Abstract
Background
Burnout and work satisfaction have been shown to be associated with risk of commuting crashes and drowsy driving. Although health care workers (HCWs) were found to have high burnout, no study has yet examined the relationship between burnout and commuting crashes in this occupational group.
Objective
The objective of this study was to examine the relationships between burnout, commuting crashes and drowsy driving among HCWs.
Methods
A cross-sectional study was conducted among 291 HCWs in a tertiary hospital, using an online survey focusing on burnout subscales, work satisfaction, commuting crashes, and drowsy driving to and from work.
Results
One third of the sample population reported commuting crashes that led to physical, mental, and quality-of-life harms in more than half of them. Burnout was not associated with commuting crashes; however, it was associated with increased drowsy driving. Nurses reported on more physical, emotional, and quality-of-life harms, and administrative staff reported on more physical harm. Low work satisfaction was significantly associated with higher severity of reported mental harm (p = 0.01).
Conclusions
Burnout and commuting crashes are more common among physician and nurses, compared to other HCWs. Work satisfaction and sense of personal accomplishment can reduce the negative outcomes of commuting crashes and may contribute to recovery of HCWs after commuting crashes.
Keywords: Health care workers, Commuting crashes, Drowsy driving, Burnout, Work satisfaction
Introduction
In recent years, there is growing interest in health care workers' (HCWs’) health and well-being (Mohanty et al. 2019). HCWs put their lives on the line and are at increased risk for a variety of physical, mental, and social risks, such as chronic illnesses, and mental and psychological distress. Burnout, a psychological response to work stress defined by the 11th version of the International Classification of Diseases (ICD-11), as one of the risks HCWs are facing due to the stressful nature of their job (De Hert 2020), and is considered an occupational phenomenon (World Health Organization 2019). It is characterized by emotional exhaustion ([EE], lack of energy at work, feelings of emptiness, and lack of emotional resources); depersonalization ([DP], feelings of detachment, boredom, irritation, or hardness at work, leading to hostility and withdrawal from work and professional relationships with patients); and reduced feelings of personal accomplishment ([PA], feelings of competency, efficiency, and productivity at work) (Maslach et al. 1996).
The literature shows that HCWs are at a greater risk for burnout compared to the general population, and even compared to other helping professions, such as teachers (Alfuqaha and Alsharah 2018; West et al. 2020). Burnout among HCWs was previously found to be associated with work stress, lack of organizational support and appreciation, working in shifts, and dealing with high levels of uncertainty, trauma, and death (Duke et al. 2020; McHugh et al. 2011; See et al. 2018). The consequences of burnout among HCWs include higher absence and turnover rates, decreased productivity, leaving the profession, and low levels of patient satisfaction (Hoff Carabetta and Collinson 2019; Willard-Grace et al. 2019). In addition, burnout and work stress have implications on the safety of HCWs and their patients, such as: medical errors, malpractice, increased infection rates in hospitals, lawsuits, and work-related injuries (Jourdain and Chênevert 2010; Tawfik et al. 2018; Welp et al. 2015).
Commuting accidents also referred to as “commuting crashes”, are traffic crashes that occur while commuting to or from work (International Labour Organization, 2010). Most European countries (apart from the UK and Denmark) recognize injuries resulted from commuting crashes as occupational injuries (German Social Accident Insurance; Walters 2007). Similarly, in Israel, injuries from motor-vehicle accidents to or from work are acknowledged as work-related injuries by the workplace, and may be compensated through social security, depending on the severity of the injury (Work Injuries Guide 2021). However, in some countries, such as the United States and United Kingdom, injuries resulted from commuting crashes are not considered as occupational injuries (International Labour Organization, 2010; United States Department of Labor 2021).
Commuting crashes among HCWs received little attention in the literature compared to other occupational injuries. In a study among surgical residents, 10% reported they were involved in traffic crashes and 40% of which occurred during the commute from work (Barger et al. 2009). In another study, over half of internal medicine interns (n = 300) reported traffic crashes or near-misses (West Tan and Shanafelt 2012). In an urgent care department, nursing staff reported they were concerned about traffic safety after night shifts, especially as they often found it difficult to stay awake while driving, pass through red lights, and cannot always remember how they arrived home (Fallis McMillan and Edwards 2011).
In addition to commuting crashes, drowsy driving is a serious issue which may result in traffic crashes, injuries, and even death. Drowsy driving is the combination of driving and sleepiness or fatigue due to lack of sleep, sleep disorder, medications, substance use or shift work (CDC 2021). HCWs are at increased risk for drowsy driving while commuting due to the nature of their work, which often includes physical, emotional, and cognitive challenges over long periods and during unusual working hours (Green et al. 2020; Smith et al. 2020; Anderson et al. 2018). In one study, almost 80% of nurses reported drowsy driving (Scott et al. 2007). In other studies, nurses reported experiencing drowsy driving on a regular basis (Smith et al. 2020). Drowsy driving was previously found to be associated with commuting crashes and near-crashes (Smith et al. 2021; Anderson et al. 2018; Westwell et al. 2021).
Long shifts, night shifts, irregular shifts, fatigue and lower seniority level were found to be associated with more commuting crashes, near-misses and drowsy driving among HCWs, while younger age and male gender were found to be associated only with more commuting crashes and near-misses (Barger et al. 2005, 2009; Zuwairy et al. 2020; Smith et al. 2021; Freedman-Weiss et al. 2021; Green et al. 2020).
Burnout has physical, mental and cognitive implications that may put drivers at risk (Koutsimani et al. 2021; Leiter and Maslach, 2009). These include lower cognitive functioning, prolonged fatigue, severe injuries and mortality below the age of 45 years (Koutsimani et al. 2021; Salvagioni et al. 2017). Burnout and work stress were found to be risk factors for both traffic crashes and drowsy driving among non-HCWs occupational groups (Useche et al. 2017a, b; Chung and Wu 2013; Salvagioni et al. 2020). For example, in a longitudinal analysis the burnout sub-scale DP was found to be a risk factor for traffic crashes among teachers (Salvagioni et al. 2020). Among bus drivers, those with high job strain or high burnout, reported significantly more traffic crashes than those with low job strain or low burnout (Useche et al. 2017a). However, in a study among military truck drivers, there were no differences in burnout between drivers who were involved in traffic crashes versus those who have not, and driving safety was not significantly associated with burnout (Rosenbloom 2021). Other burnout-related factors such as fatigue and occupational stress were also found associated with traffic crashes in a systematic review of epidemiological studies (Robb et al. 2008).
