Abstract
Workplace bullying behaviors are pervasive in some healthcare organizations leading to a difficult work environment for registered nurses. An exploratory quantitative dominant (QUANT/qual) mixed method design study was conducted to determine the differences in respondents in three midwestern states on psychological distress symptoms using WPB exposure levels and select nurse characteristics. This article identifies significant differences with perceived stress, anxiety, and posttraumatic symptoms which were reported for persons with frequent to daily WPB behavior exposure. Discussions related to significant differences found between respondents related to age and posttraumatic stress symptoms are presented. Narrative analysis on strategies used after bullying illuminated the discussion. Finally, implications related to nurse leaders and empowerment of their direct reports to resolve minor interpersonal conflicts and move swiftly to resolve escalating bullying are examined in this article.
Keywords: workplace violence, stress, anxiety, coping, retention, lateral aggression, bullying
Precis:
Workplace bullying is a problematic situation for healthcare providers and organizations. Workplace bullying can result in negative psychological outcomes for individuals and financial implications for organizations. This study examined workplace bullying exposure levels and compared them to nurse characteristics. Significant differences were found related to anxiety, perceived stress, and age and posttraumatic stress symptoms. Narrative analyses highlighted the importance of nurse leader intervention to resolve bullying behaviors in the workplace.
Organizations with cultures attenuated with workplace bullying (WPB) behaviors create stressful environments for novice nurses who are more vulnerable to that abuse (Budin, Brewer, Chao, & Kovner, 2013). WPB behaviors occur at a critical time as mentors socialize novice nurses into peer groups. These same peers and mentors are under stress themselves related to the increased workload associated with orienting novice nurses (Topa, Guglielmi, & Depolo, 2013). With these continued stressors, novice nurses may feel powerless to address WPB behaviors between peers and perceive WPB behaviors as intentionally targeted (Berry, Gillespie, Gates, & Schafer, 2012). This powerlessness may lead to psychological distress. Because of this risk, the purpose of this study was to determine the differences in perceived stress, anxiety state, and posttraumatic stress symptoms using WPB exposure levels and select nurse characteristics as well as to determine the strategies used by nurses who maintained employment on the same unit.
Background
The prevalence of WPB behaviors has been estimated to range from 27.3% to 31% for twice weekly incidents for nurses and 21.3% for daily WPB for novice nurses (Berry et al., 2012; Johnson & Rae, 2009; Simons, 2008). As occupational stressors, WPB behaviors may occur while novice nurses experience the stress and anxiety associated with learning their new role (Budin et al., 2013). In addition to stress and anxiety with the new role, WPB behaviors may lead to a sustained perceived stress and anxiety state, and subsequent risk for posttraumatic stress symptoms.
WPB Consequences
When WPB behaviors are embedded in professional peer relationships, organizational consequences occur. For example, WPB is negatively correlated to work productivity (r = −.32, p = .01; Berry et al., 2012). In response to WPB behaviors, some nurses leave the organizational unit by transferring within or exiting the organization (Vessey, Demarco, Gaffney, & Budin, 2009). Simons (2008) found a significant positive correlation between WPB and intent to leave (r = .51, p < .001). Johnson and Rae (2009) noted bullied nurses were three times more likely to express intent to leave employment. Nurses who stay on a unit attenuated with WPB behaviors may experience a loss of interest in the job (Vessey et al., 2009).
Sustained WPB behaviors are psychologically stressful related to loss of control over the situation and lack of resources for appropriate response (Duffy & Sperry, 2014). When WPB behaviors are perceived as threatening (targeted, repeated, unwanted), stress and anxiety increase. Compromised coping ability may occur through consistent negative behaviors (Lazarus & Folkman, 1984). When exposed to WPB behaviors, 90% (n=191) of nurses reported moderate to severe stress (Vessey et al., 2009).
Tehrani (2004) noted symptoms of posttraumatic stress disorder (PTSD) were present in 44% (n = 72) of care professionals exposed to chronic WPB behaviors. PTSD occurs following traumatic or life-threatening events where the reactions to events do not go away or become worse (Norris & Slone, 2013). Posttraumatic stress symptoms are experienced through feelings of hyperarousal (e.g., startling to loud noises, constantly on guard), numbing or loss of interest, and the intrusion of traumatic events through nightmares or flashbacks, or avoidance of things, persons, or situations reminding them of the trauma (National Center for PTSD, 2014).
Matthiesen and Einarsen (2004) explored posttraumatic stress symptoms among WPB targets (n = 180) from a broad range of industries. Targets who experienced WPB were found to have significant correlations (p < .01) between WPB and intrusion, avoidance, and hyperarousal (Matthiesen & Einarsen, 2004). Malik and Farooqi (2014) noted significant positive correlations between general workplace harassment and posttraumatic stress symptoms for female physicians (n = 100; r = .58, p < .01) and female nurses (n = 100; r = .52, p= <.01).
