Abstract
Introduction
Molecular diagnostics using RT-PCR has now emerged as the new diagnostic method for clinicians with the dawn of SARS-CoV-2. In India, the popularity and awareness of RT-PCR and particularly the increased availability of testing machines across hospitals has now opened up possibilities of diagnostic tests with RT-PCR. In view of the cytokine storm which is the significant reason for morbidity and mortality of COVID-19 patients, we proposed to test the usefulness of a multiplex RT-PCR test kit that simultaneously measured inflammatory markers namely, IL-6, TNF– α and IL-10 (IFM) all in one tube. The study included a group of patients who were equally allotted to two treatment arms one of which received standard of care along with a food supplement capsule as a natural anti-inflammatory (RECOVEREEZ FORTE™), and the other group received standard of care that included oral Prednisolone tablets in tapered dosage. RECOVEREEZ FORTE™ consists of potent biomolecules from cardamom extract. A natural product with substantial anti-inflammatory action when consumed early at the onset of symptoms is hereby proven by comparing gene expression profile of inflammatory markers with routinely tested inflammatory parameters such as serum IL-6, CRP and LDH. In addition to predicting worse disease outcomes beforehand, RT-PCR assay tests provides an opportunity for identifying therapeutic window aiding in practicing effective treatment strategy for COVID-19. RT-PCR analysis of IFM together being used in a single multiplex kit is being first reported and such a test as a prognosticator for disease progression does seem promising and worthy of clinicians adopting novel testing modalities in clinical practice.
Aim of the study
To study the anti-inflammatory response of RECOVEREEZ FORTE™ using RT-PCR based multiplex gene profiling of inflammatory markers in disease prognosis and show its predictability of worsening outcomes and its role in identifying therapeutic window for RECOVEREEZ FORTE™. To show the potentiality of RECOVEREEZ FORTE™ in reducing COVID-19 symptoms and SARS-CoV-2 RT-PCR Ct values of the treatment group.
Materials and methods
This was a short study of a 10-day period where the end point was the negativity of COVID-19 on RT-PCR test or the decline in cycle threshold (Ct) values of the test performed on day 10 when compared to day 0. During the course of the study, patients were given standard treatment and an oral dose of 500 mg of RECOVEREEZ FORTE™ thrice daily, or standard of care and oral Prednisolone in tapered dosage (control group). All essential interventions were included in the standard of care as decided by the attending physician. The RT-PCR results of inflammatory markers were compared to routinely tested parameters such as IL-6, CRP and LDH. Time to clinical improvement was in terms of SARS-CoV-2 RT-PCR test negativity or recovery of COVID-19 symptoms. We enrolled 64 patients, of which 32 were allocated to RECOVEREEZ FORTE ™ group and 32 to the control group.
Results
The RT-PCR analysis of elevated IFM on day 0 corresponded to above normal protein levels of routinely tested parameters such as serum IL-6, CRP and LDH on day 5. Similarly, elevated IFM on day 5 corresponded to above normal protein levels on day 10. Such an association was equally prevalent in both the control group and RECOVEREEZ FORTE™ group, stipulating that RECOVEREEZ FORTE™ may be used as an alternative to steroids. The obtained results indicate that the RT-PCR assessment predicts worse outcomes 5 days earlier. But, the RT-PCR analysis of elevated IFM on day 0 did not correspond to the above normal protein levels of other parameters on day 10. Hence, indicating that the IFM RT-PCR test cannot predict worse outcomes 10 days earlier. Also, RECOVEREEZ FORTE™ when consumed for a period of 10 days normalized LDH values, compared to the control group. Moreover, IFM RT-PCR test identified a 5-day therapeutic window for RECOVEREEZ FORTE™ against inflammation experienced by patients. In addition to the above findings, the authors also observed that majority of the patients belonging to the treatment group showed recovery from symptoms such as fever, cough, sore throat and breathlessness compared to control group by day 5. 12 (37.5%) out of 32 patients and 6 (18.75%) out of 32 patients belonging to the treatment group and control group, respectively, became SARS-CoV-2 negative by day 5, indicating a probable anti-viral action of RECOVEREEZ FORTE™ against SARS-CoV-2.
Conclusion
The IFM RT-PCR test possess 5-day early prediction ability and lacks 10-day prediction ability. Treatment with RECOVEREEZ FORTE™ indicates good anti-inflammatory action which is equivalent to steroids. Intake of RECOVEREEZ FORTE ™ for a period of 5 days depicts persistent anti-inflammatory action, recovery of COVID-19 symptoms and a probable anti-viral action. Moreover, an effective normalization of LDH may be rendered by RECOVEREEZ FORTE™ when consumed for a period of 10 days.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10787-022-00951-x.
