Abstract
Purpose:
Evaluate differences in eyecare utilization among glaucoma patients by race and socioeconomic status (SES).
Design:
Retrospective cohort study.
Subjects:
Representative 5% sample of Medicare beneficiaries >65 years with continuous part A/B enrollment between 1/1/2014 and 7/1/2014, at least one diagnosis code for glaucoma within that period, and a glaucoma diagnosis in the Chronic Conditions Warehouse before 1/1/2014.
Methods:
The following race/ethnicity categories were defined in our cohort: Non-Hispanic White, Black/African American, Hispanic and Asian/Pacific Islander. Low SES was defined as having two or more enrollment-based low-income indicators (dual eligibility for Medicare/Medicaid, Part D limited income subsidies, and eligibility for Part A and B State buy-in). Negative binomial regression analyses were carried out to compare relative rate ratios (RR) of eye care utilization among racial groups, stratified by low- and non-low-SES.
Main outcome measures:
Measured from 7/1/2014–12/31/2016: eye examinations and eye care-related office visits; eye care-related inpatient and ED encounters; eye care-related nursing home and home-visit encounters; visual field and retinal nerve fiber optical coherence tomography tests; glaucoma lasers and surgeries.
Results:
Among 78,526 participants with glaucoma, mean age was 79.1 years (SD 7.9 years), 60.9% were female, 78.4% were non-Hispanic White and 13.8% met enrollment-based criteria for low-SES. Compared to White beneficiaries, Blacks had lower counts of outpatient visits (rate ratio [RR] 0.92, 95% CI 0.90–0.93), VF tests (RR 0.92, 95% CI 0.90–0.94), but more inpatient/ED encounters (RR 2.42, 95% CI 1.55–3.78), and surgeries (RR 1.14, 95% CI 1.03–1.7). Hispanics had fewer outpatient visits (RR 0.97, 95% CI 0.95–0.98) and RNFL OCT tests (RR 0.89, 95% CI 0.86–0.93), but more inpatient/ED encounters (RR 2.32, 95% CI 1.18–4.57) and SLT (RR 1.25, 95% CI 1.11–1.42) vs. non-Hispanic Whites. In the non-low-SES group, Black vs. White disparities persisted in outpatient visits (RR 0.93 95% CI 0.92–0.95), VF (RR 0.96 95% CI 0.94–0.98), RNFL OCT (RR 0.81, 95% CI 0.78–0.83) and inpatient/ED encounters (RR 2.57, 95% CI 1.55–4.26).
Conclusions:
Disparities were found in eye care utilization among Black and Hispanic glaucoma patients. These differences persisted among Blacks after stratification by SES, suggesting systemic racism may be an independent driver in this population.
Keywords: Disparities, glaucoma, utilization, Medicare
Introduction
In the United States, glaucoma disproportionately affects individuals belonging to racial minorities. The prevalence of glaucoma is known to be higher among Black and Hispanic Americans compared to Whites1,2. Once diagnosed with glaucoma, Black patients are more likely than Whites to develop vision impairment or blindness3,4. Causes of disparities in glaucoma prevalence and outcomes are likely multifactorial, and racial differences in eye care utilization may drive some of these disparities. Black and Hispanic/Latino populations are less likely to be insured, and more likely to delay or forgo necessary healthcare, compared to non-Hispanic White populations5. Despite higher prevalence and severity of glaucoma in Black populations, eye care utilization rates are disproportionately lower than for White populations6–9.
While related to racial disparities, socioeconomic (SES) disparities are a separate and important construct. Globally, low SES is associated with a greater disease burden10: countries with higher human development indices and mean years of schooling were associated with lower glaucoma-related disability adjusted life years. In the United States, disparities have been found in the receipt of glaucoma care between Medicaid beneficiaries and those enrolled in commercial health insurance11. However, SES disparities in eye care utilization among glaucoma patients in the United States have yet to be fully charactarized12.
Examining the impact of race, socioeconomic status and the interaction between these two factors on eye care utilization in glaucoma patients may help identify social sources of disparities in glaucoma care13. In turn, a better understanding of sociodemographic influences on glaucoma care will allow for risk-stratification of patients with glaucoma and guide future research and treatment. The current study uses a national 5% sample of US Medicare beneficiaries with glaucoma to describe racial differences in the frequency of eye care-related outpatient encounters, inpatient/emergency department encounters, clinical tests, and surgical intervention. Further, we explore the intersection of race and SES in our population.
Methods
Data Source
Data for this study were derived from a nationally representative random sample of Medicare beneficiaries from 01/01/2014 until 12/31/2016 consisting of approximately 2.9 million individuals, constituting 5% of all beneficiaries. The data obtained from the Center for Medicare and Medicaid Services (CMS) contain covered inpatient/ED and outpatient fee-for-service claims.
