Abstract
Introduction:
Substance use disorders (SUDs) remain challenging maladies to treat in the United States and impose significant societal costs. Despite these challenges, a significant number of individuals endorse being in recovery from SUD. The scientific understanding of SUD recovery has evolved to include not only improvements in substance use but also improvements in personal wellness and psychosocial functioning. The devaluation of future rewards (delay discounting; DD) is broadly associated with SUD inception and outcomes. We sought to investigate the relationship between DD, time in recovery, and recovery progress.
Methods:
We conducted an online assessment of 127 individuals in recovery from SUD who the study recruited via the International Quit and Recovery Registry (IQRR). The research team obtained measures of recovery progress via the Addiction Recovery Questionnaire (ARQ) and the Treatment Effectiveness Assessment (TEA). Additionally, the study collected measures of DD, time in recovery, and endorsement of abstinence in recovery (i.e., requiring abstinence vs. not). We utilized linear regression to test for associations among these variables and performed a mediation analysis to test the role of DD in mediating the relationship between time in recovery and measures of recovery progress.
Results:
Time in recovery was positively associated with the ARQ (p<.001) and TEA (p<.001). Furthermore, an individual’s delay discounting rate mediated the relationship between time in recovery and ARQ/TEA. Of the participants, 66% endorsed recovery requiring total abstinence from alcohol and drugs. Last, through an exhaustive model selection, the study did not find an individual’s endorsement of abstinence in recovery to be a primary predictor of recovery progress.
Conclusions:
This study presents evidence that, for individuals in recovery, the temporal view (i.e., focus on immediate vs. future rewards) is a significant influence on recovery progress. Additionally, an individual’s endorsement of abstinence in recovery was not significantly associated with recovery progress, suggesting the importance of a holistic view of SUD recovery. These findings contribute to the understanding of recovery as a multidimensional process and provide further support for DD as a behavioral marker of addiction.
Keywords: Substance use disorder, Recovery, Delay discounting, Treatment, Recovery progress
1. Introduction
Substance use disorders (SUDs) continue to pose significant challenges to public health in the United States. SUDs’ direct and indirect costs to the U.S. economy are staggering, estimated at more than $740 billion per year when accounting for crime, lost work productivity, and health care (NIDA, 2017). The costs of grief for individuals and families are difficult to calculate, with deaths from tobacco, alcohol, and opioids approaching 650,000 per year (Griswold et al., 2018; Hall & Doran, 2016; Hedegaard et al., 2017). Despite these grim figures, recovery from addiction is possible. Millions of individuals report being in recovery for extended periods (Substance Abuse and Mental Health Services Administration (US) & Office of the Surgeon General (US), 2016), many without formal treatment. Even with treatment, results from previous studies suggest relapse prevalence rates between 40% and 90% for individuals in recovery from SUD (Alan Marlatt & Donovan, 2005; Alterman et al., 2000; Gossop et al., 2002; Hunt et al., 1971; Lowman et al., 1996; Maisto et al., 2006).
As a multidimensional process, recovery from substance misuse involves not only abstinence but also improvement in physical and mental health, social relationships, wellness, and quality of life (Betty Ford Institute Consensus Panel, 2007; Kelly & Hoeppner, 2015; Laudet, 2007; Pettersen et al., 2018; White, 2007). In fact, recent findings have shown that abstinence may not be necessary for successful recovery (Rosenburg et al., 2020, Witkiewitz & Tucker, 2020). Furthermore, with multiple profiles and pathways, recovery is a process of growth that extends along a continuum (Elms et al., 2018; Witkiewitz et al., 2019). Hence, understanding an individual’s progress, needs, status, and view on abstinence in recovery is essential to better identify those at higher risk of relapse and provide person-centered treatment for addiction.
Consistent with the interest in and research on the multiple pathways in recovery (Corrigan et al., 2004; Gagne et al., 2007; O’Connell et al., 2005; Piat et al., 2009), researchers developed patient-centered and recovery-oriented instruments that measure progress in recovery, such as the Addiction Recovery Questionnaire (ARQ; Iveson-Brown & Raistrick, 2016) and the Treatment Effectiveness Assessment (TEA; Ling et al., 2012). The ARQ, a measure of recovery indicators that are quite generic and suitable for routine practice, is helpful in navigating the treatment journey and assessing personal progress in recovery during the past month. The ARQ provides a framework for long-term goals, focusing on three subscales: Abstinence (e.g., disengagement from drinking and drug taking cultures), Normality (e.g., adopting a lifestyle that is incompatible with substance misuse), and Positivity (e.g., change in thinking and in responding to circumstances) (Iveson-Brown & Raistrick, 2016). The TEA assesses progress in recovery from substance use and acquires information from individuals about changes that are especially significant to them, such as employment, living situations, and social relationships, and is suitable for assessing progress at short- or long-term intervals. In addition, the TEA examines one’s personal evaluation on substance use, personal health, lifestyle, and responsibility to the community (Ling et al., 2012, 2020).
To understand human behavior and its association with substance misuse, the field of behavioral economics incorporated insights from psychology and economics to study the decision-making process among individuals with SUD (Bickel et al., 2014; Bickel et al., 2016; Vuchinich & Heather, 2003). Delay discounting (DD), one of the most studied decision processes within behavioral economics, refers to the rate at which the subjective value of a reward declines as a function of the delay to its receipt (Bickel et al., 2014). Previous studies have suggested DD as a candidate behavioral marker of SUD (Bickel et al., 2014; Bickel et al., 2019). Furthermore, DD is associated with the status of substance use, with nonusers discounting delayed rewards less often than current users (Amlung et al., 2017; Bickel et al., 2014; Bickel et al., 2019; MacKillop et al., 2011; Mitchell et al., 2005). This finding is consistent among most substances, including opiates (Madden et al., 1999), cocaine (Coffey et al., 2003), nicotine (Baker et al., 2003), and alcohol (Mitchell et al., 2005). In addition, DD predicts initiation of substance use (Audrain-McGovern et al., 2009), the severity of use (Albein-Urios et al., 2012; Johnson et al., 2007; Vuchinich & Simpson, 1998), and post-treatment outcomes (Athamneh et al., 2020; Bickel et al., 2017; De Wilde et al., 2013; Domínguez-Salas et al., 2016; Krishnan-Sarin et al., 2007; MacKillop & Kahler, 2009; Sheffer et al., 2012; Sheffer et al., 2014; Stanger et al., 2012; Stevens et al., 2014, 2015; Washio et al., 2011; Yoon et al., 2007). Moreover, previous studies have reported significant negative associations between time in recovery and DD, with those self-reporting longer time in recovery showing lower discounting rates (Athamneh et al., 2019; Tomlinson et al., 2020).
