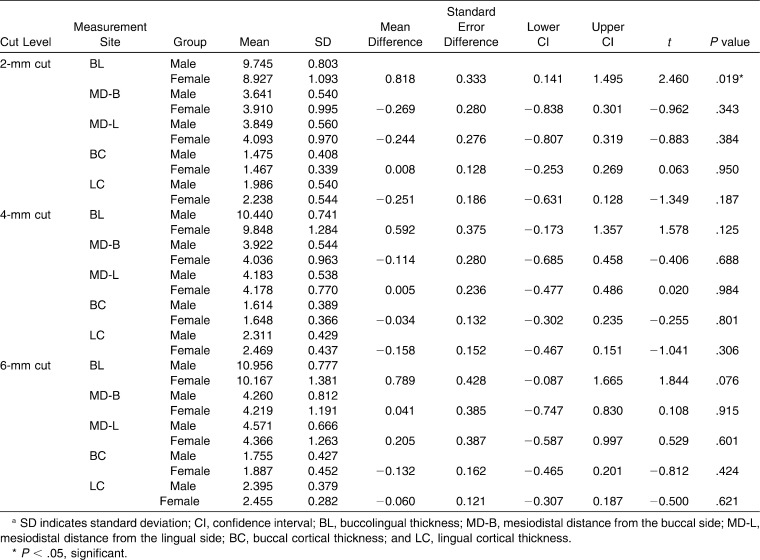
Table 5.
Comparison Between Measurements of Males and Females in the Anterior Mandibular Region (Student's t-test)a
Table 6.
Comparison Between Measurements of Males and Females in the Posterior Mandibular Region (Student's t-test)a
In the Maxilla
Anteriorly, males had significantly higher buccolingual thickness at the 2-mm and 4-mm level from the CEJ. Posteriorly, males had a significantly higher buccolingual and buccal cortical thickness at the 4-mm and 6-mm level from the CEJ.
In the Mandible
Anteriorly, there was no significant difference between sexes. Posteriorly, males had a significantly higher buccolingual thickness than females at the 2-mm level from CEJ.
Comparison Between Age Groups
Comparison between the two age groups (13–18 years) and (19–27 years) for all the measurements was significant at P < .05 and highly significant at P < .001 (Tables 7 through 10).
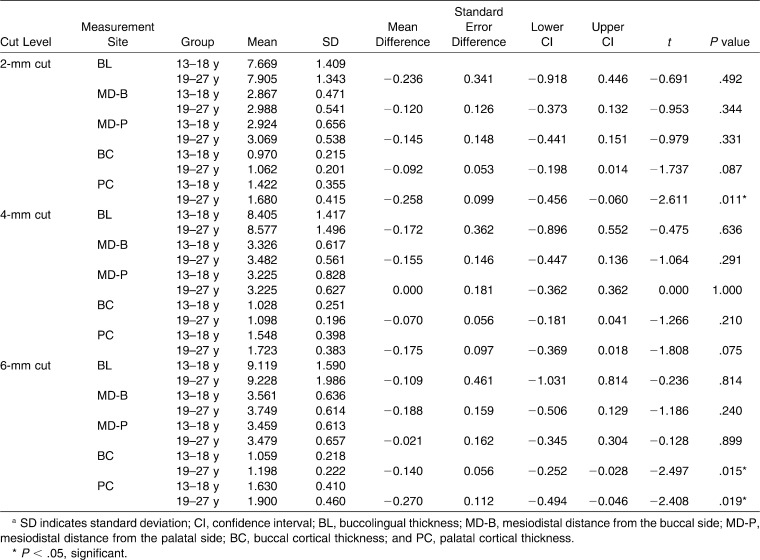
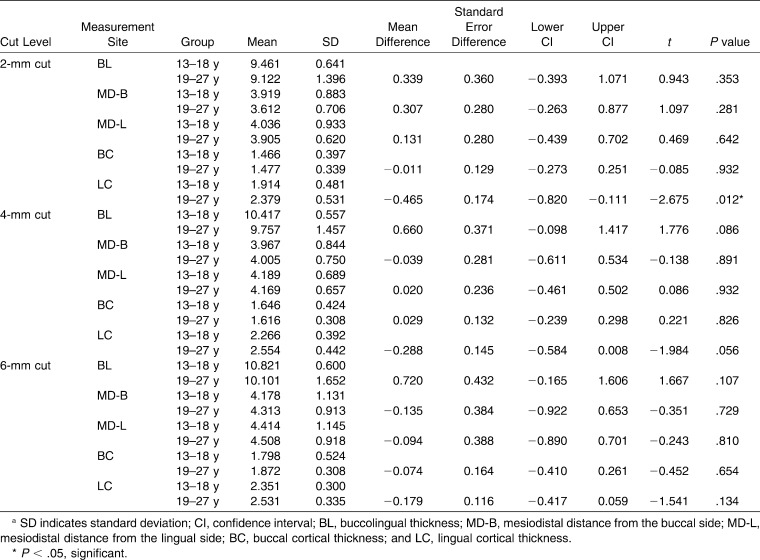
Table 7.
