Abstract
Background
Globally, hypertension is a major public health problem and a strong predictor of cardiovascular disease complications. To reduce and prevent complications from hypertension, it is important to adapt self-care behaviors. This study aimed to assess the self-care practices of adult hypertensive patients at a tertiary teaching hospital in Ethiopia.
Methods
A health facility-based prospective cross-sectional study was conducted at Jimma Medical Center in Ethiopia between February 2021 and July 2021. Binary and logistic regression was performed to assess the strength of associations between independent and dependent variables. Data entry and analysis were done using Statistical Package for social science (SPSS) software version 22.0. A p-value < 0.05 was considered to declare statistical significance.
Results
From a total of 422 respondents included to the study, male accounted 55.7% and the mean ± SD age of the respondents was 58.7 ± 9.75 years. About 53.1% of patients had poor self-care practices toward hypertension. Not attending formal education [AOR = 2.15; 95% CI (1.74, 6.39); p ≤ 0.001], uncontrolled blood pressure [AOR = 2.14 95% CI (1.27, 3.61); p = 0.003], chronic disease co-morbidity [AOR = 1.48; 95% CI (0.25, 7.73); p ≤ 0.001], unfavorable attitude toward hypertension[AOR = 3.13; 95% CI (1.95, 7.52); p ≤ 0.001], and poor social support [AOR = 2.75; 95% CI (1.45, 6.43); p ≤ 0.001] were independent predictors of poor self-care practice.
Conclusion
The level of self-care practices for hypertension in the study area was low. In particular, the level of adherence to the DASH diet, exercise, and weight control was very low. Patient-specific targeted interventions are required to improve self-care practices for hypertension.
Keywords: Blood pressure control, Hypertension, Self-care practice, Self-efficacy
Background
Hypertension (HTN) is a growing problem affecting approximately one billion people worldwide, two-thirds of them in low-income countries [1]. Alarmingly, 1.56 billion adults are estimated to have HTN in 2025 [1, 2]. HTN is a leading risk factor for cardiovascular disease (CVD) for stroke, myocardial infarction, congestive heart failure, decline, and death [1, 3, 4]. HTN is a major risk factor for CVD, causing 45% of cardiovascular morbidity and mortality worldwide [2]. In most cases, this condition remains asymptomatic until followed by a stroke, myocardial infarction, kidney failure, or vision problems [1, 5, 6].
In Ethiopia, hypertension is the most common non-communicable disease (NCD) with a prevalence rate of 19.6% [7, 8]. Uncontrolled high blood pressure can lead to heart attack and eventually heart failure and stroke, kidney failure, blindness, blood vessel rupture, and cognitive impairment [9]. HTN complications are estimated to cause about 9.4 million deaths each year, representing 17% of all deaths worldwide [10, 11]. The main cause of poor control of HTN is the inability to comply with HTN’s self-care practice [12, 13]. Self-care practices have been an important and cost-effective tool in the management and prevention of hypertension and its complications. Self-care of hypertension includes adherence to medication, intake of a low-fat diet, daily exercise, restriction of alcohol intake, smoking cessation, weight loss, self-monitoring of blood pressure (BP), regular health checkups, and reducing stress [14, 15].
Lifestyle changes, formerly known as non-drug therapies, play an important role in people with and without hypertension. It may serve as an early intervention before initiating medication in people with high blood pressure and maybe an adjunct to medication for those already on medication [16, 17]. Lifestyle changes can lower systolic blood pressure by about 4–11 mmHg. It is also estimated that for every 1 kg weight loss, blood pressure decreases by 1 mmHg [9, 17].
Although high blood pressure can be modified and treated, there is little knowledge about the treatment of hypertension in developing countries. In developing countries, more than three fourth of the burden of hypertension is attributable to a lack of knowledge and inadequate practice of self-care measures [10, 18, 19]. In previous studies conducted in Ethiopia, the prevalence of inadequate self-care practices reaches 77% [20, 21], which is very high as compared to the World Health Organization (WHO) recommendation.
Several factors have been associated with adherence to self-care activities, including socio-economic status, age, gender, educational status, place of residence, co-morbidity, access to health care, level of health literacy, length of therapy, culture, social support, self-efficacy, source of information on self-care and knowledge of disease and treatment [22–26].
Adhering to self-management practices in hypertension is essential for patient management to achieve desired treatment goals by improving quality of life, preventing complications, and reducing health care costs, but self-care practices remain low in developing countries [26–28]. Measuring the level of self-care activity for hypertension, along with determinants, is important for establishing a successful strategy for the treatment of hypertension. The literature recommends different self-care practice evaluation methods. One of the validated assessment scales routinely used is Hypertension Self-Care Activity Level Effects (H-SCALE) [29]. It addresses most of the self-care behaviors of the patients which are expected to affect glycemic control. There are studies in Ethiopia on HTN self-care practices. However, the level of hypertension self-care practices and contributing factors have not been well studied in the southwestern part of Ethiopia. Therefore, the study aimed to evaluate the self-care practices of adult hypertensive patients in an outpatient clinic of a tertiary teaching Hospital in Ethiopia.
Methods
Study setting
The current project was conducted at Jimma Medical Center in Ethiopia. Jimma Medical Center (JMC) is one of the oldest public hospitals in the country. Geographically, it is located in Jimma city 352 km southwest of Addis Ababa, the capital. With a bed size of 800, JMC is the only teaching and tertiary hospital in the southwestern part of the country. It provides services for approximately 15,000 inpatients, 160,000 outpatient attendants, 11,000 emergency cases, and 4500 deliveries per year coming to the hospital from the catchment population of about 20 million people. The medical center has over 1500 health workers. Besides serving as a referral center, the hospital serves as a teaching and research center for several health professionals at the undergraduate and postgraduate levels. The hospital has different general departments and specialty units like surgery, pediatrics and child health, internal medicine, oncology, gynecology-obstetrics, ophthalmology, dentistry, and other subspecialty clinics. The hospital provides screening and treatment services for people living with chronic disease at different specific ambulatory clinics.