Recovery outcomes and treatment success are associated with time in recovery (Foster et al., 2000a; Jin et al., 1998; Laudet, 2011; Rather & Sherman, 1989), progress in recovery (Foster et al., 2000b; Kraemer et al., 2002; Moos & Moos, 2006; Villeneuve et al., 2006), and DD (Athamneh et al., 2020; Bickel et al., 2017; De Wilde et al., 2013; Domínguez-Salas et al., 2016; Krishnan-Sarin et al., 2007; MacKillop & Kahler, 2009; Sheffer et al., 2012, 2014; Stanger et al., 2012; Stevens et al., 2014, 2015; Washio et al., 2011; Yoon et al., 2007). However, to our knowledge, studies have not examined the association between time in recovery and progress in recovery and how it may be affected by DD rates among individuals in recovery from SUD.
The current study examined the association between time in recovery (self-report), progress in recovery (as measured by ARQ and TEA scales), and rates of DD in a sample of individuals in recovery from SUD. The study collected data from the International Quit & Recovery Registry (IQRR), an ongoing online registry that aims to understand recovery and its phenotypes (Athamneh et al., 2019, 2020; Tomlinson et al., 2020). In addition, given that participants may define recovery differently (e.g., recovery being inclusive of continued substance use), the current study investigated the association between an individual's endorsement of abstinence in recovery (i.e., recovery requiring total abstinence vs. not) and progress in recovery. As progress in recovery is positively associated with treatment success, we hypothesized that one’s time in recovery would be positively associated with both ARQ and TEA scores. Additionally, we hypothesized that one’s DD rate would be inversely associated with both ARQ and TEA scores (i.e., lower DD, higher scores). Moreover, given that time in recovery is associated with lower rates of DD, which may then lead to improvement and progress in recovery, we hypothesized that rates of DD may mediate the association between time in recovery and ARQ/TEA scores.
2. Materials and methods
2.1. Participants
The study recruited participants (n=131) from the International Quit and Recovery Registry (IQRR; www.quitandrecovery.org), an online recovery community and registry created in 2011 with more than 5,000 registrants. The IQRR is discoverable through search engines or social media and is available to all adults who self-report being in recovery from substance use and seek to facilitate a deeper understanding of factors that support successful recovery from addiction. Interested individuals can become members, known as “Recovery Heroes”, by registering on the website, which includes providing demographic and contact information, as well as a personal history of substance use. After registration, members gain access to the IQRR’s social media platform where they can seek or provide support to other members and are encouraged to complete any available research assessments in which they are interested. Note that while the precise demographics of individuals in recovery from SUD are unknown, the overall demographics of the IQRR, as well as this sample, are similar to prior reports of individuals in recovery from SUD (Kaskutas et al., 2014).
Participation in this study was voluntary and consent was implied through the completion and submission of the survey. The Institutional Review Board at Virginia Polytechnic and State University approved this study. Inclusion criteria for this study required that participants be 18 years or older and self-report recovery from one or more SUDs. The study excluded from analysis individuals reporting a non-substance use addiction (e.g., gambling, overeating, excessive shopping; n = 4). The final sample included 127 participants.
2.2. Study measures
The study collected demographic characteristics including age, gender, race, ethnicity, education level, and annual income. The research team determined a participant’s primary addiction with the question “What is/was your primary addiction?” with the following response options: nicotine, alcohol, cannabis, opioids, cocaine, stimulants, prescription pain relievers, hallucinogens, dissociative anesthetics, tranquilizers/depressants, inhalants, caffeine, gambling, overeating, binge eating or other eating disorder, excessive shopping, excessive sexual activity, excessive video gaming, excessive viewing of pornography, and excessive preoccupation with activities on the internet. Additionally, the study asked participants, “How long have you been in recovery from your primary addiction?” and then they endorsed the number of days, months, and years they had been in recovery. The study converted days and months to years to compute the total number of years in recovery. The study asked participants for their endorsement of abstinence from substance use in the context of addiction recovery, specifically, we asked participants, “In your opinion, does recovery require total abstinence from all drugs and alcohol?” with the response options “Yes” and “No” (The study refers to this question as “abstinence endorsement” in analyses).
2.2.1. Delay Discounting.
The study measured delay discounting using an adjusting delay task (Koffarnus & Bickel, 2014). In this five-trial task, participants chose between a smaller, immediately available reward ($500), and a larger reward available after a delay ($1,000). Across each trial, the monetary amounts remain constant while the delay changed. This task identifies the delay at which the larger reward loses half its subjective value and efficiently estimates the discounting rate, k. All discounting rates were natural-log transformed to normalize the data and stabilize the variance.
2.2.2. Addiction Recovery Questionnaire (ARQ).
The ARQ is a 12-item measure developed and validated by Iveson-Brown and Raistrick (2016). The ARQ measures progress in recovery across three components: Normality (e.g., “had enough money to live reasonably well?”), Abstinence (e.g., been mixing with people who are problem drinkers/drug users?), and Positivity (e.g., felt generally good about yourself?). All Items were scored on a 0–3 scale (0 = “not at all”, 1 = “rarely”, 2 = “often”, 3 = “all the time”), except for 3 items that we reverse scored. The study summed the score of all items to yield a total score.
2.2.3. Treatment Effectiveness Assessment (TEA).
The 4-item TEA, developed and validated by Ling and colleagues (2012), is a brief, patient-centered instrument used to measure progress in treatment and recovery. The TEA asks patients to indicate improvements in four areas relevant to recovery; (1) substance use (the frequency and amount of use; money spent on drugs and alcohol; amount of drug craving; time spent being high/drunk, being sick, in trouble, and in other drug-using activities, etc); (2) health (physical and mental health, eating and sleeping, exercising, taking care of health problems or dental problems, etc.); (3) lifestyle (living conditions, family situation, employment, relationships, paying bills, and following through with personal or professional commitments); and (4) community (obeying laws and meeting your responsibilities to society). The study asked participants to assign a value between 1 (“none or not much better”) and 10 (“very much better”) for the four recovery-oriented domains. We obtained a total score by summing the responses for the four domains, which ranged from 4 (no measurable improvement) to 40 (significantly improved).
