Abstract
Objective:
To assess the contemporary incidence of cancers using American Samoa as a learning set for insights into similar populations.
Methods:
A retrospective observational analysis of de-identified data held in public-access databases (2004–2014) and data on uterine cancer from a hospital, both in American Samoa (2015–2016).
Results:
There were 341 new cases of cancer in 2004–2014 (111 per 100 000 women/year), including breast (20.2%), uterine (19.4%), and cervical (5.0%); and 287 in 2011–2015 (103 per 100 000 women/year), including uterine (24.0%), breast (18.5%), and cervical (5.2%). Uterine cancer increased from 21.4 to 60.3 per 100 000 women/year, becoming the most common cancer in American Samoa. In 2011–2015, the incidence-rate ratio of uterine cancer to other cancers in American Samoa was 1.3-, 3.8-, 4.6-, 7.7-, and 23-fold higher than breast, colon, cervical, ovarian, and lung cancer, respectively. Among the most recent cases (n=33), median age was 55 years (10 [30.3%] <50 years), median BMI was 38.2; and 11 (33.3%) cases had grade 3 histology.
Conclusion:
The pattern of cancers in American Samoa differs from that in the US mainland. The findings reflect significant changes in cancer incidence. Cancer control programs should evaluate the potential of uterine screening in accordance with their community’s needs and characteristics.
Keywords: Non-communicable disease, Obesity, Pacific islanders, Uterine cancer, Uterine cancer screening
1 |. INTRODUCTION
Uterine corpus cancers, including endometrial cancer, are the most common gynecologic cancer in high-income countries, with 54 644 new cases and 10 096 deaths reported in 2015 in the United States.1 Unfortunately, the diets and lifestyles of high-income countries have begun to spread internationally, leading to a rise in the incidence of endometrial cancer in low-resource countries. According to the most recent Global Cancer Statistic report in 2018,2 there were 382 069 cases (2.1% of all cancers) of newly diagnosed uterine cancer and 89 929 (0.9% of all cancers) deaths worldwide, although globally cervical cancer remains the most commonly diagnosed gynecologic cancer.
Endometrial cancer is mainly diagnosed only after it has become symptomatic with abnormal vaginal bleeding. Fortunately, its frequently slow development means that it can be successfully treated in most, but not all communities owing to multiple disparities. Screening is recommended for selected high-risk women, such as those with Lynch syndrome, and is being explored for other groups.3 To our knowledge however, no screening strategy has been shown to decrease mortality from endometrial cancer as yet.
American Samoa is a small, Polynesian island territory of the United States in the South Pacific.4 It currently has an epidemic of non-communicable diseases (NCDs), including obesity, diabetes, hypertension, and metabolic syndrome, which are becoming increasingly common globally. In fact, American Samoa has the highest incidence of obesity and diabetes in the world,4 possibly due to changes in diet and level of physical activity that are potentially related to westernization.
The relationship between obesity and cancer has been studied extensively: obesity has been associated with an increased risk of at least 13 cancers, with the highest relative risk for type 1 endometrial cancer.5 Anecdotal experience and preliminary public health data suggest that the incidence of gynecologic cancers, specifically endometrial cancer, is increasing in American Samoa. Therefore, the aim of the present study was to assess the incidence of gynecologic cancers in American Samoa with the ultimate goal of using this population as a learning set to determine whether current population cancer control practices are optimally aligned with the changing burden of cancer.
2 |. MATERIALS AND METHODS
The present retrospective observational study assessed de-identified data from public-access databases on the incidence of cancers in American Samoa between January 1, 2004, and December 31, 2014, in addition to data on uterine cancer obtained from the Lyndon Baines Johnson (LBJ) Tropical Medical Center, Faga’alu, the only hospital and pathology laboratory in American Samoa, from January 1, 2015, to December 31, 2016.