Keywords: COVID-19, Inflammation, Prognosis, IL-6, CRP, LDH, Cardamom
Introduction
COVID-19 has produced an overwhelming challenge to clinical management of patients in respiratory distress that resulted from cytokine storm produced classically in severe COVID-19 patients. Cytokine storm (CS) refers to excessive and uncontrolled release of pro-inflammatory cytokines (Fara et al. 2020; Hu et al. 2021). Clinically, it commonly presents as systemic inflammation, multiple organ failure, and high inflammatory parameters. The otherwise manageable disease which could be managed on an outpatient basis, suddenly created a panic among patients, many of whom insisted on getting admitted to hospitals due to an occasional drop in oxygen saturation levels on pulse oximeter and thereby challenging the existing system where most hospitals had few intensive care beds. Obtaining a hospital bed seemed difficult at times when there were overwhelming positive cases in a town or city, and as the caseload reduced, this situation eased out. Cardamom extracts have been shown to reduce the inflammatory cytokine storm by reducing oxidative stress by scavenging reactive oxygen species (ROS), attenuating inflammation by downregulating NF-κB, a key regulator of inflammatory disease pathogenesis (Juergens et al. 2017), and regulating nitric oxide (NO) generation. (Ryu et al. 2014). The primary bioactive components in cardamom, such as alpha terpineol (Horváth and Ács 2015) and 1,8-cineole (Worth et al. 2009), have been attributed to these therapeutic properties, particularly in respiratory disorders like asthma and COPD. According to reports, 1,8-cineole has an inhibitory effect on pro-inflammatory molecules such as cyclooxygenase (COX-1, COX-2) (Am et al. 2017) and lipoxygenase, which further supports cardamom's anti-inflammatory properties (Sengupta et al. 2005). In addition to anti-inflammatory and immunomodulatory effects, medical interventions that may prevent SARS-CoV-2 viral spike protein from interacting with the cellular angiotensin-converting enzyme 2 (ACE2) are being explored, which allows SARS-CoV-2 to attach and enter host cells (Hoffmann et al. 2020). Molecular docking reports show that α-terpinyl acetate can bind to ACE2 receptors, and 1,8 cineole can bind to SARS-CoV-2 protease Mpro, thereby inhibiting virus reproduction (Asif et al. 2020; Kumar et al. 2021). Therefore, based on thorough scientific and critical evaluation of previously published reports promising the potentialities of cardamom extract as an anti-viral, anti-oxidant, anti-inflammatory and immunomodulatory agent, we developed a standardized cardamom extract-based food supplement product (RECOVEREEZ FORTE™) that merits anti-inflammatory testing. RECOVEREEZ FORTE™ was administered to 32 subjects belonging to the treatment group. Prediction of COVID-19 patients who are likely to take a downward trend has been performed conventionally by serial monitoring of inflammatory markers such as ferritin, C-reactive protein (CRP) and d-dimers, and this has become a standard practice in most treating centers to determine the possible need for intensive care treatment apart from clinical symptoms. Most of the severe COVID-19 patients in ICU reportedly had extremely high levels of erythematosus sedimentation rate (ESR) and inflammatory parameters including CRP, and pro-inflammatory cytokines such as IL-6, TNF-α, IL-1β, IL-8. The severity was also associated with hypercoagulation, acute respiratory distress syndrome (ARDS) and disseminated intravascular coagulation (DIC) (Zhang et al. 2020). As all these tests need be done separately, and apart from the high cost of these tests, the time consumed for doing them as they were not available at all hospitals that treated severe COVID-19, prompted us to explore the use of gene expression of IL-6, TNF-α and IL-10 detected through RT-PCR that can offer an alternative to analyze all the markers in just one test. This approach would offer greater opportunity window for treating severely ill-patients with therapeutic agents before they became clinically worse. Suggested use of immunomodulatory agents reduce systemic inflammation before it overwhelmingly leads to multi-organ dysfunction, resulting in the use of corticosteroids which may be justified in concert with the use of cytokine inhibitors such as tocilizumab (IL-6 inhibitor) or anakinra (IL-1 receptor antagonist) (Siddiqi and Mehra 2020). Levels of the IL-6 and TNF-α production also depend on NF-κB activation. Detection of inflammatory biomarkers in a single time-saving multiplex RT-PCR test is critically lacking. We implemented a rapid multiplex cytokine assay to measure serum interleukin (IL)-6, IL-10 and tumor necrosis factor (TNF)-α and used it in patients with COVID-19 across a multicenter study. Clinical biomarkers are generally defined as the measurable biological indicators of the presence, severity or type of disease in medical settings (Aronson and Ferner 2017). They can help us understand attributes such as the cause of the disease, phenotype, progression or regression, prognosis, or treatment outcome (Mayeux 2004; Dobler 2019). Biomarkers lead to the advent of personalized medicine, which predominantly aims to tailor treatments to patients based on their biomarker profile and, by doing so, reduce the adverse effect of ineffective treatments and increase the benefits from effective treatments (Dobler 2019). Faultless detection, early diagnosis, effective treatment, and future prevention are the vital keys to manage COVID-19, and curb the spread. Biomarkers play a crucial role in the early observation of disease etiology, diagnosis, treatment and prognosis. We developed this present article to provide an overview of existing and emerging biomarkers for SARS-CoV-2 detection, COVID-19 diagnosis, treatment, and prognosis.
Methodology
Trial design
This study was a multicentric, open-label, randomized and controlled trial conducted from May 2021 through July 2021. The protocol was approved by the Orchid Specialty Hospital Ethics committee, and the trial was registered in Clinical Trials Registry India (CTRI—CTRI/2021/04/033143) in compliance with the International Council on Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use–Good Clinical Practice (ICH–GCP) guidelines. Written informed consent was obtained from all patients. Random assignment into either one of the groups, a 1:1 ratio to receive RECOVEREEZ FORTE™ capsules produced for 10 days at 500 mg, thrice a day plus standard care and oral Prednisolone in tapered dosage along with standard of care (control group) was performed. RECOVEREEZ FORTE™ comprises cardamom extract at 200 mg, rosemary extract at 200 mg and pepper extract at 10 mg amounting to a total 1,8-cineole content of 97 mg per capsule. The control group subjects were administered with oral Prednisolone in tapered dosage for 10 days, 100 mg × 3 times for first 3 days, 100 mg × 2 times for the next 3 days and 100 mg × 1 time for the last 4 days. The total sample size for the study was 64 with 32 subjects in each group, being studied for the gene expression of IL-6, IL-10 and TNF-α in a multiplex RT-PCR test. All patients included in the study were detected positive for COVID -19 in RT-PCR test no more than 24 h before enrolment into this study. The first sample for IFM RT-PCR study was collected on the day of enrolment into the study, designated as day 0. The end point of the study was 10 days and or COVID-19 negative report in RT-PCR.
Randomization
Randomization was done using simple random sampling method. The simple random sampling was done using computer generated simple random number table. To minimize bias, allocation concealment was performed by researchers not involved in patient care. The data analysis was carried out with external statistical support and in an impartial manner.
Patients
Patients over 18–75 years of age of either sex, diagnosed with SARS-CoV-2 infection, confirmed by polymerase chain reaction–reverse transcriptase testing, having mild to moderate disease who can take oral medicines were considered eligible for simple randomization. Exclusion criteria included patients of age less than 18 years and more than 75 years, patients with a COVID-19 positive test done more than 24 h prior to enrolment in study, pregnant and lactating women, patients who experienced severe or complicated course of COVID-19 disease, presence of acute hypoxic respiratory failure, patients who need mechanical ventilation and admitted to the ICU, patients with serious systemic infection/disease such as cardiovascular, cerebrovascular, respiratory, liver or renal disease, which in the opinion of the investigators made the patient unsuitable for enrolment or could interfere with the adherence of study protocol.
Statistical analysis
The statistical analysis was performed by IBM SPSS 26.0 software. Categorical variables are expressed using frequency and percentage. Continuous variables are presented by mean and standard deviation. To test the statistical significance of difference in proportion of categorical factors between groups (RECOVEREEZ FORTE™ group, control group), Chi square test along with Fishers exact test was used. Increasing trend of gene expression was compared with the normal reference range of protein levels by using appropriate equations in Microsoft Excel.
