Abstract
A 66-year-old man presented with a chief complaint of difficulty breathing and productive cough. CT scan of the chest revealed an endobronchial mass with associated “tree-in-bud” opacities. A bronchoscopic biopsy of the mass was performed due to clinical suspicion of malignancy. Microscopic examination revealed inflamed endobronchial mucosa, granulation tissue and abundant fragments of uncharacterized organic material, compatible with aspiration. Detailed history revealed a history of chewing “gutkha”, a form of smokeless tobacco comprising a mixture of betel nut and other condiments. Microscopic sections of a betel nut and the “gutkha mix” processed subsequently in the histology laboratory were found to be similar to the organic material found in the mass. Thus, a diagnosis of impacted betel nut mixture leading to post-obstructive pneumonia was rendered.
Keywords: Aspiration, CT, Endobronchial mass, Pneumonia, Betel nut, Gutkha
Abbreviations: DNA, deoxyribonucleic acid; CT, computed tomography; CMA, chronic micro aspiration
1. Introduction
Areca nut, commonly referred to as betel nut, is the fruit of the Areca palm. It is consumed in various forms in South and Southeast Asia and Asia Pacific [1]. A betel quid, or “gutkha” is a chewing mixture comprising of areca nut, slaked lime, catechu, betel leaves, spices, sweeteners and tobacco [2]. As a cultural practice, this mixture is either chewed or constantly kept as a quid in the gingivobuccal sulcus. Gutkha users have reported a sense of relaxation, well-being, reduced appetite and improved concentration from the use of this mixture [2]. However, long term consequences of Gutkha use, in addition to nicotine addiction, include tooth and gum discoloration, oral ulcers, periodontitis and oral submucosal fibrosis [3], a precancerous lesion. Consequently, betel nut and Gutkha consumption are associated with an increased incidence of oral cancers [4]. The main constituents of areca nut include carbohydrates, fats, proteins, polyphenols (flavonols and tannins), alkaloids (mainly arecoline), and high levels of copper [2,4]. These are known to increase collagen synthesis, reactive oxygen species production, and DNA damage. Other constituents of “gutkha”, such as slaked lime also increase cell turnover and DNA damage, and tobacco releases various nitrosamines in the mouth that cause proliferative abrasions and damage to DNA and fibroblasts [2,5]. Together, they contribute to lesions of oral mucosa such as leukoplakia, erythroplakia, oral submucous fibrosis and oral carcinogenesis.
This case describes an unusual presentation of impaction of gutkha mixture presenting as an endobronchial mass lesion leading to post-obstructive pneumonia.
2. Case presentation
A 66-year old chronic smoker was referred to see a pulmonologist for a non-resolving abnormality on CT scan. Two months prior to this current visit, he had presented in an urgent care setting, with non-productive cough, fever and chills. Chest radiograph at that time showed a left lower lobe opacity. He was empirically treated with antibiotics that resulted in resolution of his symptoms. However, follow up chest radiographs showed no significant improvement and a chest CT scan was performed. The CT scan revealed a possible endobronchial lesion obstructing the left lower lobe bronchus and associated left lower lobe “tree-in-bud” opacities (Fig. 1A, Fig. 1B, Fig. 1CA, B and 1C) with mildly enlarged lymph nodes in the aorticopulmonary window and mediastinum. Bronchoscopy showed a partially obstructive endobronchial lesion occluding the passage to the anterior, lateral and posterior segments of the left lower lobe. Several endobronchial biopsies and brushings of the lesion were performed and sent for pathologic examination. No additional debulking procedures were performed at this time. Initial microscopic examination revealed markedly inflamed endobronchial mucosal tissue, exuberant granulation tissue, acute inflammatory exudate and abundant fragments of non-polarizable, organic foreign material that could not be further characterized (Fig. 2A). The foreign material demonstrated a lattice-like arrangement of lacunar spaces containing refractile, golden brown substance surrounded by glassy, chondroid-like stroma (Fig. 2B). The organic material showed no resemblance to food particles and pill fragments, commonly encountered in pathology specimens. The possibility of aspirated organic foreign material was considered and a more detailed history was elicited from the patient and his wife. This revealed that in addition to smoking one pack of cigarettes per day for the past 45 years, the patient had been chewing an areca nut mixture (Gutkha) for a number of years. The patient was asked to bring in a sample of the mixture for pathologic examination. Formalin fixed paraffin embedded sections were prepared out of the Gutkha mixture (Fig. 2C) and an intact areca nut (Fig. 2D) and stained using H&E stains (Fig. 2E). Microscopic examination revealed identical morphologies across all three samples (i.e. areca nut, gutkha mixture and organic material in the biopsy). Thus, a diagnosis of post-obstructive pneumonia secondary to “gutkha” impaction in the bronchus was established. The patient was started on broad spectrum antibiotics, counselled on smoking and “ghutka” chewing cessation and a subsequent one month-interval CT scan showed resolution in radiologic abnormalities. (Fig. 3). No additional bronchoscopic surgical intervention was required for further management.