2.3. Statistical analysis
The study summarized sample characteristics using means (standard deviations) and frequencies (percentages). In addition, the study stratified these characteristics based on abstinence endorsement and compared them using a t-test or chi-squared test as appropriate. We conducted separate univariate linear regressions with progress in recovery variables (i.e., ARQ and TEA scores) as the outcome measure with each of the other recovery-related variable (i.e., DD, years in recovery, abstinence endorsement) and demographic characteristics (i.e., age, gender, race ethnicity, education, annual income) as the explanatory variable. To further assess the association among these variables, the team performed multivariate regression with model selection. A comprehensive and exhaustive search of the model space explored all combinations of DD, years in recovery, abstinence endorsement, and demographics, as independent variables and ARQ and TEA scores as dependent variables. The team selected the model with the lowest Bayesian Information Criterion (BIC) as the optimal model. The study team performed a post hoc power analysis using the smallest effect size observed from the univariate analysis (f2=0.15), alpha of 0.05, our sample of 127 participants achieved 99% power. The study team analyzed all data in R version 3.5.3 (R Core Team, 2019) with a significance level of 0.05.
2.3.1. Mediation Analysis.
The research team performed mediation analyses using Hayes’ method (Hayes, 2017). In this study, we performed mediation analyses to test the mediating effect of delay discounting rate (M) on the relationship between time in recovery (X) and ARQ/TEA scores (Y). The study used a bootstrapping approach to estimate the indirect effect of DD using 10,000 bootstrap random samples to determine the 95% confidence intervals (CI). A 95% CI for the indirect effect coefficient provides evidence for a significant mediating effect if the CI does not include zero. The study reported all results as standardized estimates.
3. Results
We show means (SD) and frequencies (%) of demographic variables for the total sample in Table 1; and we present frequencies for substance use, discounting rates, and ARQ/TEA scores in Table 2. Briefly, participants were 46.8 years old on average, 59.8% female, 88.3% White, and 92.1% non-Hispanic. Participants reported being in recovery from substance use for 10.48 years on average (range: .003–45.6 years) and 44.9% reported that alcohol was their primary addiction. A majority of participants (66%) endorsed recovery requiring total abstinence from alcohol and drugs. When examining sample characteristics stratified by abstinence endorsement, the study observed several significant differences (Table S1; see supplement). Individuals who endorsed recovery requiring total abstinence were significantly older (p=.005), reported greater time in recovery (p<.001), had lower rates of delay discounting (p=.007), and higher ARQ (p<.001) and TEA (p=.009) scores. Note of those participants who reported prior treatment (n=104), a significant association existed with recovery requiring abstinence and participating in a 12-step treatment program (OR: 8.75, 95% CI: 3.05-31.85).
Table 1.
Sample Demographics (N = 127).
| Demographics | Frequency (%) / Mean (SD) |
|---|---|
| Ageb | 46.8 (16.7) |
| Gendera | |
| Female | 76 (59.8) |
| Male | 51 (40.2) |
| Racea | |
| Asian | 4 (3.1) |
| Black or African American | 7 (5.5) |
| White | 112 (88.3) |
| Other | 4 (3.1) |
| Ethnicitya | |
| Hispanic | 10 (7.9) |
| Non-Hispanic | 117 (92.1) |
| Education levela | |
| High school diploma/GED or less | 23 (18.1) |
| Some college with no degree | 37 (29.1) |
| Completed a 2-year college degree or higher | 67 (52.8) |
| Incomea | |
| Less than $9,999 | 27 (21.3) |
| $10,000-$29,999 | 30 (23.6) |
| $30,000-$49,999 | 19 (15.0) |
| $50,000-$79,999 | 19 (15.0) |
| $80,000+ | 27 (21.2) |
| Refuse to answer | 5 (3.9) |
Frequency (%)
Mean (SD)
Table 2.
Recovery Characteristics
| Characteristics | Frequency (%) / Mean (SD) |
|---|---|
| Primary Addictiona | |
| Alcohol | 57 (44.9) |
| Opioids | 25 (19.7) |
| Other | 45 (35.4) |
| Time in recovery – yearsb | 10.48 (11.86) |
| Delay discounting rate – In(k)b | −4.90 (2.36) |
| ARQ Scoreb | 27.08 (6.24) |
| TEA Scoreb | 31.86 (7.08) |
| Does Recovery Require Total Abstinence?a | |
| Yes | 84 (66.1) |
| No | 43 (33.9) |
Frequency (%)
Mean (SD)
To understand the relationship between ARQ/TEA scores and other recovery-related variables (e.g., discounting rate, years in recovery, abstinence endorsement) and demographic characteristics, the research team performed univariate linear regression (Table 3). For ARQ score, the study identified time in recovery (F(1,125)=60.14;p<.001), discounting rate (F(1,125)=46.73; p<.001), abstinence endorsement (F(1,125)=13.43; p<.001), age (F(1,125)=72.09; p <.001), education (F(4,122)=8.236; p<.001), and income (F(22,104)=3.197; p<.001) as significant predictors, but not gender (F(1,126)=0.442; p=.508), race (F(5,122)=1.182; p =.322), or ethnicity (F(1,126)=0.032; p=.859). For TEA score, the study identified time in recovery (F(1,125) = 42.78; p<.001), discounting rate (F(1,125)=18.38; p<.001), abstinence endorsement (F(1,125)=7.517; p=.007), age (F(1,125)=26.86; p<.001), and education (F(4,122)=2.835; p=.027) as significant predictors, but not gender (F(1,125)=0.075; p=.784), race (F(5,121)=2.119; p=.067), ethnicity (F(1,125)=0.594; p=.442), or income (F(22,104) = 1.511; p=.086).
Table 3.
Univariate linear regression associations of ARQ/TEA scores and recovery variables.
| Variable | ARQ Score | P-value | TEA Score | P-Value |
|---|---|---|---|---|
| Time in recovery | F(1,125) = 60.14 | <.001 | F(1,125) = 42.78 | <.001 |
| Discounting rate | F(1,125) = 46.73 | <.001 | F(1,125) = 18.38 | <.001 |
| Abstinence group | F(1,125) = 13.43 | <.001 | F(1,125) = 7.517 | .007 |
| Age | F(1,125) = 72.09 | <.001 | F(1,125) = 26.86 | <.001 |
| Gender | F(1,125) = 0.524 | .470 | F(1,125) = 0.075 | .784 |
| Race | F(5,121) = 1.195 | .316 | F(5,121) = 2.119 | .067 |
| Ethnicity | F(1,125) = 0.039 | .842 | F(1,125) = 0.594 | .442 |
| Education | F(4,122) = 8.236 | <.001 | F(4,122) = 2.835 | .027 |
| Income | F(22,104) = 3.197 | <.001 | F(22,104) = 1.511 | .086 |
The study team performed multivariate regression with model selection to further understand the relationship between ARQ/TEA scores, discounting rate, years in recovery, abstinence endorsement, and demographic variables (Table 4). For ARQ, the final model with lowest BIC included age (p<.001), discounting rate (p<.001), and years in recovery (p=.002) as significant predictors. For TEA, the final model with lowest BIC included discounting rate (p=.023) and years in recovery (p<.001). Of note, abstinence endorsement did not persist as a significant predictor for ARQ score or TEA score. Within both of these models, years in recovery and discounting rate were significantly associated with one another (p<.001)
Table 4.
