Abstract
Objective:
To systematically review the relationship between malocclusions and masticatory performance. In addition, we will perform a qualitative analysis of the methodological soundness of the studies.
Materials and Methods:
A literature survey was done by applying the Medline database (www.ncbi.nim.nih.gov) in the period from January 1965 to June 2009, using the “Medical Subject Headings” term malocclusion crossed with various combinations of the following terms: masticatory performance, masticatory efficiency, and chewing efficiency. The articles were separated into two main topics: (1) the influence of malocclusion treatment (orthognathic surgery) and (2) the influence of malocclusion type and severity.
Results:
The search strategy used identified 78 articles. After selection according to the inclusion/exclusion criteria, 12 articles qualified for the final analysis. The research quality and methodological soundness were high in one study, medium in 10 studies, and low in one study. The most serious shortcomings comprised the clinical trials and controlled clinical trials designs with small sample sizes and inadequate description of selection criteria. Lack of method error analysis and the absence of blinding in measurements were other examples of shortcomings.
Conclusions:
Malocclusions cause decreased masticatory performance, especially as it relates to reduced occlusal contacts area. The influence of malocclusion treatment (orthognathic surgery) on masticatory performance is only measurable 5 years after treatment.
Keywords: Masticatory performance, Malocclusion, Orthognathic surgery, Systematic review
INTRODUCTION
Mastication represents the first stage of the digestive process, during which foods are physically broken down into smaller particles to increase their surface area, thereby facilitating enzymatic processing during later stages of digestion.1,2 Mastication can be measured by several means, including masticatory ability, efficiency, and performance. Masticatory ability is a subjective measure, a perception of how well subjects think they break down foods.3 Efficiency pertains to the number of masticatory cycles (ie, number of chews) required to reduce foods to a certain size,4 and masticatory performance, the most common and powerful measure used, pertains to the particle size distribution of food chewed after a standardized number of cycles.4,5
Several factors influence masticatory performance, including body size, bite force,6 number of functional tooth units,7 occlusal contact area,8 and malocclusions.9 Although not as potent a factor as the mutilated dentition, malocclusions can negatively affect subjects' ability to process and break down foods.10 Unfortunately, most of the studies evaluating the relationship between malocclusions and mastication are not conclusive in terms of identifying the subtle influences of the different types of malocclusions on masticatory performance.
Given this background, a systematic review was warranted, focusing on the relationship between malocclusions and masticatory performance. Furthermore, a qualitative analysis of the methodological soundness of the studies in the review was performed.
MATERIALS AND METHODS
Search Strategies
A literature survey was done by applying the Medline database (www.ncbi.nim.nih.gov) in the period from January 1965 to June 2009, using the “Medical Subject Headings” term malocclusion crossed with various combinations of the following terms: masticatory performance, masticatory efficiency, and chewing efficiency.
Selection Criteria
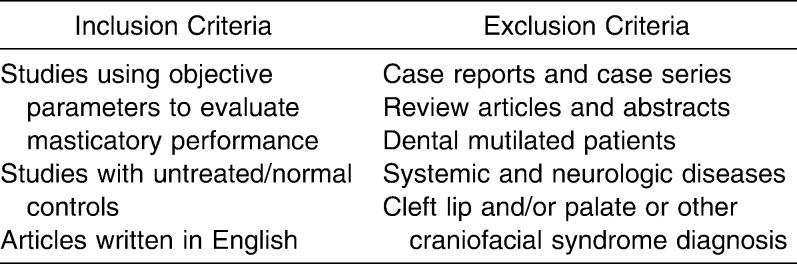
The inclusion and exclusion criteria are given in detail in Table 1.
Table 1.