Even though there is evidence that traffic crashes and drowsy driving are associated with burnout, there is a paucity of data regarding this relationship among HCWs, and there are currently no studies regarding the association between burnout and commuting crashes among this population. Only one study showed that burnout, together with lower quality of life and depression, increased the risk for traffic crashes involvement among HCWs (West Tan and Shanafelt 2012). Commuting crashes may have long-term implications on the physical and emotional wellbeing of HCWs. It is important to examine the associations between burnout and commuting crashes to improve the safety, health, and wellbeing of HCWs.
Objective
The objective of this study was to examine the relationships between burnout, commuting crashes and drowsy driving among HCWs.
Methods
A cross-sectional study was carried out among HCWs including: physicians, nurses, para-medical and administrative staff, using an online survey addressing commuting crashes, drowsy driving, burnout, and work satisfaction. HCWs were recruited from Rambam Medical Center (RMC) during September–November 2020.
RMC is located in the city of Haifa which is the center of the third-most populous metropolitan area in the country with an estimated population of half a million (Israel Central Bureau of Statistics-ICBS 2018). There are several main road axes that connect the city with the suburbs and nearby towns. Due to being a populous metropolitan area, during rush-hours entrances to the city can get crowded. Public transportation such as buses, trains and the bus-rapid transit system are also available for commuters. A recent report indicates Haifa is placed 9th out of 16 large cities in Israel, in the risk of being involved in a traffic crash with casualties (The National Authority for Road Safety 2021). RMC is the largest hospital in the Northern area of Israel, with 5900 employees and 1000 beds which can be extended to another 1000 emergency beds. Most physicians and nurses work in shifts, while administrative and para-medical staff work mostly during office hours. Some para-medical staff have on-call shifts as well. RMC provides free parking for all hospital employees, shuttle buses for shift-workers twice a day and taxis for on-call-night-shift-workers. The organization policy is to assist workers who were injured during working hours, including commuting injuries, to claim work injury social security benefits. Workers are also entitled to use their sick-leave days in cases of commuting crashes injuries.
Sample and sampling method
Ethical approval was obtained from the hospital’s Institutional Review Board. The survey was distributed among a convenience sample of HCWs. The survey was sent via a link to organizational emails and as a text massage to personal mobile phones of all hospital employees. Participants received two reminders to complete the research questionnaire. All workers who were employees of the hospital at the time of the survey were eligible to participate. Participation was anonymous and voluntary. Questionnaire completion was between 10 and 15 min.
Two hundred and ninety-one HCWs replied to the survey including: 60 physicians (21%), 107 nurses (37%), 65 para-medical staff (social workers, psychologists, dieticians and physiotherapists) (22%), and 59 administrative and support staff (human resources workers, secretaries, maintenance) (20%). These proportions are similar to their actual proportion of these sectors in the hospital (22, 33, 21, and 24%, respectively).
Questionnaire
The questionnaire was adopted from research tools in the literature in the fields of burnout and commuting crashes (Maslach Jackson and Leiter 1996; Barger et al. 2005; Ayas et al. 2006). The questionnaire was further developed in consultation with health professionals and tested for internal validity (Cronbach’s alpha). The following measures were included:
Dependent variables
Involvement in commuting crashes or drowsy driving incidents (while commuting to or from work): number of occurrences, time of occurrences, absences from work (number of days) (Barger et al. 2005; Ayas et al. 2006).
Severity of emotional, physical, or quality-of-life harms on a 5-point Likert scale (1 = not at all, 5 = very much), for example, “To what extent did you suffer physical harm due to a work-related-motor-vehicle accident?”
Independent variables
- The Abbreviated Maslach Burnout Inventory ([aMBI]; Maslach and Jackson 1986): nine items on a 7-point Likert scale (0 = not at all, 6 = everyday). The aMBI consists of three subscales on which each individual receives subscale scores:
- Emotional exhaustion (EE), three items: lack of energy to confront the working day, followed by feelings of being emptied and exhausted from emotional resources, and feelings of apathy and detachment in relation to work. A higher score on this scale indicates a high sense of EE. For example, “I feel emotionally drained from my work”, α = 0.80.
- Depersonalization (DP), three items: feelings of detachment, coldness, boredom, irritation, or hardness to the point of hostility, leading to withdrawal from work and professional relationships with clients or patients. A higher score on this scale indicates a high sense of DP. For example, “I feel I treat some patients as if they were impersonal objects”, α = 0.70.
- Personal accomplishment (PA), three items: feelings of competence, efficiency, and productivity. PA scale was reversed so that a higher score indicates a low sense of PA. For example, “I feel exhilarated after working closely with my patients”, α = 0.69.
-
2.
The overall aMBI reliability was α = 0.76. The aMBI was previously used in studies on burnout among HCWs such as physicians (Shaikh et al. 2019; McManus et al. 2004, 2002). The validity and reliability of the aMBI have been established by Riley Mohr and Waddimba (2018).
-
3.
Work satisfaction based on one item, “Please rate your overall satisfaction from your work”, on a scale of 1–10 (1 = not at all, 10 = very much).
-
4.
Work characteristics: sector (medical, nursing, para-medical, administrative), seniority (years), and shifts (number per week).
-
5.
Sociodemographic characteristics: age, gender, family status, education, financial status, and reported health status.
Data analysis
Descriptive statistics of prevalence rates, means, and standard deviations (S.D.) were computed for participants’ demographics. One-way ANOVA test was conducted to compare mean scores of the burnout sub-scales, work satisfaction, commuting crashes, and drowsy driving, among sectors. A series of multiple linear regressions were conducted to predict the factors associated with commuting crashes and drowsy driving. The models were controlled for work satisfaction, burnout subscales (EE, DP and PA), sector (physicians, nurses, para-medical and administrative), on-call shifts (yes/no), evening and night shifts (number of shifts per week), seniority (years), and gender (male/ female). The p value was set as < 0.05 for statistical significance. All statistical processing and analysis were performed using SPSS software, version 25 (IBM Corp., Armonk, N.Y., USA).
Results
Sample characteristics
Of the 291 HCWs who answered the research questionnaire, the average age was close to 45 years (SD = 10.70), most were women (79.7%), married (75.9%), and with higher education (81.5%). The sample included physicians (20.6%), nurses (36.8%), para-medical (22.3%) and administrative staff (20.3%). Most participants were working in a full-time position (72.5%) and 35.7% in on-call shifts. Most respondents reported their health status was good to very good (79.7%), and a quarter reported they had a chronic illness (24.1%). Table 1 presents the sample characteristics.
Table 1.