Study design and period
A hospital-based cross-sectional study was conducted from February 2021 to July 2021.
Study population
The study population for the current study was all adult hypertensive patients on follow-up at the ambulatory clinic of JMC during the study period and fulfills the inclusion criteria.
Inclusion and exclusion criteria
All adult hypertensive patients aged 18 years and above on follow-up for greater than 3 months were included in the study. We excluded patients who were seriously ill and unable to respond to interviews during the data collection period.
Sample size determination and sampling procedure
The sample size was determined using a single population proportion formula based on the following assumptions: considering 95% of confidence level, 5% margin of error, and 51% prevalence of poor self-care practice [30]. A minimum sample size was 384. Considering a 10% non-response rate, we recruited a total of 422 study participants consecutively over the study period. Participants were selected using a simple random sampling technique.
Data collection tools and methods
Pretested structured questionnaires adapted from validated scales, published articles [30–34], and modified to the context of the study were used to collect data from participants. The tool contains socio-demographic information, clinical profile of patient, Self-efficacy measure, Social support, self-care practices, knowledge and attitude related information, and questions. Data were collected by the interviewer-administered questionnaire. Data were collected by three trained nurses with a Bachelor of Science degree. Blood pressure was considered when an average systolic BP > 130 and diastolic BP > 80 mmHg for at least three consecutive follow-up appointments in patients younger than 60 years old [35].
Outcome measures and validating methods
| A | Self-efficacy | The patient’s self-efficacy is confidence in his or her ability to perform tasks. It is drawn from a five-item scale. Feedback options range from 0 (completely not confident) to 5 (completely confident). Respondents who scored 4 or higher were classified as having good self-efficacy, and if they scored below 4, it was considered poor self-efficacy [34] |
| B | Social support | Social support is when the patient has friends and others, including family, present in times of need or crisis to give them a bigger picture and a positive image of themselves. The Multidimensional Perceived Social Support Scale (MSPSS) was used to measure social support. The MSPSS is a 12-item measure that rates the adequacy of social support on a 7-point Likert-type scale ranging from 1 = strongly disagree to 7 = strongly agree. Total score from 12 to 84; with scores higher and equal to 64 indicates better (good) social support [36] |
| C | Self-care practice | Self-care practice was assessed using the impact of hypertension-related self-care activity level [29]. The H-SCALE is a self-report questionnaire that includes six categories of self-care behaviors, which include medication adherence, a low-salt diet, physical activity, smoking cessation, weight management, and abstinence from alcohol. Good self-care practices are considered when the patient scores average or higher on the H-SCALE questions |
| D | Medication adherence | Three items were used to evaluate adherence to the prescribed medication. Then add the answer to each item with a score range of 0 to 21. Participants scoring 21 points are considered adherent [37] |
| E | Blood pressure (BP) monitoring | Good blood pressure monitoring was considered when BP was measured one time per month and more than once per month for uncontrolled BP [38] |
| F | Diet quality | Diet quality was assessed based on the 11-item Dietary Approach to Stop Hypertension Quality (DASH-Q) scale. These factors allow us to evaluate healthy food intake related to the nutritional content of the DASH diet. Responses were summarized and ranged from 0 to 77. A score of fewer than 32 was considered poor diet quality. A score of 33–51 corresponds to the average quality of the diet and a score of 52 or higher corresponds to good diet quality [39] |
| G | Physical activity | Physical activity was assessed on two items and summarized responses on ranges from 0 to 14 score. Participants with a score of 8 or higher were considered to comply with the physical activity recommendations [40, 41] |
| H | Weight management | The patient’s weight management over the past 30 days was rated on a 10-item scale. Response categories range from strongly disagree [1] to strongly agree [5]. Summarize the responses to calculate a score in the 10–50 range. Participants reporting a score of 40 or higher were considered adherent to good weight management practices [33, 42] |
| I | Alcohol intake | The amount of alcohol consumed was evaluated on a 3-item scale. The participant who stated that they did not drink alcohol at all in the last 7 days, or generally did not drink alcohol at all, are considered abstainers [43] |
| J | Knowledge | Hypertension evaluation of lifestyle and management (HELM) scale was used to assess the knowledge of respondents. If a participant answers above the median knowledge question, it is considered “knowledgeable” or good knowledge [32] |
| K | Attitude | A “favorable attitude” is considered when a patient answers a question about attitude with an average or higher score |
Data processing and analysis
Data were entered into epi info and exported to the Statistical Package for Social Science (SPSS) version 22.0 for analysis. Descriptive statistics were used for the analysis of patient characteristics. Chi-square tests and logistic regression analysis were done to determine the presence of a statistically significant association between explanatory variables and the outcome variable. Factors associated with self-care practices were identified using bivariate and multivariable logistic regression analysis. Before analysis factors such as independence of errors, linearity in the logit for continuous variables, multicollinearity, and outliers were checked. Odds Ratio (OR), p-value, and their 95% Confidence Intervals (CI) were calculated, and the result was considered statistically significant at p < 0.05.
Data quality management
The quality of the data was ensured through the development of appropriate data collection materials. Two-day training on study objectives, data retrieval, and the collection was given for the data collectors. Overall activity was monitored by the study's lead investigator.
Ethical considerations
Ethical clearance was collected from the institutional review board of the institute of health, Jimma University. A permission and support letter were also obtained from the management committee of the hospital. Patients signed an informed consent form to participate in the study. The raw data were not made available to anyone and were not used as the determinant of the subjects. All steps in data collection and compilation were conducted and supervised by the principal investigator. Strict confidentiality was assured through anonymous recording and coding of questionnaires and placed in a safe place.
