Abstract
Objective:
To compare the different methods of pain control intervention during fixed orthodontic appliance therapy.
Materials and Methods:
A computerized literature search was performed in MEDLINE (1966–2009), The Cochrane Library (Issue 4, 2009), EMBASE (1984–2009), and CNKI (1994–2009) to collect randomized controlled trials (RCTs) for pain reduction during orthodontic treatment. Data were independently extracted by two reviewers and a quality assessment was carried out. The Cochrane Collaboration's RevMan5 software was used for data analysis. The Cochrane Oral Health Group's statistical guidelines were followed.
Results:
Twenty-six RCTs were identified and six trials including 388 subjects were included. Meta-analysis showed that ibuprofen had a pain control effect at 6 hours and at 24 hours after archwire placement compared with the placebo group. The standard mean difference was −0.47 and −0.48, respectively. There was no difference in pain control between ibuprofen, acetaminophen, and aspirin. Other analgesics such as tenoxicam and valdecoxib had relatively lower visual analog scale (VAS) scores in pain perception. Low-level laser therapy (LLLT) was also an effective approach for pain relief with VAS scores of 3.30 in the LLLT group and 7.25 in the control group.
Conclusions:
Analgesics are still the main treatment modality to reduce orthodontic pain despite their side effects. Some long-acting nonsteroidal anti-inflammatory drugs (NSAIDs) and cyclo-oxygenase enzyme (COX-2) inhibitors are recommended for their comparatively lesser side effects. Their preemptive use is promising. Other approaches such as LLLT have aroused researchers' attention.
Keywords: Pain, Orthodontic treatment, Fixed orthodontic appliance, Meta-analysis, Randomized clinical trials
INTRODUCTION
Pain and discomfort are common clinical symptoms in orthodontic patients, especially 2 to 4 days after fixed orthodontic appliances are placed. It has even been suggested that orthodontic pain can discourage some patients from seeking treatment and might cause a number of patients to discontinue treatment.1 After an orthodontic procedure, it is typical to experience pain and soreness 24 hours after placement of the appliance. The pain generally occurs after placement of the first archwire2–4 and subsides after a week.5
Researchers attributed the initial and delayed pain response to hyperalgesia of the periodontal ligament. This hyperalgesia makes the periodontal ligament sensitive to released algogens such as histamine, bradykinin, prostaglandins, and serotonin.6 The increase in the levels of these mediators elicits a pain response following orthodontic force application.
At present there is no universal recommendation on the use of analgesics in pain reduction. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and acetaminophen are commonly recommended. Their analgesic action has been explained by their ability to inhibit the synthesis of prostaglandins at the site of the tissue injury. This is thought to be through inhibition of the cyclo-oxygenase enzymes COX-1 and COX-2.7
Because the use of analgesics has side effects, they are contraindicated in patients who are allergic to those drugs. To find alternatives for pain relief, researchers have looked for other new, but safer approaches, such as low-level laser therapy (LLLT).8–12 LLLT is a new internationally accepted designation and is defined as laser treatment in which the energy output is low enough so as not to cause a rise in the temperature of the treated tissue above 36.5°C or normal body temperature.13 Because of its lower energy output and intensity, its effects are mainly nonthermal and biostimulatory. The mechanism of laser analgesia is its anti-inflammatory and regenerative effects on neurons and its conditioning effect on tooth enamel.14,15
Since the measurements of pain intensity are diverse, most of the studies have utilized a visual analog scale (VAS), which is designed to present the subject with a rating scale with minimum constraints16 to evaluate pain perception. The VAS is a line whose ends are anchored and measures the pain intensity by a gradated scale from 0 to 10. The subject is expected to mark a location on the line corresponding to the amount of pain experienced, considering 0 as no pain and 10 as unbearable pain intensity. The distance of the mark from the end of the scale is then taken to represent a “pain score.” Most subjects with pain understand the concept and can quickly make the measurement.
At present, there are some animal models established to evaluate pain relief and tooth movement through animal behavior.17,18 These procedures followed the Guidelines of Animal Research or were approved by the institutional review board of the universities. However, these studies have limited clinical significance, are inconsistent and less pertinent than clinical studies, and offer results that can only be extrapolated to the human with great caution. Researchers tend to design more reasonable ethical human intervention experiments and to seek a relatively more efficient way to control orthodontic pain. Among these studies, randomized clinical trials (RCTs) and systematic reviews with meta-analysis are believed to be the better way to provide more practical and reliable suggestions and information for clinical practice.19,20
The purpose of this systematic review is to compare the clinical outcome of different methods of pain intervention. Two questions are put forward: (1) Are medications still the main treatment modality to reduce orthodontic pain? (2) Are there any other new approaches proved to be more effective in pain control?