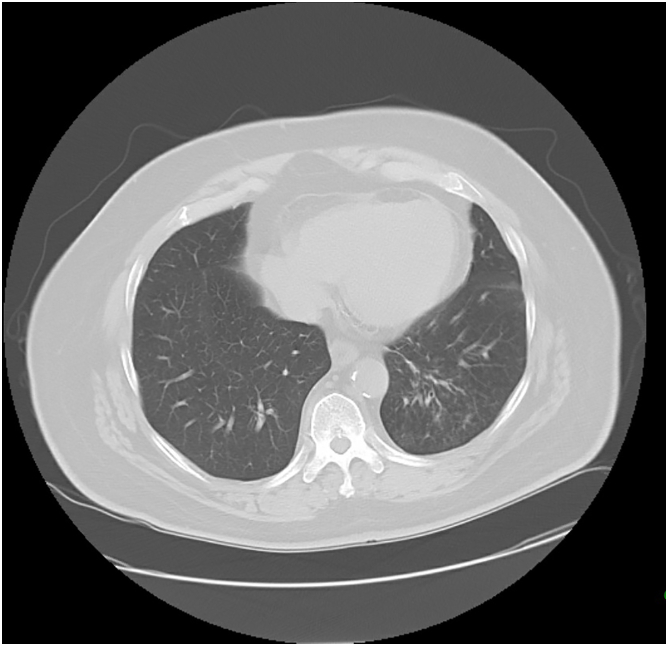
Fig. 1A.
CT scan (non-contrast, lung window) showing endobronchial lesion obstructing the left lower lobe bronchus and associated left lower lobe “tree-in-bud” opacities.
Fig. 1B.
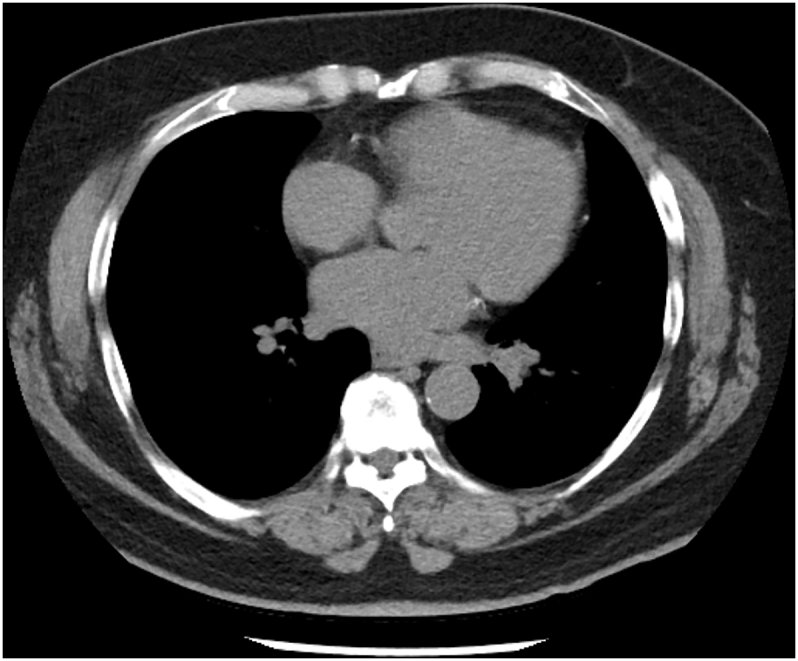
CT scan (non-contrast, mediastinal window and) corresponding to Fig. 1A demonstrated mildly enlarged lymph nodes in the aorticopulmonary window and inferior left mediastinum.