Results
Socio-demographic characteristics of participants
From a total of 422 respondents included in the study, males accounted for 55.7% and the mean ± SD age of the respondents was 58.7 ± 9.75 years. Nearly one-third (65.9%) of the respondents were married. About 33.9% of respondents had no formal education and 63% of the participants reside in an urban area. One-fifth of the participants had no regular income. About 278 (65.9%) of patients live with immediate family (Table 1).
Table 1.
Socio-demographic characteristics of study participants at follow-up clinic
| Variable | Category | Frequency | Percent |
|---|---|---|---|
| Age (years) | Mean ± SD | 58.7 ± 9.75 | |
| 18–35 | 30 | 7.1 | |
| 36–50 | 271 | 64.2 | |
| > 51 | 121 | 28.7 | |
| Gender | Male | 235 | 55.7 |
| Female | 187 | 44.3 | |
| Educational status | Unable to read and write | 143 | 33.9 |
| Primary school | 119 | 28.2 | |
| Secondary school | 96 | 22.7 | |
| College and above | 64 | 15.2 | |
| Marital status | Single | 42 | 10 |
| Married | 278 | 65.9 | |
| Divorced | 31 | 7.3 | |
| Widowed | 71 | 16.8 | |
| Occupation | Gov’t/non-gov’t employee | 89 | 21.1 |
| Self-employee | 224 | 53.1 | |
| Unemployed | 109 | 25.8 | |
| Residence | Urban | 266 | 63.0 |
| Rural | 156 | 37.0 | |
| Average monthly Income (ETB) | No regular income | 109 | 25.8 |
| ≤ 3000 | 191 | 45.3 | |
| > 3000 | 122 | 28.9 | |
| Living status | Living with immediate family | 278 | 65.9 |
| Living with extended family | 115 | 27.2 | |
| Living alone | 29 | 6.9 | |
ETB Ethiopian Birr
Clinical characteristics of participants
From the total of the included participants, more than one-fifth (26.8%) of them had had a family history of hypertension. About, 48.1% of participants had BMI above the recommended weight. About 249 (59%) of participants had uncontrolled hypertension. Nearly one-fifth (31.5%) of participants had chronic disease co-morbidity. About 114 (27%) of respondents missed their follow-up schedule (Table 2).
Table 2.
Clinical characteristics of study participants at follow-up clinic
| Variables | Category | Frequency | Percent |
|---|---|---|---|
| Family history of hypertension | Yes | 113 | 26.8 |
| No | 309 | 73.2 | |
| Body mass index | Underweight(< 18) | 26 | 6.2 |
| Normal (18–24.99) | 193 | 45.7 | |
| Overweight (25–29.99) | 173 | 41.0 | |
| Obese(> 30) | 30 | 7.1 | |
| Follow-up schedules | Every 2 weeks | 16 | 3.8 |
| Every month | 217 | 51.4 | |
| Every 2 months | 182 | 43.1 | |
| Every 3 months | 7 | 1.7 | |
| Blood pressure control status | Uncontrolled | 249 | 59 |
| Controlled | 173 | 41 | |
| Chronic disease co-morbidity | Yes | 133 | 31.5 |
| No | 289 | 68.5 | |
| Disease duration since diagnosis (years) | < 3 | 105 | 24.9 |
| 3–5 | 101 | 23.9 | |
| > 5 | 216 | 51.2 | |
| Treatment duration since diagnosis(years) | < 5 | 206 | 48.8 |
| ≥ 5 | 216 | 51.2 | |
| Adherence to the follow-up schedule | Yes | 308 | 73 |
| No** | 114 | 27 |
**Missed at least one follow-up schedule within the last 3 months
Therapeutic life change and self-care practice-related information
Of a total of included patients, 245 (58.1%) of them had good knowledge about self-care practice of hypertension. The majority (85.8%) of patients got information about self-care practice from a health care professional. About 282 (58.8%) of the participants had good knowledge about HTN self-care practice and 243 (50.6%) of the participants had a favorable attitude towards HTN self-care practice. More than half (51.9%) of participants had good social support and 259 (61.4%) had poor self-efficacy (Table 3).
Table 3.
