Abstract
Background
Primary diffuse large B-cell lymphoma of the bone (PB-DLBCL) is a rare type of extra-nodal lymphoma. This study aimed to examine the clinical characteristics, outcomes, treatment modalities and risk of central nervous system relapse (CNSR) among adult Jordanian patients with PB-DLBCL.
Methods
This retrospective study included patients aged >16 years who were diagnosed with PB-DLBCL and treated at our hospital between 2002 and 2021. Clinical characteristics, treatment modalities, outcomes and CNSR events were extracted from the hospital’s data system and analysed. Patients were categorised into unifocal (UF) and multifocal (MF) PB-DLBCL groups according to the number of bone sites involved. The involvement of only one site was defined as UF, whereas the involvement of two or more sites was defined as MF.
Results
In total, 12 patients were diagnosed with PB-DLBCL. Their median age was 47.5 years (range, 17–80 years). The male:female ratio was 1:1. There were eight patients in the UF PB-DLBCL group and four in the MF PB-DLBCL group. All patients received treatment with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone. In the UF PB-DLBCL group, the male:female ratio was 5:3, the median age was 41 years, and the follow-up duration was 9–135 (mean, 83.3) months. In the MF PB-DLBCL group, the male:female ratio was 1:3, the median age was 51.5 years, and the survival time was 3–11 (mean, 7) months. Three patients with vertebral UF PB-DLBCL underwent early vertebroplasty without complications. The most common site involved was the vertebral column. Most patients with UF PB-DLBCL achieved complete remission (CR), whereas no patients with MF PB-DLBCL achieved CR.
Conclusion
PB-DLBCL is rare in adult Jordanian patients. UF PB-DLBCL is more common than MF PB-DLBCL. Patients with UF PB-DLBCL had a good prognosis. Patients with MF PB-DLBCL had a high international prognostic index score, risk of CNSR and short survival time.
Keywords: primary diffuse large B-cell lymphoma of the bone, WHO classification of primary bone lymphoma, unifocal, multifocal
Introduction
Primary bone lymphoma is a rare type of neoplastic disorder. It is estimated to constitute 1% of all lymphomas, with diffuse large B-cell lymphoma (DLBCL) being the most common histological type.1–6
Studies describing the clinical manifestations and treatment modalities of PB-DLBCL remain controversial as most of the research results are from Western countries. Therefore, we conducted this retrospective study to better understand the clinical characteristics, treatment modalities and outcomes of PB-DLBCL in adult Jordanian patients.
Materials and Methods
This 19-year retrospective study was approved by the Institutional Review Board Committee (IRB) of King Abdullah University Hospital (KAUH). The need for informed consent was waived by the IRB due to the retrospective nature of the study, and the data was anonymised. This study included patients diagnosed with PB-DLBCL and treated at KAUH between 2002 and 2021.
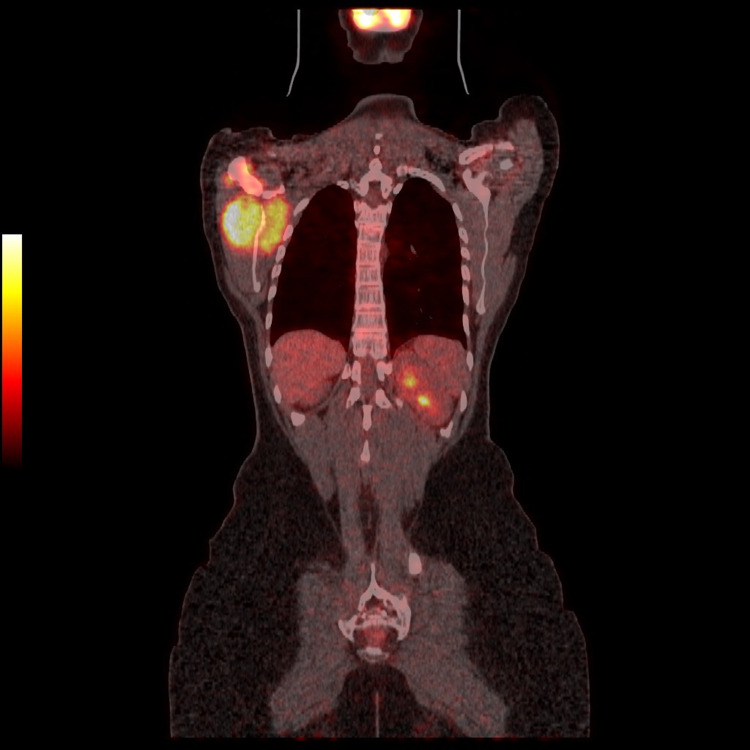
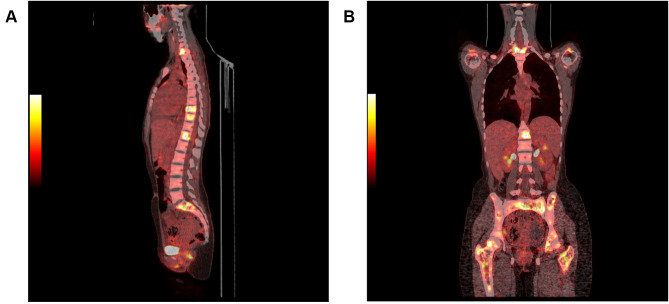
