Abstract
Background
Autism spectrum disorders (ASD) are characterized by impairment in social interaction, impairment in communication and lack of flexibility of thought and behavior. Acupuncture, which involves the use of needles or pressure to specific points on the body, is used widely in Traditional Chinese Medicine and increasingly within a western medical paradigm. It has sometimes been used as a treatment aimed at improving ASD symptoms and outcomes, but its clinical effectiveness and safety has not been rigorously reviewed.
Objectives
To determine the effectiveness of acupuncture for people with ASD in improving core autistic features, as well as communication, cognition, overall functioning and quality of life, and to establish if it has any adverse effects.
Search methods
We searched the following databases on 30 September 2010: CENTRAL (The Cochrane Library, 2010, Issue 3), MEDLINE (1950 to September 2010 Week 2), EMBASE (1980 to 2010 Week 38), PsycINFO, CINAHL, China Journal Full‐text Database, China Master Theses Full‐text Database, China Doctor Dissertation Full‐text Database, China Proceedings of Conference Database, Index to Taiwan Periodical Literature System, metaRegister of Controlled Trials and the Chinese Clinical Trials Registry. We also searched AMED (26 February 2009) and Dissertation Abstracts International (3 March 2009), but these were no longer available to the authors or editorial base at the date of the most recent search. TCMLARS (Traditional Chinese Medical Literature Analysis and Retrieval System) was last searched on 3 March 2009.
Selection criteria
We included randomized and quasi‐randomized controlled trials. We included studies comparing an acupuncture group with at least one control group that used no treatment, placebo or sham acupuncture treatment in people with ASD. We excluded trials that compared different forms of acupuncture or compared acupuncture with another treatment.
Data collection and analysis
Two review authors independently extracted trial data and assessed the risk of bias in the trials. We used relative risk (RR) for dichotomous data and mean difference (MD) for continuous data.
Main results
We included 10 trials that involved 390 children with ASD. The age range was three to 18 years and the treatment duration ranged from four weeks to nine months. The studies were carried out in Hong Kong, mainland China and Egypt.
Two trials compared needle acupuncture with sham acupuncture and found no difference in the primary outcome of core autistic features (RFRLRS total score: MD 0.09; 95% CI ‐0.03 to 0.21, P = 0.16), although results suggested needle acupuncture might be associated with improvement in some aspects of the secondary outcomes of communication and linguistic ability, cognitive function and global functioning.
Six trials compared needle acupuncture plus conventional treatment with conventional treatment alone. The trials used different primary outcome measures and most could not demonstrate effectiveness of acupuncture in improving core autistic features in general, though one trial reported patients in the acupuncture group were more likely to have improvement on the Autism Behavior Checklist (RR 1.53; 95% CI 1.09 to 2.16, P = 0.02) and had slightly better post‐treatment total scores (MD ‐5.53; 95% CI ‐10.76 to ‐0.31, P = 0.04). There was no evidence that acupuncture was effective for the secondary outcome of communication and linguistic ability, though there seemed to be some benefit for the secondary outcomes of cognitive function and global functioning.
Two trials compared acupressure plus conventional treatment with conventional treatment alone and did not report on the primary outcome. Individual study results suggested there may be some benefit from acupressure for certain aspects of the secondary outcomes of communication and linguistic ability, cognitive function and global functioning.
Four trials reported some adverse effects, though there was little quantitative information, and at times both intervention and control groups experienced them. Adverse effects noted included bleeding, crying due to fear or pain, irritability, sleep disturbance and increased hyperactivity. None of the trials reported on quality of life.
There are a number of problems with the evidence base: the trials were few in number and included only children; six of the trials were at high risk of bias; they were heterogeneous in terms of participants and intervention; they were of short duration and follow‐up; they reported inconsistent and imprecise results, and, due to carrying out large numbers of analyses, they were at risk of false positivity.
Authors' conclusions
Current evidence does not support the use of acupuncture for treatment of ASD. There is no conclusive evidence that acupuncture is effective for treatment of ASD in children and no RCTs have been carried out with adults. Further high quality trials of larger size and longer follow‐up are needed.
Keywords: Adolescent; Child; Child, Preschool; Humans; Acupuncture Therapy; Acupuncture Therapy/methods; Child Development Disorders, Pervasive; Child Development Disorders, Pervasive/therapy; Randomized Controlled Trials as Topic; Treatment Outcome
Plain language summary
Acupuncture for people with autism spectrum disorders (ASD)
Autism spectrum disorders (ASD) are lifelong disorders of development. People with ASD have particular difficulties with social interaction and communication and they lack flexibility in their thinking and behavior. No cure is currently available but interventions may improve symptoms. Acupuncture involves using needles or pressure on specific areas of the body and is an important therapeutic method in Traditional Chinese Medicine. It is also being used more and more in countries in the west for a range of ailments. Acupuncture has been considered as a possible intervention to improve ASD symptoms, but it has not been thoroughly evaluated to see if it works and is safe.
We wanted to evaluate the effectiveness and safety of acupuncture for ASD by systematically reviewing all studies of acupuncture for ASD where people were randomly allocated to a treatment or control group (placebo, sham or no treatment), i.e. randomized controlled trials (RCTs). We searched through 15 databases, most recently in September 2010, and read over the titles and abstracts to make sure we identified everything relevant. We found10 RCTs to include in this review. These studies, which were carried out in Hong Kong, mainland China and Egypt, involved 390 children aged between three and 18 years.
Two studies compared needle acupuncture with sham acupuncture and found no difference in core autistic features. Results did suggest that needle acupuncture might be associated with improvement in other areas of communication and linguistic ability, cognitive function and global functioning.
Six studies compared needle acupuncture plus conventional treatment with conventional treatment alone. They used a range of tools to measure core autistic features and most could not show that acupuncture led to improvement in these. One trial did report, though, that needle acupuncture led to an improvement in scores on Autism Behavior Checklist. There was no evidence for improvement due to acupuncture on communication and linguistic ability but it might be beneficial for cognitive function and global functioning.
Two studies compared acupressure plus conventional treatment with conventional treatment alone and found no difference in core autistic features, although acupressure seemed to improve some aspects of the secondary outcomes.
Problems that were noted by parents of study participants included crying due to fear or pain, bleeding, sleep disturbance and increased hyperactivity. It is unclear if these were due to the acupuncture treatment. Half of the trials reported some negative effects but did not report how often or how severe these were and sometimes the problems occurred in both the treatment and control groups. None of the studies used measures of quality of life.
Overall, acupuncture did not seem to be effective in improving core features of ASD but it might have improved certain developmental and functioning outcomes, at least in the short term.
There are problems with assessing acupuncture due to the quality of the evidence. There were a small number of studies and they were all conducted with children. Moreover, there is a high likelihood that they may have been biased due to the methods used not being rigorous enough, the wide variety in the people and interventions in the studies, the inconsistent and imprecise reporting of results and the large number of analyses carried out, which make it more likely a significant result will be found just by chance.
In conclusion, current evidence does not support the use of acupuncture for the treatment of ASD. We need high quality trials of larger size and longer follow‐up as the evidence base at present has many limitations.
Background
Description of the condition
Autism spectrum disorders (ASD) are developmental disorders characterized by the triad of impairments of social interaction, social communication and social imagination (Wing 1997). Repetitive and stereotyped behaviors are often associated with ASD (Wing 1997). The term ASD includes autistic disorder, Asperger syndrome and pervasive developmental disorder (not otherwise specified) (Faras 2010). The impairments of ASD can have a severe impact on learning and social functioning that may persist into adulthood. ASD have an estimated prevalence of 3.3 to 116 children per 10,000 (Burd 1987; Baird 2006), and there might be an increasing trend as higher prevalence rates have been reported in more recent studies (Williams 2008).
ASD have multiple etiologies. There are a few specific genetic conditions that can be associated with ASD (Folstein 1991). There is ample evidence for complex genetic susceptibility (Folstein 1991; Muhle 2004). Environmental factors such as toxic exposures, teratogens, perinatal insults and prenatal infections including rubella and cytomegalovirus, also contribute to a small proportion of cases (Muhle 2004). ASD was once also linked to MMR vaccination (Wakefield 1998), but the original evidence was later found to be fraudulent (Godlee 2011) and other epidemiological studies refuted the link (Madsen 2002; Taylor 2002). It is suggested that ASD might result from an interaction between genetic, environmental and immunological factors, with oxidative stress as a mechanism linking these risk factors (Chauhan 2006). Recently, research has focused on the role of synapse structure and function as central to the development of ASD and suggests possible targets for interventions (Rapin 2008).
ASD can present quite differently and they are often comorbid with conditions such as epilepsy (Muhle 2004), mood disorders (major depressive disorder, bipolar disorder, specific phobic disorder, separation anxiety disorder, social phobia, generalized anxiety disorder, obsessive compulsive disorder) and behavioral disorders (attention‐deficit hyperactivity disorder, oppositional defiant disorder) (Leyfer 2006), which render it difficult to be sure about the effectiveness of therapies. Furthermore, the problems and manifestations of ASD might change with time like other developmental abnormalities. Therefore, it is likely that outcomes of treatment will depend on timing of therapy in relation to age and onset or progression of problems.
Description of the intervention
Various behavioral interventions for ASD are widely used without rigorously documented evidence (Bryson 2003). Pharmacological treatments have been, at best, useful adjuncts to behavioral intervention for attention deficits, sleep disturbance, mood disorder, self‐harm or aggression to others (Gringras 2000; Posey 2001). Many aspects of ASD are still debatable, with elusive and complex etiologies, and no effective therapy exists, although there is broad consensus that early intensive intervention is warranted (Bryson 2003). Frustrated parents are therefore eager to explore different forms of complementary and alternative medicine (CAM) (AAP 2001; Levy 2003; Harrington 2006; Wong 2006a; Wong 2006b; Hanson 2007). Estimates of the use of CAM in children with ASD in the USA range from 31.7% in Philadelphia (Levy 2003) to 95% in New York and New Jersey (Harrington 2006). However, very few patients (less than 1%) use acupuncture in the United States (Hanson 2007; Harrington 2006; Levy 2003) or in Canada (Wong 2006b). A recent study found that 40% of children with ASD in Hong Kong reported previous use of CAM, with acupuncture being the most common form (used by 48% of respondants) (Wong 2009).
Acupuncture is a procedure in which specific body areas, the meridian points, are pierced with fine needles for therapeutic purposes. Meridian points (acupoints) are points on the body surface that when stimulated are thought to cause therapeutic effects. Acupuncture is one of the major modalities of treatment in Traditional Chinese Medicine. Its use can be traced back more than 2000 years in China (Wu 1996), and the intervention spread to Korea, Japan, Vietnam and other places in East Asia. Acupuncture further spread to Europe in the 17th to the 19th centuries via translations of Asian medical texts by Portuguese, French, Dutch and Danish missionaries and physicians traveling to China and Japan. In the 20th century, acupuncture was codeveloped with biomedical science in Europe and then in the USA (Helms 2007).
Nowadays there are basically two different paradigms of acupuncture for treatment of diseases, namely the Traditional Chinese Medicine (TCM) paradigm and the medical acupuncture paradigm. In the TCM paradigm, how acupuncture restores the homeostasis of the body and cures disease involves complex theories of regulation of five elements (fire, earth, metal, water, and wood), Yin and Yang, Qi, blood and body fluids. By stimulating various meridian points, disharmony and dysregulation of organ systems is corrected to relieve symptoms and restore natural internal homeostasis (Maciocia 1989).
Reported to be a relatively simple, inexpensive and safe treatment, acupuncture has been well accepted by Chinese patients and is widely used in various neurological and other disorders as an alternative treatment approach (Johansson 1993). Acupuncture is also increasingly practiced in some Western countries (NIH 1998). However, acupuncture has been reported to be associated with various adverse events and complications, including fainting, metal allergy, infection, pneumothorax, stroke, subarachnoid and cerebral hemorrhage (Zhang 2010). The risk of these complications can be reduced by sterilization of needles and good acupuncture skills (Leung 2009).
How the intervention might work
The concept of wellness, which has been used in the context of alternative medicine since the 1950s (Dunn 1961), means a healthy balance of the mind, body and spirit. Wellness programs offer alternative medicine techniques to improve wellbeing, although the effectiveness of these techniques in improving health remains controversial.
Like much CAM, the TCM approach to treating ASD is holistic. The pathogenesis of ASD according to TCM is "derangement and insufficiency of brain and mind" (Chen 2008). The pathologic involvement is in the brain, relating to the heart, pericardium, liver, spleen and kidney in TCM theory (Chen 2008). In traditional Chinese acupuncture theory, nearly 400 acupoints on the body surface are interrelated to various functions linked through 14 meridians to various organs or viscera of the human body. By stimulating various meridian points, acupuncture may be able to correct the disharmony and dysregulation of organ systems, which might be involved in various dimensions of ASD, to relieve symptoms and restore the mind and body. The scientific basis of how acupuncture could ameliorate different cognitive and behavioral dimensions of autism has not been well studied and the mechanisms of how acupuncture works are likely to be very complex, given the vast number of acupoints involved in the treatment of this complicated disease. Possible mechanisms of acupuncture for the treatment of ASD include regulation of neurotransmitters such as glutamate (Lee 2010) and gamma‐aminobutyric acid (GABA) (Fu 2009; Yoon 2010), which were shown to be disturbed in many patients with ASD (Carlson 2011; Chao 2010). Acupuncture can also modulate neurotrophins (Manni 2010), neuroimmune response (Li 2009), neuroinflammation (Yang 2010), oxidative stress (Wang 2011) and apoptosis of neural tissues (Zhang 2008), which contribute to the pathogenesis of ASD (Araghi‐Niknam 2003; Sajdel‐Sulkowska 2009; Correia 2010; Sheikh 2010a; Sheikh 2010b; Buehler 2011; Young 2011).
In the medical acupuncture paradigm, investigators try to identify anatomical correlates and physiological and biochemical mechanisms that may explain the rationale of acupuncture within a modern science framework. Electrical impedance of connective tissues can be measured around meridian points (Wong 2010) and connective tissues associated with meridians may have lower electrical impedance than non‐meridian tissues (Ahn 2005). There is currently no strong evidence to show the correspondence of meridians or acupoints to any anatomical feature. Proponents believe a close proximity exists between acupoints and the nervous system (Fu 2000). One study (Dung 1984) investigated the anatomical features of acupoints and found that structures in the vicinity of acupoints exclusively involved nerves. Therefore, it is hypothesized that by inserting fine needles into these nerve‐innervated acupoints, a sequence of neurological responses would be elicited. These responses can occur locally or close to the site of application (Jansen 1989), or at a distance, mediated mainly by sensory neurons to many structures within the central nervous system (Magnusson 1994). This can lead to activation of pathways affecting various physiological systems in the brain as well as in the periphery (Sun 2001; Liu 2004; Middlekauff 2004). The effect of acupuncture has been demonstrated in animal and human studies to be due to direct neural stimulation; changes in neurotransmitters such as endorphin (Lin 2008), serotonin (Moazzami 2010) and endocannabinoid (Wang 2009), and modification of immunological markers (Kim 2010) or endocrinological signals (Stux 1998).
Why it is important to do this review
It is worrying that many CAM therapies including acupuncture that claim to be effective in ASD have not actually undergone stringent scientific testing. It is claimed acupuncture is effective in treating virtually all diseases; however, it remains uncertain whether the existing evidence supports its use for people with ASD. Acupuncture is one of most common forms of CAM and an evidence‐based systematic review regarding its use in people with ASD needs to be undertaken.
Objectives
To determine the effectiveness and safety of acupuncture therapy in people with autism spectrum disorders.
Methods
Criteria for considering studies for this review
Types of studies
Randomized controlled clinical trials, including those using a quasi‐random method for allocation of treatment, i.e., trials using alternate allocation or allocation by birth date. We will also include cross‐over trials.
Types of participants
People of any age with ASD such as autistic disorder, Asperger syndrome or pervasive developmental disorder diagnosed by standard criteria such as the Diagnostic and Statistical Manual (DSM) (APA 2000) or International Classification of Diseases (ICD) criteria (WHO 1992). We will accept diagnosis by assessment tools such as Autism Diagnostic Observation Scale (ADOS) (Lord 1997), Autism Diagnostic Interview‐Revised (ADI‐R) (Lord 1994), the Diagnostic Interview for Social and Communication Disorders (DISCO) (Wing 1999) and the developmental, dimensional and diagnostic interview (Skuse 2004).
Types of interventions
Trials evaluating all forms of acupuncture therapy including acupressure, laser acupuncture or electroacupuncture regardless of number of times treatment is given or length of treatment period. We included either traditional acupuncture in classical meridian points or contemporary acupuncture in non‐meridian or trigger points regardless of the source or methods of stimulation (for example, hand, needle, laser or electrical stimulation).
The control interventions could be no treatment, placebo acupuncture or sham acupuncture. Placebo acupuncture refers to a needle attached to the skin surface (not penetrating the skin but at the same acupoints) (Furlan 2005). Sham acupuncture refers to a needle placed in an area close to but not in acupuncture points (Furlan 2005) or subliminal skin electrostimulation via electrodes attached to the skin (SCSSS 1999).
We investigated the comparisons listed below:
acupuncture only compared with no treatment;
acupuncture only compared with placebo or sham treatment;
acupuncture in addition to baseline medication or treatment compared with the same baseline medication or treatment alone;
acupuncture in addition to baseline medication or treatment compared with placebo or sham treatment in addition to the same baseline medication or treatment.
We excluded trials that compared only different forms of acupuncture or compared acupuncture with other forms of treatment.
Types of outcome measures
Primary outcomes
Core features of ASD, i.e. social interaction, communication and behavioral problems including stereotypy or restricted, repetitive patterns of behavior, interests or activities, as measured by validated instruments and behavioral observations, such as Aberrant Behavior Checklist (ABC) (Aman 1986), Ritvo‐Freeman Real Life Rating Scale (RFRLRS) (Freeman 1986), Autism Treatment Evaluation Checklist (ATEC) (Rimland 1999) and Autism Diagnostic Observation Scale (ADOS) (Lord 1997).
Secondary outcomes
Communication and linguistic ability, as measured by standardized instruments such as Reynell Language Developmental scale (RLDS) (Edwards 1997) and the Symbolic Play Test (SPT) (Lowe 1976).
Cognitive functioning, as measured by standardized instruments such as Griffiths Mental Developmental Scale (GMDS) (Griffiths 1996) and the Leiter International Performance Scale‐Revised (Leiter‐R) (Leiter 1980).
Global functioning, as measured by standardized instruments such as Pediatric Evaluation Disability Inventory (PEDI) (Haley 1992) and the Functional Independence Measure for Children (WeeFIM) (Msall 1994).
Quality of life, as measured by standardized instruments such as WHOQOL‐BREF (WHO 1993).
Frequency of adverse effects, such as needle pain, tiredness, bleeding, faintness, syncope, and pneumothorax (Ernst 2001).
Search methods for identification of studies
We ran the initial searches for this review in February 2009 and repeated them in September 2010. The relocation of the editorial base between these dates meant that two databases (AMED and Dissertation Abstracts International ) were no longer available and these searches could not be updated. One database (PsycINFO) was available on a different platform so the search strategy was adapted for it. We searched a number of English language and Chinese language databases. The search strategy for the Chinese databases used the Chinese translation (in either simplified or complex character) of autism, which is equivalent to 'Self Shut‐Off Syndrome' in Hong Kong and Taiwan and 'Lonely Syndrome' in Mainland China.
Electronic searches
We searched the following databases.
Cochrane Central Register of Controlled Trials (CENTRAL) 2010, Issue 3, part of the Cochrane Library (searched 30 September 2010) MEDLINE, 1950 to September Week 3, 2010 (searched 30 September 2010) EMBASE, 1980 to 2010 Week 38 (searched 30 September 2010) PsycINFO via OVID, 1806 to February Weeek 4 2009 (searched February 2009) PsycINFO via EBSCOhost ,1887 to September 2010 (searched 30 September 2010) CINAHL, 1937 to September 2010, (searched 1 October 2010) metaRegister of Controlled Trials ( searched 30 September 2010) AMED:1985 to February 2009 (searched 26 February 2009) Dissertation Abstracts International ( searched 3 March 2009)
The search strategies for these databases are in Appendix 1.
We also searched the following Chinese databases.
TCMLARS (Traditional Chinese Medical Literature Analysis and Retrieval System) (3 March 2009) Chinese Clinical Trials Registry (30 September 2010) China Journal Full‐text Database (30 September 2010) China Master Theses Full‐text Database (30 September 2010) China Doctor Dissertation Full‐text Database (30 September 2010) China Proceedings of Conference Database (30 September 2010) Index to Taiwan Periodical Literature System (30 September 2010)
The search strategies for the Chinese databases are in Appendix 2.
Searching other resources
We searched the reference lists of all relevant papers for further studies. There was no language restriction in the search and inclusion of studies.
Data collection and analysis
Selection of studies
Two review authors (DKLC and WXC) independently reviewed titles and abstracts retrieved from the searches and selected all potentially relevant studies. We obtained copies of these articles and the same review authors independently reviewed them against the inclusion criteria of the study. Review authors were not blinded to the names of the authors, institutions or journal of publication. We resolved any disagreements by consensus.
Data extraction and management
We extracted the following data:
Study methods
Design (for example, parallel or crossover design).
Randomization method (including list generation).
Method of allocation concealment.
Blinding method.
Stratification factors.
Participants
Inclusion/exclusion criteria.
Number (total/per group).
Age and sex distribution.
Specific diagnosis/diagnostic subtypes.
Comorbidities.
Duration of disorder.
Previous treatments.
Intervention and control
Type of acupuncture.
Details of treatment regime including duration of treatment.
Type of control.
Details of control treatment including drug dosage.
Details of co‐interventions.