Therapeutic life change and self-care practice-related information of study participants at follow-up clinic
| Variable | Category | Frequency | Percent |
|---|---|---|---|
| Knowledge towards self-care practice of hypertension | Good | 245 | 58.1 |
| Poor | 177 | 41.9 | |
| Source of information about self-care practice | Health care professional | 363 | 85.8 |
| Relatives and friends | 31 | 7.3 | |
| Media | 15 | 3.6 | |
| Attitude towards hypertension and self-care practice | Favorable | 224 | 53.1 |
| Unfavorable | 198 | 46.9 | |
| Self-efficacy | Good | 259 | 61.4 |
| Poor | 163 | 38.6 | |
| Social support | Good | 219 | 51.9 |
| Poor | 203 | 48.1 |
Level of hypertension self-care practices
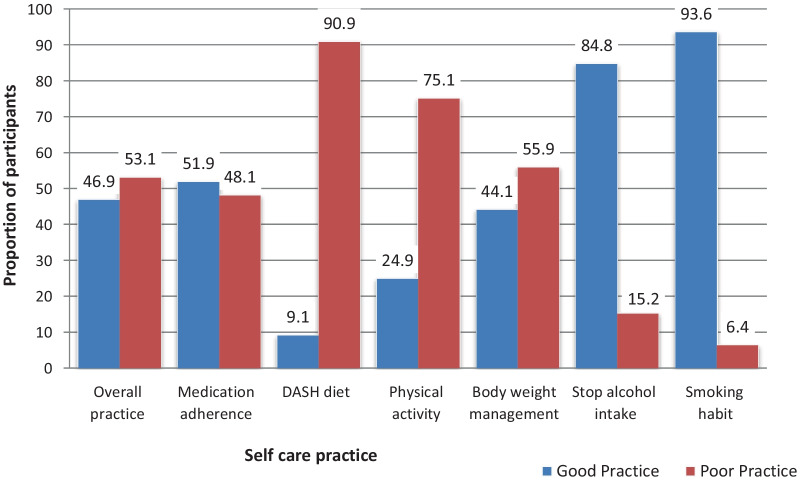
The median score for self-care practice was 77 with a maximum score of 131. Out of the total respondents, 224 (53.1%) patients had overall poor self-care practice with 95% CI (49.37%, 57.13%). The median score for adherence to the prescribed medication was 19 with a maximum score of 21. About 203 (48.1%) of patients poorly adhered to their antihypertensive. The median score for dietary approach for stopping hypertension (DASH) practice was 17 with a maximum score of 55. Most of the participants 329 (78%) practiced low diet quality, 53 (12.6%) practiced medium diet quality and 40 (9.4%) practiced good diet quality. The median score for physical activity engagement was 6 with a maximum score of 12. About 317 (75.1%) respondents’ had a poor practice of the recommended physical activity. The median score for weight management practice among the participants was 36 with a maximum score of 48. More than half of respondents 236 (55.9%) had poor weight management practice. Few numbers 27 (6.4%) of participants were current smokers and 64 (15.2%) were alcoholics (Fig. 1).
Fig. 1.
Level of self-care practice among study participants at follow-up clinic
Factors associated with self-care practice
Bivariate analysis showed statistically significant associations between educational level, blood pressure control, disease co-morbidity, attitude to hypertension, adherence to follow-up schedule, and social support of the respondents. On multivariable logistic regression analysis revealed lack of formal education, disease co-morbidity, uncontrolled blood pressure, unfavorable attitude to hypertension, poor adherence to following up schedule, and poor social support were determinants for self-care practices. Patients who cannot read and write were two times more likely to practice poor self-care [AOR = 2.15; 95% CI (1.74,6.39); p ≤ 0.001] as compared to those who attended tertiary and above education. Hypertensive patients with uncontrolled BP were two times more likely to practice poor self-care [AOR = 2.14 95% CI (1.27, 3.61); p = 0.003] as compared to those who had controlled blood pressure. The probability of poor self-care was 1.48 times more likely among patients who had disease co-morbidity [AOR = 1.48; 95% CI (0.25, 7.73); p ≤ 0.001] as compared to those with no co-morbidity. Patients who had unfavorable attitudes were three times more likely to practice poor self-care [AOR = 3.13; 95% CI (1.95, 7.52); p ≤ 0.001] as compared to those patients with a favorable attitude. Additionally, hypertensive patients with poor social support were almost three times more likely to practice poor self-care practice [AOR = 2.75; 95% CI (1.45, 6.43); p ≤ 0.001] as compared to patients with good social support (Table 4).
Table 4.
Factors associated with self-care practice of study participants at follow-up clinic
| Variables | Self-care practice | COR (95% CI) | AOR (95% CI) | p-value | ||
|---|---|---|---|---|---|---|
| Poor (n) | Good (n) | |||||
| Age (years) | 18–35 | 12 | 18 | 1.00 | 1.00 | |
| 36–50 | 141 | 130 | 1.85 (0.87, 7.68)* | 1.34 (0.209, 3.33) | 0.119 | |
| > 51 | 71 | 50 | 1.25 (0.17, 5.22)* | 1.07 (0.22, 8.31) | 0.214 | |
| Gender | Male | 123 | 112 | 1.00 | ||
| Female | 101 | 86 | 0.85 (0.41–10.46) | |||
| Educational status | Unable to read and write | 97 | 46 | 2.18 (0.73,13.38)** | 2.15 (1.74, 6.39) | < 0.001 |
| Primary school | 69 | 50 | 1.53 (0.92, 7.49)* | 1.56 (0.81, 4.27) | 0.136 | |
| Secondary school | 31 | 65 | 2.61 (1.15, 5. 85)* | 1.24 (0.67, 5.21) | 0.218 | |
| College and above | 27 | 37 | 1.00 | 1.00 | ||
| Residence | Urban | 131 | 135 | 1.00 | ||
| Rural | 93 | 63 | 1.62 (0.48–7.35) | |||
| Occupation | Gov’t/non-gov’t employee | 41 | 46 | 1.00 | ||
| Self-employee | 113 | 111 | 0.47 (0.25–2.43) | |||
| Unemployed | 70 | 39 | 1.31 (0.96–3.44) | |||
| Living status | Living with immediate family | 150 | 128 | 1.00 | ||
| Living with extended family | 65 | 50 | 0.94 (0.52–4.18) | |||
| Living alone | 9 | 20 | 1.23 (0.70–3.91) | |||
| Blood pressure control | Uncontrolled | 107 | 66 | 4.26 (2.55, 11.34)** | 2.14 (1.27, 3.61) | 0.003 |
| Controlled | 117 | 132 | 1.00 | 1.00 | ||
| Co-morbidity status | Yes | 79 | 54 | 1.35 (0.43, 5. 83)** | 1.48 (0.25, 7.73) | < 0.001 |
| No | 145 | 144 | 1.00 | 1.00 | ||
| Adherence to follow-up | Yes | 152 | 156 | 1.00 | 1.00 | |
| No | 72 | 42 | 2.73 (0.98, 8.32)** | 0.89(0.327,2.71) | 0.067 | |
| Attitude to hypertension | Unfavorable | 117 | 81 | 3.67 (2.26, 10. 98)** | 3.13(1.95,7.52) | < 0.001 |
| Favorable | 107 | 117 | 1.00 | 1.00 | ||
| Social support | Poor | 121 | 82 | 3.17 (2.08, 11. 65)** | 2.75 (1.45, 6.43) | < 0.001 |
| Good | 103 | 116 | 1.00 | 1.00 | ||
**p-value < 0.05; *p value < 0.25
Discussion
Self-management is an important non-pharmacological approach that facilitates blood pressure control. It is essential for the prevention and treatment of hypertension [44]. This study aimed to determine the level of self-care in hypertensive patients in relation to antihypertensive drug compliance and therapeutic lifestyle changes. The overall level of self-care practice in this study was 53.1% (49.37%, 57.13%). This is consistent with a study in Nigeria [45] (47.4%) and a previous study conducted in a research setting [46] (55.3%). However, the result of this study was lower than the results of studies conducted in Addis Ababa [20] (77%), Durame [27] (72.7%), and MizanTepi [47]. Meanwhile, the result of this study was higher than those of studies conducted not only in Iran [48] (27%), but also in Harar [49] (37.9%) and Nekemte [50] (31.1%). These discrepancies may relate to differences in the population's lifestyle, cultural, economic situation, access to health care facilities, and educational attainment.