Linear regression associations of ARQ/TEA scores and recovery characteristics after model selection.
| ARQ Scores | TEA Scores | |||
|---|---|---|---|---|
| Adjusted coef. (95% CI)a | p-value | Adjusted coef. (95% CI) a | p-value | |
| Time in recovery | 0.7275 (0.2743 1.1805) | .002 | 1.3657 (0.8480 1.8833) | <.001 |
| Discounting rate | −0.7450 (−1.1206 −0.3701) | <.001 | −0.5673 (−1.0562 −0.0785) | .023 |
| Age | 0.1234 (0.0621 0.1846) | <.001 | ---- | --- |
Note: CI = confidence interval
Model selection was performed to investigate the inclusion of age, gender, years of education, race, ethnicity, and income. Note after model selection, only time in recovery, discounting rate, and age remained in the model for ARQ score, and only time in recovery and discounting remained in the model for TEA score.
To understand the relationship between time in recovery, ARQ/TEA scores, and discounting rate, we performed mediation analyses. Mediation analyses indicated that DD mediated the relationship between years in recovery and ARQ score (β = 0.138; 95% CI = 0.049 - 0.247; Figure 1), accounting for 24%, of the observed effect. In addition, DD mediated the relationship between years in recovery and TEA score (β = 0.075; 95% CI = 0.008 - 0.164 ; Figure 1), accounting for 15% of the observed effect.
Figure 1.
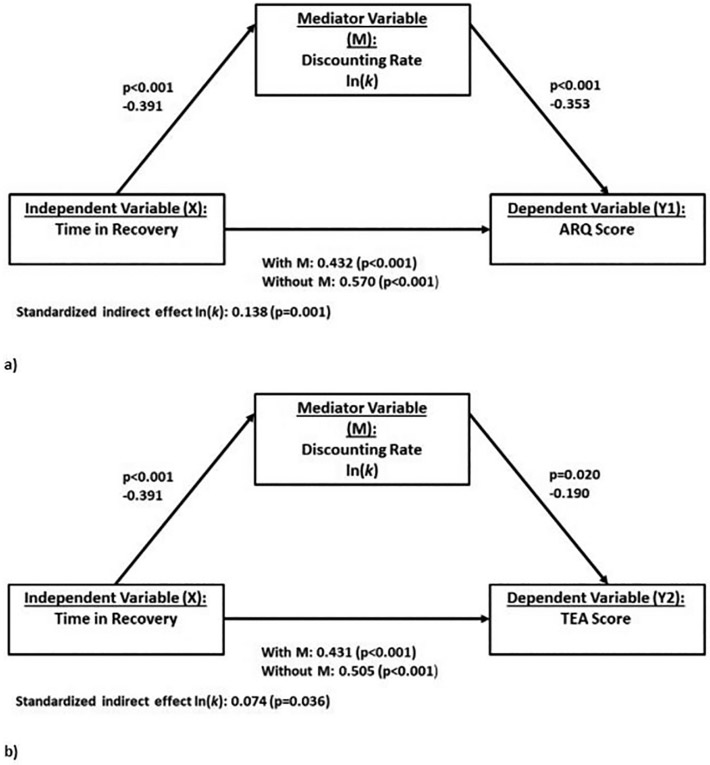
Mediation analyses for the relationship between time in recovery and recovery progress scores as mediated by delay discounting rate (ln(k)). Panel (a) depicts mediation analysis with ARQ score as the dependent variable (Y1). Panel (b) depicts mediation analysis with TEA score as the dependent variable (Y2). Standardized β estimates of the linear regression between each set of variables are depicted along the arrows. Note panels (a) and (b) represent two separate mediation analyses, not one analysis with multiple mediators.
4. Discussion
The current study investigated associations among time in recovery, recovery progress, and delay discounting, in a sample of individuals in recovery from SUD from the International Quit and Recovery Registry (IQRR). Additionally, we investigated if an individual’s endorsement of abstinence in recovery (i.e., recovery requiring total abstinence from drugs/alcohol or not) was associated with progress in recovery. Our results indicated a significant association between DD, age, time in recovery, and ARQ score. In addition, our results indicated a significant association between DD, time in recovery, and TEA score. Moreover, DD mediated the relationship between time in recovery and ARQ/TEA scores. Notably, while the study observed group differences in ARQ/TEA scores as a function of abstinence endorsement at the univariate level, these differences did not persist at the multivariate level and were better accounted for by discounting rate, time in recovery, and age. Next we discuss these results in further detail.
In accordance with our hypothesis, DD rate (ln(k)) had a mediating role in the relationship time in recovery and past 30-day recovery outcomes, as measured by the ARQ, with significant indirect effects that accounted for 24% of the total effect. As previously mentioned, the ARQ recognizes the gradual and multifaceted nature of the recovery process by including three different domains: Abstinence, Normality and Positivity. Although only few published studies have used the ARQ, many studies in the recovery field have investigated similar domains (Johannessen et al., 2019; Kelly et al., 2018; Martinelli et al., 2020; Muller et al., 2017). ARQ’s abstinence subscale assesses disengagement from drug culture, including not only abstinence from use but also stepping-stones to recovery, such as the use of substitute prescriptions and the existence of a positive social network. ARQ’s normality subscale assesses quality of life indicators of the recovery process that are likely incompatible with substance misuse, such as financial, social and living conditions, daily and criminal activities. ARQ’s positivity subscale assesses psychological constructs that indicate the state of changed responses to situations, such as optimism, self-esteem and confidence. Importantly, the ARQ is the result of multiple iterations with service users, concerned others and health professionals, such as addiction specialists, generic health professionals and commissioners, suggesting strong community support for its items (Iveson-Brown & Raistrick, 2016).
The results of the mediation analysis are consistent with previous findings assessing the three relationships involved. First, studies have shown significant positive associations between recovery length and specific aspects of recovery progress, as measured by the ARQ subscales, such as abstinence from drug use (Jin et al., 1998; Rather & Sherman, 1989; Subbaraman & Witbrodt, 2014), normality indicators, such as quality of life (Hibbert & Best, 2011; John F. Kelly et al., 2018), housing and criminal activities (Martinelli et al., 2020), and positivity indicators, such as self-esteem (Hibbert & Best, 2011). Second, as mentioned, previous literature has demonstrated a negative association between recovery length and DD rates. Third, other studies have indicated a negative association between DD rates and constructs related to ARQ subscale components among individuals in recovery from substance use, such as physical health, psychological health, social relationships and environment (Lemos, et al., 2020; Bickel et al., 2017; De Wilde et al., 2013; Domínguez-Salas et al., 2016; Krishnan-Sarin et al., 2007; MacKillop & Kahler, 2009; Sheffer et al., 2012, 2014; Stanger et al., 2012; Stevens et al., 2014, 2015; Washio et al., 2011; Yoon et al., 2007), and abstinence self-efficacy (i.e., confidence to resist substance use) (Athamneh et al., 2019).