The data used in the study were regularly collected as part of ongoing cancer control efforts in American Samoa. De-identified data from the publicly accessible American Samoa Department of Health (DOH) and US National Comprehensive Cancer Control Program6 databases were analyzed over several time periods. All of the data were extracted from these sources and, therefore, exempt from IRB review. Crude incidence was calculated by using the population recorded in the most contemporary census (either 2000 or 2010) as the denominator. When census database periods did not exactly coincide, imputed annualized rates were used as the denominator based on the most contemporaneously available adjacent periods by interpolating the two census results using a linear annualized incidence rate.
For comparison, data on US mainland cancer incidence were obtained from the U.S. Cancer Statistics Data Visualizations Tool,1 which includes data from both the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program and Centers for Disease Control and Prevention’s National Program of Cancer Registries. Summary data from the American Samoa DOH annual reports and other DOH publications were used to cross-check these results.
Because cancer data are typically transferred from the hospital pathology department to the cancer control programs over many years following a quality control process (e.g., diagnosis adjudication), more recent data for the present study were collected directly from the LBJ hospital and pathology laboratory. These more recent study data were collected for the most recent 24 months available (2015–2016), including the number of biopsies and the results for women with abnormal uterine bleeding. Due to travel cost limitations, most residents have initial health screening tests (e.g., for breast, colon, and cervical cancer) and diagnostic studies performed on the island, and travel to the United States or New Zealand for the necessary treatment. Therefore, all cancers diagnosed on the island of American Samoa are recorded at the LBJ facility.
Data were reported by simple statistics, including median and number (percentage) using a recent version of Excel (Microsoft, Redmond, WA, USA).
3 |. RESULTS
According to the 2000 and 2010 US censuses, there were 28 027 and 27 349 women living in American Samoa, respectively. According to the American Samoa Comprehensive Cancer Control Program, from 2004 to 2014, there were 341 new cases of cancer diagnosed among women (111 per 100 000 women/year), including 69 (20.2%) breast, 66 (19.4%) corpus uteri, and 17 (5.0%) cervical cancer cases. No cases of uterine corpus sarcomas were diagnosed.
For the most recently reported 5-year period (2011 to 2015), a total of 287 new cases were diagnosed (103 per 100 000 persons/year), including 69 (24.0%) corpus uteri, 53 (18.5%) breast, and 15 (5.2%) cervical cancer (Fig. 1). During this 5-year interval, the incidence of uterine cancer was 1.3-fold higher than breast, 3.8-fold higher than colon, 4.6-fold higher than cervical, 7.7-fold higher than ovarian, and 23-fold higher than lung cancer. By incidence, uterine cancer has been the most common cancer in American Samoa since 2011, exceeding breast, lung, and colorectal cancer, which are the three most common cancers among women in the US mainland.7
FIGURE 1.