Patient Selection
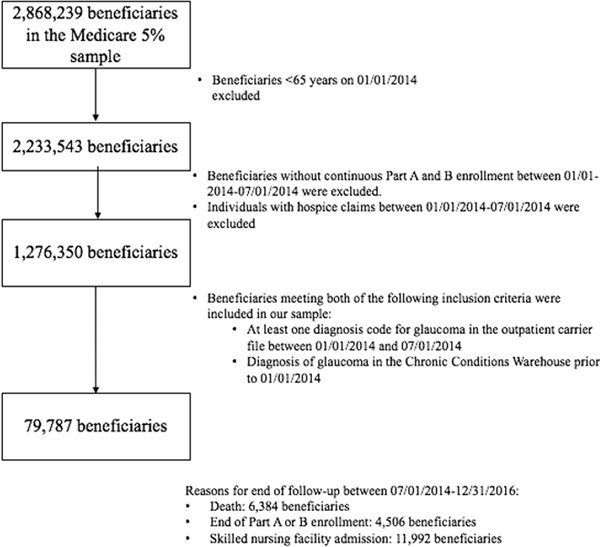
A cohort of glaucoma patients was created by including beneficiaries who met the following criteria: age >65 on January 1st, 2014, continuous part A and B Medicare enrollment between January 1st, 2014 and July 1st, 2014, at least one diagnosis code for glaucoma (International Classification of Diseases, Ninth revision [ICD-9] codes 365.1–365.9 and ICD-10 codes H40.1-H40.9, H42) in the outpatient carrier file during the 6-month enrollment period (between 01/01/2014 and 07/01/2014) and diagnosis of glaucoma in the Chronic Conditions Warehouse prior to January 1st, 2014 and present in the 5% sample as of January 1st, 2014. Beneficiaries younger than 65 years, without continuous Part A and B enrollment and/or with hospice claims during the 6-month enrollment period were excluded (Figure 1).
Figure 1:
Flowchart of participants in the Medicare 5% sample enrolled in this study based on enrollment criteria
Race/ethnicity and socioeconomic status measures
The following race/ethnicity categories were defined in our cohort: Non-Hispanic White, Black/African American, Hispanic and Asian/Pacific Islander. Medicare categories for race and ethnicity have been found to be valid when compared to the gold-standard of self-reported race/ethnicity, especially among Black/African American beneficiaries14. Socioeconomic status (SES) was defined using Medicare enrollment-based low-income indicators, including dual eligibility for Medicare/Medicaid, Part D limited income subsidies, and eligibility for Part A and B State buy-in. To ensure adequate capture, only individuals with 2 or more of these indicators were classified as low SES15.
Outcomes
Eye care utilization outcomes of interest were derived from claims data using common procedural terminology (CPT) codes, and included the following categories of outcomes: 1) eye examinations and eye care-related office visits and consultations (Common Procedural Terminology [CPT] codes 92002, 92004, 92012, 92014, 92018, 92019 excluding post-operative code 99024; evaluation and management codes 9201–5, 99211–5, 99241–5, 99354, 99355); 2) eye care-related inpatient and emergency department encounters (CPT codes 99221–3, 99231–3, 99251–5, 99281–5); 3) nursing home and home visit encounters (CPT codes 99301–9, 99310, 99315, 99231–3, 99251–5, 99281–5, 99301–9, 99310, 99315, 99318, 99325–7, 99334–7, 99342–5, 99347–50); 4) visual field (CPT codes 92081–3) and retinal nerve fiber optical coherence tomography (RNFL OCT) tests (CPT codes 92133, 92134); and 5) glaucoma lasers or surgeries including selective laser trabeculoplasty, trabeculectomy, aqueous shunt placement and minimally invasive glaucoma surgery with or without concurrent cataract extraction (CPT codes 66170, 66172. 66183, 0192T, 66180, 67255, 0191T, 0253T, 0191T, 0376T, 0474T, 0449T, 0450T, 66711, 65820, 66990, 66999, 66174, 66175, 66999, 66183, 66179, 66180). Only CPT codes associated with a provider specialty code for an ophthalmologist (18), optometrist (41) or ambulatory care center (49) were included. CPT codes were not restricted to those associated with a primary diagnosis of glaucoma. Utilization outcomes were assessed between July 1st, 2014 and December 31st, 2016.
Statistical Analyses
Descriptive statistics were used to determine annual frequencies of eye care utilization by race. Frequency of outcomes was calculated in 100 person-years, accounting for variation in follow-up time. Multiple CPT codes for the same category occurring on the same day were counted as one visit or procedure. Negative binomial regression analyses were carried out to compare relative rate ratios (RR) of eye care utilization among racial groups as compared to non-Hispanic Whites. To understand the interaction between race and SES, separate negative binomial regression analyses were carried out comparing relative RR of eye care utilization between racial groups stratified by low-SES and non-low-SES. Models were adjusted for age, medical comorbidities (assessed using a single numerical comorbidity score that combines measures of the Charlson comorbidity index and the Elixhauser comorbidity classification, and that has performed better at predicting short-and long-term mortality than either individual index)16 and glaucoma type and severity based on ICD-9 and −10 codes to account for potential closer monitoring of patients with more severe disease.
