Abstract
The novel SARS-CoV-2 has directly and indirectly impacted patients with acute coronary syndrome (ACS). The onset of the COVID-19 pandemic correlated with an abrupt decline in hospitalizations with ACS and increased out-of-hospital deaths. Worse outcomes in ACS patients with concomitant COVID-19 have been reported, and acute myocardial injury secondary to SARS-CoV-2 infection is recognized. A rapid adaptation of existing ACS pathways has been required such that overburdened health care systems may manage both a novel contagion and existing illness. As SARS-CoV-2 is now endemic, future research is required to better define the complex interplay of COVID-19 infection and cardiovascular disease.
Keywords: COVID-19, Acute coronary syndrome, ST-elevation myocardial infarction, Non–ST-elevation myocardial infarction
Key points
-
•
The COVID-19 pandemic has resulted in wide-ranging direct and indirect consequences for patients with ACS.
-
•
A sudden, unexpected decline in hospitalizations for ACS and an increase in out-of-hospital deaths coincided with the onset of the COVID-19 pandemic.
-
•
ACS in patients with COVID-19 is associated with excess rates of adverse events, particularly when medical intervention is delayed.
-
•
During the COVID-19 pandemic, many patients with ACS have been required to undergo alternative diagnostic and therapeutic strategies due to reorganization of health care resources.
-
•
Studies to further elucidate the complex relationship between SARS-CoV-2 infection and myocardial injury or infarction are required.
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has resulted in the most significant infectious disease outbreak and public health emergency for a century. Declared a pandemic by the World Health Organization in March 2020, coronavirus disease 2019 (COVID-19) has infected millions and caused excess mortality and morbidity across the world. Health care systems have been required to restructure and adapt to an entirely novel disease entity, while providing routine and emergency care for existing illness.
Patients with acute coronary syndrome (ACS) provide one such example in which these challenges intersected (Fig. 1 ). The diagnosis and treatment of acute myocardial infarction (MI) has attracted much scientific attention during the COVID-19 pandemic by virtue of several critical issues:
-
1.
An internationally observed reduction in hospital admission rates for ACS1 , 2
-
2.
SARS-CoV-2 infection is associated with myocardial injury,3 accentuated predominantly in patients with underlying cardiometabolic risk factors4
-
3.
There are perceived diagnostic challenges with discrimination between COVID-19–related and non–COVID-19–related myocardial injury and infarction5
-
4.
Health care system reorganization limited the availability of ACS diagnostic tools and therapeutic strategies6
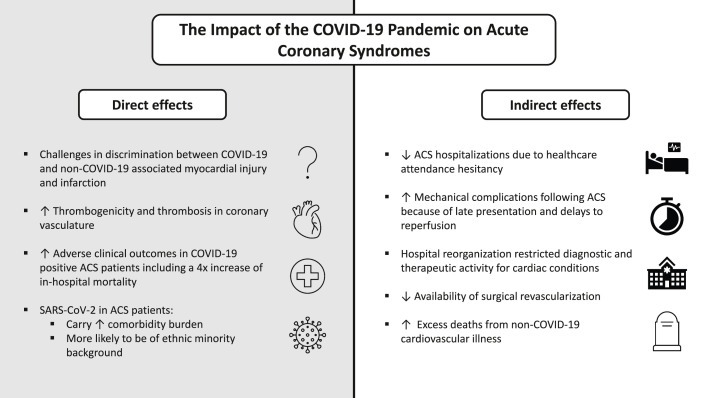
Fig. 1.
The direct and indirect effects of the COVID-19 pandemic on patient with acute coronary syndromes.
The present article addresses these challenges and discusses findings of the International COVID-ACS and UK-ReVasc registries, studies unique in their scope and investigation of the direct and indirect effects of the COVID-19 pandemic on patients with ACS.