MATERIALS AND METHODS
Literature Search and Study Selection
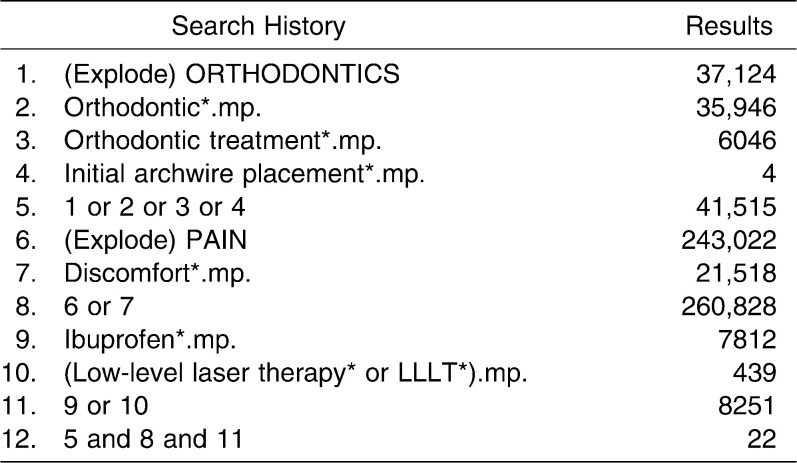
A computerized literature search was performed using MEDLINE (1966–2009) (Table 1), The Cochrane Library (Issue 4, 2009), EMBASE (1984–2009), and CNKI (1994–2009) with no language restriction. Randomized controlled trials and controlled clinical trials conducted in humans were identified. A number of useful references and appropriate search strategies were received from the Cochrane Handbook for Systematic Reviews of Interventions.21 Two reviewers independently conducted the study selection using pilot-tested forms22 (Table 1). Titles and abstracts of all potential relevant studies were identified before retrieval of the full articles. Full articles were obtained if there was insufficient data in the title and abstract to make a clear decision.
Table 1.
MEDLINE (Ovid) Search Strategy (Use “*” for Truncation)
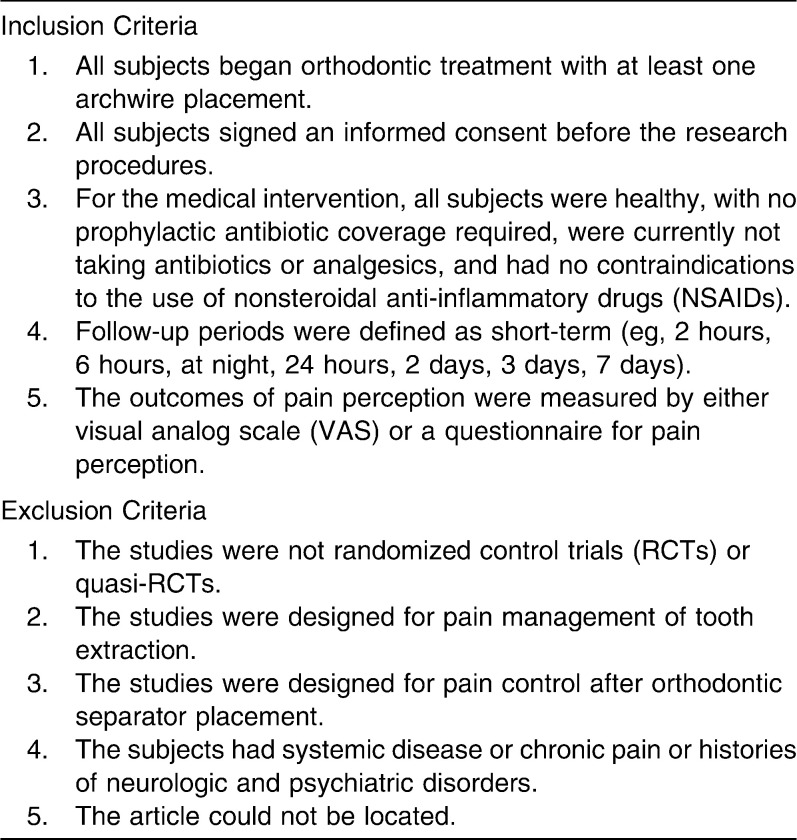
Selection Criteria
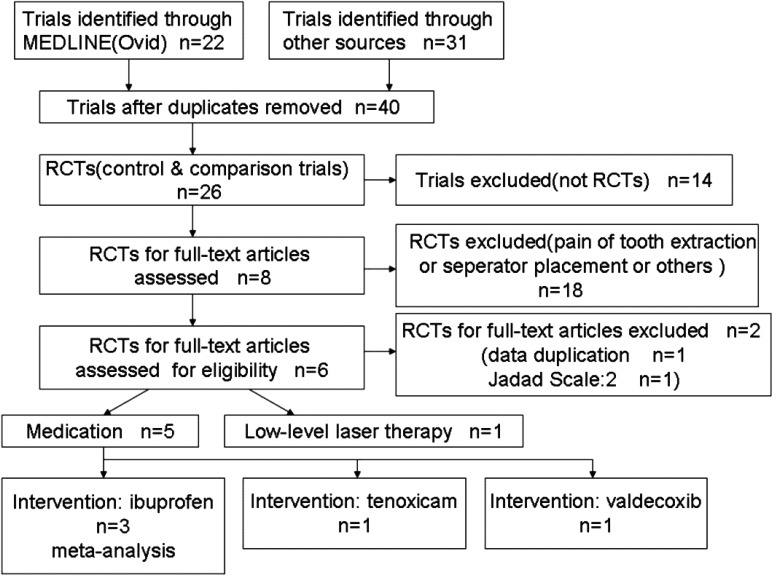
The inclusion and exclusion criteria are listed in Table 2. Two reviewers independently evaluated the quality of the searched articles to establish whether the studies met the inclusion criteria. Disagreements were resolved by discussion, and a third reviewer consulted where necessary. The articles in their reference lists were also scanned to be optimally identified. All studies meeting the inclusion criteria underwent validity assessment and data extraction. Studies rejected at this or subsequent stages were recorded in Figure 1, which describes the review retrieval flow from selection to meta-analysis.