PB-DLBCL was diagnosed via guided bone biopsy, histological examination, and immunohistochemical (IHC) analysis for CD20, PAX-5, CD10, Bcl-2, Bcl-6 and MUM-1. Accordingly, each lymphoma was categorised into germinal centre B-cell (GCB) and non-germinal centre B-cell (NGCB) types. The inclusion criteria were as follows: having undergone radiological examination and positron emission tomography (PET) upon diagnosis (Figure 1, Figure 2A and B), having a follow-up time of ≥3 months and not presenting with significant lymphadenopathy or any other extra-nodal site involvements other than the bone, with the exception of bone marrow involvement, as all patients included in the study underwent bone marrow biopsy as part of cancer staging at the time of diagnosis.
Figure 1.
PET scan showing unifocal bone involvement of the scapula with mass.
Figure 2.
(A) PET scan showing with multifocal bone involvement of the vertebral column. (B) PET scan showing multifocal bone involvement pelvis, femur, vertebra, and scapulae.
Categorisation: According to PET scan results, patients were categorised into unifocal (UF) and multifocal (MF) PB-DLBCL groups according to the number of bone sites involved. The involvement of only one site was defined as UF, whereas the involvement of two or more sites was defined as MF. We considered more than one vertebral involvement as MF.
Data on patient characteristics, such as age, sex, clinical manifestations, including B symptoms upon diagnosis, symptom duration (from symptom onset until diagnosis), treatment modalities and survival duration after treatment were extracted from the computer registry file system of KAUH. Survival time was calculated from the time of diagnosis to the time of the last hospital visit, and information about the time of death was extracted from the Jordanian Civil Status and Passport Department. Additionally, data about risk factors, such as serum lactate dehydrogenase (LDH) levels, were obtained. Human immunodeficiency virus (HIV) testing is not routinely performed as most patients do not want to undergo it and the prevalence of HIV among Jordanians is low (<0.1%).7 CNSR was diagnosed via lumbar puncture to examine the cerebrospinal fluid (CSF). The presence of lymphoma cells was determined via cytology, flow cytometry of the CSF and contrast-enhanced radiological examination.8
For response assessment, we used the response criteria based on the International Working Group consensus response evaluation criteria in lymphoma (RECIL 2017).9
International Prognostic Index (IPI) score
The patients’ IPI score was calculated based on the following, with 1 point being assigned to each: age of ≥60 years, increased LDH levels, stage III–IV disease, Eastern Cooperative Oncology Group performance status score and >1 extra-nodal site of disease.10
Results
Patient Characteristics
The clinical characteristics of patients are shown in Tables 1 and 2. In total, 261 patients aged >16 years were diagnosed with at KAUH. Among them, 12 (4.6%) were diagnosed with PB-DLBCL, with a median age of 47.5 years (range, 17–80 years) and a male:female ratio of 1:1.
Table 1.