Initial Inclusion and Exclusion Criteria for the Retrieved Studies
Data Collection and Analysis
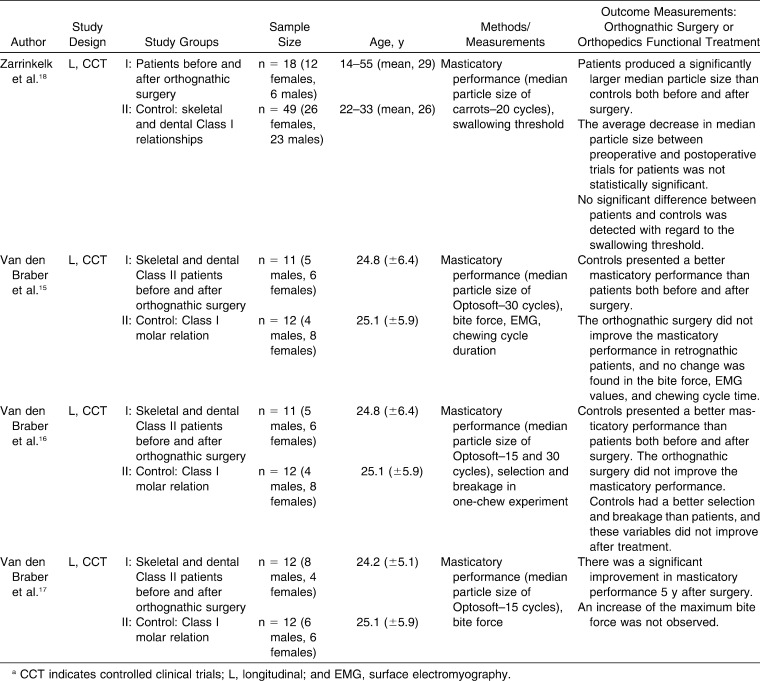
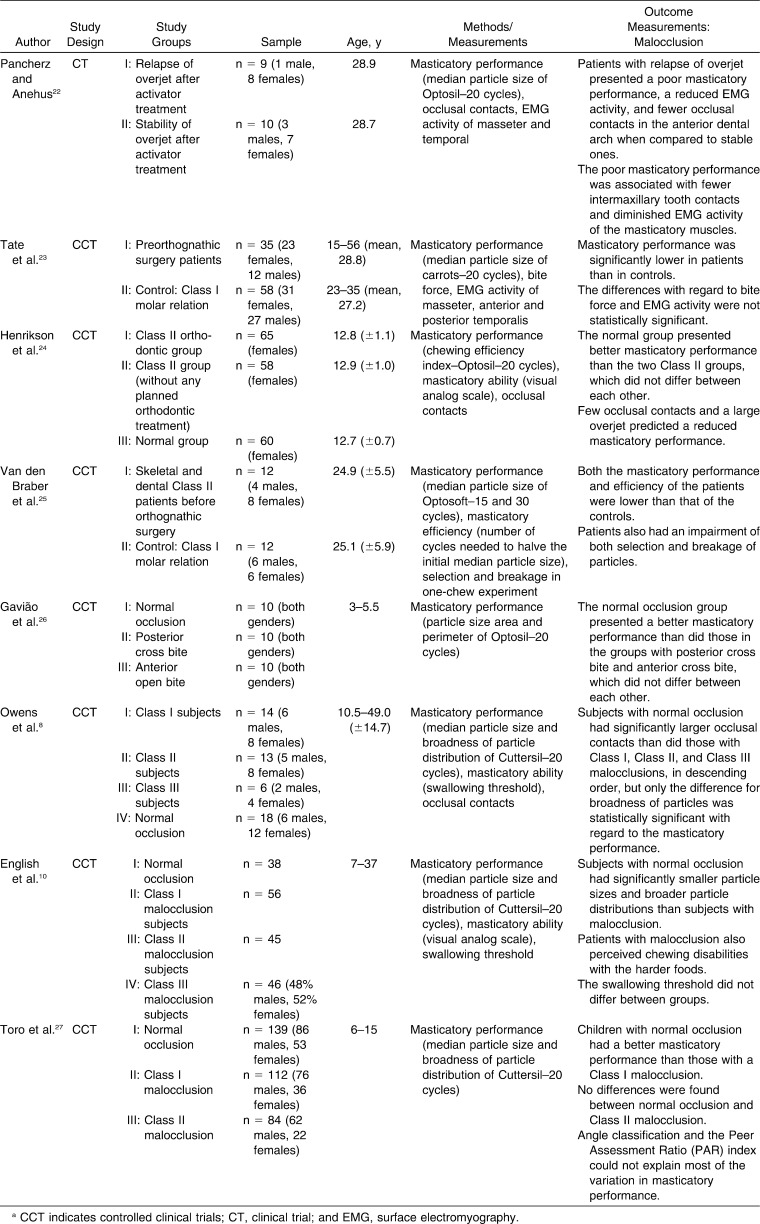
Data were collected on the following items: author, year of publication, study design, study groups, methods/measurements, and outcome measurements. The articles were separated into two main topics: (1) the influence of malocclusion treatment (orthognathic surgery) (Table 2) and (2) the influence of malocclusion type and severity (Table 3).