Results
Patients
Of the 80 patients who were screened for eligibility, 64 met inclusion criteria and underwent enrolment with randomization. 32 patients were allocated to get RECOVEREEZ FORTETM (500 mg, three times per day) and 32 received oral Prednisolone in tapered dosage (control group), 100 mg × 3 times for first 3 days, 100 mg × 2 times for the next 3 days and 100 mg × 1 time for the last 4 days. The mean age of patients in this trial was 40.75 ± 11.73 years, 56.3% are males, rest are females, over 18–75 years of age of either sex, diagnosed with SARS-CoV-2 infection, confirmed by RT-PCR testing, having mild to moderate disease who can take oral medicines were considered eligible for randomization. The patients enrolled in the study were categorized to three different age groups as follows: young adults (18–35 years), middle aged adults (36–55 years) and older adults (above 56 years).
Outcomes
RT-PCR results of inflammatory markers compared to abnormal elevated levels of routinely tested inflammatory parameters
Gene expression of inflammatory markers IL-6, TNF-α and IL-10 (IFM) were serially analyzed on day 0, day 5 and day 10 using whole blood as the specimen (Supplementary Table 3). The expression of IFM was studied using RT-PCR. Patients with increasing trend of IFM expression were identified by examining their cycle threshold (Ct) values; patients with Ct values below 30 were considered to be in the increasing trend group, while patients with Ct values above 30 were considered to be in the decreasing trend group. An increasing trend of IL-6, TNF- α and IL-10 were seen in both groups and the trends showed equally good results.
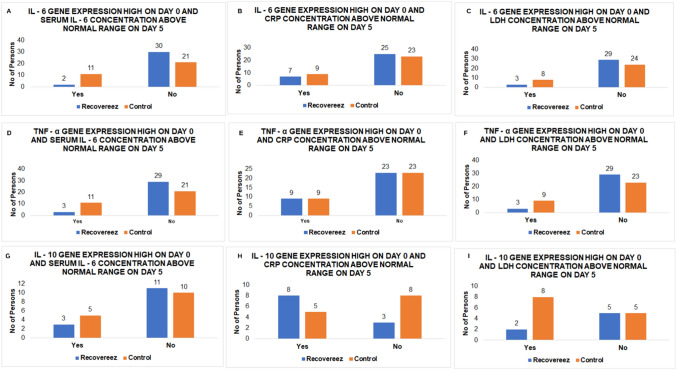
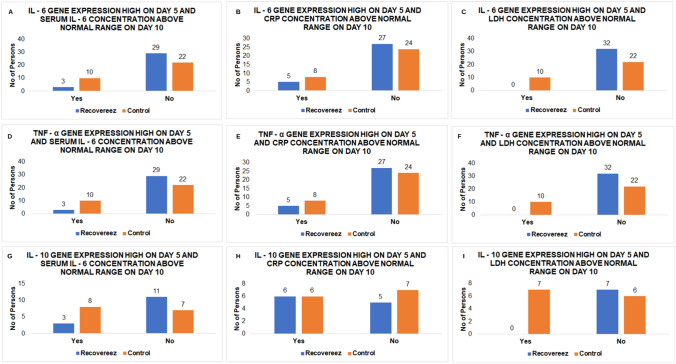
13 (20.31%) out of 64 patients showed an increasing trend of IL-6 gene on day 0 accompanied by serum IL-6 levels above normal range on day 5, out of which 2 (6.25%) and 11 (34.38%) subjects belonged to the treatment and control group, respectively (p value = 0.010) (Table 1, Fig. 1a). Thirteen (20.31%) patients’ IL-6 gene was elevated on day 5 and serum IL-6 level was above normal range on day 10. Out of the 13 patients, 3 (9.38%) patients belonged to the treatment group and 10 (31.25%) patients belonged to the control group (Table 2, Fig. 2a).This indicates that RT-PCR analysis of IL-6 gene can predict abnormal serum IL-6 levels 5 days earlier and the potential of RECOVEREEZ FORTE™ in maintaining the normal levels of serum IL-6 in majority of the patients. None of the patients had elevated IL-6 gene expressed on day 0 and serum IL-6 above normal range from day 5 to day 10 (Table 3), indicating lack of 10-day prediction ability of the RT-PCR analysis. A similar trend was also observed when IL-6 gene analyzed on day 0 was compared to CRP on day 5 (Table 1, Fig. 1b) and IL-6 gene analyzed on day 5 was compared to CRP on day 10 (Table 2, Fig. 2b). None of the patients showed an association of increased IL-6 gene expression on day 0 and above normal levels of CRP from day 5 to day 10 (Table 3). This indicates that RT-PCR analysis of IL-6 gene can predict abnormal CRP levels 5 days earlier and the potential of RECOVEREEZ FORTE™ in maintaining the normal levels of CRP in majority of the patients Elevated IL-6 gene expression on day 0 corresponded to above normal levels of LDH in 11 (17.19%) out of 64 patients on day 5, out of which 3 (9.38%) belonged to the treatment group and 8 (25%) belonged to the control group (p value = 0.001) (Table 1) (Fig. 1c). Ten (15.63%) patients in total had IL-6 gene expression high on day 5 and LDH level above normal range on day 10, out of which 10 (31.25%) belonged to the control group and none belonged to the treatment group (p value = 0.001) (Table 2) (Fig. 2c). None of the patients showed an association of increased IL-6 gene expression on day 0 and above normal levels of LDH on day 5 which further elevated from day 5 to day 10 (Table 3). Similar outcomes were also obtained when day 0 TNF-α gene and IL-10 gene were compared with serum IL-6, CRP and LDH on day 5 and day 10 (Tables 1, 2, 3, Figs. 1d–i, 2d–i). As a result, the foregoing findings clearly demonstrate the ability of IFM RT-PCR analysis to predict frequently evaluated parameters such as IL-6, CRP and LDH 5 days before aberrant levels were identified. Additionally, observations among majority of the RECOVEREEZ FORTE™ group also advocate the potentiality of RECOVEREEZ FORTE™ in maintaining normal levels of the routinely tested parameters when consumed for a period of 5 days (in the case of serum IL-6 and CRP) to 10 days (in the case of LDH), such an effect is not seen in the control group.
Table 1.