Table 2.
Inclusion and Exclusion Criteria in the Analysis
Figure 1.
Flow diagram of study selection and meta-analysis.
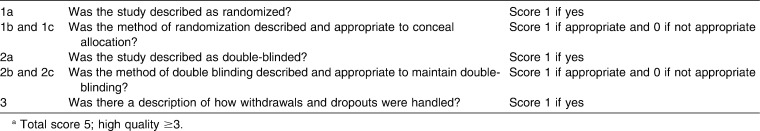
Methodologic Quality
According to the principles and procedures of a meta-analysis,23 two reviewers independently assessed each selected study for methodologic quality, based on the criteria defined by Jadad et al.24, maximum score 5 and high/acceptable score ≥3 (Table 3). All of the included studies should have “acceptable” methodologic quality.
Table 3.
Methodological Quality Criteriaa of Jadad et al.24
Data Extraction and Meta-analysis
Data were extracted from each study independently and entered into a computerized database. The information extracted included the name of the first author, year of publication, mean scores of experimental and control groups, and standard deviation of experimental and control groups. Differences were resolved by discussion to reach consensus between the reviewers.
Meta-analysis was conducted with the help of RevMan 5 software provided by the Cochrane Collaboration. Standard mean difference and 95% confidence interval (CI) were calculated using continuous data of the selected studies. Statistical tests of heterogeneity were used to assess whether the observed variability in study results was greater than that expected to occur by chance. The heterogeneity between studies was assessed using a Q statistical test by examining the type of participants, interventions, and outcomes in each study. Meta-analyses were done only if there were studies of similar comparisons reporting the same outcome measures.25,26
RESULTS
Study Selection and Data Summary
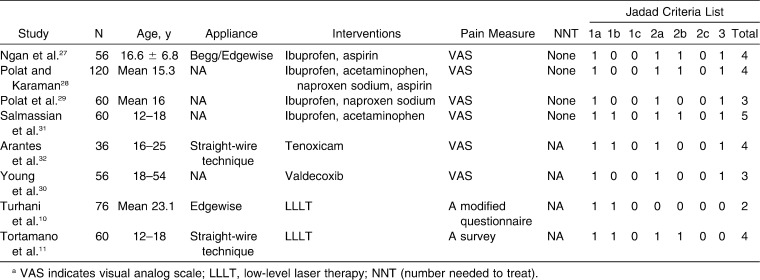
Characteristics of the trials
Of the eight qualified trials (Ngan et al.27, Polat and Karaman28, Polat' et al.29, Young et al.30, Turhani et al.10, Salmassian et al.31, Arantes et al.32, Tortamano et al.11), one trial (Polat et al.29) was excluded due to data duplication with authors' other trial (Polat and Karaman28) and another (Turhani et al.10) was judged not to be a double-blinded RCT with its Jadad Scale at 2.
Six eligible trials (Ngan et al.27, Polat and Karaman28, Young et al.30, Salmassian et al.31, Arantes et al.32, Tortamano et al.11), comprising 388 subjects, met the inclusion criteria. All trials were conducted at university dental clinics and all trials declared that patients had signed the necessary consent informs. The data summary of these eight trials and their Jadad Scale are presented in Table 4.
Table 4.