Socio-demographic, occupational and health characteristics of the total sample of patients (n = 291)
| Characteristic | Mean, S.D | |
|---|---|---|
| Age | 44.90 ± 10.70 | |
| Number of Children | 2.27 ± 1.38 | |
| Number of people in household | 3.70 ± 1.49 | |
| n | % | |
| Gender | ||
| Men | 59 | 20.3 |
| Women | 232 | 79.7 |
| Family status | ||
| Married | 221 | 75.9 |
| Not married | 70 | 24.1 |
| Education | ||
| High school/professional | 54 | 18.5 |
| BA/MA | 174 | 59.8 |
| PhD/MD | 63 | 21.7 |
| Sector | ||
| Physicians | 60 | 20.6 |
| Nurses | 107 | 36.8 |
| Para-medical | 65 | 22.3 |
| Administrative | 59 | 20.3 |
| Work capacity | ||
| Part-time | 80 | 27.5 |
| Full-time | 211 | 72.5 |
| Working on-call shifts (yes) | 104 | 35.7 |
| Health status | ||
| Bad-pretty good | 59 | 20.3 |
| Good/very good | 232 | 79.7 |
| Chronic illness (yes) | 70 | 24.1 |
Respondents were asked about their experience with commuting crashes and drowsy driving: number of incidents, timing of the incidents, and the severity of the physical, mental, and quality-of-life harms as result of the incidents. The results are presented in Table 2.
Table 2.
Commuting crashes and drowsy driving among the total sample and according to sector (Chi-Square)
| Physicians | Nurses | Para-medical | Administrative | Total | χ2 | |
|---|---|---|---|---|---|---|
| At least one crash | 25 (41.67%) | 39 (36.45%) | 14 (21.54%) | 12 (20.34%) | 90 (30.9%) | 10.55* |
| Time of crash | ||||||
| On the way to work | 5 (20.8%) | 19 (51.4%) | 5 (35.7%) | 8 (66.7%) | 37 (42.5%) | 8.93* |
| On the way from work | 19 (79.2%) | 18 (48.6%) | 9 (64.3%) | 4 (33.3%) | 50 (57.5%) | |
| Severity of injury | ||||||
| Physical | 10 (40%) | 22 (56.4%) | 6 (42.9%) | 9 (75%) | 47 (52.5%) | 4.76 |
| Mental | 13 (52%) | 28 (71.8%) | 8 (57.1%) | 6 (50%) | 55 (61.1%) | 3.46 |
| Quality of life | 11 (44%) | 27 (69.2%) | 9 (64.3%) | 3 (25%) | 50 (55.6%) | 9.28* |
| At least one drowsy driving incident | 42 (70%) | 75 (70.1%) | 24 (36.9%) | 23 (39.0%) | 164 (56.4%) | 29.97*** |
| Time of incident | ||||||
| On the way to work | 2 (4.8%) | 5 (7.2%) | 3 (13%) | 1 (4.8%) | 11 (7.1%) | 1.76 |
| On the way from work | 40 (95.2%) | 64 (92.8%) | 20 (87.0%) | 20 (95.2%) | 144 (92.9%) | |
| Injury severity | ||||||
| Mental | 20 (47.6%) | 26 (35.6%) | 3 (13.0%) | 4 (19.0%) | 53 (33.3%) | 10.22* |
| Quality of life | 18 (42.9%) | 14 (20%) | 5 (21.7%) | 5 (23.8%) | 42 (26.9%) | 7.54 |
*p < 0.05, **p < 0.01, ***p < 0.001
Of 31% of HCWs involved in at least one motor-vehicle accident, over half (56.4%) had at least one incident of drowsy driving. Most commuting crashes and drowsy driving incidents occurred while driving to or from work home, among all sectors. More than half had physical, mental, or quality-of-life harms as result of the of commuting crashes, and about one third had mental or quality-of-life harms as result of drowsy driving incidents (33.3% and 26.9%, respectively). Among the sectors, physicians and nurses had the highest rate of commuting crashes and drowsy driving. Nurses reported the highest number of mental and quality-of-life harms and administrative staff reported the most physical harm, as result of commuting crashes. Physicians reported the highest mental and quality-of-life harms as a result of drowsy driving.
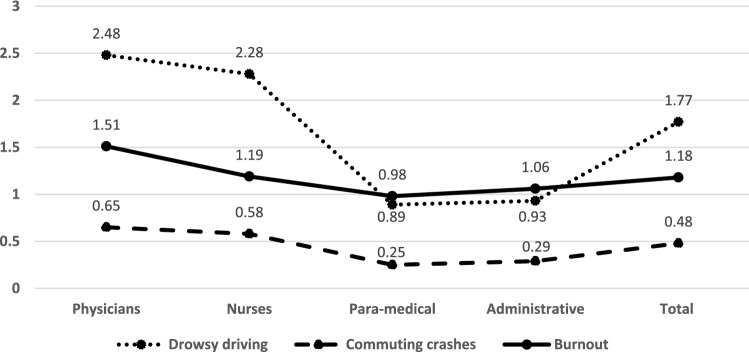
Participants were asked to report on their burnout levels and work satisfaction. Table 3 shows the results of the burnout sub-scales and overall burnout score and work satisfaction, according to sector and total sample. Figure 1 summarizes the means of the overall burnout score, commuting crashes and drowsy driving according to sector.
Table 3.
Mean scores of burnout subscales and work satisfaction among the total sample and according to sector
| Burnout (0–6) Mean (S.D.) | Physicians (n = 60) | Nurses (n = 107) | Para-medical (n = 65) | Administrative (n = 59) | Total (n = 291) | F (ANOVA) |
|---|---|---|---|---|---|---|
| EE | 2.38 (1.62) | 2.03 (1.48) | 1.51 (1.23) | 1.66 (1.57) | 1.91 (1.51) | 4.43** a, b |
| DP | 1.24 (1.32) | 0.68 (1.09) | 0.58 (1.01) | 0.50 (0.99) | 0.74 (1.13) | 5.47** a, b, c |
| PA | 0.89 (0.84) | 0.84 (1.03) | 0.84 (1.18) | 1.02 (1.38) | 0.89 (1.11) | 0.37 |
| Overall burnout | 1.51 (0.99) | 1.19 (0.85) | 0.98 (0.83) | 1.06 (0.96) | 1.18 (0.91) | 4.03** a, b |
| Work satisfaction (1–10) mean (S.D.) | 7.07 (2.02) | 7.23 (1.95) | 7.78 (1,82) | 8.05 (1.78) | 7.49 (1.93) | 3.85* a |
EE emotional exhaustion, DP depersonalization, PA personal accomplishment
*p < 0.05, **p < 0.01, ***p < 0.001
aPhysicians-administrative
bPhysicians-para-medical
cPhysicians-nurses
Fig. 1.
Means of overall burnout, commuting crashes and drowsy driving according to sector (physicians, nurses, para-medical, administrative)
The total burnout score was 1.18 (SD = 0.91). The highest score was reported in the EE subscale (mean = 1.91, SD = 1.51). Physicians had the highest burnout scores for all sub-scales and overall score. Administrative staff had the highest work satisfaction.
