Abstract
Purpose:
The objectives of the current study were to (1) assess associations between household structure (i.e., living with spouse compared to living alone, with children, or with a spouse and children), presence of children, and mental distress in April 2020 and change in mental distress (between April and August 2020); and (2) determine whether these associations are moderated by income or sex.
Participants:
A total of 2,214 adults aged 25–55 from the April and August 2020 waves of the Understanding America study were included in the analytic sample.
Study Method:
Multivariable, survey-weighted linear regression models were used to examine associations between explanatory variables (i.e., household structure and number of children) and outcome variables (mental distress in April and change in mental distress), measured via the Patient Health Questionnaire (PHQ)-4.
Results:
In adjusted models, each additional child under the age of 12 was associated with lower mental distress in April 2020 (β = −.30, p = .002). Having children aged 13 to 18 and household structure were not significantly associated with mental distress. In interaction models, living with children only was associated with decreased mental distress among individuals reporting low income (interaction β = −1.28, p = .016) but not high income. Similarly, living with children only was associated with decreased mental distress in females (interaction β = −1.09, p = .025) but not males.
Conclusion:
This study supports prior literature that demonstrates the positive association of child rearing with psychological well-being and suggests that these benefits may be present even under stay-at-home orders in the early stages of the U.S. COVID-19 pandemic.
Keywords: mental distress, COVID-19, family structure, parenting paradox
The emergence of COVID-19 in the United States has created unprecedented challenges that have rendered many individuals financially unstable (Goodell, 2020) and emotionally vulnerable (Li et al., 2020). The well-being of families may be particularly at risk as a result of changes in relationships and routines during COVID-19, which may disproportionately affect children’s coping abilities and parental burden (Prime et al., 2020; Russell et al., 2020). Although evidence suggests that there has been a rise in mental distress throughout the pandemic (Kirzinger et al., 2020), there is scarce research on the association between household structure and mental distress. Understanding these associations is key to informing public health response and long-term consequences of particular living situations.
Polls conducted in March 2020 highlighted the distressing nature of the pandemic (Holingue et al., 2020). Data from the Kaiser Family Foundation poll in April 2020 found that nearly half of adults in the U.S. were experiencing negative mental health effects from worry and stress over the virus (Kirzinger et al., 2020; McGinty et al., 2020). The COVID-19 pandemic has increased the amount of time that many adults are spending at home, which could have varying implications for mental health depending on household structure. People living alone may be particularly at risk for experiencing loneliness during the COVID-19 pandemic (McGinty et al., 2020). Among young (ages 16–34) and middle-aged (ages 35–59) adults, living alone has been associated with an increased risk for common mental disorders (Jacob et al., 2019), including a nearly two-fold increase in anxiety and depressive disorders, compared to those who are married or cohabiting (Joutsenniemi et al., 2006).Families with children may also be disproportionately affected as nearly every daycare and school across the U.S. closed at the beginning of the pandemic. Classes shifted to virtual learning models, affecting over 55 million students in kindergarten through 12th grade (Golberstein et al., 2020). In addition to everyday parenting, many parents quickly assumed the role of primary educator while potentially balancing competing demands from employment. The experience of COVID-19 related stressors, coupled with symptoms of anxiety and depression, has been linked to higher parental perceived stress (Brown et al., 2020; Spinelli et al.,2020).
Notably, however, having children in the home can be associated with both positive and negative mental outcomes. This phenomenon is known as the parenting paradox (Rizzo et al., 2013): Although childcare is demanding and time-consuming, parents tend to value their time with children as it promotes familial connectedness and has high intrinsic value for the parent (Bianchi et al., 2006). The latter is particularly true of interactive childcare, such as playing with a child, as opposed to routine care such as feeding or bathing a child (Offer, 2014). Previous research highlights that the type of interaction may be highly gendered (McDonnell et al., 2019) and may have discrete implications for well-being by the sex of the parent. For example, routine childcare is more stressful and less engaging for mothers than it is for fathers (Offer, 2014), and these associations may further depend on the age of the child (Roeters & Gracia, 2016).Thus, studies investigating associations between caregiving for children during the COVID-19 pandemic and mental distress should account for sex of the parent and child age.
The stresses of child rearing are likely amplified among single parents, partially due to lower levels of financial and emotional support (Sobolewski & King, 2005). These lower levels of support may result in poorer mental health for single parents compared to parents who are married or cohabiting (Crosier et al., 2007). These challenges may be particularly relevant during the COVID-19 pandemic, as single parents may be unable to rely on supportive family and friends throughout shelter-in-place orders.
Finally, income inequalities have repeatedly been linked to psychological outcomes (Patel et al., 2018; Pickett et al., 2006). These inequalities are likely to be widened during the COVID-19 pandemic as a result of job loss (U.S. Department of Labor, 2020). Indeed, data from April 2020 suggest that individuals belonging to a low-income household (less than $40,000 per year) have disproportionately experienced negative impacts to their mental health during the COVID-19 pandemic compared to those who make $40,000 or more (Kirzinger et al.,2020).
As the world enters a new phase with COVID-19, many novel stressors are emerging. Families are faced with particular challenges of additional child rearing and educational duties, and people who live alone may experience distress due to isolation. The added responsibilities of childcare may be particularly distressing for women, who have historically provided the bulk of care. Furthermore, households with low economic resources may experience high levels of stress, and the financial effects may compound stress differently based on household structure. To our knowledge, however, only one study has examined mental distress and household structure during the pandemic, finding that there was no relationship between household structure and mental distress or well-being (Veldhuis et al., 2021). Our study builds on these findings by considering age of children and potential moderation by income and sex. Exploring this topic has the potential to identify groups who are at greatest risk for mental distress.
The objectives of this study are to (1) assess associations between household structure (i.e., living with spouse compared to living alone, with children, or with a spouse and children), presence of children, and mental distress in April 2020 and change in mental distress (between April and August 2020) during the COVID-19 pandemic; and (2) determine whether these associations are moderated by income or sex.