In accordance with our second hypothesis, the mediation analyses we presented here explored the relationship between DD rate on time in recovery and the TEA scores (Figure 1). As mentioned previously, the TEA assesses longer-term recovery progress across four domains (substance use, health, lifestyle, and community). An individual’s DD rate (ln(k)) had a mediating role between time in recovery and the TEA score with significant indirect effects that accounted for 15% of the total effect. These results are consistent with existing literature indicating significant associations between positive recovery progress (i.e., improvement in recovery outcomes) and DD rates (Athamneh et al., 2020; Sheffer et al., 2012, 2014). These results were consistent with our hypothesis that length of time in recovery was positively associated with TEA scores and consistent with previous findings of significant associations between length of time in recovery and delay discounting rates (Athamneh et al., 2019; Tomlinson et al., 2020). Moreover, this is the first study to report a significant relationship between delay discounting and the TEA. Consistent with our hypothesis, we report a significant negative association between DD rate and TEA scores. Results of the exhaustive model selection indicated that TEA scores were best predicted by discounting rate and time in recovery, which provides evidence that time in recovery and DD rate both contribute to longer-term recovery progress.
Overall, the results of these mediation analyses support DD as a potential intervention to improve the recovery process. Previous studies have shown that interventions can change discounting rates in individuals with substance use disorders. For example, Episodic Future Thinking, an intervention that consists of engaging participants in vivid simulation of realistic future events (Atance & O’Neill, 2001), has significantly decreased DD in smokers (Athamneh et al., 2020; Stein et al., 2016, 2018) and alcohol users (Mellis et al., 2019). Moreover, in an alcohol use disorder cohort, EFT interventions reduced both discounting and demand intensity for alcohol (Snider et al., 2016). In this sense, changing one’s valuation of the future may help to positively augment the recovery process. In addition, higher DD rates were associated with lower recovery progress in this study. Perhaps by identifying and targeting individuals with higher DD rates in recovery with unique and additional resources would aid in their recovery progress. We note that variables outside this study could also serve as intervention targets. The current study is clinically relevant and provides evidence for effective interventions that modify patients’ future valuation into treatment approaches.
Finally, we investigated whether a participant’s endorsement of abstinence in recovery (i.e., whether recovery requires total abstinence from alcohol and drugs) was associated with self-reported progress in recovery (as measured by ARQ/TEA). At the univariate level, several characteristics were significantly different between those endorsing recovery requiring total abstinence versus not. Participants endorsing abstinence had significantly higher ARQ/TEA scores, were older, reported being in recovery longer, and had lower DD rates compared to those endorsing nonabstinent recovery. However, after performing a multivariate regression with model selection, group differences in ARQ/TEA scores were best accounted for by age, time in recovery, and DD rate. In addition and interestingly, 53% of the participants who did not indicate participation in a 12-step treatment program felt recovery required abstinence compared to 91% of those who participated in a 12-step treatment program. In total, our results are consistent with other studies that have reported that younger age (Dawson et al., 2007; Sobell et al., 1996; Subbaraman & Witbrodt, 2014) and shorter length of time in recovery (Subbaraman & Witbrodt, 2014) are associated with nonabstinent recovery.
We acknowledge several potential limitations in this study. First, the majority of the sample (88.3%) was White, and therefore the results may not generalize to other populations. Second, the observational nature of the study potentially limits the ability to understand the temporal relationship between outcome variables; future longitudinal studies will be helpful to better understand these relationships. Moreover, we acknowledge that differences exist in the time frames that several measures assessed (i.e., ARQ/TEA assess retrospectively, DD assesses momentarily), but the study collected all of these measures in the same session and they likely reflect present circumstances. Third, while this study investigated the relationships among time in recovery, recovery progress, and DD, the study did not collect several variables that could influence these outcomes. Variables such as perceived stress, psychiatric comorbidities, and social support could affect these measures and future studies in this line of research would benefit from their inclusion. Additionally, given that the study did not define recovery for participants, the endorsement of abstinence likely depended on an individual’s personal definition and therefore we may not be measuring the same construct in all participants. Last, while the IQRR is a powerful tool to investigate the phenotype of recovery, our participant pool is limited to individuals with access to an Internet connection and those who self-select to join the IQRR, potentially introducing bias into our sample.
5. Conclusion
This study examined associations between time in recovery from a substance use disorder, measures of progress in recovery, and DD in a sample of individuals in recovery from SUDs. We report that time in recovery was positively associated with scores on measures of short-term and long-term recovery progress. Furthermore this relationship was mediated by an individual’s DD rate, whereby individuals with lower discounting rates reported greater progress in recovery from SUD. Additionally, we investigated if an individual’s endorsement of abstinence in recovery (i.e., recovery requiring total abstinence or not) was associated with recovery progress. We report that an individual’s endorsement of abstinence in recovery was not the best predictor of progress in recovery, which was best accounted for by time in recovery, age, and DD rate. These findings contribute to the understanding of recovery as a multidimensional process and provide further support for DD as a behavioral marker of addiction.
Supplementary Material
Highlights.
Recovery from substances use disorders (SUD) is a multidimensional process
Delay discounting (DD) is broadly associated with SUD outcomes
DD mediates relationship between time in recovery and recovery progress
Funding Information
This work was supported by the Fralin Biomedical Research Institute at Virginia Tech Carilion and in part by NIH/NIAAA R01AA027381.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
Although the following activities/relationships do not create a conflict of interest pertaining to this manuscript, in the interest of full disclosure, Dr. Bickel would like to report the following: W. K. Bickel is a principal of HealthSim, LLC; BEAM Diagnostics, Inc.; and Red 5 Group, LLC. In addition, he serves on the scientific advisory board for Sober Grid, Inc.; and Ria Health; serves as a consultant for Boehringer Ingelheim International; and works on a project supported by Indivior, Inc. None of the other authors report any potential conflicts of interest.