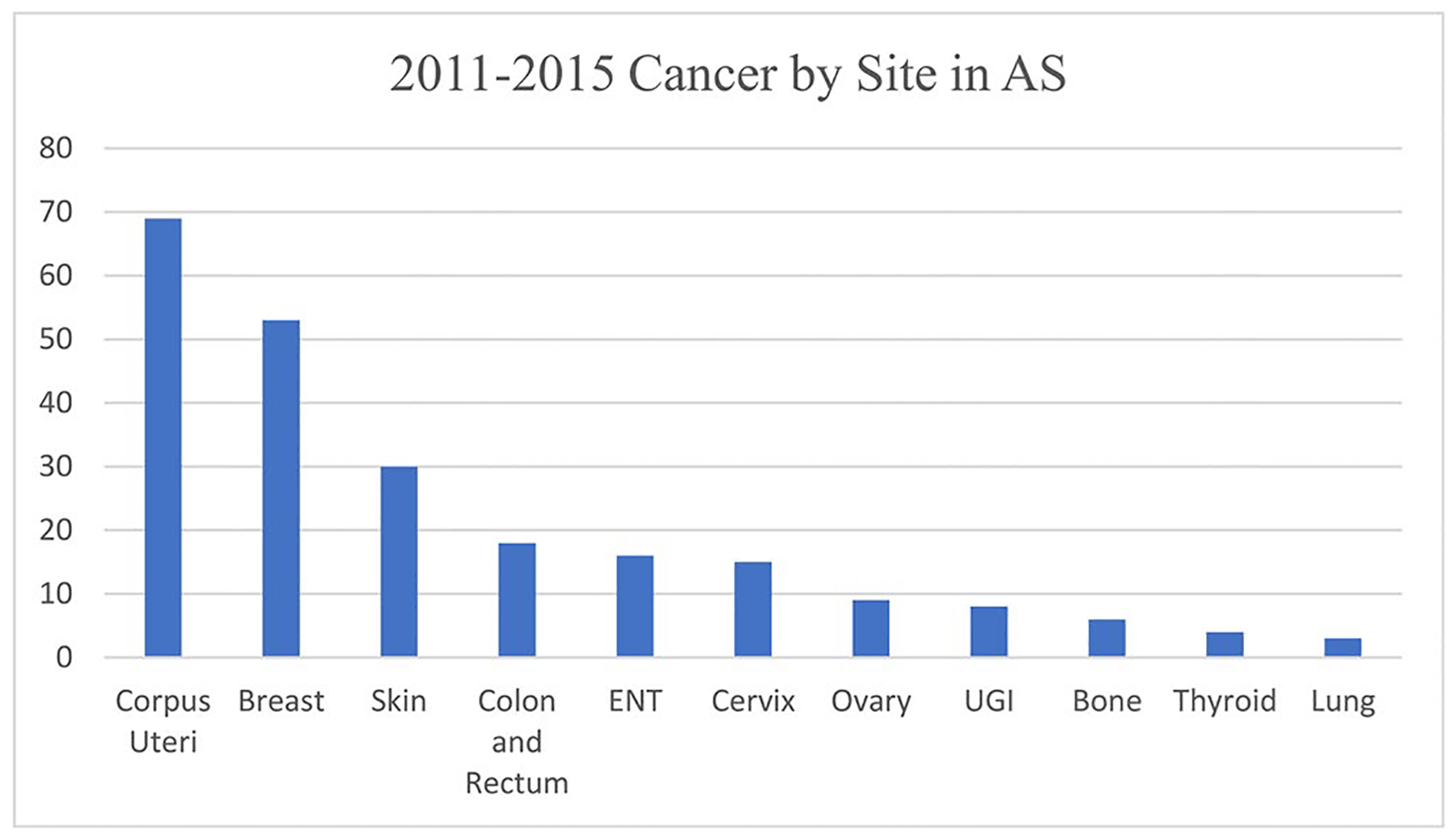
Number of cases of cancer by site of diagnosis in American Samoa, 2011–2015. Abbreviations: ENT, ear, nose, throat; UGI, upper gastrointestinal tract.
For the periods 2004–2014, 2011–2015, and 2015–2016, the annual incidence of uterine cancer increased from 21.4 to 50.5 to 60.3 per 100 000 women/year, with a respective increase of 138% and 186%. According to the SEER database, the incidence of uterine cancer in 2004, 2011, and 2016 in the United States was, respectively, 25.1, 27.2, and 27.9, and the most common cancers in women were breast, lung and bronchus, colorectal, and then uterine cancer8 (Fig. 2).
FIGURE 2.