In the U.S., the prevalence for PTSD is 11.7% (Norris & Slone, 2013). Almost all humans have had exposure to traumatic events at some point in their lives. However, systematic and persistent WPB may lead to PTSD (Tehrani, 2004).
Purpose
Nurses must successfully address the WPB behaviors directed towards them to stop the internal emotional response to these behaviors (Berry et al., 2012). Likewise, healthcare organizations must address the seriousness of WPB behaviors (American Nurses Association, 2015). Additionally, the strategies nurses used to maintain employment without psychological distress symptoms are unknown in a work environment attenuated with high frequency of WPB behaviors. Therefore, the purpose of this study was to determine the differences in perceived stress, anxiety state, and posttraumatic stress symptoms based on WPB exposure levels and select nurse characteristics as well as to determine the strategies used by nurses who maintained employment on the same unit. It was hypothesized that there would be a significant difference in perceived stress, anxiety state, and posttraumatic stress symptoms between novice nurses based on WPB exposure levels.
Methods
A sequential quantitative dominant (QUANT/qual) mixed method study was conducted with nurses in three Midwestern states still employed at the same facility and unit from a prior study conducted in 2010 (Berry et al., 2012). A two-phase research design was used for this study (Creswell & Plano Clark, 2011; Morse & Niehaus, 2009). In Phase I, a quantitative web-based survey was implemented with the study sample. In Phase II, semi-structured interviews were conducted with a subset of the Phase I study sample (Figure 1). The mixing of quantitative and qualitative data occurred within the discussion to further describe emergent findings on what constitutes WPB behaviors, why WPB behaviors continue, and how these nurses continued to cope and reach out for social support as they worked through or stopped WPB in their initial position (Creswell & Plano Clark, 2011; Morse & Niehaus, 2009). University Institutional Review Board (IRB) approval was secured prior to study procedures.
Figure 1.
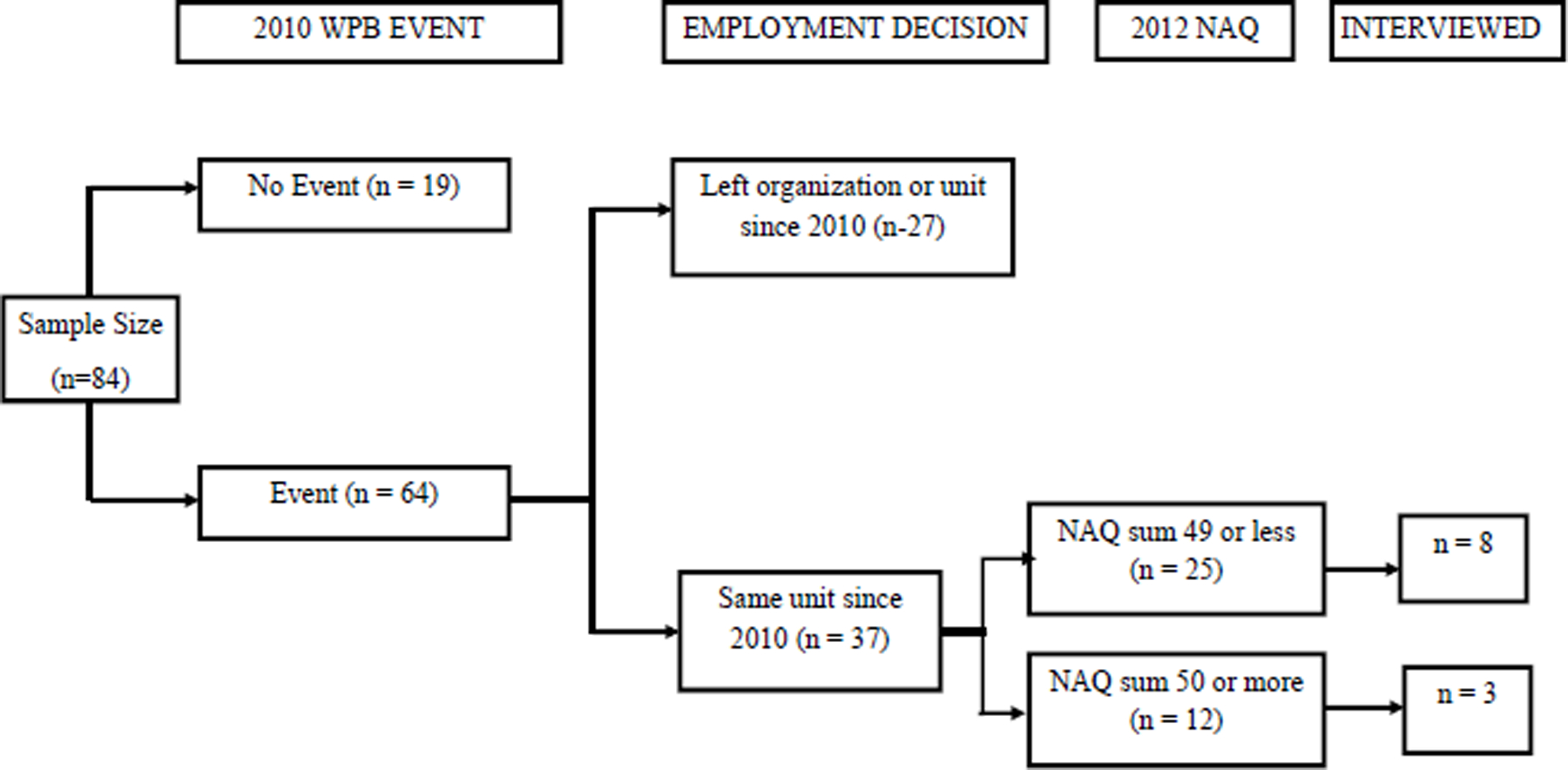
Decision Tree on Selection Process for Interview
Phase I Survey.
