Abstract
Cancer stem cell (CSC) refers to cancer cells with stem cell properties, that is, they have the ability of “self-renewal” and “differentiation.” Cancer stem cells exist in cancer cells and are the “culprit” of cancer recurrence and metastasis. It is difficult to be found because of its small amount, and it is difficult for anticancer drugs to produce effects on it. At present, the isolation and identification of cancer stem cells from many solid tumors are still quite difficult, mainly due to the lack of specific molecular markers of cancer stem cells. In this review, cancer stem cell surface markers and functional markers in urinary system were summarized. These markers can provide molecular targets for cancer therapy.
1. Introduction
Great progress has been made in the treatment of cancer; however, the treatment is even less ideal [1]. In addition to local operation, the traditional radiotherapy and chemotherapy can hardly cure urinary carcinoma [2]. The increasingly recognized complexity of human cancers and the heterogeneity of malignant tumor cells have posed a major challenge to the development of effective therapies in urinary carcinoma [3]. A small group of stem cell-like tumor cells has been found in tumor tissue [4]. The cells have the potential of self-renewal, unlimited proliferation, and multidirectional differentiation [4]. Although the number is small, they play an important role in tumor formation, recurrence, and metastasis [5]. These cells are called cancer stem cells or tumor-initiating cells [6]. Cancer stem cells have their own characteristics: (1) self-renewal ability: cancer stem cells are produced by symmetric division to complete self-replication; (2) differentiation potential: generation of tumor cells with different degrees of differentiation through asymmetric division; (3) heterogeneity: functional heterogeneity among cancer stem cells [6].
The discovery of cancer stem cells has undoubtedly opened up a new way to better understand tumor biology and explore new methods for cancer treatment. However, until now, no one knows which cells are cancer stem cells. The cells which have stem cell features can be separated and purified by flow cytometry (FACS) and magnetic-activated cell sorting (MACS) by surface markers and functional markers [7]. Among these markers, which are the specific markers of urologic oncology stem cells are still controversial. In this paper, we will review the widely studied and newly discovered tumor markers in urologic oncology stem cells, so as to provide targets for the radical treatment of urologic oncology.
2. Prostate Cancer
Prostatic epithelial cells which consist of two layers of epithelial cells, basal cells, glandular epithelial cells, and neuroendocrine cells are a complex tissue in structure and function [8]. In addition, there is a small group of special types of cells with self-renewal ability and differentiation potential, so they are called “prostate stem cells” [8]. The cells express cytokeratin 5 and 19 (CK5, CK19), androgen receptor (AR), prostate-specific antigen (PSA), and prostatic acid phosphatase (PAP) [8]. The origin of prostate cancer stem cells is still controversial. Prostate cancer stem cells are derived from normal stem cells, transient expanded epithelial cells, or terminal differentiated coelomocytes [9]. Prostate cancer stem cell markers can provide targets for the treatment of prostate cancer [10]. At present, some prostate cancer stem cell markers such as CD44 and CD133 have been widely studied (Figure 1). Some new markers have been found, such as integrin α2, α6, β1, c-Met, aldehyde dehydrogenase 1 (ALDH1), ABCG2, CD166, Sox2, and EZH2 (Figure 1).
Figure 1.
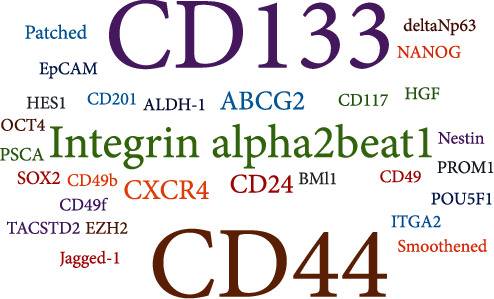
Word cloud: visualization of the surface markers for prostate cancer.
2.1. CD44
CD44, a cell surface protein, plays a role in cell adhesion and signal transduction [11]. It has been identified as a surface marker for prostate cancer stem cells [12]. CD44+ cells obtained from prostate transplantation tumor have tumorigenicity, clonogenic capacity, and metastatic potential [13]. CD44+ cells from LnCAP, PC3, and DU145 cells have stronger proliferation and tumorigenesis than CD44− cells [14]. The genes related to the proliferation, regeneration, and differentiation of stem cells, such as Sox2, OCT3/4, SMO, and β-catenin, were highly expressed in CD44+ prostate cancer cell [15].