In this study, the rate of using a low-quality diet was 78% (69.66%, 84.47%). This result is higher than studies conducted in Durame [27], (42.5%) [27], Harar [49], (18.2%) [43], Saudi Arabia [45] (20.7%) [45] and Uganda [51] (24.4%). This may be due to differences in dietary perceptions on dietary management by region and country. In addition, differences in measurement tools, socio-economic and socio-cultural values may cause fluctuations in results.
In this study, non-adherence to physical activity was 75.1% (68.77%, 88.90%). This is consistent with a study done in Durame [27] (83.9%) and Saudi [52] (76.8%). However, this result was higher than the studies conducted in Addis Ababa [12, 53] (50.6% -68.6%) This may be due to limited facilities or the lack of a structural framework for exercise around the workplace as well as for the general public in the study area. In addition, patients' perceptions and attitudes toward physical activity may limit its practice.
The smoking rate in this study was 6.4%. This finding was lower than other studies done in Ethiopia [27, 49], India [54], Kenya [55] Nigeria [56, 57], Canada [58], Korea [59], and Iran [60]. In addition, the prevalence of alcohol use in this study was 15.2%. This was in line with other studies in Ethiopia [25, 27], Ghana [61], Kenya [55]. However, this result was much lower than studies conducted in other regions of Nigeria [56, 57] and Korea [59]. Differences in survey results may be related to differences in socio-cultural and religious viewpoints. Smoking and drinking within the community are not encouraged in this area of study.
Educational level showed a statistically significant relationship with self-management practice. Patients who cannot read and write were twice more likely to have poor self-care than patients with higher education. This was in line with the other studies done in Ethiopia [27, 62]. This may be due to cognitive differences between patients with formal education and those without formal education. Patients who cannot read and write overlook sources of information such as posters, flyers, and other written materials.
The probability of poor self-care practice was higher and statistically significant among patients with chronic disease co-morbidity. This finding was consistent with the other studies from Ethiopian settings [27, 53, 63]. This may be due to symptoms of co-morbidity that interfere with self-management of high blood pressure, or lifestyle changes caused by the co-morbidity. In addition, comorbid conditions exacerbate the patient's symptoms and prevent them from adapting to lifestyle changes [64].
In this study, people with uncontrolled blood pressure were twice as likely to be poorly self-managing as those with controlled blood pressure. This was in line with other studies [49, 62, 65, 66]. This may be due to the fact that good self-care habits can help control blood pressure.
This study also showed the impact of social support on self-management practices in patients with arterial hypertension. Patients with poor social support were nearly three times more likely to have poor self-management than patients with good social support. This was consistent with other studies [25, 53, 67]. This can be attributed to several aspects, of social support in stress management, and psychoactive self-help activities, that positively impact patients’ lifestyle changes. This study also showed a statistically significant relationship between attitudes toward hypertension and self-management practices. Patients with unfavorable were three times more likely to have poor self-care than patients with positive attitudes. This may be because hypertensive patients understand the complications of the disease and can engage in effective self-management to prevent these complications.
Limitation of the study
As this is a one-hospital study, it will be difficult to generalize. Because the study participants’ self-management practices were based on self-report, there may be memory bias and social desirability bias.
Conclusion
The level of self-care practices for hypertension in the study area was low. In particular, the level of adherence to the DASH diet, exercise, and weight control was very low. Not attending formal education, uncontrolled BP, poor social support, and unfavorable attitude, and living with chronic disease co-morbidity were independent predictors of poor self-care practices. Improving self-management practices for hypertension requires targeted, patient-specific interventions.
Acknowledgements
We would like to acknowledge Jimma University for the approval of ethical clearance and funding support of this study. We would like to express our gratitude for health care professionals of Jimma Medical Center for their unreserved support during the work. Our acknowledgment extends to the study participants, data collectors, and supervisors who participated in the study.
Abbreviations
- AOR
Adjusted odds ratio
- CVD
Cardiovascular disease
- COR
Crude odds ratio
- CI
Confidence interval
- BP
Blood pressure
- DASH
Dietary approach to stop hypertension
- DASH-Q
Dietary approach to stop hypertension quality
- ETB
Ethiopian Birr
- HTN
Hypertension
- HELM
Hypertension evaluation of lifestyle and management
- H-SCALE
Hypertension-related self-care activity level
- JMC
Jimma Medical Center
- MSPSS
Multidimensional Perceived Social Support Scale
- NCD
Non-communicable disease
- SPSS
Statistical package for social science
- WHO
World Health Organization
Authors’ contributions
The analysis was conceptualized by TM, HF and AF. Data collection was managed by TM, BB and AG. Data analysis was conducted by TM and AF. TM drafted the manuscript. All authors participated in editing, feedback and revisions. All authors read and approved the final manuscript.