The study sample was obtained from a previous study of novice nurses (n = 197) in practice less than three years (Berry et al., 2012). From this previous sample, 75% of the nurses (n = 148) agreed to further contact for research when completing the first survey as approved by the original IRB. In 2012, approximately 18 months after the first survey, letter invitations were mailed with the URL link to an internet survey along with a unique study identification number. After entering the web-based survey, respondents received instructions and informed consent. Informed consent was implied by entering the survey. Of the 84 respondents who completed the study survey, 37 nurses documented a targeted or observed WPB event in the 2010 study in their first position as a novice nurse. These 37 nurses had continued their employment on the same unit at the time of the second survey (2012) and composed the analytical study sample. Demographic data from the 2010 study were used in further analysis (i.e., ethnicity, gender, age, educational attainment) along with other categorical variables (i.e., history of bullying prior to RN licensure, working on unit prior to RN licensure).
Quantitative measures.
Respondents completed a five-component survey. The first component, the Negative Acts Questionnaire (NAQ), is a 22-item inventory measuring exposure to targeted WPB behaviors over a six-month period (Einarsen et al., 2009). The NAQ uses an ordinal scale with items weighted for a six-month exposure frequency (never = 0, now and then = 2, monthly = 6, weekly = 25, and daily = 125) (Simon, 2008). Summed scores ranged from 0 – 1,302 for the sample data with a Cronbach’s alpha .89. A dichotomous categorical variable was developed by using the sum of 49 or less (infrequent WPB behaviors) and 50 or above (frequent to daily WPB behaviors). The cutoff sum of 50 or above was used based on work by Simons (2008) who determined the demarcation point to capture those respondents exposed to twice weekly WPB.
The second component, the 10-item Perceived Stress Scale, assessed perceived stress in the sample over the past month (Cohen, Kamarch, & Mermelstein, 1983). This ordinal scale (1 = “none” to 4 = “often”) has four positively stated items that were reverse coded. All items then were summed, with scores ranging from 0 – 22 for the sample data. Cronbach’s alpha was .92.
The third component was the state anxiety scale, a 20-item subscale of the State Trait Anxiety Inventory (Spielberger et al., 1976). This component measured how respondents feel “right now”. This ordinal scale (1 = “Not at all” to 4 = “Very much so”) has nine items that were reverse coded and then all items were summed. Scores ranged from 20 – 76 and Cronbach’s alpha .96.
The fourth component, the Posttraumatic Stress Disorder Checklist – Civilian Version (PCL-C), screened for posttraumatic stress symptoms (National Center for PTSD, 2010). The PCL-C is a 17-item ordinal scale (1 = “Not at all” to 4 = “Extremely”) with a total symptom severity score ranging from 17 – 57 for the study sample. Cronbach’s alpha was .95. The PCL-C has a test-retest reliability ranging from .77 to .96, strong internal consistency reliability for the subscales ranging from .85 to .87, and internal consistency of .94 for the instrument as a whole (Blake et al., 1995). A score above 30 indicates the potential for a diagnosis of posttraumatic stress disorder (Bliese, Wright, Adler, & Cabrera, 2008).
The final component was a demographic survey. The survey solicited questions about (1) prior work history on unit before RN licensure, (2) prior bullying outside of the work environment, (3) age, (4) gender, and (5) ethnicity.
Data analysis.