Methods
Study Sample
Data for this study come from the Understanding America study (UAS). UAS participants were selected using address based sampling, in which postal records are used to select a random sample from a listing of residential addresses (Lavrakas, 2008). Eligible individuals include adults 18 and older in the contacted households. The UAS panel consists of 10 nationally representative cohorts (the University of Southern California, 2020) enrolled in the sample between 2014 and 2020. The current analysis uses data from the UAS waves 235 (April 2020 Monthly Survey, administered April 1st through April 28th with a total of 5,478 respondents) and 256 (August 2020 Monthly Survey, administered August 5th through September 1st with a total of 6,238 respondents), which assess participant responses to the COVID-19 pandemic. Survey weights in the UAS align sample distributions of key demographic characteristics (e.g., sex, race/ethnicity) to their population counterparts based on the Basic Monthly Current Population Survey.
Measures
Mental Distress
The primary outcome measures stem from the 4-item version of the Patient Health Questionnaire (PHQ-4). This measure is a brief self-report questionnaire consisting of 2 items that assess depressive symptoms and 2 items that assess anxiety symptoms over a two-week period (Löwe et al., 2010). Response options include “not at all,” “several days,” “more than half the days,” and “nearly every day.” The total score is calculated by adding the scores of all 4 items; higher scores represent greater levels of mental distress (Kroenke et al., 2009). The PHQ-4 is valid and reliable (α = .78) for assessing depression and anxiety in the general population (Löwe et al., 2010). To calculate difference in mental distress over time, PHQ-4 scores in April 2020 (UAS 235) were subtracted from scores in August 2020 (UAS 256), creating a continuous change score (range: −12 to 12).
Historical Depressive Symptoms
In earlier (pre-April 2020) waves of data collections, participants completed the 8-item version of the Center for Epidemiologic Studies Depression Scale (CESD-8; Bracke et al., 2008; Radloff, 1977). Answers range from 0 (none or almost none of the time) to 3 (all or almost all the time). The number of symptoms (count: 0–8) a respondent previously endorsed as occurring “all or almost all the time” in the past 7 days was used as a historical measure of depressive symptoms. The CESD-8 scale shows high reliability (α = .90) and validity among middle-aged U.S. adults (Cosco et al., 2017). The most recent CESD-8 was used for participants with multiple CESD-8 measurements from prior waves (46% of the sample had a CESD-8 from June 2019; 36% from June 2017; and 18% from May 2015). Continuously measured prepandemic CESD-8 scores were included as a covariate in all models.
Household Variables
The primary exposure of interest was household structure, which was assessed using the respondent-reported relationships of household members. Household structure was assigned to the following categories: living alone; living with spouse only; living with children only; living with spouse and children only. All other combinations of household structure (32.5% of households), including extended family and nonfamily members, were not assessed due to the heterogeneity of this population. In addition, household structure was further characterized by identifying the number of children living in the household. Children were split into two age groups, and the total number of children in each age group per household were each used as a continuous measure: children aged 12 or below (range: 0–6) and children aged 13 to 18 (range:0–4).
Other Sociodemographic Items
Sociodemographic factors included the following: age (in years); sex (female or male); race/ethnicity (White, Black, African American, or Other [includes American Indian or Alaska Native, Asian, Native Hawaiian or Pacific Islander, and multiracial]); education (high school degree or below, attended some college or received a two-year degree, bachelor’s degree, or graduate degree); household income, measured as the total combined 12-month income of all members currently living the respondent’s household (less than 30k, 30–59k, 60k and above); and currently have a job (yes or no). A household income of $60,000 was selected as the cutoff for low versus high income as it roughly corresponds to the median income in the U.S. in 2018 (Guzman, 2019).
Statistical Analyses
Multivariable, survey-weighted linear regression was used to examine the associations of household characteristics (i.e., household structure and number of children) as explanatory variables and total PHQ-4 score in April 2020 and PHQ-4 score change from April to August 2020 as the outcomes. The analysis was restricted to individuals aged 25 to 55 and with complete information on all analytic variables (187 participants [~8%] excluded for incomplete data). Age restrictions were implemented to reduce confounding by age; age categories (by decade, beginning at age 25) were selected if greater than one third of the group had children in the home. We then estimated two additional models with an interaction term of each primary predictor (household structure and number of children) with sex and household income separately for both April 2020 mental distress and change in distress (eight models total).
Sensitivity analyses were included to allow for potentially different results based on distinct threshold (i.e., cutoff for low income) and similarities of living situation (i.e., living with spouse and living with significant other). All analyses used the UAS survey weights and adjusted complex survey design, allowing these results to generalize to the U.S. adult population. All analyses were performed in Stata 16 using the svy commands (Statacorp, 2017).
Results
Sample Description
A total of 2,214 adults ages 25–55 were included in this analysis. The majority of the participants were female (52%), White (75%), currently working (67%), and living with a partner (73%). Most had some postsecondary education (67%) and an annual income of greater than $60,000 (54%). CESD-8 total scores ranged from 0 to 8 with a mean of 1.9 (SE = .07). Over one third of participants endorsed no CESD-8 symptoms at their most recent measurement, and only 20% reported experiencing more than three of the symptoms. PHQ-4 total scores in April 2020 ranged from 0 to 12 with a mean of 2.9 (SE = .10). On average, participants showed less distress in August 2020 (change: −.86 [SE = .08]). The household structure analyses included a subgroup of this sample who fell into one of four household categories: living alone, living with spouse only, living with kids only, living with spouse and kids. Sample characteristics are presented in Table 1.
Table 1.