Funding
This study was sponsored by Jimma University, Ethiopia.
Availability of data and materials
All materials and data are available from the corresponding author without any restriction.
Declarations
Ethical approval and consent to participate
Ethical approval for the study was obtained from institutional review board (IRB) of Institute of Health, Jimma University. Data were collected after informed verbal consent is obtained from the participants. Confidentiality of the information was maintained by excluding names as identification in the questionnaire and keeping their privacy during the data collection.
Consent for publication
Not applicable.
Competing interests
The authors declared that they have no competing interests. The funder had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kaptoge S, Pennells L, De Bacquer D, Cooney MT, Kavousi M, Stevens G, et al. World Health Organization cardiovascular disease risk charts: revised models to estimate risk in 21 global regions. Lancet Glob Health. 2019;7(10):e1332–e1345. doi: 10.1016/S2214-109X(19)30318-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bacha D, Abera H. Knowledge, attitude and self-care practice towards control of hypertension among hypertensive patients on follow-up at St. Paul’s hospital, Addis Ababa. Ethiop J Health Sci. 2019;29(4). [DOI] [PMC free article] [PubMed]
- 3.Hypertension R. Detection. Evaluation, and Management: a Scientific Statement From the American Heart Association Hypertension [Internet] [citirano 2020 Lipnja 6] Dostupno na: https://www.ahajournalsorg/doi/101161/HYP. 2018;84. [DOI] [PMC free article] [PubMed]
- 4.Chia YC, Ching SM. Prevalence and predictors of resistant hypertension in a primary care setting: a cross-sectional study. BMC Fam Pract. 2014;15(1):1–7. doi: 10.1186/1471-2296-15-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Whelton PK, Carey RM, Aronow WS, Casey DE, Jr, Collins KJ, Dennison Himmelfarb C, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):1269–1324. doi: 10.1161/HYP.0000000000000066. [DOI] [PubMed] [Google Scholar]
- 6.WHO. A global brief on Hypertension. WHO. 2013.
- 7.Kibret KT, Mesfin YM. Prevalence of hypertension in Ethiopia: a systematic meta-analysis. Public Health Rev. 2015;36(1):14. doi: 10.1186/s40985-015-0014-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abebe SM, Andargie G, Shimeka A, Alemu K, Kebede Y, Wubeshet M, et al. The prevalence of non-communicable diseases in northwest Ethiopia: survey of Dabat Health and Demographic Surveillance System. BMJ Open. 2017;7(10):e015496. doi: 10.1136/bmjopen-2016-015496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dorans KS, Mills KT, Liu Y, He J. Trends in Prevalence and Control of Hypertension According to the 2017 American College of Cardiology/American Heart Association (ACC/AHA) Guideline. J Am Heart Assoc. 2018;7(11). [DOI] [PMC free article] [PubMed]
- 10.World Health Organization. Regional Office for the Eastern Mediterranean. World Health Day 2013: control your blood pressure control your life: high blood pressure control it with legislation. 2013. https://apps.who.int/iris/handle/10665/113247.
- 11.Fagard RH. Resistant hypertension. Heart. 2012;98(3):254–261. doi: 10.1136/heartjnl-2011-300741. [DOI] [PubMed] [Google Scholar]
- 12.Bacha D, Abera H. Knowledge, attitude and self-care practice towards control of hypertension among hypertensive patients on follow-up at St Paul’s Hospital, Addis Ababa. Ethiop J Health Sci. 2019;29(4):421–430. doi: 10.4314/ejhs.v29i4.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Belko N, Creel E, Thomas P. APRNs application of transtheoretical basis to improve adherence to treatment regimen in hypertensive patients.
- 14.Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–3104. doi: 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]
- 15.AlHadlaq RK, Swarelzahab MM, AlSaad SZ, AlHadlaq AK, Almasari SM, Alsuwayt SS, et al. Factors affecting self-management of hypertensive patients attending family medicine clinics in Riyadh, Saudi Arabia. J Fam Med Primary Care. 2019;8(12):4003. doi: 10.4103/jfmpc.jfmpc_752_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Appel LJ. Lifestyle modification as a means to prevent and treat high blood pressure. J Am Soc Nephrol. 2003;14(suppl 2):S99–S102. doi: 10.1097/01.asn.0000070141.69483.5a. [DOI] [PubMed] [Google Scholar]
- 17.Durai V, Muthuthandavan AR. Knowledge and practice on lifestyle modifications among males with hypertension. Indian J Comm Health. 2015;27(1):143–149. [Google Scholar]
- 18.Mengistu MD. Pattern of blood pressure distribution and prevalence of hypertension and prehypertension among adults in Northern Ethiopia: disclosing the hidden burden. BMC Cardiovasc Disord. 2014;14(1):33. doi: 10.1186/1471-2261-14-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Riegel B, Moser DK, Anker SD, Appel LJ, Dunbar SB, Grady KL, et al. State of the science: promoting self-care in persons with heart failure: a scientific statement from the American Heart Association. Circulation. 2009;120(12):1141–1163. doi: 10.1161/CIRCULATIONAHA.109.192628. [DOI] [PubMed] [Google Scholar]
- 20.Tibebu A, Mengistu D, Negesa L. Adherence to recommended lifestyle modifications and factors associated for hypertensive patients attending chronic follow-up units of selected public hospitals in Addis Ababa, Ethiopia. Patient Prefer Adherence. 2017;11:323–330. doi: 10.2147/PPA.S126382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Buda ES, Hanfore LK, Fite RO, Buda AS. Lifestyle modification practice and associated factors among diagnosed hypertensive patients in selected hospitals, South Ethiopia. Clin Hypertens. 2017;23(1):26. doi: 10.1186/s40885-017-0081-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hu H, Li G, Arao T. Prevalence rates of self-care behaviors and related factors in a rural hypertension population: a questionnaire survey. Int J Hypertens. 2013;2013:8. doi: 10.1155/2013/526949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Motlagh SFZ, Chaman R, Sadeghi E, Eslami AA. Self-care behaviors and related factors in hypertensive patients. Iran Red Crescent Med J. 2016;18(6). [DOI] [PMC free article] [PubMed]
- 24.Beigi MA, Zibaeenezhad MJ, Aghasadeghi K, Jokar A, Shekarforoush S, Khazraei H. The effect of educational programs on hypertension management. Int Cardiovasc Res J. 2014;8(3):94–98. [PMC free article] [PubMed] [Google Scholar]
- 25.Labata BG, Ahmed MB, Mekonen GF, Daba FB. Prevalence and predictors of self care practices among hypertensive patients at Jimma University Specialized Hospital, Southwest Ethiopia: cross-sectional study. BMC. 2019. [DOI] [PMC free article] [PubMed]
- 26.Akhter N. Self-management among patient with hypertension in Bangladesh: prince of Songkla University; 2010.