Association of elevated IFM gene expression on day 0 and above normal range of inflammatory parameters on day 5
| Treatment arm | IFM gene expression elevated on day 0 and serum concentration of inflammatory parameters above normal range on day 5 | p value | |||
|---|---|---|---|---|---|
| Yes | No | Total | |||
| IL-6 gene V/S serum IL-6 | Recovereez Forte™ | 2 (6.25%) | 30 (93.75%) | 32 | 0.010 |
| Control | 11 (34.38%) | 21 (65.62%) | 32 | ||
| IL-6 gene V/S CRP | Recovereez Forte™ | 7 (21.88%) | 25 (78.12%) | 32 | 0.773 |
| Control | 9 (28.13%) | 23 (71.87%) | 32 | ||
| IL-6 gene V/S LDH | Recovereez Forte™ | 3 (9.38%) | 29 (90.62%) | 32 | 0.001 |
| Control | 8 (25%) | 24 (75%) | 32 | ||
| TNF-α gene V/S serum IL-6 | Recovereez Forte™ | 3 (9.38%) | 29 (90.62%) | 32 | 0.031 |
| Control | 11 (34.38%) | 21 (65.62%) | 32 | ||
| TNF-α gene V/S CRP | Recovereez Forte™ | 9 (28.13%) | 23 (71.87%) | 32 | 1.000 |
| Control | 9 (28.13%) | 23 (71.87%) | 32 | ||
| TNF-α gene V/S LDH | Recovereez Forte™ | 3 (9.38%) | 29 (71%) | 32 | 0.106 |
| Control | 9 (28.13%) | 23 (71.87%) | 32 | ||
| IL-10 gene V/S serum IL6 | Recovereez Forte™ | 3 (21.43%) | 11 (21.43%) | 14 | 0.681 |
| Control | 5 (33.33%) | 10 (66.67%) | 15 | ||
| IL-10 gene V/S CRP | Recovereez Forte™ | 8 (57.14%) | 3 (42.86%) | 11 | 0.122 |
| Control | 5 (33.33%) | 8 (66.67%) | 13 | ||
| IL-10 gene V/S LDH | Recovereez Forte™ | 2 (14.29%) | 5 (85.71%) | 7 | 0.349 |
| Control | 8 (53.33%) | 5 (46.67%) | 13 | ||
Number of subjects who showed high gene expression of IL-6,TNF-α and IL-10 on day 0 and serum concentrations of IL-6 protein, CRP and LDH above normal range on day 5
Fig. 1.
Gene expression of IFM on day 0 compared to protein levels of other inflammatory parameters assessed on day 5: a Number of subjects who showed high gene expression of IL-6 on day 0 and a correlation to the serum concentrations of IL-6 protein above normal range on day 5. b Number of subjects who showed high gene expression of IL-6 on day 0 and a correlation to the serum concentrations of CRP above normal range on day 5. c Number of subjects who showed high gene expression of IL-6 on day 0 and a correlation to the serum concentrations of LDH above normal range on day 5. d Number of subjects who showed high gene expression of TNF-α on day 0 and a correlation to the serum concentrations of IL-6 protein above normal range on day 5. e Number of subjects who showed high gene expression of TNF-α on day 0 and a correlation to the serum concentrations of CRP above normal range on day 5. f Number of subjects who showed high gene expression of TNF-α on day 0 and a correlation to the serum concentrations of LDH above normal range on day 5. g Number of subjects who showed high gene expression of IL-10 on day 0 and a correlation to the serum concentrations of IL-6 protein above normal range on day 5. h Number of subjects who showed high gene expression of IL-10 on day 0 and a correlation to the serum concentrations of CRP above normal range on day 5. i Number of subjects who showed high gene expression of IL-10 on day 0 and a correlation to the serum concentrations of LDH above normal range on day 5.
Table 2.
Association of elevated IFM gene expression on day 5 and above normal range of inflammatory parameters on day 10
| IFM gene expression elevated on day 5 and serum concentration of inflammatory parameters above normal range on day 10 | p value | ||||
|---|---|---|---|---|---|
| Yes | No | Total | |||
| IL-6 gene V/S serum IL6 | Recovereez Forte™ | 3 (9.38%) | 29 (90.62%) | 32 | 0.059 |
| Control | 10 (31.25%) | 22 (68.75%) | 32 | ||
| IL-6 gene V/S CRP | Recovereez Forte™ | 5 (15.63%) | 27 (84.37%) | 32 | 0.535 |
| Control | 8 (25%) | 24 (75%) | 32 | ||
| IL-6 gene V/S LDH | Recovereez Forte™ | 0 (0%) | 32 (100%) | 32 | 0.001 |
| Control | 10 (31.25%) | 22 (68.75%) | 32 | ||
| TNFα gene V/S serum IL6 | Recovereez Forte™ | 3 (9.38%) | 29 (90.62%) | 32 | 0.059 |
| Control | 10 (31.25%) | 22 (68.75%) | 32 | ||
| TNF-α gene V/S CRP | Recovereez Forte™ | 5 (15.63%) | 27 (84.37%) | 32 | 0.535 |
| Control | 8 (25%) | 24 (75%) | 32 | ||
| TNFα gene V/S LDH | Recovereez Forte™ | 0 (0%) | 32 (100%) | 32 | 0.001 |
| Control | 10 (31.25%) | 22 (68.75%) | 32 | ||
| IL-10 gene V/S serum IL6 | Recovereez Forte™ | 3 (27.27%) | 11 (72.73%) | 14 | 0.128 |
| Control | 8 (61.54%) | 7 (38.46%) | 15 | ||
| IL-10 gene V/S CRP | Recovereez Forte™ | 6 (54.55%) | 5 (45.45%) | 11 | 1.000 |
| Control | 6 (46.15%) | 7 (53.85%) | 13 | ||
| IL-10 gene V/S LDH | Recovereez Forte™ | 0 (0%) | 7 (100%) | 7 | 0.044 |
| Control | 7 (53.85%) | 6 (46.15%) | 13 | ||
Number of subjects who showed high gene expression of IL-6,TNF-α and IL-10 on day 5 and serum concentrations of IL-6 protein, CRP and LDH above normal range on day 10
Fig. 2.
Gene expression of IFM on day 5 compared to protein levels of other inflammatory parameters assessed on day 10: a number of subjects who showed high gene expression of IL-6 on day 5 and a correlation to the serum concentrations of IL-6 protein above normal range on day 10. b Number of subjects who showed high gene expression of IL-6 on day 5 and a correlation to the serum concentrations of CRP above normal range on day 10. c Number of subjects who showed high gene expression of IL-6 on day 5 and a correlation to the serum concentrations of LDH above normal range on day 10. d Number of subjects who showed high gene expression of TNF-α on day 0 and a correlation to the serum concentrations of IL-6 protein above normal range on day 10. e Number of subjects who showed high gene expression of TNF-α on day 5 and a correlation to the serum concentrations of CRP above normal range on day 10. f Number of subjects who showed high gene expression of TNF-α on day 5 and a correlation to the serum concentrations of LDH above normal range on day 10. g Number of subjects who showed high gene expression of IL-10 on day 5 and a correlation to the serum concentrations of IL-6 protein above normal range on day 10. h Number of subjects who showed high gene expression of IL-10 on day 5 and a correlation to the serum concentrations of CRP above normal range on day 10. i Number of subjects who showed high gene expression of IL-10 on day 5 and a correlation to the serum concentrations of LDH above normal range on day 10
Table 3.