Participant Characteristics Among UAS Sample Ages 25–55
| Model | Number of children (n = 2,214) | Household structure (n = 1,495) |
|---|---|---|
| Sociodemographic characteristics—N (%) | ||
| Age | 40.1 (0.24) | 40.8 (0.28) |
| Sex | ||
| Female | 1,151 (52.0%) | 725 (48.5%) |
| Male | 1,063 (48.0%) | 770 (51.5%) |
| Race | ||
| White | 1,663 (75.1%) | 1,163 (77.8%) |
| Black | 265 (12.0%) | 159 (10.6%) |
| Other | 286 (12.9%) | 173 (11.6%) |
| Education level | ||
| High school or less | 741 (33.5%) | 450 (30.1%) |
| Some college or Associate’s degree | 559 (25.3%) | 344 (23.0%) |
| Bachelor’s degree | 507 (22.8%) | 374 (25.0%) |
| Graduate degree | 407 (18.4%) | 327 (21.9%) |
| Household income | ||
| Less than 30k | 499 (22.5%) | 295 (19.7%) |
| Less than 60k | 528 (23.9%) | 339 (22.7%) |
| 60k+ | 1,187 (53.6%) | 861 (57.6%) |
| Currently working | ||
| Yes | 1,471 (66.5%) | 1,055 (70.6%) |
| No | 743 (33.5%) | 440 (29.4%) |
| Living with a partner | ||
| Yes | 1,621 (73.2%) | 1,175 (78.6%) |
| No | 593 (26.8%) | 320 (21.4%) |
| Household characteristics | ||
| Household structure—N (%) | ||
| Alone | — | 276 (18.5%) |
| Living with spouse | — | 314 (20.9%) |
| Living with kids | — | 98 (6.6%) |
| Living with spouse and kids | — | 807 (54.0%) |
| Number of children—mean (SE) | ||
| Ages 0–12 | 0.65 (0.03) | — |
| Ages 12–18 | 0.27 (0.02) | — |
| Mental distress—mean (SE) | ||
| PHQ-4 score in April 2020 | 2.90 (0.10) | 2.79 (0.12) |
| Change in PHQ-4 score | −0.86 (0.08) | −0.77 (0.10) |
| Latest CES-D score | 1.89 (0.07) | 1.70 (0.08) |
Correlates of Mental Distress
Unadjusted Analyses
In unadjusted bivariate tests, household structure was not associated with mental distress (i.e., PHQ-4 total score) in April 2020 or change in mental distress between April 2020 and August 2020. Number of children aged 12 or below was associated with lower mental distress in April 2020 (β = −.25, 95% CI: −.43, −.08), but not change in mental distress. Number of children aged 13–18 showed no associations with mental distress in April or with the change over time.
Adjusted Analyses
In adjusted models, household structure was not associated with mental distress in April 2020 or change in mental distress. In models looking at number of children under 12, compared to households with no children, each additional child under the age 12 was associated with a decrease in mental distress in April 2020 (β = −.30, p = .002; Table 2, Figure 1). This finding was significant when adjusting sociodemographic variables (age, sex, race, education, household income, living with a partner, and currently having a job) and historical CESD-8 score. Having children between the ages of 13 and 18 and household structure were not significantly associated with mental distress in April 2020 or change in mental distress (both p > .05). The strength of association and significance of other variables varied across models (household structure and number of children), but generally, being Black/African American, compared to White, was associated with lower levels distress in April 2020, whereas currently not working and historical depressive symptoms were associated with higher levels of mental distress in April 2020 (both p < .05). In contrast, being Black/African American, compared to White, and having a graduate degree, relative to high school or less, was associated with a significant increase in mental distress (p < .005). Having an annual household income of $60,000 or above, relative to less than $30,000, was associated with a significant decrease in distress over time (p = .04). A summary of these results is available in Table 2.
Table 2.
Multivariable Linear Regression Models Estimating 1) PHQ-4 Total Score in April 2020 and 2) Change in PHQ-4 Score Between April and August 2020 by a) Household Structure and b) Number of Children in the Household, Stratified by Age of Children
| Outcome Primary predictor | Mental distress in April Household structure Number = 1,495 |
Change in mental distress Household structure Number = 1.495 |
Mental distress in April Number of children (by age) N = 2.214 |
Change in mental distress Number of children (by age) N= 2.214 |
||||
|---|---|---|---|---|---|---|---|---|
| β | [95% CI] | β | [95% CI] | β | [95% CI] | β | [95% CI] | |
| Household structure (ref: spouse only) | ||||||||
| Alone | −0.21 | [−0.97, 0.55] | −0.40 | [−1.03, 0.23] | — | — | — | — |
| Kids only | −0.14 | [−0.87, 0.59] | −0.71 | [−1.47, 0.05] | — | — | — | — |
| Spouse and kids | 0.04 | [−0.54, 0.62] | −0.12 | [−0.61, 0.37] | — | — | — | — |
| Number of children | ||||||||
| # children ≤12 | — | — | — | — | −0.30 | [−0.49–0.11]* | 0.09 | [−0.08, 0.27] |
| # children 13–18 | — | — | — | — | −0.02 | [−0.31, 0.26] | −0.02 | [−0.28, 0.24] |
| Age | −0.02 | [−0.04, 0.01] | 0.01 | [−0.01, 0.04] | −0.02 | [−0.05, 0.00] | 0.02 | [−0.00, 0.03] |
| Sex (ref: female) | ||||||||
| Male | −0.34 | [−0.78, 0.10] | −0.06 | [−0.45, 0.33] | −0.26 | [−0.63, 0.11] | −0.02 | [−0.36, 0.32] |
| Race (ref: White) | ||||||||
| Black | −1.34 | [−2.03–0.64]* | 1.06 | [0.38, 1.74]* | −1.19 | [−1.75–0.63]* | 0.81 | [0.25, 1.37]* |
| Other | −0.11 | [−0.79, 0.58] | 0.39 | [−0.32, 1.11] | −0.26 | [−0.77, 0.25] | 0.31 | [−0.21, 0.84] |
| Education (ref: high school or less) | ||||||||
| Some college/Associate’s | 0.05 | [−0.54, 0.63] | −0.01 | [−0.54, 0.52] | 0.14 | [−0.34, 0.61] | 0.15 | [−0.28, 0.57] |
| Bachelor’s | 0.53 | [−0.05, 1.12] | 0.14 | [−0.35, 0.64] | 0.49 | [−0.02, 1.00] | 0.33 | [−0.10, 0.77] |
| Graduate degree | 0.48 | [−0.21, 1.17] | 0.63 | [0.03, 1.22]* | 0.32 | [−0.28, 0.93] | 0.80 | [0.27, 1.33]* |
| Household Income (ref: <30k) | ||||||||
| 30 to less than 60k | −0.09 | [−0.79, 0.62] | −0.07 | [−0.80, 0.66] | −0.01 | [−0.63, 0.61] | −0.04 | [−0.62, 0.53] |
| 60k+ | −0.35 | [−1.12, 0.42] | −0.50 | [−1.23, 0.23] | 0.00 | [−0.60, 0.60] | −0.59 | [−1.15–0.03]* |
| Current job (ref: yes) | ||||||||
| No job | 0.61 | [0.04, 1.18]* | −0.27 | [−0.74, 0.21] | 0.81 | [0.35, 1.27]* | −0.25 | [−0.64, 0.14] |
| Live with partner (ref: no) | ||||||||
| Living with partner | — | — | — | — | 0.06 | [−0.40, 0.51] | 0.33 | [−0.11, 0.77] |
| Historical depression score (CESD-8) | 0.54 | [0.41, 0.67]* | 0.06 | [−0.03, 0.15] | 0.50 | [0.40, 0.60]* | 0.06 | [−0.03, 0.15] |
Note. Models are adjusted for age, sex, race, education, household income, current work status, living with a partner (number of children models only), and historical depressive symptoms.