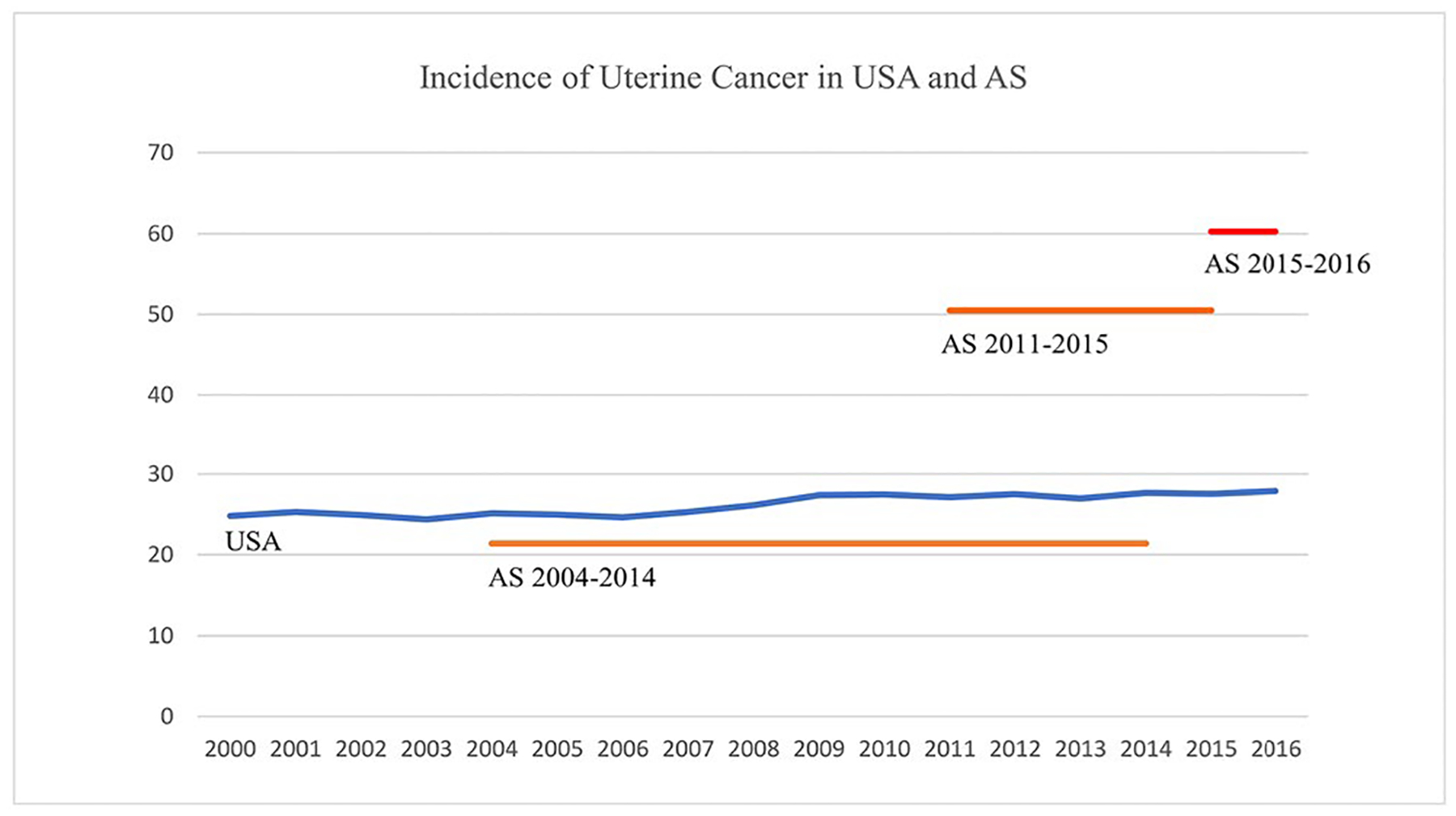
Annual number of uterine cancer cases in American Samoa and the United States.