A series of multiple linear regression analyses were conducted to examine factors associated with commuting crashes and drowsy driving, and factors associated with physical, mental, and quality-of-life harms as result of commuting crashes. The results of the multiple linear regression analyses for commuting crashes and drowsy driving and factors associated with physical, mental and quality-of-life harms as result of commuting crashes are shown in Tables 4, 5.
Table 4.
Multiple linear regression analyses on predictors of commuting crashes and drowsy driving among HCW (n = 290)
| Commuting crashes | Drowsy driving | |||||
|---|---|---|---|---|---|---|
| B | SE | Βeta | B | SE | Βeta | |
| Work satisfaction | − 0.06 | 0.03 | − 0.13 | − 0.07 | 0.06 | − 0.08 |
| EE | 0.03 | 0.04 | 0.06 | 0.18 | 0.08 | 0.15* |
| DP | 0.09 | 0.05 | 0.12 | 0.00 | 0.09 | 0.00 |
| PA | − 0.05 | 0.04 | − 0.07 | − 0.17 | 0.08 | − 0.11* |
| Nurses | − 0.06 | 0.14 | − 0.03 | 0.30 | 0.26 | 0.08 |
| Para-medical | − 0.31 | 0.15 | − 0.16* | − 1.20 | 0.29 | − 0.28*** |
| Administrative | − 0.26 | 0.16 | − 0.13 | − 0.82 | 0.31 | − 0.19* |
| On-call shifts | 0.08 | 0.11 | 0.05 | 0.07 | 0.21 | 0.02 |
| Evening shifts | − 0.08 | 0.05 | − 0.12 | − 0.04 | 0.10 | − 0.02 |
| Night shifts | 0.07 | 0.07 | 0.09 | 0.17 | 0.13 | 0.10 |
| Seniority | 0.00 | 0.00 | 0.01 | − 0.04 | 0.01 | − 0.27*** |
| Gender | 0.21 | 0.13 | 0.10 | − 0.70 | 0.26 | − 0.16* |
| Overall model | F (12, 277) = 2.96*** | < 0.001 | F (12, 277) = 24.11*** | < 0.001 | ||
| Adjusted R2 = 0.08 | Adjusted R2 = 0.29 | |||||
EE emotional exhaustion, DP depersonalization, PA personal accomplishment
*p < 0.05, **p < 0.01, ***p < 0.001
Table 5.
Multiple linear regression analyses on predictors of reported severity of physical, mental and quality of life harm as result of commuting crashes among HCW who were involved in at least one traffic accident (n = 90)
| Physical | Mental | Quality of life | |||||||
|---|---|---|---|---|---|---|---|---|---|
| B | SE | Βeta | B | SE | Βeta | B | SE | Βeta | |
| Work satisfaction | − 0.03 | 0.06 | − 0.06 | − 0.20 | 0.08 | − 0.35* | − 0.16 | 0.08 | − 0.28 |
| EE | − 0.04 | 0.08 | − 0.07 | 0.11 | 0.10 | 0.15 | 0.04 | 0.11 | 0.06 |
| DP | 0.00 | 0.09 | 0.00 | -0.10 | 0.11 | − 0.11 | − 0.17 | 0.12 | − 0.19 |
| PA | 0.29 | 0.10 | 0.31** | 0.11 | 0.13 | 0.09 | 0.18 | 0.14 | 0.14 |
| Nurses | 0.60 | 0.27 | 0.33* | 0.89 | 0.33 | 0.37** | 0.82 | 0.37 | 0.34* |
| Para-medical | 0.40 | 0.31 | 0.16 | 0.01 | 0.38 | 0.00 | 0.16 | 0.42 | 0.05 |
| Administrative | 1.04 | 0.34 | 0.39*** | − 0.06 | 0.41 | − 0.02 | − 0.23 | 0.46 | − 0.07 |
| On-call shifts | 0.17 | 0.21 | 0.09 | 0.05 | 0.25 | 0.02 | − 0.08 | 0.28 | − 0.03 |
| Night shifts | 0.14 | 0.08 | 0.21 | 0.10 | 0.10 | 0.11 | − 0.09 | 0.11 | − 0.10 |
| Seniority | 0.01 | 0.01 | 0.12 | 0.00 | 0.01 | − 0.01 | − 0.02 | 0.01 | − 0.18 |
| Gender | 0.06 | 0.29 | 0.02 | 0.09 | 0.36 | 0.03 | − 0.19 | 0.40 | − 0.06 |
| Overall model | F (11, 78) = 2.19* | F (11, 78) = 3.65*** | F (11, 78) = 2.04*** | ||||||
| Adjusted R2 = 0.13 | Adjusted R2 = 0.24 | Adjusted R2 = 0.11 | |||||||
EE emotional exhaustion, DP depersonalization, PA personal accomplishment
*p < 0.05, **p < 0.01, ***p < 0.001
Results of the multivariate regressions show that the models were significant for predicting commuting crashes and drowsy driving incidents. The independent variables accounted for 8% of the variance in commuting crashes and 29% in drowsy driving. Belonging to the para-medical sector lowered the probability of having commuting crashes (p = 0.04). Other factors that were associated with more commuting crashes that came close to significant, were high DP (p = 0.07) and low work satisfaction (p = 0.06).
For drowsy driving, high EE (p = 0.02) and PA (p = 0.03) were both associated with increased reported drowsy driving. Physicians were at higher risk for drowsy driving compared to para-medical (p < 0.001) and administrative staff (p = 0.01). Lower seniority (p < 0.001) and male gender (p = 0.01) were also associated with increased drowsy driving.
Burnout sub-scales were not associated with severity of physical, emotional, and quality-of-life harms as result of commuting crashes, except for low PA that was associated with physical harm (p = 0.01). Nurses had the highest risk for physical, emotional and quality-of-life harms, and administrative staff for physical harm only. Work satisfaction was significant for mental harm and close to significant in quality-of-life harm (p = 0.06).
Discussion
The current study examined the association between burnout, work satisfaction and commuting crashes among HCWs. About one-third of participants were involved in commuting crashes and more than half reported physical, mental, and quality-of-life harms as a result. Physicians and nurses reported the highest proportion of commuting crashes and drowsy driving. The multiple linear regressions showed none of the burnout sub-scales were associated with commuting crashes. However, increased DP and low work satisfaction were close to significance. High EE and low PA were associated with increased number of drowsy driving incidents. Low PA was associated with physical harm due to commuting crashes. Low work satisfaction was significantly associated with mental harm and was close to significance with quality-of-life harm due to commuting crashes.