Results
The sample of Medicare beneficiaries meeting inclusion criteria was comprised of 78 526 individuals, with a mean age of 79.1 years (SD 7.9 years). 60.9% of beneficiaries in our sample were female and 78.4% were non-Hispanic White (Table 1). Within the sample of Medicare beneficiaries meeting eligibility criteria for age and enrollment status, the prevalence of glaucoma was 6.2%. The prevalence of glaucoma in our sample was 5.8% among Whites, 10.8% among Blacks, 6.3% among Hispanics and 7.3% among Asians. Diagnosis codes for glaucoma severity were not available in 63.1% of beneficiaries. In regression analyses, beneficiaries with missing severity codes were treated as a separate group and were not removed from the analyses. The proportion of individuals with a diagnosis code for severe glaucoma was 8.5% among White beneficiaries, 11.3% among Blacks, 9% among Hispanics and 8.8% among Asians (p<0.001). Overall, 13.8% of beneficiaries with glaucoma met criteria for low-SES. The proportion of beneficiaries meeting low-SES criteria was 7.5% among Whites, 29.3% among Blacks, 48.0% among Hispanics and 47.4% among Asians (p<0.001).
Table 1:
Cohort characteristics
| Characteristics | Total (N=1 276 350) | Non-Hispanic White (N=1 055 989) | Black/Afric an American (N=95 516) | Hispanic (N=67 083) | Asian/Pacif ic Islander (N=32 576) | p-value |
|---|---|---|---|---|---|---|
| Beneficiaries with diagnosis codes for glaucoma, n (%) | 78 526 (6.2) | 61 543 (5.8) | 10 363 (10.8) | 4 247 (6.3) | 2 373 (7.3) | |
|
| ||||||
| Age, mean (SD) | 79.1 (7.9) | 79.5 (7.9) | 77.5 (7.8) | 78.0 (7.4) | 78.1 (7.6) | <0.001a |
| Female, n (%) | 47 794 (60.9) | 37 191 (60.4) | 6 550 (63.2) | 2 665 (62.8) | 1 388 (58.5) | <0.001b |
| Enrollment-based socioeconomic status, n (%) | ||||||
| Full/partial dual eligibility for Medicare & Medicaid | 10 825 (13.8) | 4 640 (7.5) | 3 031 (29.2) | 2 029 (47.8) | 1 125 (47.4) | <0.001b |
| Part A/B state buy-in | 10 065 (12.8) | 4 119 (6.7) | 2 854 (27.5) | 1 975 (46.5) | 1 117 (47.1) | <0.001b |
| Full/partial Part D limited income subsidies | 12 305 (15.7) | 5 493 (8.9) | 3 488 (33.7) | 2 175 (51.2) | 1 149 (48.4) | <0.001b |
| Two or more low-income indicators ( | 10 841 (13.8) | 4 636 (7.5) | 3 041 (29.3) | 2 040 (48.0) | 1 124 (47.4) | <0.001b |
| Glaucoma prevalence (%)c | 6.2 | 5.8 | 10.8 | 6.3 | 7.3 | |
| Diagnosis code for severe glaucoma, n(%) | 6 995 (8.9) | 5 228 (8.5) | 1 176 (11.3) | 383 (9.0) | 208 (8.8) | <0.001b |
ANOVA
Pearson’s X2 test
Calculated by dividing the number of beneficiaries with glaucoma meeting eligibility criteria, divided by all beneficiaries in the Medicare 5% enhanced sample >65 years, excluding beneficiaries without continuous Medicare enrollment and those with hospice claims between 1/1/14–7/1/14.
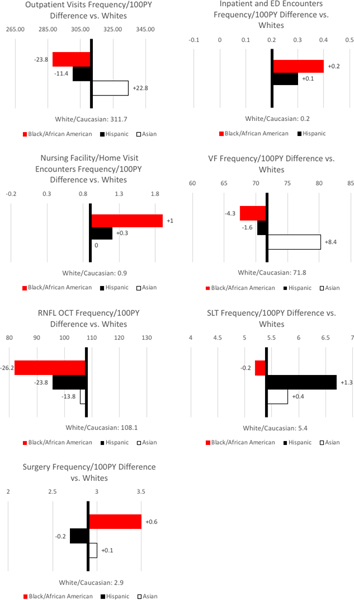
Differences in eye care utilization by race
Compared to White beneficiaries, Black beneficiaries had lower frequencies/100 person-years (100PY) of outpatient visits (287.9 vs. 311.7; rate ratio [RR] 0.92, 95% CI 0.90–0.93), VF tests (67.5 vs. 71.8; RR 0.92, 95% CI 0.90–0.94), RNFL OCT tests (81.9 vs. 108.1; RR 0.76, 95% CI 0.75–0.78), but higher frequencies/100PY of inpatient/ED encounters (0.4 vs. 0.2; RR 2.42, 95% CI 1.55–3.78), nursing facility/home visit encounters (1.9 vs. 0.8; RR 2.99, 95% CI 2.18–4.11) and surgery (3.5 vs. 2.9; RR 1.14, 95% CI 1.03–1.7) (Figure 2; Table 2). Hispanic beneficiaries had lower frequencies/100PY than Whites of outpatient visits (300.3 vs. 311.7; RR 0.97, 95% CI 0.95–0.98) and RNFL OCT tests (95.7 vs. 108.1; RR 0.89, 95% CI 0.86–0.93), but higher frequencies of inpatient/ED encounters (0.3 vs. 0.2; RR 2.32, 95% CI 1.18–4.57), nursing facility/home visit encounters (1.2 vs. 0.8; RR 1.72, 95% CI 1.05–2.81) and SLT (6.7 vs 5.4; RR 1.25, 95% CI 1.11–1.42). Asian beneficiaries had higher frequencies/100PY than Whites of outpatient visits (334.5 vs. 311.7; RR 1.07, 95% CI 1.05–1.10) and VF tests (70.2 vs 71.8; RR 1.10, 95% CI 1.07–1.14). No other differences were found between race/ethnicity categories.