Demographic and Clinical Characteristics of Patients with UF PB -DLBL (n=8)
| Cases | ||||||||
|---|---|---|---|---|---|---|---|---|
| Patient | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
| Age | 36 | 46 | 80 | 17 | 56 | 28 | 49 | 25 |
| Sex | F | F | M | F | M | M | M | M |
| Site | Sacrum | Scapula | Clavicle | Femur | L3 | Femur | T3 | T10 |
| Symptoms | Pain | Mass | Mass | Pain | Pain | Pain | Pain | Pain |
| Fracture | No | No | No | No | Yes | Yes | Yes | Yes |
| GC/NGC type | GC | GC | NGC | GC | NGC | GC | NGC | NGC |
| Duration of symptoms (m) | 6 | 2 | 4 | 3 | 6 | 5 | 8 | 3 |
| Serum LDH | H | H | N | H | H | H | H | H |
| IPI index | 1 | 1 | 3 | 1 | 1 | 1 | 1 | 1 |
| Survival in months | 143 | 97 | 81 | 132 | 108 | 33 | *9 | 95 |
Abbreviations: UFPB-DLBCL, unifocal, primary bone diffuse large B-cell lymphoma; F, female; M, male; L3, third lumbar vertebra; T3, third thoracic vertebrae; P, pelvis; H, high; N, normal; * 9 patients died owing to severe left ventricular impairment; GC, germinal center; NGC, non-germinal center.
Table 2.
Demographic and Clinical Characteristics of Patients with MF PB -DLBL (n=4)
| Patients | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| Age | 54 | 22 | 49 | 71 |
| Sex | M | F | F | F |
| Site | T12-L5 F, H, P | C7- T3, H.P | T5-L3 | T1-L3 |
| Symptoms | Pain | Pain | Pain | Pain, SC |
| Duration of symptoms (m) | 14 | 18 | 23 | 25 |
| Serum LDH | H | H | N | H |
| IPI index | 3 | 4 | 4 | 4 |
| Survival in months | 11 | 7 | 7 | 3 |
| GC/NGC | GC | GC | NGC | NGC |
| CNSR | Yes | Yes | Yes | No |
Abbreviations: MF PB-DLBCL, multifocal primary bone diffuse large B-cell lymphoma; F, female; M, male; t12-l5, third thoracic vertebra-fifth lumbar vertebra; C7-T3, seventh cervical vertebra-third thoracic vertebra; T5-L3, fifth thoracic vertebra-third lumbar vertebra; T1-L3, first thoracic vertebra-third lumbar vertebra; P, pelvis; H, high; N, normal, m, month; GC, germinal center; NGC, non-germinal center.
In the UF PB-DLBCL group, there were 8 patients, with a male:female ratio of 5:3, median age of 41 years (range, 17–80 years), mean age of 42 years and follow-up duration of 9–135 (mean, 83.3) months. In the MF PB-DLBCL group, there were 4 patients, with a male:female ratio of 1:3, median age of 51.5 years (range, 22–71 years) and survival time of 3–11 (mean, 7) months. Among patients with UF PB-DLBCL, there were 5 with GCB and 3 with NGCB. Among patients with MF PB-DLBCL, 2 had GCB and 2 had NGCB.
Sites of Bone Involvement
The vertebrae (n = 7) were the most common site of bone involvement, followed by the pelvis and femur (n = 2), scapulae (n = 1) and clavicle (n = 1). All patients with MF PB-DLBCL had vertebral involvement, and only one patient with MF PB-DLBCL presented with spinal as well as long-bone involvement.
Clinical Presentation of PB-DLBCL
Pain was present at the site of bone involvement in all patients. Three patients with MF bone involvement had B symptoms, but no patients with UF involvement had B symptoms. All patients with vertebral involvement had fractures. Three patients had masses in the scapulae, clavicles and femur. The median symptom duration in the UF PB-DLBCL group was 4.5 (range, 2–8) months. In the MF PB-DLBCL group, the median symptom duration was 20.5 (range, 18–25) months.
Treatment Modalities
All patients received rituximab, cyclophosphamide, doxorubicin, vincristine and prednisolone (R-CHOP), and only one patient with scapula involvement was treated with R-CHOP combined with radiotherapy. Three patients with UF vertebral involvement underwent early vertebroplasty prior to chemotherapy during bone curettage biopsy.
IPI Score
In the UF PB-DLBCL group, 7 patients had an IPI score of 1 and 1 patient had an IPI score of 3. In the MF PB-DLBCL group, 3 patients had an IPI score of 4 and 1 patient had an IPI score of 3.
Central Nervous System Relapse
Three of four patients with MF PB-DLBCL had CNSR, but none with UF PB-DLBCL had CNSR.
Bone Marrow Involvement
Bone marrow involvement was present in three patients with MF PB-DLBCL but none of the patients with UF PB-DLBCL.
Chemotherapy Complications
One patient with spinal MF involvement had vertebral collapse after the first cycle of R-CHOP, thereby resulting in spinal cord compression and, eventually, death.