Characteristics of commuting crashes and drowsy driving among HCWs
Reports on commuting crashes and drowsy driving among HCWs vary among different studies. For example, commuting crashes among physicians range in studies between 10 and 56% (Barger et al. 2009; West Tan and Shanafelt 2012; Freedman-Weiss et al. 2021) and drowsy driving ranges between 13 and 80% among nurses (Vedaa et al. 2019; Scott et al. 2007; Dorrian et al. 2006, 2008). Our findings regarding reported commuting crashes and drowsy driving falls approximately in the middle of these ranges. We found that most reported commuting crashes and drowsy driving incidents occurred on the way home from work, which is concurrent with previous findings (Anderson et al. 2018; Barger et al. 2005). More than half of those who reported commuting crashes in the current study, also reported physical, mental, or quality-of-life harms as a consequence. Previous literature showed that work-related injuries affect the physical and mental health of HCWs, and may result in high absence, turnover, and costs (Cooke and Stephens 2017; Joseph and Joseph 2016). Since shift-work was previously associated with traffic crashes (Zuwairy et al. 2020; Freedman-Weiss et al. 2021), it is likely that among HCWs, traffic crashes will occur more commonly during commuting. Our findings raise the importance of treating commuting crashes as occupational traffic crashes universally. Recognizing commuting crashes as work-related, may lead to organizations taking actions to prevent and minimize the risk factors that contribute to commuting crashes.
Associations between commuting crashes, drowsy driving and burnout
There is a paucity of data regarding the association between traffic crashes and more specifically, between commuting crashes and burnout among HCWs. Only one previous study examined the relationship between traffic crashes and burnout among HCWs (West Tan and Shanafelt 2012), while others examined this relationship among different working populations (Useche et al. 2017a, b; Salvagioni et al. 2020). Our study attempts to fill this gap in the literature by exploring the association between burnout and commuting crashes and drowsy driving among HCWs.
Our findings show that after controlling for confounders, some aspects of burnout (EE and PA) were related to reports on drowsy driving but not to commuting crashes. Previous studies showed that burnout can influence mental and physical capacities (Deligkaris et al. 2014), and can compromise physical and cognitive skills, such as executive functions, attention and memory that are required for driving safely (Deligkaris et al. 2014; Oosterholt et al. 2012), which puts workers who experience burnout at risk. Therefore, although burnout was not associated with more commuting crashes among HCWs in the current study, it still affected drowsy driving which in turn may increase the risk of commuting crashes among HCWs.
Differences between sectors in burnout, commuting crashes, drowsy driving and resulted harms
Nurses and physicians reported the highest level of burnout, compared to the other sectors in this study. Nurses and physicians also reported the most commuting crashes and drowsy driving. Burnout among physicians and nurses has been previously examined in many studies and systematic reviews (Rotenstein et al. 2018; Chemali et al. 2019). It was found that physicians and nurses report high burnout and this is related to the many aspects of their occupation including long shifts, night shifts, and high exposure to trauma and death (Duke et al. 2020; See et al. 2018). The same causes for burnout (i.e., shift work and exposure to trauma) were also previously found to be associated with traffic crashes (Tawfik et al. 2018; Welp et al. 2015), which may explain why physicians and nurses in the current study reported higher frequency of both, compared to other sectors. These findings indicate that physicians and nurses should be treated as high-risk populations in terms of burnout and commuting crashes. Reducing burnout symptoms and fostering supportive working conditions, may contribute to road safety among these at-risk occupational groups.
Compared to physicians and nurses, administrative staff reported lower burnout and involvement in commuting crashes. However, they still reported more physical harm as result of commuting crashes. Physicians and nurses, on the other hand, reported more mental harm. Since burnout has a strong association with mental health disorders, such as: depression, anxiety and stress (Schonfeld and Bianchi 2016; Creedy et al. 2017), it is not surprising that those who experienced burnout also reported more mental health harms as result of the crash. The crash, as a stressful and traumatic experience, could have contributed the deterioration of mental health (Kenardy et al. 2015) that was already impacted by the experience of burnout, and therefore, physicians and nurses who experienced more burnout were also more prone to mental health adversities as a result of the crash.
The relationship between personal accomplishment, work satisfaction and harms as result of commuting crashes
The burnout subscale PA and low work satisfaction were both associated with different types of harm as result of commuting crashes. This may suggest that the sense of accomplishment, capacity, and fulfillment experienced at work has a protective effect from harms as a result of work-related injuries. Previous findings showed that work satisfaction is associated with returning to work after an injury or long illness (Libeson et al. 2020; Bloom et al. 2019). It could be that improving work satisfaction and sense of PA from work, may assist the recovery of HCWs affected by commuting crashes.
Sociodemographic associations with drowsy driving
The sociodemographic characteristics associated with drowsy driving included male gender and lower seniority. These were previously found to be associated with traffic crashes among HCWs and the general population (Zuwairy et al. 2020; Rios et al. 2020; Freedman-Weiss et al. 2021; The National Authority for Road Safety 2020), which strengthens the validity of our findings. These findings reflect the importance of raising awareness and allocating resources towards the safety of younger workers and male workers who are at higher risk for both burnout and commuting crashes (Dyrbye et al. 2014; Barger et al. 2005).
Study limitations
The current study had a few limitations. First, this was a small sample and most of the respondents were women, which may limit the generalizability of the findings. However, it should be noted that the majority of workers in the hospital are women (65%). Therefore, our sample is close to the true gender proportions. Second, all hospital workers were invited to participate. However, the study’s outcomes were not blinded from participants, and therefore, it could be that people chose to participate, because they had some experience with commuting crashes or drowsy driving. We do not have information regarding those who did not reply to the survey. All this could potentially have led to an overestimation of traffic accidents, drowsy driving and burnout. Conversely, the study revolves around sensitive issues and there might have been social desirability effect, which may result in an underestimation of burnout and the adverse outcomes of commuting crashes.
Third, the study was conducted in the midst of the COVID-19 pandemic. HCWs were at the frontline of this pandemic and, therefore, were exposed to its risks and negative impact, such as psychological distress, anxiety, depression, and burnout (Williamson et al. 2020; Denning et al. 2021). This may have contributed to higher reports of burnout. However, in this study, burnout prevalence and means were low among all sectors. One explanation can be social desirability. Another explanation is the increased public attention and organizational support at the time of the pandemic, that could potentially have led to an underestimation of burnout and overestimation of work satisfaction among HCWs in the current study. In addition, since this study was based on self-reports, there is likely to be some information and recall bias. To increase the accuracy of the self-reported information, respondents received full confidentiality and anonymity. The possible effect of confounding variables such as sector, gender, and work conditions were adjusted for in the regression analyses.
Conclusions
The current study reveals that some aspects of burnout are related to drowsy driving but not to commuting crashes among HCWs. Both commuting crashes and drowsy driving were more commonly reported among physicians and nurses compared to other sectors. Our findings indicate that work satisfaction and sense of PA are associated with less severe harms of commuting crashes. This suggest that improving the sense of work accomplishment and satisfaction may contribute to the recovery of HCWs after commuting crashes.