COVID-19 and the cardiovascular system: a changing landscape
It rapidly became apparent that the SARS-CoV-2 virus would have wide-reaching consequences for patients with cardiovascular disease, because such risk factor profiles were recognized to portend an increased risk of hospitalization and mortality after infection.7 Yet perhaps more unexpected was the sudden and unheralded decline in cases of heart attack observed at the outset of the COVID-19 pandemic. For example, in one of the first such reports, De Filippo and colleagues documented a 25% reduction in hospital admissions for all ACS in Northern Italy.2 These data that have since been replicated in larger and more robust analyses that also show preponderance for greater decreases in non–ST-elevation acute coronary syndrome (NSTE-ACS) presentations.1 , 8 Moreover, increases in out-of-hospital cardiac arrest and death at home when compared with prepandemic periods were described, suggesting that many patients were forgoing medical attention.9 , 10
Where did all the heart attacks go? Viral respiratory infections are well recognized to increase the risk of acute MI,11 so why was this not reflected in greater hospital attendances during the initial waves of the pandemic? Proposed theories comprised: (1) a desire from patients to self-manage symptoms at home (perhaps compounded by societal pressures to quarantine), (2) a reduction in activity levels that may provoke MI, or (3) a fear of COVID-19 contagion in health care settings.12
Against the backdrop of falling heart attack case rates, a story of the complex interplay between SARS-CoV-2 infection and cardiovascular disease developed, fueled by rapid dissemination of knowledge via social media platforms.13 Case series described spontaneous and excess microthrombi and macrothrombi development in multiple vascular beds,14 myocarditis masquerading as ST-elevation myocardial infarction (STEMI),15 and elevated rates of myocardial injury in patients with COVID-19 infection.16
However, the exact degree and frequency of acute myocardial injury in patients with COVID-19, and its relationship with the cardiovascular system, has been difficult to accurately define. In perhaps the most robust study to investigate its prevalence, Lala and colleagues reported acute myocardial injury by means of cardiac troponin elevation in 36% of 2736 patients hospitalized with COVID-19.17 Elevated levels correlated with disease severity, as troponin concentrations 3 times the upper reference limit were associated with a 3-fold increased risk of mortality.17 Multiple hypotheses have been presented for the direct impact of SARS-CoV-2 on the cardiovascular system, ranging from supply-demand mismatch-mediated ischemia, intravascular thrombosis and endotheliitis, systemic hypoxia, or direct viral insult and injury—each a result of a systemic inflammatory cascade as the SARS-CoV-2 viral spike protein binds to angiotensin-converting enzyme 2 receptors.18 , 19 Indeed, discrimination between COVID-19–related and non–COVID-19–related myocardial injury has been intensely debated and acknowledged to present significant diagnostic and therapeutic uncertainty for frontline clinicians.20
An important group comprises those patients who present with ACS while concurrently infected with COVID-19. Such cases were documented in early observations to experience greater rates of adverse outcomes.21 The worse clinical courses may be explained by:
-
1.
Direct pathophysiological consequences of SARS-CoV-2 infection that may lead to an increased propensity for plaque rupture and thrombus propagation22 and/or,
-
2.
Indirect patient and system-related factors that created delay in receipt of timely medical care.
It became clear that descriptive and mechanistic observational studies were required to better understand this multifaceted disease process.
Acute coronary syndrome and concomitant COVID-19: The International COVID-ACS registry
The International COVID-ACS Registry was designed to evaluate the characteristics and outcomes of ACS patients with concurrent COVID-19 infection.23 As it became clear that this population represented a unique challenge,24 the study was established in March 2020 to elucidate potential mechanisms that may account for the adverse outcomes observed.
The International COVID-ACS Registry has provided a pragmatic means of investigator-initiated data collection via an online web-hosted portal. Lead investigators were cognisant of increased clinical demands, redeployed research personnel, and redistributed funding streams during this period. The criteria for study inclusion were as follows: (1) COVID-19 positive (or high index suspicion according to clinical status and chest imaging findings25) and (2) invasive coronary angiography undertaken for suspected ACS.
A consortium of international investigators collected data from 144 STEMI and 121 NSTE-ACS patients with concomitant COVID-19 infection. The key findings of the study were consistent regardless of ACS subtype (Table 1 ).23 Compared with pre-COVID-19 control cohorts taken from the UK-based British Cardiovascular Intervention Society (BCIS) National PCI Audit,26 and English data from the Myocardial Ischaemia National Audit Project (MINAP) databases,27 COVID-19 positive ACS patients had:
-
1.
A greater burden of comorbidity
-
2.
Longer delays seeking medical attention, and, in the case of STEMI, less frequently received timely reperfusion therapy
-
3.
Higher rates of intensive care unit admission for ventilatory and/or hemodynamic support
-
4.
Greater adverse in-hospital clinical events, including a more than doubling of cardiogenic shock
-
5.
A 4-fold increase of in-hospital mortality
Table 1.