Denotes significance at a p < .05 level.
Figure 1.
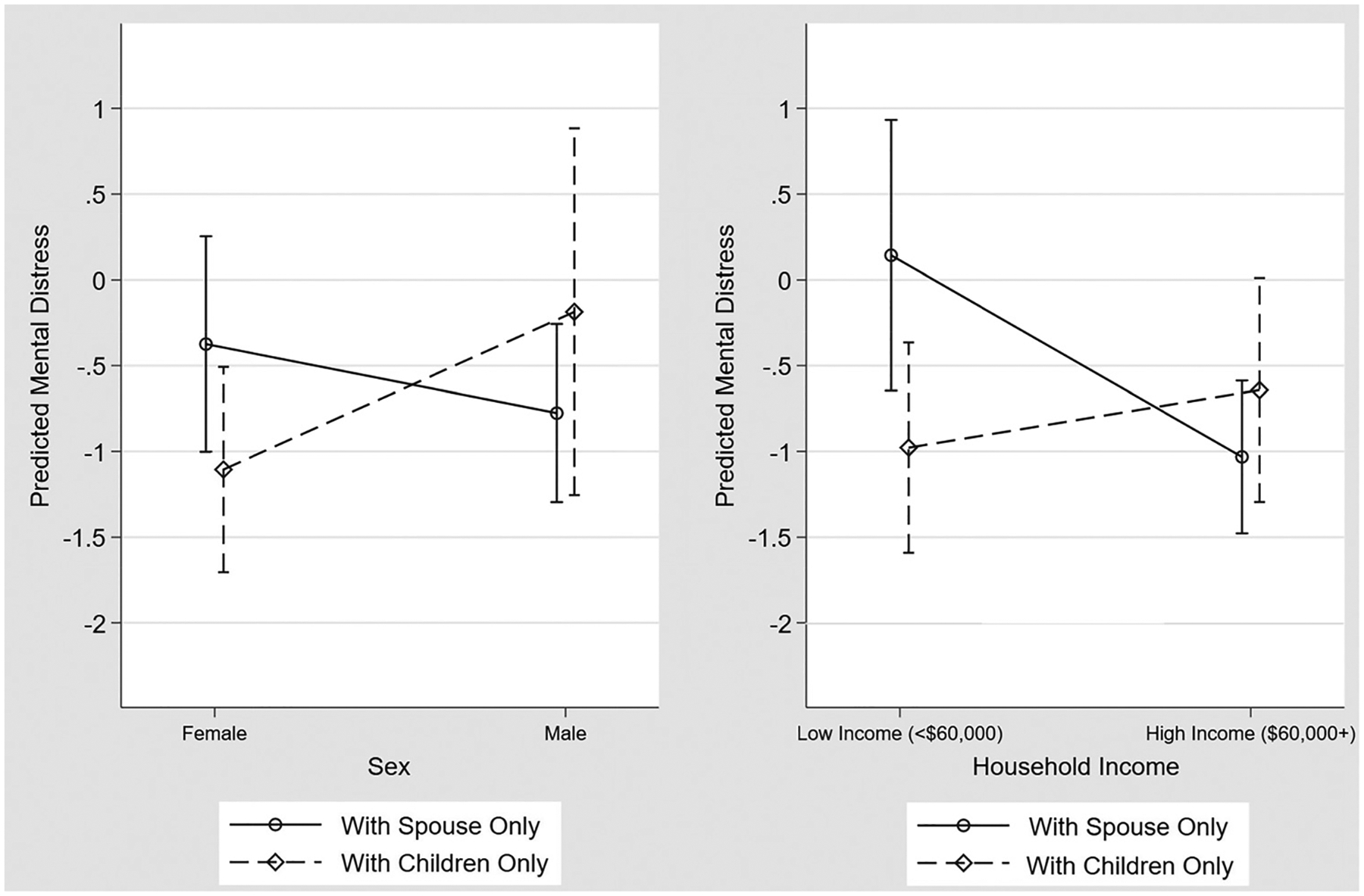
Predicted PHQ-4 Score and 95% Confidence Interval by Household Structure (Spouse Only [Ref] and Children Only), Stratified by Sex (Left) and Income (Right) and Adjusted for Age, Sex, Race, Education, Household Income, Current Work Status, Living With a Partner, and Historical Depressive Symptoms
Moderation Analyses
Additional models included interaction terms between the primary exposures (i.e., household structure and number of children) and sex and income to investigate differential effects among males/females and high/low-income groups. Living with children only, relative to living with spouse only in a low-income home, was associated with decreased mental distress among individuals reporting low income (interaction β = −1.28, p = .016) but not high income (association = −.94, p = .086). Similarly, living with children only, relative to living with a spouse only and being female, was associated with decreased stress among females (interaction β = −1.09, p = .025) but not males (association = −.18, p = .783). No other interaction terms were statistically significant. A summary of these results is available in Tables 3 and 4.
Table 3.