Association of IFM gene expression on day 0 and above normal range of inflammatory parameters on day 5 which further elevated from day 5 to day 10
| IFM gene expression elevated on day 0 and serum concentration of inflammatory parameters above normal range on day 5 and further elevated from day 5 to day 10 | p value | ||||
|---|---|---|---|---|---|
| Yes | No | Total | |||
| IL-6 gene V/S serum IL-6 | Recovereez Forte™ | 0 (0%) | 32 (100%) | 32 | 1.000 |
| Control | 0 (0%) | 32 (100%) | 32 | ||
| IL-6 gene V/S CRP | Recovereez Forte™ | 0 (0%) | 32 (100%) | 32 | 1.000 |
| Control | 0 (0%) | 32 (100%) | 32 | ||
| IL-6 gene V/S LDH | Recovereez Forte™ | 0 (0%) | 32 (100%) | 32 | 1.000 |
| Control | 0 (0%) | 32 (100%) | 32 | ||
| TNF-α gene V/S serum IL-6 | Recovereez Forte™ | 0 (0%) | 32 (100%) | 32 | 1.000 |
| Control | 0 (0%) | 32 (100%) | 32 | ||
| TNF-α gene V/S CRP | Recovereez Forte™ | 0 (0%) | 32 (100%) | 32 | 1.000 |
| Control | 0 (0%) | 32 (100%) | 32 | ||
| TNF-α gene V/S LDH | Recovereez Forte™ | 0 (0%) | 32 (100%) | 32 | 1.000 |
| Control | 0 (0%) | 32 (100%) | 32 | ||
| IL-10 gene V/S serum IL-6 | Recovereez Forte™ | 0 (0%) | 14 (100%) | 14 | 1.000 |
| Control | 0 (0%) | 15 (100%) | 15 | ||
| IL-10 gene V/S CRP | Recovereez Forte™ | 0 (0%) | 11 (100%) | 11 | 1.000 |
| Control | 0 (0%) | 13 (100%) | 13 | ||
| IL-10 gene V/S LDH | Recovereez Forte™ | 0 (0%) | 7 (100%) | 7 | 1.000 |
| Control | 0 (0%) | 13 (100%) | 13 | ||
Number of subjects who showed high gene expression of IL-6,TNF-α and IL-10 on day 0 and serum concentrations of IL-6 protein, CRP and LDH above normal range on day 5 and further elevated from day 5 to day 10
Symptomatology of RECOVEREEZ FORTE™ group and control group
The symptomatology of all patients belonging to the RECOVEREEZ FORTE™ group and control group is mentioned in Supplementary Table 2. The effect of the medication given in either group is tabulated in Table 4.
-
(i)
RECOVEREEZ FORTE™ group
Considering the highest number of patients who recovered from symptoms, 5 (71.43%) out of 7 (63.64%) young adults who had fever on day 0 recovered from the same on day 5. Similarly, 5 (41.67%) out of 12(66.67%) middle aged adults and 2 (66.67%) out of 3 (100%) older adults recovered from fever on day 5. 4 (40%) out of 10 (90.91%) young adults who had cough on day 0 recovered from the symptom by day 5; likewise, 7 (53.85%) out of 13 (72.22%) middle aged adults recovered from cough on day 7 and 2 (66.67%) out of 3 (100%) older age adults recovered on day 5. A similar trend was also observed in the case of patients who experienced sore throat and breathlessness.
-
(ii)
Control group
Table 4.
Relievement of symptoms in RECOVEREEZ FORTE™ group and control group
| Group | Category | Variables | Fever, n (%) | Cough, n (%) | Sore throat, n (%) | Breathlessness, n (%) |
|---|---|---|---|---|---|---|
| RECOVEREEZ FORTE™ (n = 32) | Young adults (18–35) (n = 11) | Present on day 0 | 7 (63.64%) | 10 (90.91%) | 9 (81.81%) | 8 (72.73%) |
| Absent by day 2 | 1 (14.29%) | 0 (0%) | 2 (22.22%) | 2 (25%) | ||
| Absent by day 5 | 5 (71.43%) | 4 (40%) | 4 (44.44%) | 2 (25%) | ||
| Absent by day 7 | 0 (0%) | 3 (30%) | 3 (33.33%) | 1 (12.5%) | ||
| Absent by day 10 | 1 (14.29%) | 3 (30%) | 0 (0%) | 2 (25%) | ||
| Not negative by day 10 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (12.5%) | ||
| Middle age (36–55) (n = 18) | Present on day 0 | 12 (66.67%) | 13 (72.22%) | 9 (50%) | 4 (22.22%) | |
| Absent by day 2 | 5 (41.67%) | 0 (0%) | 0 (0%) | 0 (0%) | ||
| Absent by day 5 | 5 (41.67%) | 4 (30.77%) | 3 (33.33%) | 2 (50%) | ||
| Absent by day 7 | 1 (8.33%) | 7 (53.85%) | 5 (55.56%) | 2 (50%) | ||
| Absent by day 10 | 1 (8.33%) | 1 (7.69%) | 1 (11.11%) | 0 (0%) | ||
| Not negative by day 10 | 0 (0%) | 1 (7.69%) | 0 (0%) | 0 (0%) | ||
| Old age (above 56) (n = 3) | Present on day 0 | 3 (100%) | 3 (100%) | 1 (33.33%) | 1 (33.33%) | |
| Absent by day 2 | 1 (33.33%) | 0 (0%) | 0 (0%) | 0 (0%) | ||
| Absent by day 5 | 2 (66.67%) | 2 (66.67%) | 1 (100%) | 0 (0%) | ||
| Absent by day 7 | 0 (0%) | 1 (33.33%) | 0 (0%) | 1 (100%) | ||
| Absent by day 10 | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | ||
| Not negative by day 10 | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | ||
| Control (n = 32) | Young adults (18–35) (n = 13) | Present on day 0 | 10 (76.92%) | 7 (53.85%) | 8 (61.54%) | 5 (45.45%) |
| Absent by day 2 | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | ||
| Absent by day 5 | 2 (20%) | 1 (14.29%) | 1 (12.5%) | 0 (0%) | ||
| Absent by day 7 | 5 (50%) | 2 (28.57%) | 5 (62.5%) | 3 (60%) | ||