There is a need to address the risk of commuting crashes and drowsy driving among HCWs as they pose a risk to their safety and wellbeing. This could include the implementation of a policy of mandatory 12 h rest between shifts, and shorter evening and night shifts to provide sufficient time to rest and regain strength (Vedaa et al. 2019). Hospitals can also supply high-risk workers with technologies to detect and prevent drowsy driving (Jang and Ahn 2020). Interventions to improve work satisfaction by creating a positive and supportive work environment may also contribute to the prevention of commuting crashesamong HCWs. It is important to provide adequate physical and mental services to HCWs to avoid the risk of burnout, commuting crashes, and drowsy driving. The physical and mental wellbeing of HCWs should be a first priority in health organizations, as HCWs are in charge of saving lives and treating vulnerable patients. Improving HCWs wellbeing and preventing burnout can also reduce costs resulting from absenteeism, sick leave, and turnover.
Acknowledgements
The authors have no relevant acknowledgments to disclose.
Author contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by NH and MEH. The first draft of the manuscript was written by NH and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
This study received no funds.
Data availability
Data and materials are available upon request to the corresponding authors.
Declarations
Conflict of interest
The authors declare they have no conflicts of interests to disclose.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Neta Hagani and Michal Englard Hershler have contributed equally to this work.
References
- Alfuqaha O, Alsharah H. Burnout among nurses and teachers in Jordan: a comparative study. Arch Psychiat Psychother. 2018;20(2):55–65. doi: 10.12740/APP/80168. [DOI] [Google Scholar]
- Anderson C, Ftouni S, Ronda JM, Rajaratnam SM, Czeisler CA, Lockley SW. Self-reported drowsiness and safety outcomes while driving after an extended duration work shift in trainee physicians. Sleep. 2018;41(2):zsx195. doi: 10.1093/sleep/zsx195. [DOI] [PubMed] [Google Scholar]
- Ayas NT, Barger LK, Cade BE, Hashimoto DM, Rosner B, Cronin JW, Speizer FE, Czeisler CA. Extended work duration and the risk of self-reported percutaneous injuries in interns. JAMA. 2006;296(9):1055–1062. doi: 10.1001/jama.296.9.1055. [DOI] [PubMed] [Google Scholar]
- Barger LK, Cade BE, Ayas NT, Cronin JW, Rosner B, Speizer FE, Czeisler CA. Extended work shifts and the risk of motor vehicle crashes among interns. N Engl J Med. 2005;352(2):125–134. doi: 10.1056/NEJMoa041401. [DOI] [PubMed] [Google Scholar]
- Barger LK, Lockley SW, Rajaratnam SM, Landrigan CP. Neurobehavioral, health, and safety consequences associated with shift work in safety-sensitive professions. Curr Neurol Neurosci. 2009;9(2):155–164. doi: 10.1007/s11910-009-0024-7. [DOI] [PubMed] [Google Scholar]
- Bloom J, Dorsett P, McLennan V. Investigating employment following spinal cord injury: outcomes, methods, and population demographics. Disabil Rehabil. 2019;41(20):2359–2368. doi: 10.1080/09638288.2018.1467968. [DOI] [PubMed] [Google Scholar]
- Centers for disease control and prevention- CDC (2021). Drowsy driving: asleep at the wheel. https://www.cdc.gov/sleep/features/drowsy-driving.html Accessed 31 Dec 2021
- Chemali Z, Ezzeddine FL, Gelaye B, Dossett ML, Salameh J, Bizri M, Dubale B, Fricchione G. Burnout among healthcare providers in the complex environment of the Middle East: a systematic review. BMC Pub Hea. 2019;19(1):1–21. doi: 10.1186/s12889-019-7713-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung YS, Wu HL. Effect of burnout on accident involvement in occupational drivers. Trans Res Record. 2013;2388(1):1–9. doi: 10.3141/2388-01. [DOI] [Google Scholar]
- Cooke CE, Stephens JM. Clinical, economic, and humanistic burden of needlestick injuries in healthcare workers. Med Devic (auckland, NZ) 2017;10:225–235. doi: 10.2147/MDER.S140846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creedy DK, Sidebotham M, Gamble J, Pallant J, Fenwick J. Prevalence of burnout, depression, anxiety and stress in Australian midwives: a cross-sectional survey. BMC Pregnancy Childb. 2017;17(1):13. doi: 10.1186/s12884-016-1212-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Hert S. Burnout in healthcare workers: prevalence, impact and preventative strategies. Local Reg Anesth. 2020;13:171–183. doi: 10.2147/LRA.S240564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deligkaris P, Panagopoulou E, Montgomery AJ, Masoura E. Job burnout and cognitive functioning: a systematic review. Work Stress. 2014;28(2):107–123. doi: 10.1080/02678373.2014.909545. [DOI] [Google Scholar]
- Denning M, Goh ET, Tan B, Kanneganti A, Almonte M, Scott A, Martin G, Clarke J, Sounderajah V, Markar S, Przybylowicz J. Determinants of burnout and other aspects of psychological well-being in healthcare workers during the COVID-19 pandemic: a multinational cross-sectional study. PLoS ONE. 2021;16(4):e0238666. doi: 10.1371/journal.pone.0238666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorrian J, Lamond N, van den Heuvel C, Pincombe J, Rogers AE, Dawson D. A pilot study of the safety implications of Australian nurses’ sleep and work hours. Chronobiol Int. 2006;23(6):1149–1163. doi: 10.1080/07420520601059615. [DOI] [PubMed] [Google Scholar]
- Dorrian J, Tolley C, Lamond N, van den Heuvel C, Pincombe J, Rogers AE, Drew D. Sleep and errors in a group of Australian hospital nurses at work and during the commute. Appl Ergon. 2008;39(5):605–613. doi: 10.1016/j.apergo.2008.01.012. [DOI] [PubMed] [Google Scholar]
- Duke NN, Gross A, Moran A, Hodsdon J, Demirel N, Osterholm E, Sunni M, Pitt MB. Institutional factors associated with burnout among assistant professors. Teach Learn Med. 2020;32(1):61–70. doi: 10.1080/10401334.2019.1638263. [DOI] [PubMed] [Google Scholar]
- Dyrbye LN, West CP, Satele D, Boone S, Tan L, Sloan J, Shanafelt TD. Burnout among US medical students, residents, and early career physicians relative to the general US population. Acad Med. 2014;89(3):443–451. doi: 10.1097/ACM.0000000000000134. [DOI] [PubMed] [Google Scholar]