Figure 2:
Utilization Rates in Person-Years by Race
Table 2:
Negative binomial regression results assessing rate ratio for each utilization category by racial group, accounting for age, comorbidities and glaucoma severity.
| Incident Rate Ratio | ||||
|---|---|---|---|---|
| Outcomes | Non-Hispanic White | Black (Or African American) | Hispanic | Asian/Pacific Islander |
| Outpatient eye examinations, office visits, consultations | 1.00 (1.00, 1.00) | 0.92 (0.90, 0.93) | 0.97 (0.95, 0.98) | 1.07 (1.05, 1.10) |
| Inpatient, emergency department encounters nursing home and home visits | 1.00 (1.00, 1.00) | 2.42 (1.55, 3.78) | 2.32 (1.18, 4.57) | n ≤ 10 |
| Nursing facility and home visit encounters | 1.00 (1.00, 1.00) | 2.99 (2.18, 4.11) | 1.72 (1.05, 4.11) | 1.47 (0.76, 2.82) |
| VF tests | 1.00 (1.00, 1.00) | 0.92 (0.90, 0.94) | 0.97 (0.95, 1.00) | 1.10 (1.07, 1.14) |
| RNFL OCT | 1.00 (1.00, 1.00) | 0.76 (0.75, 0.78) | 0.89 (0.86, 0.93) | 0.99 (0.94, 1.03) |
| SLT | 1.00 (1.00, 1.00) | 0.94 (0.86, 1.03) | 1.25 (1.11, 1.42) | 1.06 (0.90, 1.26) |
| Glaucoma surgeries | 1.00 (1.00, 1.00) | 1.14 (1.03, 1.27) | 0.92 (0.78, 1.10) | 1.02 (0.82, 1.26) |
Differences in eye care utilization by race and socioeconomic status
Within the low SES group, Black beneficiaries had lower counts of VF tests (RR 0.95, 95% CI 0.90–0.99) and RNFL OCT tests (RR 0.79 95% CI 0.74–0.83) vs Whites (Table 3). Low SES Hispanic and Asian beneficiaries had higher counts of outpatient visits (Hispanic: RR 1.07 95% CI 1.04–1.11; Asian: RR 1.24 95% CI 1.19–1.29), VF tests (Hispanic: RR 1.21 95% CI 1.15–1.27; Asian: RR 1.32 95% CI 1.25–1.40), RNFL OCT tests (Hispanic: RR 1.08 95% CI 1.02–1.15; Asian: RR 1.24 95% CI 1.15–1.34) and SLT (Hispanic: RR 1.97 95% CI 1.58–2.47; Asian: RR 1.51 95% CI 1.14–1.99). Low SES Hispanic beneficiaries additionally had lower counts of nursing facility/home visit encounters compared to low SES Whites (RR 0.45, 95% CI 0.26–0.78).
Table 3:
Negative binomial regression results assessing rate ratio for each utilization category with interactions by race, stratified by SES, accounting for age, comorbidities and glaucoma severity.