Data were visually screened for missing data points using the Statistical Package for the Social Sciences (PASW Statistics, version 21, SPSS, Inc., Chicago, IL). Randomly occurring missing values were controlled using SPSS Missing Values Analysis. Data were replaced with the mode for that variable when 1.8% or less of the items were missing at random (Tabachnick & Fidell, 2007). Descriptive statistics described respondent data. Mann Whitney statistics were conducted to determine differences in perceived stress, anxiety state, and posttraumatic stress symptoms based on WPB exposure levels and other nurse characteristics. A posthoc power analysis using GPower (Faul, Erdfeld, Lang, & Buchner, 2007) was performed. Sufficient power (87%) was achieved to conduct the planned analyses based on the study sample size and Mann Whitney statistic for two independent group comparisons. The resulting Cohen’s d effect size was 1.13.
Phase II Interviews
The purpose of Phase II was to qualitatively explore the strategies used by nurses who experienced or observed a WPB event, and managed in spite of, or stopped, WPB, while remaining on the same unit with their same employer. All respondents who qualified for the Phase I procedures were asked to participate in a 1:1 interview. Over a period of eight months, 11 nurses completed the interview procedures (Figure 1). Telephone interviews were facilitated by using a semi-structured interview guide. Questions inquired as to why respondents thought WPB behaviors occurred, what they did to cope after, or to stop WPB, and other actions taken to continue working on the same unit after WPB occurred.
Qualitative rigor and data analysis.
Rigor was established by building trustworthiness using Lincoln and Guba (1985) criteria. Subject matter experts assisted in development and review of the semi-structured interview guide (Lincoln & Guba, 1985). The interviews were conducted by phone, recorded digitally by the primary investigator, then transcribed verbatim by a paid transcription service. The primary author verified the accuracy of the transcripts by listening to the audio recordings, amending transcripts as needed. Verified transcripts were transferred into NVivo 8 (QSR International, Doncaster, VIC, Australia) for analysis. An audit trail was developed and maintained to document coding discussions, decisions, and dispute resolution between investigators. Lincoln and Guba (1985) state the audit trail is the “single most important trustworthiness technique” (p. 283) for maintaining the truth-value, applicability, consistency, and neutrality of the content analysis. After prolonged contact with narratives, line-by-line content analyses were conducted separately and together by investigators to code responses, and to group findings under themes. Expert member checking occurred periodically for themes and subthemes to safeguard against bias by co-investigators in managing paradigm or contract disjunctions (Lincoln & Guba, 1985). Linkages between narratives were refined into structured themes and subthemes through multiple comparisons and discussion between investigators on coping with, working through, or stopping WPB (Creswell & Plano Clark, 2011; Morse & Niehaus, 2009). The researchers used the qualitative data to make comparisons to the quantitative data for a better understanding of the psychological distress symptoms associated with the continuation of WPB behaviors in healthcare (Morse & Niehaus, 2009).
Phase I Quantitative Results
Of the 84 nurses who responded to the survey, 37 respondents met the criteria for Phase I inclusion. Respondents were mostly white (89.2%) and female (91.9%) (Table 1). The mean age was 28.8 years (S.D. 6.3), ranging from 22 to 47 years in 2010. Most respondents (n = 22, 59.5%) answered yes to being a target of WPB behaviors with 32% (n= 12) of respondents being exposed to frequent to daily WPB behaviors (Table 1).
Table 1.
Respondent Characteristics, Coping Styles, and WPB exposure (n = 37) to Interviewed (n = 11)
| Characteristics and Variables | Survey, n (%) | Interviewed, n (%) |
|---|---|---|
| Race | ||
| White | 33 (89.2) | 10 (90.9) |
| Person of color | 4 (10.8) | 1 (9.1) |
| Female | 34 (91.9) | 9 (81.9) |
| Educational Level | ||
| Associate’s | 16 (43.2) | 6 (54.5) |
| Bachelor’s | 21 (56.8) | 5 (45.5) |
| Prior History (positive history) | ||
| Bullied prior to RN licensure | 13 (35.1) | 5 (45.5) |
| Worked in facility prior to RN licensure | 13 (35.1) | 5 (45.5) |
| Target Orientation (Are you bullied?) | ||
| Never | 15 (40.5) | 4 (36.4) |
| Yes, but rarely | 15 (40.5) | 7 (63.6) |
| Yes, now and then | 5 (13.5) | 0 |
| Yes, several times a week | 2 (5.4) | 0 |
| NAQ weighed score | ||
| Infrequent exposure (0 – 49) | 25 (67.6) | 8 (72.7) |
| Frequent to daily exposure (50 or above) | 12 (32.4%) | 3 (27.3) |
The first phase of this study was to determine the differences in perceived stress, anxiety state, and posttraumatic stress symptoms based on WPB behavior exposure and other nurse characteristics (gender, education, ethnicity, age) while maintaining same unit employment. Respondents (n=12) who experienced frequent to daily WPB exposure scored significantly higher for perceived stress (Md = 11 vs. 3, U = 37.0, p < .001), anxiety state (Md = 49 vs. 32, U = 43.5, p = .001), and posttraumatic stress symptoms (Md = 37.5 vs. 21, U = 45.0, p = .001) as compared to respondents (n = 25) who experienced infrequent WPB behavior exposure. There were no differences for perceived stress or anxiety state when compared by age groups. However, there was a significant difference between respondents 30 years and older (n = 14, Md = 33) and 29 years and younger (n = 23, Md = 21) for posttraumatic stress symptoms (U = 86.5, p = .018). No differences in perceived stress, anxiety state, and posttraumatic stress symptoms were noted when comparing groups based on previous work history on the unit prior to RN licensure, history of bullying outside of work, gender, educational attainment, race, or type of social support used.