References
- Alan Marlatt G, & Donovan DM (2005). Relapse Prevention: Maintenance Strategies in the Treatment of Addictive Behaviors. Guilford Press. [Google Scholar]
- Albein-Urios N, Martinez-González JM, Lozano O, Clark L, & Verdejo-García A (2012). Comparison of impulsivity and working memory in cocaine addiction and pathological gambling: Implications for cocaine-induced neurotoxicity. Drug and Alcohol Dependence, 126(1-2), 1–6. [DOI] [PubMed] [Google Scholar]
- Alterman AI, McKay JR, Mulvaney FD, Cnaan A, Cacciola JS, Tourian KA, Rutherford MJ, & Merikle EP (2000). Baseline prediction of 7-month cocaine abstinence for cocaine dependence patients. Drug and Alcohol Dependence, 59(3), 215–221. [DOI] [PubMed] [Google Scholar]
- Amlung M, Vedelago L, Acker J, Balodis I, & MacKillop J (2017). Steep delay discounting and addictive behavior: a meta-analysis of continuous associations: Delay discounting and addiction. Addiction, 112(1), 51–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atance CM, & O’Neill DK (2001). Episodic future thinking. Trends in Cognitive Sciences, 5(12), 533–539. [DOI] [PubMed] [Google Scholar]
- Athamneh LN, DeHart WB, Pope D, Mellis AM, Snider SE, Kaplan BA, & Bickel WK (2019). The phenotype of recovery III: Delay discounting predicts abstinence self-efficacy among individuals in recovery from substance use disorders. Psychology of Addictive Behaviors: Journal of the Society of Psychologists in Addictive Behaviors, 33(3), 310–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Athamneh LN, Lemos RF, Basso JC, Tomlinson DC, Craft WH, Stein MD, & Bickel WK (2020). The phenotype of recovery II: The association between delay discounting, self-reported quality of life, and remission status among individuals in recovery from substance use disorders. In Experimental and Clinical Psychopharmacology, 10.1037/pha0000389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Athamneh LN, Stein MD, Lin EH, Stein JS, Mellis AM, Gatchalian KM, Epstein LH, & Bickel WK (2020). Setting a goal could help you control: Comparing the effect of health goal versus general episodic future thinking on health behaviors among cigarette smokers and obese individuals. Experimental and Clinical Psychopharmacology. 10.1037/pha0000351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Audrain-McGovern J, Rodriguez D, Epstein LH, Cuevas J, Rodgers K, & Wileyto EP (2009). Does delay discounting play an etiological role in smoking or is it a consequence of smoking? Drug and Alcohol Dependence, 103(3), 99–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker F, Johnson MW, & Bickel WK (2003). Delay discounting in current and never-before cigarette smokers: similarities and differences across commodity, sign, and magnitude. Journal of Abnormal Psychology. https://psycnet.apa.org/journals/abn/112/3/382.html?uid=2003-05990-007 [DOI] [PubMed] [Google Scholar]
- Betty Ford Institute Consensus Panel. (2007). What is recovery? A working definition from the Betty Ford Institute. Journal of Substance Abuse Treatment, 33(3), 221–228. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Athamneh LN, Basso JC, Mellis AM, DeHart WB, Craft WH, & Pope D (2019). Excessive discounting of delayed reinforcers as a trans-disease process: Update on the state of the science. Current Opinion in Psychology, 30, 59–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Johnson MW, Koffarnus MN, MacKillop J, & Murphy JG (2014). The behavioral economics of substance use disorders: reinforcement pathologies and their repair. Annual Review of Clinical Psychology, 10, 641–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Koffarnus MN, Moody L, & Wilson AG (2014). The behavioral- and neuro-economic process of temporal discounting: A candidate behavioral marker of addiction. Neuropharmacology, 76 Pt B, 518–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Moody L, & Higgins ST (2016). Some current dimensions of the behavioral economics of health-related behavior change. Preventive Medicine, 92, 16–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Moody LN, Eddy CR, & Franck CT (2017). Neurocognitive dysfunction in addiction: Testing hypotheses of diffuse versus selective phenotypic dysfunction with a classification-based approach. Experimental and Clinical Psychopharmacology, 25(4), 322–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffey SF, Gudleski GD, Saladin ME, & Brady KT (2003). Impulsivity and rapid discounting of delayed hypothetical rewards in cocaine-dependent individuals. Experimental and Clinical Psychopharmacology, 11(1), 18–25. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Salzer M, Ralph RO, Sangster Y, & Keck L (2004). Examining the factor structure of the recovery assessment scale. Schizophrenia Bulletin, 30(4), 1035–1041. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, & Grant BF (2007). Rates and correlates of relapse among individuals in remission from DSM-IV alcohol dependence: a 3-year follow-up. Alcoholism, Clinical and Experimental Research, 31(12), 2036–2045. [DOI] [PubMed] [Google Scholar]
- De Wilde B, Verdejo-García A, Sabbe B, Hulstijn W, & Dom G (2013). Affective decision-making is predictive of three-month relapse in polysubstance-dependent alcoholics. European Addiction Research, 19(1), 21–28. [DOI] [PubMed] [Google Scholar]
- Dominguez-Salas S, Díaz-Batanero C, Lozano-Rojas OM, & Verdejo-García A (2016). Impact of general cognition and executive function deficits on addiction treatment outcomes: Systematic review and discussion of neurocognitive pathways. Neuroscience and Biobehavioral Reviews, 71, 772–801. [DOI] [PubMed] [Google Scholar]
- Elms E, Savic M, Bathish R, Best D, Manning V, & Lubman DI (2018). Multiple Pathways to Recovery, Multiple Roads to Well-Being: An Analysis of Recovery Pathways in the Australian Life in Recovery Survey. Alcoholism Treatment Quarterly, 36(4), 482–498. [Google Scholar]
- Foster JH, Peters TJ, & Marshall EJ (2000a). Quality of life measures and outcome in alcohol-dependent men and women. Alcohol, 22(1), 45–52. [DOI] [PubMed] [Google Scholar]
- Foster JH, Peters TJ, & Marshall EJ (2000b). Quality of life measures and outcome in alcohol-dependent men and women. Alcohol, 22(1), 45–52. [DOI] [PubMed] [Google Scholar]
- Gagne C, White W, & Anthony WA (2007). Recovery: a common vision for the fields of mental health and addictions. Psychiatric Rehabilitation Journal, 31(1), 32–37. [DOI] [PubMed] [Google Scholar]
- Gossop M, Stewart D, Browne N, & Marsden J (2002). Factors associated with abstinence, lapse or relapse to heroin use after residential treatment: protective effect of coping responses. Addiction , 97(10), 1259–1267. [DOI] [PubMed] [Google Scholar]