Multivariable Linear Regression Models With Interaction Terms Estimating 1) PHQ-4 Total Score in April 2020 and 2) Change in PHQ-4 Score Between April and August 2020 by a) Household Structure and b) Number of Children in the Household, Stratified by Age of Children, and Their Interaction With Income
| Outcome Primary predictor | Mental distress in April Household structure N= 1,495 |
Change in Mental Distress Household structure N = 1,495 |
Mental distress in April Number of Children (by age) N= 2,214 |
Change in Mental Distress Number of Children (by age) N = 2,214 |
||||
|---|---|---|---|---|---|---|---|---|
| β | [95% CI] | β | [95% CI] | β | [95% CI] | β | [95% CI] | |
| Household structure (ref: spouse only) | ||||||||
| Alone | −0.20 | [−1.42, 1.02] | −0.87 | [−1.88, 0.13] | — | — | — | — |
| Kids only | 0.00 | [−1.12, 1.11] | −1.28 | [−2.32–0.24]* | — | — | — | |
| Spouse and Kids | 0.04 | [−1.08, 1.15] | −0.73 | [−1.70, 0.23] | — | — | — | |
| Number of children | ||||||||
| # children ≤12 | — | — | — | — | −0.44 | [−0.73–0.15]* | 0.05 | [−0.24, 0.34] |
| # children 13–18 | — | — | — | — | 0.26 | [−0.23, 0.76] | −0.09 | [−0.50, 0.32] |
| Annual Household Income (ref: <60k) | ||||||||
| ≥$60,000 | −0.26 | [−1.48, 0.97] | −1.18 | [−2.10–0.25]* | −0.01 | [−0.56, 0.55] | −0.64 | [−1.12–0.16]* |
| Household structure by income interaction | ||||||||
| Alone & high income | 0.02 | [−1.48, 1.52] | 0.84 | [−0.38, 2.05] | — | — | — | — |
| Kids Only & high income | −0.72 | [−2.04, 0.60] | 1.51 | [0.26, 2.76]* | — | — | — | — |
| Spouse and Kids & high income | 0.00 | [−1.28, 1.29] | 0.95 | [−0.15, 2.04] | — | — | — | — |
| Number of children by income interaction | ||||||||
| # children ≤12 & high income | — | — | — | — | 0.22 | [−0.13, 0.56] | 0.07 | [−0.26, 0.40] |
| # children 13–18 & high income | — | — | — | — | −0.46 | [−1.06, 0.14] | 0.12 | [−0.40, 0.64] |
Note. All models are adjusted for age, race, education, sex, current work status, living with a partner (number of children models only), and historical depressive symptoms.
Denotes significance at a p < .05 level.
Table 4.
Multivariable Linear Regression Models With Interaction Terms Estimating 1) PHQ-4 Total Score in April 2020 and 2) Change in PHQ-4 Score Between April and August 2020 by a) Household Structure and b) Number of Children in the Household, Stratified by Age of Children, and Their Interaction With Sex
| Outcome Primary predictor | Mental distress in April Household structure N= 1,495 |
Change in mental distress Household structure N = 1,495 |
Mental distress in April Number of Children (by age) N = 2,214 |
Change in mental distress Number of Children (by age) N = 2,214 |
||||
|---|---|---|---|---|---|---|---|---|
| β | [95% CI] | β | [95% CI] | β | [95% CI] | β | [95% CI] | |
| Household structure (ref: spouse only) | ||||||||
| Alone | 0.04 | [−0.94, 1.02] | −0.59 | [−1.55, 0.37] | — | — | — | |
| Kids only | 0.18 | [−0.66, 1.03] | −1.09 | [−2.05–0.13]* | — | — | ||
| Spouse and kids | 0.43 | [−0.33, 1.18] | −0.33 | [−1.11, 0.46] | — | — | ||
| Number of children | ||||||||
| # children ≤12 | — | — | — | — | −0.33 | [−0.59–0.07]* | 0.04 | [−0.22, 0.29] |
| # children 13–18 | — | — | — | — | −0.25 | [−0.74, 0.24] | −0.15 | [−0.60, 0.31] |
| Sex (ref: female) | ||||||||
| Male | 0.18 | [−0.85, 1.21] | −0.40 | [−1.23, 0.43] | 0.07 | [−0.24, 0.38] | 0.10 | [−0.21, 0.41] |
| Household structure by sex interaction | ||||||||
| Alone & Male | −0.47 | [−1.88, 0.95] | 0.35 | [−0.86, 1.56] | — | — | — | — |
| Kids Only & Male | −0.74 | [−2.43, 0.94] | 1.32 | [−0.17, 2.81] | — | — | — | — |
| Spouse and Kids & Male | −0.73 | [−1.90, 0.43] | 0.39 | [−0.61, 1.38] | ||||
| Number of children by sex interaction | ||||||||
| # children ≤12 & Male | — | — | — | — | 0.06 | [−0.34, 0.47] | −0.13 | [−0.47, 0.21] |
| # children 13–18 & Male | — | — | — | — | −0.21 | [−0.73, 0.32] | 0.25 | [−0.23, 0.73] |
Note. All models are adjusted for age, race, education, household income, current work status, living with a partner (number of children models only), and historical depressive symptoms.
Denotes significance at a p < .05 level.
Sensitivity Analyses
Using a more stringent household income cutoff for low income ($30,000) in the moderation analyses revealed additional significant interactions in the household structure models. Living alone, with children only, or with spouse and children, relative to spouse only in a low-income home, was associated with decreased distress for both low-income (interaction β = −2.29, −2.80, and −1.86, respectively) and high-income groups (association = −2.03, −2.01, and −2.05, respectively). The income cutoff showed no significant interactions in other moderation analyses looking at distress in April 2020 and number of children. Combining categories of comparable living situations (e.g., living with spouse only and living with significant other only) did not change the overall results.
Discussion
Our findings, based on data collected during the April and August 2020 waves of a nationally representative survey panel, found no significant differences in mental distress in April 2020 or change in mental distress in individuals living with a spouse compared to individuals living alone or with other immediate family members (e.g., spouse and children). This finding is consistent with literature that proposes no differences in mental health symptoms based on household structure (Cramer, 1993), but is in contrast to recent studies that suggest that individuals living alone fare worse than those living with others (Jacob et al., 2019). Individuals living alone may be less concerned about exposing friends and family to the virus (Shanafelt et al., 2020), may be used to living alone, or have fewer stressors than people living with others.
This study suggests that having children ages 12 and under in the household is associated with lower mental distress in April 2020, whereas having children ages 13 to 18 in the household is not associated with mental distress. Findings for this study are consistent with previous literature that suggests that parents experience high levels of well-being when spending time caring for young children (Roeters & Gracia, 2016). This may be true particularly during stay-at-home orders, which were enacted almost ubiquitously across all 50 states in April. Many parents were able to spend additional time with their children, and, as a result of the caregiving responsibilities, were prompted to implement practices that are known to be beneficial to mental health and resilience, including routine breaks from work, establishing a schedule, improving and increasing communication, and engaging in activities as a family (Prime et al., 2020). Having a family is associated with an increased sense of purpose and responsibility for parents, which has positive impacts on health (Pollitt et al., 2018). These effects may be enhanced during the pandemic as a result of the need to provide support and a sense of normalcy for children during a highly stressful time.