Data Summary of Eight Qualified Trials and Their Jadad Scalea
Data analysis
Medicine
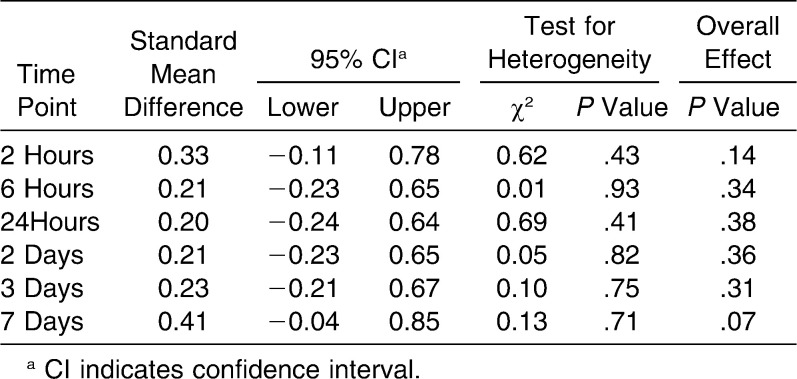
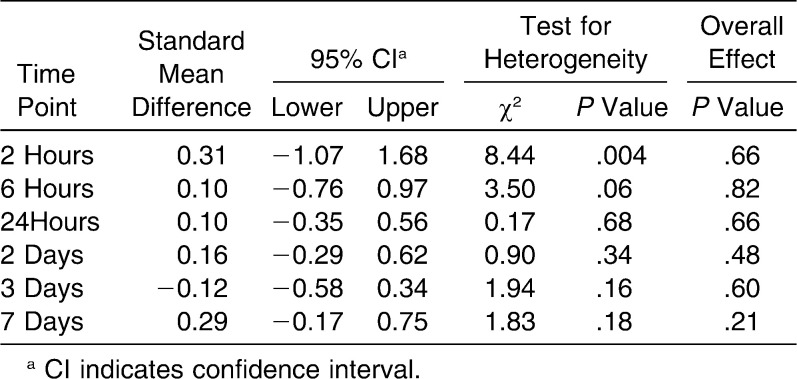
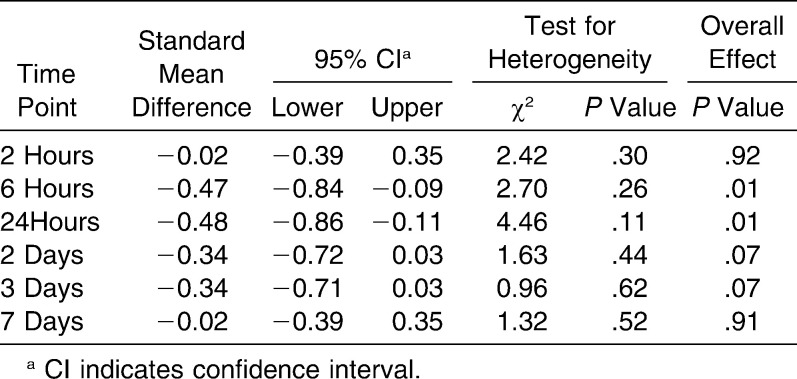
Ibuprofen vs control groups: meta-analysis
Ibuprofen was used as a representative NSAIDs on the basis of its efficacy for postoperative relief of dental pain. Acetaminophen was believed not to affect tooth movement, and aspirin was the traditional NSAID. The question of whether ibuprofen had an advantage in pain relief compared to acetaminophen and aspirin needs to be further studied. Totally, three trials were included in this group. According to different control groups and inactive group, the meta-analysis was divided into three subgroups: (1) ibuprofen vs acetaminophen (Polat and Karaman28 and Salmassian et al.31); (2) ibuprofen vs aspirin (Ngan et al.27 and Polat and Karaman28; (3) ibuprofen vs placebo (Ngan et al.27, Polat and Karaman28 and Salmassian et al.31). Meta-analyses of these three subgroups are summarized in Tables 5–7.
Table 5.
Meta-analysis Data Summary: Ibuprofen vs Acetaminophen
Table 6.
Meta-analysis Data Summary: Ibuprofen vs Aspirin
Table 7.
Meta-analysis Data Summary: Ibuprofen vs Placebo
In subgroup 1, at different time points within 7 days, the standard mean difference ranged between 0.20 and 0.41, indicating the results slightly favored the control group (acetaminophen). Though acetaminophen appeared to have a better effect on pain relief than ibuprofen, this difference did not reach statistical significance with an overall P > .05. In subgroup 2, similar results appeared between ibuprofen and aspirin.
In subgroup 3, compared with the placebo, ibuprofen was indicated to be more effective for pain relief at 6 hours and at 24 hours when the initial archwire was placed. The standard mean differences were −0.47 and −0.48 at 6 hours and 24 hours, respectively, and the overall P values were all .01 (P < .05), showing that the results favored the experimental group (ibuprofen) more than the control group (placebo). However, after 24 hours, the standard mean difference still favored the ibuprofen group, but its effects had no statistically significant difference with the placebo (P > .05) (Figure 2).
Figure 2.