| Absent by day 10 | 3 (30%) | 4 (57.14%) | 2 (25%) | 2 (40%) | ||
| Not negative by day 10 | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | ||
| Middle age (36–55) (n = 13) | Present on day 0 | 8 (61.54%) | 9 (69.23%) | 7 (53.84%) | 4 (22.22%) | |
| Absent by day 2 | 0 (0%) | 0 (0%) | 0 (%) | 0 (0%) | ||
| Absent by day 5 | 1 (12.5%) | 1 (11.11%) | 0 (%) | 0 (0%) | ||
| Absent by day 7 | 1 (12.5%) | 5 (55.56%) | 3 (42.86%) | 1(25%) | ||
| Absent by day 10 | 6 (75%) | 3 (33.33%) | 2 (28.57%) | 0 (0%) | ||
| Not negative by day 10 | 0 (0%) | 0 (0%) | 2 (28.57%) | 3 (75%) | ||
| Old age (above 56) (n = 6) | Present on day 0 | 6 (100%) | 4 (66.67%) | 2 (33.33%) | 2 (33.33%) | |
| Absent by day 2 | 1 (16.67%) | 0 (0%) | 0 (0%) | 0 (0%) | ||
| Absent by day 5 | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | ||
| Absent by day 7 | 3 (50%) | 2 (50%) | 0 (0%) | 1 (50%) | ||
| Absent by day 10 | 1 (16.67%) | 1 (25%) | 1 (50%) | 1 (50%) | ||
| Not negative by day 10 | 1 (16.67%) | 1 (25%) | 1 (50%) | 0 (0%) |
Number of patients who showed recovery from symptoms by day 2, 5, 7 and 10
Considering the highest number of patients who recovered from symptoms, 5 (50%) out of 10 (76.92%) young adults who had fever on day 0 recovered on day 7. Similarly, 6 (75%) out of 8 (61.54%) middle aged adults and 3 (50%) out of 6(100%) older adults recovered from fever on day 10 and day 7, respectively. Moreover, there was 1 (16.67%) out of 6(100%) older adults who failed to recover throughout the study period. 4 (57.14%) out of 7 (53.85%) young adults who had cough on day 0 recovered from the symptom by day 10; likewise, 5 (55.56%) out of 9 (69.23%) middle aged adults and 2 (50%) out of 4 (66.67%) older age adults who had cough on day 0 recovered on day 7. A similar trend was also observed in the case of patients who experienced sore throat and breathlessness. There was 1 (25%) older adult who did not recover from cough during the study period (Table 4).
A few of the older adults in the control group showed persistence in fever, cough and sore throat on day 10, whereas there was no incidence of persistence of symptoms in the RECOVEREEZ FORTE™ group. Likewise, few of the middle-aged adults in the control group did not recover from sore throat and breathlessness. In the RECOVEREEZ FORTE™ group, only 1 (7.69%) middle-aged adult did not recover from cough (Table 4).
The above observations indicate that most of the patients belonging to the RECOVEREEZ FORTE™ group recovered earlier than control group. Hence, RECOVEREEZ FORTE™ may be used for relieving symptoms earlier in COVID-19. Owing to the fact that the younger population recovered faster in both the study groups, it is important to note that the older population of the adults are recovered faster in RECOVEREEZ FORTE™ group than the control group. Thus, indicating a faster symptom relieving potential of RECOVEREEZ FORTE™ compared to prednisolone.
Assessment of SARS-CoV-2 RT-PCR results
When the numbers of patients who tested negative on day 5 in both study groups were compared, it was found that 12 (37.5%) of the 32 patients in the RECOVEREEZ FORTE™ group tested negative, whereas only 6 (18.75%) of the 32 patients in the control group tested negative on day 5 (Table 5) (Supplementary Table 1). This finding indicates the potential of RECOVEREEZ FORTE™ in addition to its role in relieving symptoms and maintenance of normal levels of IL-6, CRP and LDH.
Table 5.
Effect of treatment on SARS-CoV-2 RT-PCR results
| Group | Variables | n (%) |
|---|---|---|
| RECOVEREEZ FORTE™ (n = 32) | SARS-CoV-2 RT-PCR Ct values reduced on day 10 from day 0 | 14 (43.75%) |
| Negative by day 5 | 12 (37.5%) | |
| Negative by day 10 | 6 (18.75%) | |
| Control (n = 32) | SARS-CoV-2 RT-PCR Ct values reduced on day 10 respect to day 0 | 16 (50%) |
| Negative by day 5 | 6 (18.75%) | |
| Negative by day 10 | 5 (15.62%) | |
| SARS-CoV-2 RT-PCR Ct values increased on day 10 from day 0 | 5 (15.62%) |
The number of patients whose SARS-CoV-2 RT-PCR Ct values decreased from day 0 to day 10, increased from day 0 to day 10, and tested negative on days 5 and 10
Safety outcomes
There were no patients in the RECOVEREEZ FORTE™ group who dropped out owing to major side effects. Patients taking RECOVEREEZ FORTE™ had minor gastrointestinal side effects such as gastroesophageal reflux. There were no negative changes in vital markers (liver function, renal function, serum electrolyte) during the study (data not shown). No patients dropped out or reported side effects in the control group.