- 27.Buda ES, Hanfore LK, Fite RO, Buda AS. Lifestyle modification practice and associated factors among diagnosed hypertensive patients in selected hospitals, South Ethiopia. Biomed Central. 2017. [DOI] [PMC free article] [PubMed]
- 28.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002;288(19):2469–2475. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 29.Warren-Findlow J, Seymour RB. Prevalence rates of hypertension self-care activities among African Americans. J Natl Med Assoc. 2011;103(6):503–512. doi: 10.1016/s0027-9684(15)30365-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ademe S, Aga F, Gela D. Hypertension self-care practice and associated factors among patients in public health facilities of Dessie town, Ethiopia. BMC Health Serv Res. 2019;19(1):1–9. doi: 10.1186/s12913-019-3880-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Parkerson G, Jr, Broadhead W, Tse C. Validation of the duke social support and stress scale. Fam Med. 1991;23(5):357–360. [PubMed] [Google Scholar]
- 32.Schapira MM, Fletcher KE, Hayes A, Eastwood D, Patterson L, Ertl K, et al. The development and validation of the hypertension evaluation of lifestyle and management knowledge scale. J Clin Hypertens. 2012;14(7):461–466. doi: 10.1111/j.1751-7176.2012.00619.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Warren-Findlow J, Basalik DW, Dulin M, Tapp H, Kuhn L. Preliminary validation of the hypertension self-care activity level effects (H-SCALE) and clinical blood pressure among patients with hypertension. J Clin Hypertens. 2013;15(9):637–643. doi: 10.1111/jch.12157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Warren-Findlow J, Seymour RB, Huber LRB. The association between self-efficacy and hypertension self-care activities among African American adults. J Community Health. 2012;37(1):15–24. doi: 10.1007/s10900-011-9410-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Association AH. A report of American heart association task force on clinical practice guidelines. Report. 2017.
- 36.Mcdowell. Measuring health: a guide to rating scales. Stat Med. 1989;8:1308–9.
- 37.Lavsa SM, Holzworth A, Ansani NT. Selection of a validated scale for measuring medication adherence. J Am Pharm Assoc. 2011;51(1):90–94. doi: 10.1331/JAPhA.2011.09154. [DOI] [PubMed] [Google Scholar]
- 38.Organization WH. Technical package for cardiovascular disease management in primary health care. WHO. 2018.
- 39.Warren-Findlow J, Reeve CL, Racine EF. Psychometric validation of a brief self-report measure of diet quality: the DASH-Q. J Nutr Educ Behav. 2017;49(2):92–99. doi: 10.1016/j.jneb.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 40.Wijndaele K, Duvigneaud N, Matton L, Duquet W, Delecluse C, Thomis M, et al. Sedentary behaviour, physical activity and a continuous metabolic syndrome risk score in adults. Eur J Clin Nutr. 2009;63(3):421–429. doi: 10.1038/sj.ejcn.1602944. [DOI] [PubMed] [Google Scholar]
- 41.Yen IH, Kaplan GA. Poverty area residence and changes in physical activity level: evidence from the Alameda County Study. Am J Public Health. 1998;88(11):1709–1712. doi: 10.2105/ajph.88.11.1709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Saad AP. Association between health literacy and weight management behaviors among individuals with hypertension: data from the newest vital sign: The University of North Carolina at Charlotte; 2016.
- 43.Khavari K, Farber P, Douglass F. A scale for the indirect assessment of alcohol intake. The alcohol use predictor scale. J Stud Alcohol. 1979;40(7):683–692. doi: 10.15288/jsa.1979.40.683. [DOI] [PubMed] [Google Scholar]
- 44.Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334–1357. doi: 10.1161/HYPERTENSIONAHA.120.15026. [DOI] [PubMed] [Google Scholar]
- 45.Ajiboye RO, Okafor NA, Ojo IC. Knowledge and practice of lifestyle modification among hypertensive patients in a General Hospital Lagos. IOSR J Nurs Health Sci (IOSR-JNHS). 2020;9(2).
- 46.Abdulwahed A, Seid A, Yimam E. Level of self-care practice and associated factors among hypertensive patients in Jimma University Specialized Hospital, south west Ethiopia. Unpublished 2016.