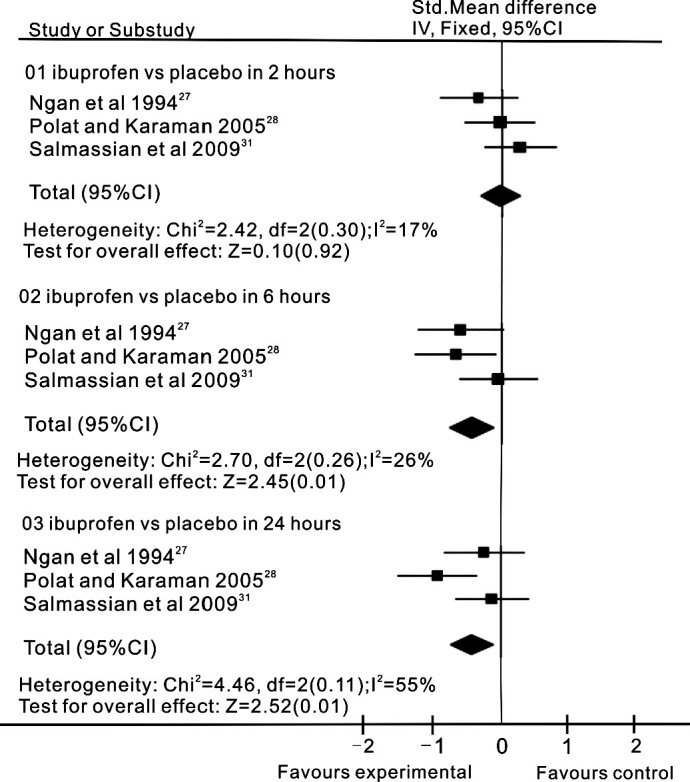
Ibuprofen (experimental) and placebo (control) groups for meta-analysis results, reported in standard mean difference (95% confidence interval), show evidence favoring ibuprofen for pain reduction at 6 hours and at 24 hours after activation of fixed orthodontic treatment.
Valdecoxib
One RCT was obtained. Young et al.30 reported that the scores of VAS were 4.6, 6.6, 8.8, respectively, when measuring experienced discomfort in preemptive, postoperative, and placebo use. This suggests that preemptive analgesics might be an approach to prevent discomfort associated with initial archwire placement in healthy adults.
Tenoxicam
One RCT was obtained. Arantes et al.32 reported that pain intensity in the tenoxicam group was lower than in the placebo groups. The difference in pain intensity between the experimental and control groups was greatest at 12 hours when assessed after activation of orthodontic treatment.
Low-level Laser Therapy
One trial was included for this group, and there was some evidence to support the use of LLLT for pain reduction during fixed orthodontic appliance therapy. However, many diverse opinions existed concerning this kind of clinical trial, such as duration of treatment, dosage (radiant power, frequency, energy density), and pain measure, which caused us to preclude a meta-analysis.
In a study by Tortamano et al.,11 the patients in the LLLT group had less oral pain and a lower intensity of pain. The VAS score for the most painful day was 3.30 in the LLLT group compared with 7.25 in the control group with no laser treatment, and 8.55 in the placebo group with simulated laser treatment. Meanwhile, pain ceased on the third day in the LLLT group, but on the fifth day in the control and placebo groups. This indicated the efficacy of LLLT for pain control after placement of the first orthodontic archwire.
DISCUSSION
For treatment of pain induced by fixed orthodontic appliance, this systematic review found evidence favoring medicine and low-level laser therapy for pain relief in the short term.
Few in vivo studies were found in the literature search since pain is a subjective phenomenon that is difficult to assess. Many variables come into play when one attempts to measure and quantify it.33–35 It is dependent upon factors such as age, gender, individual pain threshold, the magnitude of the force applied, present emotional state and stress, cultural differences, and previous pain experiences.34 However, as clinical trials, especially well-designed randomized clinical trials, provide more useful information and practical suggestions, it is imperative to offer an update on the interventions of pain during fixed orthodontic appliance therapy, especially after initial archwire placement.
Of six included trials, three reported using an orthodontic appliance, including edgewise, Begg, and straight-wire technique. All of these appliances are considered conventional appliances compared with the self-ligating bracket systems. It is believed these appliances result in similar pain experience, and therefore their data are synthesized in this meta-analysis.
Since gastric ulceration, bleeding disorders, allergy, etc are among the common adverse effects in NSAIDs, orthodontic researchers and clinicians have devoted themselves to finding much safer analgesics from the many kinds of NSAIDs. At first, ibuprofen was chosen to be safe and effective. But clinical trials revealed that the effect of ibuprofen on pain relief was limited.