Discussion
Hypercytokinemia is an uncontrolled hyperinflammatory reaction that is predominantly seen in COVID-19 cases and generally occurs when a localized inflammatory response to a viral or bacterial infection spreads across the body. Elevated cytokine levels lead to vascular damage, endothelial dysfunction, and paracrine/metabolic dysregulation, thereby resulting in damaged multiple organ systems (Bhaskar et al. 2020; Ragab et al. 2020). TNF-α, IL-1β, IL-8 and MCP-1 rise early in hypercytokinemia, expediating a sustained increase in IL-6. Along with other pleiotropic cytokines, IL-6 steers an acute phase response and elevates serum ferritin, CRP, and other pro-coagulant factors (Bhaskar et al. 2020). Our research discovered that the RT-PCR assay used to detect inflammatory genes such as IL-6, TNF-α and IL-10 in COVID-19 patients has a good 5-day early predictability. A statistically significant association was observed in the gene expression of IFM assessed on day 0 and protein levels of other routinely tested inflammatory parameters (serum IL-6, CRP and LDH) on day 5. A similar trend was also observed when gene expression of IFM was assessed on day 5 and protein levels of other inflammatory parameters were assessed on day 10. This association suggests that RT-PCR analysis of inflammatory markers when done earlier can predict the risk of abnormal elevated levels of inflammatory parameters which would be detected 5 days later. Moreover, instead of assessing the protein markers much later, RT-PCR analysis of IFM done earlier provides a predictable and conclusive analysis of the patient’s inflammatory status and aids in providing effective treatment at the right time to alleviate health risks. RT-PCR analysis of IFM lacked 10-day early predictability as there was no association between increased IFM assessed on day 0 and elevated routinely tested inflammatory parameters on day 10. The majority of the patients who showed the above-mentioned trend belonged equally to the control and treatment group, indicating the persistent anti-inflammatory action possessed by RECOVEREEZ FORTE™ and hence it may be regarded equivalent to steroids. The consumption of RECOVEREEZ FORTE™ for a period of 5 days would be beneficial to lower the fatal inflammatory response of the body when contracted with the virus. IL-10 being a COVID-19 indicator (Huang et al. 2021; Islam et al. 2021; Dhar et al. 2021) was observed to be enhanced majorly in the control group than the treatment group, stipulating reduced chance of disease worsening in the treatment group (Supplementary Table 3). LDH being a profound routinely tested parameter indicates lung damage or injury in severe COVID-19 patients (Serrano-Lorenzo et al. 2021; Chen et al. 2020; Szarpak et al. 2020). When elevated IFM was compared with elevated LDH levels 5 days later, a majority of the patients belonging to the control group showed increased LDH levels than the treatment group. Moreover, by day 10 none of the patients belonging to the treatment group showed LDH levels that surpassed the normal range, indicating that by consuming RECOVEREEZ FORTE for a period of 10 days LDH levels would be normalized. When symptomatology of study population was analyzed, most of the patients belonging to the RECOVEREEZ FORTE™ group recovered earlier than control group. Even though the younger population recovered relatively faster in both the study groups, it is important to note that the older population of the adults recovered faster when treated with RECOVEREEZ FORTE™, thus indicating a faster symptom relieving potential of RECOVEREEZ FORTE™ compared to prednisolone. Additionally, when the number of patients who tested SARS-CoV-2 negative on day 5 in both study groups were compared, it was found that 12 (37.5%) of the 32 patients in the RECOVEREEZ FORTE™ group tested negative, whereas only 6 (18.75%) of the 32 patients in the control group tested negative on day 5 (Table 5) (Supplementary Table 1), indicating a potential role of RECOVEREEZ FORTE™ in early SARS-CoV-2 negativity. Hence, the authors suggests the use of RECOVEREEZ FORTE™ as a treatment option for effective anti-inflammatory action, relievement of symptoms and anti-viral action against SARS-CoV-2. Also, multiplex RT-PCR test targeting IL-6, TNF-α and IL-10 would aid in prognosticating inflammation and predicting the abnormality of routinely tested parameters 5 days earlier.
Conclusion
The present investigation on the RT-PCR analysis of IFM of 64 subjects proved to be successful in prognosticating inflammation. The IFM RT-PCR test possess 5-day early prediction ability and lacks 10-day prediction ability of routinely tested parameters such as IL-6, CRP and LDH. Treatment with RECOVEREEZ FORTE™ indicates good anti-inflammatory action which is equivalent to steroids. Intake of RECOVEREEZ FORTE™ for a period of 5 days depicts persistent anti-inflammatory action. Moreover, LDH levels can effectively be normalized by RECOVEREEZ FORTE™ when consumed for a period of 10 days. IL-10 being a COVID-19 severity indicator was observed to be elevated in the control group than the treatment group, indicating that the disease did not worsen upon consuming RECOVEREEZ FORTE™. Hence, early intake of RECOVEREEZ FORTE™ provides persistent anti-inflammatory action, normalizes LDH levels, mitigates COVID-19 severity, possesses faster symptom relieving action and plays role in early SARS-CoV-2 RT-PCR test negativity. Likewise, multiplex RT-PCR testing of inflammatory markers opens doors for easy prognostication of inflammation and prediction of abnormal levels of routinely tested parameters.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors thank the patients for their willingness to be part of this trial and also the treating clinicians; Dr. Ajit Mandlecha, Dr. Gous Mujawar and Dr. Aslam for their valuable contributions. The authors thank Zum Heilen Diagnostic & Therapeutics Pvt. Ltd. for the financial support in conducting this trial and for providing RECOVEREEZ FORTETM. The authors also thank the staff of Vishwanand Kendra and Shree Sai Hospital, Pune, Maharashtra India for their assistance in conducting the study.
Author contributions
PV designed the trial and was the principal investigator, with overall responsibility for conducting the trial and for medical oversight of trial implementation. NS drafted the manuscript, structured the final report and reviewed the interpreted data. AH organized and performed the data analysis. AM reviewed the interpreted data. All authors reviewed the final report. NS: writing—original draft preparation; structuring of final report; reviewing the interpreted data. PV: principal investigator; conceptualization; supervision and medical oversight of trial implementation. AM; reviewing. AH: data analysis; data organization.
Funding
This research was funded and supported by Zum Heilen Diagnostic & Therapeutics Pvt. Ltd.
Data availability
Data supporting reported results that is not given here is available on request from the corresponding author. This data is not publicly available due to privacy requirements. The datasets generated during and/or analysed during the current study are not publicly available due to privacy reasons but are available from the corresponding author on reasonable request.
Declarations
Conflict of interest
Dr. Prashanth is the Director of Zum Heilen Diagnostic & Therapeutics Pvt. Ltd. The authors have no relevant financial or non-financial interests to disclose.
Ethics approval and consent to participate (human ethics, animal ethics or plant ethics)
Prior to the study, the protocol was approved by the Orchid Specialty Hospital Ethics committee, and the trial was registered in Clinical Trials Registry India (CTRI—CTRI/2021/04/033143) in compliance with the International Council on Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use—Good Clinical Practice (ICH–GCP) guidelines. All participating patients were informed about the objectives and risks of participation and gave written informed consent. This study was approved by the Orchid Specialty Hospital Ethics committee, and the trial was registered in Clinical Trials Registry India (CTRI—CTRI/2021/04/033143) in compliance with the International Council on Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use–Good Clinical Practice (ICH–GCP) guidelines.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
All the authors mentioned in the manuscript have agreed for authorship, read and approved the manuscript, and have given consent for submission and subsequent publication of the manuscript. No images or videos of patients included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Nourin Shakeeb, Email: nourinshakeeb16@gmail.com.
Prashanth Varkey, Email: drpvarkey@gmail.com.
Aimy Hynse, Email: aimyhynse26@gmail.com.