| Non-Hispanic White | Black (or African American) | Hispanic | Asian/Pacific Islander | |
|---|---|---|---|---|
|
| ||||
|
Low-SES
| ||||
| Outpatient eye examinations, office visits, consultations | 1.00 (1.00, 1.00) | 0.97 (0.94, 1.00) | 1.07 (1.04, 1.11) | 1.24 (1.19, 1.29) |
| Inpatient, emergency department encounters | 1.00 (1.00, 1.00) | 1.76 (0.62, 4.99) | n ≤ 10 | n ≤ 10 |
| Nursing facility and home visit encounters | 1.00 (1.00, 1.00) | 1.30 (0.84, 2.02) | 0.45 (0.26, 0.78) | n ≤ 10 |
| Visual field (VF) tests | 1.00 (1.00, 1.00) | 0.95 (0.90, 0.99) | 1.21 (1.15, 1.27) | 1.32 (1.25, 1.40) |
| Retinal nerve fiber layer optical coherence tomography (RNFL OCT) tests | 1.00 (1.00, 1.00) | 0.79 (0.74, 0.83) | 1.08 (1.02, 1.15) | 1.24 (1.15, 1.34) |
| Selective laser trabeculoplasties (SLT) | 1.00 (1.00, 1.00) | 1.09 (0.88, 1.35) | 1.97 (1.58, 2.47) | 1.51 (1.14, 1.99) |
| Glaucoma surgeries | 1.00 (1.00, 1.00) | 1.14 (0.86, 1.51) | 1.16 (0.84, 1.60) | 1.37 (0.94, 1.98) |
|
| ||||
| Non-Low-SES | ||||
|
| ||||
| Outpatient eye examinations, office visits, consultations | 1.00 (1.00, 1.00) | 0.93 (0.92, 0.95) | 0.98 (0.95, 1.00) | 1.06 (1.02, 1.10) |
| Inpatient, emergency department encounters | 1.00 (1.00, 1.00) | 2.57 (1.55, 4.26) | n ≤ 10 | n ≤ 10 |
| Nursing facility and home visit encounters | 1.00 (1.00, 1.00) | 1.45 (0.98, 2.16) | 1.23 (0.62, 2.45) | n ≤ 10 |
| Visual field (VF) tests | 1.00 (1.00, 1.00) | 0.96 (0.94, 0.98) | 0.99 (0.96, 1.02) | 1.14 (1.10, 1.19) |
| Retinal nerve fiber layer optical coherence tomography (RNFL OCT) tests | 1.00 (1.00, 1.00) | 0.81 (0.78, 0.83) | 0.92 (0.88, 0.96) | 0.99 (0.93, 1.05) |
| Selective laser trabeculoplasties (SLT) | 1.00 (1.00, 1.00) | 0.97 (0.88, 1.07) | 1.05 (0.89, 1.25) | 0.99 (0.79, 1.24) |
| Glaucoma surgeries | 1.00 (1.00, 1.00) | 1.23 (1.09, 1.38) | 0.97 (0.78, 1.21) | 1.03 (0.78, 1.35) |
Within the non-low-SES group, Black beneficiaries had lower counts of outpatient visits (RR 0.93 95% CI 0.92–0.95), VF tests (RR 0.96 95% CI 0.94–0.98), RNFL OCT tests (RR 0.81 95% CI 0.78–0.83), but higher counts of inpatient/ED visits (RR 2.57, 95% CI 1.55–4.26) and glaucoma surgery (RR 1.23, 95% CI 1.09–1.38) vs. Whites (Table 3). Non-low-SES Hispanic beneficiaries had lower counts of RNFL OCT tests (RR 0.92, 95% CI 0.88–0.96) vs. non-low-SES White beneficiaries. Asian beneficiaries in the non-low-SES group had higher counts of outpatient visits (RR 1.06, 95% CI 1.02–1.10), VF tests (RR 1.14, 95% CI 1.10–1.19) than White beneficiaries in this group.
Discussion
Here we demonstrate significant differences in eye care utilization among Black/African American, Hispanic and Asian Medicare beneficiaries compared to their White counterparts. Despite the higher prevalence and severity of glaucoma in Black and Hispanic populations, we found lower age and glaucoma-severity adjusted counts of outpatient ophthalmology visits and glaucoma testing among this population. Such disparities were less pronounced among Asian beneficiaries. Importantly, differences in utilization between Black and White beneficiaries persisted when frequencies were stratified by SES group. However, differences between other racial/ethnic groups and Whites were in larger part explained by socioeconomic status.
While Black and Hispanic beneficiaries with glaucoma were less likely to receive outpatient eye examinations or consultations than Whites, they were more likely to have inpatient, ED, nursing facility or home visit encounters with an ophthalmologist. The high relative risk and wide confidence intervals found in ED, inpatient, nursing facility and home visit encounters among Black and Hispanic beneficiaries compared to Whites are likely due to the small sample size of participants who have undergone eye examinations in acute settings (Table S1, available at https://www.aaojournal.org). A prior study using Medicare claims data showed that Black beneficiaries with glaucoma were more likely than Whites to have no eye examinations within a 10-year period, but there were similar rates of examinations among individuals with regular access to care17, without distinguishing between eye examinations received in outpatient settings and those received in inpatient/ED settings. In our study, the variation in eye care utilization by healthcare setting points to more irregular access to preventative eye care among Black and Hispanic beneficiaries, with less regular monitoring of disease progression, as evidenced by the lower frequencies of glaucoma testing among Black and Hispanic beneficiaries compared to Whites, and a greater likelihood of receiving eye care in acute settings such as inpatient and ED encounters. Barriers in access to care for racial minorities are well-documented and include lower levels of health insurance coverage, geographic variations in access to high-quality care, and systematic racial differences in quality of care18.