Washout period in cross‐over design.
Follow‐up data
Duration of follow‐up.
Dates of treatment withdrawal and reasons for treatment withdrawal.
Withdrawal rates.
Outcome data as described above
Analysis data
Methods of analysis (intention‐to‐treat/per‐protocol analysis).
Comparability of groups at baseline (yes/no).
Statistical techniques.
WX Chen entered data into Review Manager 5.1 (RevMan 2011) and DKL Cheuk checked it.
Assessment of risk of bias in included studies
For each included study, two review authors (DKLC and WXC) independently completed the Cochrane Collaboration's tool for assessing risk of bias (Higgins 2011, section 8.5.1). We resolved any disagreement with a third review author (VW). We assessed the degree to which:
the allocation sequence was adequately generated ("sequence generation");
the allocation was adequately concealed ("allocation concealment");
knowledge of the allocated interventions was adequately prevented during the study ("blinding");
incomplete outcome data were adequately addressed;
reports of the study were free of suggestion of selective outcome reporting;
the study was apparently free of other problems that could put it at high risk of bias.
We allocated each domain one of three possible categories for each of the included studies: low risk of bias, high risk of bias and unclear risk of bias (i.e., the risk of bias is uncertain or unknown).
Measures of treatment effect
Binary outcomes
We used risk ratio (RR) with 95% confidence intervals (CI) for binary outcomes.
Continuous outcomes
We used mean difference (MD) with 95% CI for continuous outcomes. If studies used different scales to measure the same outcomes, we calculated standardized mean difference (SMD) with 95% CI.
All analyses included all participants in the treatment groups to which they were allocated if data were available.
Unit of analysis issues
There might be unit of analysis issues if cross‐over trials were included in the meta‐analysis. We planned to assess cross‐over trials to see whether: (i) the cross‐over design was suitable; (ii) there was a carry‐over effect; (iii) only first period data were available; (iv) correct analysis had been performed, and (v) results were comparable with those from parallel‐group trials. Where appropriate, we planned to combine the results of the cross‐over trials with results of parallel‐group trials.
If conducting a meta‐analysis combining the results of cross‐over trials, we planned to use the inverse variance methods recommended by Elbourne 2002. If data presented from a cross‐over trial were restricted (and more information was not available from the original investigators), we planned to use the presented data within the first phase only, up to the point of cross‐over. This was done for one included study.
Dealing with missing data
We contacted authors to supply data missing from included studies. We assessed missing data and attrition for each included study. If fewer than 70% of patients allocated to the treatments were reported on at the end of the trial for a particular outcome, we planned not use such data as they were considered to be too prone to bias. We noted differential dropout in the intervention group and assessed reasons as these could potentially bias the study results. All included studies had fewer than 30% of participants with missing data.
Assessment of heterogeneity
We assessed clinical heterogeneity by comparing the distribution of important participant factors between trials (age, gender, specific diagnosis/diagnostic subtypes, duration of disorder, associated neuropsychiatric diseases) and by comparing trial characteristics (randomization concealment, blinding, losses to follow‐up, treatment type, co‐interventions). We assessed statistical heterogeneity by examining I2 (Higgins 2011, section 9.5.2), a quantity which describes approximately the proportion of variation in point estimates that is due to heterogeneity rather that sampling error. In addition, we employed the Chi2 test of homogeneity to determine the strength of evidence that heterogeneity was genuine.
Assessment of reporting biases
We planned to do funnel plots (effect size against standard error) if sufficient studies (more than ten) were found. Asymmetry could be due to publication bias, but could also be due to a relationship between trial size and effect size. In the event that a relationship was found, we would have examined clinical diversity of the studies (Higgins 2011, section 10.4), but as none of the outcomes were reported by more than ten studies, we did not construct a funnel plot. We will do a funnel plot in an update of the review if appropriate.
Data synthesis
Where the interventions were the same or similar enough, we synthesized results in a meta‐analysis if there was no important clinical heterogeneity. We used both the fixed‐effect model and the random‐effects model in the meta‐analysis. These two methods are based on different assumptions and we were uncertain which assumption was more appropriate for the acupuncture trials. The fixed‐effect provided the best estimate of the typical treatment effect, assuming that the observed differences among study results were solely due to chance. The random‐effects model estimated the average treatment effect, assuming the treatment effects being estimated in the different studies were not identical, but followed some distribution (Higgins 2011, section 9.4.2). Since both models will yield similar results if there is no significant heterogeneity among the trials, we will report only results of the fixed‐effect model if there is no significant heterogeneity. If there is significant heterogeneity, we will report results of both models.
Subgroup analysis and investigation of heterogeneity
Large number of subgroup analyses may lead to misleading conclusions (Higgins 2011, section 9.6.2). We had planned only three exploratory subgroup analyses focusing on different age groups, diagnostic subtypes and level of disease severity. However, we were unable to perform any of these subgroup analyses because of insufficient data.
Sensitivity analysis
We performed sensitivity analyses to assess the impact of studies with different levels of risk of bias, by including only those with adequate methods of allocation concealment such as telephone randomization and adequate blinding, while excluding those trials with inadequate or unclear concealment of randomization, or unblinded trials.
Results
Description of studies
Results of the search
The electronic searches yielded a total of 346 records. We did not find any additional record from other sources. After we removed duplicates, 320 records remained. We screened all these records and excluded 296 records based on information in the title or abstract. We obtained full texts of the remaining 24 records. We excluded 13 records (reporting seven trials) and included 11 records (reporting 10 trials) for further analysis.
Included studies
Ten randomized controlled trials met the inclusion criteria (Wong 2002; Wang 2007; Wong 2007; Yan 2007; Allam 2008; Wong 2008; Zhou 2008; Chan 2009; Wong 2010a; Wong 2010b). One trial was published in two papers (Wang 2007). We have summarized the essential characteristics of these RCTs in the Characteristics of included studies table.
Location of studies
Five serial trials were performed in the same institute in Hong Kong (Wong 2002; Wong 2007; Wong 2008; Wong 2010a; Wong 2010b). One trial was performed in another institute in Hong Kong (Chan 2009). Three trials took place in different cities in China (Wang 2007; Yan 2007; Zhou 2008) and one in Egypt (Allam 2008).
Characteristics of participants
The 10 trials included a total of 196 participants in the intervention groups and 194 participants in the control groups. The participants included were all aged between three and 18 years, but more restrictive age groups (mostly young children) were targeted by most trials.
The diagnosis of ASD was based on DSM‐IV, ADI‐R and Childhood Autism Rating Scale (CARS) in four trials (Wong 2002 ; Wong 2007; Allam 2008; Wong 2010a); on DSM‐IV, ADI‐R and ADOS in two trials (Wong 2008; Wong 2010b), and on ICD‐10 and the Chinese Classification and Diagnostic Criteria of Mental Disorders version 3 (CCMD‐3) in one trial (Wang 2007). Three studies relied on standardized measures alone: Yan 2007 used the Autism Behavior Checklist, Peabody Picture Vocabulary Test (PPVT) and CARS; Zhou 2008 used the Autism Behavior Checklist alone and the trialists also required that participants had language delay diagnosed by China Rehabilitation Research Center (CRRC) sign‐significance relations scale (Zhou 2008), and Chan 2009 did not describe the means of diagnosis.
Exclusion criteria were reported in only six trials (Wong 2002; Wang 2007; Wong 2007; Wong 2008; Wong 2010a; Wong 2010b). Only one trial provided information on the duration of ASD before entering the trial (Wang 2007). None of the trials reported comorbidities or previous treatments.
Study design
Nine trials used a parallel group design (Wong 2002; Wang 2007; Wong 2007; Yan 2007; Allam 2008; Zhou 2008; Chan 2009; Wong 2010a; Wong 2010b). The remaining trial used a cross‐over design but the two groups were compared only for the initial treatment period and therefore it can also be considered as a parallel group design for the purposes of analysis (Wong 2008).
Intervention
Needle acupuncture was performed in eight trials, including acupuncture to tongue only (Wong 2002; Wong 2007; Wong 2010a) or scalp only (Allam 2008), or involving different parts of the body (Wang 2007; Yan 2007; Wong 2008; Wong 2010b). In three of these trials, the acupoints were stimulated by electric current (electroacupuncture) (Wang 2007, Wong 2008; Wong 2010b). The two remaining trials investigated acupressure without needle puncture (Zhou 2008; Chan 2009). Acupoints chosen were universally applied to all patients in the intervention group in eight trials (Wong 2002; Wang 2007; Wong 2007; Allam 2008; Zhou 2008; Chan 2009; Wong 2010a; Wong 2010b), but with individual variations depending on symptom complex of each patient in two trials (Yan 2007; Wong 2008). In one trial (Allam 2008), acupuncture was applied with the medical acupuncture (scalp acupuncture) paradigm while the remaining nine trials were based on the TCM paradigm.
Duration of treatment ranged from four weeks to nine months. It was uniformly applied to all patients in eight trials (Wong 2002; Wang 2007; Wong 2007; Allam 2008; Wong 2008; Chan 2009; Wong 2010a; Wong 2010b) and variable and individualized in two trials (Yan 2007; Zhou 2008). Duration of follow‐up was variable and ended soon after treatment was completed in all trials.
Comparisons
No study compared either needle acupuncture or acupressure versus no treatment. No study compared either needle acupuncture or acupressure versus sham acupuncture (without conventional treatment). Two studies compared needle acupuncture plus conventional treatment versus sham acupuncture plus conventional treatment (Wong 2010a; Wong 2010b). Six studies compared needle acupuncture plus conventional treatment versus conventional treatment alone (Allam 2008; Wong 2002; Wang 2007; Wong 2007; Yan 2007; Wong 2008). Two studies compared acupressure plus conventional treatment versus conventional treatment alone (Chan 2009; Zhou 2008). The conventional therapy was standardized in only four trials (Wang 2007; Yan 2007; Allam 2008; Zhou 2008). For the remaining six trials, the child's usual individualized therapy was continued throughout the trial period (Wong 2002; Wong 2007; Wong 2008; Chan 2009; Wong 2010a; Wong 2010b).
Outcome Measures
Core features of ASD
Six trials used validated instruments to assess treatment outcomes for different clinical aspects of ASD. Autistic features were assessed by the Ritvo‐Freeman Real Life Scale (RFRLRS) in four trials (Wong 2002; Wong 2008; Wong 2010a; Wong 2010b); the Aberrant Behavior Checklist (ABC) in two trials (Wong 2008; Wong 2010b); the Autism Treatment Evaluation Checklist (ATEC) in two trials (Wong 2007; Wong 2008); the Autism Diagnostic Observation Scale (ADOS) in one trial (Wong 2008); the Autism Behavior Checklist and Social Adaptive Behavior Scale (SABS) in one trial (Wang 2007). One trial also used non‐validated parental report of autistic features as one of the clinical outcome measures (Wong 2010b).
Communication and linguistic ability
Communication and linguistic ability was assessed by the Reynell Developmental Language Scale (RLDS) in three trials (Wong 2007; Wong 2010a; Wong 2010b); the Symbolic Play Test (SPT) in three trials (Wong 2007; Wong 2008; Wong 2010a); the Arabic Language Test (ALT) in one trial (Allam 2008); the Peabody Picture Vocabulary Test (PPVT) in one trial (Wang 2007), and the China Rehabilitation Research Center (CRRC) sign‐significance relations scale in one trial (Zhou 2008).
Cognitive functioning
Cognitive function and overall development was assessed by the Griffith Mental Developmental Scale (GMDS) in one trial (Wong 2010a); the Leiter International Performance Scale‐Revised (Leiter‐R) in one trial (Wong 2010b), and the Chinese version of Psychoeducational Profile (CPEP) in one trial (Yan 2007).
Global functioning
Global functioning was evaluated by the Functional Independence Measure for children (WeeFIM) in five trials (Wong 2002; Wong 2007; Wong 2008; Wong 2010a; Wong 2010b); the Pediatric Evaluation of Disability Inventory (PEDI) in one trial (Wong 2010b), and the Clinical Global Impression Scale (CGIS) in four trials (Wong 2002; Wong 2007; Wong 2008; Wong 2010b). One trial used parent's rating questionnaires, which had not been previously validated, as the sole clinical outcome measure (Chan 2009). One trial reported non‐standardised basic developmental assessment results as one of the outcomes (Zhou 2008).
Adverse effects
Five trials specifically monitored adverse effects of acupuncture (Wong 2002; Wong 2007; Wong 2008; Wong 2010a; Wong 2010b).
Additional outcomes
In addition, Parental Stress Index (PSI) was reported in one trial (Wong 2002). Positron emission tomography (PET) parameters were used to investigate the changes of cerebral 18F‐fluoro‐deoxyglucose (FDG) metabolism in one trial (Wong 2007) and quantitative electroencephalogram (EEG) parameters were used to investigate physiological changes of cerebral cortex in one trial (Chan 2009).
Excluded studies
We excluded seven trials after studying full texts of the papers. Five studies were non‐randomized trials (Ma 2006; Yuan 2007; Wu 2008; Yuan 2009a; Yuan 2009b). We excluded Zhang 2005 and Liu 2008 because they compared acupuncture with other treatments and did not employ a placebo, sham or no treatment control group. The reasons for exclusion of these trials are detailed in the Characteristics of excluded studies table. One trial was published in four records (Zhang 2005). Another trial was published in two papers (Liu 2008) and a third trial was published in three papers (Yuan 2009b).
Risk of bias in included studies
The distribution of risk of bias in different aspects of the included studies is shown in Figure 1 and Figure 2.
1.
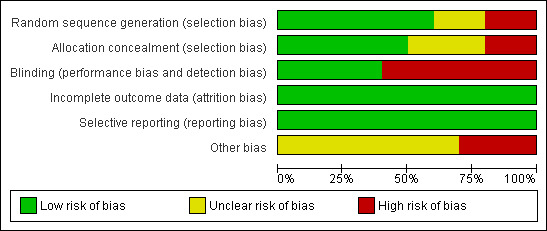
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
2.
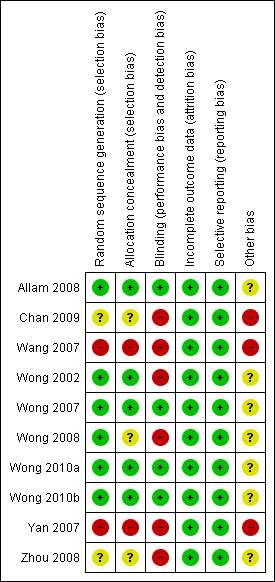
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Among the 10 included RCTs, two were quasi‐randomized clinical trials where allocation was based on sequence of clinic attendance (Wang 2007; Yan 2007) and hence these were judged as being at high risk of bias. The randomization method was not described in two trials (Zhou 2008; Chan 2009) and in one trial (Wong 2008), the randomization sequence was generated by block randomization and it was unclear whether concealment of randomization was adequate or not. The sequence generation and concealment of randomization appeared adequate for the remaining five trials (Wong 2002; Wong 2007; Allam 2008; Wong 2010a; Wong 2010b).
Blinding
One trial explicitly stated that no blinding of therapists or outcome assessors or participants was performed (Chan 2009). Three trials did not report on blinding (Wang 2007; Yan 2007; Zhou 2008) and it was highly likely that therapists and outcome assessors and participants were not blinded as there was no placebo or sham treatment and acupuncture is a salient procedure that is difficult to blind if no specific effort is made. The outcome assessors were blinded to group allocation in the remaining six trials (Wong 2002; Wong 2007; Allam 2008; Wong 2008; Wong 2010a; Wong 2010b). Although the acupuncture therapists were not blinded in these trials, this was unlikely to cause bias as the acupuncturists were not involved in the care of the participants otherwise and they were not involved in outcome assessment. Parents of participants were blinded in three trials (Wong 2007; Wong 2010a; Wong 2010b) and participants were also blinded in two trials with sham control treatment (Wong 2010a; Wong 2010b). Although participants were not blinded in other trials, this was unlikely to cause bias as children with ASD might not fully comprehend the treatment or the trial itself.
Incomplete outcome data
Outcome data were complete in six trials (Wong 2002; Yan 2007; Allam 2008; Zhou 2008; Chan 2009; Wong 2010a). Dropouts with incomplete data occurred in three trials (Wong 2007; Wong 2008; Wong 2010b). Most dropouts were fully accounted for and the reasons given were probably unrelated to treatment assigned. The proportion of missing data was less than 30% in all these trials (Wong 2007; Wong 2008; Wong 2010b). Dropouts were excluded without report of number or reason in one trial (Wang 2007).
Selective reporting
All specified outcomes appear to have been reported in all trials.
Other potential sources of bias
The conventional treatment that participants received was not standardized in six trials ( Wong 2002; Wong 2007; Wong 2008; Chan 2009; Wong 2010a; Wong 2010b) and this might introduce bias as different conventional treatments combined with acupuncture might have different effects. In addition, the acupoints used were variable in one trial (Yan 2007), which might have differential effects and cause bias. Other sources of bias included the electrical stimulation frequency being dependent on syndrome differentiation according to the TCM theory in one trial (Wong 2008); treatment duration varying among participants in two trials (Yan 2007; Zhou 2008), and treatment groups being different at baseline in one trial (Yan 2007). The comparability of the treatment groups at baseline was also questionable in another trial because no baseline characteristics were reported (Allam 2008).
Effects of interventions
For the meta‐analysis on the effects of intervention, we will report only the results of the fixed‐effect model if there is no significant heterogeneity. If there is significant heterogeneity, we report results of both the fixed‐effect and the random‐effects models.
Needle acupuncture plus conventional treatment versus sham acupuncture plus conventional treatment
Two trials reported this comparison (Wong 2010a; Wong 2010b).
Primary outcome
Core features of ASD
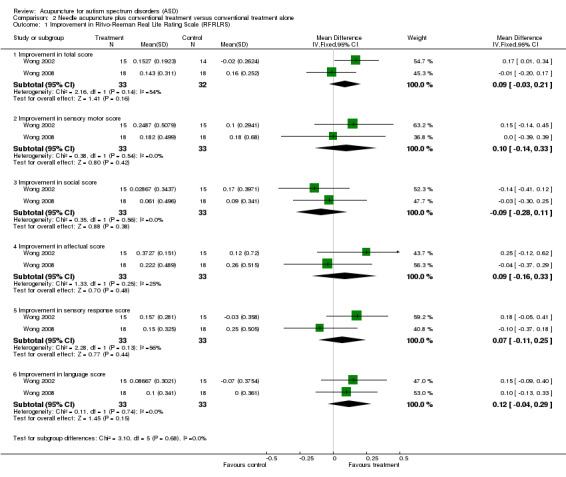
Both trials reported Ritvo‐Freeman Real Life Rating Scale (RFRLRS) (Wong 2010a; Wong 2010b). When their results were combined, there was no significant difference between the intervention and the control groups on total score (MD 0.09; 95% CI ‐0.03 to 0.21, two trials, 105 participants) or any domain score (sensory motor: MD 0.02, 95% CI ‐0.13 to 0.17; social: MD 0.09, 95% CI ‐0.09 to 0.26; sensory response: MD 0.04, 95% CI ‐0.12 to 0.21; affectual: MD 0.14, 95% CI ‐0.07 to 0.34; language: MD 0.11, 95% CI ‐0.02 to 0.24; two trials, 105 participants) (Analysis 1.1; Figure 3).
1.1. Analysis.
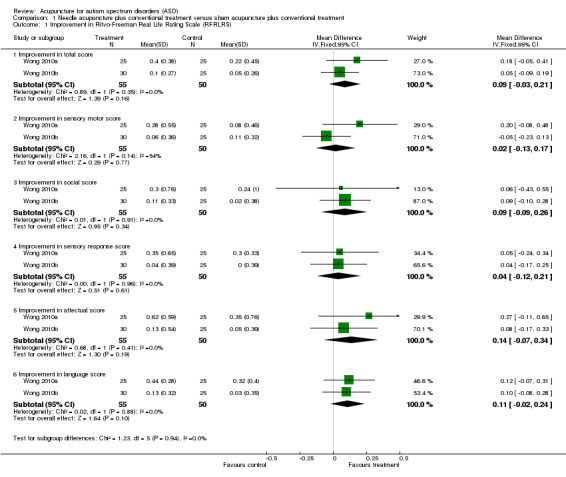
Comparison 1 Needle acupuncture plus conventional treatment versus sham acupuncture plus conventional treatment, Outcome 1 Improvement in Ritvo‐Freeman Real Life Rating Scale (RFRLRS).
3.
Forest plot of comparison 1: Needle acupuncture plus conventional treatment versus sham acupuncture plus conventional treatment; analysis 1.1 ‐ Improvement in Ritvo‐Freeman Real Life Rating Scale (RFRLRS).
One trial reported on the Aberrant Behavior Checklist (ABC), with the results showing no significant difference between the intervention and the control groups in any domain score (irritability: MD 1.00, 95% CI ‐2.16 to 4.16; lethargy: MD 0.63, 95% CI ‐2.78 to 4.04; stereotypy: MD 0.64, 95% CI ‐1.26 to 2.54; hyperactivity: MD 1.1, 95% CI ‐2.25 to 4.45; inappropriate speech: MD 0.05, 95% CI ‐1.00 to 1.10; one trial, 55 participants) (Analysis 1.2).
1.2. Analysis.
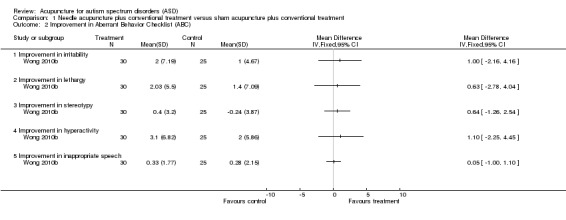
Comparison 1 Needle acupuncture plus conventional treatment versus sham acupuncture plus conventional treatment, Outcome 2 Improvement in Aberrant Behavior Checklist (ABC).