Table 2.
Masticatory Performance Studies in Orthognathic Surgical Patientsa
Table 3.
Masticatory Performance Studies Regarding Different Malocclusion Typesa
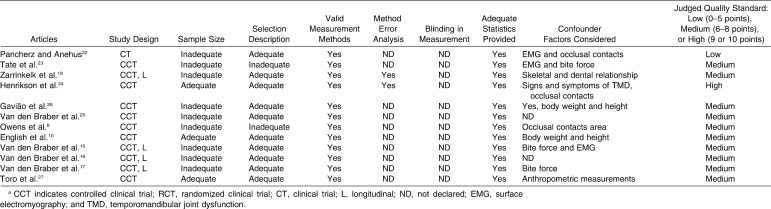
In addition, to document the methodological soundness of each article, a quality evaluation was performed with respect to preestablished characteristics,11,12 evaluating the following eight variables: (1) study design (randomized clinical trials, prospective trials, or controlled clinical trials [CCTs]—3 points; clinical trials [CTs]—1 point); (2) adequate sample size—1 point; (3) adequate selection description—1 point; (4) valid measurement methods—1 point; (5) use of method error analysis—1 point; (6) blinding in measurement—1 point; (7) adequate statistics provided—1 point; and (8) confounders included in analysis—1 point. Each study was categorized as low (0–5 points), medium (6–8 points), or high (9 or 10 points). The data extraction and quality scoring from each article were assessed independently by two researchers who selected the articles by reading the title and abstracts. All of the articles that appeared to meet the inclusion criteria were selected. One hundred percent agreement was obtained in this phase between the two researchers. The reference lists of the selected articles were also searched manually for additional relevant publications that might have been missed in the database searches.13
RESULTS
The search strategy yielded 78 articles. After selection according to the inclusion/exclusion criteria, 12 articles qualified for the final analysis (Tables 2 and 3). The research quality and methodological soundness were high in one study, medium in 10 studies, and low in one study (Table 4). The most serious shortcomings were the CT and CCT designs with small sample sizes and inadequate description of selection criteria. Lack of method error analysis and the absence of blinding in measurements were other examples of shortcomings. However, the choice of statistical methods was explained in all articles. Considering the use of confounding variables, only two studies did not report any factor. In all other reports, confounding variables, such as surface electromyography, occlusal contacts, bite force, signs and symptoms of temporomandibular joint dysfunction, and anthropometric measurements, were declared. All measurement methods used in the studies were valid.
Table 4.
Quality Evaluation of the Retrieved Studiesa
DISCUSSION
This systematic review aimed to select all clinical trials verifying the relationship between malocclusion and masticatory performance. No previous review study could be found. Twelve studies were retrieved. From a methodological point of view, it was notable that all of the studies used examination methods without blinding design. In all studies, the methods used to detect and analyze the relationship between malocclusion and masticatory performance were valid and well known. However, great variations in test food and number of cycles were observed, which could make comparisons among all studies difficult.1,14 On the other hand, studies15–17 published by the same group were found, allowing more comprehensive conclusions based on their results.