Response Criteria
Seven patients with UF PB-DLBCL achieved complete remission (CR), but none of the patients with MF PB-DLBCL achieved CR.
Discussion
To the best of our knowledge, this the first study to describe Jordanian patients with PB-DLBCL. In this study, PB-DLBCL constituted for 4.6% of all cases of PB-DLBCL, which is less than what has been reported in other studies11,12 and different from a report from China that showed a lower frequency of 0.01%.13 The median age of our patients with PB-DLBCL was younger than that reported in other studies.14 No sex bias was observed for PB-DLBCL.15 However, comparing PB-DLBCL subtypes, we noticed male predominance among those with UF PB-DLBCL and female predominance among those with MF PB-DLBCL. This finding differs from the results reported in other studies showing male predominance in both types.14–16 Female predominance in MF PB-DLBCL in our study may be due to the fact that the diagnosis was delayed in most of our female patients because the bone pain was attributed to rheumatological causes, resulting in a long symptom duration before diagnosis.
Regarding IHC subtypes, we found that the GCB type was predominant among those with UF PB-DLBCL, whereas both GCB and NGCB subtypes occurred in equal proportions among those with MF PB-DLBCL. As our study included a small number of patients, the effect of GCB and NGCB subtypes on prognosis was not clear.14,17,18
The main symptoms were pain, masses and fractures. Fractures were present in patients with vertebral involvement and have been shown to be the most common symptom of PB-DLBCL.1,3,5,8–14,14,15,15–17
Our study revealed the absence of B symptoms in patients with UF PB-DLBCL as opposed to their presence in patients with MF PB-DLBCL. Additionally, patients with MF PB-DLBCL had higher IPI scores, bone marrow involvement and CNSR. These observations in our patients suggest that MF PB-DLBCL represents an advanced stage of the disease.
In our study, the vertebrae were the most common site of involvement in both types of PB-DLBCL, which corroborates the results of other previous studies.5,18 Notably, another study showed the predominance of appendicular bone involvement.14
All patients received R-CHOP chemotherapy. Out of eight patients with UF PB-DLBCL, six achieved CR, but none of the patients with MF PB-DLBCL achieved CR, which is in agreement with the results of another study.14
Three patients with UF vertebral involvement underwent early percutaneous vertebroplasty before starting R-CHOP chemotherapy and none of them relapsed. This suggests that early vertebroplasty may be beneficial in patients with vertebral UF PB-DLBCL, as shown in a previous case report.19 One patient with MF vertebral involvement developed vertebral collapse with spinal cord compression after the first dose of R-CHOP. Hence, vertebroplasty should also be considered in cases of MF vertebral involvement.
In conclusion, our retrospective study with a small number of patients, which reflects the rarity of PB-DLBCL, showed that UF PB-DLBCL has a better prognosis than MF PB-DLBCL and that MF PB-DLBCL represents an advanced stage of the disease.
Acknowledgments
The authors would like to thank Enago for editing this manuscript.
Funding Statement
There is no funding to report.
Ethics Statement and Informed Consent
All procedures performed in studies involving human participants were following the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Ethics Committee of King Abdullah University Hospital (785/2018) approved this retrospective study. The need to obtain informed consent was waived, as the study was a retrospective study, and there was no additional risk to patients. All data were anonymized to maintain patient privacy.
Disclosure
Dr Duha M Al-Shorafat reports honorarium from Allergan/AbbVie and MERCK, outside the submitted work. The authors report that there are no other competing interests to declare.