Summary of key findings from the International COVID-ACS registry
| COVID-STEMI (n = 144) | Pre-COVID-19 STEMI Controls (n = 24,961) | COVID NSTE-ACS (n = 121) | Pre-COVID NSTE-ACS Controls (n = 46,389) | |
|---|---|---|---|---|
| Baseline Characteristics | ||||
| Mean age, y (SD) | 64 (13) | 66 (13) | 67 (13) | 70 (13) |
| Male | 78% | 72% | 79% | 66% |
| Hypertension | 65% | 45% | 68% | 58% |
| Hyperlipidemia | 46% | 29% | 63% | 34% |
| Diabetes mellitus | 34% | 21% | 39% | 31% |
| Chronic kidney disease | 10% | 4% | 20% | 10% |
| Symptom onset to admission, min (IQR) | 339.0 (175.0–1481.5) | 173.0 (107.0–387.0) | 417.0 (157.0–2904.0) | 295.0 (130.0–1021.0) |
| Door-to-balloon time, min (IQR) | 83.0 (37.0–336.0) | 37.0 (31.0–109.0) | - | - |
| Postprocedure | ||||
| ICU admission | 46% | NA | 34% | NA |
| Ventilation | 21% | 4% | 12% | 0.4% |
| Pressor support | 27% | 5% | 19% | 0.9% |
| Mechanical support device | 6% | 3% | 0.8% | 0.6% |
| In-hospital outcomes | ||||
| Death | 23% | 6% | 7% | 1% |
| Myocardial infarction | 6% | NA | 4% | NA |
| Stent thrombosis | 1% | NA | 0% | NA |
| Bleeding | 3% | 0.3% | 3% | 0.1% |
| Stroke | 2% | 0.1% | 0.8% | 0.1% |
| Cardiogenic shock | 20% | 9% | 5% | 1% |
| Length of hospital stay, d (IQR) | 6.5 (2.7–12.7) | 3.0 (2.0–5.0) | 6.9 (3.4–18.4) | 5.0 (3.0–8.0) |
Pre-COVID-19 STEMI controls were taken from the British Cardiovascular Intervention Society 2018 to 2019 National Audit database. Pre-COVID-19 NSTE-ACS controls were taken from the Myocardial Ischaemia National Audit Project 2019 database.
Abbreviations: IQR, interquartile range; NA, data not available; NSTE-ACS, non–ST-elevation acute coronary syndrome; SD, standard deviation; STEMI, ST-elevation myocardial infarction.
Adapted from Kite TA, Ludman PF, Gale CP, et al. International Prospective Registry of Acute Coronary Syndromes in Patients With COVID-19. J Am Coll Cardiol. 2021;77(20):2466-2476.
These results have been replicated in similar observational studies that have described in-hospital mortality rates of 23% to 33% in COVID-19 positive STEMI patients, and the predilection for SARS-CoV-2 infection in ACS patients with greater baseline comorbidities and of minority ethnic background (Table 2 ).28 , 29 Furthermore, elevated rates of unfavorable presenting characteristics such as out-of-hospital cardiac arrest, heart failure, and cardiogenic shock in COVID-19–positive STEMI patients have consistently been described in the literature.23 , 28, 29, 30
Table 2.
Key characteristics and outcomes of COVID-19–positive ACS registry studies
| Study | Duration | Design | Size | Inclusion Criteria | Comparator Group | Treatment Delays | Diabetes Mellitus | OHCA | Cardiogenic Shock | In-Hospital Mortality | Other Key Findings |
|---|---|---|---|---|---|---|---|---|---|---|---|
| International COVID-ACS Registry Kite et al,23 2021 |
March 2020 – July 2020 | Prospective, multicenter, international | 144 STEMI, 121 NSTE-ACS | Only if underwent invasive angiography | Pre-COVID-19 BCIS and MINAP databases | Yes | 36% | STEMI: 9% NSTE-ACS: 1% |
STEMI: 20% NSTE-ACS: 5% |
STEMI:23% NSTE-ACS: 7% |
|
| NACMI Registry Garcia et al,28 2021 |
January 2020 – December 2020 | Prospective, multicenter, United States & Canada | 230 STEMI | Invasive angiography and medically managed patients | Historical propensity-matched cohort from Midwest STEMI Consortium | Yes | 46% | 11% | 18% | 33% |
|
| Spanish Infarct Code Registry Rodriguez-Leor et al,30 2021 |
March 2020 – April 2020 | Retrospective, multicenter, Spain | 91 STEMI | Invasive angiography and medically managed patients | Contemporary COVID-19–negative controls | No | 23% | 8% | 10% | 23% |
|
| MINAP registry Rashid et al,29 2021 |
March 2020 – May 2020 | Retrospective, multicenter, England | 153 STEMI, 311 NSTE-ACS | Angiography and medically managed patients | Contemporary COVID-19 negative controls | Yes | 38% | Combined STEMI/NSTE-ACS: 4% | Combined STEMI/NSTE-ACS: 10% | Combined STEMI/NSTE-ACS: 24% |
|
Abbreviations: ACS, acute coronary syndrome; BCIS, British Cardiovascular Intervention Society; MINAP, Myocardial Ischaemia National Audit Project; NACMI, North American COVID-19 Myocardial Infarction; NSTE-ACS, non–ST-elevation acute coronary syndrome; OHCA, out-of-hospital cardiac arrest; STEMI, ST-elevation myocardial infarction.