- Fallis WM, McMillan DE, Edwards MP. Napping during night shift: practices, preferences, and perceptions of critical care and emergency department nurses. Crit Care Nurse. 2011;31(2):e1–e11. doi: 10.4037/ccn2011710. [DOI] [PubMed] [Google Scholar]
- Freedman-Weiss MR, Heller DR, White EM, Chiu AS, Jean RA, Yoo PS. Driving safety among surgical residents in the era of duty hour restrictions. J Surg Educ. 2021;78(3):770–776. doi: 10.1016/j.jsurg.2020.08.041. [DOI] [PubMed] [Google Scholar]
- German social accident insurance. Work-related accidents definition of terms. https://www.dguv.de/en/facts-figures/definitions-terms/index.jsp Accessed 30 Dec 2021
- Green W, Gao X, Li K, Banz BC, Wu J, Crowley MJ, Camenga DR, Vaca FE. The association of sleep hygiene and drowsiness with adverse driving events in emergency medicine residents. West J Emerg Med. 2020;21(6):219–224. doi: 10.5811/westjem.2020.8.47357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoff T, Carabetta S, Collinson GE. Satisfaction, burnout, and turnover among nurse practitioners and physician assistants: a review of the empirical literature. Med Care Res Rev. 2019;76(1):3–31. doi: 10.1177/1077558717730157. [DOI] [PubMed] [Google Scholar]
- International labour organization (2010). World social security report 2010/11. https://www.ilo.org/wcmsp5/groups/public/---dgreports/---dcomm/---publ/documents/publication/wcms_146566.pdf Accessed 30 Dec 2021
- Israel central bureau of statistics (2018). Localities, population and density per Sq. Km., by metropolitan area and selected localities. https://www.cbs.gov.il/he/publications/DocLib/2018/2.%20ShnatonPopulation/st02_25.pdf Accessed 28 Dec 2021
- Jang SW, Ahn B. Implementation of detection system for drowsy driving prevention using image recognition and IoT. Sustainability. 2020;12(7):3037. doi: 10.3390/su12073037. [DOI] [Google Scholar]
- Joseph B, Joseph M. The health of the healthcare workers. Indian J Occup Env Med. 2016;20(2):71–72. doi: 10.4103/jfmpc.jfmpc_431_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jourdain G, Chênevert D. Job demands–resources, burnout and intention to leave the nursing profession: a questionnaire survey. Int J Nurs Stud. 2010;47(6):709–722. doi: 10.1016/j.ijnurstu.2009.11.007. [DOI] [PubMed] [Google Scholar]
- Kenardy J, Heron-Delaney M, Warren J, Brown E. The effect of mental health on long-term health-related quality of life following a road traffic crash: results from the UQ SuPPORT study. Injury. 2015;46(5):883–890. doi: 10.1016/j.injury.2014.11.006. [DOI] [PubMed] [Google Scholar]
- Koutsimani P, Montgomery A, Masoura E, Panagopoulou E. Burnout and Cognitive Performance. Int J Env Res Pub Health. 2021;18(4):2145. doi: 10.3390/ijerph18042145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leiter MP, Maslach C. Burnout and workplace injuries: a longitudinal analysis. In: Am R, Quick J, Perrewé P, editors. Stress and quality of working life: the positive and the negative. NC: Charlotte; 2009. pp. 3–18. [Google Scholar]
- Libeson L, Downing M, Ross P, Ponsford J. The experience of return to work in individuals with traumatic brain injury (TBI): a qualitative study. Neuropsychol Rehabil. 2020;30(3):412–429. doi: 10.1080/09602011.2018.1470987. [DOI] [PubMed] [Google Scholar]
- Maslach C, Jackson SE. Maslach burnout inventory. Palo Alto, CA: Consulting Psychologists Press; 1986. [Google Scholar]
- Maslach C, Jackson SE, Leiter MP. MBI: maslach burnout inventory. Palo Alto, CA: Consulting Psychology Press; 1996. [Google Scholar]
- McHugh MD, Kutney-Lee A, Cimiotti JP, Sloane DM, Aiken LH. Nurses’ widespread job dissatisfaction, burnout, and frustration with health benefits signal problems for patient care. Health Affair. 2011;30(2):202–210. doi: 10.1377/hlthaff.2010.0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McManus IC, Keeling A, Paice E. Stress, burnout and doctors' attitudes to work are determined by personality and learning style: a twelve-year longitudinal study of UK medical graduates. BMC Med. 2004;2(29):1–12. doi: 10.1186/1741-7015-2-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McManus IC, Winder BC, Gordon D. The causal links between stress and burnout in a longitudinal study of UK doctors. Lancet. 2002;359(9323):2089–2090. doi: 10.1016/s0140-6736(02)08915-8. [DOI] [PubMed] [Google Scholar]
- Mohanty A, Kabi A, Mohanty AP. Health problems in healthcare workers: a review. J Family Med Prim Care. 2019;8(8):2568. doi: 10.4103/jfmpc.jfmpc_431_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oosterholt BG, Van der Linden D, Maes JH, Verbraak MJ, Kompier MA. Burned out cognition- cognitive functioning of burnout patients before and after a period with psychological treatment. Scand J Work, Env Hea. 2012;38(4):358–369. doi: 10.5271/sjweh.3256. [DOI] [PubMed] [Google Scholar]
- Riley MR, Mohr DC, Waddimba AC. The reliability and validity of three-item screening measures for burnout: evidence from group-employed health care practitioners in upstate New York. Stress Health. 2018;34(1):187–193. doi: 10.1002/smi.2762. [DOI] [PubMed] [Google Scholar]
- Rios PA, Mota EL, Ferreira LN, Cardoso JP, Ribeiro VM, Souza BS. Factors associated with traffic accidents among drivers: findings from a population-based study. Cien Saude Colet. 2020;25:943–955. doi: 10.1590/1413-81232020253.1192201. [DOI] [PubMed] [Google Scholar]
- Robb G, Sultana S, Ameratunga S, Jackson R. A systematic review of epidemiological studies investigating risk factors for work-related road traffic crashes and injuries. Inj Prev. 2008;14(1):51–58. doi: 10.1136/ip.2007.016766. [DOI] [PubMed] [Google Scholar]
- Rosenbloom T. Job burnout, effort-reward imbalance and time pressure as predictors of safety among military truck drivers. J Trans Health. 2021;9:101248. doi: 10.1016/j.jth.2021.101248. [DOI] [Google Scholar]
- Rotenstein LS, Torre M, Ramos MA, Rosales RC, Guille C, Sen S, Mata DA. Prevalence of burnout among physicians: a systematic review. JAMA. 2018;320(11):1131–1150. doi: 10.1001/jama.2018.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salvagioni DA, Melanda FN, Mesas AE, González AD, Gabani FL, Andrade SM. Physical, psychological and occupational consequences of job burnout: a systematic review of prospective studies. PLoS ONE. 2017;12(10):e0185781. doi: 10.1371/journal.pone.0185781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salvagioni DA, Mesas AE, Melanda FN, Dos Santos HG, González AD, Girotto E, de Andrade SM. Prospective association between burnout and road traffic accidents in teachers. Stress Health. 2020;36(5):629–638. doi: 10.1002/smi.2958. [DOI] [PubMed] [Google Scholar]