To assess potential ascertainment or diagnostic bias, endometrial biopsies performed in American Samoa were evaluated. The LBJ pathology records indicated that, in the most recent 24 months (2015–2016), 33 cases of uterine cancers were diagnosed from 291 endometrial biopsies. The indication for all biopsies was abnormal uterine bleeding. Thus, abnormal bleeding had a positive predictive value (PPV) of 11.3% (33/291) for uterine cancer. Among the cases of uterine cancer with available data (n=33), the median age at diagnosis was 55 years, and 10 (30.3%) women were younger than 50 years at diagnosis. The median body mass index (BMI, calculated as weight in kilograms divided by the square of height in meters) at diagnosis was 38.2, and 30 (90.9%) women had a BMI above 30. The distribution of histology was grade 1 (n=17; 51.5%), grade 2 (n=5; 15.2%), and grade 3 (n=11; 33.3%).
Cancer mortality data were only available from the de-identified cancer control program database. From 2004 to 2012, the leading cause of cancer death was lung cancer, followed by gynecologic cancer, and breast cancer. Uterine cancer was the leading cause of death due to gynecologic cancer, followed by cervical and ovarian cancer (Fig. 3). Throughout this time period, ovarian cancer was the leading gynecologic cause of cancer-related death in the US mainland.
FIGURE 3.
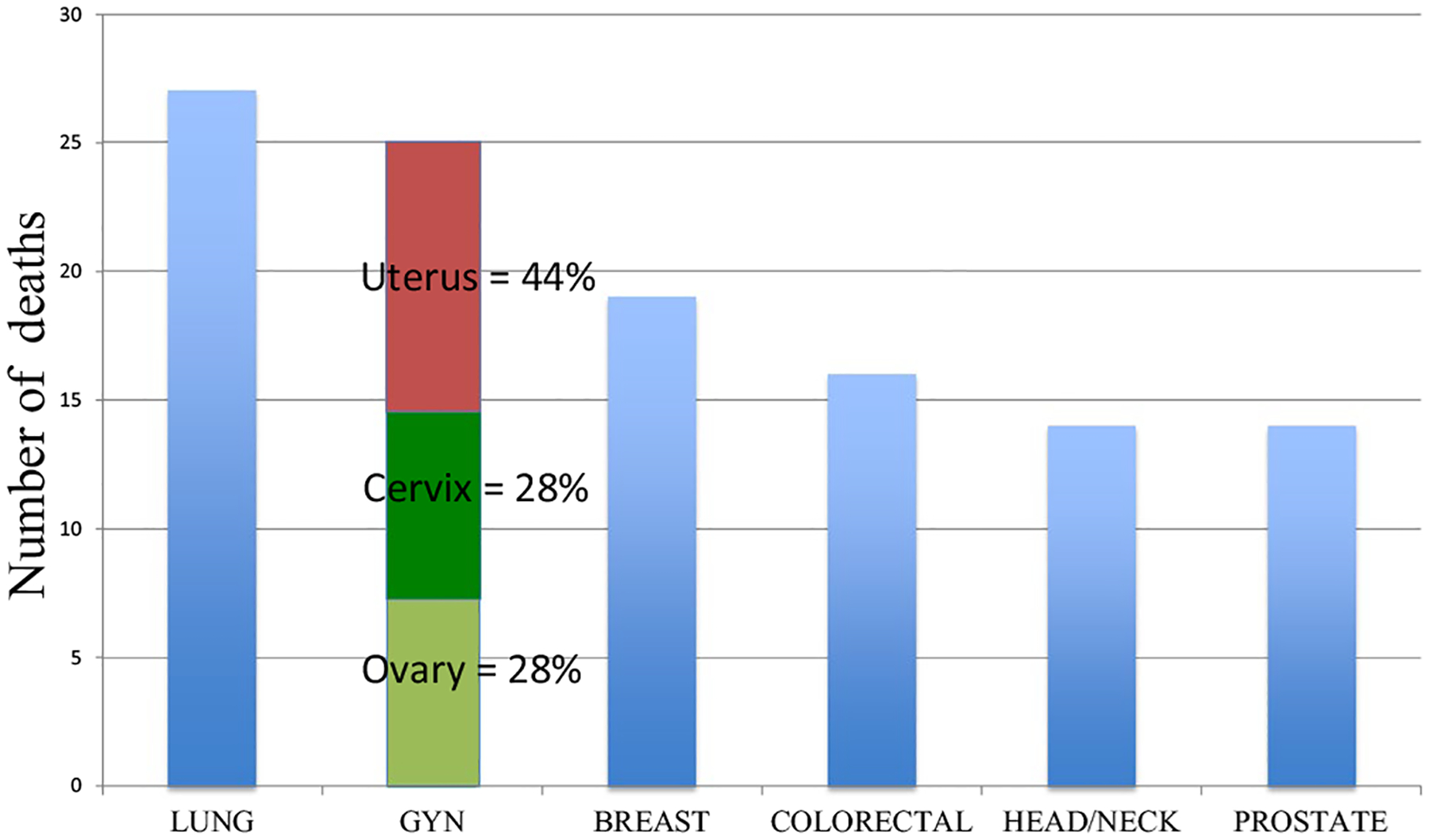
Annual number of deaths by type of cancer in American Samoa, 2004–2012.
4 |. DISCUSSION
A WHO study published in 2005 ranked American Samoa as the second most overweight country in the world, reporting that 93.5% of the adult population were overweight and 74.6% were obese.9 In 2014, the age-standardized mean BMIs were 32.2 (95% confidence interval [CI], 30.5–33.7) for men and 34.8 (95% CI, 33.2–36.3) for women.10,11 In addition, the reported prevalence of severe obesity and morbid obesity was 33.4% and more than 15%, respectively, among women in American Samoa. At the same time, the age-standardized prevalence of adult diabetes was 31% (95% CI, 19–44) among men and 33% (95% CI, 21–47) among women.
As the local traditional diet has been replaced by a more westernized diet, NCDs have become the main cause of premature illness and death on this Pacific Island. Although not proven, the etiology of this trend is possibly due to the associated epidemic of NCDs, specifically obesity, which may be a result of westernized lifestyle changes in American Samoa.4,9–11 The present study has now documented changes in cancer trends that may also be related.