In addition to racial differences in the frequencies of outpatient visits and glaucoma testing, we found that Black and Hispanic beneficiaries were more likely to undergo glaucoma procedures, with Blacks being more likely than Whites to receive glaucoma surgery, while Hispanics were more likely to receive SLT procedures. A previous analysis of utilization rates among Medicare beneficiaries with glaucoma has shown that rates of glaucoma surgery are higher in Blacks than in Whites, consistent with our findings17. Nevertheless, other studies analyzing glaucoma surgery rates among all Medicare beneficiaries, irrespective of glaucoma diagnosis, have found a lower rate of glaucoma surgery among Blacks compared to Whites, after adjusting for expected glaucoma prevalence8,19. These previous findings suggest that, as a population, Black individuals are underdiagnosed and undertreated. However, after receiving a glaucoma diagnosis, Black patients are more likely than Whites to undergo surgery. In our sample, we hypothesize that Black beneficiaries with glaucoma received less monitoring, as evidenced by the lower counts of outpatient examinations and glaucoma testing and had more severe and progressive disease at presentation, resulting in a greater likelihood of needing glaucoma surgery. Indeed, in our sample, a higher proportion of Black beneficiaries had a diagnosis code for severe glaucoma compared to Whites. A second potential explanation for both the higher rate of glaucoma procedures among Black and Hispanic patients may be due to differences in patient medication adherence and physician perceptions of adherence. Glaucoma medication adherence, key to preventing disease progression among glaucoma patients20,21, has been shown to be lower among Black patients than Whites22,23, and providers may choose SLT or surgery over medical treatment for glaucoma if they suspect that a patient will not adhere to medications. Similarly, perceptions of medication adherence among physicians are associated with race, with physicians in other settings being more likely to under-estimate medication adherence among Black patients than Whites24. Finally, in addition to glaucoma severity and medication adherence, patient race alone has been shown to influence physician recommendations, irrespective of clinical factors, appropriateness, insurance coverage and physician characteristics25.
While prior studies have reported on either race- or SES-based disparities in glaucoma care, studies of race or SES alone may be insufficient to fully understand the social and economic contributors of disparities in health13. Here, we report rates of glaucoma care utilization by race, stratified by low- and non-low-SES groups. We found that disparities among Black relative to White beneficiaries persisted regardless of socioeconomic status. Within both low- and non-low-SES groups, Black individuals continued to have lower rates of glaucoma testing and higher rates of eye care utilization in inpatient/ED settings. Black beneficiaries also continued to have higher rates of glaucoma surgery within the non-low-SES group. These findings suggest that for Black beneficiaries, SES alone does not explain disparities in eye care utilization. A similar pattern has been reported in intersectional studies of disparities related to other health measures, such as opioid use and pediatric outcomes26,27. This pattern may be explained by the Minorities Diminishing Returns Theory (MDRT)28,29, which suggests that while differences in access to resources (i.e., SES differences) play an important role in health disparities, additional barriers to accessing good health outcomes, such as racism, exert their effect downstream of SES. Systemic racism, persistent inter-generational inequities in housing, healthcare, education and political representation, is rooted in structural discrimination and can itself be a direct barrier to eye care utilization, resulting in disparities among Black patients regardless of their SES30,31. This is reflected in the difficulty of relieving race-based disparities by interventions targeting improving SES alone32–34. Moreover, MDRT provides an explanatory framework for why healthcare disparities are not limited to low SES individuals, as demonstrated in the present study28,29.
Unlike Black beneficiaries, low-SES Asian and Hispanic beneficiaries had similar or higher rates of utilization compared to White counterparts. While these results may suggest that racial disparities may not play as large a roll in differences in eyecare utilization among these racial minorities, a large proportion of Asian and Hispanic communities in the United States have undocumented immigrant status, limiting their access to federal and state benefits, including Medicare and Medicaid35–38. Research that does not include undocumented immigrants, such as the present study, may underestimate healthcare disparities, particularly among Hispanic and Asian patients. One study published in 1996 demonstrated that laws designed to bar undocumented immigrants from medical care can lead to reductions in utilization of ophthalmic care39,40. To date, there is limited ophthalmologic research focusing on care for undocumented immigrants in the US. Further research is needed to improve healthcare, and specifically eye care services for undocumented immigrants.
Our study had several noteworthy strengths. We utilized a large, representative sample of 78 526 Medicare beneficiaries age 65 years and older with glaucoma and measured outcomes over an 18-month period. Third, our analysis evaluates the interaction between race and SES in glaucoma care, which has been understudied. However, the results of this study should be interpreted in light of several limitations. First, claims-based procedure and visit codes in Medicare rely on accurate coding by practicing physicians. This may lead to some systematic overreporting or underreporting of certain outcomes. Second, while regression analyses were adjusted for glaucoma severity using ICD-9 and ICD-10 coding by physicians, due to underutilization of severity codes, glaucoma severity may have been unclassified for some individuals. If, for example, Black patients tended to have more severe glaucoma which was not documented as such, we may have underestimated the magnitude of eye care disparities faced by Black patients. Third, enrollment-based indicators of low income are only proxies for assessing SES and are not precise enough to detect all variation in socioeconomic status, especially among beneficiaries in the non-low-SES group who do not meet criteria for dual Medicaid/Medicare coverage, limited income subsidies, or state buy-in. One particular drawback of using Medicaid/Medicare dual coverage is that eligibility for Medicaid varies by state, resulting in an SES indicator that is not uniform across all beneficiaries15. Furthermore, we were unable to measure other socioeconomic variables such as neighborhood, education and occupation.