- Griswold MG, Fullman N, Hawley C, Arian N, Zimsen SRM, Tymeson HD, Venkateswaran V, Tapp AD, Forouzanfar MH, Salama JS, Abate KH, Abate D, Abay SM, Abbafati C, Abdulkader RS, Abebe Z, Aboyans V, Abrar MM, Acharya P, … Gakidou E (2018). Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet, 392(10152), 1015–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall W, & Doran C (2016). How Much Can the USA Reduce Health Care Costs by Reducing Smoking? [Review of How Much Can the USA Reduce Health Care Costs by Reducing Smoking?]. PLoS Medicine, 13(5), e1002021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2017). Introduction to Mediation, Moderation, and Conditional Process Analysis, Second Edition: A Regression-Based Approach. Guilford Publications. [Google Scholar]
- Hedegaard H, Warner M, & Miniño AM (2017). Drug overdose deaths in the United States, 1999--2015. https://stacks.cdc.gov/view/cdc/44356 [PubMed] [Google Scholar]
- Hibbert LJ, & Best DW (2011). Assessing recovery and functioning in former problem drinkers at different stages of their recovery journeys. Drug and Alcohol Review, 30(1), 12–20. [DOI] [PubMed] [Google Scholar]
- Hunt WA, Walker Barnett L, & Branch LG (1971). Relapse rates in addiction programs. Journal of Clinical Psychology, 27(4), 455–456. [DOI] [PubMed] [Google Scholar]
- Iveson-Brown K, & Raistrick D (2016). A brief Addiction Recovery Questionnaire derived from the views of service users and concerned others. Drugs: Education, Prevention and Policy, 23(1), 41–47. [Google Scholar]
- Jin H, Rourke SB, Patterson TL, Taylor MJ, & Grant I (1998). Predictors of relapse in long-term abstinent alcoholics. Journal of Studies on Alcohol, 59(6), 640–646. [DOI] [PubMed] [Google Scholar]
- Johannessen DA, Nordfjærn T, & Geirdal AØ (2019). Change in psychosocial factors connected to coping after inpatient treatment for substance use disorder: a systematic review. Substance Abuse Treatment, Prevention, and Policy, 14(1), 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Bickel WK, & Baker F (2007). Moderate drug use and delay discounting: a comparison of heavy, light, and never smokers. Experimental and Clinical Psychopharmacology, 15(2), 187–194. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Greene MC, & Bergman BG (2018). Beyond Abstinence: Changes in Indices of Quality of Life with Time in Recovery in a Nationally Representative Sample of U.S. Adults. Alcoholism, Clinical and Experimental Research, 42(4), 770–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, & Hoeppner B (2015). A biaxial formulation of the recovery construct. Addiction Research & Theory, 23(1), 5–9. [Google Scholar]
- Koffarnus MN, & Bickel WK (2014). A 5-trial adjusting delay discounting task: accurate discount rates in less than one minute. Experimental and Clinical Psychopharmacology, 22(3), 222–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer KL, Maisto SA, Conigliaro J, McNeil M, Gordon AJ, & Kelley ME (2002). Decreased alcohol consumption in outpatient drinkers is associated with improved quality of life and fewer alcohol-related consequences. In Journal of General Internal Medicine (Vol. 17, Issue 5, pp. 382–386). 10.1007/s11606-002-0045-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnan-Sarin S, Reynolds B, Duhig AM, Smith A, Liss T, McFetridge A, Cavallo DA, Carroll KM, & Potenza MN (2007). Behavioral impulsivity predicts treatment outcome in a smoking cessation program for adolescent smokers. Drug and Alcohol Dependence, 88(1), 79–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet AB (2007). What does recovery mean to you? Lessons from the recovery experience for research and practice. Journal of Substance Abuse Treatment, 33(3), 243–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet AB (2011). The case for considering quality of life in addiction research and clinical practice. Addiction Science & Clinical Practice, 6(1), 44–55. [PMC free article] [PubMed] [Google Scholar]
- Ling W, Farabee D, Liepa D, & Wu L-T (2012). The Treatment Effectiveness Assessment (TEA): an efficient, patient-centered instrument for evaluating progress in recovery from addiction. Substance Abuse and Rehabilitation, 3(1), 129–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ling W, Farabee D, Nadipelli VR, & Perrochet B (2020). An Updated Version of the Treatment Effectiveness Assessment (TEA). Substance Abuse and Rehabilitation, 11, 21–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowman C, Allen J, Stout RL, & The Relapse Research Group. (1996). Replication and extension of Marlatt’s taxonomy of relapse precipitants: overview of procedures and results. Addiction , 91(12), 51–72. [PubMed] [Google Scholar]
- MacKillop J, Amlung MT, Few LR, Ray LA, Sweet LH, & Munafò MR (2011). Delayed reward discounting and addictive behavior: a meta-analysis. Psychopharmacology, 216(3), 305–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, & Kahler CW (2009). Delayed reward discounting predicts treatment response for heavy drinkers receiving smoking cessation treatment. Drug and Alcohol Dependence, 104(3), 197–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madden GJ, Bickel WK, & Jacobs EA (1999). Discounting of delayed rewards in opioid-dependent outpatients: exponential or hyperbolic discounting functions? Experimental and Clinical Psychopharmacology, 7(3), 284–293. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Clifford PR, Stout RL, & Davis CM (2006). Drinking in the year after treatment as a predictor of three-year drinking outcomes. Journal of Studies on Alcohol, 67(6), 823–832. [DOI] [PubMed] [Google Scholar]
- Martinelli TF, Nagelhout GE, Bellaert L, Best D, Vanderplasschen W, & van de Mheen D (2020). Comparing three stages of addiction recovery: long-term recovery and its relation to housing problems, crime, occupation situation, and substance use. Drugs: Education, Prevention and Policy, 27(5), 387–396. [Google Scholar]
- Mellis AM, Snider SE, Deshpande HU, LaConte SM, & Bickel WK (2019). Practicing prospection promotes patience: Repeated episodic future thinking cumulatively reduces delay discounting. Drug and Alcohol Dependence, 204, 107507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell JM, Fields HL, D’Esposito M, & Boettiger CA (2005). Impulsive responding in alcoholics. Alcoholism, Clinical and Experimental Research, 29(12), 2158–2169. [DOI] [PubMed] [Google Scholar]
- Moos RH, & Moos BS (2006). Rates and predictors of relapse after natural and treated remission from alcohol use disorders. Addiction , 101(2), 212–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller AE, Skurtveit S, & Clausen T (2017). Building abstinent networks is an important resource in improving quality of life. Drug and Alcohol Dependence, 180, 431–438. [DOI] [PubMed] [Google Scholar]
- National Institute of Drug Abuse (NIDA). (2017). Trends & Statistics. NIDA. https://www.drugabuse.gov/related-topics/trends-statistics [Google Scholar]