On the basis of limited data sources from differing time periods, the recent and trending profile of cancer in American Samoa seems to consistently indicate that uterine cancer is increasing in incidence and has become the most common cancer in the population, even when men are included. This increasing incidence has clinical, social, and political implications that should elicit a response from leadership in these areas. The increasing incidence is accompanied by a lower median age (55 years in American Samoa vs 62 years in the US mainland) and a higher average grade of disease as compared with cases typically seen in consensus data from the US mainland.7
The characteristics of cancer in the United States may be changing similarly on the basis of worsening NCD rates throughout the country. As a result, cancer control programs should evaluate the needs of their populations, including the potential of population-based uterine cancer screening, in accordance with the specific characteristics of the communities. Screening for endometrial cancer was briefly considered when the program to prevent breast cancer using selective estrogen receptor modulators (SERMs) was initiated, owing to the association of this class of medication with endometrial cancer.12 However, because of the poor PPV of sonography and the relatively low prevalence of endometrial cancer, screening was abandoned during that time.
Even with the current rise of NCDs in the US mainland, the prevalence of uterine cancer in the general population is still perceived to be less than the prevalence of breast cancer among women on SERMs.13,14 However, in some populations, as demonstrated here for American Samoa, the incidence of uterine cancer may exceed that of breast cancer.14,15 Although it is not higher than breast cancer in the general US mainland population, the prevalence of uterine cancer in American Samoa is similar to that of other cancers that generally have screening programs (e.g., breast, colon, prostate, and cervical cancer). Relative incidence is not the only metric for determining the appropriateness of screening, but it is useful for evaluating the need for a screening program relative to other traditional screening strategies.