Also, there are still many controversies on the use of NSAIDs because of their potential influence on tooth movement.36,37 Acetaminophen is preferred because it does not inhibit prostaglandin synthesis and has no deleterious effects on tooth movement.38–40 Meta-analysis has revealed that there is no difference in pain relief between ibuprofen, acetaminophen, and aspirin. Although compared with a placebo, ibuprofen has a better effect on pain control and there always exists the placebo effect. This calls for properly performed double-blind trials to avoid this psychological effect. Recently, some long-acting NSAIDs such as tenoxicam and COX-2 inhibitors such as valdecoxib were studied, and they have proved to be more effective and convenient than other analgesics. Recent research towards their preemptive use as well as concentration on the ideal dosage of those agents is promising.
Considering the side effects of analgesics, other approaches have been tested to reduce pain from orthodontic procedures. Data have shown the efficacy of LLLT for pain control after placement of the first archwire.10,11 LLLT for pain relief is believed to be noninvasive and easy to administer, with no known adverse tissue reactions. The reason for reducing its clinical use would be the total time (32–37.5 minutes) for application to both dental arches. Also, LLLT should be applied immediately after orthodontic appliance bonding in clinics.11 A well-designed double-blind trial is another limitation. How could the laser therapy be handled between the experimental and control groups so that the operators and patients are both blinded to the difference? Face mask or glasses are suggested by researchers in the included studies, but whether these approaches can be properly performed to eliminate experimental bias needs further investigation.
Apart from medication and LLLT, many researchers have been exploring other effective ways for pain management during fixed orthodontic treatment. The use of vibratory stimulation to reduce orthodontic pain was first reported by Marie et al.,41 but on detailed analysis it was found that once the discomfort sets in, most of the patients were not able to tolerate the vibrations. Bartlett et al.42 compared pretreatment and follow-up calls and the effects of each on pain perception after initial archwire placement and found that a telephone call can reduce patients' self-reported pain. Chewing gum or a plastic wafer was also suggested. Hwang et al.43 observed pain relief in the majority of patients after chewing wafers (56%), but the rest of the subjects reported increased discomfort.
However, all of these suggested pain management methods were devoid of well-designed RCTs, and therefore were excluded from this systematic review. Because of the limited amount of comparative evidence, there is an apparent need for high-quality RCTs to further investigate the effectiveness of these methods for interventions during fixed orthodontic appliance therapy. Orthodontic researchers and clinicians need to explore more effective treatment techniques, combinations, or approaches to evaluate and manage orthodontic pain experienced by patients.
CONCLUSIONS
Analgesics are still the main treatment modality to reduce orthodontic pain. However, the pharmacologic actions as well as their side effects should be identified before prescribing these medications in routine clinical practice.
Some long-acting NSAIDs and COX-2 inhibitors are interestingly recommended for their comparatively fewer side effects, and their preemptive use is promising.
Other relatively safer approaches such as LLLT have aroused researchers' attention. Up to now, there is still limited evidence to suggest their benefit in the use of LLLT, vibratory stimulation, and other nonpharmacologic modalities.
Acknowledgments
We acknowledge Professor SHI Zong-dao for his guidance in conducting this systematic review and meta-analysis.
REFERENCES
- 1.Oliver R. G, Knapman Y. M. Attitudes to orthodontic treatment. Br J Orthod. 1985;12:179–188. doi: 10.1179/bjo.12.4.179. [DOI] [PubMed] [Google Scholar]
- 2.Scheurer P. A, Firestone A. R, Burgin W. B. Perception of pain as a result of orthodontic treatment with fixed appliances. Eur J Orthod. 1996;18:349–357. doi: 10.1093/ejo/18.4.349. [DOI] [PubMed] [Google Scholar]