Secondary outcomes
Communication and linguistic ability
Both trials reported Reynell Language Developmental Scale (RDLS) (Wong 2010a; Wong 2010b). When their results were combined, the improvement in comprehension age was significantly higher in the intervention group than in the control group (MD 0.14; 95% CI 0.02 to 0.25, P = 0.02; two trials, 105 participants) (Analysis 1.3). However, there was no significant difference in the expression age between the two groups (MD 0.05, 95% CI ‐0.10 to 0.20; two trials, 105 participants). There is no statistically significant heterogeneity in this outcome between the trials. One trial (Wong 2010a) reported results of Symbolic Play Test (SPT) and there was no significant difference between the two groups (total score: MD 2.20, 95% CI ‐0.35 to 4.75; language age: MD 2.36, 95% CI ‐0.59 to 5.31; one trial, 50 participants) (Analysis 1.4).
1.3. Analysis.
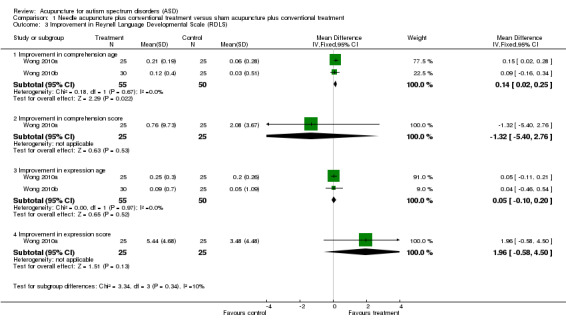
Comparison 1 Needle acupuncture plus conventional treatment versus sham acupuncture plus conventional treatment, Outcome 3 Improvement in Reynell Language Developmental Scale (RDLS).
1.4. Analysis.
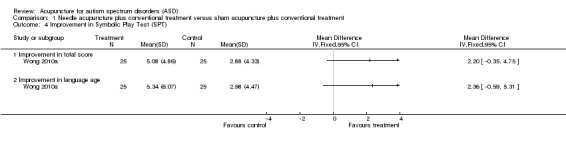
Comparison 1 Needle acupuncture plus conventional treatment versus sham acupuncture plus conventional treatment, Outcome 4 Improvement in Symbolic Play Test (SPT).
Cognitive function
One trial (Wong 2010a) reported results of Griffiths Mental Developmental Scale (GMDS) and there was no significant difference between the intervention and the control groups in any of the domain scores (general quotient: MD 3.46, 95% CI ‐2.00 to 8.92; mental age: MD 2.54, 95% CI ‐0.67 to 5.75; locomotor: MD ‐1.20, 95% CI ‐4.45 to 2.05; personal‐social: MD 3.36, 95% CI ‐0.08 to 6.80; hearing and speech: MD 1.33, 95% CI ‐3.39 to 6.05; eye hand coordination: MD 1.08, 95% CI ‐3.88 to 6.04; performance: MD 4.92, 95% CI ‐1.69 to 11.53; practical reasoning: MD 5.92, 95% CI ‐4.02 to 15.86; one trial, 50 participants) (Analysis 1.5).
1.5. Analysis.
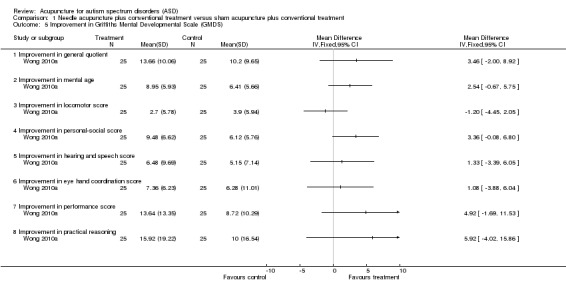
Comparison 1 Needle acupuncture plus conventional treatment versus sham acupuncture plus conventional treatment, Outcome 5 Improvement in Griffiths Mental Developmental Scale (GMDS).
Another trial (Wong 2010b) reported results of Leiter International Performance Scale‐Revised (Leiter‐R) and there was no significant difference between the intervention and the control groups in any of the domain scores (visualization and reasoning full IQ: MD 1.26, 95% CI ‐4.29 to 6.81; attention and memory composite score: MD ‐0.31, 95% CI ‐4.73 to 4.11; visualization and reasoning growth composite score: MD 5.73, 95% CI ‐3.99 to 15.45; attention and memory growth composite score: MD ‐0.21, 95% CI ‐8.99 to 8.57; one trial, 55 participants) (Analysis 1.6).
1.6. Analysis.
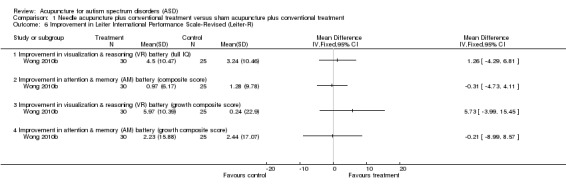
Comparison 1 Needle acupuncture plus conventional treatment versus sham acupuncture plus conventional treatment, Outcome 6 Improvement in Leiter International Performance Scale‐Revised (Leiter‐R).
Global functioning
Both trials reported Functional Independent Measure of children (WeeFIM) as a measure of global functioning (Wong 2010a; Wong 2010b). When their results were combined, the intervention group showed greater improvement in total score (fixed‐effect model, MD 3.31; 95% CI 1.40 to 5.22, P = 0.0007; two trials, 105 participants) and self‐care domain score (fixed‐effect model, MD 2.15; 95% CI 0.82 to 3.49, P = 0.002; 2 trials, 105 participants) and cognition (fixed‐effect model, MD 0.70; 95% CI 0.09 to 1.30, P = 0.02; 2 trials, 105 participants) compared to the control group (Analysis 1.7). However, there was significant statistical heterogeneity between the two trials in total score and self‐care score, and the difference between the two groups in these scores were not statistically significant using the random‐effects model (total score: MD 3.08, 95% CI ‐0.61 to 6.71; self‐care: MD 2.10, 95% CI ‐0.69 to 4.88; two trials, 105 participants).
1.7. Analysis.
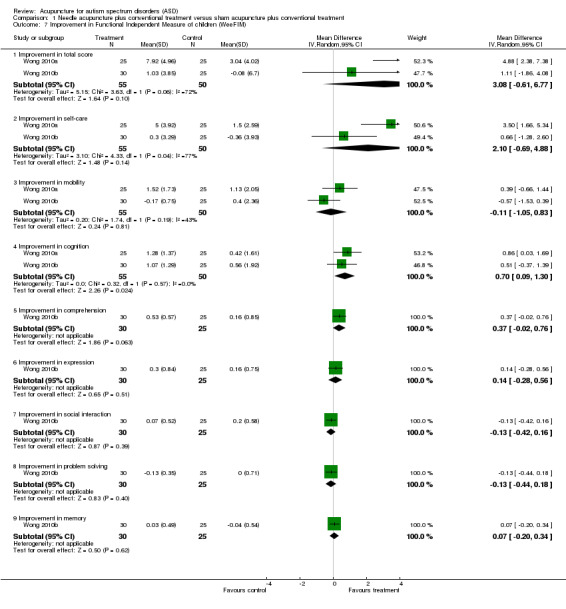
Comparison 1 Needle acupuncture plus conventional treatment versus sham acupuncture plus conventional treatment, Outcome 7 Improvement in Functional Independent Measure of children (WeeFIM).
One trial (Wong 2010b) also reported results of Pediatric Evaluation of Disability Inventory (PEDI) and there was significantly greater improvement in self‐care (caregiver assistance scale: MD 1.97; 95% CI 0.02 to 3.92, P = 0.05; one trial, 55 participants) and social function (caregiver assistance scale: MD 3.91, 95% CI 2.20 to 5.62, P < 0.00001; one trial, 55 participants) in the intervention group compared to the control group (Analysis 1.8). In addition, the same trial (Wong 2010b) reported results of Clinical Global Impression Scale (CGIS) and there were significantly more patients in the intervention group who experienced more than or equal to 25% improvement compared to the control group (RR 1.50; 95% CI 1.07 to 2.11, P = 0.02; one trial, 55 participants) (Analysis 1.9).
1.8. Analysis.
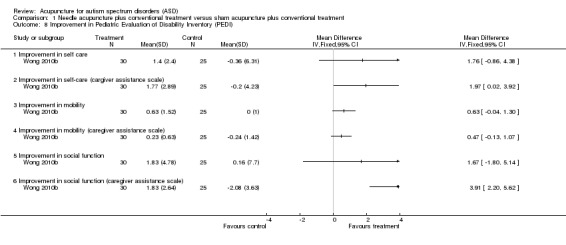
Comparison 1 Needle acupuncture plus conventional treatment versus sham acupuncture plus conventional treatment, Outcome 8 Improvement in Pediatric Evaluation of Disability Inventory (PEDI).
1.9. Analysis.
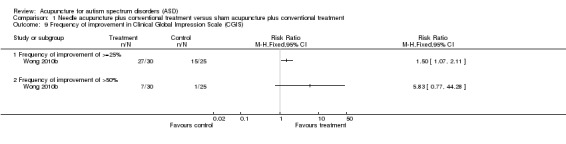
Comparison 1 Needle acupuncture plus conventional treatment versus sham acupuncture plus conventional treatment, Outcome 9 Frequency of improvement in Clinical Global Impression Scale (CGIS).
Quality of life
Neither trial reported this outcome.
Adverse effects
One trial reported initial crying for fear and possible pain occurring in the first few sessions (Wong 2010a). No information was available on the number of participants who experienced these adverse effects or whether there was any difference between the intervention and the control groups. The other trial reported that some participants experienced superficial bleeding or crying and irritability during acupuncture (Wong 2010b).
Needle acupuncture plus conventional treatment versus conventional treatment alone
Six trials reported this comparison (Allam 2008; Wong 2002; Wang 2007; Wong 2007; Yan 2007; Wong 2008).
Primary outcome
Core features of ASD
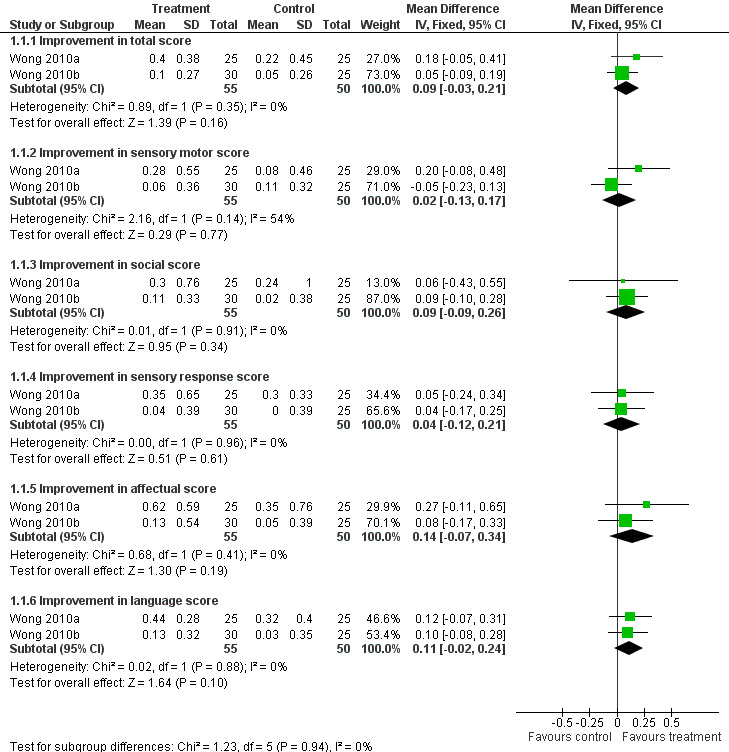
Two trials reported Ritvo‐Reeman Real Life Rating Scale (RFRLRS) (Wong 2002; Wong 2008). When their results were combined, there was no significant difference between the intervention and the control groups in total score (MD 0.09; 95% CI ‐0.03 to 0.21; 2 trials, 65 participants) or any domain score (sensory motor: MD 0.10, 95% CI ‐0.14 to 0.33; social: MD ‐0.09, 95% CI ‐0.28 to 0.11; affectual: MD 0.09, 95% CI ‐0.16 to 0.33; sensory response: MD 0.07, 95% CI ‐0.11 to 0.25; language: MD 0.12, 95% CI ‐0.04 to 0.29; two trials, 65 participants) (Analysis 2.1; Figure 4).
2.1. Analysis.
Comparison 2 Needle acupuncture plus conventional treatment versus conventional treatment alone, Outcome 1 Improvement in Ritvo‐Reeman Real Life Rating Scale (RFRLRS).
4.
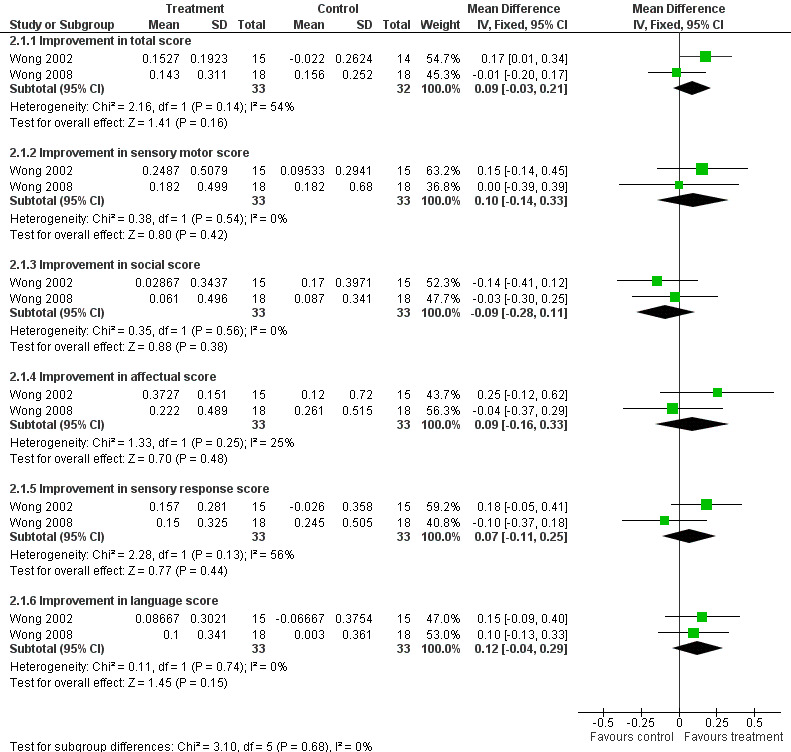
Forest plot of comparison 2: Needle acupuncture plus conventional treatment versus conventional treatment alone; analysis 2.1 ‐ Improvement in Ritvo‐Reeman Real Life Rating Scale (RFRLRS).
Two trials reported Autism Treatment Evaluation Checklist (ATEC) (Wong 2007; Wong 2008). The pooled results showed no significant difference between the intervention and the control groups in total score (MD 6.28; 95% CI ‐0.15 to 13.61; two trials, 57 participants) or any domain score (communication and speech: MD 1.43, 95% CI ‐0.21 to 3.07; sociability: MD 1.82, 95% CI ‐1.39 to 5.03; sensory and cognitive awareness: MD 2.48, 95% CI ‐0.04 to 5.00; physical health and behavior: MD 0.49, 95% CI ‐1.95 to 2.93; two trials, 57 participants) (Analysis 2.2; Figure 5). As a sensitivity analysis excluding Wong 2008 because of its high risk of bias, the result of the remaining study (Wong 2007) indicated that the intervention group had greater Improvement in communication and speech score (MD 2.84; 95% CI 0.61 to 5.07, P = 0.01; one trial, 21 participants)
2.2. Analysis.
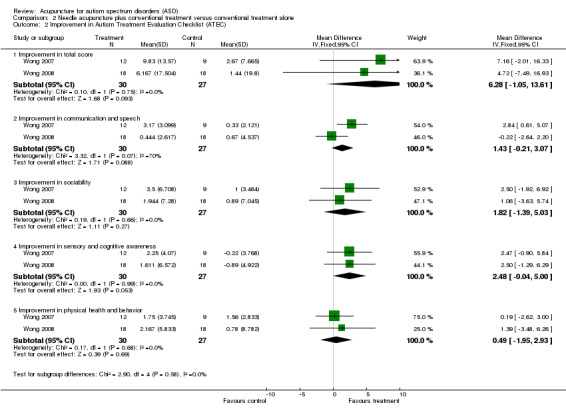
Comparison 2 Needle acupuncture plus conventional treatment versus conventional treatment alone, Outcome 2 Improvement in Autism Treatment Evaluation Checklist (ATEC).
5.
Forest plot of comparison 2: Needle acupuncture plus conventional treatment versus conventional treatment alone; analysis 2.2 ‐ Improvement in Autism Treatment Evaluation Checklist (ATEC).
One trial reported Aberrant Behavior Cheklist (ABC) (Wong 2008) and found no significant difference between the intervention and the control groups in total score (MD 6.06; 95% CI ‐7.05 to 19.16; one trial, 36 participants) or any domain score (irritability: MD 2.78, 95% CI ‐1.42 to 6.98; lethargy: MD 1.61, 95% CI ‐2.79 to 6.01; stereotypy: MD 0.86, 95% CI ‐1.06 to 2.79; hyperactivity: MD 0.47, 95% CI ‐5.33 to 4.38; inappropriate speech: MD 1.28, 95% CI ‐0.12 to 2.68; one trial, 36 participants) (Analysis 2.3). The same trial also found no significant difference in Autism Diagnostic Observation Scale (ADOS) between the intervention and the control groups (communication: MD ‐0.33, 95% CI ‐1.44 to 0.77; social interaction: MD 0.00, 95% CI ‐1.44 to 1.44; one trial, 36 participants) (Analysis 2.4).
2.3. Analysis.
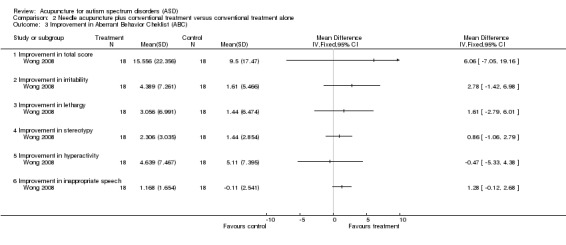
Comparison 2 Needle acupuncture plus conventional treatment versus conventional treatment alone, Outcome 3 Improvement in Aberrant Behavior Cheklist (ABC).
2.4. Analysis.
Comparison 2 Needle acupuncture plus conventional treatment versus conventional treatment alone, Outcome 4 Improvement in Autism Diagnostic Observation Scale (ADOS).
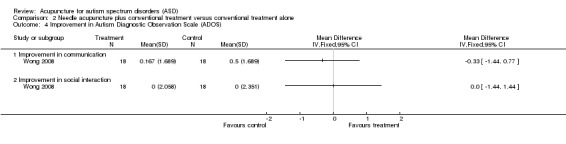
One trial reported Autism Behavior Checklist (Wang 2007). Significantly more patients in the intervention group showed improvement compared to the control group (RR 1.53; 95% CI 1.09 to 2.16, P = 0.02; one trial, 60 participants) (Analysis 2.5). The intervention group also showed significantly lower post‐treatment total score (indicating better outcomes) (MD ‐5.53; 95% CI ‐10.76 to ‐0.31, P = 0.04; one trial, 60 participants) and scores in the sensory domain (MD ‐2.23; 95% CI ‐4.08 to ‐0.39, P = 0.02; one trial, 60 participants), physical domain (MD ‐1.87; 95% CI ‐3.55 to ‐0.19, P = 0.03; one trial, 60 participants) and self‐care domain (MD ‐2.00; 95% CI ‐3.57 to ‐0.44, P = 0.01; one trial, 60 participants) compared to the control group (Analysis 2.6). The same trial (Wang 2007) also reported results of Social Adaptive Behavior Scale (SABS) and significantly more patients in the intervention group showed improvement compared to the control group (RR 3.33; 95% CI 1.02 to 10.92, P = 0.05; one trial, 60 participants) (Analysis 2.7). The intervention group also showed significantly greater improvement in the SABS score compared to the control group (MD 2.95; 95% CI 0.47 to 5.43, P = 0.02; one trial, 60 participants) (Analysis 2.8). However, this trial was excluded in sensitivity analysis because of its high risk of bias.
2.5. Analysis.
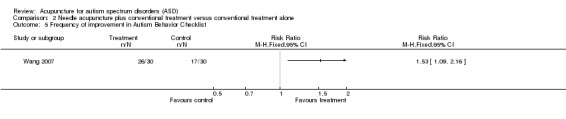
Comparison 2 Needle acupuncture plus conventional treatment versus conventional treatment alone, Outcome 5 Frequency of improvement in Autism Behavior Checklist.
2.6. Analysis.
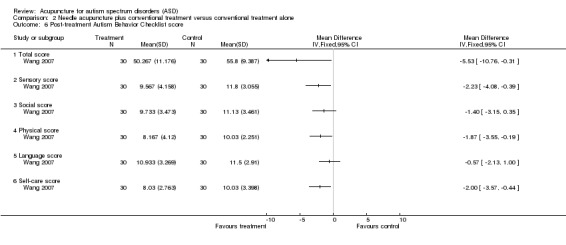
Comparison 2 Needle acupuncture plus conventional treatment versus conventional treatment alone, Outcome 6 Post‐treatment Autism Behavior Checklist score.
2.7. Analysis.
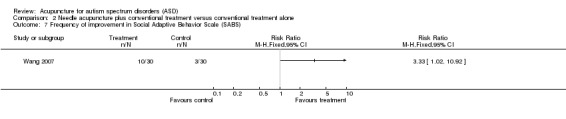
Comparison 2 Needle acupuncture plus conventional treatment versus conventional treatment alone, Outcome 7 Frequency of improvement in Social Adaptive Behavior Scale (SABS).