Fig. 1C.
CT scan (non-contrast, coronal view) of the lung and mediastinum.
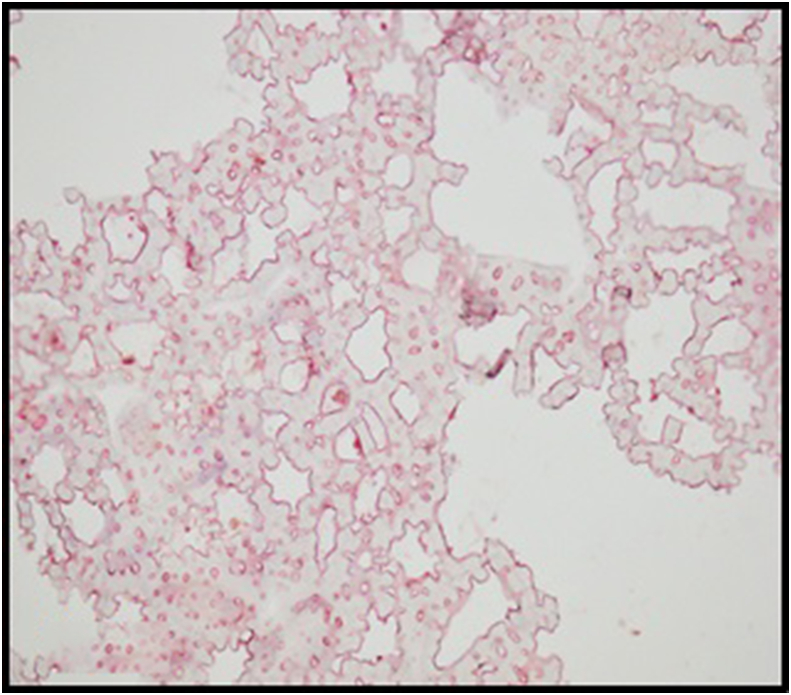
Fig. 2A.
Inflamed endobronchial mucosal tissue with fragments of non-polarizable, organic foreign material on the left (H&E, 20X).
Fig. 2B.
Foreign material showing lattice-like arrangement of lacunar spaces containing refractile, golden brown material surrounded by glassy, chondroid-like stroma (H&E, 20X). (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
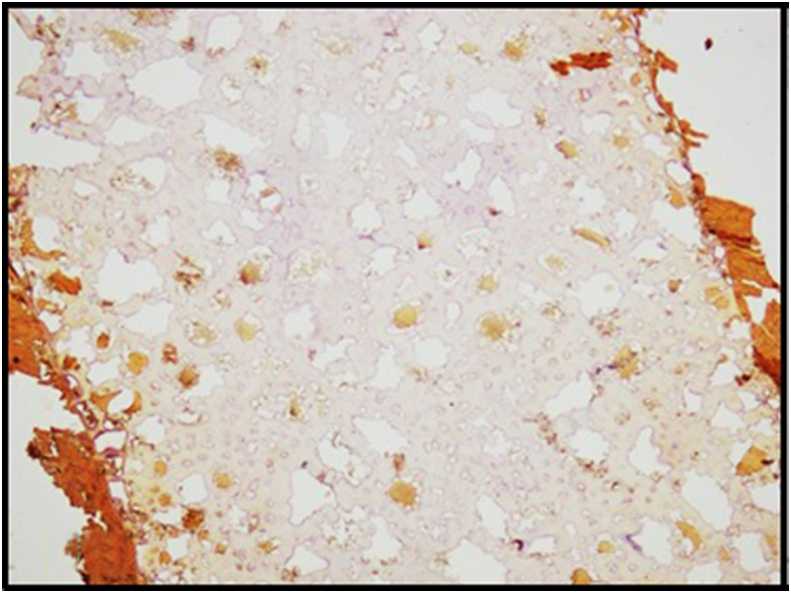
Fig. 2C.