To explore the possibility of a diagnostic bias, the number of biopsies done for women with abnormal uterine bleeding was used to determine the PPV for uterine cancer. The finding was consistent with a previous study16; thus, the increase in uterine cancers is not likely to be due to a diagnostic or ascertainment bias. In addition, the histology of the biopsies was not weighted toward hyperplasia or other premalignant diagnoses, making it less likely that the change in incidence is due to ascertainment bias.
In American Samoa, data on cancer are typically transferred from the LBJ pathology department to the databases and cancer control programs used in the present analysis. Because this process takes years to be completed, additional data for the most recent 24 months were taken directly from the LBJ Tropical Medical Center. However, this might have introduced differences, such as lack of adjudication, making the inclusion of the hospital data subject to different biases relative to the cancer control data. This potential bias was addressed by assessing the characteristics of the cases of uterine cancer. The number of biopsies done, the PPV, and other parameters were close too expected values, suggesting that the recent data from the hospital are concordant with those from the other databases used in this report.
In addition to its rising incidence, uterine cancer has other characteristics that may support effective screening. First, it has a long preclinical and localized disease state that can result in high rates of successful treatment for screen-detected cancers. Second, it is not thought to be susceptible to the lead-time bias and over-treatment that currently overshadows the benefits of breast and prostate cancer screening. Third, the present finding of a median age of diagnosis 8 years younger in American Samoa than in the US mainland population suggests that treatment may be less morbid than it would be if diagnosed in an older cohort with more co-morbidities and potentially increasing BMI. Overall, uterine cancer has characteristics that may make it amenable to prevention strategies tailored to the specific needs of a community.
Screening frequency must be optimized prospectively, however uterine cancer is unlikely to require yearly testing and may parallel colon cancer screening intervals (e.g. 5 years or more). Screening modality must also be confirmed prospectively, but due to the poor PPV of sonography, endometrial sampling of some kind is likely to play a role. Currently, there are highly sensitive and specific potential screening methods for detection that may be effective in reducing mortality.14–18 In the future, newer methods may displace endometrial histologic sampling as their costs rapidly decrease.19
The present study has methodologic limitations. First, it is possible that some residents travelled and had cancer diagnosed in a facility outside American Samoa. Such cases would lead to underestimation of the incidence of uterine cancer or other cancers among the population, and would strengthen the present conclusions. Second, there was a relatively short period of observation (2004–2016), a relatively small population (28 027 women), and a relatively small absolute number of uterine cancer diagnoses (99 cases). However, the direction of the associations was consistent regardless of whether the data were grouped by time or denominator, and therefore should be useful to raise other hypotheses. Similarly, a sensitivity analysis that varied the years used for comparisons did not alter the result. For example, the evaluated time periods were varied by 1-year, 2-year, and 5-year intervals and results recalculated, with no difference in the direction of the changes or trends. In addition, alternative methods for calculating results, such as varying the census data denominator, did not alter the direction of the results, regardless of which year of census data was used. Therefore, the data were presented in their original format as contained in the databases for greater transparency. A strength of the study is the relatively stable population, which experienced an average annual decline of 0.24% over the study period.
The present observations should be confirmed, either by studying the American Samoa population for a longer period or by studying similar populations with more rigorous techniques for as long as possible. Nevertheless, the present report of a notable change in traditional cancer burden should spur efforts from all stakeholders to evaluate current practices and optimize population health for their specific international communities. High-income countries may already be experiencing the rise of uterine cancer and its consequences.14,15
ACKNOWLEDGMENTS
The authors thank the following for assistance with the study: American Samoa Department of Health, Lyndon B. Johnson Tropical Medical Center, Departments of Obstetrics and Gynecology and Pathology, and American Samoa Cancer Control Program. Gianluca Del Priore, NYGO, New York, NY created the figures.
Footnotes
CONFLICTS OF INTEREST
The authors have no conflicts of interest.