2.8. Analysis.
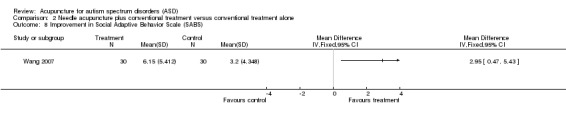
Comparison 2 Needle acupuncture plus conventional treatment versus conventional treatment alone, Outcome 8 Improvement in Social Adaptive Behavior Scale (SABS).
Secondary outcomes
Communication and linguistic ability
Two trials reported Symbolic Play Test (SPT) (Wong 2007; Wong 2008). The pooled results showed no significant difference between the intervention and the control groups in the total score (MD 0.77, 95% CI ‐0.83 to 2.37, two trials, 57 participants) (Analysis 2.9). One of these 2 trials (Wong 2007) also reported the language age and found no difference between the intervention and the control groups (MD 1.88, 95% CI ‐0.70 to 4.46, one trial, 21 participants) (Analysis 2.9).
2.9. Analysis.
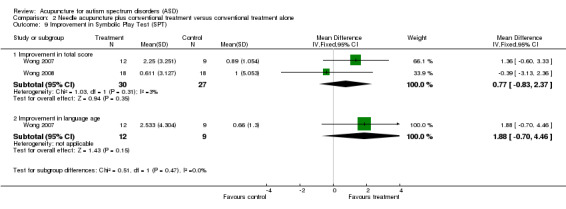
Comparison 2 Needle acupuncture plus conventional treatment versus conventional treatment alone, Outcome 9 Improvement in Symbolic Play Test (SPT).
One trial reported Reynell Language Developmental Scale (RLDS) (Wong 2007) and found no significant difference between the intervention and the control groups (comprehension age: MD 0.45, 95% CI ‐0.17 to 1.07; comprehension score: MD 1.69, 95% CI ‐1.55 to 4.94; expression age: MD 0.57, 95% CI ‐0.08 to 1.22; expression score: MD 1.28, 95% CI ‐2.79 to 5.35; one trial, 21 participants) (Analysis 2.10). One trial reported Arabic Language Test (ALT) (Allam 2008) and found no significant difference between the intervention and the control groups in any of the domain scores (attention: MD 0.30, 95% CI ‐0.40 to 1.00; receptive semantics: MD 2.4, 95% CI ‐0.64 to 5.44; expressive semantics: MD ‐0.30, 95% CI 3.28 to 2.68; one trial, 20 participants) (Analysis 2.11). Another trial reported Peabody Picture Vocabulary Test (PPVT) (Wang 2007) and found no significant difference between the intervention and the control groups (MD 5.37; 95% CI ‐1.04 to 11.78; one trial, 60 participants) (Analysis 2.12).
2.10. Analysis.
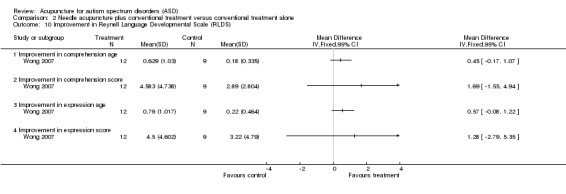
Comparison 2 Needle acupuncture plus conventional treatment versus conventional treatment alone, Outcome 10 Improvement in Reynell Language Developmental Scale (RLDS).
2.11. Analysis.
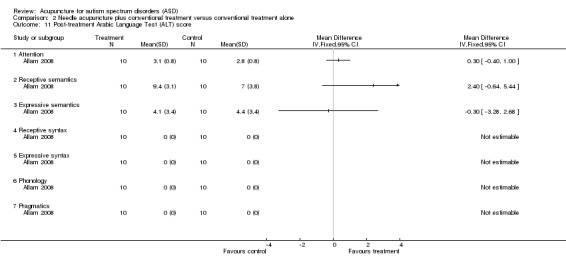
Comparison 2 Needle acupuncture plus conventional treatment versus conventional treatment alone, Outcome 11 Post‐treatment Arabic Language Test (ALT) score.
2.12. Analysis.
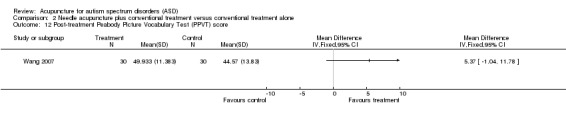
Comparison 2 Needle acupuncture plus conventional treatment versus conventional treatment alone, Outcome 12 Post‐treatment Peabody Picture Vocabulary Test (PPVT) score.
Cognitive function
One trial (Yan 2007) reported Chinese version of Psychoeducational Profile (CPEP), which is a validated score of developmental and cognitive function, with 100 points indicating age‐appropriate performance level. There were significantly more patients in the intervention group who experienced improvement of more than or equal to 16 points (RR 3.67; 95% CI 1.20 to 11.19, P = 0.02; one trial, 40 participants) or eight points of improvement (RR 1.80; 95% CI 1.13 to 2.86, P = 0.01; one trial, 40 participants) compared to the control group (Analysis 2.13). The intervention group showed greater improvement in total score (MD 10.75, 95% CI 3.82 to 17.68, P = 0.002; one trial, 40 participants), and scores of imitation (MD 18.25, 95% CI 10.18 to 26.32, P < 0.00001; one trial, 40 participants) and speech (MD 19.15, 95% CI 6.78 to 31.52, P = 0.002; one trial, 40 participants) compared to the control group (Analysis 2.14). However, this trial was excluded in sensitivity analysis because of high risk of bias.
2.13. Analysis.
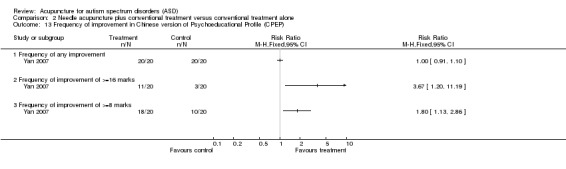
Comparison 2 Needle acupuncture plus conventional treatment versus conventional treatment alone, Outcome 13 Frequency of improvement in Chinese version of Psychoeducational Profile (CPEP).
2.14. Analysis.
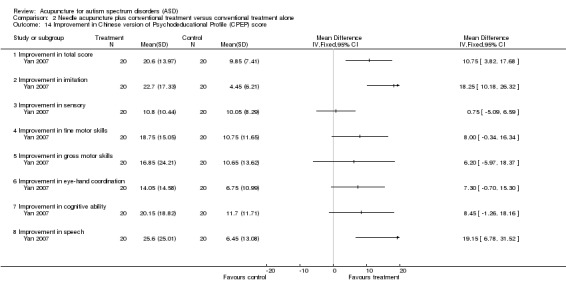
Comparison 2 Needle acupuncture plus conventional treatment versus conventional treatment alone, Outcome 14 Improvement in Chinese version of Psychodeducational Profile (CPEP) score.
Global functioning
Three trials reported Functional Independence Measure of Children (WeeFim) (Wong 2002; Wong 2007; Wong 2008). When their results were combined, there was significantly greater improvement in total score (fixed‐effect model, MD 4.34; 95% CI 2.79 to 5.89, P < 0.00001; three trials, 85 participants); self‐care score (fixed‐effect model; MD 2.50; 95% CI 0.48 to 4.52, P = 0.02; three trials, 85 participants) and cognition score (fixed‐effect model, MD 3.92; 95% CI 2.13 to 5.72, P < 0.00001; three trials, 85 participants) in the intervention group compared to the control group (Analysis 2.15). However, there was significant statistical heterogeneity in these outcomes between the three trials. Only the cognition score remained significantly different between the two groups in the random‐effects model (MD 5.19; 95% CI 0.03 to 10.34, P = 0.05; three trials, 85 participants). In a sensitivity analysis, when two trials with high risk of bias were removed (Wong 2002; Wong 2008), the remaining trial (Wong 2007) revealed that the intervention group had greater Improvement in total score (MD 4.09; 95% CI 2.15 to 6.03, P < 0.0001; one trial, 21 participants), self‐care score (MD 4.10; 95% CI 0.67 to 7.52, P = 0.02; one trial, 21 participants), and cognition score (MD 8.38; 95% CI 4.41 to 12.35, P < 0.0001; one trial, 21 participants) (Analysis 2.16).
2.15. Analysis.
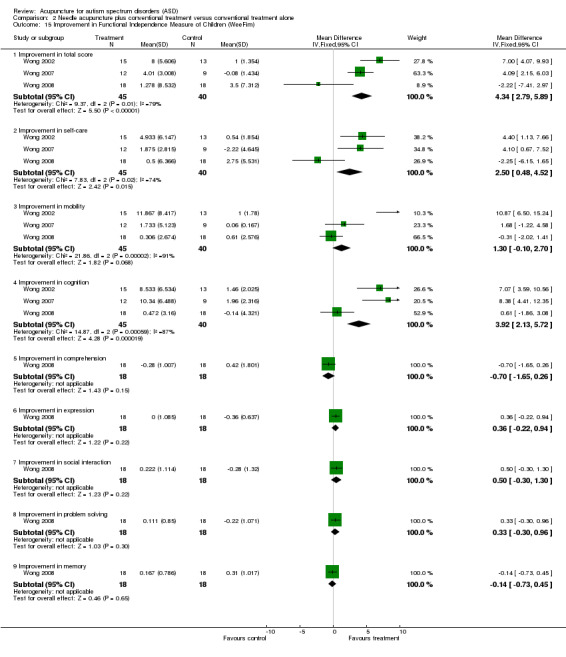
Comparison 2 Needle acupuncture plus conventional treatment versus conventional treatment alone, Outcome 15 Improvement in Functional Independence Measure of Children (WeeFim).
2.16. Analysis.
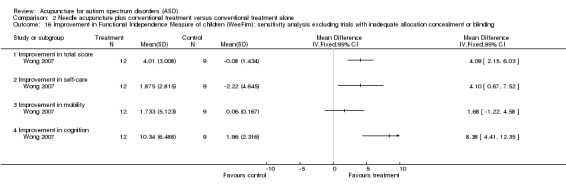
Comparison 2 Needle acupuncture plus conventional treatment versus conventional treatment alone, Outcome 16 Improvement in Functional Independence Measure of children (WeeFim): sensitivity analysis excluding trials with inadequate allocation concealment or blinding.
One trial reported Clinical Global Impression Scale (CGIS) (Wong 2008) and found that the intervention group had significantly lower CGIS score (indicating a better outcome) compared to the control group (MD ‐0.61; 95% CI ‐1.05 to ‐0.17, P = 0.006; one trial, 36 participants) (Analysis 2.17). Another trial (Wong 2002) reported that repetitive behavior was significantly better in the intervention group compared to the control group (MD ‐0.80; 95% CI ‐1.30 to ‐0.30, P = 0.002; 1 trial, 30 participants) (Analysis 2.17). A third trial (Wong 2007) showed that significantly more patients in the intervention group showed better CGIS compared to the control group (RR 3.85; 95% CI 1.31 to 11.31, P = 0.01; one trial, 21 participants) (Analysis 2.18). In a sensitivity analysis, the first two trials were excluded (Wong 2002; Wong 2008) because of high risk of bias.
2.17. Analysis.
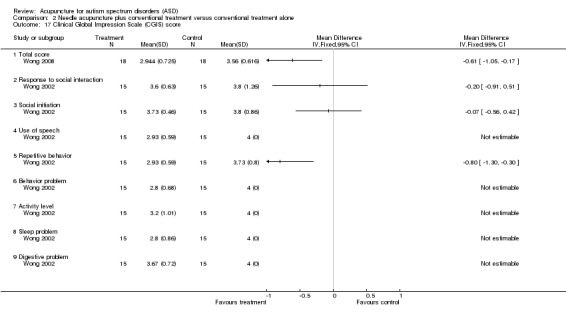
Comparison 2 Needle acupuncture plus conventional treatment versus conventional treatment alone, Outcome 17 Clinical Global Impression Scale (CGIS) score.
2.18. Analysis.
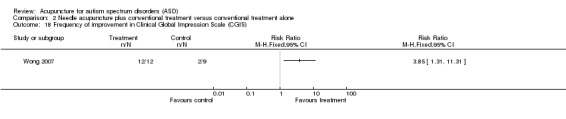
Comparison 2 Needle acupuncture plus conventional treatment versus conventional treatment alone, Outcome 18 Frequency of improvement in Clinical Global Impression Scale (CGIS).
Quality of life
None of the six trials reported this outcome.
Adverse effects
Three trials did not report any adverse effects (Wang 2007; Yan 2007; Allam 2008). Two trials reported initial crying for fear and possible pain occurring in the first few sessions of acupuncture (Wong 2002; Wong 2007). However, most children adapted easily and tolerated the technique well. There was no information on the number of participants who experienced these adverse effects or whether there was difference between the intervention and the control groups. One trial reported worsening of sleeping pattern (sleeping late at night, usually during holidays) in one participant in the intervention group (Wong 2008). Another child in the intervention group showed worsening of hyperactivity and ritualistic behavior, but at the same time he had improvement in expressive language and meaningful vocalization. The parents thought that the negative changes were minor and did not affect the child's functioning.
Acupressure plus conventional treatment versus conventional treatment alone
Two trials reported this comparison (Zhou 2008; Chan 2009).
Primary outcome
Core features of ASD
Neither trial reported on our primary outcome.
Secondary outcomes
Communication and linguistic ability
One trial reported China Rehabilitation Research Council (CRRC) sign‐significance relations scale (Zhou 2008) and found that the intervention group had significantly more patients who achieved a better score in the domain of communication attitude compared to the control group (RR 1.64; 95% CI 1.02 to 2.63, P = 0.04; 1 trial, 30 participants) (Analysis 3.1). However, there was no significant difference in overall improvement (MD 1.31; 95% CI 0.92 to 1.87; one trial, 30 participants) or in other domains between the two groups. This trial was at high risk of bias.
3.1. Analysis.
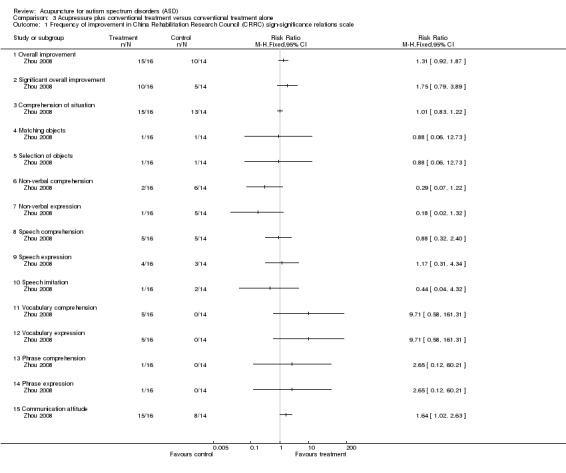
Comparison 3 Acupressure plus conventional treatment versus conventional treatment alone, Outcome 1 Frequency of improvement in China Rehabilitation Research Council (CRRC) sign‐significance relations scale.
Cognitive function
One trial (Zhou 2008) reported basic developmental assessment results. Significantly more patients in the intervention group showed improvement in non‐verbal comprehension (RR 1.64; 95% CI 1.02 to 2.63, P = 0.04; 1 trial, 30 participants) and matching (RR 1.88; 95% CI 1.09 to 3.21, P = 0.02; 1 trial, 30 participants) compared to the control group (Analysis 3.2). However, there was no significant difference in other developmental aspects between the two groups. In a sensitivity analysis, this trial was excluded because of high risk of bias.
3.2. Analysis.
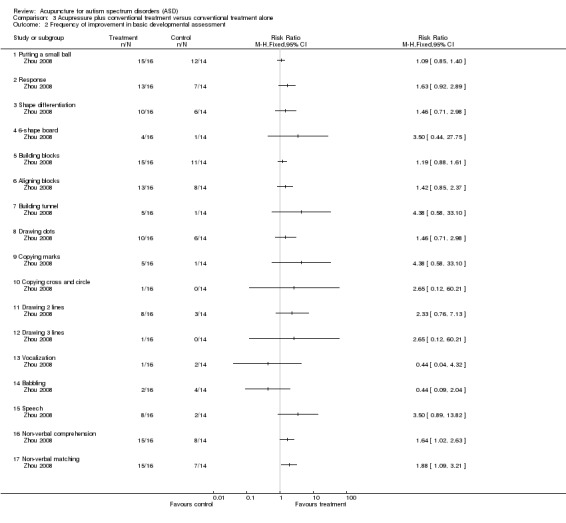
Comparison 3 Acupressure plus conventional treatment versus conventional treatment alone, Outcome 2 Frequency of improvement in basic developmental assessment.
Global functioning
One trial (Chan 2009) reported results of the Parents' Rating Questionnaire that the intervention group had significantly greater overall improvement (MD 0.56; 95% CI 0.15 to 0.97, P = 0.007; one trial, 32 participants) and improvements in language (MD 0.78, 95% CI 0.38 to 1.18, P=0.0001; one trial, 32 participants) and social interaction (MD 0.65, 95% CI 0.20 to 1.10, P=0.004; one trial, 32 participants) compared to the control group (Analysis 3.3). This trial was at high risk of bias.
3.3. Analysis.
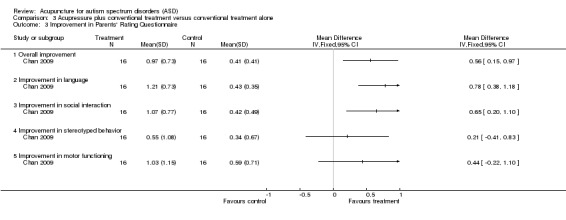
Comparison 3 Acupressure plus conventional treatment versus conventional treatment alone, Outcome 3 Improvement in Parents' Rating Questionnaire.
Quality of life
Neither trial reported on this outcome.
Adverse effects
The two trials did not report any adverse effects (Chan 2009; Zhou 2008).
Discussion
Summary of main results
All the trials in the current review involved children only and therefore the results are relevant to children only. Three of ten included studies applied acupuncture to the tongue only. This is a specialized technique that may not be readily applicable to many societies where acupuncture is practised. We found that acupuncture might result in improvement in some outcomes in children with ASD. When needle acupuncture (by manual or electrical stimulation) plus conventional treatment was compared to sham acupuncture plus conventional treatment, the intervention seemed to result in better language comprehension (by RDLS, pooled result of two trials), cognition (by WeeFIM, pooled result of two trials), self‐care (by PEDI, single trial), social function (by PEDI, single trial) and a higher likelihood of greater than or equal to 25% improvement in global function (by CGIS, single trial). Compared to conventional treatment alone, needle acupuncture plus conventional treatment might result in overall improvement in autistic features (by Autism Behavior Checklist and SABS, single trials), speech (by CPEP, single trial), cognition (by CPEP in single trial and by WeeFim in three trials), global functioning (by CGIS in three trials), self‐care (by Autism Behavior Checklist, single trial), sensory functioning (by Autism Behavior Checklist, single trial), imitation (by CPEP, single trial), repetitive behavior (by CGIS, single trial), and physical health (by Autism Behavior Checklist, single trial). Compared to conventional treatment alone, acupressure plus conventional treatment might result in improvement in overall global functioning (by parent's rating, single trial), communication attitude (by CRRC sign‐significance relations scale, single trial), non‐verbal communication and matching (by basic developmental assessment, single trial), and language and social interaction (by parent rating, single trial).
A majority of the favorable outcomes of acupuncture were demonstrated by single trials only and few outcomes were supported by a pooled result of more than one trial. Moreover, most effect size estimates for the above significant outcomes were not precise and had large confidence intervals, whether they were based on single or multiple trials (i.e., two or three). In addition, the results were not entirely consistent within and across different studies as different scales measuring the same attribute gave different results in the included studies. For some outcomes measured on the same scales, there was significant statistical heterogeneity and the combined effect estimate was not statistically significant when the random‐effects model was used instead of the fixed‐effect model. This indicated that the significant result was not sufficiently robust to enable a firm conclusion. In addition, a large number of comparisons were made for different subscores in many different domains in many different outcome scales, which would inflate the risk that certain outcomes were significant just by chance, especially if there was just borderline significance with the P value close to 0.05. Therefore, some of the significant results listed above might represent false positive results. When the results were scrutinized by precision of estimates, consistency within and across different studies, absence of significant heterogeneity and highly significant P value, none of the above significant results impressed as showing a significant and reliable beneficial effect from acupuncture.
Overall completeness and applicability of evidence
There were only 10 randomized controlled trials investigating the use of acupuncture in people with ASD. They recruited small numbers of participants (20 to 60), who were all children. None of the trials provided calculation of sample size before initiation of recruitment. As a result, the trials probably had insufficient statistical power to detect significant differences between the intervention and the control groups and are therefore prone to false negative results. Since the trials were all heterogeneous with respect to study design (presence or absence of sham control); participants (different age groups with variable diagnostic criteria and severity of ASD); acupuncture methods (needle acupuncture or acupressure, manual or device or electrical stimulation, different acupoints in different parts of the body); duration of treatment; co‐interventions (different types of conventional education program or behavior therapy in different settings), and outcome measures (variable tools measuring different aspects), only a few outcome measures in a few trials could be combined in meta‐analyses, which hopefully might have increased the statistical power. However, the results were still quite heterogeneous and no robust conclusions could be drawn. In addition, many of these significant results had low precision and were not consistent within or across studies and therefore no reliable conclusion about the efficacy of acupuncture could be made.
Furthermore, existing RCTs were of short duration and short follow‐up. It is uncertain whether the possible short‐term effects of acupuncture could be maintained in the long term with or without continuous acupuncture treatment. Since the behavioral symptoms of ASD could vary day by day or evolve with the growth and development of the child, a single assessment at the end of treatment in all the included trials might not fully reflect the effect of acupuncture.