2.2. CD133
CD133 is a glycoprotein with five transmembrane domains, which is expressed in different types of stem cells and endothelial progenitor cells [16]. CD133 has been used to isolate cancer stem cells in many cancer types, including prostate cancer [17]. CD133+ cells derived from prostate cancer tissue showed more proliferative and aggressive than CD133− cells [18]. These cells have similar phenotype with normal prostate stem cells [18]. Both CD133+ prostate cancer stem cells and normal prostate stem cells express basal cell markers, but not androgen receptors (AR) [18]. In addition, the tumorigenicity of CD133+ cells from DU145 cells was similar to that of CD133− ones [18]. Based on these evidences, CD133 may be a not suitable stem cell marker for prostate cancer. Interestingly, CD44+/α2β1hi/CD133+ prostate cancer cells have self-renewal ability and can differentiate into prostate cells that can express AR and PAP [19]. In the case of doubts about CD133, more specific prostate cancer stem cell markers need to be used with CD133 to target prostate cancer stem cells.
2.3. Aldehyde Dehydrogenase 1 (ALDH1)
ALDH1, expressed widely in normal tissues, has been used as a functional marker for cancer stem cells [20–22]. It can convert aldehydes into carboxylic acids and participate in the degradation of intracellular toxic substances and cell protection [23]. Compared with normal prostate tissues, ALDH1 expressed higher in prostate cancer tissues [24, 25]. High expressed ALDH1 level was associated with the higher Gleason score, the higher the pathological grade, and the lower overall survival rate of prostate cancer patients [24, 25]. ALDH1high murine prostate stem cells have high proliferation potential in vitro and more effective in generating prostatic tissue in vivo [26]. ALDH1 may act as detoxification enzymes to protect stem cells from toxic compounds [27]. If ALDH1 can be effectively inhibited, prostate cancer stem cells will not escape the attack of traditional chemoradiotherapy.
2.4. ATP Binding Membrane Transporter (ABCG2)
ABCG2 is an ATP binding membrane transporter, which can pump antitumor drugs out of cancer cells and protect the cells from killing [28]. ABCG2 is also associated with multidrug resistance of prostate cancer [29]. The cells, enriched by ABCG2, were called side population (SP) cells [29]. SP cells have the characteristics of cancer stem cells, such as drug resistance [30]. ABCG2+/AR+ prostate cancer stem cells can survive under castration, chemotherapy, and hypoxia environment [31]. So, ABCG2 can be used as a functional marker to target prostate cancer stem cells. However, Patrawala et al. [32] found that ABCG2+ cells and ABCG2− cells from DU145 cells have similar tumorigenicity. Some ABCG2− DU145 cells also have the ability to generate ABCG2+ ones [32]. ABCG2-mediated androgen efflux decreased the nuclear AR expression and induced cell growth in HPr-1-AR (nontumorigenic) and CWR-R1 (tumorigenic) prostate cell lines [31]. It seems that ABCG2 as a specific marker of prostate cancer stem cells is still controversial. However, all this evidence indicated that ABCG2 maintains the characteristics of AR+ prostate cancer stem cells.
2.5. Integrin α2β1
Integrin is a kind of collagen receptor or extracellular matrix protein, which plays an important role in cell survival, proliferation, and metastasis [33]. The growth and metastasis of prostate cancer were closely related to the expression of integrin [34]. Goel et al. [35] found that most α and β integrins were out of control in prostate cancer. The expression of α2 in lymph node metastasis was higher than that in primary tumor [35]. β1 expressed higher in the high tumor grade [35]. Both prostate cancer cells and prostate cancer stem cells express high levels of Integrin α2β1 [36]. DU145 and PC3 cells with docetaxel treatment expressed significantly higher α2β1 levels than untreated ones [36, 37]. α2β1high DU145 and PC3 cells were more invasive than α2β1low ones [36, 37].