References
- Am B, Zagorchev P, Filipova MD, Lukanov J. Effects of 1,8-cineole on the activity of cyclooxygenase and cyclooxygenase 1 and cyclooxygenase 2 isoforms. Nat Prod Chem Res. 2017 doi: 10.4172/2329-6836.1000253. [DOI] [Google Scholar]
- Aronson JK, Ferner RE. Biomarkers—a general review. Curr Protoc Pharmacol. 2017;76:9.23.1–9.23.17. doi: 10.1002/cpph.19. [DOI] [PubMed] [Google Scholar]
- Asif M, Saleem M, Saadullah M, Yaseen HS, Al Zarzour R. COVID-19 and therapy with essential oils having antiviral, anti-inflammatory, and immunomodulatory properties. Inflammopharmacology. 2020;28:1153–1161. doi: 10.1007/s10787-020-00744-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhaskar S, Sinha A, Banach M, Mittoo S, Weissert R, Kass JS, Rajagopal S, Pai AR, Kutty S. Cytokine storm in COVID-19-immunopathological mechanisms, clinical considerations, and therapeutic approaches: the REPROGRAM consortium position paper. Front Immunol. 2020;11:1648. doi: 10.3389/fimmu.2020.01648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X-Y, Huang M-Y, Xiao Z, Yang S, Chen X-Q. Lactate dehydrogenase elevations is associated with severity of COVID-19: a meta-analysis. Crit Care. 2020;24:459. doi: 10.1186/s13054-020-03161-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhar SK, Vishnupriyan K, Damodar S, Gujar S, Das M. IL-6 and IL-10 as predictors of disease severity in COVID-19 results from meta-analysis and regression. Heliyon Patients. 2021;7:e06155. doi: 10.1016/j.heliyon.2021.e06155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobler CC. Biomarkers in respiratory diseases. Breathe Sheff Engl. 2019;15:265–266. doi: 10.1183/20734735.0329-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fara A, Mitrev Z, Rosalia RA, Assas BM. Cytokine storm and COVID-19: a chronicle of pro-inflammatory cytokines. Open Biol. 2020;10:200160. doi: 10.1098/rsob.200160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu N-H, Nitsche A, Müller MA, Drosten C, Pöhlmann S. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280.e8. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horváth G, Ács K. Essential oils in the treatment of respiratory tract diseases highlighting their role in bacterial infections and their anti-inflammatory action: a review. Flavour Fragr J. 2015;30:331–341. doi: 10.1002/ffj.3252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu B, Huang S, Yin L. The cytokine storm and COVID-19. J Med Virol. 2021;93:250–256. doi: 10.1002/jmv.26232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang F, Liu X, Sun X, Li Z. IL-10 served as an indicator in severe COVID-19 patients. J Med Virol. 2021;93:1233–1235. doi: 10.1002/jmv.26580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam H, Chamberlain TC, Mui AL, Little JP. Elevated interleukin-10 levels in COVID-19: potentiation of pro-inflammatory responses or impaired anti-inflammatory action? Front Immunol. 2021;12:2485. doi: 10.3389/fimmu.2021.677008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juergens LJ, Racké K, Tuleta I, Stoeber M, Juergens UR. Anti-inflammatory effects of 1,8-cineole (eucalyptol) improve glucocorticoid effects in vitro: a novel approach of steroid-sparing add-on therapy for COPD and asthma? Synergy. 2017;5:1–8. doi: 10.1016/j.synres.2017.08.001. [DOI] [Google Scholar]
- Kumar S, Kashyap P, Chowdhury S, Kumar S, Panwar A, Kumar A. Identification of phytochemicals as potential therapeutic agents that binds to Nsp15 protein target of coronavirus (SARS-CoV-2) that are capable of inhibiting virus replication. Phytomedicine. 2021;85:153317. doi: 10.1016/j.phymed.2020.153317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayeux R. Biomarkers: potential uses and limitations. NeuroRx. 2004;1:182–188. doi: 10.1602/neurorx.1.2.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ragab D, Salah Eldin H, Taeimah M, Khattab R, Salem R. The COVID-19 cytokine storm; what we know so far. Front Immunol. 2020;11:1446. doi: 10.3389/fimmu.2020.01446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryu S, Park H, Seol GH, Choi I-Y. 1,8-Cineole ameliorates oxygen-glucose deprivation/reoxygenation-induced ischaemic injury by reducing oxidative stress in rat cortical neuron/glia. J Pharm Pharmacol. 2014;66:1818–1826. doi: 10.1111/jphp.12295. [DOI] [PubMed] [Google Scholar]
- Sengupta A, Ghosh S, Bhattacharjee S. Dietary cardamom inhibits the formation of azoxymethane-induced aberrant crypt foci in mice and reduces COX-2 and iNOS expression in the colon. Asian Pac J Cancer Prev APJCP. 2005;6:118–122. [PubMed] [Google Scholar]
- Serrano-Lorenzo P, Coya ON, López-Jimenez A, Blázquez A, Delmiro A, Lucia A, Arenas J, Martín MA, Santos-Lozano A, Cueto-Felgueroso C, Pozo AF, de Miguel-Reyes M. Plasma LDH: a specific biomarker for lung affectation in COVID-19? Pract Lab Med. 2021;25:e00226. doi: 10.1016/j.plabm.2021.e00226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siddiqi HK, Mehra MR. COVID-19 illness in native and immunosuppressed states: a clinical-therapeutic staging proposal. J Heart Lung Transplant. 2020;39:405–407. doi: 10.1016/j.healun.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szarpak L, Ruetzler K, Safiejko K, Hampel M, Pruc M, Koda, L.K.-, Filipiak, K.J., Jaguszewski, M.J., Lactate dehydrogenase level as a COVID-19 severity marker. Am J Emerg Med. 2020 doi: 10.1016/j.ajem.2020.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worth H, Schacher C, Dethlefsen U. Concomitant therapy with cineole (Eucalyptole) reduces exacerbations in COPD: a placebo-controlled double-blind trial. Respir Res. 2009;10:69. doi: 10.1186/1465-9921-10-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang W, Zhao Y, Zhang F, Wang Q, Li T, Liu Z, Wang J, Qin Y, Zhang X, Yan X, Zeng X, Zhang S. The use of anti-inflammatory drugs in the treatment of people with severe coronavirus disease 2019 (COVID-19): the perspectives of clinical immunologists from China. Clin Immunol Orlando Fla. 2020;214:108393. doi: 10.1016/j.clim.2020.108393. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data supporting reported results that is not given here is available on request from the corresponding author. This data is not publicly available due to privacy requirements. The datasets generated during and/or analysed during the current study are not publicly available due to privacy reasons but are available from the corresponding author on reasonable request.