The influence of malocclusion treatment (orthognathic surgery) on masticatory performance showed that mastication was still hampered in comparison to results obtained from controls, even after surgical correction. In addition, surgical correction did not improve masticatory performance significantly.15,16,18 However, it was suggested that after surgery, some time is needed in order for the muscles to adapt to the new bone position. The muscle fibers are stretched and may also decrease bite force when compared to the situation before surgery.15,19 This fact was confirmed when a significant increase in masticatory performance was noted 5 years after surgery.17
According to these results, it is important to consider that longitudinal studies with short postsurgical time evaluation should be observed cautiously, since the musculature may need a long time to readapt the new incorporated modifications. It seems that at least 5 years are needed to measure a real improvement in masticatory performance.17
In addition, simultaneous evaluation of number and area of occlusal contacts, bite force, muscle thickness, amount of lateral jaw movement, pain, and muscle activity are encouraged in order to control all co-variables after orthognathic surgery, once masticatory performance may be influenced by all of these factors.6,20,21
The influence of malocclusion type and severity on masticatory performance was also investigated. In general, malocclusions caused decreased masticatory performance.8,10,22–27 Undoubtedly poor masticatory performance is associated with fewer intermaxillary tooth contacts. In addition, a diminished muscle activity was noted.22 A reduced platform to grind the food affects masticatory performance.6 Subjects with a reduced occlusal contacts area cannot pulverize their food to the same extent as subjects with more occlusal units, in a fixed number of chewing strokes. Fontijn-Tekamp et al.28 reported that the number of occlusal units was the most important factor that affected the median particle size of masticatory performance and the swallowing threshold. Similar results were previously reported.7 Occlusal contacts promote mandibular stability at maximal intercuspation29 and have an influence on chewing function8 and masticatory muscle activity.30
Masticatory performance is also influenced by bite force. It is believed that bite force increases with teeth in occlusal contact.31,32 In all selected studies, only Tate et al.23 evaluated bite force and masticatory performance in orthodontic patients. The differences with regard to bite force in preorthognathic surgery patients and Class I molar relation was not statistically significant. However, in this study, sample size and selection description were considered inadequate for drawing any further conclusions. Therefore, the correction of malocclusion through orthodontic treatment becomes an important resource with which to improve occlusal contacts and, consequently, masticatory performance.
CONCLUSIONS
Malocclusions cause decreased masticatory performance, especially as it relates to a reduced occlusal contacts area.
The influence of malocclusion treatment (orthognathic surgery) on masticatory performance is only measurable 5 years after treatment.
Acknowledgments
The authors are grateful to the Brazilian fostering agencies: Fundação de Amparo a Pesquisa do Estado de Minas Gerais (FAPEMIG) and Fundação de Amparo Pesquisa do Estado do Rio Grande do Sul (FAPERGS), which supported the present study.
REFERENCES
- 1.Pereira L. J, Gavião M. B. D, van der Bilt A. Influence of oral characteristics and food products on masticatory function. Acta Odontol Scand. 2006;64:193–201. doi: 10.1080/00016350600703459. [DOI] [PubMed] [Google Scholar]