Comparison Between Measurements of the Two Age Groups (13–18 Years and 19–27 Years) in the Anterior Maxillary Region (Student's t-test)a
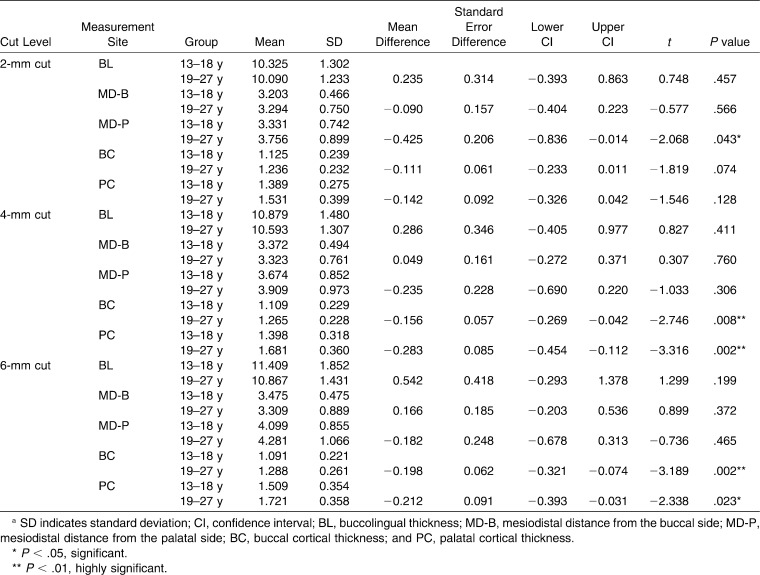
Table 8.
Comparison Between Measurements of the Two Age Groups (13–18 Years and 19–27 Years) in the Posterior Maxillary Region (Student's t-test)a
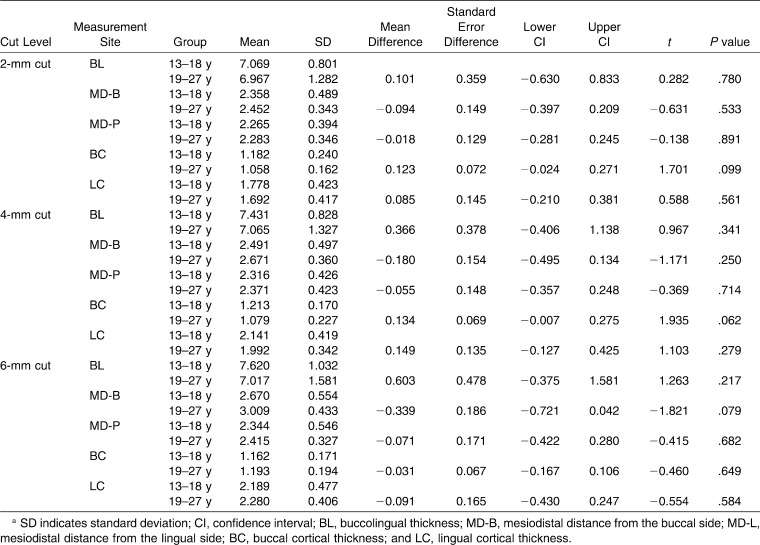
Table 9.