On the other hand, adverse effects of pain and irritability were common although major adverse effects were not reported in the trials. There is no evidence that acupuncture might worsen symptoms of ASD. However, rare adverse effects might not be detected in trials with a small number of participants.
In conclusion, the existing evidence on the effectiveness of acupuncture for treatment of ASD is far from complete. It remains uncertain whether acupuncture is effective or not; which form of acupuncture (needle acupuncture or acupressure) is more likely to be effective; how acupuncture should be delivered (appropriate acupoints, method of stimulation, frequency and duration of therapy), and what types of ASD patients would most likely benefit. However, acupuncture is unlikely to worsen ASD and adverse effects are usually mild.
Quality of the evidence
The methodological quality of the included trials is variable and none is considered to be free of significant bias. Important potential biases in the included studies included problems in sequence generation, which might be just quasi‐randomization instead of genuine randomization (Wang 2007; Yan 2007). Allocation concealment was absent or unclear in some trials (Wang 2007; Yan 2007; Wong 2008; Zhou 2008; Chan 2009). Blinding of outcome assessors was not attempted or was unclear in several trials (Wang 2007; Yan 2007; Zhou 2008; Chan 2009). Many trials did not include a placebo or sham control group and therefore the placebo effect could not be excluded (Wong 2002; Wang 2007; Wong 2007; Yan 2007; Allam 2008; Wong 2008; Zhou 2008; Chan 2009). Baseline characteristics might not be comparable in several trials (Yan 2007; Allam 2008), making comparisons of outcomes prone to bias. Acupuncture methods used were not standardized within the intervention or the control group in some trials (Yan 2007; Wong 2008; Zhou 2008), nor were different methods stratified within a treatment group, making it difficult to draw conclusions about effectiveness of a particular acupuncture protocol. In addition, the conventional treatments used in some trials were not standardized (Wong 2002; Wong 2007; Wong 2008; Chan 2009; Wong 2010a; Wong 2010b) and might have enormous individual variations, which would mask or bias the results.
Potential biases in the review process
We searched extensively in the international and Chinese literature. Some studies that were not published in English or Chinese and not reached by our search strategies might have been missed. Publication bias was also possible.
Other review authors may have chosen to categorise the study comparisons differently (see Methods:Types of interventions). Our view is that although some of our comparisons are similar, there are important differences. Because we cannot exclude the presence of synergistic effect if acupuncture is used with certain medications and it is possible that acupuncture is not effective when used alone but is effective when used with medications, we chose to separate comparisons 1 and 3, and comparisons 2 and 4. In addition, although all comparisons are between acupuncture and no acupuncture (i.e., all lie within the scope of current review), a placebo effect might be prominent and hence comparisons with placebo might be quite different from comparisons with no treatment, which is why we chose to separate comparisons 1 and 2, and comparisons 3 and 4.
Other review authors may also have made different decisions concerning how to combine the data. We considered carefully whether we could combine results of different assessment tools for the primary outcome of 'core features of ASD'. However, we thought that the combined results might be misleading clinically as the outcome measures (i.e., different assessment tools) were designed to measure different behaviors, which are complex, and the tools have different components and constructs. They are clinically very heterogeneous and therefore we concluded that we should not combine the different scales using standardized mean differences.
Agreements and disagreements with other studies or reviews
As far as we know, this is the first systematic review of acupuncture therapy for ASD. In 2009, there was a review (Rossignol 2009) for novel and emerging treatments for ASD and it concluded that acupuncture was considered a grade 'C' recommendation for ASD, indicating that it was supported by at least one non‐randomized controlled trial or two case series studies. Although some RCTs were published after that review, there is still no sufficient evidence to support acupuncture for ASD at present.
Authors' conclusions
Implications for practice.
There is no evidence within this review that any form of acupuncture is effective in the treatment of ASD. We cannot rule out that certain forms of acupuncture might ameliorate certain aspects of ASD in some patients. However, it is not known what types of patients will benefit from what types of acupuncture therapy. Adverse effects are usually mild but severe adverse effects might also occur rarely. Parents who intend to let their children with ASD receive acupuncture need to be counseled adequately on the uncertain benefits and potential risks.
Implications for research.
Further high quality studies with larger sample sizes are needed. Sample size should be calculated before participant recruitment and adequate sample size should be obtained to increase power. The randomization method used should be rigorous and concealed. Although blinding of the therapist applying acupuncture is difficult, blinding of the parents, the other care providers and outcome assessors should be attempted in order to minimise performance and assessment biases. Since ASD is heterogeneous with other associated problems, it is difficult to be certain about the efficacy of therapies. Therefore, validated diagnostic tools and outcome measures should be used and should ideally be administered by assessors not involved in the usual care of the patients. As acupuncture might be beneficial only for some but not all autistic features, it is important to have detailed assessment of different features of autism and different intellectual, behavioral and functional domains. Sham or placebo control should be used as far as possible to minimize placebo effect. If different acupuncture protocols are involved because of variations in severity, symptom complexity or disease categorization based on TCM theories, it is important to recruit more patients and stratify them for randomization, or restrict the trial to a homogeneous group of patients to evaluate a single acupuncture protocol, so that effectiveness of a particular acupuncture method can be ascertained. The conventional treatment that is to be combined with acupuncture should be standardized as far as possible to minimise confounding the acupuncture effect. Although it is almost unavoidable to have individualized elements in all education or behavioral programs, attempts should be made to recruit patients in similar programs provided by a small number of educators or therapists in the same setting to minimise variations. Since ASD is a lifelong disorder with symptom fluctuations or evolution with time, a longer follow‐up period with serial measurements of outcomes is also important to determine the genuine efficacy of acupuncture and its long‐term effects. RCTs should also be performed in adults with ASD.
What's new
| Date | Event | Description |
|---|---|---|
| 24 July 2013 | Amended | Minor edit to reference |
History
Protocol first published: Issue 2, 2009 Review first published: Issue 9, 2011
| Date | Event | Description |
|---|---|---|
| 29 January 2009 | Amended | Converted to new review format |
Acknowledgements
We thank Margaret Anderson, Trials Search Coordinator of Cochrane Developmental, Psychosocial and Learning Problems Group, for searching relevant databases. We also thank Ms Vanessa Chu, research assistant, for administrative help, and librarians of the University of Hong Kong for retrieval of relevant literature.
Appendices
Appendix 1. Search strategies
Search strategy for CENTRAL
#1MeSH descriptor Acupuncture Therapy explode all trees #2acupunc* #3acupress* #4electroacupunc* #5meridian* #6acupoint* #7(#1 OR #2 OR #3 OR #4 OR #5 OR #6) #8MeSH descriptor Child Development Disorders,Pervasive explode all trees #9MeSH descriptor Communication, this term only #10autis* #11PDD #12pervasive development disorder* #13language near/3 delay* #14communicat* #15speech near/3 disorder* #16childhood schizophrenia #17kanner* #18asperg* #19(#8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14OR #15 OR #16 OR #17 OR #18) #20(#7 AND #19)
Search strategy for MEDLINE
1 exp Acupuncture Therapy/ 2 acupunc$.tw. 3 acupunc$.tw. 4 electroacupunc$.tw. 5 meridian$.tw. 6 acupoints$.tw. 7 6 or 4 or 1 or 3 or 2 or 5 8 exp Child Development Disorders, Pervasive/ 9 Communication/ 10 autis$.tw. 11 pdd.tw. 12 pervasive developmental disorder$.tw. 13 (language adj3 delay$).tw. ) 14 communicat$.tw. 15 (speech adj3 disorder$).tw. 16 childhood schizophrenia.tw. 17 kanner$.tw. 18 asperg$.tw. 19 or/8‐18 20 7 and 19 21 randomized controlled trial.pt. 22 controlled clinical trial.pt. 23 randomized.ab. 24 drug therapy.fs. 25 randomly.ab. 26 trial.ab. 27 groups.ab. 28 placebo.ab. 29 or/21‐28 ( 30 exp animals/ not humans.sh. 31 29 not 30 32 20 and 31
Search strategy for EMBASE
1 exp Acupuncture Therapy/ 2 acupunc$.tw. 3 electroacupunc$.tw. 4 meridian$.tw. 5 acupoints$.tw. 6 acupress$.tw. 7 or/1‐6 8 Autism/ 9 autis$.tw. 10 pdd.tw. 11 pervasive developmental disorder$.tw. 12 (language adj3 delay$).tw. 13 communicat$.tw. 14 (speech adj3 disorder$).tw. 15 childhood schizophrenia.tw. 16 kanner$.tw. 17 asperg$.tw. 18 exp interpersonal communication/ 19 or/8‐18 20 7 and 19 21 random$.tw. 22 factorial$.tw. 23 crossover$.tw. 24 cross over$.tw. 25 cross‐over$.tw. 26 placebo$.tw. 27 (doubl$ adj blind$).tw. 28 (singl$ adj blind$).tw. 29 assign$.tw. 30 allocat$.tw. 31 volunteer$.tw. 32 Crossover Procedure/ 33 double‐blind procedure.tw. 34 Randomized Controlled Trial/ 35 Single Blind Procedure/ 36 or/21‐35 37 20 and 36
Search strategy for PsycINFO via EBSCOhost (September 2010)
S40 S20 and S39
S39 S21 or S22 or S23 or S24 or S25 or S26 or S27 or S28 or S29 or S30 or
S31 or S32 or S33 or S34 or S35 or S36 or S37 or S38
S38 control*
S37 (tripl* N3 blind* ) or (tripl* N3 mask*)
S36 (trebl* N3 blind* ) or (trebl* N3 mask*)
S35 (trebl* N3 blind* ) or (trebl* N3 mask*)
S34 (doubl* N3 blind* ) or (doubl* N3 mask*)
S33 (singl* N3 blind*) or (singl* N3 mask*)
S32 prospectiv*
S31 evaluat* N3 stud*
S30 research N3 design
S29 clinical N3 trial*
S28 randomi?ed controlled trial*
S27 comparative stud*
S26 random*
S25 placebo*
S24 DE "Followup Studies"
S23 DE placebo
S22 DE "Treatment Outcomes" OR DE "Psychotherapeutic Outcomes"
S21 DE Treatment Effectiveness Evaluation
S20 S7 and S19
S19 (S8 or S9 or S10 or S11 or S12 or S13 or S14 or S15 or S16 or S17 or S18)
S18 asperg*
S17 kanner*
S16 childhood schizophrenia
S15 speech N3 disorder*
S14 communicat*
S13 language N3 delay*
S12 pervasive developmental disorder*
S11 pdd
S10 autis*
S9 DE communication
S8 De autism
S7 S1 or S2 or S3 or S4 or S5 or S6
S6 acupoints*
S5 meridian*
S4 electroacupunc*
S3 acupress*
S2 Acupunc*
S1 DE Acupuncture
Search strategy for PsycINFO via OVID (February 2009)
1 exp Acupuncture/ 2 acupunc$.tw. 3 acupress$.tw. 4 electroacupunc$.tw. 5 meridian$.tw. 6 acupoints$.tw. 7 6 or 4 or 1 or 3 or 2 or 5 8 exp Autism/ 9 Communication/ 10 autis$.tw. 11 pdd.tw. 12 pervasive developmental disorder$.tw. 13 (language adj3 delay$).tw. 14 communicat$.tw. 15 (speech adj3 disorder$).tw. 16 childhood schizophrenia.tw. 17 kanner$.tw. 18 asperg$.tw. 19 11 or 9 or 17 or 12 or 15 or 14 or 8 or 18 or 16 or 10 or 13 20 7 and 19 21 Treatment Effectiveness Evaluation/ 22 exp Treatment Outcomes/ 23 Psychotherapeutic Outcomes/ 24 PLACEBO/ 25 exp Followup Studies/ 26 placebo$.tw. 27 random$.tw. 28 comparative stud$.tw. 29 randomi#ed controlled trial$.tw. 30 (clinical adj3 trial$).tw. 31 (research adj3 design).tw. 32 (evaluat$ adj3 stud$).tw. 33 (prospectiv$ adj3 stud$).tw. 34 ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$)).tw. 35 control$.tw. 36 35 or 27 or 25 or 33 or 32 or 28 or 21 or 26 or 22 or 34 or 30 or 24 or 23 or 31 or 29 37 36 and 20
Search strategy for CINAHL
S38 S8 and S20 and S37
S37 S21 or S22 or S23 or S24 or S25 or S26 or S27 or S28 or S29 or S30 or
S31 or S32 or S33 or S34 or S35 or S36
S36 (evaluat* study or evaluat* research) or (effectiv* study or
effectiv* research) or (prospectiv* study or prospectiv* research)
S35 placebo*
S33 cross over*
S32 crossover*
S31 (MH "Crossover Design")
S30 (tripl* N3 mask*) or (tripl* N3 blind*)
S29 (trebl* N3 mask*) or (trebl* N3 blind*)
S28 (doubl* N3 mask*) or (doubl* N3 blind*)
S27 (singl* N3 mask*) or (singl* N3 blind*)
S26 (clinic* N3 trial*) or (control* N3 trial*)
S25 (random* N3 allocat* ) or (random* N3 assign*)
S24 randomis* or randomiz*
S23 (MH "Meta Analysis")
S22 (MH "Clinical Trials+")
S21 MH random assignment
S20 (S9 or S10 or S11 or S12 or S13 or S14 or S15 or S16 or S17 or S18 or S19)
S19 childhood schizophrenia
S18 speech N3 disorder*
S17 language N3 delay*
S16 communicat*
S15 (MH "Communication")
S14 pervasive development* disorder*
S13 pdd*
S12 kanner*
S11 asperg*
S10 autis*
S9 (MH "Child Development Disorders, Pervasive+")
S8 S1 or S2 or S3 or S4 or S5 or S6 or S7
S7 (MH "Meridians+")
S6 acupoints*
S5 meridian*
S4 electroacupunc*
S3 acupress*
S2 acupunc*
S1 (MH "Acupuncture+")
Search terms for metaRegister of Controlled Trials
acupressure and autis*
acupuncture and autis*
Search strategy for AMED (last searched February 2009) 1 exp Acupuncture Therapy/ 2 acupunc$.tw. 3 acupress$.tw. 4 electroacupunc$.tw. 5 meridian$.tw. 6 acupoints$.tw. 7 6 or 4 or 1 or 3 or 2 or 5 8 Communication/ 9 autis$.tw. 10 pdd.tw. 11 pervasive developmental disorder$.tw. 12 (language adj3 delay$).tw. 13 communicat$.tw. 14 (speech adj3 disorder$).tw. 15 childhood schizophrenia.tw. 16 kanner$.tw. 17 asperg$.tw. 18 Autism/ 19 11 or 9 or 17 or 12 or 15 or 14 or 8 or 18 or 16 or 10 or 13 20 7 and 19
Appendix 2. Search strategy for TCMLARS, Chinese Clinical Trials Registry, China Journal Full‐text Database, China Master Theses Full‐text Database, China Doctor Dissertation Full‐text Database, China Proceedings of Conference Database, and Index to Taiwan Periodical Literature System and Index to Taiwan Periodical Literature System
1. "ZiBiZheng"(Self Shut‐off Syndrome) or GuDuZheng (lonely Syndrome)
2. "ZhenJiu" (Acupuncture) or "ZhenCi" (Acupuncture) or "DianZhen" (Electro‐acupuncture) or "ZhenYa" (Acupressure) or "ErZhen" (Ear Acupuncture) or "TiZhen" (Body acupuncture) or "SheZhen" (Tongue acupuncture) or "TouPiZhen" (Scalp acupuncture) or "XueWei" (acupoints)
3. 1 and 2
Appendix 3. Data Extraction Form ‐ Acupuncture for ASD
Trial Reference ID
METHODS
| Design: Randomisation method: Method of allocation concealment: Blinding method: Stratification factors: |
PARTICIPANTS
| Inclusion criteria: Exclusion criteria: Number of participants (Intervention : control): Number of males (Intervention : control): Age: Specific diagnosis/diagnostic subtypes: Comorbidities: Duration of autism: Previous treatment: |
INTERVENTIONS
| Intervention group: Control group: Washout period in cross‐over design: |
OUTCOMES
| Outcome measures used: |
NOTES
| Dropouts (with reasons): Duration of follow‐up: Methods of analysis (intention‐to‐treat/per‐protocol analysis): Comparability of groups at baseline (yes/no): Statistical techniques: Remarks: |
Data and analyses
Comparison 1. Needle acupuncture plus conventional treatment versus sham acupuncture plus conventional treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Improvement in Ritvo‐Freeman Real Life Rating Scale (RFRLRS) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Improvement in total score | 2 | 105 | Mean Difference (IV, Fixed, 95% CI) | 0.09 [‐0.03, 0.21] |
| 1.2 Improvement in sensory motor score | 2 | 105 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.13, 0.17] |
| 1.3 Improvement in social score | 2 | 105 | Mean Difference (IV, Fixed, 95% CI) | 0.09 [‐0.09, 0.26] |
| 1.4 Improvement in sensory response score | 2 | 105 | Mean Difference (IV, Fixed, 95% CI) | 0.04 [‐0.12, 0.21] |
| 1.5 Improvement in affectual score | 2 | 105 | Mean Difference (IV, Fixed, 95% CI) | 0.14 [‐0.07, 0.34] |
| 1.6 Improvement in language score | 2 | 105 | Mean Difference (IV, Fixed, 95% CI) | 0.11 [‐0.02, 0.24] |
| 2 Improvement in Aberrant Behavior Checklist (ABC) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 Improvement in irritability | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Improvement in lethargy | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Improvement in stereotypy | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 Improvement in hyperactivity | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.5 Improvement in inappropriate speech | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Improvement in Reynell Language Developmental Scale (RDLS) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Improvement in comprehension age | 2 | 105 | Mean Difference (IV, Fixed, 95% CI) | 0.14 [0.02, 0.25] |
| 3.2 Improvement in comprehension score | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | ‐1.32 [‐5.40, 2.76] |
| 3.3 Improvement in expression age | 2 | 105 | Mean Difference (IV, Fixed, 95% CI) | 0.05 [‐0.10, 0.20] |
| 3.4 Improvement in expression score | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | 1.96 [‐0.58, 4.50] |
| 4 Improvement in Symbolic Play Test (SPT) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Improvement in total score | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Improvement in language age | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Improvement in Griffiths Mental Developmental Scale (GMDS) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 Improvement in general quotient | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Improvement in mental age | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 Improvement in locomotor score | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.4 Improvement in personal‐social score | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.5 Improvement in hearing and speech score | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.6 Improvement in eye hand coordination score | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.7 Improvement in performance score | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.8 Improvement in practical reasoning | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Improvement in Leiter International Performance Scale‐Revised (Leiter‐R) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.1 Improvement in visualization & reasoning (VR) battery (full IQ) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 Improvement in attention & memory (AM) battery (composite score) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 Improvement in visualization & reasoning (VR) battery (growth composite score) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.4 Improvement in attention & memory (AM) battery (growth composite score) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Improvement in Functional Independent Measure of children (WeeFIM) | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 Improvement in total score | 2 | 105 | Mean Difference (IV, Random, 95% CI) | 3.08 [‐0.61, 6.77] |
| 7.2 Improvement in self‐care | 2 | 105 | Mean Difference (IV, Random, 95% CI) | 2.10 [‐0.69, 4.88] |
| 7.3 Improvement in mobility | 2 | 105 | Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐1.05, 0.83] |
| 7.4 Improvement in cognition | 2 | 105 | Mean Difference (IV, Random, 95% CI) | 0.70 [0.09, 1.30] |
| 7.5 Improvement in comprehension | 1 | 55 | Mean Difference (IV, Random, 95% CI) | 0.37 [‐0.02, 0.76] |
| 7.6 Improvement in expression | 1 | 55 | Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.28, 0.56] |
| 7.7 Improvement in social interaction | 1 | 55 | Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.42, 0.16] |
| 7.8 Improvement in problem solving | 1 | 55 | Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.44, 0.18] |
| 7.9 Improvement in memory | 1 | 55 | Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.20, 0.34] |
| 8 Improvement in Pediatric Evaluation of Disability Inventory (PEDI) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.1 Improvement in self care | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Improvement in self‐care (cargiver assistance scale) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 Improvement in mobility | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.4 Improvement in mobility (caregiver assistance scale) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.5 Improvement in social function | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.6 Improvement in social function (caregiver assistance scale) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Frequency of improvement in Clinical Global Impression Scale (CGIS) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 9.1 Frequency of improvement of >=25% | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 Frequency of improvement of >50% | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 2. Needle acupuncture plus conventional treatment versus conventional treatment alone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Improvement in Ritvo‐Reeman Real Life Rating Scale (RFRLRS) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Improvement in total score | 2 | 65 | Mean Difference (IV, Fixed, 95% CI) | 0.09 [‐0.03, 0.21] |
| 1.2 Improvement in sensory motor score | 2 | 66 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.14, 0.33] |
| 1.3 Improvement in social score | 2 | 66 | Mean Difference (IV, Fixed, 95% CI) | ‐0.09 [‐0.28, 0.11] |
| 1.4 Improvement in affectual score | 2 | 66 | Mean Difference (IV, Fixed, 95% CI) | 0.09 [‐0.16, 0.33] |
| 1.5 Improvement in sensory response score | 2 | 66 | Mean Difference (IV, Fixed, 95% CI) | 0.07 [‐0.11, 0.25] |
| 1.6 Improvement in language score | 2 | 66 | Mean Difference (IV, Fixed, 95% CI) | 0.12 [‐0.04, 0.29] |
| 2 Improvement in Autism Treatment Evaluation Checklist (ATEC) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Improvement in total score | 2 | 57 | Mean Difference (IV, Fixed, 95% CI) | 6.28 [‐1.05, 13.61] |
| 2.2 Improvement in communication and speech | 2 | 57 | Mean Difference (IV, Fixed, 95% CI) | 1.43 [‐0.21, 3.07] |
| 2.3 Improvement in sociability | 2 | 57 | Mean Difference (IV, Fixed, 95% CI) | 1.82 [‐1.39, 5.03] |
| 2.4 Improvement in sensory and cognitive awareness | 2 | 57 | Mean Difference (IV, Fixed, 95% CI) | 2.48 [‐0.04, 5.00] |
| 2.5 Improvement in physical health and behavior | 2 | 57 | Mean Difference (IV, Fixed, 95% CI) | 0.49 [‐1.95, 2.93] |
| 3 Improvement in Aberrant Behavior Cheklist (ABC) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Improvement in total score | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Improvement in irritability | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 Improvement in lethargy | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.4 Improvement in stereotypy | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.5 Improvement in hyperactivity | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.6 Improvement in inappropriate speech | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Improvement in Autism Diagnostic Observation Scale (ADOS) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Improvement in communication | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Improvement in social interaction | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Frequency of improvement in Autism Behavior Checklist | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6 Post‐treatment Autism Behavior Checklist score | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.1 Total score | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 Sensory score | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 Social score | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.4 Physical score | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.5 Language score | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.6 Self‐care score | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Frequency of improvement in Social Adaptive Behavior Scale (SABS) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8 Improvement in Social Adaptive Behavior Scale (SABS) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9 Improvement in Symbolic Play Test (SPT) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 9.1 Improvement in total score | 2 | 57 | Mean Difference (IV, Fixed, 95% CI) | 0.77 [‐0.83, 2.37] |
| 9.2 Improvement in language age | 1 | 21 | Mean Difference (IV, Fixed, 95% CI) | 1.88 [‐0.70, 4.46] |
| 10 Improvement in Reynell Language Developmental Scale (RLDS) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 Improvement in comprehension age | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 Improvement in comprehension score | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.3 Improvement in expression age | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.4 Improvement in expression score | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Post‐treatment Arabic Language Test (ALT) score | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 11.1 Attention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.2 Receptive semantics | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.3 Expressive semantics | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.4 Receptive syntax | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.5 Expressive syntax | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.6 Phonology | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.7 Pragmatics | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Post‐treatment Peabody Picture Vocabulary Test (PPVT) score | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 13 Frequency of improvement in Chinese version of Psychoeducational Profile (CPEP) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 13.1 Frequency of any improvement | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.2 Frequency of improvement of >=16 marks | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.3 Frequency of improvement of >=8 marks | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 Improvement in Chinese version of Psychodeducational Profile (CPEP) score | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 14.1 Improvement in total score | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.2 Improvement in imitation | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.3 Improvement in sensory | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.4 Improvement in fine motor skills | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.5 Improvement in gross motor skills | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.6 Improvement in eye‐hand coordination | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.7 Improvement in cognitive ability | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.8 Improvement in speech | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 Improvement in Functional Independence Measure of Children (WeeFim) | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 15.1 Improvement in total score | 3 | 85 | Mean Difference (IV, Fixed, 95% CI) | 4.34 [2.79, 5.89] |
| 15.2 Improvement in self‐care | 3 | 85 | Mean Difference (IV, Fixed, 95% CI) | 2.50 [0.48, 4.52] |
| 15.3 Improvement in mobility | 3 | 85 | Mean Difference (IV, Fixed, 95% CI) | 1.30 [‐0.10, 2.70] |
| 15.4 Improvement in cognition | 3 | 85 | Mean Difference (IV, Fixed, 95% CI) | 3.92 [2.13, 5.72] |
| 15.5 Improvement in comprehension | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | ‐0.70 [‐1.65, 0.26] |
| 15.6 Improvement in expression | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | 0.36 [‐0.22, 0.94] |
| 15.7 Improvement in social interaction | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | 0.5 [‐0.30, 1.30] |
| 15.8 Improvement in problem solving | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | 0.33 [‐0.30, 0.96] |
| 15.9 Improvement in memory | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | ‐0.14 [‐0.73, 0.45] |
| 16 Improvement in Functional Independence Measure of children (WeeFim): sensitivity analysis excluding trials with inadequate allocation concealment or blinding | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 16.1 Improvement in total score | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.2 Improvement in self‐care | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.3 Improvement in mobility | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.4 Improvement in cognition | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 Clinical Global Impression Scale (CGIS) score | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 17.1 Total score | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.2 Response to social interaction | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.3 Social initiation | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.4 Use of speech | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.5 Repetitive behavior | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.6 Behavior problem | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.7 Activity level | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.8 Sleep problem | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.9 Digestive problem | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18 Frequency of improvement in Clinical Global Impression Scale (CGIS) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 3. Acupressure plus conventional treatment versus conventional treatment alone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Frequency of improvement in China Rehabilitation Research Council (CRRC) sign‐significance relations scale | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Overall improvement | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Significant overall improvement | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Comprehension of situation | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Matching objects | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.5 Selection of objects | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.6 Non‐verbal comprehension | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.7 Non‐verbal expression | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.8 Speech comprehension | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.9 Speech expression | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.10 Speech imitation | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.11 Vocabulary comprehension | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.12 Vocabulary expression | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.13 Phrase comprehension | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.14 Phrase expression | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.15 Communication attitude | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Frequency of improvement in basic developmental assessment | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Putting a small ball | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Response | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Shape differentiation | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 6‐shape board | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.5 Building blocks | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.6 Aligning blocks | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.7 Building tunnel | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.8 Drawing dots | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.9 Copying marks | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.10 Copying cross and circle | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.11 Drawing 2 lines | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.12 Drawing 3 lines | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.13 Vocalization | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.14 Babbling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.15 Speech | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.16 Non‐verbal comprehension | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.17 Non‐verbal matching | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Improvement in Parents' Rating Questionnaire | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Overall improvement | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Improvement in language | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 Improvement in social interaction | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.4 Improvement in stereotyped behavior | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.5 Improvement in motor functioning | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Allam 2008.