The principal mechanistic finding of the International COVID-ACS Registry was that time taken for patients to render the hospital was prolonged when compared with pre-COVID controls, and that this was associated with poorer clinical outcomes (symptom onset to admission: COVID-STEMI vs controls: median 339.0 minutes vs 173.0 minutes; P < .001; COVID NSTE-ACS vs controls: 417.0 minutes vs 295.0 minutes; P = .012). In addition, a lengthening of door-to-balloon time in the STEMI subgroup was also observed (COVID-STEMI vs controls: median 83.0 minutes vs 37.0 minutes; P < .001). These delays to reperfusion have also been noted in analyses of COVID-19–negative patients hospitalized with STEMI,31 , 32 thereby suggesting that pathways and well-established systems of care struggled to adapt to the obligatory organizational changes, screening of patients, and preparation of personnel in the catheter laboratory. Such insights in STEMI patients, irrespective of COVID-19 status, provide valuable information and add credence to early hypotheses that deferment in seeking and receiving medical care may, in part, explain the excess mortality rates observed. Public health communications that requested the public “stay at home,” alongside a perceived fear of COVID-19 contagion, appear to have impacted patterns of health care–seeking behavior.
Studies to date have often focused on COVID-19–positive patients with STEMI. The unique scope of the International COVID-ACS registry also afforded insights into patients with NSTE-ACS who underwent an invasive strategy. A striking observation existed that magnitude increases of cardiogenic shock and in-hospital mortality compared with prepandemic controls were similar across both COVID-19–positive ACS subgroups (see Table 1). It is well-established that superior outcomes after STEMI are driven by a time-critical concept dependent on expeditious mechanical reperfusion of an occluded coronary artery. For NSTE-ACS, however, the underlying pathophysiology differs and the association with time from symptom onset to angiography (with or without revascularization) is not nearly as strong when compared with STEMI.33 Although limited by a small number of events in the NSTE-ACS group, acceptance that a median time difference of approximately 2 hours until attendance at hospital between COVID-19–positive NSTE-ACS and pre–COVID-19 control patients would result in such marked differences in outcome is initially problematic. Although confounding factors could be at play, in a cohort of patients who carry a greater comorbidity burden (especially those with concomitant COVID-19 in the COVID-ACS registry),34 the direct effect of COVID-19 infection could be playing a greater part in this ACS subgroup. Worse outcomes in COVID-19–positive NSTE-ACS patients have been associated with excess thrombogenicity, comparable to reports in COVID-19 positive STEMI cases.22 This concept surely warrants further investigation.35
Percutaneous coronary intervention in patients typically treated with coronary artery bypass grafting: the UK-ReVasc registry
Beyond the direct effects of SARS-CoV-2 infection on the global population, the COVID-19 pandemic continues to indirectly impact on mortality and morbidity. Specifically, health care system reorganization, together with changes in patient and clinician behavior, have resulted in restricted access to previously established care pathways, with suggestions that this has led to an increase in deaths from cardiovascular disease.36
In particular, reduced availability of intensive care unit support for procedures such as coronary artery bypass grafting (CABG) and valvular surgery resulted in an up to 80% reduction in cardiac surgical activity during the first wave of the COVID-19 pandemic.37 In the United Kingdom, National Health Service resources were largely reconfigured to only provide care for emergency cases, with clinicians requested to defer treatment for all other patients in preparation for the expected surge of patients with COVID-19 who would require hospitalization and ventilatory support.38
The UK-ReVasc Registry was therefore established as a prospective multicenter registry to investigate the characteristics and outcomes of patients with patterns of coronary artery disease (CAD) that in ordinary circumstances would have been deemed most suitable for CABG surgery,39 but who were instead treated with percutaneous coronary intervention (PCI) because of pandemic-enforced constraints on surgical activity and access to ventilators.40
The registry reported on 215 patients (75% of whom presented with NSTE-ACS) from across the UK and found in-hospital major adverse cardiovascular events were no different when compared with a conventional pre–COVID-19 all-comer PCI population from the British Cardiovascular Intervention Society (BCIS) National Audit database, despite greater complexity of CAD and a more comorbid population in the UK-ReVasc Registry. Low rates of death, MI, stroke, and unplanned revascularization in the registry population persisted out to 30 days follow-up. When compared with isolated CABG data from the United Kingdom, in-hospital mortality was similar, although lower rates of major bleeding and shorter length of hospital stay were observed in the UK-ReVasc Registry group.