Phase II Qualitative Results
Interviewees were mostly white (90.9%) and female (81.9%) (Table 1). Half of the interviewees (n=5) maintained employment at the same facility after RN licensure. The interviewees predominantly used a problem-focused coping style when experiencing work conflict. Three interviewees experienced frequent to daily exposure to WPB behaviors (Table 1). Content analysis based on the interviewee transcripts revealed four themes: (a) Construct of Bullying, (b) Permissive Culture of Bullying, (c) The Toxic Effects of Bullying, and (d) Fostering a Positive Work Culture.
In Construct of Bullying, respondents described behaviors, incidents, and situations by peer and nurse leaders they perceived as bullying. Respondents internally questioned the behaviors of others, but never confirmed aggressors’ intentions. One respondent said, “I’ve noticed that people are really mean to her. And even – I tend to be aware of it, but sometimes, I catch myself being short with her. You know, rolling my eyes as I walk away.” Other bullying behaviors included gossiping, broken confidences by nurse leaders, screaming or verbal abuse, “eating their young”, equal opportunity bullying (picking on everyone), tough love, sink or swim, and refusal to assist when asked. Organizational practices considered bullying occurred when perceived as unfair, such as mandatory overtime, no breaks related to patient acuity, or down time away from the unit.
In a Permissive Culture of Bullying, the negative actions, attitudes, or interactions created an environment that enabled, ignored, or rewarded WPB behaviors. Respondents believed nurse leaders and human resources representatives minimized WPB behaviors through a sincere lack of recognition, ignoring, or minimizing their complaints. Perpetrators targeted newer, less experienced employees in general, where the “low man on the totem pole” created an easier target. One respondent stated of an aggressor “…she targets newer nurses and I think she targets less experienced nurses…”
The Toxic Effects of Bullying represented the personal reactions to perceived WPB behaviors. Suppressing emotions, blocking and refocusing on the work, and rationalizing the stressful environment helped respondents to work through WPB behaviors and continue patient care. However, six of 11 respondents were making plans to leave, from applying for licensure in a different state to applying to other facilities. Leaving was difficult for one respondent:
“I will be [leaving] just as soon as I get, as soon as I close on my house, which will be any week now. I have already started applying for other jobs. I haven’t gotten calls yet but I have started looking and kind of preparing myself mentally because as I said before, I do care about my residents. They’re- I’ve actually did clinical at this facility when I was in nursing school so I guess I’ve gotten attached to them. They’re like my friends and family so I’ve been preparing myself mentally that eventually I will be leaving and it might be months down the road but I definitely will be going.”
In Fostering a Positive Work Culture, all respondents provided excerpts on their sources and quality of support. Family support provided an avenue for venting but onsite peer support provided interventions ranging from immediate support by nurses who experienced the same bullying, being listened to by nurses considered friends, and other nurses expressing the behaviors were not only targeted at respondents but also directed towards others. Strategies on confronting aggressors were not always professional. Respondents were told to “fight back” or call the perpetrator “stupid.” However, being prepared for disruptive physicians, being a “team player,” or “buddying up” inside the facility were offered as strategies to maintaining employment and decreasing stressful encounters. Rituals, prayer, music, and maintaining close relationships with the work group or patients helped to refocus respondents who continued to be targets of WPB behaviors.
Discussion
Of the nurses (n = 64) who documented WPB events in the 2010 study, 27 nurses did not remain on their unit, representing 40% attrition in 18 months. In addition, half of the nurses (n=6) interviewed were actively looking for other positions or making plans to leave. WPB behaviors continued to be pervasive at the peer level in some healthcare organizations. Unaddressed interpersonal WPB behaviors leading an employee to terminate employment potentially can cost healthcare organizations $22,000 to $64,000 per replacement (Robert Wood Johnson Foundation, 2009), posing a significant burden to the financial viability of any healthcare facility. If a large facility with 1,000 RNs lost 40% of its staff yearly to WPB behaviors, estimated replacement costs would be between $8.8 and $25.6 million annually. Although WPB is not the only reason attrition takes place, six out of the eleven nurses interviewed were already looking for positions elsewhere.