References
- 1.Messina C, Christie D, Zucca E, et al. Primary and secondary bone lymphomas. Cancer Treat Rev. 2015;41(3):235–246. doi: 10.1016/j.ctrv.2015.02.001 [DOI] [PubMed] [Google Scholar]
- 2.Beal K, Allen L, Yahalom J. Primary bone lymphoma: treatment results and prognostic factors with long‐term follow‐up of 82 patients. Cancer. 2006;12:2652–2656. doi: 10.1002/cncr.21930 [DOI] [PubMed] [Google Scholar]
- 3.Liu CX, Xu TQ, Xu L, et al. Primary lymphoma of bone: a population-based study of 2558 patients. Ther Adv Hematol. 2020;11:2040620720958538. doi: 10.1177/2040620720958538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cai L, Stauder MC, Zhang YJ, et al. Early-stage primary bone lymphoma: a retrospective, multicenter Rare Cancer Network (RCN) Study. Int J Radiat Oncol Biol Phys. 2012;83(1):284–291. doi: 10.1016/j.ijrobp.2011.06.1976 [DOI] [PubMed] [Google Scholar]
- 5.Ramadan KM, Shenkier T, Sehn LH, Gascoyne RD, Connors JM. A clinicopathological retrospective study of 131 patients with primary bone lymphoma: a population-based study of successively treated cohorts from the British Columbia Cancer Agency. Ann Oncol. 2007;18:129–135. doi: 10.1093/annonc/mdl329 [DOI] [PubMed] [Google Scholar]
- 6.Wu H, Zhang L, Shao H, et al. Prognostic significance of soft tissue extension, international prognostic index, and multifocality in primary bone lymphoma: a single institutional experience. Br J Haematol. 2014;166(1):60–68. doi: 10.1111/bjh.12841 [DOI] [PubMed] [Google Scholar]
- 7.HIV AND AIDS IN THE MIDDLE EAST & NORTH AFRICA (MENA) [Home page on the interent]. Available from: avert.org/professionals/hiv-around-world/middle-east-north-africa-mena. Accessed March 13, 2022.
- 8.Scott BJ, Douglas VC, Tihan T, et al. A systematic approach to the diagnosis of suspected central nervous system lymphoma. JAMA Neurol. 2013;3:311–319. doi: 10.1001/jamaneurol.2013.606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Younes A, Hilden P, Coiffier B, et al. International Working Group consensus response evaluation criteria in lymphoma (RECIL 2017). Ann Oncol. 2017;28(7):1436–1447. doi: 10.1093/annonc/mdx097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.International Non-Hodgkin’s Lymphoma Prognostic Factors Project. A predictive model for aggressive non-Hodgkin’s lymphoma. N Eng J Med. 1993;14:987–994. [DOI] [PubMed] [Google Scholar]
- 11.Limb D, Dreghorn C, Murphy JK, Mannion R. Primary lymphoma of bone. Int Orthop. 1994;18(3):180–183. doi: 10.1007/BF00192476 [DOI] [PubMed] [Google Scholar]
- 12.Freeman C, Berg JW, Cutler SJ. Occurrence and prognosis of extranodal lymphomas. Cancer. 1972;29(1):252–260. [DOI] [PubMed] [Google Scholar]
- 13.Shen H, Wei Z, Zhou D, et al. Primary extra‑nodal diffuse large B‑cell lymphoma: a prognostic analysis of 141 patients. Oncol Lett. 2018;16(2):1602–1614. doi: 10.3892/ol.2018.8803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu H, Bui MM, Leston DG, et al. Clinical characteristics and prognostic factors of bone lymphomas: focus on the clinical significance of multifocal bone involvement by primary bone large B-cell lymphomas. BMC cancer. 2014;14(1):1–9. doi: 10.1186/1471-2407-14-900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu CX, Xu TQ, Xu L, et al. Primary lymphoma of bone: a population-based study of 2558 patients. Ther Adv Hematol. 2020;11:2040620720958538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Messina C, Ferreri AJ, Govi S, Bruno‐Ventre M, Gracia Medina EA, Porter D; International Extranodal Lymphoma Study Group (IELSG). Clinical features, management and prognosis of multifocal primary bone lymphoma: a retrospective study of the international extranodal lymphoma study group (the IELSG 14 study). Br J Haematol. 2014;164(6):834–840. doi: 10.1111/bjh.12714 [DOI] [PubMed] [Google Scholar]
- 17.Heyning FH, Hogendoorn PC, Kramer MH, Holland CT, Dreef E, Jansen PM. Primary lymphoma of bone: extranodal lymphoma with favourable survival independent of germinal centre, post-germinal centre or indeterminate phenotype. J Clin Pathol. 2009;62:820–824. doi: 10.1136/jcp.2008.063156 [DOI] [PubMed] [Google Scholar]
- 18.Zhang X, Zhu J, Song Y, et al. Clinical characterization and outcome of primary bone lymphoma: a retrospective study of 61 Chinese patients. Sci Rep. 2016;6(1):28834. doi: 10.1038/srep28834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jia P, Li J, Chen H, et al. Percutaneous Vertebroplasty for Primary Non-Hodgkin’s Lymphoma of the Thoracic Spine: case Report and Review of the Literature. Pain Physician. 2017;20(5):E727–E735. [PubMed] [Google Scholar]