To the best of our knowledge, the UK-ReVasc Registry is the only prospective study that has collected data on this specific and novel patient cohort who were required to undergo an alternative mode of revascularization due to the impact of the COVID-19 pandemic. It affords examination of contemporary PCI techniques in a group of patients with high rates of multivessel disease (96%) and left main stem disease (52%), that according to international guidelines should primarily be reserved for CABG.41
Even so, only short-term outcomes have been reported and initial findings perhaps generate more questions than answers. In a population with anatomically complex CAD, does revascularization with contemporary PCI techniques provide comparable and durable longer-term results that are comparable to CABG surgery? Have calcium modification techniques and newer generation drug-eluting stents evolved such that historical revascularization trials require updating to best inform current practice? Longer-term follow-up is required, and ongoing, to inform these important discussions.
Discussion
As we enter the next stages of the COVID-19 pandemic, with decreasing rates of mortality driven by improved therapeutics and mass vaccination strategies, now seems an appropriate juncture to reflect on the impact of this unprecedented crisis. Focus must now shift away from COVID-19 itself and examine the consequences of the SARS-CoV-2 virus on other areas of health service delivery and care.
Cardiovascular disease remains the leading cause of morbidity and mortality globally and is associated with 17.8 million deaths annually.42 Patients with cardiovascular disease have been one of the hardest hit groups during the pandemic period, directly because of SARS-CoV-2 predilection to cause severe infection and death in people with such comorbidities, but also indirectly because of restricted availability and access to routine and urgent health care provision that is recognized to improve clinical outcomes.6 These 2 effects are well illustrated by the International COVID-ACS and UK-ReVasc registries.23 , 39
Governments and public health institutions mandated their citizens to stay at home and reduce social interaction to avoid contagion, particularly those of older age and at high risk of complications after SARS CoV-2 infection.43 Yet, it is this group of individuals, in whom the cardiovascular disease is most prevalent,44 that will have been disadvantaged the most from delays in receiving timely diagnosis and treatment.45 For instance, surges in mechanical complications after ACS have been described during the pandemic, with reports of ventricular septal and free wall rupture,46 , 47 acute functional mitral regurgitation,48 and cardiogenic shock not seen in such frequency since before the establishment of primary PCI networks.49
Perhaps the most noteworthy impact of the pandemic has yet to be quantified. Concerns regarding the provision of care for noncommunicable diseases such as cardiovascular disease and cancer have been raised, but arguably overlooked because of the imminent threat of COVID-19–positive patients overwhelming acute hospitals. Although some patients were able to undergo an alternative treatment strategy, many have been left struggling to access timely and appropriate health care. Analyses from electronic health record and mortality in England estimate that up to 100,000 excess deaths from indirect effects of the COVID-19 pandemic have occurred in patients with cardiovascular disease, predominantly due to reduced supply of, and demand for, cardiac services.50 Beyond this, we are only beginning to see the repercussions of delayed and suboptimal revascularization in patients with ACS that will lead to larger infarct size, adverse ventricular remodeling, heart failure, and arrhythmias.51
Despite the immeasurable suffering caused by COVID-19, it remains remarkable that in the face of adversity health care systems and professionals have remained resilient despite these unprecedented challenges. The 2 multicenter registries presented in this report are examples of the clinical and research communities collaborating to better understand the implications of COVID-19 for patients with ACS. Despite the stark messages delivered, they highlight areas that require further focus and investigation to ensure improved care for our patients. Future concerted research initiatives, support from national political leaders, and robust public education campaigns are therefore required to ameliorate the adverse direct and indirect impact caused by the ongoing COVID-19 pandemic.
Summary
The COVID-19 pandemic has proven a “double threat” to patients with ACS. First, the complex interplay of direct SARS-CoV-2 infection, diagnostic uncertainty in the acute setting, and time delays to hospital in this population have contributed to excess morbidity and mortality. Second, a shift of attention and resource from established service pathways to focus on the surges of COVID-19–positive patients requiring emergency care has required modification of traditionally accepted treatment approaches. Given recent acknowledgment that SARS-CoV-2 endemicity is now inevitable,52 improved public health messaging and adaptation of existing health care systems to provide optimal treatment to both COVID-19 and non–COVID-19 patients is required. Future clinical research initiatives to better understand the COVID-19 and multiple mechanistic factors at play in patients with ACS are essential.
Tribute to Professor Tony Gershlick
Finally, this article would be incomplete without remembrance of Professor Tony Gershlick, pioneer interventional cardiologist, esteemed clinical trialist, revered mentor, and friend to many who died of COVID-19 in November 2020. The chief investigator of both the COVID-ACS and UK-ReVasc registry studies, Tony’s passion for research over a long and distinguished career has resulted in a remarkable impact on cardiovascular care in the United Kingdom and beyond.