2.6. CXCR4
CXCR4 is a GPCR (G-protein coupled receptor) composed of 352 amino acids and has seven transmembrane structures [38]. CXCR4 is mainly expressed in embryonic stem cells, hematopoietic stem cells, endothelial stem cells, and other pluripotent stem cells [39]. CXCR4 is involved in a variety of physiological mechanisms in vivo, including HIV-1 virus infection [40], hematopoietic function [41], embryonic development [42], and tumor migration [43]. CXCR4 is a specific receptor for chemokine stromal cell-derived factor-1 (CXCL12) [44]. In our previous study, we confirmed the CXCR4/CXCL12 axis regulates self-renew, differentiation, and tumorigenicity of DU145 and PC3 cells [45]. CXCR4 and CD133 coexpressed in prostate epithelial cells and cancer cells of patients specimens [46]. CXCR4 induced a more aggressive phenotype in prostate cancer [47].
2.7. Sox2, EZH2, and Oct4
Both sex-determining region Y-box 2 (Sox2) and enhancer of zeste homolog 2 (EZH2) play important roles in the development of human embryonic stem cells [48, 49]. Sox2 is a transcription factor, which plays a key role in maintaining the self-renewal and undifferentiated state of embryonic stem cells [48]. EZH2 is necessary for the in vitro reconstruction of embryonic stem cells and plays a key role in embryonic formation [49]. Sox2 and EZH2 also play a key role in prostate cancer stem cells (PCSCs). Ugolkov et al. [50] found that EZH2 and Sox2 were closely related in prostate cancer, and almost 90% Sox2+ prostate cancer was EZH2+ type by immunohistochemistry and tissue microarray. Oct4, also referred to as POUF51 and Oct3/4, works synergistically with Sox2 for maintaining pluripotency of cells [51]. Although Sox2, EZH2, and Oct4 are not used as prostate cancer stem cell markers, more and more studies confirmed the regulatory roles of these genes in PCSC. EZH2 was upregulated in PCSCs compared with non-PCSCs [52]. A recent study in our group showed that inhibition of EZH2-mediated histone methylation improves the radiotherapy for PCSC [53]. Sox2 regulates self-renewal and anchorage-independent growth of DU145 spheres depending on EGFR expression [54]. Sox2/Oct4 overexpression in PCSCs contributes to tumor initiation and progression [55]. Sox2/Oct4 positive cells that isolated from prostate cancer tissues have the stem cell properties [55].
3. Bladder Cancer
The basal cell layer of normal bladder epithelium contains undifferentiated cells [56]. These cells move to the surface of bladder cavity gradually and complete the differentiation in this process [56]. In view of the this reason, many studies on bladder cancer stem cells focus on bladder regenerative basal cell layer. CD44, CD133, and other markers are expressed in both the basal cell layer and bladder cancer stem cells (Figure 2).
Figure 2.
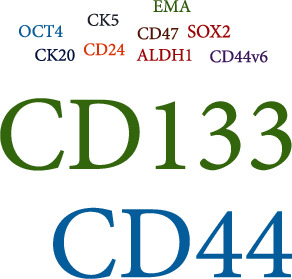
Word cloud: visualization of the surface markers for bladder cancer.
3.1. CD44
McKenney et al. [57] found CD44+ cells in the basal cell layer of normal urothelial epithelium and urothelial carcinoma. Chan et al. [58] isolated and identified a subpopulation of primary bladder cancer cells based on CD44+, CK5+, and CK20− and further confirmed that this subpopulation can induce tumorigenesis in nude mice. In addition, the tumorigenicity of CD44+ cells was 10-200 times higher than that of CD44− ones from nude mice [58]. In bladder cancer tissue, epithelial membrane antigen (EMA) negative CD44 variant subtype (CD44v6) positive cells account for about 30% of cancer cells [59]. These cells have a higher self-renewal ability compared with parental tumors cells [59]. Therefore, tumor initiation ability of CD44+ cells is confirmed, and CD44 can be used as a sorting marker of bladder cancer stem cells (BCSCs).
3.2. CD133
Zhu et al. [60] demonstrated that CD133 was highly expressed in mouse bladder cancer cells (MCSCs) by flow cytometry (FACS) and quantitative PCR. Bentivegna et al. [61] isolated CD133+ cells by immunofluorescence analysis and cytogenetic analysis in 49 samples of bladder cancer tissues. The cells were identified as BCSCs by transplantation in nude mice [61]. Huang et al. [62] demonstrated the stem cell-like characteristics of CD133+ subpopulation of human bladder cancer cell J82. All this evidence showed that CD133 can also be used as surface markers for sorting BCSCs.