It is important to note, however, that these effects may not be universally experienced by parents. Recent studies have shown that the impact of COVID-19 among parents varies with caregiver burden and other crisis-related hardships (Gassman-Pines et al., 2020), perceptions of children’s stress (Russell et al., 2020), and the availability of resources to meet caregiver needs (Griffith, 2020). Therefore, while this study shows that young children, on average, are associated with reduced mental distress among parents, there are likely nuances in the experience of mental distress among parents as a result of these factors and other characteristics of family and work structure (e.g., age of children, flexibility of job, support system).
Not surprisingly, parents of adolescents are less likely to engage in caregiving activities as children in this age range are increasingly autonomous. While some earlier studies have suggested that rising parent–child tension in adolescence causes parental distress (Laursen et al., 1998), there is little empirical evidence showing child-induced distress. Prior studies have suggested numerous possibilities for this lack of evidence, including interperson variability in the experience of demands and reward of child rearing and the notion that reward and burdens of child rearing offset each other (Umberson et al., 2010). This may be especially true during the pandemic; adolescents are likely to experience additional COVID-19-related stress, relative to younger children, due to decreased socialization and increased household stressors (e.g., job loss, illness) that teenagers can better detect and process (“Teen Mental Health,” 2020).
The data showed no main effects of income in April 2020. There are many plausible explanations for these findings. For example, self-report of household income is prone to measurement error (Moore & Welniak, 2000) and may not accurately represent one’s actual household income, particularly during the COVID-19 pandemic. Furthermore, there is substantial variation in household size (between 0 and 11 housemates reported in this population of UAS participants). As expected, a livable income for one household may not be equivalent to the livable income of another. In analyses looking at change in mental distress, high income is associated with significantly lower mental distress. Moreover, these data showed a significant interaction between household structure and income in adjusted models, such that living with children only, relative to living with spouse only in a low-income home, was associated with decreased mental distress among low-income but not high-income individuals. It is likely that, over time, low income became increasingly burdensome, particularly among large families who lost access to free or reduced-price meals for school-age children and had to purchase learning tools or childcare that were not necessary prior to the pandemic.
Our findings show no significant difference in mental distress between males and females in April 2020 or across time. However, we did see that living with children, relative to females living with spouse only, was associated with decreased distress among females but not males. These findings are contrary to research showing lower rates of depression and anxiety among males (Altemus et al., 2014), especially during the pandemic, when women have reported disproportionate worry over coronavirus-related concerns (Frederiksen et al., 2020). Many sources hypothesized that men may be taking on additional household responsibilities during the pandemic (Carlson et al., 2020; Levs, 2020; Miller, 2020), leading to an increase in mental distress, but polls administered in October 2020 show that gender gaps in household responsibilities have remained consistent (Barroso, 2021). Instead, it may be that men are experiencing a greater negative impact on their mental health as a result of newfound isolation and job responsibilities, narrowing the traditional gap in mental distress (Mastroianni, 2020).
Black individuals show lower mental distress at baseline (before the pandemic began), consistent with previous studies (Hasin & Grant, 2015). However, as the pandemic progressed, being Black was associated with a significant increase in mental distress. This may be a result of the racial inequities that minority communities face, such as disproportionate involvement in service occupations (coined “essential” during the pandemic), which have been associated with high levels of mental distress partially due to high risk of exposure to COVID-19 (Kamal et al., 2020). In addition, Black people have been subject to trauma from witnessing police brutality and experiencing systemic racism and racial stereotyping throughout the pandemic (Christiani et al., 2021), which have been associated with increased mental distress (Schmittet al., 2014).
Despite many strengths, such as the use of a nationally representative study population, this study is not without limitations. First, we lacked data on relationship quality, marital satisfaction, and child mental health, which could mediate the association between household variables and mental distress. Investigating these potential mediators is an important direction for future studies. Second, we were unable to account for differences in timing of school closures and learning supports (e.g., tablets/computers, tutors), which likely influenced the relationship between living with children and mental distress. Understanding the impact of specific schooling situations (e.g., remote learning vs. hybrid) on mental distress could inform policy and allocation of learning supports.
This study supports previous research suggesting positive effects of child rearing and demonstrates that parents with young children may be particularly likely to experience these benefits (e.g., increased likelihood of taking routine breaks from work, spending time outside, and having set wake and bedtime schedules; Craig & Churchill, 2021) during the COVID-19 pandemic. Engaging in these physical and emotional activities, which come naturally with childcare, may also facilitate mental well-being among those not currently providing care. These data are unique in that they capture mental health of the U.S. population early in the pandemic at a time when nearly all schools were closed, and all states were under stay-at-home orders. These findings are among the first to document the consequences of specific living situations on mental health, which could be used to inform public health interventions to reduce mental distress on a population level.
Public Significance Statement.
Few studies have evaluated the association between household structure and mental well-being during the COVID-19 pandemic. This study builds on existing literature to explore whether the relationship differs by child age or is moderated by income and sex. Findings have the potential to inform family-oriented public health interventions.
Acknowledgments
The Understanding America Study is funded from several sources, including the Social Security Administration and the National Institute on Aging under grant 5U01AG054580. The survey that collected the mental health and COVID-19 related data used in this article was funded by the Center for Economic and Social Research at USC. Work on the current manuscript was in part supported by a RAPID Grant from the National Science Foundation (Grant number 2028683). Ms. Smail was supported by the National Institute on Aging Epidemiology and Biostatistics of Aging Training Program (T32AG000247). Kira E. Riehm was supported by the National Institute of Mental Health Mental Health Services and Systems Training Program (5T32MH109436-03) and by a Doctoral Foreign Study Award from the Canadian Institutes of Health Research. Cindy B. Veldhuis’ participation in this research was made possible through a National Institutes of Health/NIAAA Ruth Kirschstein Postdoctoral Research Fellowship (F32AA025816).