Clinics care points
This article focuses on the indirect and direct effects of the COVID-19 pandemic on the diagnosis, treatment, and outcomes of patients with ACS. The following points should be considered by care providers when approaching this important patient population:
-
•
In COVID-19–positive patients, discrimination between ACS and acute myocardial injury is a challenge. In hospitalized COVID-19 patients, elevated cardiac enzymes occur in approximately one-third and portend an increased risk of morbidity and mortality.
-
•
Patients with ACS are more likely to experience delays in receipt of timely care during the COVID-19 pandemic because of changes in health care–seeking behavior and care pathway modifications.
-
•
As compared with pre–COVID-19 cohorts, STEMI and NSTE-ACS patients with concomitant COVID-19 infection experience greater rates of in-hospital bleeding, stroke, cardiogenic shock, and mortality. Delayed medical intervention appears to be a significant mechanistic factor.
-
•
Owing to the indirect effect of the COVID-19 pandemic on health care delivery, many patients with ACS have undergone alternative revascularization strategies (eg, PCI rather than CABG). Short-term outcomes are robust but follow-up of such cohorts is necessary to establish whether long-term clinical outcomes are acceptable.
-
•
The direct and indirect effects of the COVID-19 pandemic on patients with ACS have yet to be precisely defined. Future investigations should aim to understand the complex interplay of SARS-CoV-2 infection and MI. Understanding and addressing the indirect impact of COVID-19 on patients with established cardiovascular disease is of critical importance to optimize care and improve outcomes.
Acknowledgments
Disclosure
C.P. Gale reports personal fees from AstraZeneca, Amgen, Bayer, Boehringer-Ingelheim, Daiichi Sankyo, Vifor Pharma, Menarini, Wondr Medical, Raisio Group, and Oxford University Press; grants from BMS, Abbott, British Heart Foundation, National Institute for Health Research, Horizon 2020, and ESC, outside the submitted work. N. Curzen reports unrestricted research grants from Boston Scientific, HeartFlow, and Beckman Coulter, and speaker/consultancy fees from Boston, Abbott, and HeartFlow outside the submitted work. The remaining authors have no conflicts of interest to declare.
References
- 1.Mafham M.M., Spata E., Goldacre R., et al. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet. 2020;396(10248):381–389. doi: 10.1016/S0140-6736(20)31356-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.De Filippo O., D'Ascenzo F., Angelini F., et al. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med. 2020;383(1):88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bonow R.O., Fonarow G.C., O'Gara P.T., et al. Association of coronavirus disease 2019 (COVID-19) with myocardial injury and mortality. JAMA Cardiol. 2020;5(7):751–753. doi: 10.1001/jamacardio.2020.1105. [DOI] [PubMed] [Google Scholar]
- 4.Richardson S., Hirsch J.S., Narasimhan M., et al. Presenting characteristics, Comorbidities, and outcomes Among 5700 patients hospitalized with COVID-19 in the New York city area. JAMA. 2020;323(20):2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sandoval Y., Januzzi J.L., Jr., Jaffe A.S. Cardiac troponin for Assessment of myocardial injury in COVID-19: JACC review Topic of the Week. J Am Coll Cardiol. 2020;76(10):1244–1258. doi: 10.1016/j.jacc.2020.06.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ball S., Banerjee A., Berry C., et al. Monitoring indirect impact of COVID-19 pandemic on services for cardiovascular diseases in the UK. Heart. 2020;106(24):1890–1897. doi: 10.1136/heartjnl-2020-317870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhou F., Yu T., Du R., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garcia S., Albaghdadi M.S., Meraj P.M., et al. Reduction in ST-segment elevation cardiac Catheterization Laboratory Activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2022;77(16):1994–2003. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rashid M., Gale C.P., Curzen N., et al. Impact of COVID19 pandemic on the incidence and management of out of hospital cardiac arrest in patients presenting with acute myocardial infarction in England. J Am Heart Assoc. 2020;9(22) doi: 10.1161/JAHA.120.018379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wu J., Mamas M.A., Mohamed M.O., et al. Place and causes of acute cardiovascular mortality during the COVID-19 pandemic. Heart. 2020;107(2):113–119. doi: 10.1136/heartjnl-2020-317912. [DOI] [PubMed] [Google Scholar]
- 11.Kwong J.C., Schwartz K.L., Campitelli M.A. Acute myocardial infarction after Laboratory-Confirmed Influenza infection. N Engl J Med. 2018;378(26):2540–2541. doi: 10.1056/NEJMc1805679. [DOI] [PubMed] [Google Scholar]
- 12.Krumholz H. Where have all the heart attacks gone? New York Times. 2020 [Google Scholar]