In conclusion, in a representative sample of Medicare beneficiaries with glaucoma, we detected significant racial disparities in eye care utilization. Black and Hispanic beneficiaries were less likely than Whites to have outpatient follow-up and glaucoma testing but more likely to undergo procedural intervention for glaucoma. Disparities between Black and White beneficiaries persisted after stratifying by SES group suggesting systemic racism may be an independent driver of differences seen in this population, whereas disparities between Hispanic and Asian vs White beneficiaries in our sample were largely explained by SES.
Supplementary Material
Racial disparities in eye care utilization among glaucoma patients exist among Hispanic and Black/African American Medicare beneficiaries. Disparities remained significant among Black/African Americans after controlling for socioeconomic status.
Financial support:
National Institutes of Health/National Eye Institute, Bethesda, MD (K23 EY032634-01); National Institutes of Health/National Eye Institute, Bethesda, MD (1R21EY032953).The sponsor or funding organization had no role in the design or conduct of this research.
Footnotes
Conflict of interest: No conflicting relationship exists for any author
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Tielsch JMSA, Katz J, Royall RM, Quigley HA, Javitt J. Racial variations in the prevalenc eof primary open-angle glaucoma . The Baltimore Eye Survey. . JAMA. 1991;266(3):369–374. [PubMed] [Google Scholar]
- 2.Varma RY-LM, Francis BA, et al. Prevalence of open-angle glaucoma and ocular hypertension in Latinos: the Los Angeles Latino Eye Study. Ophthalmology. 2004;111(8):1439–1448. [DOI] [PubMed] [Google Scholar]
- 3.Prager AJLJ, Cioffi GA, Blumberg DM. Self-reported Function, Health Resource Use, and Total Health Care Costs Among Medicare Beneficiaries With Glaucoma. . JAMA Ophthalmol. 2016;134(4):357–365. [DOI] [PubMed] [Google Scholar]
- 4.Bramley TPP, Walt J, Juhasz M, Hansen JE. . Self-reported Function, Health Resource Use, and Total Health Care Costs Among Medicare Beneficiaries with Glaucoma. JAMA Ophthalmol. 2016;134(4):357–365. [DOI] [PubMed] [Google Scholar]
- 5.Chen JV-BA, Mortensen K., et al. Racial and ethnic disparities in health care access and utilization under the affordable care act. Medical Care. 2016;54(2):140–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Javitt JMM, Nicholson GA., et al. Racial and ethnic disparities in health care access and utilization under the affordable care act. Undertreatment of glaucoma among Black AMericans. NEJM. 1991;325(20):1418–1422. [DOI] [PubMed] [Google Scholar]
- 7.Wang FJJ, Tielsch JM. Racial variation in treatment for glaucoma and cataract among Medicare recipients. Ophthalmic Epidemiology. 1997;4(2):253–256. [DOI] [PubMed] [Google Scholar]
- 8.Glynn RJGJ, Bohn RL, et al. . Old age and race as determinants of initiation of glaucoma therapy. Am J Epidemiol. 1993:395–406. [DOI] [PubMed] [Google Scholar]
- 9.Devgan UYF, Kim E, Coleman AL. Surgical undertreatment of glaucoma in black beneficiaries of medicare. Arch Ophthalmol. 2000;118(2):253–256. [DOI] [PubMed] [Google Scholar]
- 10.Wu J, Yu X, Ping X, et al. Socioeconomic disparities in the global burden of glaucoma: an analysis of trends from 1990 to 2016. Graefes Arch Clin Exp Ophthalmol. 2020;258(3):587–594. [DOI] [PubMed] [Google Scholar]
- 11.Elam ARAC, Musch DC, Lee PP, Stein JD. Large disparities in receipt of glaucoma care between enrolees in Medicaid and those with commercial health insurance Ophthalmology. 2017;124(10):1442–1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang X, Cotch MF, Ryskulova A, et al. Vision health disparities in the United States by race/ethnicity, education, and economic status: findings from two nationally representative surveys. Am J Ophthalmol. 2012;154(6 Suppl):S53–62 e51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams JP Dr. Social sources of racial disparities in health. Health Aff (Millwood). 2005;24(2):325–334. [DOI] [PubMed] [Google Scholar]
- 14.Jarrin OFNA, Grafova IB, Dong XQ, Lin H. Validity of race and ethnicity codes in Medicare administrative data compared to gold-standard self-reported race collected during routin home health care visits. Med Care. 2020;58(1):e1–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Samson LW, Finegold K, Ahmed A, et al. . Examining Measures of Income and Poverty in Medicare Administrative Data. Applied Methods. 2017;55:e158–e163. [DOI] [PubMed] [Google Scholar]
- 16.Kim DHGR, Avorn J, et al. . Validaiton of a Claims-Based Frailty Index Against Physical Performance and Adverse Health Outcomes in the Health and Retirement Study. J Gerontol A Biol Sci Med Sci. 2019;74(8):1271–1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ostermann JSF, Herndon, Lee PP. Racial Differences in Glaucoma Care. Arch Ophthalmol. 2005;123:1693–1698. [DOI] [PubMed] [Google Scholar]