Comparison Between Measurements of the Two Age Groups (13–18 Years and 19–27 Years) in the Anterior Mandibular Region (Student's t-test)a
Table 10.
Comparison Between Measurements of the Two Age Groups (13–18 Years and 19–27 Years) in the Posterior Mandibular Region (Student's t-test)a
In the Maxilla
Anteriorly, the group aged 19–27 years had a significantly thicker palatal cortex at the 2-mm level from the CEJ and higher buccal and palatal cortical thicknesses at 6 mm. Posteriorly, the group aged 19–27 years had a significantly higher mesiodistal palatal distance at the 2-mm level at the CEJ and a thicker buccal and palatal cortex with a highly significant difference at the 4-mm and 6-mm level from the CEJ.
In the Mandible
Anteriorly, there was no significant difference between the two groups. Posteriorly, the group aged 19–27 years had a significantly thicker lingual cortex at the 2-mm level from the CEJ.
DISCUSSION
Many factors could affect the success rates and effectiveness of mini-implants used for establishing skeletal orthodontic anchorage. Some of these factors are implant related (type, diameter, and length of the implant), patient related (sex, age, physical status), surgical related (direction of mini-implant placement and placement torque), orthodontic related (magnitude and timing of force), location related (peri-implant bone quantity, cortical bone thickness, keratinized versus oral mucosa), and implant-maintenance related.1 The exact role of these factors, however, is not fully understood.1 The present study investigated the anatomic data gathered from 100 CBCT images to determine the optimal sites for mini-implant placement by studying two elements that are related to the mini-implant location factor: interradicular bone dimensions and cortical bone thickness. Three-dimensional measurements of the interradicular spaces at 3 vertical levels (2 mm, 4 mm, and 6 mm) from the CEJ were performed. Intraobserver reliability was established for the measurement method of this study. The availability of a relatively large number of CBCT images for this study allowed the researchers to overcome the shortcoming of limited sample size in several previous studies.11,12,18
Most studies on this topic have aimed to determine the safest sites for mini-screw placement by focusing on the posterior region of the jaws.8–11 The fact, however, that mini-implants are often useful in the anterior region for space closure4 or correction of overbite problems6 necessitated the evaluation of the anterior region as well. To fulfill this objective in the present study, data on interradicular distances and cortical bone thicknesses were provided for all the teeth, both anteriorly and posteriorly, to provide the clinician with a comprehensive anatomic map of the maxilla and the mandible.
In this study the CEJ was selected as the starting point for the measurements, unlike other studies11,19 that used the alveolar crest, which could be affected by different periodontal problems. As it is advisable to place the mini-implants in areas of attached gingival,20 the maximum level of measurement in this study was selected to be 6 mm from CEJ. Lim et al.21 excluded levels higher than 6 mm in their study on interradicular soft tissue for the same reason.
The results of this study showed a consistent increase in the buccolingual thickness and the mesiodistal distances both buccally and palatally/lingually in most of the studied sites in the maxilla and the mandible when moving apically and posteriorly. One exception was the mesiodistal buccal distance between the maxillary first and second molars. The means of the different measurements in this study were found to be in agreement with those obtained in other similar studies.8,11,12,18
Limited data are available in the literature describing the buccal cortical thickness. The results of this study showed that in the maxilla the buccal cortical thickness had a certain pattern: the thickness increased as the cuts moved apically from the CEJ to the 4-mm level, and then they decreased again at the 6-mm level. This is in agreement with the study by Baumgaertel and Hans15 on dry skulls. In the mandible, the thickness increased gradually in the apical direction; the highest was between the first and second molar, and the lowest was between the central incisors. Monnert et al.19 reported the lowest thickness between the lateral incisor and canine. Lingual and palatal cortical bone thicknesses showed a gradual increase as the cuts moved apically.