- O’Connell M, Tondora J, Croog G, Evans A, & Davidson L (2005). From rhetoric to routine: assessing perceptions of recovery-oriented practices in a state mental health and addiction system. Psychiatric Rehabilitation Journal, 28(4), 378–386. [DOI] [PubMed] [Google Scholar]
- Pettersen H, Landheim A, Skeie I, Biong S, Brodahl M, Benson V, & Davidson L (2018). Why Do Those With Long-Term Substance Use Disorders Stop Abusing Substances? A Qualitative Study. Substance Abuse: Research and Treatment, 12, 1178221817752678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piat M, Sabetti J, Couture A, Sylvestre J, Provencher H, Botschner J, & Stayner D (2009). What does recovery mean for me? Perspectives of Canadian mental health consumers. Psychiatric Rehabilitation Journal, 32(3), 199–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rather BC, & Sherman MF (1989). Relationship between alcohol expectancies and length of abstinence among Alcoholics Anonymous members. Addictive Behaviors, 14(5), 531–536. [DOI] [PubMed] [Google Scholar]
- R Core Team. (2020). R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. https://www.R-project.org/ [Google Scholar]
- Rosenberg H, Grant J, & Davis AK (2020). Acceptance of Non-Abstinence as an Outcome Goal for Individuals Diagnosed With Substance Use Disorders: A Narrative Review of Published Research. Journal of Studies on Alcohol and Drugs, 81(4), 405–415. [PubMed] [Google Scholar]
- Sheffer CE, Christensen DR, Landes R, Carter LP, Jackson L, & Bickel WK (2014). Delay discounting rates: A strong prognostic indicator of smoking relapse. Addictive Behaviors, 39(11) 1682–1689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheffer C, MacKillop J, McGeary J, Landes R, Carter L, Yi R, Jones B, Christensen D, Stitzer M, Jackson L, & Bickel W (2012). Delay Discounting, Locus of Control, and Cognitive Impulsiveness Independently Predict Tobacco Dependence Treatment Outcomes in a Highly Dependent, Lower Socioeconomic Group of Smokers. The American Journal on Addictions / American Academy of Psychiatrists in Alcoholism and Addictions, 21(3), 221–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snider SE, LaConte SM, & Bickel WK (2016). Episodic Future Thinking: Expansion of the Temporal Window in Individuals with Alcohol Dependence. Alcoholism, Clinical and Experimental Research, 40(7), 1558–1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Cunningham JA, & Sobell MB (1996). Recovery from alcohol problems with and without treatment: prevalence in two population surveys. American Journal of Public Health, 86(7), 966–972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanger C, Ryan SR, Fu H, Landes RD, Jones BA, Bickel WK, & Budney AJ (2012). Delay discounting predicts adolescent substance abuse treatment outcome. Experimental and Clinical Psychopharmacology, 20(3), 205–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein JS, Tegge AN, Turner JK, & Bickel WK (2018). Episodic future thinking reduces delay discounting and cigarette demand: an investigation of the good-subject effect. Journal of Behavioral Medicine, 41(2), 269–276. [DOI] [PubMed] [Google Scholar]
- Stein JS, Wilson AG, Koffarnus MN, Daniel TO, Epstein LH, & Bickel WK (2016). Unstuck in time: episodic future thinking reduces delay discounting and cigarette smoking. Psychopharmacology, 233(21-22), 3771–3778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens L, Goudriaan AE, Verdejo-Garcia A, Dom G, Roeyers H, & Vanderplasschen W (2015). Impulsive choice predicts short-term relapse in substance-dependent individuals attending an in-patient detoxification programme. Psychological Medicine, 45(10), 2083–2093. [DOI] [PubMed] [Google Scholar]
- Stevens L, Verdejo-García A, Goudriaan AE, Roeyers H, Dom G, & Vanderplasschen W (2014). Impulsivity as a vulnerability factor for poor addiction treatment outcomes: a review of neurocognitive findings among individuals with substance use disorders. Journal of Substance Abuse Treatment, 47(1), 58–72. [DOI] [PubMed] [Google Scholar]
- Subbaraman MS, & Witbrodt J (2014). Differences between abstinent and non-abstinent individuals in recovery from alcohol use disorders. Addictive Behaviors, 39(12), 1730–1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (US), & Office of the Surgeon General (US). (2016). Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health. US Department of Health and Human Services. [PubMed] [Google Scholar]
- Tomlinson DC, Tegge AN, Athamneh LN, & Bickel WK (2020). The phenotype of recovery IV: Delay discounting predicts perceived stress and a chance locus of control in individuals in recovery from substance use disorders. Addictive Behaviors Reports, 12, 100320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villeneuve PJ, Challacombe L, Strike CJ, Myers T, Fischer B, Shore R, Hopkins S, & Millson PE (2006). Change in health-related quality of life of opiate users in low-threshold methadone programs. In Journal of Substance Use (Vol. 11, Issue 2, pp. 137–149). 10.1080/14659890500256945 [DOI] [PubMed] [Google Scholar]
- Vuchinich RE, & Heather N (2003). Choice, Behavioral Economics, and Addiction. Elsevier. [Google Scholar]
- Vuchinich RE, & Simpson CA (1998). Hyperbolic temporal discounting in social drinkers and problem drinkers. Experimental and Clinical Psychopharmacology, 6(3), 292–305. [DOI] [PubMed] [Google Scholar]
- Washio Y, Higgins ST, Heil SH, McKerchar TL, Badger GJ, Skelly JM, & Dantona RL (2011). Delay discounting is associated with treatment response among cocaine-dependent outpatients. Experimental and Clinical Psychopharmacology, 19(3), 243–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White WL (2007). Addiction recovery: its definition and conceptual boundaries. Journal of Substance Abuse Treatment, 33(3), 229–241. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, & Tucker JA (2020). Abstinence Not Required: Expanding the Definition of Recovery from Alcohol Use Disorder. Alcoholism, Clinical and Experimental Research, 44(1), 36–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Wilson AD, Pearson MR, Montes KS, Kirouac M, Roos CR, Hallgren KA, & Maisto SA (2019). Profiles of recovery from alcohol use disorder at three years following treatment: can the definition of recovery be extended to include high functioning heavy drinkers? In Addiction (Vol. 114, Issue 1, pp. 69–80). 10.1111/add.14403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon JH, Higgins ST, Heil SH, Sugarbaker RJ, Thomas CS, & Badger GJ (2007). Delay discounting predicts postpartum relapse to cigarette smoking among pregnant women. Experimental and Clinical Psychopharmacology, 15(2), 176–186. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