A significant finding was that WPB exposure was linked to stress, anxiety, and posttraumatic stress symptoms unrelated to gender, race, educational attainment, prior history of being bullied, or work history on the unit prior to RN licensure. One explanation might be that nurses internalizing the emotions rather than confront the more senior peers because their concerns about WPB behaviors were minimized by peers and nurse leaders. Respondents expressed the futility in reporting WPB behaviors. In addition, respondents were encouraged by their senior peers to use verbal abuse to stop the perpetrator. If these victimized nurses adopted the same level of negative behaviors exhibited by coworkers, WPB behaviors can become normalized (Hutchinson et al., 2010). Brotheridge, Lee, and Power (2012) found targets responded to aggression by using aggression and required help to stop the aggression constructively. However, emotions and stress with confrontation made targets perceive their confrontation as ineffective (Brotheridge et al., 2012).
Of those nurses remaining on the unit, 32.4% were exposed to WPB behaviors at least twice weekly with almost 60% feeling targeted and unable to defend themselves. Researchers studying stressful nursing practice endorse problem-focused (proactive coping) as more effective when managing stress from trauma care (Gillespie & Gates, 2013) and patient aggression (Gillespie, Gates, Miller, & Howard, 2010). Use of emotion-focused coping style (e.g., humor, prayer, voicing negative feelings, blaming oneself) may reduce the negative emotional responses to stressful situations, and may be more useful to those needing to accept the reality of that which they cannot change (Lazarus, 1999). Music, prayer, and maintaining close relationships with coworkers and patients helped to distract respondents from WPB behaviors and refocus on patient care. In terms of coping strategies used with peer work conflict, those interviewed avoided the perpetrators and suppressed emotions to focus on patient care.
Nurses need to be empowered with clear professional expectations to stop conflict or WPB behaviors, or ask for help (St-Pierre. 2012). Targets and other employee bystanders need to be educated to speak up when other nurses act inappropriately, unacceptably, or hurtfully. Nurse leaders must coach novice nurses on professionally addressing WPB behaviors. When witnessing WPB behaviors, nurse leaders must intervene and coach perpetrators to stop the WPB behaviors that make an unhealthy work environment (St-Pierre, 2012).
Respondents 30 years or older had a higher median score for posttraumatic stress symptoms. Recovery from any critical incident, trauma, or threat, may take weeks or months but any nurse exposed to continued, accumulating, and adverse WPB behaviors may develop or exacerbate prior posttraumatic stress symptoms (de Boer, Lok, van’t Verlaat, Duivenvoorden, Bakker, & Smit, 2001). Healthcare professionals also may underestimate the effect of these stressors on their ability to function effectively (deBoer et al., 2001). Taking care of oneself emotionally is essential before posttraumatic stress symptoms impede the nurse’s ability to perform. Employee Assistance Programs may provide some benefit to these employees.
Teamwork is essential in the complex arena of healthcare to help the next group of new employees (Baker, Day, & Salas, 2006). One respondent validated this conclusion by expressing a desire to protect the next group of novice nurses coming into their unit. In addition, respondents gave several proactive steps for working with perpetrators: finding a “buddy to work with”, “knowing the needs” of disruptive physicians, and preparing for difficult persons.
This study was limited by a small sample size. Although adequate power was achieved for the quantitative analyses, the findings are not representative of how all nurses would respond to WPB behaviors. In addition, nurses experiencing severe WPB behaviors may have experienced discomfort and opted not to participate. The study also depended on self-reports of the respondents, potentially creating response bias.
Conclusions
No nurse is immune to psychological distress of prolonged WPB behaviors, whether directed towards them or others. Nurse leaders need to empower their direct reports to resolve minor intraprofessional conflicts but also must move swiftly to resolve escalating conflict and WPB when novice nurses are ineffective at defending themselves. When confronted with work conflict and WPB behaviors, seasoned and new nurses need to mindfully consider their stress triggers when responding to perpetrators. All healthcare professionals and the organizations where they work need to collaborate to create a safe and healthy work environment. Healthcare organizations should implement business practices and education that promote healthcare employees’ physical and psychological safety, health, and wellbeing. Future research should focus on target, observer, and nurse leader empowerment and self-advocacy to create and maintain safe, professional working environments to prevent further victimization and attrition from healthcare.
Acknowledgement:
The study was funded by the American Nurses Foundation as a 2011 National Nursing Staff Development Organization/ANF Scholar.