Footnotes
All authors have no potential conflicts of interest to disclose. The project described in this article relies on data from survey (s) administered by the Understanding America Study, which is maintained by the Center for Economic and Social Research (CESR) at the University of Southern California. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of USC or UAS. For any questions or more information about the UAS, contact Tania Gutsche, Project and Panel Manager, Center for Economic and Social Research, University of Southern California, at tgutsche@usc.edu.
References
- Altemus M, Sarvaiya N, & Neill Epperson C (2014). Sex differences in anxiety and depression clinical perspectives. Frontiers in Neuroendocrinology, 35(3), 320–330. 10.1016/j.yfrne.2014.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barroso A (2021). For American couples, gender gaps in sharing household responsibilities persist amid pandemic. Pew Research Center. https://www.pewresearch.org/fact-tank/2021/01/25/for-american-couples-gender-gaps-in-sharing-household-responsibilities-persist-amid-pandemic/ [Google Scholar]
- Bianchi S, Robinson J, & Milkie M (2006). Changing rhythms of American family life. Russell Sage Foundation Milky. [Google Scholar]
- Bracke P, Levecque K, & Van de Velde S (2008). The psychometric properties of the CES-D 8 depression inventory and the estimation of cross-national differences in the true prevalence of depression. Universiteit Leuven. https://biblio.ugent.be/publication/866310 [Google Scholar]
- Brown SM, Doom JR, Lechuga-Peña S, Watamura SE, & Koppels T (2020). Stress and parenting during the global COVID-19 pandemic. Child Abuse & Neglect, 10(Part 2), Article 104699. 10.1016/j.chiabu.2020.104699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson DL, Petts R, & Pepin J (2020). U.S. couples’ divisions of housework and childcare during COVID-19 pandemic SocArXiv. 10.31235/osf.io/jy8fn [DOI] [Google Scholar]
- Christiani L, Clark CJ, Greene S, Hetherington MJ, & Wager E (2021). Masks and racial stereotypes in a pandemic: The case for surgical masks. Journal of Race, Ethnicity and Politics. Advance online publication. 10.2139/ssrn.3636540 [DOI] [Google Scholar]
- Cosco TD, Prina M, Stubbs B, & Wu YT (2017). Reliability and validity of the center for epidemiologic studies depression scale in a population-based cohort of middle-aged U.S. adults. Journal of Nursing Measurement, 25(3), 476–485. 10.1891/1061-3749.25.3.476 [DOI] [PubMed] [Google Scholar]
- Craig L, & Churchill B (2021). Dual-earner parent couples’ work and care during COVID-19. Gender, Work & Organization, 28(S1), 514–527. 10.1111/gwao.12497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cramer D (1993). Living alone, marital status, gender and health. Journal of Community & Applied Social Psychology, 3(1), 1–15. 10.1002/casp.2450030102 [DOI] [Google Scholar]
- Crosier T, Butterworth P, & Rodgers B (2007). Mental health problems among single and partnered mothers. The role of financial hardship and social support. Social Psychiatry and Psychiatric Epidemiology, 42(1), 6–13. 10.1007/s00127-006-0125-4 [DOI] [PubMed] [Google Scholar]
- Frederiksen B, Gomez I, Salganicoff A, & Ranji U (2020, March 20) Coronavirus: A look at gender differences in awareness and actions. Kaiser Family Foundation. https://www.kff.org/coronavirus-covid-19/issue-brief/coronavirus-a-look-at-gender-differences-in-awareness-and-actions/ [Google Scholar]
- Gassman-Pines A, Ananat EO, & Fitz-Henley J (2020). COVID-19 and parent–psychological well-being. Pediatrics, 146(4), Article e2020007294, 10.1542/peds.2020-007294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golberstein E, Wen H, & Miller BF (2020). Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatrics, 174(9), 819–820. 10.1001/jamapediatrics.2020.1456 [DOI] [PubMed] [Google Scholar]
- Goodell JW (2020). COVID-19 and finance: Agendas for future research. Finance Research Letters, 35, Article 101512. 10.1016/j.frl.2020.101512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffith AK (2020). Parental burnout and child maltreatment during the COVID-19 pandemic. Journal of Family Violence. 10.1007/s10896-020-00172-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guzman G (2019). U.S. median household income up in 2018 from 2017 U. S. Census Bureau. https://www.census.gov/library/stories/2019/09/us-median-household-income-up-in-2018-from-2017.html [Google Scholar]
- Hasin DS, & Grant BF (2015). The national epidemiologic survey on alcohol and related conditions (NESARC) waves 1 and 2: Review and summary of findings. Social Psychiatry and Psychiatric Epidemiology, 50(11), 1609–1640. 10.1007/s00127-015-1088-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holingue C, Kalb LG, & Riehm KE (2020). Mental distress in the United States at the beginning of the 2019 coronavirus disease (COVID-19) pandemic. American Journal of Public Health, 110, 1628–1634. 10.2105/AJPH.2020.305857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacob L, Haro JM, & Koyanagi A (2019). Relationship between living alone and common mental disorders in the 1993, 2000 and 2007 national psychiatric morbidity surveys. PLOS ONE, 14(5), Article e021518210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joutsenniemi K, Martelin T, Martikainen P, Pirkola S, & Koskinen S (2006). Living arrangements and mental health in Finland. Journal of Epidemiology and Community Health, 60(6), 468–475. 10.1136/jech.2005.040741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamal R, Panchal N, & Garfield R (2020). Both remote and on-site workers are grappling with serious mental health consequences of COVID-19. Kaiser Family Foundation. https://www.kff.org/policy-watch/both-remote-and-on-site-workers-are-grappling-with-serious-mental-health-consequences-of-covid-19/ [Google Scholar]
- Kirzinger A, Kearney A, Hamel L, & Brodie M (2020)., April KFF health tracking poll—Early April 2020: The impact of coronavirus on life in America. Kaiser Family Foundation. https://www.kff.org/coronavirus-covid-19/report/kff-health-tracking-poll-early-april-2020/ [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW, & Löwe B (2009). An ultra-brief screening scale for anxiety and depression: The PHQ-4. Psychosomatics, 50(6), 613–621. 10.1176/appi.psy.50.6.613 [DOI] [PubMed] [Google Scholar]