REFERENCES
- 1.U.S. Cancer Statistics Working Group. U.S. Cancer Statistics Data Visualizations Tool, based on November 2017 submission data (1999–2015). www.cdc.gov/cancer/dataviz. Accessed May 12, 2019.
- 2.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. [DOI] [PubMed] [Google Scholar]
- 3.Hereditary colorectal (colon) cancer. https://www.cdc.gov/genomics/disease/colorectal_cancer/medical_options.htm. Accessed June 9, 2019.
- 4.The World Factbook. https://www.cia.gov/library/publications/the-world-factbook/geos/aq.html. Accessed May 11, 2019.
- 5.Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K. Body Fatness and Cancer-Viewpoint of the IARC Working Group. N Engl J Med. 2016;375:794–798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Comprehensive Cancer Control Program: Comprehensive Cancer Control Plans – U.S. Territories/Pacific Island Jurisdictions. https://www.cdc.gov/cancer/ncccp/ccc_plans.htm. Accessed May 12, 2019.
- 7.Cancer Stat Facts: Common Cancer Sites. https://seer.cancer.gov/statfacts/html/common.html. Accessed May 11, 2019.
- 8.Table 7.5 Cancer of the Corpus and Uterus, NOS(Invasive). https://seer.cancer.gov/csr/1975_2016/browse_csr.php?sectionSEL=7&pageSEL=sect_07_table.05. Accessed May 11, 2019.
- 9.American Samoa NCD Risk Factors: STEPS Report. 2007. http://www.who.int/chp/steps/Printed_STEPS_Report_American_Samoa.pdf. Accessed May 12, 2017.
- 10.Noncommunicable Disease Risk Factor Collaboration. Worldwide trends in diabetes since 1980: A pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016;387:1513–1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Noncommunicable Disease Risk Factor Collaboration. Trends in adult body-mass index in 200 countries from 1975 to 2014: A pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet. 2016;387:1377–1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nahari C, Tepper R, Beyth Y, Flex D, Figer A, Cohen I. Long-term transvaginal ultrasonographic endometrial follow-up in postmenopausal breast cancer patients with tamoxifen treatment. Gynecol Oncol. 1999;74:222–226. [DOI] [PubMed] [Google Scholar]
- 13.Wickerham DL, Fisher B, Wolmark N, et al. Association of tamoxifen and uterine sarcoma. J Clin Oncol. 2002;20:2758–2760. [DOI] [PubMed] [Google Scholar]
- 14.Mullins MA, Cote ML. Beyond obesity: The rising incidence and mortality rates of uterine corpus cancer. J Clin Oncol. 2019;37:1851–1853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Del Priore G, Matthews R. Will screening for endometrial cancer soon be routine? Contemp Ob/Gyn. 2019;64:21–24. [Google Scholar]
- 16.Del Priore G, Williams R, Harbatkin CB, Wan LS, Mittal K, Yang GC. Endometrial brush biopsy for the diagnosis of endometrial cancer. J Reprod Med. 2001;46:439–443. [PubMed] [Google Scholar]
- 17.de Leon MC, Wu HH, Lennon AE, Del Priore G. Novel approach to outpatient endometrial biopsy to detect endometrial cancer. J Reprod Med. 2016;61:243–248. [PubMed] [Google Scholar]
- 18.Sierecki AR, Gudipudi DK, Montemarano N, Del Priore G. Comparison of endometrial aspiration biopsy techniques: Specimen adequacy. J Reprod Med. 2008;53:760–764. [PubMed] [Google Scholar]
- 19.Nair N, Camacho-Vanegas O, Rykunov D, et al. Genomic analysis of uterine lavage fluid detects early endometrial cancers and reveals a prevalent landscape of driver mutations in women without histopathologic evidence of cancer: A prospective cross-sectional study. PLoS Med. 2016;13:e1002206. [DOI] [PMC free article] [PubMed] [Google Scholar]