| Methods | Design: parallel groups Randomization method: according to randomization tables Method of allocation concealment: group assignment in sealed envelope Blinding: outcome assessor (language therapist) was blinded Stratification: not used |
|
| Participants | Inclusion criteria: age 4‐7 years and fulfilled DSM‐IV and ADI‐R criteria and CARS score >=30 Exclusion criteria: no Number of participants (intervention:control): 10:10 Number of males (intervention:control): 7:5 Age: overall mean 5.5 years (SD 1.22 years), range 4‐7 years Specific diagnosis/diagnostic subtypes: information not available Comorbidities: information not available Duration of autism: information not available Previous treatment: information not available |
|
| Interventions | Intervention group: scalp acupuncture + language therapy Scalp acupuncture at 8 acupoints: Du 20, 26, GV 17, 3 temple needles, and Yamamoto YNSA 2 points: cerebrum and aphasia points. Needles (0.3 x 30mm, disposable, single‐use stainless steel) were inserted to a depth of 1/2 to 1 cm until qi was achieved. Rapid manual stimulation was applied upon insertion and removal of needles. Needles were retained in place for 20 minutes each session, twice weekly for 2 months followed by a period of 2 weeks' rest. This cycle was repeated through the 9 months (total number of 50 acupuncture sessions) Language therapy was individualized and aimed at improving attention, receptive and verbal abilities Control group: language therapy alone (same as intervention group) |
|
| Outcomes | Arabic Language Test | |
| Notes | No dropouts Duration of follow‐up: 9 months Acupuncture paradigm: medical acupuncture paradigm, scalp acupuncture Training or qualification of acupuncture therapist: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation according to randomization tables |
| Allocation concealment (selection bias) | Low risk | Group assignment in sealed envelope |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Outcome assessor was blinded. Although acupuncture therapist was likely not blinded, he was not involved in the care of participants otherwise or in outcome assessment. Therefore this is unlikely to introduce bias. Unblinding of autistic children is also considered unlikely to introduce bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data were complete |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | Unclear risk | Baseline characteristics were not described for treatment groups and it is unclear whether the intervention and the control group were comparable. No placebo or sham control was used and hence there might be placebo effect |
Chan 2009.
| Methods | Design: parallel groups Randomization method: information not available Method of allocation concealment: information not available Blinding: therapist and parents (outcome assessors) and patients were not blinded Stratification: not used |
|
| Participants | Inclusion criteria: children with autism in special education centers in Hong Kong Exclusion criteria: no Number of participants (intervention:control): 16:16 Number of males (intervention:control): 13:13 Age: intervention group: mean 6.85 years (SD 1.76 years); control group: mean 6.89 years (SD 1.77 years) Specific diagnosis/diagnostic subtypes: information not available Comorbidities: information not available Duration of autism: information not available Previous treatment: information not available |
|
| Interventions | Intervention group: seven‐star needle stimulation (acupressure) + conventional educational program Stimulation was performed 5 days per week for 6 weeks (total 30 treatment sessions). During the session, the therapist applied seven‐star needle stimulation by tapping the skin quickly (approximately 20 times per 5 seconds) with the dermatoneural medical hammer. The stimulation was performed on the 2 sides on the child's back along the spine (about half an inch on each side) from the lumbar to the thoracic region, along the midline on the front side of the body, and also on the dorsal and posterior parts of the head. Each stimulation site was tapped 3 times, with a distance of about 2cm between each tap Control group: conventional educational program alone |
|
| Outcomes | Parent's rating questionnaire Quantitative electroencephalogram |
|
| Notes | Dropouts: none Duration of follow‐up: 6 weeks Acupuncture paradigm: Traditional Chinese Medicine paradigm Training or qualification of acupuncture therapist: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Information not available |
| Blinding (performance bias and detection bias) All outcomes | High risk | Therapist and parents (outcome assessors) and patients were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data were complete |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | High risk | The assessment instrument (Parent's Rating Questionnaires) was specifically designed for the current study. It has not been validated for use in assessment of children with ASD. The conventional educational program was variable for each patient and may introduce bias. No placebo or sham control was used and hence there might be placebo effect |
Wang 2007.
| Methods | Design: parallel groups Randomization method: according to sequence of clinic attendance Method of allocation concealment: information not available Blinding: not described Stratification: not used |
|
| Participants | Inclusion criteria: age <12 years, ASD diagnosed by ICD‐10 criteria or Chinese Classification and Diagnostic Criteria of Mental Disorders version 3 (CCMD‐3), and could finish 2 courses of acupuncture Exclusion criteria: child with schizophrenia, Asperger syndrome, Heller syndrome or Rett syndrome, dropout during therapy, use of other intervention during therapy Number of participants (intervention:control): 30:30 Number of males (intervention:control): 24:23 Age: intervention group: mean 5.14 years (SD 1.53 years); control group: mean 5.46 years (SD 1.68 years) Specific diagnosis/diagnostic subtypes: information not available Comorbidities: information not available Duration of autism: intervention group: mean 2.40 years (SD 1.12 years); control group: mean 2.77 years (SD 1.26 years) Previous treatment: information not available |
|
| Interventions | Intervention group: electroacupuncture + behavioral therapy Electroacupuncture at GV20 (needles inserted backwards to a depth of 15‐20mm), EX‐HN1 (needles inserted at the direction of GV20 to a depth of 15‐20mm), GV24, GB13, EX‐HN3, GV17, GB19, PC6, speech areas I, II, III on the head. Acupuncture needles used had diameter 0.3mm and length 40mm. Electrical stimulation was given at 75Hz with cross‐shaped copper cathode at GV20, EX‐HN1 and anode at PC6, using Life Message Apparatus (SMS‐03). Electroacupuncture was applied once daily, 50 min/session, 5 sessions per week for 2 month course for 2 courses. Behavioral therapy: one‐to‐one intensive systematic therapy to eliminate abnormal sensation and behavior, and develop simple skills, so that children can gradually improve social and language functioning. Behavioral therapy was given once daily, 60 minutes per session, 5 sessions per week for 2 month course for 2 courses. Control group: behavioral therapy alone (same as intervention group) |
|
| Outcomes | Autism Behavior Checklist improvement Autism Behavior Checklist scores Peabody Picture Visual Test (PPVT) Social Adaptive Behavior Scale (SABS) improvement SABS score |
|
| Notes | Dropouts were not reported. Duration of follow‐up: 4 months Acupuncture paradigm: Traditional Chinese Medicine paradigm Training or qualification of acupuncture therapist: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Random group allocation according to sequence of clinic attendance |
| Allocation concealment (selection bias) | High risk | Random group allocation according to sequence of clinic attendance. The allocation is likely not concealed |
| Blinding (performance bias and detection bias) All outcomes | High risk | No blinding was described. Since the intervention involves acupuncture, it is highly likely that the treating physicians and patients were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data were complete but some dropouts might have been excluded from analyses |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | High risk | Patients who dropped out were excluded. The number of dropouts and reasons were not reported. This might cause bias. No placebo or sham control was used and hence there might be placebo effect |
Wong 2002.
| Methods | Design: parallel groups Randomization method: computer random generation of group assignment for each patient Method of allocation concealment: computerized allocation of groups Blinding: outcome assessors were blinded to group allocation; therapist and parents and patients were not blinded Stratification: not used |
|
| Participants | Inclusion criteria: age 3‐15 years, ASD diagnosed by DSM‐IV and ADI‐R, Childhood Autism Rating Scale (CARS) score>30 Exclusion criteria: children with associated neurological disorders such as tuberous sclerosis, fragile X syndrome and epilepsy Number of participants (intervention:control): 15:15 Number of males (intervention:control): 15:14 Age: intervention group: mean 7.67 years (SD 2.82 years); control group: mean 6.67 years (SD 2.97 years). Specific diagnosis/diagnostic subtypes: information not available Comorbidities: information not available Duration of autism: information not available Previous treatment: information not available |
|
| Interventions | Intervention group: tongue acupuncture + conventional educational program Tongue acupuncture: needle acupuncture was applied at 5 points on the tongue, using Hwato acupuncture needles (made in China) with diameter 0.3 mm and length 40 mm. The child sat on the mother's lap with the head tilted around 45 degrees upwards. Sterile gauze was used to pick up and station the tongue with the examiner's left hand. The child was encouraged to open up his/her mouth, which was the usual mouth posture of those with persistent drooling. Quick and accurate needle insertion into 5 acupoints was performed with the examiner's right hand. The acupuncture procedure lasted for <15 seconds/session, daily for 5 days/week for 8 weeks (total 40 sessions) Control group: conventional educational program alone (same as intervention group) |
|
| Outcomes | Ritvo‐Freeman Real Life Rating Scale (RFRLRS) Functional Independence Measure for children (WeeFIM) Parental Stress Index (PSI) Clinical Global Impression Scale (CGIS) Side effects |
|
| Notes | Dropouts: none. Duration of follow‐up: 8 weeks. Acupuncture paradigm: Traditional Chinese Medicine paradigm Training or qualification of acupuncture therapist: Bachelor degree in medicine and Chinese medicine, professor of acupuncture in China, 20 years of experience in acupuncture |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Group allocation was done by random computerized assignment for each case |
| Allocation concealment (selection bias) | Low risk | Group allocation was concealed because of random computerized group allocation for each case |
| Blinding (performance bias and detection bias) All outcomes | High risk | Outcome assessors for most outcomes were blinded. However, parents were not blinded and they were involved in some outcome assessment which may potentially introduce bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data were complete except for a small proportion of items (<30%) in the assessment instruments that were missing |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | Unclear risk | Conventional educational and behavioral program was variable for each patient and may introduce bias. No placebo or sham control was used and hence there might be placebo effect |
Wong 2007.
| Methods | Design: parallel groups Randomization method: computer random generation of group assignment for each patient Method of allocation concealment: computerized allocation of groups Blinding: outcome assessors and parents were blinded to group allocation; therapist and patients were not blinded. Stratification: not used |
|
| Participants | Inclusion criteria: age 3‐16 years, ASD diagnosed by DSM‐IV and ADI‐R, Childhood Autism Rating Scale (CARS) score>30 Exclusion criteria: children with associated neurological disorders such as tuberous sclerosis, fragile X syndrome and epilepsy. Number of participants (intervention:control): 16:11 Number of males (intervention:control): 16:11 Age: intervention group: mean 10.17 years (SD 3.93 years); control group: mean 8.75 years (SD 4.62 years). Specific diagnosis/diagnostic subtypes: information not available Comorbidities: information not available Duration of autism: information not available Previous treatment: information not available |
|
| Interventions | Intervention group: tongue acupuncture + conventional educational and behavioral program Tongue acupuncture: needle acupuncture was applied using Hwato acupuncture needles (made in China) with diameter 0.3 mm and length 40 mm to 5 points on the tongue (Run Ze (1cm from the tongue tip, needle inserted to 1cm deep obliquely), Guan Zhu (0.5cm from tongue tip, needle to 0.3cm deep obliquely), Tian Men (center of tongue base, needle to 0.5‐1cm deep perpendicularly), Di You (0.5 cm from tongue base on both sides, needle to 0.5cm deep perpendicularly). The child sat on the mother's lap with the head tilted around 45 degrees upwards. Sterile gauze was used to pick up and station the tongue with the examiner's left hand. The child was encouraged to open up his/her mouth, which was the usual mouth posture of those with persistent drooling. Quick and accurate needle insertion into 5 acupoints was performed with the examiner's right hand. The acupuncture procedure lasted for <15 seconds/session, daily for 5 days/week for 8 weeks (total 40 sessions). Control group: conventional educational and behavioral program alone |
|
| Outcomes | Autism Treatment Evaluation Checklist (ATEC) Reynell Language Developmental Scale (RLDS) Symbolic Play Test (SPT) Functional Independence Measure for children (WeeFIM) Clinical Global Impression Scale (CGIS) Frequncy of patients with >=10% increase in cortical mean standardized uptake value maximum (SUVmax) and standardized uptake value average (SUVavg) on positron emission tomography (PET) Side effects |
|
| Notes | Dropouts: Intervention group: 4 (3 due to technical reason (erroneous calibration of PET scanner), 1 refused 2nd PET assessment); Control group: 2 (1 due to technical reason (erroneous calibration of PET scanner), 1 refused 2nd PET assessment) Duration of follow‐up: 8 weeks Acupuncture paradigm: Traditional Chinese Medicine paradigm Training or qualification of acupuncture therapist: Bachelor degree in medicine and Chinese medicine, professor of acupuncture in China, 20 years of experience in acupuncture |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Group allocation was done by random computerized assignment for each case |
| Allocation concealment (selection bias) | Low risk | Group allocation was concealed because of random computerized group allocation for each case |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Outcome assessors and parents were blinded. Although acupuncture therapist was not blinded, he was not involved in the care of participants otherwise or in outcome assessment. Therefore this is unlikely to introduce bias. Unblinding of autistic children is also considered unlikely to introduce bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Incomplete data were all explained and unrelated to outcome. Missing data constituted <30% of outcome data and similar in both groups |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | Unclear risk | Conventional educational and behavioral program was variable for each patient and may introduce bias. No placebo or sham control was used and hence there might be placebo effect |
Wong 2008.
| Methods | Design: cross‐over study Randomization method: computer‐generated block randomisation table Method of allocation concealment: information not available Blinding: outcome assessors were blinded to group allocation; therapist and parents and patients were not blinded. Stratification: by age and severity of autism (according to Childhood Autism Rating Scale (CARS) score) |
|
| Participants | Inclusion criteria: age 3‐12 years, ASD diagnosed by DSM‐IV and ADI‐R and ADOS Exclusion criteria: children with epilepsy on antiepileptic drugs, or other neurological, psychiatric or genetic disorders, or had experienced acupuncture in the past one year. Parents who are unable to finish the questionnaire assessments were also excluded Number of participants (intervention:control): 18:18 Number of males (intervention:control): 17:17 Age: intervention group: mean 7.4 years (SD 2.215 years); control group: mean 7.62 years (SD 2.367 years). Specific diagnosis/diagnostic subtypes: information not available Comorbidities: information not available Duration of autism: information not available Previous treatment: information not available |
|
| Interventions | Intervention group: electroacupuncture + conventional education program Electroacupuncture: 5 acupoints were stimulated (GV20, EX‐HN3, bilateral HT7, bilateral SP6, and bilateral auricular brain points). Hwato sterile disposable single use acupuncture needles were used. Needles used for body acupuncture measured 0.25mm in diameter and 25mm in length, while that used for auricular acupuncture measured 0.25mm in diameter and 13mm in length. Needles were inserted transversely for 13‐25mm at GV20 and EX‐HN3, perpendicularly for 13‐25mm at HT7 and SP6, and perpendicularly for 5‐10mm at auricular points. The same acupuncturist provided acupuncture for all participants. The "De Qi" sensation was elicited as far as possible. The Hwato SDZ‐II electronic acupuncture treatment instrument was used for electrical stimulation. Continuous wave form was applied at amplitude tolerable to participants. The treatment provided was based on syndrome differentiation according to Traditional Chinese Medicine theory. Participants with deficiency syndrome, deficiency‐excess complex syndrome, and excess syndrome received electronic stimulation at frequencies of 25Hz, 50Hz, and 75 Hz respectively. The acupoints were stimulated for 30 minutes/session, daily for 3 days/week for 8 weeks (total 24 sessions) Control group: conventional education program alone 4 weeks after treatment, participants in intervention group received no electroacupuncture and participants in control group received 8 weeks of electroacupuncture |
|
| Outcomes | Aberrant Behavioral Checklist (ABC) Autism Treatment Evaluation Checklist (ATEC) Ritvo‐Freeman Real Life Rating Scale (RFRLRS) Autism Diagnostic Observation Scale (ADOS) Functional Independence Measure for children (WeeFIM) Symbolic Play Test (SPT) Clinical Global Impression Scale (CGIS) Side effects |
|
| Notes | Dropouts: Intervention group: 4 (1 unable to attend acupuncture sessions according to the allotted time slots, 1 withdrew after the 1st acupuncture session because parents found it too inconvenient to travel to the acupuncture clinic, both attended end‐of treatment assessment; 2 lost to follow‐up with unknown reasons and did not undergo final assessment); Control group: 2 (1 unable to attend acupuncture sessions according to the allotted time slots after cross over but attended final assessment, 1 lost to follow‐up with unknown reason and did not undergo final assessment) Duration of follow up: 20 weeks Acupuncture paradigm: Traditional Chinese Medicine paradigm Training or qualification of acupuncture therapist: PhD, professor of acupuncture in China, registered Chinese Medicine practitioner in Hong Kong, 20 years of experience in acupuncture |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Allocation sequence is generated by computer block randomization |
| Allocation concealment (selection bias) | Unclear risk | No information is available |
| Blinding (performance bias and detection bias) All outcomes | High risk | Outcome assessors for most outcomes were blinded. However, parents were not blinded and they were involved in some outcome assessment which may potentially introduce bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Incomplete data were mostly explained and unrelated to outcome. Missing data constituted <30% of outcome data and similar in both groups |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | Unclear risk | Conventional education program was variable for each patient and may introduce bias. Acupoints varied with syndromic diagnosis based on TCM theory and may introduce bias. No placebo or sham control was used and hence there might be placebo effect |
Wong 2010a.