- 13.Aggarwal N.R., Alasnag M., Mamas M.A. Social media in the era of COVID-19. Open Heart. 2020;7(2) doi: 10.1136/openhrt-2020-001352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Klok F.A., Kruip M., van der Meer N.J.M., et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Doyen D., Moceri P., Ducreux D., et al. Myocarditis in a patient with COVID-19: a cause of raised troponin and ECG changes. Lancet. 2020;395(10235):1516. doi: 10.1016/S0140-6736(20)30912-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shi S., Qin M., Shen B., et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5(7):802–810. doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lala A., Johnson K.W., Januzzi J.L., et al. Prevalence and impact of myocardial injury in patients hospitalized with COVID-19 infection. J Am Coll Cardiol. 2020;76(5):533–546. doi: 10.1016/j.jacc.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Akhmerov A., Marban E. COVID-19 and the heart. Circ Res. 2020;126(10):1443–1455. doi: 10.1161/CIRCRESAHA.120.317055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Libby P., Luscher T. COVID-19 is, in the end, an endothelial disease. Eur Heart J. 2020;41(32):3038–3044. doi: 10.1093/eurheartj/ehaa623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Giustino G., Pinney S.P., Lala A., et al. Coronavirus and cardiovascular disease, myocardial injury, and arrhythmia: JACC focus Seminar. J Am Coll Cardiol. 2020;76(17):2011–2023. doi: 10.1016/j.jacc.2020.08.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stefanini G.G., Montorfano M., Trabattoni D., et al. ST-elevation myocardial infarction in patients with COVID-19: clinical and angiographic outcomes. Circulation. 2020;141(25):2113–2116. doi: 10.1161/CIRCULATIONAHA.120.047525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Choudry F.A., Hamshere S.M., Rathod K.S., et al. High thrombus burden in patients with COVID-19 presenting with ST-elevation myocardial infarction. J Am Coll Cardiol. 2020;76(10):1168–1176. doi: 10.1016/j.jacc.2020.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kite T.A., Ludman P.F., Gale C.P., et al. International prospective registry of acute coronary syndromes in patients with COVID-19. J Am Coll Cardiol. 2021;77(20):2466–2476. doi: 10.1016/j.jacc.2021.03.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bangalore S., Sharma A., Slotwiner A., et al. ST-Segment elevation in patients with Covid-19 - a case series. N Engl J Med. 2020;382(25):2478–2480. doi: 10.1056/NEJMc2009020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Simpson S., Kay F.U., Abbara S., et al. Radiological society of North America Expert Consensus Statement on reporting chest CT findings related to COVID-19. Endorsed by the society of Thoracic Radiology, the American College of Radiology, and RSNA - secondary Publication. J Thorac Imaging. 2020;35(4):219–227. doi: 10.1097/RTI.0000000000000524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ludman P. British Cardiovascular Intervention Society database: insights into interventional cardiology in the United Kingdom. Heart. 2019;105(16):1289. doi: 10.1136/heartjnl-2018-314533. [DOI] [PubMed] [Google Scholar]
- 27.Wilkinson C., Weston C., Timmis A., et al. The myocardial Ischaemia national Audit Project (MINAP) Eur Heart J Qual Care Clin Outcomes. 2020;6(1):19–22. doi: 10.1093/ehjqcco/qcz052. [DOI] [PubMed] [Google Scholar]
- 28.Garcia S., Dehghani P., Grines C., et al. Initial findings from the North American COVID-19 myocardial infarction registry. J Am Coll Cardiol. 2021;77(16):1994–2003. doi: 10.1016/j.jacc.2021.02.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rashid M., Wu J., Timmis A., et al. Outcomes of COVID-19-positive acute coronary syndrome patients: a multisource electronic healthcare records study from England. J Intern Med. 2021;290(1):88–100. doi: 10.1111/joim.13246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rodriguez-Leor O., Cid Alvarez A.B., Perez de Prado A., et al. In-hospital outcomes of COVID-19 ST-elevation myocardial infarction patients. EuroIntervention. 2021;16(17):1426–1433. doi: 10.4244/EIJ-D-20-00935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.De Luca G., Verdoia M., Cercek M., et al. Impact of COVID-19 pandemic on mechanical reperfusion for patients with STEMI. J Am Coll Cardiol. 2020;76(20):2321–2330. doi: 10.1016/j.jacc.2020.09.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Xiang D., Xiang X., Zhang W., et al. Management and outcomes of patients with STEMI during the COVID-19 pandemic in China. J Am Coll Cardiol. 2020;76(11):1318–1324. doi: 10.1016/j.jacc.2020.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ting H.H., Chen A.Y., Roe M.T., et al. Delay from symptom onset to hospital presentation for patients with non-ST-segment elevation myocardial infarction. Arch Intern Med. 2010;170(20):1834–1841. doi: 10.1001/archinternmed.2010.385. [DOI] [PubMed] [Google Scholar]
- 34.McManus D.D., Gore J., Yarzebski J., et al. Recent trends in the incidence, treatment, and outcomes of patients with STEMI and NSTEMI. Am J Med. 2011;124(1):40–47. doi: 10.1016/j.amjmed.2010.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Matsushita K., Hess S., Marchandot B., et al. Clinical features of patients with acute coronary syndrome during the COVID-19 pandemic. J Thromb Thrombolysis. 2021;52(1):95–104. doi: 10.1007/s11239-020-02340-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wadhera R.K., Shen C., Gondi S., et al. Cardiovascular deaths during the COVID-19 pandemic in the United States. J Am Coll Cardiol. 2021;77(2):159–169. doi: 10.1016/j.jacc.2020.10.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mohamed Abdel Shafi A., Hewage S., Harky A. The impact of COVID-19 on the provision of cardiac surgical services. J Card Surg. 2020;35(6):1295–1297. doi: 10.1111/jocs.14631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.NHS England Next steps on NHS response to COVID-19: Letter from Sir Simon Stevens and Amanda Pritchard. 2020. https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/20200317-NHS-COVID-letter-FINAL.pdf Available at: Accessed 10th September 2021.