Based on the findings of the present study, the optimal site for mini-implant placement in the anterior maxilla is the interradicular space between the central and lateral incisors and between the lateral incisor and canine in the anterior mandible. These sites had the highest buccolingual and cortical thicknesses and mesiodistal distance. In the posterior region of the maxilla and the mandible the most suitable sites are between the second premolar and the first molar and between the first and second molars, which was also recommended in previous studies.8,12,18
In the present study, males had a significantly thicker buccolingual dimension and buccal cortical thickness than females in both the maxilla and the mandible. Kim et al.22 found no statistical difference between sexes in the interradicular measurements of the posterior maxilla, probably because of the small sample size (35 patients). In the maxilla, the older age group (19–27 years) had a significantly higher buccal and palatal cortical thickness both anteriorly and posteriorly. In the mandible, the older age group had a significantly thicker lingual cortex. In the study by Swasty et al.,13 the age group of 40–49 years had a significantly higher buccal cortical thickness in the mandible. In the present study more significant differences were found between the sexes and age groups in the maxilla than in the mandible, which could be due to the difference in sample size. Thus, it would be expected that mini-implants placed in males and in those older than 18 years to have higher success rates because of the higher interradicular dimensions and thicker cortical bone thickness, especially in the maxilla.
CONCLUSIONS
The optimal site for mini-implant placement in the anterior region is between the central and lateral incisors in the maxilla and between the lateral incisor and the canine in the mandible at the 6-mm level from the CEJ. At the buccal aspect of the posterior region of both jaws, the optimal sites are between the second premolar and the first molar and between the first and second molars. Palatally, the optimal site is between the first and second premolars as it has the advantage of the highest cortical thickness. The more apical the site, the safer the placement.
The males and the age group older than 18 years had a significantly higher buccolingual, palatal, and buccal cortical thickness at specific levels and sites in the maxilla and the mandible.
Acknowledgments
The authors would like to thank Dr. M. Bornstein, Head of Radiology Unit, Clinic of Oral Surgery and Stomatology, University of Bern, Switzerland, for providing us with the access to the CBCT images used in this study.
REFERENCES
- 1.Reynders R, Ronchi L, Bipat S. Mini-implants in orthodontics: a systematic review of the literature. Am J Orthod Dentofacial Orthop. 2009;135:564.e1–564.e19. doi: 10.1016/j.ajodo.2008.09.026. [DOI] [PubMed] [Google Scholar]
- 2.Park H. S, Kwon O. W, Sung J. H. Nonextraction treatment of an open bite with micro screw anchorage. Am J Orthod Dentofacial Orthop. 2006;130:391–402. doi: 10.1016/j.ajodo.2005.07.014. [DOI] [PubMed] [Google Scholar]
- 3.Roth A, Yildirim M, Diedrich P. Forced eruption with microscrew anchorage for preprosthetic leveling of the gingival margin. J Orofac Orthop. 2004;65:513–519. doi: 10.1007/s00056-004-0430-z. [DOI] [PubMed] [Google Scholar]
- 4.Park Y. C, Choi Y. J, Choi N. C, Lee J. S. Esthetic segmental retraction of maxillary anterior teeth with a palatal appliance and orthodontic mini-implants. Am J Orthod Dentofacial Orthop. 2007;131:537–544. doi: 10.1016/j.ajodo.2005.05.051. [DOI] [PubMed] [Google Scholar]
- 5.Kanomi R. Mini-implant for orthodontic anchorage. Am J Orthod Dentofacial Orthop. 1997;31:763–767. [PubMed] [Google Scholar]