| Methods | Design: parallel groups Randomization method: Computer random generation of group assignment for each patient Method of allocation concealment: computerized allocation of groups Blinding: outcome assessors and parents and patients were blinded to group allocation; therapist was not blinded. Stratification: not used |
|
| Participants | Inclusion criteria: age 3‐11 years, ASD diagnosed by DSM‐IV and ADI‐R, Childhood Autism Rating Scale (CARS) score>30 Exclusion criteria: children with associated neurological disorders or epilepsy Number of participants (Intervention:control): 25:25 Number of males (Intervention:control): 21:23 Age: intervention group: mean 6.23 years (SD 1.87 years); control group: mean 6 years (SD 1.99 years). Specific diagnosis/diagnostic subtypes: information not available Comorbidities: information not available Duration of autism: information not available Previous treatment: information not available |
|
| Interventions | Intervention group: tongue acupuncture + conventional educational and behavioral program Tongue acupuncture: needle acupuncture was applied using Hwato acupuncture needles (made in China) with diameter 0.3 mm and length 40 mm to 5 points on the tongue (Run Ze (1cm from the tongue tip, needle inserted to 1cm deep obliquely), Guan Zhu (0.5cm from tongue tip, needle to 0.3cm deep obliquely), Tian Men (center of tongue base, needle to 0.5‐1cm deep perpendicularly), Di You (0.5 cm from tongue base on both sides, needle to 0.5cm deep perpendicularly)). The child sat on the mother's lap with the head tilted around 45 degrees upwards. Sterile gauze was used to pick up and station the tongue with the examiner's left hand. The child was encouraged to open up his/her mouth, which was the usual mouth posture of those with persistent drooling. Quick and accurate needle insertion into 5 acupoints was performed with the examiner's right hand. The acupuncture procedure lasted for <15 seconds/session, daily for 5 days/week for 8 weeks (total 40 sessions) Control group: sham acupuncture + conventional educational and behavioral program Sham acupuncture: same procedure as tongue acupuncture in intervention group, except that the rough end of the acupuncture needle was used to touch the 5 acupoints instead of puncturing by the sharp end of the needle |
|
| Outcomes | Griffiths Mental Developmental Scale (GMDS) Ritvo‐Freeman Real Life Rating Scale (RFRLRS) Reynell Language Developmental Scale (RLDS) Symbolic Play Test (SPT) Functional Independence Measure for children (WeeFIM) Side effects |
|
| Notes | Dropouts: none Duration of follow‐up: 8 weeks Acupuncture paradigm: Traditional Chinese Medicine paradigm Training or qualification of acupuncture therapist: Bachelor degree in medicine and Chinese medicine, professor of acupuncture in China, 20 years of experience in acupuncture |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Group allocation was done by random computerized assignment for each case |
| Allocation concealment (selection bias) | Low risk | Group allocation was concealed because of random computerized group allocation for each case |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Outcome assessors and parents and patients were blinded. Although acupuncture therapist was not blinded, he was not involved in the care of participants otherwise or in outcome assessment. Therefore this is unlikely to introduce bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data were complete |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | Unclear risk | Conventional educational and behavioral program was variable for each patient and may introduce bias |
Wong 2010b.
| Methods | Design: parallel groups Randomization method: a computer generated randomisation numbers. Each child was randomly assigned by drawing an opaque envelop containing a randomisation number Method of allocation concealment: computer generated randomisation number in an opaque envelop Blinding: outcome assessors and parents and patients were blinded to group allocation; therapist was not blinded. Stratification: by age and severity of autism (according to Childhood Autism Rating Scale (CARS) score) |
|
| Participants | Inclusion criteria: age 3‐18 years, ASD diagnosed by DSM‐IV and ADI‐R and ADOS Exclusion criteria: children with epilepsy on antiepileptic drugs, or had experienced acupuncture in the past 6 months Number of participants (Intervention:control): 31:28 Number of males (Intervention:control): 25:22 Age: intervention group: mean 9.17 years (SD 4.12 years); control group: mean 9.56 years (SD 4.22 years). Specific diagnosis/diagnostic subtypes: information not available Comorbidities: information not available Duration of autism: information not available Previous treatment: information not available |
|
| Interventions | Intervention group: electroacupuncture + conventional interventional or educational program Electroacupuncture: sterile disposable 0.3x4cm acupuncture needles (Hwato, made in China) were inserted into 8 acupoints (EX‐HN1, EX‐HN3, PC6, HT7, LR3, AT3, TF4, SP6). The treatment took place with the child in either a supine or sitting position. A portable electroacupuncture machine (Model Hwato SDZ‐II, Electronic Acupuncture Treatment Instrument, Suzhou Medical Appliance Factory, China) was connected to the handles of the acupuncture needles to provide electrical stimulation for 30 minutes. Spacing‐density wave stimulation was applied. The acupoints were stimulated for 30 minutes/session, daily for 3 days/week for 4 weeks (total 12 sessions). Control group: sham electroacupuncture + conventional interventional or educational program Sham acupuncture: needles were inserted into and maintained at superficial level at points 3‐5mm from the selected acupoints of the intervention group. Electrical stimulation was the same as in the intervention group. |
|
| Outcomes | Functional Independence Measure for children (WeeFIM) Aberrant Behavioral Checklist (ABC) Pediatric Evaluation of Disability Inventory (PEDI) Leiter International Performance Scale‐Revised (Leiter‐R) Ritvo‐Freeman Real Life Rating Scale (RFRLRS) Reynell Language Developmental Scale (RLDS) Clinical Global Impression Scale (CGIS) Parental report in 22 items Side effects |
|
| Notes | Dropouts: Intervention group: 1 (did not receive allocated intervention because of conflict between acupuncture and own autism training program); Control group: 3 (2 due to conflict between acupuncture and own autism training program, 1 due to non‐compliance after 3 sessions) Duration of follow‐up: 4 weeks Acupuncture paradigm: Traditional Chinese Medicine paradigm Training or qualification of acupuncture therapist: PhD, professor of acupuncture in China, registered Chinese Medicine practitioner in Hong Kong, 20 years of experience in acupuncture |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Group allocation was done by computer generated randomization number |
| Allocation concealment (selection bias) | Low risk | Group allocation was concealed by computer generated randomization number in an opaque envelope |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Outcome assessors and parents and patients were blinded. Although acupuncture therapist was not blinded, he was not involved in the care of participants otherwise or in outcome assessment. Therefore this is unlikely to introduce bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data were complete as dropouts also attended assessments |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | Unclear risk | Conventional interventional or educational program was variable for each patient and may introduce bias |
Yan 2007.
| Methods | Design: parallel groups Randomization method: according to sequence of clinic attendance Method of allocation concealment: not described Blinding: not described Stratification: not used |
|
| Participants | Inclusion criteria: children with ASD diagnosed by Aberrant Behavioral Checklist (ABC) and Childhood Autism Rating Scale (CARS) and Peabody Picture Vocabulary Test (PPVT) Exclusion criteria: no Number of participants (Intervention:control): 20:20 Number of males (Intervention:control): 19:19 Age: intervention group: mean 5.51 years (SD 1.73 years); control group: mean 4.55 years (SD 1.3 years). Specific diagnosis/diagnostic subtypes: information not available Comorbidities: information not available Duration of autism: information not available Previous treatment: information not available |
|
| Interventions | Intervention group: acupuncture + applied behavior analysis (ABA) training + sensory integration training + educational program Acupuncture: needles were inserted to the following main acupoints: GV24, GV20, EX‐HN1, GV17, GV18, PC6, HT7, PC8, ST36, KI7, KI3, speech area 2 and 3, sensory area, psychosensory area, visual area, auricular area, and frontal 5 points. Patients with hyperactivity were treated additionally at SI3, SJ6, LU7, LU3, ST42, and BL58. Patients with restricted activity and echolalia were treated additionally at ST40 and LU3. Patients with hoarse or low voice were treated additionally at LU10, KD6, Ren 23, and GV15. Patients with insomnia were treated additionally at KD6 and BL62. Needles were left for 25 minutes/session, daily for 5 days/week for 6‐weekly courses for total 2‐3 courses. Control group: applied behavior analysis (ABA) training + sensory integration training + educational program |
|
| Outcomes | Chinese version of Psychoeducational Profile (CPEP) Frequency of improvement in CPEP |
|
| Notes | Dropouts: none Duration of follow‐up: 18 weeks Acupuncture paradigm: Traditional Chinese Medicine paradigm Training or qualification of acupuncture therapist: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Random group allocation according to sequence of clinic attendance |
| Allocation concealment (selection bias) | High risk | Random group allocation according to sequence of clinic attendance. The allocation is likely not concealed |
| Blinding (performance bias and detection bias) All outcomes | High risk | No blinding was described. Since the intervention involves acupuncture, it is highly likely that the treating physicians and patients were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data were complete |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | High risk | The mean age of the intervention group and that of the control group differs by 1 year. The baseline score on Imitation was lower in the intervention group. These baseline differences may confound treatment effects. Acupoints and treatment duration varied among patients and might introduce bias. No placebo or sham control was used and hence there might be placebo effect |
Zhou 2008.
| Methods | Design: parallel groups Randomization method: not described Method of allocation concealment: not described Blinding: not described Stratification: not used |
|
| Participants | Inclusion criteria: age 2‐10 years, ASD diagnosed by Aberrant Behavioral Checklist (ABC), language delay diagnosed by China Rehabilitation Research Center (CRRC) sign‐significance relations scale Exclusion criteria: no Number of participants (Intervention:control): 16:14 Number of males (Intervention:control): 12:10 Age: intervention group: mean 5.6 years (SD 2.3 years); control group: mean 5.8 years (SD 2.6 years). Specific diagnosis/diagnostic subtypes: information not available Comorbidities: information not available Duration of autism: information not available Previous treatment: information not available |
|
| Interventions | Intervention group: acupressure + language therapy Acupressure: thumb was used to apply pressure in a clockwise direction to the following acupoints: LI20, GV26, ST4, about 100 times for each point, and then upper lip muscles were massaged for 2‐3 minutes. Index and middle fingers were used to apply pressure similarly to the following acupoints: ST7, SJ17, ST6, Ren23, Ren24, and cheek, lower lip, submental and parapharyngeal muscles were slowly massaged for 2‐3 minutes, then upper and lower lip muscles were opposed together. Then pressure was applied to the following acupoints: DU15, DU16, DU17, DU20, GV14, about 100 times for each point, and frontal and temporal regions on the head were massaged. The whole treatment lasted for 45 minutes/session, daily for 5 days/week, for 6‐9 months. Control group: language therapy alone (same as intervention group) |
|
| Outcomes | Frequency of improvement in China Rehabilitation Research Center (CRRC) sign‐significance relations scale Frequency of improvement in basic developmental assessment |
|
| Notes | Dropouts: none Duration of follow‐up: 9 months Acupuncture paradigm: Traditional Chinese Medicine paradigm Training or qualification of acupuncture therapist: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Information not available |
| Blinding (performance bias and detection bias) All outcomes | High risk | No blinding was described. Since the intervention involves acupressure, it is highly likely that the treating physicians and patients were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data were complete |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | Unclear risk | Treatment duration varied among patients and might introduce bias. No placebo or sham control was used and hence there might be placebo effect |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Liu 2008 | RCT comparing acupuncture with sensory integration therapy; no placebo or sham or no treatment control |
| Ma 2006 | Non‐randomized clinical trial |
| Wu 2008 | Non‐randomized clinical trial |
| Yuan 2007 | Non‐randomized clinical trial. Acupuncture compared with integrative therapy; no placebo or sham or no treatment control |
| Yuan 2009a | Non‐randomized clinical trial. Acupuncture compared with behavioral intervention; no placebo or sham or no treatment control |
| Yuan 2009b | Non‐randomized clinical trial. Acupuncture compared with behavioral education and sensory integration training; no placebo or sham or no treatment control |
| Zhang 2005 | Non‐randomized clinical trial. Acupuncture compared with herbal medicine, no placebo or sham or no treatment control |
Differences between protocol and review
The descriptions of primary and secondary outcomes were modified in the review for better clarity.
The primary outcome was changed from "Behavioral observations and standardized assessments of autistic behaviors" to: "Core features of ASD, i.e. social interaction, communication and behavioral problems including stereotypy or restricted, repetitive patterns of behavior, interests or activities, as measured by validated instruments and behavioral observations, such as Aberrant Behavior Checklist (ABC) (Aman 1986), Ritvo‐Freeman Real Life Rating Scale (RFRLRS) (Freeman 1986), Autism Treatment Evaluation Checklist (ATEC) (Rimland 1999), and Autism Diagnostic Observation Scale (ADOS) (Lord 1997)."
The descriptions of measures for secondary outcomes were largely deleted.
Contributions of authors
DKL Cheuk: conceiving the review; designing the review; coordinating the review; data collection for the review; designing search strategies; undertaking searches; screening search results; organizing retrieval of papers; screening retrieved papers against eligibility criteria; appraising risk of bias in papers; extracting data from papers; writing to authors of papers for additional information; obtaining and screening data on unpublished studies; data management for the review; entering data into Review Manager 5; analysis of data; interpretation of data; providing a methodological perspective; providing a clinical perspective; writing the protocol and final review.
WX Chen: data collection for the review; designing search strategies; undertaking searches; screening search results; organizing retrieval of papers; screening retrieved papers against eligibility criteria; appraising quality of papers; extracting data from papers; writing to authors of papers for additional information; obtaining and screening data on unpublished studies; data management for the review; entering data into Review Manager 5; analysis of data; interpretation of data; providing a methodological perspective; providing a clinical perspective; writing the protocol and final review.
V Wong: conceiving the review, designing the review; coordinating the review; appraising quality of papers; writing to authors of papers for additional information; interpretation of data; providing a clinical perspective; writing the protocol; providing general advice on the review; performing previous work that was the foundation of the current review; writing the protocol and final review.
Sources of support
Internal sources
The University of Hong Kong, Hong Kong.
External sources
No sources of support supplied
Declarations of interest
Daniel KL Cheuk ‐ none known.
Virginia Wong and Wen Xiong Chen were involved in a funded project on 'Integration of Traditional Chinese Medicine (Acupuncture) in Interventional Program of Children with Autistic Spectrum Disorder (or Autism)' with Tung Wah Group of Hospitals locally in Hong Kong that was performed from 2004‐2007. Paper published: WX Chen, WL Liu, V Wong. Electroacupuncture for Children with Autism Spectrum Disorder. Pilot study of 2 cases. The Journal of Alternative and Complementary Medicine 14(8); 1057‐1‐65, 2008.
Edited (no change to conclusions)
References
References to studies included in this review
Allam 2008 {published data only}
- Allam H, Eldine NG, Helmy G. Scalp acupuncture effect on language development in children with autism: a pilot study. Journal of Alternative and Complementary Medicine 2008;14(2):109‐14. [DOI] [PubMed] [Google Scholar]
Chan 2009 {published data only}
- Chan AS, Cheung M, Sze SL, Leung WW. Seven‐star needle stimulation improves language and social interaction of children with autistic spectrum disorders. American Journal of Chinese Medicine 2009;37(3):495‐504. [DOI] [PubMed] [Google Scholar]
Wang 2007 {published data only}
- Wang CN, Liu Y, Wei XH, Li LX. Effects of electroacupuncture combined with behavior therapy on intelligence and behavior of children of autism [Dian Zhen Pei He Xing Wei Liao Fa Dui Gu Du Zheng Huan Er Xing Wei Neng Li Ji Zhi Neng De Ying Xiang]. Chinese Acupuncture & Moxibustion 2007;27(9):660‐2. [PubMed] [Google Scholar]
- Wang CN, Shang SY, Wei XH. The influence of electroacupuncture plus behavior therapy on social behavior ability in autism children [Dian Zhen Pei He Xing Wei Liao Fa Dui Gu Du Zheng She Hui Shi Ying Xing Wei Neng Li De Ying Xiang]. Shanghai Journal of Acupuncture and Moxibustion 2006;25(12):19‐20. [Google Scholar]
Wong 2002 {published and unpublished data}
- Wong V, Sun JG. Research on tongue acupuncture in children with autism. The 9th International Child Neurology Congress & The 7th Asian & Oceanian Congress of Child Neurology. 2002.
Wong 2007 {unpublished data only}
- Wong V, Sun JG, Yeung DWC. Randomized controlled trial of using tongue acupuncture in autism spectrum disorder using PET scan for clinical correlation. Unpublished manuscript.