- 3.Soltis J. E, Nakfoor P. R, Bowman D. C. Changes in ability of patients to differentiate intensity of forces of applied to maxillary central incisors during orthodontic treatment. J Dent Res. 1971;50:590–596. doi: 10.1177/00220345710500031101. [DOI] [PubMed] [Google Scholar]
- 4.Jones M. L. An investigation into the initial discomfort caused by placement of an archwire. Eur J Orthod. 1984;6:48–54. doi: 10.1093/ejo/6.1.48. [DOI] [PubMed] [Google Scholar]
- 5.Ngan P, Kess B, Wilson S. Perception of discomfort by patients undergoing orthodontic treatment. Am J Orthod Dentofacial Orthop. 1989;96:47–53. doi: 10.1016/0889-5406(89)90228-x. [DOI] [PubMed] [Google Scholar]
- 6.Krishnan V. Orthodontic pain: from causes to management—a review. Eur J Orthod. 2007;29:170–179. doi: 10.1093/ejo/cjl081. [DOI] [PubMed] [Google Scholar]
- 7.Vane J. R. Inhibition of prostaglandin synthesis as a mechanism of action for aspirin-like drugs. Nat New Biol. 1971;231:237–239. doi: 10.1038/newbio231232a0. [DOI] [PubMed] [Google Scholar]
- 8.Lim H. M, Lew K. K, Tay D. K. A clinical investigation of the efficacy of low level laser therapy in reducing orthodontic postadjustment pain. Am J Orthod Dentofacial Orthop. 1995;108:614–622. doi: 10.1016/s0889-5406(95)70007-2. [DOI] [PubMed] [Google Scholar]
- 9.Limpanichkul W, Godfrey K, Srisuk N, Rattanayatikul C. Effects of low-level laser therapy on the rate of orthodontic tooth movement. Orthod Craniofac Res. 2006;9:38–43. doi: 10.1111/j.1601-6343.2006.00338.x. [DOI] [PubMed] [Google Scholar]
- 10.Turhani D, Scheriau M, Kapral D, Benesch T, Jonke E, Bantleon H. P. Pain relief by single low-level laser irradiation in orthodontic patients undergoing fixed appliance therapy. Am J Orthod Dentofacial Orthop. 2006;130:371–377. doi: 10.1016/j.ajodo.2005.04.036. [DOI] [PubMed] [Google Scholar]
- 11.Tortamano A, Lenzi D. C, Haddad A. C, Bottino M. C, Dominguez G. C, Vigorito J. W. Low-level laser therapy for pain caused by placement of the first orthodontic archwire: a randomized clinical trial. Am J Orthod Dentofacial Orthop. 2009;136:662–667. doi: 10.1016/j.ajodo.2008.06.028. [DOI] [PubMed] [Google Scholar]
- 12.Youssef M, Ashkar S, Hamade E, Gutknecht N, Lampert F, Mir M. The effect of low-level laser therapy during orthodontic movement: a preliminary study. Lasers Med Sci. 2008;23:27–33. doi: 10.1007/s10103-007-0449-7. [DOI] [PubMed] [Google Scholar]
- 13.Harris D. M. Biomolecular mechanisms of laser biostimulation. J Clin Laser Med Surg. 1991;8:277–280. [Google Scholar]
- 14.Okamoto H, Iwase T, Saito T, Morioka T. The possible application of He-Ne laser for dental plaque control. J Jpn Soc Laser Med. 1993;14:3–7. [Google Scholar]
- 15.Roberts-Harry D. P. Laser etching of teeth for orthodontic bracket placement: a preliminary clinical study. Lasers Surg Med. 1992;12:467–470. doi: 10.1002/lsm.1900120502. [DOI] [PubMed] [Google Scholar]
- 16.Linacre J. M. Visual analogue scales. Rasch Measurements Transactions. 1998;12:639. [Google Scholar]
- 17.de Carlos F, Cobo J, Perillan C, Garcia M. A, Arguelles J, Vijande M, Costales M. Orthodontic tooth movement after different coxib therapies. Eur J Orthod. 2007;29:596–599. doi: 10.1093/ejo/cjm072. [DOI] [PubMed] [Google Scholar]
- 18.Shibazaki T, Yozgatian J. H, Zeredo J. L, Gonzales C, Hotokezaka H, Koga Y, Yoshida N. Effect of celecoxib on emotional stress and pain-related behaviors evoked by experimental tooth movement in the rat. Angle Orthod. 2009;79:1169–1174. doi: 10.2319/121108-629R.1. [DOI] [PubMed] [Google Scholar]
- 19.Coward D. D. Partial randomization design in a support group intervention study. West J Nurs Res. 2002;24:406–421. doi: 10.1177/01945902024004008. [DOI] [PubMed] [Google Scholar]
- 20.Torabinejad M, Bahjri K. Essential elements of evidenced-based endodontics: steps involved in conducting clinical research. J Endod. 2005;31:563–569. doi: 10.1097/01.don.0000164137.28104.2f. [DOI] [PubMed] [Google Scholar]
- 21.Higgins J. P. T, Green S. The Cochrane Library. Chichester, UK: John Wiley & Sons Ltd; 2005. Cochrane handbook for systematic reviews of interventions 4.2.5. [Google Scholar]
- 22.Cicchetti D. V. Assessing inter-rater reliability for rating scales: resolving some basic issue. Br J Psychiatry. 1976;129:452–456. doi: 10.1192/bjp.129.5.452. [DOI] [PubMed] [Google Scholar]
- 23.Torabinejad M, Bahjri K. Essential elements of evidenced-based endodontics: steps involved in conducting clinical research. J Endod. 2005;31:563–569. doi: 10.1097/01.don.0000164137.28104.2f. [DOI] [PubMed] [Google Scholar]