Gutkha mixture histology showing similar architecture as the foreign material (Paraffin embedded, H&E, 20X).
Fig. 2D.
Intact areca nut histology, showing similar architecture as the foreign material (Paraffin embedded, H&E, 20X).
Fig. 2E.
Gutkha mixture histology showing similar architecture as the foreign material (Paraffin embedded, H&E, 20X).
Fig. 3.
CT scan 4 month post bronchoscopy showing resolution of the lesion.
3. Discussion
Chewing betel nuts is a fairly common cultural practice in South and South-east Asia and Asia Pacific. A subset of this population, continues this practice even after settling and immigrating to nations outside the Asian belt [2].
Chronic bronchial foreign body aspiration is commonly seen in children, especially toddlers. Persistent cough, recurrent wheezing/pneumonia, and fever are the common symptoms. Complications such as atelectasis, bronchiectasis, and bronchial fistula may also develop [6]. Foreign body aspiration in adults is uncommon and typically presents as a choking event followed by persistent coughing [7]. The clinical presentation in this case was more insidious and the imaging findings was suspicious of an occult mass lesion with post-obstructive changes. This is not an uncommon scenario; as per Hewlett JC et al. [7], most adult patients do not recall an obvious episode of aspiration. While clinicians are cognisant of witnessed aspiration events or aspiration bronchopneumonia in debilitated individuals or those with an unprotected airway, both treating physicians as well as pathologists often miss the diagnosis of foreign body inhalation and chronic microaspiration (CMA) [8].
A systematic metanalysis review of literature on foreign body inhalation in adults by Sehgal IS et al. revealed that non-resolving pneumonia was the most common radiological finding in these subjects and a vast of majority of these cases were due to metallic objects such as pins, whistles, screws etc [9]. Occasionally, organic material (peanuts, betelnuts, lentil seeds etc) could be grossly identified at the time of bronchoscopic examination, especially if the clinical presentation was acute or aspiration was witnessed. However, many cases of adult microaspiration and foreign body inhalation, present insidiously with impaction in peripheral segmental branches. Furthermore, as seen in this case, inhaled and aspirated agents often get buried in an overgrowth of inflammatory exudate and granulation tissue, making it difficult to ascertain the nature of the obstruction at the time of the biopsy. Aspirated material in CMA most often comprises of food or vegetable matter in various stages of degeneration associated with multinucleated giant cells and foci of organizing pneumonia. Occasionally, pill fragments and filler substances may be identified pathologically in cases of CMA. While surgical pathologists are attuned to recognize organic food matter, pill fragments, inhaled/injected polarizable particles in the lung, the unusual nature of the impacted foreign material further added to the diagnostic dilemma. As noted by Sehgal IS et al., eating habits, occupation and local customs dictate the nature of the foreign bodies encountered at the time of aspiration in an ethnically diverse population [9].
4. Conclusion
This case report is unusual on two fronts; not only was there chronic impaction of a foreign object in the lower lobe bronchus, the nature of the impacted material was also bewildering. This case is an interesting example of a benign finding mimicking a neoplasm radiologically. It is important to be aware of the appearance of common foreign materials to correctly identify them and avoid a misdiagnosis. In this case, the history of “gutkha” chewing was elicited only after microscopic evidence of organic material in the biopsy. Thorough clinical history, and high index of suspicion often help unearth these zebras hiding in plain sight.