- 2.van der Bilt A, Engelen L, Abbink J, Pereira L. J. Effects of adding fluids to solid foods on muscle activity and number of chewing cycles. Eur J Oral Sci. 2007;115:198–205. doi: 10.1111/j.1600-0722.2007.00448.x. [DOI] [PubMed] [Google Scholar]
- 3.Carlsson G. E. Masticatory efficiency: the effect of age, the loss of teeth and prosthetic rehabilitation. J Int Dent. 1984;34:93–97. [PubMed] [Google Scholar]
- 4.Bates J. F, Stafford G. D, Harrison A. Masticatory function—a review of the literature. J Oral Rehab. 1976;3:57–67. doi: 10.1111/j.1365-2842.1976.tb00929.x. [DOI] [PubMed] [Google Scholar]
- 5.Slagter A. P, Bosman F, van der Glas H. W, van der Bilt A. Human jaw–elevator muscle activity and food comminution in the dentate and edentulous state. Arch Oral Biol. 1993;38:195–205. doi: 10.1016/0003-9969(93)90028-k. [DOI] [PubMed] [Google Scholar]
- 6.Fontijn-Tekamp F. A, Slagter A. P, van der Bilt A, et al. Biting and chewing in overdentures, full dentures, and natural dentitions. J Dent Res. 2000;79:1519–1524. doi: 10.1177/00220345000790071501. [DOI] [PubMed] [Google Scholar]
- 7.Hatch J. P, Shinkai R. S, Sakai S, Rugh J. D, Paunovich E. D. Determinants of masticatory performance in dentate adults. Arch Oral Biol. 2001;46:641–648. doi: 10.1016/s0003-9969(01)00023-1. [DOI] [PubMed] [Google Scholar]
- 8.Owens S, Buschang P. H, Throckmorton G. S, Palmer L, English J. Masticatory performance and areas of occlusal contact and near contact in subjects with normal occlusion and malocclusion. Am J Orthod Dentofacial Orthop. 2002;12:602–609. doi: 10.1067/mod.2002.122829. [DOI] [PubMed] [Google Scholar]
- 9.Buschang Peter H. Masticatory ability and performance: the effects of mutilated and maloccluded dentitions. Semin Orthod. 2006;12:92–101. [Google Scholar]
- 10.English J. D, Buschang P. H, Throckmorton G. S. Does malocclusion affect masticatory performance? Angle Orthod. 2002;72:21–27. doi: 10.1043/0003-3219(2002)072<0021:DMAMP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Antczak A. A, Tang J, Chalmers T. C. Quality assessment of randomized control trials in dental research I. Methods. J Periodont Res. 1986;21(4):305–314. doi: 10.1111/j.1600-0765.1986.tb01464.x. [DOI] [PubMed] [Google Scholar]
- 12.Jadad A. R, Moore R. A, Carroll D, Jenkinson C, Reynolds D. J, Gavaghan D. J, McQuay H. J. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 13.Andrade A. S, Gameiro G. H, Derossi M, Gavião M. B. D. Posterior crossbite and functional changes—a systematic review. Angle Orthod. 2009;79:380–385. doi: 10.2319/030708-137.1. [DOI] [PubMed] [Google Scholar]
- 14.Gambareli F. R, Serra M. D, Pereira L. J, Gavião M. B. D. Influence of measurement technique, test food, teeth and muscle force interactions in masticatory performance. J Texture Stud. 2007;38:2–20. [Google Scholar]
- 15.van den Braber W, van der Glas H, van der Bilt A, Bosman F. Masticatory function in retrognathic patients, before and after mandibular advancement surgery. J Oral Maxillofac Surg. 2004;62:549–554. doi: 10.1016/j.joms.2003.06.016. [DOI] [PubMed] [Google Scholar]
- 16.van den Braber W, van der Bilt A, van der Glas H. W, Bosman F, Rosenberg A, Koole R. The influence of orthognathic surgery on masticatory performance in retrognathic patients. J Oral Rehabil. 2005;32:237–241. doi: 10.1111/j.1365-2842.2004.01436.x. [DOI] [PubMed] [Google Scholar]
- 17.van den Braber W, van der Bilt A, van der Glas H, Rosenberg T, Koole R. The influence of mandibular advancement surgery on oral function in retrognathic patients: a 5-year follow-up study. J Oral Maxillofac Surg. 2006;64:1237–1240. doi: 10.1016/j.joms.2006.04.019. [DOI] [PubMed] [Google Scholar]