- 6.Xun C, Zeng X, Wang X. Microscrew anchorage in skeletal anterior open-bite treatment. Angle Orthod. 2007;77:47–56. doi: 10.2319/010906-14R.1. [DOI] [PubMed] [Google Scholar]
- 7.Park H. S, Lee S. K, Kwon O. W. Group distal movement of teeth using microscrew implant anchorage. Angle Orthod. 2005;75:602–609. doi: 10.1043/0003-3219(2005)75[602:GDMOTU]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 8.Carano A, Velo A, Incorvati I, Poggio P. Clinical application of the mini-screw-anchorage-system (M.A.S.) in the maxillary alveolar bone. Prog Orthod. 2004;5:212–230. [PubMed] [Google Scholar]
- 9.Carano A, Melsen B. Implants in orthodontics. Prog Orthod. 2005;6:62–69. [PubMed] [Google Scholar]
- 10.Park H. S. An anatomic study using CT images for the implantation of micro-implants. Korean J Orthod. 2002;32:435–441. [Google Scholar]
- 11.Poggio P. M, Incorvati C, Velo S, Carano A. “Safe zones”: a guide for miniscrew positioning in the maxillary and mandibular arch. Angle Orthod. 2006;76:191–197. doi: 10.1043/0003-3219(2006)076[0191:SZAGFM]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 12.Deguchi T, Nasu M, Murakami K, Yabuuchi T, Kamioka H, Takano-Yamamoto T. Quantitative evaluation of cortical bone thickness with computed tomographic scanning for orthodontic implants. Am J Orthod Dentofacial Orthop. 2006;129:721.e7–721.e12. doi: 10.1016/j.ajodo.2006.02.026. [DOI] [PubMed] [Google Scholar]
- 13.Swasty D, Lee J. S, Huang J. C, Maki K, Gansky S. A, Hatcher D, Miller A. J. Anthropometric analysis of the human mandibular cortical bone as assessed by cone-beam computed tomography. J Oral Maxillofac Surg. 2009;67:491–500. doi: 10.1016/j.joms.2008.06.089. [DOI] [PubMed] [Google Scholar]
- 14.Park J, Cho H. J. Three-dimensional evaluation of interradicular spaces and cortical bone thickness for placement and initial stability for microimplants in adults. Am J Orthod Dentofacial Orthop. 2009;136:314.e1–314.e12. doi: 10.1016/j.ajodo.2009.01.023. [DOI] [PubMed] [Google Scholar]
- 15.Baumgaertel S, Hans B. Buccal cortical bone thickness for mini-implant placement. Am J Orthod Dentofacial Orthop. 2009;136:230–235. doi: 10.1016/j.ajodo.2007.10.045. [DOI] [PubMed] [Google Scholar]
- 16.Ono A, Motoyoshi M, Shimizu N. Cortical bone thickness in the buccal posterior region for orthodontic mini-implants. Int J Oral Maxillofac Surg. 2008;37:334–340. doi: 10.1016/j.ijom.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 17.Motoyoshi M, Matsuoka M, Shimizu N. Application of orthodontic mini-implants in adolescents. Int J Oral Maxillofac Surg. 2007;36:695–699. doi: 10.1016/j.ijom.2007.03.009. [DOI] [PubMed] [Google Scholar]
- 18.Hu K. S, Kang M. K, Kim T. W, Kim K. H, Kim H. J. Relationships between dental roots and surrounding tissues for orthodontic miniscrew installation. Angle Orthod. 2009;79:37–45. doi: 10.2319/083107-405.1. [DOI] [PubMed] [Google Scholar]
- 19.Monnerat C, Restle L, Mucha J. N. Tomographic mapping of mandibular interradicular spaces for placement of orthodontic mini-implants. Am J Orthod Dentofacial Orthop. 2009;135:428.e1–428.e9. doi: 10.1016/j.ajodo.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 20.Melsen B. Mini-implants: where are we? J Clin Orthod. 2005;39:539–547. [PubMed] [Google Scholar]
- 21.Lim W. H, Lee S. K, Wikesjö U. M, Chun Y. S. A descriptive tissue evaluation at maxillary interradicular sites: implications for orthodontic implant placement. Clin Anat. 2007;20:760–765. doi: 10.1002/ca.20513. [DOI] [PubMed] [Google Scholar]
- 22.Kim S. H, Yoon H. G, Cho Y. S, Hwang E. H, Kook Y. A, Nelson G. Evaluation of interdental space of the maxillary posterior area for orthodontic mini-implants with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2009;135:635–641. doi: 10.1016/j.ajodo.2007.06.013. [DOI] [PubMed] [Google Scholar]