Biography
Peggy Ann Berry, MSN, RN, COHN-S, SPHR is a doctoral candidate at the University of Cincinnati, a NIOSH Education and Resource Grant recipient and American Nurses Foundation Scholar. She is a past Graduate Nurse Intern to OSHA, Malcolm Baldrige Examiner, and a Founding Fellow with the U. S. Academy of Workplace Bullying, Mobbing, and Abuse.
Dr. Gordon L. Gillespie, Ph.D., research focuses on the prevention of workplace violence in healthcare settings. During his 17 years of professional nursing experience, he responded to countless incidents of patients, visitors, and coworkers involved in violent altercations. During this tenure, he became cognizant of how the lack of effective communication and the general work environment contributed to acts of violence.
Dr. Bonnie S. Fisher received her PhD in political science from Northwestern University in 1988. She served three years on the faculty of the department of city and regional planning at the Ohio State University before joining the faculty at UC in 1991. Dr. Fisher was the principal investigator for four federally funded research projects involving the victimization of college students, the sexual victimization of college women, violence against college women, and campus-level responses to a report of sexual assault.
Dr. Denise Gormley, Ph.D. is an Assistant Professor and Executive Director of the Graduate MSN Program at the College of Nursing. Her teaching expertise is in the specialty of nursing administration and her research interests are in organizational influences on nurse worker turnover, retention, productivity, and patient safety.
Mr. Jared Haynes, MS is a biostatistician with the Aeromedical Consultation Service for Wright Patterson Air Force Base.
Contributor Information
Peggy Ann Berry, University of Cincinnati.
Dr. Gordon L. Gillespie, University of Cincinnati
Dr. Bonnie S. Fisher, University of Cincinnati.
Dr. Denise Gormley, University of Cincinnati
Mr. Jared Haynes, Aeromedical Consultation Service for Wright Patterson Air Force Base.
References
- American Nurses Association, (2015). American Nurses Association Position Statement on Incivility, Bullying, and Workplace Violence Retrieved from http://nursingworld.org/DocumentVault/Position-Statements/Practice/Position-Statement-on-Incivility-Bullying-and-Workplace-Violence.pdf
- Baker DP, Day R, & Salas E (2006). Teamwork as an essential component of high-reliability organizations. Health Services Research: Impacting Health Practice and Policy Through State-of-Art Research and Thinking, 41(4 Pt 2), 1576–1598. doi: 10.1111/j.1475-6773.2006.00566.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry PA, Gillespie GL, Gates D, & Schafer J (2012). Novice nurse productivity after workplace bullying. Journal of Nursing Scholarship, 44(1), 80–87. doi: 10.1111/j.1547-5069.2011.01436.x [DOI] [PubMed] [Google Scholar]
- Blake DB, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, & Keane TM (1995). The development of a clinician-administered PTSD scale. Journal of Traumatic Stress, 8(1), 75–90. doi: 0894-9867/95/0100-0075507.50/1 [DOI] [PubMed] [Google Scholar]
- Bliese PD, Wright KM, Adler AB, Cabrera O, Castro CA, & Hoge CW (2008). Validating the primary care Postraumatic Stress Disorder Screen and Posttraumatic Stress Disorder Checklist with soldiers returning from combat. Journal of Consulting and Clinical Psychology, 76(2), 272–281. doi: 10.1037/0022-006x.76.2.272 [DOI] [PubMed] [Google Scholar]
- Brotheridge CM, Lee RT, & Power JL (2012). Am I my own worst enemy? The experiences of bullying targets who are also aggressors. Career Development International, 17(4), 358–374. doi: 10.1108/13620431211255833 [DOI] [Google Scholar]
- Budin WC, Brewer CS, Chao Y-Y &, Kovner C (2013). Verbal abuse from nurse colleagues and work environment of early career Registered Nurses. Journal of Nursing Scholarship, 45(3), 308–316. doi: 10.1111/jnu.12033 [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarch T, & Mermelstein R (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396. [PubMed] [Google Scholar]
- Creswell JW, & Plano Clark VL (2011). Designing and conducting mixed methods research Thousand Oaks, CA: SAGE Publications [Google Scholar]
- deBoer J, Lok A, van’t Verlaat E, Duivenvoorden HJ, Bakker AB, & Smit BJ (2011). Work-related critical incidents in hospital-based health care providers and the risk of post-traumatic stress symptoms, anxiety, and depression: A meta-analysis. Social Science & Medicine, 73, 316–326. doi: 10.1016/j.socscimed.2011.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffy M, & Sperry L (2014). Overcoming mobbing: A recovery guide for workplace aggression and bullying Oxford, NY: Oxford University Press. [Google Scholar]