- 39.Kite T.A., Ladwiniec A., Owens C.G., et al. Outcomes following PCI in CABG candidates during the COVID-19 pandemic: the prospective multicentre UK-ReVasc registry. Catheter Cardiovasc Interv. 2021;99(2):305–313. doi: 10.1002/ccd.29702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Harky A., Harrington D., Nawaytou O., et al. COVID-19 and cardiac surgery: the perspective from United Kingdom. J Card Surg. 2020;36(5):1649–1658. doi: 10.1111/jocs.15039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Neumann F.J., Sousa-Uva M., Ahlsson A., et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40(2):87–165. doi: 10.1093/eurheartj/ehy855. [DOI] [PubMed] [Google Scholar]
- 42.Group W.C.R.C.W. World Health Organization cardiovascular disease risk charts: revised models to estimate risk in 21 global regions. Lancet Glob Health. 2019;7(10):e1332–e1345. doi: 10.1016/S2214-109X(19)30318-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.World Health Organization Coronavirus disease (COVID-19) advice for the public. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public Available at: Accessed 13 October 2021.
- 44.Bae S., Kim S.R., Kim M.N., et al. Impact of cardiovascular disease and risk factors on fatal outcomes in patients with COVID-19 according to age: a systematic review and meta-analysis. Heart. 2021;107(5):373–380. doi: 10.1136/heartjnl-2020-317901. [DOI] [PubMed] [Google Scholar]
- 45.Kiss P., Carcel C., Hockham C., et al. The impact of the COVID-19 pandemic on the care and management of patients with acute cardiovascular disease: a systematic review. Eur Heart J Qual Care Clin Outcomes. 2021;7(1):18–27. doi: 10.1093/ehjqcco/qcaa084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Alsidawi S., Campbell A., Tamene A., et al. Ventricular septal rupture complicating delayed acute myocardial infarction presentation during the COVID-19 pandemic. JACC Case Rep. 2020;2(10):1595–1598. doi: 10.1016/j.jaccas.2020.05.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Albiero R., Seresini G. Subacute left ventricular free wall rupture after delayed STEMI presentation during the COVID-19 pandemic. JACC Case Rep. 2020;2(10):1603–1609. doi: 10.1016/j.jaccas.2020.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kunkel K.J., Anwaruddin S. Papillary Muscle rupture due to delayed STEMI presentation in a patient self-Isolating for Presumed COVID-19. JACC Case Rep. 2020;2(10):1633–1636. doi: 10.1016/j.jaccas.2020.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Moroni F., Gramegna M., Ajello S., et al. Collateral Damage: medical care avoidance behavior Among patients with myocardial infarction during the COVID-19 pandemic. JACC Case Rep. 2020;2(10):1620–1624. doi: 10.1016/j.jaccas.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Banerjee A., Chen S., Pasea L., et al. Excess deaths in people with cardiovascular diseases during the COVID-19 pandemic. Eur J Prev Cardiol. 2021;28(14):1599–1609. doi: 10.1093/eurjpc/zwaa155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sutton M.G., Sharpe N. Left ventricular remodeling after myocardial infarction: pathophysiology and therapy. Circulation. 2000;101(25):2981–2988. doi: 10.1161/01.cir.101.25.2981. [DOI] [PubMed] [Google Scholar]
- 52.Phillips N. The coronavirus is here to stay - here's what that means. Nature. 2021;590(7846):382–384. doi: 10.1038/d41586-021-00396-2. [DOI] [PubMed] [Google Scholar]