- Schonfeld IS, Bianchi R. Burnout and depression: two entities or one? J Clin Psychol. 2016;72(1):22–37. doi: 10.1002/jclp.22229. [DOI] [PubMed] [Google Scholar]
- Scott LD, Hwang WT, Rogers AE, Nysse T, Dean GE, Dinges DF. The relationship between nurse work schedules, sleep duration, and drowsy driving. Sleep. 2007;30(12):1801–1807. doi: 10.1093/sleep/30.12.1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- See KC, Zhao MY, Nakataki E, Chittawatanarat K, Fang WF, Faruq MO, Wahjuprajitno B, Arabi YM, Wong WT, Divatia JV, Palo JE. Professional burnout among physicians and nurses in asian intensive care units: a multinational survey. Intens Care Med. 2018;44(12):2079–2090. doi: 10.1007/s00134-018-5432-1. [DOI] [PubMed] [Google Scholar]
- Shaikh AA, Shaikh A, Kumar R, Tahir A. Assessment of burnout and its factors among doctors using the abbreviated Maslach burnout inventory. Cureus. 2019;11(2):e4101. doi: 10.7759/cureus.4101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith A, McDonald AD, Sasangohar F. The impact of commutes, work schedules, and sleep on near-crashes during nurses’ post shift-work commutes: a naturalistic driving study. IISE Trans Occup Ergon Hum Factors. 2021;9:13–22. doi: 10.1080/24725838.2021.1945708. [DOI] [PubMed] [Google Scholar]
- Smith A, McDonald AD, Sasangohar F. Night-shift nurses and drowsy driving: a qualitative study. Int J Nurs Stud. 2020;112:103600. doi: 10.1200/JCO.2011.39.7380. [DOI] [PubMed] [Google Scholar]
- Tawfik DS, Profit J, Morgenthaler TI, Satele DV, Sinsky CA, Dyrbye LN, Tutty MA, West CP, Shanafelt TD. Physician burnout, well-being, and work unit safety grades in relationship to reported medical errors. Mayo Clin Proc. 2018;93(11):1571–1580. doi: 10.1016/j.mayocp.2018.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The National Authority for Road Safety (2020). [Trends in road safety in Israel 2013–2029]. Division of information and research. https://www.gov.il/he/departments/publications/reports/trends_2019 Accessed Aug 30 2021
- The national authority for road safety (2021). Risk measures for road safety in large and medium size cities in Israel. https://www.gov.il/BlobFolder/reports/safety_risk_indices_2020/he/research_safety_risk_indices_2020.pdf Accessed 23 Jan 2022
- United states department of labor (2021). Occupational safety and health administration. determining if injuries and illnesses are work-related when employees commute from home to work and from a hotel to a worksite. https://www.osha.gov/laws-regs/standardinterpretations/2021-03-17 Accessed 30 Dec 2021
- Useche S, Alonso F, Cendales B, Autukevičiūtė R, Serge A. Burnout, job strain and road accidents in the field of public transportation: the case of city bus drivers. J Env Occup Sci. 2017;6(1):1–7. doi: 10.5455/jeos.20170202074636. [DOI] [Google Scholar]
- Useche S, Cendales B, Alonso F, Serge A. Comparing job stress, burnout, health and traffic crashes of urban bus and BRT drivers. Am J Appl Psychol. 2017;5(1):25–32. doi: 10.12691/ajap-5-1-5. [DOI] [Google Scholar]
- Vedaa Ø, Harris A, Erevik EK, Waage S, Bjorvatn B, Sivertsen B, Moen BE, Pallesen S. Short rest between shifts (quick returns) and night work is associated with work-related accidents. Int Arch Occ Env Hea. 2019;92(6):829–835. doi: 10.1007/s00420-019-01421-8. [DOI] [PubMed] [Google Scholar]
- Walters D (2007). International comparison of occupational disease and injury compensation schemes. A research report prepared for the industrial injuries advisory council (IIAC). Cardiff University. https://www.ucm.es/data/cont/media/www/pag-62918/untitled%20folder/InternationalComparisonsReport.pdf Accessed 30 Dec 2021
- Westwell A, Cocco P, Van Tongeren M, Murphy E. Sleepiness and safety at work among night shift NHS nurses. Occup Med. 2021;71(9):439–445. doi: 10.1093/occmed/kqab137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson V, Murphy D, Greenberg N. COVID-19 and experiences of moral injury in front-line key workers. Occup Med. 2020;70(5):317–319. doi: 10.1093/occmed/kqaa052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welp A, Meier LL, Manser T. Emotional exhaustion and workload predict clinician-rated and objective patient safety. Front Psychol. 2015;5:1573. doi: 10.3389/fpsyg.2014.01573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West CP, Dyrbye LN, Sinsky C, Trockel M, Tutty M, Nedelec L, Carlasare LE, Shanafelt TD. Resilience and burnout among physicians and the general US working population. JAMA Netw Open. 2020;3(7):e209385. doi: 10.1001/jamanetworkopen.2020.9385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West CP, Tan AD, Shanafelt TD. Association of resident fatigue and distress with occupational blood and body fluid exposures and motor vehicle incidents. Mayo Clin Proc. 2012;87(12):1138–1144. doi: 10.1016/j.mayocp.2012.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willard-Grace R, Knox M, Huang B, Hammer H, Kivlahan C, Grumbach K. Burnout and health care workforce turnover. Ann Fam Med. 2019;17(1):36–41. doi: 10.1370/afm.2338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [Work injuries guide]. https://www.kolzchut.org.il/he/%D7%9E%D7%93%D7%A8%D7%99%D7%9A_%D7%9C%D7%A0%D7%A4%D7%92%D7%A2%D7%99_%D7%A2%D7%91%D7%95%D7%93%D7%94 Accessed 23 June 2021
- World health organization. Burn-out an “occupational phenomenon”: international classification of diseases (2019). https://www.who.int/mental_health/evidence/burn-out/en/ Accessed 25 Mar 2021
- Zuwairy MS, Harith AA, Nobuyaki H, Naim NM, Yon R. Road traffic accidents: a descriptive study of commuting injury among healthcare workers in Malaysia 2014–2016. Int J Pub Health Clin Sci. 2020;7(1):58–71. doi: 10.32827/ijphcs.7.1.58. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data and materials are available upon request to the corresponding authors.