- Einarsen S, Hoel H, & Notelaers G (2009). Measuring exposure to bullying and harassment at work: Validity, factor structure and psychometric properties of the Negative Acts Questionnaire-Revised. Work & Stress, 23(1), 24–44. doi: 10.1080/02678370902815673 [DOI] [Google Scholar]
- Faul F, Erdfeld E, Lang A-G, & Buchner A (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39, 175–191. doi: 10.3758/BRM.4149 [DOI] [PubMed] [Google Scholar]
- Gillespie GL, & Gates DM (2013). Using proactive coping to manage the stress of trauma patient care. Journal of Trauma Care, 20(1), 44–50. doi: 10.1097/JTN.0b013e18286608e [DOI] [PubMed] [Google Scholar]
- Gillespie GL, Gates DM, Miller M, Howard PK (2010). Workplace violence in healthcare settings: Risk factors and protective strategies. Rehabilitation Nursing 35(5), 177–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchinson M, Wilkes L, Jackson D, & Vickers MH (2010). Integrating individual, work group and organizational factors: Testing a multidimensional model of bullying in the nursing workplace. Journal of Nursing Management, 18, 173–181. [DOI] [PubMed] [Google Scholar]
- Johnson SL, & Rea RE (2009). Workplace bullying: Concerns for nurse leaders. The Journal of Nursing Administration, 39(2), 84–90. [DOI] [PubMed] [Google Scholar]
- Lazarus RS (1999). Stress and emotion: A new synthesis New York, NY: Springer Publishing Company. [Google Scholar]
- Lazarus RS, & Folkman S (1984). Stress, appraisal, and coping New York, NY: Springer Publishing Company. [Google Scholar]
- Lincoln YS, & Guba EG (1985). Naturalistic inquiry Newbury Park, CA: Sage Publications [Google Scholar]
- Malik S, & Farooqi YN (2014). General and sexual harassment as predictors of posttraumatic stress symptoms among female health professionals. World Journal of Medical Sciences, 10 (1), 43–49. doi: 10.5829/idosi.wjms.2014.10.1.81128 [DOI] [Google Scholar]
- Matthiesen SB, & Einarsen S (2004). Psychiatric distress and symptoms of PTSD among victims of bullying at work. British Journal of Guidance & Counselling, 32(3), 335–356. doi: 10:1080/03069880410001723558 [Google Scholar]
- Morse JM, & Niehaus L (2009). Mixed Method Design: Principles and Procedures Walnut Creek, CA: Left Coast Press [Google Scholar]
- National Center for PTSD (2014). DSM-5 Criteria for PTSD Retrieved from http://www.ptsd.va.gov/professional/PTSD-overview/dsm5_criteria_ptsd.asp
- Norris FH, & Slone LB (2013). Understanding research on epidemiology of trauma and PTSD. PTSD Research Quarterly: Advancing Science and Promoting Understanding of Traumatic Stress, 24(2–3). [Google Scholar]
- Simons S (2008). Workplace bullying experienced by Massachusetts registered nurses and the relationship to intention to leave the organization. Advance in Nursing Science, 32(2), E48–E59. [DOI] [PubMed] [Google Scholar]
- St-Pierre I (2012). How nursing managers respond to intraprofessional aggression: Novel strategies to an ongoing challenge. The Health Care Manager, 31(3), 247–258. doi: 10.1097.HCM,0b013e3182619e4f [DOI] [PubMed] [Google Scholar]
- Robert Wood Johnson Foundation (2009). Business case/cost of nurse turnover Retrieved from: http://www.rwjf.org/en/research-publications/find-rwjf-research/2009/07/wisdom-at-work-retaining-experienced-nurses/business-case-cost-of-nurse-turnover.html
- Tabachnick BG, & Fidell LS (2007). Cleaning up your act: Screening data prior to analysis. In Tabachnick BG & Fidell LS (Eds.), Using multivariate statistics (pp. 60–116). Boston, MA: Pearson Education, Inc. [Google Scholar]
- Tehrani N (2004). Bullying: A source of chronic posttraumatic stress. British Journal of Guidance & Counselling, 32(3), 357–366. [Google Scholar]
- Topa G, Guglielmi D, & Depolo M (2004). Mentoring and group identification as antecedents of satisfaction and health among nurses: What role do bullying experiences play? Nurse Education Today, 34, 507–512. doi: 10/1016/j.nedt.2013.07.006 [DOI] [PubMed] [Google Scholar]
- Vessey J, Demarco R, Gaffney D, & Budin W (2009). Bullying of staff registered nurses in the workplace: A preliminary study for developing personal and organizational strategies for the transformation of hostile to healthy workplace environments. Journal of Professional Nursing, 25(5): 299–306. doi: 10.1016/j.profnurs.2009.01.022 [DOI] [PubMed] [Google Scholar]