- 24.Jadad A. R, Moore R. A, Carroll D, Jenkinson C, Reynolds D. J, Gavaghan D. J, McQuay H. J. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 25.Egger M, Smith G. D. Meta-analysis: potentials and promise. BMJ. 1997;315:1371–1374. doi: 10.1136/bmj.315.7119.1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Egger M, Smith G. D, Phillips A. N. Meta-analysis: principles and procedures. BMJ. 1997;315:1533–1537. doi: 10.1136/bmj.315.7121.1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ngan P, Wilson S, Shanfeld J, Amini H. The effect of ibuprofen on the level of discomfort in patients undergoing orthodontic treatment. Am J Orthod Dentofacial Orthop. 1994;106:88–95. doi: 10.1016/S0889-5406(94)70025-7. [DOI] [PubMed] [Google Scholar]
- 28.Polat O, Karaman A. L. Pain control during fixed orthodontic appliance therapy. Angle Orthod. 2005;75:214–219. doi: 10.1043/0003-3219(2005)075<0210:PCDFOA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 29.Polat O, Karaman A. L, Durmus E. Effects of preoperative ibuprofen and naproxen sodium on orthodontic pain. Angle Orthod. 2005;75:791–796. doi: 10.1043/0003-3219(2005)75[791:EOPIAN]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 30.Young A. N, Taylor R. W, Taylor S. E, Linnebur S. A, Buschang P. H. Evaluation of preemptive valdecoxib therapy on initial archwire placement discomfort in adults. Angle Orthod. 2006;76:251–259. doi: 10.1043/0003-3219(2006)076[0251:EOPVTO]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 31.Salmassian R, Oesterle L. J, Shellhart W. C, Newman S. M. Comparison of the efficacy of ibuprofen and acetaminophen in controlling pain after orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 2009;135:516–521. doi: 10.1016/j.ajodo.2007.05.020. [DOI] [PubMed] [Google Scholar]
- 32.Arantes G. M, Arantes V. M, Ashmawi H. A, Posso I. P. Tenoxicam controls pain without altering orthodontic movement of maxillary canines. Orthod Craniofac Res. 2009;12:14–19. doi: 10.1111/j.1601-6343.2008.01432.x. [DOI] [PubMed] [Google Scholar]
- 33.Sergl H. G, Klages U, Zentner A. Pain and discomfort during orthodontic treatment: causative factors and effects on compliance. Am J Orthod Dentofacial Orthop. 1998;114:684–691. doi: 10.1016/s0889-5406(98)70201-x. [DOI] [PubMed] [Google Scholar]
- 34.Bergius M, Kiliaridis S, Berggren U. Pain in orthodontics. A review and discussion of the literature. J Orofac Orthop. 2000;61:125–137. doi: 10.1007/BF01300354. [DOI] [PubMed] [Google Scholar]
- 35.Erdinc A. M, Dincer B. Perception of pain during orthodontic treatment with fixed appliances. Eur J Orthod. 2004;26:79–85. doi: 10.1093/ejo/26.1.79. [DOI] [PubMed] [Google Scholar]
- 36.Sandy J. R, Harris M. Prostaglandin and tooth movement. Eur J Orthod. 1984;6:175–182. doi: 10.1093/ejo/6.3.175. [DOI] [PubMed] [Google Scholar]
- 37.Kyrkanides S, O'Banion M. K, Subtelny J. D. Non-steroidal anti-inflammatory drugs in orthodontic tooth movement: metalloproteinase activity and collagen synthesis by endothelial cells. Am J Orthod Dentofacial Orthop. 2000;118:203–209. doi: 10.1067/mod.2000.105872. [DOI] [PubMed] [Google Scholar]
- 38.Kehoe M. J, Cohen S. M, Zarrinia K, Cowan A. The effect of acetaminophen, ibuprofen, and misoprostol on prostaglandin E2 synthesis and the degree and rate of orthodontic tooth movement. Angle Orthod. 1996;66:339–350. doi: 10.1043/0003-3219(1996)066<0339:TEOAIA>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 39.Roche J. J, Cisneros G. J, Acs G. The effect of acetaminophen on tooth movement in rabbits. Angle Orthod. 1997;67:231–236. doi: 10.1043/0003-3219(1997)067<0231:TEOAOT>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 40.Arias O, Marquez-Orozco M. C. Aspirin, acetaminophen, and ibuprofen: their effects on orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 2006;130:364–370. doi: 10.1016/j.ajodo.2004.12.027. [DOI] [PubMed] [Google Scholar]
- 41.Marie S. S, Powers M, Sheridan J. J. Vibratory stimulation as a method of reducing pain after orthodontic appliance adjustment. J Clin Orthod. 2003;37:205–208. [PubMed] [Google Scholar]
- 42.Bartlett B. W, Firestone A. R, Vig K. W. L, Beck F. M, Marucha P. T. The influence of a structured telephone call on orthodontic pain and anxiety. Am J Orthod Dentofacial Orthop. 2005;128:435–441. doi: 10.1016/j.ajodo.2004.06.033. [DOI] [PubMed] [Google Scholar]
- 43.Hwang J. Y, Tee C. H, Huang A. T, Taft L. Effectiveness of thera-bite wafers in reducing pain. J Clin Orthod. 1994;28:291–292. [PubMed] [Google Scholar]