Summary conflict of interest statements
None.
Funding information
None.
Notation of prior abstract publication/presentation
None.
Declaration of competing interest
The authors whose names are listed below certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Acknowledgements
None.
Contributor Information
Swati Bhardwaj, Email: Swat.bhrdwj@gmail.com.
Paul A. Chung, Email: Paul.chung1@northwestern.edu.
Recep Nigdelioglu, Email: rcpnig@gmail.com.
Michal Reid, Email: Michal.reid@lumc.edu.
Monica Lockhart, Email: Mlockha43@gmail.com.
Sean M. Forsythe, Email: Sforsy1@lumc.edu.
References
- 1.Gupta P.C., Ray C.S. Epidemiology of betel quid usage. Ann. Acad. Med. Singapore. 2004;33(4 suppl):31–36. [PubMed] [Google Scholar]
- 2.Sankhla B., Kachhwaha K., Hussain S.Y., Saxena S., Sireesha S.K., Bhargava A. Genotoxic and carcinogenic effect of gutkha: a fast-growing smokeless tobacco. Addict. Health. 2018;10(1):52–63. doi: 10.22122/ahj.v10i1.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maher R., Maher R., Lee A.J., Warnakulasuriya K.A., Lewis J.A., Johnson N.W. Role of areca nut in the causation of oral submucous fibrosis: a case-control study in Pakistan. J. Oral Pathol. Med. 1994;23(2):65–69. doi: 10.1111/j.1600-0714.1994.tb00258.x. [DOI] [PubMed] [Google Scholar]
- 4.IARC Working Group on the Evaluation of Carcinogenic Risk to Humans . Lyon (FR): International Agency for Research on Cancer. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans; 2004. Betel-quid and areca-nut chewing and some areca-nut-derived nitrosamines.https://www.ncbi.nlm.nih.gov/books/NBK316567/ No. 85) Available from: [PMC free article] [PubMed] [Google Scholar]
- 5.Nair J., Ohshima H., Friesen M., Croisy A., Bhide S.V., Bartsch H. Tobacco-specific and betel nut-specific N-nitroso compounds: occurrence in saliva and urine of betel quid chewers and formation in vitro by nitrosation of betel quid. Carcinogenesis. 1985;6(2):295–303. doi: 10.1093/carcin/6.2.295. [DOI] [PubMed] [Google Scholar]
- 6.Boufersaoui A., Smati L., Benhalla K.N., et al. Foreign body aspiration in children: experience from 2624 patients. Int. J. Pedatr. Otorhinolaryngol. 2013;77:1683–1688. doi: 10.1016/j.ijporl.2013.07.026. [DOI] [PubMed] [Google Scholar]
- 7.Hewlett J.C., Rickman O.B., Lentz R.J., Prakash U.B., Maldonado F. Foreign body aspiration in adult airways: therapeutic approach. J. Thorac. Dis. 2017;9(9):3398–3409. doi: 10.21037/jtd.2017.06.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mukhopadhyay S., Katzenstein A.L. Pulmonary disease due to aspiration of food and other particulate matter: a clinicopathologic study of 59 cases diagnosed on biopsy or resection specimens. Am. J. Surg. Pathol. 2007;31(5):752–759. doi: 10.1097/01.pas.0000213418.08009.f9. [DOI] [PubMed] [Google Scholar]
- 9.Sehgal I.S., Dhooria S., Ram B., et al. Foreign body inhalation in the adult population: experience of 25,998 bronchoscopies and systematic review of the literature. Respir. Care. 2015 Oct;60(10):1438–1448. doi: 10.4187/respcare.03976. [DOI] [PubMed] [Google Scholar]