- 18.Zarrinkelk H. M, Throckmorton G. S, Ellis E, III, Sinn D. P. A longitudinal study of changes in masticatory performance of patients undergoing orthognathic surgery. J Oral Maxillofac Surg. 1995;53:777–782; discussion, 782–783. doi: 10.1016/0278-2391(95)90331-3. [DOI] [PubMed] [Google Scholar]
- 19.Finn R. A, Throckmorton G. S, Bell W. H, et al. Biomechanical considerations in the surgical correction of mandibular deficiency. Oral Surg. 1980;38:257. [PubMed] [Google Scholar]
- 20.van der Bilt A, Engelen L, Pereira L. J, van der Glas H. W, Abbink J. H. Oral physiology and mastication. Physiol Behav. 2006;89:22–27. doi: 10.1016/j.physbeh.2006.01.025. [DOI] [PubMed] [Google Scholar]
- 21.Castelo P. M, Gavião M. B. D, Perreira L. F, Bonjardim L. R. Masticatory muscle thickness, bite force, and occlusal contacts in young children with unilateral posterior crossbite. Eur J Orthod. 2007;29:149–156. doi: 10.1093/ejo/cjl089. [DOI] [PubMed] [Google Scholar]
- 22.Pancherz H, Anehus M. Masticatory function after activator treatment. An analysis of masticatory efficiency, occlusal contact conditions and EMG activity. Acta Odontol Scand. 1978;36:309–316. doi: 10.3109/00016357809029081. [DOI] [PubMed] [Google Scholar]
- 23.Tate G. S, Throckmorton G. S, Ellis E, III, Sinn D. P. Masticatory performance, muscle activity, and occlusal force in pre orthognathic surgery patients. J Oral Maxillofac Surg. 1994;52:476–481; discussion, 482. doi: 10.1016/0278-2391(94)90344-1. [DOI] [PubMed] [Google Scholar]
- 24.Henrikson T, Ekberg E. C, Nilner M. Masticatory efficiency and ability in relation to occlusion and mandibular dysfunction in girls. Int J Prosthodont. 1998;11:125–132. [PubMed] [Google Scholar]
- 25.van den Braber W, van der Glas H. W, van der Bilt A, Bosman F. Chewing efficiency of pre-orthognathic surgery patients: selection and breakage of food particles. Eur J Oral Sci. 2001;109:306–311. doi: 10.1034/j.1600-0722.2001.00092.x. [DOI] [PubMed] [Google Scholar]
- 26.Gavião M. B, Raymundo V. G, Sobrinho L. C. Masticatory efficiency in children with primary dentition. Pediatr Dent. 2001;23:499–505. [PubMed] [Google Scholar]
- 27.Toro A, Buschang P. H, Throckmorton G, Roldán S. Masticatory performance in children and adolescents with Class I and II malocclusions. Eur J Orthod. 2006;28:112–119. doi: 10.1093/ejo/cji080. [DOI] [PubMed] [Google Scholar]
- 28.Fontijn-Tekamp F. A, van der Bilt A, Abbink J. H, Bosman F. Swallowing threshold and masticatory performance in dentate adults. Physiol Behav. 2004;432:431–436. doi: 10.1016/j.physbeh.2004.08.026. [DOI] [PubMed] [Google Scholar]
- 29.Rodrigues C. H, Mori M, Rodrigues A. A, Nascimento E. J, Gonçalves F. M, Santana K. C. Distribution of different types of occlusal contacts at maximal intercuspal position in deciduous dentition. J Clin Pediatr Dent. 2003;27:339–346. doi: 10.17796/jcpd.27.4.l2r48wx81t5l8325. [DOI] [PubMed] [Google Scholar]
- 30.Ferrario V, Serrao G, Dellavia C, Caruso E, Sforza C. Relationship between the number of occlusal contacts and masticatory muscle activity in healthy young adults. J Craniomandibular Pract. 2002;20:91–98. doi: 10.1080/08869634.2002.11746196. [DOI] [PubMed] [Google Scholar]
- 31.Sonnesen L, Bakke M, Solow B. Bite force in pre-orthodontic children with unilateral crossbite. Eur J Orthod. 2001;23:741–749. doi: 10.1093/ejo/23.6.741. [DOI] [PubMed] [Google Scholar]
- 32.Sonnesen L, Bakke M. Molar bite force in relation to occlusion, craniofacial dimensions, and head posture in pre-orthodontic children. Eur J Orthod. 2005;27:58–63. doi: 10.1093/ejo/cjh069. [DOI] [PubMed] [Google Scholar]