- 47.Ermias ATT. Lifestyle modification practice and associated factors among diagnosed hypertensive patients in Mizan Tepi University Teaching Hospital South west Ethiopia PAMJ. Clin Med. 2019;2.
- 48.Khorsandi M, Roozbahani N, Zade Zf, editors. A survey on health beliefs relation with self—care practice among the elderly hypertension in Iran (2013) 2014.
- 49.Nadewu AN, Geda B. Adherence to healthy lifestyle among hypertensive patients in Harar Region, Eastern Ethiopia. Prim Health Care. 2018 doi: 10.4172/2167-1079.1000308. [DOI] [Google Scholar]
- 50.Fetensa G, Milkiyas N, Besho M, Hasen T, Teshoma M, Wakuma B, Etefa W, Fayisa L. Assessment of knowledge and practice of life style modification among hypertensive patients at Nekemte Specialized Hospital, Western Oromia. J Cardiovasc Dis Diagn. 2019.
- 51.Tusubira AK, Nalwadda CK, Akiteng AR, et al. Self-care practices and needs in patients with hypertension, diabetes, or both in rural Uganda: a mixed-methods study. UINCD. 2020.
- 52.Bakhsh LA, Adas AA, Murad MA, Nourah RM, Hanbazazah SA, Aljahdali AA, Alshareef RJ. Awareness and knowledge on hypertension and its SelfCare practices among hypertensive patients in Saudi Arabia. Ann Int Med Dental Res. 2017;3(5).
- 53.Tibebu A, Mengistu D, Negesa L. Adherence to recommended lifestyle modifications and factors associated for hypertensive patients attending chronic follow-up units of selected public hospitals in Addis Ababa, Ethiopia. Dovepress. 2017;11:323–330. doi: 10.2147/PPA.S126382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Durai V, Muthuthandavan AR. Knowledge and Practice on lifestyle modifications among males with hypertension. Indian J Comm Health. 2015;27:143. [Google Scholar]
- 55.Kimani S, Mirie W, Chege M, Okube OT, Muniu S. Association of lifestyle modification and pharmacological adherence on blood pressure control among patients with hypertension at Kenyatta National Hospital, Kenya: a cross-sectional study. BMJ Open. 2019;9(1):e023995. doi: 10.1136/bmjopen-2018-023995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ezeala-Adikaibe BA, Mbadiwe N, Okudo G, et al. Factors associated with medication adherence among hypertensive patients in a tertiary health center: a cross-sectional study. Arch Commun Med Public Health. 2455–5479.
- 57.Adisa R, Ilesanmi OA, Fakeye TO. Treatment adherence and blood pressure outcome among hypertensive out-patients in two tertiary hospitals in Sokoto, Northwestern Nigeria. BMC Cardiovasc Disord. 2018;18(1):194. doi: 10.1186/s12872-018-0934-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gee ME, Bienek A, Campbell NR, Bancej CM, Robitaille C, Kaczorowski J, et al. Prevalence of, and barriers to, preventive lifestyle behaviors in hypertension (from a national survey of Canadians with hypertension) Am J Cardiol. 2012;109(4):570–575. doi: 10.1016/j.amjcard.2011.09.051. [DOI] [PubMed] [Google Scholar]
- 59.Yang MH, Kang SY, Lee JA, Kim YS, Sung EJ, Lee K-Y, et al. The effect of lifestyle changes on blood pressure control among hypertensive patients. Korean J Fam Med. 2017;38(4):173–180. doi: 10.4082/kjfm.2017.38.4.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Akbarpour S, Khalili D, Zeraati H, Mansournia MA, Ramezankhani A, Fotouhi A. Healthy lifestyle behaviors and control of hypertension among adult hypertensive patients. Sci Rep. 2018;8(1):8508. doi: 10.1038/s41598-018-26823-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Obirikorang Y, Obirikorang C, Acheampong E, Anto E, Amoah B, Fosu E, Amehere J, Batu E, Brenya P, Amankwaa B, Adu E, Akwasi A, Asiwu R. Adherence to lifestyle modification among hypertensive clients: a descriptive cross-sectional study. Open Access Library J. 2018;5:1–13. doi: 10.4236/oalib.1104375. [DOI] [Google Scholar]
- 62.Gebremichael GB, Berhe KK, Beyene BG. Self-care practices and associated factors among adult hypertensive patients in Ayder Comprehensive Specialized Hospital, Tigray, Ethiopia. BMC. 2019;12:489. doi: 10.1186/s13104-019-4502-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Niriayo YL, Ibrahim S, Kassa TD, et al. Practice and predictors of self-care behaviors among ambulatory patients with hypertension in Ethiopia. PLoS ONE. 2019;14(6):e0218947. doi: 10.1371/journal.pone.0218947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bryan Williams GM, Spiering W, et al. Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3007. doi: 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]
- 65.Logan AG, Irvine MJ, McIsaac WJ, Tisler A, Rossos PG, Easty A, et al. Effect of home blood pressure telemonitoring with self-care support on uncontrolled systolic hypertension in diabetics. Hypertension. 2012;60(1):51–57. doi: 10.1161/HYPERTENSIONAHA.111.188409. [DOI] [PubMed] [Google Scholar]
- 66.Beune EJ, Moll van Charante EP, Beem L, Mohrs J, Agyemang CO, Ogedegbe G, et al. Culturally adapted hypertension education (CAHE) to improve blood pressure control and treatment adherence in patients of African origin with uncontrolled hypertension: cluster-randomized trial. PLoS ONE. 2014;9(3):e90103. doi: 10.1371/journal.pone.0090103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sewunet Ademe FAaDG. Hypertension self-care practice and associated factors among patients in public health facilities of Dessie town, Ethiopia. BMC Health Serv Res. 2019. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All materials and data are available from the corresponding author without any restriction.