- Laursen B, Coy KC, & Collins WA (1998). Reconsidering changes in parent–child conflict across adolescence: A meta-analysis. Child Development, 69(3), 817–832. 10.1111/j.1467-8624.1998.tb06245.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavrakas PJ (2008). Encyclopedia of survey research methods (Vol. 2, 1st ed.). Sage. 10.4135/9781412963947 [DOI] [Google Scholar]
- Levs J (2020, June 18). One upside of COVID-19: Kids are spending more time with dads. Scientific American. [Google Scholar]
- Li Z, Ge J, Yang M, Feng J, Qiao M, Jiang R, Bi J, Zhan G, Xu X, Wang L, Zhou Q, Zhou C, Pan Y, Liu S, Zhang H, Yang J, Zhu B, Hu Y, Hashimoto K, & Yang C (2020). Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain, Behavior, and Immunity, 88, 916–919. 10.1016/j.bbi.2020.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe B, Wahl I, Rose M, Spitzer C, Glaesmer H, Wingenfeld K, Schneider A, & Brähler E (2010). A 4-item measure of depression and anxiety: Validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. Journal of Affective Disorders, 122(1–2), 86–95. 10.1016/j.jad.2009.06.019 [DOI] [PubMed] [Google Scholar]
- Mastroianni B (2020). How COVID-19 is impacting men’s mental health differently. Healthline. https://www.healthline.com/health-news/how-covid-19-is-impacting-mens-mental-health-differently [Google Scholar]
- McDonnell C, Luke NK, & Short SE (2019). Happy moms, happier dads: Gendered caregiving and parents’ affect. Journal of Family Issues, 40(17), 2553–2581. 10.1177/0192513X19860179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinty EE, Presskreischer R, Han H, & Barry CL (2020). Psychological distress and loneliness reported by U.S. adults in 2018 and April 2020. JAMA: Journal of the American Medical Association, 324(1), 93–94. 10.1001/jama.2020.9740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller C (2020, May 8). Survey finds half of men think they do most homeschooling and 3% of women agree. Scary Mommy. https://www.scarymommy.com/women-more-housework-pandemic/ [Google Scholar]
- Moore JC, & Welniak EJ (2000). Income measurement error in surveys: A review. Journal of Official Statistics, 16(4), 331–361. [Google Scholar]
- Offer S (2014). Time with children and employed parents’ emotional well-being. Social Science Research, 47, 192–203. 10.1016/j.ssresearch.2014.05.003 [DOI] [PubMed] [Google Scholar]
- Patel V, Burns JK, Dhingra M, Tarver L, Kohrt BA, & Lund C (2018). Income inequality and depression: A systematic review and meta-analysis of the association and a scoping review of mechanisms. World Psychiatry, 17(1), 76–89. 10.1002/wps.20492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickett KE, James OW, & Wilkinson RG (2006). Income inequality and the prevalence of mental illness: A preliminary international analysis. Journal of Epidemiology and Community Health, 60(7), 646–647. 10.1136/jech.2006.046631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollitt AM, Robinson BA, & Umberson D (2018). Gender conformity, perceptions of shared power, and marital quality in same- and different-sex marriages. Gender & Society, 32(1), 109–131. 10.1177/0891243217742110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prime H, Wade M, & Browne DT (2020). Risk and resilience in family well-being during the COVID-19 pandemic. American Psychologist, 75(5), 631–643. 10.1037/amp0000660 [DOI] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D scale. Applied Psychological Measurement, 1(3), 385–401. 10.1177/014662167700100306 [DOI] [Google Scholar]
- Rizzo K, Schiffrin H, & Liss M (2013). Insight into the parenthood paradox: Mental health outcomes of intensive mothering. Journal of Child and Family Studies, 22(5), 614–620. 10.1007/s10826-012-9615-z [DOI] [Google Scholar]
- Roeters A, & Gracia P (2016). Child care time, parents’ well-being, and gender: Evidence from the American Time Use Survey. Journal of Child and Family Studies, 25(8), 2469–2479. 10.1007/s10826-016-0416-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell BS, Hutchison M, Tambling R, Tomkunas AJ, & Horton AL (2020). Initial challenges of caregiving during COVID-19: Caregiver burden, mental health, and the parent–child relationship. Child Psychiatry and Human Development, 51, 671–682. 10.1007/s10578-020-01037-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmitt MT, Branscombe NR, Postmes T, & Garcia A (2014). The consequences of perceived discrimination for psychological well-being: A meta-analytic review. Psychological Bulletin, 140(4), 921–948. 10.1037/a0035754 [DOI] [PubMed] [Google Scholar]
- Shanafelt T, Ripp J, & Trockel M (2020). Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA: Journal of the American Medical Association, 323(21), 2133–2134. 10.1001/jama.2020.5893 [DOI] [PubMed] [Google Scholar]
- Sobolewski J, & King V (2005). The importance of the coparental relationship for nonresident fathers’ ties to children. Journal of Marriage and Family, 67(5), 1196–1212. 10.1111/j.1741-3737.2005.00210.x [DOI] [Google Scholar]
- Spinelli M, Lionetti F, Pastore M, & Fasolo M (2020). Parents’ stress and children’s psychological problems in families facing the COVID-19 out-break in Italy. Frontiers in Psychology, 11, Article 1713. 10.3389/fpsyg.2020.01713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statacorp. (2017). Stata statistical software: Release 15 [Computer software].
- Teen mental health. (2020). 4-H. https://4-h.org/wp-content/uploads/2020/06/4-H-Mental-Health-Report-6.1.20-FINAL.pdf
- The University of Southern California. (2020). Understanding America study. https://uasdata.usc.edu/index.php
- U.S. Department of Labor. (2020). Unemployment insurance weekly claims.
- Umberson D, Pudrovska T, & Reczek C (2010). Parenthood, childlessness, and well-being: A life course perspective. Journal of Marriage and Family, 72(3), 612–629. 10.1111/j.1741-3737.2010.00721.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veldhuis CB, Nesoff ED, McKowen ALW, Rice DR, Ghoneima H, Wootton AR, Papautsky EL, Arigo D, Goldberg S, & Anderson JC (2021). Addressing the critical need for long-term mental health data during the COVID-19 pandemic: Changes in mental health from April to September 2020. Preventive Medicine, 146, Article 106465. 10.1016/j.ypmed.2021.106465 [DOI] [PMC free article] [PubMed] [Google Scholar]