Wong 2008 {published and unpublished data}
- Wong CL. Acupuncture and autism spectrum disorders ‐ an assessor‐blinded randomized controlled trial (M Phil). Hong Kong: University of Hong Kong, 2008. [Google Scholar]
Wong 2010a {published and unpublished data}
- Wong VC, Sun JG. Randomized controlled trial of acupuncture versus sham acupuncture in autism spectrum disorder. Journal of Alternative and Complementary Medicine 2010;16(5):545‐53. [DOI] [PubMed] [Google Scholar]
Wong 2010b {published and unpublished data}
- Wong VCN, Chen WX. Randomized controlled trial of electro‐acupuncture for autism spectrum disorder. Alternative Medicine Review 2010;15(2):136‐46. [PubMed] [Google Scholar]
Yan 2007 {published data only}
- Yan Y, Wei Y, Chen Y, Chen M. Effect acupuncture on rehabilitation training of child's autism. Chinese Acupuncture & Moxibustion 2007;27(7):503‐5. [PubMed] [Google Scholar]
Zhou 2008 {published data only}
- Zhou H, Zhang P. The effect of language therapy combined with point massage on communication disability in autism children. China Practical Medical 2008;3(23):24‐6. [Google Scholar]
References to studies excluded from this review
Liu 2008 {published data only}
- Liu G, Yuan LX. Acupuncture for autistic children: clinical research [Zhen Ci Zhi Liao Er Tong Zi Bi Zheng Lin Chuang Yan Jiu]. Liaoning Journal of Traditional Chinese Medicine 2008;35(2):273‐4. [Google Scholar]
- Liu G, Yuan LX. Clinical observe of acupuncture treat autism. Chinese Archives of Traditional Chinese Medicine 2007;25(12):2497‐8. [Google Scholar]
Ma 2006 {published data only}
- Ma RL, Yang Q, Jin R. Effect of acupuncture combined behavior intervention on children with autism [Zhen Ci Pei He Xing Wei Gan Yu Liao Fa Dui Er Tong Zi Bi Zheng Xing Wei De Ying Xiang]. Chinese Journal of Integrated Traditional and Western Medicine 2006;26(5):419‐22. [PubMed] [Google Scholar]
Wu 2008 {published data only}
- Wu ZF. The clinical applied research with JIN's 3‐needle therapy in treating autism children (MA). Guangzhou: University of Chinese Medicine, 2008. [Google Scholar]
Yuan 2007 {published data only}
- Yuan Q, Chai T, Lang JY, Wang RC, Wu ZF. Effect of acupuncture for autism in children: an observation of 40 cases. Journal of Guangzhou University of Traditional Chinese Medicine 2007;24(3):208‐14. [Google Scholar]
Yuan 2009a {published data only}
- Yuan Q, Wang RC, Wu ZF, Zhao Y, Bao XJ, Jin R. Observation on clinical therapeutic effect of JIN's 3‐needling therapy on severe autism [Jin San Zhen Zhi Liao Zhong Du Zi Bi Zheng Liao Xiao Dui Zhao Guan Cha]. Chinese Acupuncture & Moxibustion 2009;29(3):177‐80. [PubMed] [Google Scholar]
Yuan 2009b {published data only}
- Yuan Q, Wu ZF, Wang RC, Liu G, Bao XJ, Lang JY. Analysis of therapeutic effect of Jin's three‐needling therapy on children autism with different TCM syndrome types [Jin San Zhen Zhi Liao Er Tong Zi Bi Zheng Bu Tong Zhong Yi Zheng Xing Liao Xiao Fen Xi]. Journal of Guangzhou University of Tranditional Chinese Medicine 2009;26(3):241‐4. [Google Scholar]
- Yuan Q, Wu ZF, Wang RC, Zhao Y, LangJY. Therapeutic effect of acupuncture on clinical symptoms in autistic children. Journal of New Chinese Medicine 2009;41(3):83‐5. [Google Scholar]
- Yuan, Q, Wu ZF, Wang RC, Deng JJ, Zhou HL, Lang JY. Observation on the therapeutic effect of acupuncture treatment of autism children [Zhen Ci Dui Bu Tong Bing Qinq Cheng Du Er Tong Zi Bi Zheng Liao Xiao Fen Xi]. Acupuncture Research 2009;34(3):183‐7. [PubMed] [Google Scholar]
Zhang 2005 {published data only}
- Zhang Q. Clinical and experimental research on acupuncture for autistic children with language disorder. Guangzhou: University of Chinese Medicine, 2001. [Google Scholar]
- Zhang Q, Jin R. Clinical research on acupuncture treatment of aphasia in autism children. World Journal of Acupuncture‐Moxibustion 2005;15(4):19‐22. [Google Scholar]
- Zhang Q, Yu R, Pang J, Zhou Y, Zhou Y, Jin R. Acupuncture induced changes of the event related potential P3 latency and wave amplitude in autistic children with language disorder. Chinese Journal of Clinical Rehabilitation 2005;9(20):10‐1. [Google Scholar]
- Zhang Q, Yu R, Pang J, Zhou Y, Zhou Y, Jin R. Effect of acupuncture in improving intelligence and language disorder of autistic children. Chinese Journal of Clinical Rehabilitation 2005;9(28):112‐3. [Google Scholar]
Additional references
AAP 2001
- Committee on Children with Disabilities. Counseling families who choose complementary and alternative medicine for their child with chronic illness or disability. Pediatrics 2001;107(3):598‐601. [PubMed] [Google Scholar]
Ahn 2005
- Ahn AC, Wu J, Badger GJ, Hammerschlag R, Langevin HM. Electrical impedance along connective tissue planes associated with acupuncture meridians. BMC Complementary and Alternative Medicine 2005;5:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Aman 1986
- Aman M, Singh N. Aberrant Behaviour Checklist: Manual. New York: Slosson Educational Publications, 1986. [Google Scholar]
APA 2000
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders DSM‐IV‐TR Fourth Edition (Text Revision). American Psychiatric Association, 2000. [Google Scholar]
Araghi‐Niknam 2003
- Araghi‐Niknam M, Fatemi SH. Levels of Bcl‐2 and P53 are altered in superior frontal and cerebellar cortices of autistic subjects. Cellular and Molecular Neurobiology 23;6:945‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Baird 2006
- Baird G, Simonoff E, Pickles A, Chandler S, Loucas T, Meldrum D, et al. Prevalence of disorders of the autism spectrum in a population cohort of children in South Thames: the Special Needs and Autism Project (SNAP). Lancet 2006;368(9531):210‐5. [DOI] [PubMed] [Google Scholar]
Bryson 2003
- Bryson SE, Rogers SJ, Fombonne E. Autism spectrum disorders: early detection, intervention, education, and psychopharmacological management. Canadian Journal of Psychiatry 2003;48(8):506‐16. [DOI] [PubMed] [Google Scholar]
Buehler 2011
- Buehler MR. A proposed mechanism for autism: an aberrant neuroimmune response manifested as a psychiatric disorder. Medical Hypotheses 2011;76:863‐70. [DOI] [PubMed] [Google Scholar]
Burd 1987
- Burd L, Fisher W, Kerbeshian J. A prevalence study of pervasive developmental disorders in North Dakota. Journal of American Academy of Child and Adolescent Psychiatry 1987;26(5):700‐3. [DOI] [PubMed] [Google Scholar]
Carlson 2011
- Carlson GC. Glutamate receptor dysfunction and drug targets across models of autism spectrum disorders. Pharmacology Biochemistry and Behavior 15 Feb 2011 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chao 2010
- Chao HT, Chen HC, Samaco RC, Xue M, Chahrour M, Yoo J, et al. Dysfunction in GABA signalling mediates autism‐like stereotypies and Rett syndrome phenotypes. Nature 2010;468:263‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chauhan 2006
- Chauhan A, Chauhan V. Oxidative stress in autism. Pathophysiology 2006;13(3):171‐81. [DOI] [PubMed] [Google Scholar]
Chen 2008
- Chen WX, WL Liu, Wong VC. Electroacupuncture for children with autism spectrum disorder: pilot study of 2 cases. Journal of Alternative and Complementary Medicine 2008;14(8):1057‐65. [DOI] [PubMed] [Google Scholar]
Correia 2010
- Correia CT, Coutinho AM, Sequeira AF, Sousa IG, Lourenço Venda L, Almeida JP, et al. Increased BDNF levels and NTRK2 gene association suggest a disruption of BDNF/TrkB signaling in autism. Genes Brain and Behaviour 2010;9(7):841‐8. [DOI] [PubMed] [Google Scholar]
Dung 1984
- Dung HC. Anatomical features which contribute to the formation of acupuncture points. American Journal of Acupuncture 1984;12:139‐44. [Google Scholar]
Dunn 1961
- Dunn HL. High‐Level Wellness. Arlington, VA: Beatty Press, 1961. [Google Scholar]
Edwards 1997
- Edwards S, Fletcher P, Garman M, Hughes A, Letts C, Sinka I. The Reynell Developmental Language Scales III. Windsor: NFER‐Nelson, 1997. [Google Scholar]
Elbourne 2002
- Elbourne DR, Altman DG, Higgins JPT, Curtin F, Worthington HV, Vail A. Meta‐analyses involving cross‐over trials: methodological issues. International Journal of Epidemiology 2002;31(1):140‐9. [DOI] [PubMed] [Google Scholar]
Ernst 2001
- Ernst E, White AR. Prospective studies of the safety of acupuncture: a systematic review. American Journal of Medicine 2001;110:481‐5. [DOI] [PubMed] [Google Scholar]
Faras 2010
- Faras H, Al Ateeqi N, Tidmarsh L. Autism spectrum disorders. Annals of Saudi Medicine 2010;30(4):295‐300. [DOI] [PMC free article] [PubMed] [Google Scholar]
Folstein 1991
- Folstein SE, Piven J. Etiology of autism: genetic influences. Pediatrics 1991;87(5 Pt 2):767‐73. [PubMed] [Google Scholar]
Freeman 1986
- Freeman BJ, Ritvo ER, Yokota A, Ritvo A. A scale for rating symptoms of patients with the syndrome of autism in real life settings. Journal of the American Academy of Child and Adolescent Psychiatry 1986;25(1):130‐6. [DOI] [PubMed] [Google Scholar]
Fu 2000
- Fu H. What is the material base of acupuncture? The nerves!. Medical Hypotheses 2000;54(3):358‐9. [DOI] [PubMed] [Google Scholar]
Fu 2009
- Fu LW, Longhurst JC. Electroacupuncture modulates vIPAG release of GABA through presynaptic cannabinoid CB1 receptors. Journal of Applied Physiology 2009;106:1800‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Furlan 2005
- Furlan AD, Tulder MW, Cherkin DC, Tsukayama H, Lao L, Koes BW, Berman BM. Acupuncture and dry‐needling for low back pain. Cochrane Database of Systematic Reviews 2005, Issue 1. [DOI: 10.1002/14651858.CD001351.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Godlee 2011
- Godlee F, Smith J, Marcovitch H. Wakefield's article linking MMR vaccine and autism was fraudulent. British Medical Journal 2011;342:c7452. [DOI] [PubMed] [Google Scholar]
Griffiths 1996
- Griffiths R, Huntley M. The Griffiths Mental Development Scales: From Birth to 2 Years. Henley‐on‐Thames, UK: Test Agency Ltd, 1996. [Google Scholar]
Gringras 2000
- Gringras P. Practical paediatric psychopharmacological prescribing in autism. Autism 2000;4(3):229‐47. [Google Scholar]
Haley 1992
- Haley SM, Coster WJ, Ludlow LH, Haltiwanger JT, Andrellos PJ. Pediatric Evaluation of Disability Inventory (PEDI). San Antonio TX: Pearson, 1992. [Google Scholar]
Hanson 2007
- Hanson E, Kalish LA, Bunce E, Curtis C, McDaniel S, Ware J, et al. Use of complementary and alternative medicine among children diagnosed with autism spectrum disorder. Journal of Autism and Developmental Disorders 2007;37(4):628‐36. [DOI] [PubMed] [Google Scholar]
Harrington 2006
- Harrington JW, Rosen L, Garnecho A, Patrick PA. Parental perceptions and use of complementary and alternative medicine practices for children with autistic spectrum disorders in private practice. Journal of Developmental and Behavioral Pediatrics 2006;27(2 Suppl):S156‐61. [DOI] [PubMed] [Google Scholar]
Helms 2007
- Helms JM. Acupuncture energetics: a clinical approach for physicians. Stuttgart: Thieme Publishing Group, 2007. [Google Scholar]
Higgins 2011
- Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. Chichester, UK: The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. [Google Scholar]
Jansen 1989
- Jansen G, Lundeberg T, Kjartansson S, Samuelson UE. Acupuncture and sensory neuropeptides increase cutaneous blood flow in rats. Neuroscience Letters 1989;97:305‐9. [DOI] [PubMed] [Google Scholar]
Johansson 1993
- Johansson K, Lindgren I, Widner H. Can sensory stimulation improve the functional outcome in stroke patients. Neurology 1993;43:2189‐92. [DOI] [PubMed] [Google Scholar]
Kim 2010
- Kim SK, Bae H. Acupuncture and immune modulation. Autonomic Neuroscience: Basic and Clinical 2010;157:38‐41. [DOI] [PubMed] [Google Scholar]
Lee 2010
- Lee GJ, Yin CS, Choi SK, Choi S, Yang JS, Lee H, et al. Acupuncture attenuates extracellular glutamate level in global ischemia model of rat. Neurology Research 2010;Suppl 1:79‐83. [DOI] [PubMed] [Google Scholar]
Leiter 1980
- Leiter 1980. Leiter International Performance Scale Instruction manual. Revised. Wood Dale, IL: Stoelting, 1980. [Google Scholar]
Leung 2009
- Leung PC, Zhang L, Cheng KF. Acupuncture: Complications are preventable not adverse events. Chinese Journal of Integrative Medicine 2009;15(3):229‐32. [DOI] [PubMed] [Google Scholar]
Levy 2003
- Levy SE, Mandell DS, Merhar S, Ittenbach RF, Pinto‐Martin JA. Use of complementary and alternative medicine among children recently diagnosed with autistic spectrum disorder. Journal of Developmental and Behavioral Pediatrics 2003;24(6):418‐23. [DOI] [PubMed] [Google Scholar]
Leyfer 2006
- Leyfer OT, Folstein SE, Bacalman S, Davis NO, Dinh E, Morgan J, et al. Comorbid psychiatric disorders in children with autism: interview development and rates of disorders. Journal of Autism and Developmental Disorders 2006;36(7):849‐61. [DOI] [PubMed] [Google Scholar]
Li 2009
- Li J, Liu JM, Liu XQ, Liang FX, Wang H. Influence on electroacupuncture at "Qiangzhuang" acupoints for neuro‐immune regulation of sub‐acute aged rats. Chinese Acupuncture and Moxibustion 2009;29(11):905‐9. [PubMed] [Google Scholar]
Lin 2008
- Lin JG, Chen WL. Acupuncture analgesia: a review of its mechanisms of actions. American Journal of Chinese Medicine 2008;36(4):635‐45. [DOI] [PubMed] [Google Scholar]
Liu 2004
- Liu JH, Yan J, Yi SX, Chang XR, Lin YP, Hu JM. Effects of electroacupuncture on gastric myoelectric activity and substance P in the dorsal vagal complex of rats. Neuroscience Letters 2004;356(2):99‐102. [DOI] [PubMed] [Google Scholar]
Lord 1994
- Lord C, Rutter M, Couteur A. Autism Diagnostic Interview‐Revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism & Developmental Disorders 1994;24:659‐85. [DOI] [PubMed] [Google Scholar]
Lord 1997
- Lord C, Rutter M, DiLavore PC. Autism Diagnostic Observation Scale ‐ Generic. Chicago, IL: University of Chicago Press, 1997. [Google Scholar]
Lowe 1976
- Lowe M, Costello AJ. Manual for the symbolic play test. Windsor: National Foundation for Educational Research, 1976. [Google Scholar]
Maciocia 1989
- Maciocia G. Foundations of Chinese Medicine: A comprehensive Text for Acupuncturists and Herbalists. Edinburgh: Churchill Livingstone, 1989. [Google Scholar]
Madsen 2002
- Madsen KM, Hviid A, Vestergaard M, Schendel D, Wohlfahrt J, Thorsen P, et al. A population‐based study of measles, mumps, and rubella vaccination and autism. New England Journal of Medicine 2002;347:1477‐82. [DOI] [PubMed] [Google Scholar]
Magnusson 1994
- Magnusson M, Johansson K, Johansson BB. Sensory stimulation promotes normalization of postural control after stroke. Stroke 1994;25:1176‐80. [DOI] [PubMed] [Google Scholar]
Manni 2010
- Manni L, Albanesi M, Guaragna M, Barbaro Paparo S, Aloe L. Neurotrophins and acupuncture. Autonomic Neuroscience: Basic and Clinical 2010;157:9‐17. [DOI] [PubMed] [Google Scholar]
Middlekauff 2004
- Middlekauff HR, Shah JB, Yu JL, Hui K. Acupuncture effects on autonomic responses to cold pressor and handgrip exercise in healthy humans. Clinical Autonomic Research 2004;12(2):113‐8. [DOI] [PubMed] [Google Scholar]
Moazzami 2010
- Moazzami A, Tjen‐A‐Looi SC, Guo ZL, Longhurst JC. Serotonergic projection from nucleus raphe pallidus to rostral ventrolateral medulla modulates cardiovascular reflex responses during acupuncture. Journal of Applied Physiology 2010;108:1336‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
Msall 1994
- Msall ME, DiGaudio K, Rogers BT, LaForest S, Catanzaro NL, Campbell J, et al. The functional independence measure for children (WeeFIM). Conceptual basis and pilot use in children with developmental disabilities. Clinical Pediatrics 1994;33:421‐30. [DOI] [PubMed] [Google Scholar]
Muhle 2004
- Muhle R, Trentacoste SV, Rapin I. The genetics of autism. Pediatrics 2004;113(5):e472‐86. [DOI] [PubMed] [Google Scholar]
NIH 1998
- NIH Consensus Conference. Acupuncture. JAMA 1998;280:1518‐24. [PubMed] [Google Scholar]
Posey 2001
- Posey DJ, McDougle CJ. Pharmacotherapeutic management of autism. Expert Opinion on Pharmacotherapy 2001;2(4):587‐600. [DOI] [PubMed] [Google Scholar]
Rapin 2008
- Rapin I, Tuchman RF. What is new in autism?. Current Opinion in Neurology 2008;21(2):143‐9. [DOI] [PubMed] [Google Scholar]
RevMan 2011 [Computer program]
- The Cochrane Collaboration. Review Manager (RevMan). Version 5.1. Copenhagen: The Nordic Cochrane Centre: The Cochrane Collaboration, 2011.
Rimland 1999
- Rimland B, Edelson SM. Autism Treatment Evaluation Checklist (ATEC). Available online: http://www.autism.com/ari/atec/atec‐online.htm 1999.
Rossignol 2009
- Rossignol DA. Novel and emerging treatments for autism spectrum disorders: a systematic review. Annals of Clinical Psychiatry 2009;21(4):213‐36. [PubMed] [Google Scholar]
Sajdel‐Sulkowska 2009
- Sajdel‐Sulkowska EM, Xu M. Increase in cerebellar neurotrophin‐3 and oxidative stress markers in autism. Cerebellum 2009;8:366‐72. [DOI] [PubMed] [Google Scholar]
SCSSS 1999
- Swedish Collaberation on Sensory Stimulation in Stroke. Sensory stimulation after stroke: a randomized controlled trial. Cerebrovascular Diseases 1999;9(Suppl 11):28. [Google Scholar]
Sheikh 2010a
- Sheikh AM, Malik M, Wen G, Chauhan A, Chauhan V, Gong CX, et al. BDNF‐Akt‐Bcl2 antiapoptotic signaling pathway is compromised in the brain of autistic subjects. Journal of Neuroscience Research 2010;88:2641‐7. [DOI] [PubMed] [Google Scholar]
Sheikh 2010b
- Sheikh AM, Li X, Wen G, Tauqeer Z, Brown WT, Malik M. Cathepsin D and apoptosis related proteins are elevated in the brain of autistic subjects. Neuroscience 2010;165:363‐70. [DOI] [PubMed] [Google Scholar]
Skuse 2004
- Skuse D, Warrington R, Bishop D, Chowdhury U, Lau J, Mandy W, et al. The developmental, dimensional and diagnostic interview (3di): a novel computerized assessment for autism spectrum disorders. Journal of the American Academy of Child and Adolescent Psychiatry 2004;43:548‐58. [DOI] [PubMed] [Google Scholar]
Stux 1998
- Stux G, Pomeranz B. Chapter 2 ‐ Scientific Basis of Acupuncture. Basics of Acupuncture. 4th Edition. New York: Springer, 1998:6‐23. [Google Scholar]
Sun 2001
- Sun HL, Li XM. Clinical study on treatment of cerebral apoplexy with penetration needling of scalp acupoints [Tou xue tou ci zhi liao nao zu zhong lin chuang yan jiu]. Chinese Acupuncuture and Moxibustion 2001;21(5):275‐8. [Google Scholar]
Taylor 2002
- Taylor B, Miller E, Lingam R, Andrews N, Simmons A, Stowe J. Measles, mumps, and rubella vaccination and bowel problems or developmental regression in children with autism: population study. British Medical Journal 2002;324:393‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wakefield 1998
- Wakefield AJ, Murch SH, Anthony A, Linnell J, Casson DM, Malik M, et al. Ileal‐lymphoid‐nodular hyperplasia, non‐specific colitis, and pervasive developmental disorder in children. Lancet 1998;351:637‐41. [DOI] [PubMed] [Google Scholar]
Wang 2009
- Wang Q, Peng Y, Chen S, Gou X, Hu B, Du J, et al. Pretreatment with electroacupuncture induces rapid tolerance to focal cerebral ischemia through regulation of endocannabinoid system. Stroke 2009;40:2157‐64. [DOI] [PubMed] [Google Scholar]
Wang 2011
- Wang H, Pang Y, Xue B, Wang X, Zhao F, Jia J. The anti‐oxidative effect of electro‐acupuncture in a mouse model of Parkinson's disease. PLoS One 2011;6(5):e19790. [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO 1992
- World Health Organization. International Statistical Classification of Diseases and Related Health Problem, Tenth Revision. Geneva: World Health Organization, 1992. [Google Scholar]
WHO 1993
- World Health Organization. WHOQoL Study Protocol. WHO (MNH7PSF/93.9). Geneva: WHO, 1993. [Google Scholar]
Williams 2008
- Williams E, Thomas K, Sidebotham H, Emond A. Prevalence and characteristics of autistic spectrum disorders in the ALSPAC cohort. Developmental Medicine and Child Neurology 2008;50(9):672‐7. [DOI] [PubMed] [Google Scholar]
Wing 1997
- Wing L, Leekam SR, Libby SJ, Gould J, Larcombe M. The diagnostic interview for social and communication disorders: background, inter‐rater reliability and clinical use. Journal of Child Psychology and Psychiatry 2002;43:307‐25. [DOI] [PubMed] [Google Scholar]
Wing 1999
- Wing L. Diagnostic Interview for Social and Communication Disorders (DISCO). 10. Kent: The National Autistic Society, 1999. [Google Scholar]
Wong 2006a
- Wong HH, Smith RG. Patterns of complementary and alternative medical therapy use in children diagnosed with autism spectrum disorders. Journal of Autism and Developmental Disorders 2006;36(7):901‐9. [DOI] [PubMed] [Google Scholar]
Wong 2006b
- Wong HH, Smith RG. Patterns of complementary and alternative medical therapy use in children diagnosed with autism spectrum disorders. Journal of Autism and Development Disorders 2006;36(7):901‐9. [DOI] [PubMed] [Google Scholar]
Wong 2009
- Wong VC. Use of Complementary and Alternative Medicine (CAM) in Autism Spectrum Disorder (ASD): Comparison of Chinese and Western Culture (Part A). Journal of Autism and Developmental Disorders 2009;39(3):454‐3. [DOI] [PubMed] [Google Scholar]
Wong 2010
- Wong FW, Lim CE, Smith W. A new bioimpedance research device (BIRD) for measuring the electrical impedance of acupuncture meridians. Journal of Alternative and Complementary Medicine 2010;16(3):257‐64. [DOI] [PubMed] [Google Scholar]
Wu 1996
- Wu JN. A short history of acupuncture. Journal of Alternative and Complementary Medicine 1996;2:19‐21. [DOI] [PubMed] [Google Scholar]
Yang 2010
- Yang EJ, Jiang JH, Lee SM, Hwang HS, Lee MS, Choi SM. Electroacupuncture reduces neuroinflammatory responses in symptomatic amyotrophic lateral sclerosis model. Journal of Neuroimmunology 2010;223:84‐91. [DOI] [PubMed] [Google Scholar]
Yoon 2010
- Yoon SS, Kim H, Choi KH, Lee BH, Lee YK, Lim SC, et al. Acupuncture suppresses morphine self administration through the GABA receptors. Brain Research Bulletin 2010;81:625‐30. [DOI] [PubMed] [Google Scholar]
Young 2011
- Young AMH, Campbell E, Lynch S, Suckling J, Powis SJ. Aberrant NF‐kappaB expression in autism spectrum condition: a mechanism for neuroinflammation. Frontiers in Psychiatry 2011;2:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhang 2008
- Zhang HZ, Zhang LX, She YF, Li WL, Zhang XJ, Zhang RJ. Effect of electroacupuncture on apoptosis of hippocampus tissue in mice with vascular dementia. Acupuncture Research 2008;33(6):377‐81. [PubMed] [Google Scholar]
Zhang 2010
- Zhang J, Shang H, Gao X, Ernst E. Acupuncture‐related adverse events: a systematic review of the Chinese literature. Bulletin of World Health Organization 2010;88:915‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]