- 18.Health Care. In: Bulatao RAAN, ed. Understanding Racial and Ethnic Differences in Health in Late Life: A Research Agenda. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- 19.Wang FJJ, Tielsch JM. Racial variations in treatment for glaucoma and cataract among Medicare recipients. Ophthalmic Epidemiology. 1997;4(2):89–100. [DOI] [PubMed] [Google Scholar]
- 20.Nordstrom BLFD, Mozaffari E, Quigley HA, Walker AM. Persistence and Adherence with Topical Glaucoma Therapy. Am J Ophthalmol. 2005;140(4):598–606. [DOI] [PubMed] [Google Scholar]
- 21.Boland MVCD, Frazier T, Plyler R, Friedman DS. Electronic monitoring to assess adherence with once-daily glaucoma medications and risk factors for nonadherence: the automated dosing reminder study. JAMA Ophthalmol. 2014;132(7):838–844. [DOI] [PubMed] [Google Scholar]
- 22.Rees GCX, Cheung CY, Aunt T, Friedman DS, Crowston JG, Lamoureux EL. Beliefs and adherence to glaucoma treatment: a comparison of patients form diverse cultures. J Glaucoma. 2014;23(5):293–298. [DOI] [PubMed] [Google Scholar]
- 23.Dreer LEGC, Campbell L, Wood A, Gao L, Owsley C. Glaucoma medication adherence among African Americans: program development. Optom Vis Sci. 2013;90(8):883–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.LKaK JD. Patient and provider assessments of adherence and the sources of disparities: evidence from diabetes care. Health Services Research. 2005;40:1803–1817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.van Ryn MBD, Malat J, Griffin J. Physicians’ perceptions of patients’ social and behavioral characteristics and race disparities in treatment recommendations for men with coronary artery disease. . Am J Public Health. 2006;96(2):351–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Friedman JKD, Schenberk T, et al. Assessment of Racial/Ethnic an dIncome Disparities in the Prescription of Opioids and Other Controlled Medications in California. JAMA Intern Med. 2019;179(4):469–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Assari S CC, Bazargan M. Association between parental educational attainment and youth outcomes and role of race/ethnicity. JAMA Netw Open. 2019;2(11):e1916018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.S A. Health disparities due to diminished return among black Americans: public policy solutions. Soc Issues Policy Rev. 2018;12(1):112–145. [Google Scholar]
- 29.S. A. Unequal gain of equal resources across racial groups. Int J Health Policy Manag. 2018;7(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Viruell-Fuentes EA MP, Abdulrahim S. More than culture: Structural racism, intersectionality theory and immigrant health. Soc Sci & Med. 2012;75(12):2099–2106. [DOI] [PubMed] [Google Scholar]
- 31.Scott AWEA, Nwanyanwu K. Addressing disparities in eye care—the time is now. JAMA Ophthalmol. 2021;Published online August 5, 2021. [DOI] [PubMed] [Google Scholar]
- 32.Dankwa-Mullan IRK, Williams K, et al. The science of eliminating health disparities: summary and analysis of the NIH summit recommendations. Am J Public Health. 2010;100(1):S12–S18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.EL Y NIH summit: the science of eliminating health disparities. J Child Adolesc Psychiatr Nurs. 2009;22(2):109–110. [DOI] [PubMed] [Google Scholar]
- 34.Apter AJCA. Eliminating health disparities: what have we done and what do we do next? J Allergy Clin Iommunol. 2009;123(6):1237–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.B B. Estimates of the unauthorized immigrant population residing in the United States: January 2015-January 2018. Department of Homeland Security;2021. [Google Scholar]
- 36.JT k. Retrictions on undocumented immigrants’ access to health services: the public health implications of welfare reform. American journal of public health. 2003;93(10):1630–1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nandi AGS, Lopez G, et al. . Access to and use of health services among undocumented Mexican immigrants in a US urban area. American journal of public health. 2008;98(11):2011–2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fernandez ARR. Undocumented immigrants and access to health care. JAMA Intern Med. 2017;177(4):536–537. [DOI] [PubMed] [Google Scholar]
- 39.Marx JLTA, Grayson G, Lowry LP, et al. The effects of California Proposition 187 on ophthalmology clnic utilization at an inner-city urban hospital. Ophthalmology 1996;103(5):847–851. [DOI] [PubMed] [Google Scholar]
- 40.Saffra NAET, Jacob CE, et al. Cost-effective treatment of ocular surface squamous neoplasia for an undocumented and uninsured New York City patient: a case report. J Med Case Rep. 2020;14(1):174. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.