3.3. CD47
CD47, also known as integrin-associated protein (IAP), exists on the cell surface and belongs to the transmembrane glycoprotein of immunoglobulin superfamily [63]. The expression of CD47 is related to tumor immunity and prognosis [64]. CD47 is widely expressed in bladder cancer cells [65], however, expressed higher in BCSCs than other cancer cells [66]. CD47 could bind to the macrophage surface receptor SIRPα and block macrophage phagocytosis [67]. CD47 may be a target for bladder cancer immunotherapy and a BCSC marker.
3.4. ALDH1A1
ALDH1A1 is a member of aldehyde dehydrogenase gene families [68]. ALDH1A1+ bladder cancer cells had higher tumorigenicity than ALDH1A1− cancer cells both in vivo and in vitro [69, 70]. The ALDH1A1+ bladder cancer cells can represent CSCs in bladder cancer. Bladder cancer patients with the high expression of ALDH1A1 were significantly associated with poor prognosis [71].
3.5. Cytokeratin
Cytokeratin (CK) is a major skeletal protein, which exists in keratinocytes of epithelial cells [72]. The expression of CK reflects cell differentiation and can be used as a common tumor diagnostic marker [73]. As mentioned above, CD44+CK5+CK20− bladder cancer cells were BCSCs; CK20 was not expressed in these cells [58]. CK17 exists in urothelial basal cells and has strong tumorigenicity [74]. He et al. [74] confirmed that CK17+/CK18−/CK20− could be used for isolation and identification BCSCs. CK20, CK17, and CK18 may be considered as markers related to BCSCs.
3.6. Oct3/4
OCT4 is a key regulator of tumor progression, aggressive behavior, and metastasis of bladder cancer [75]. Atlasi et al. [76] found that bladder transitional cell carcinoma with high Oct3/4 expression has faster tumor progression and shorter tumor-related survival time than superficial bladder transitional cell carcinoma with medium and low expression of Oct3/4. It maintains self-renewal and differentiation of bladder cancer cells [76]. Bentivegna et al. [61] isolated BCSCs with high expression of Oct4 from the tissues of patients with bladder cancer and proved the stem cell-like properties of these cells. Oct4 may lead to tumorigenesis and is closely related to the treatment resistance or recurrence of bladder cancer [61].
4. Renal Carcinoma
Compared with other urological tumors, the research of renal cancer stem cells is later [77]. Although some markers have been studied (Figure 3), whether these markers can be used as specific surface markers for identification of renal cancer stem cells still needs to be confirmed in subsequent experiments.
Figure 3.
Word cloud: visualization of the surface markers for renal carcinoma.
4.1. CD133
CD133+ renal adult stem cells in human renal cortex have proliferation and self-renewal ability and can differentiate into renal tubular epithelial cells and vascular endothelial cells [78]. CD24+CD133+ epithelial cells isolated from glomerular capsule have the potential to differentiate into osteocytes, adipocytes, and nerve cells in vitro and can induce the formation of renal tubular structure in vivo [79]. CD133+ cells were involved in the formation of new blood vessels in renal cell carcinoma, but it is not clear whether these markers can be used to isolate and identify renal cancer stem cells [80].
4.2. CXCR4
CXCR4 is an important marker of renal cell carcinoma stem cells [81]. The number of renal cancer stem cells and the expression of CXCR4 increased with the increase of malignancy of RCC [81]. The cancer cells isolated from patients with stage IV renal carcinoma (RCC) had more obvious characteristics of tumor stem cells than those from patients with stage I RCC [81]. CXCR4 was expressed in both types of cells [79]. In the experiment of tumor formation, stage IV RCC cells were more likely to form tumors than stage I RCC cells [81]. Compared with other markers, CXCR4 is considered to be the most reliable stem cell marker of RCC.
5. Summary
Cancer stem cell theory brings a revolutionary change to cancer research. It has promoted the exploration of biological characteristics and molecular mechanism of cancer cells and provided a new clear and reliable direction for the understanding of the origin and the clinical treatment of cancer. The research of urological cancer stem cells started relatively late, facing great opportunities and challenges. If the specific surface markers of cancer stem cells can be identified, drugs targeting cancer stem cells will also be developed and applied, and the cure of cancer will not be just a dream in people's hearts.
Acknowledgments
This review was supported by the National Natural Science Foundation of China (grant no. 81972784).
Conflicts of Interest
The authors declared no potential conflicts of interest with respect to the authorship and publication of this article
References
- 1.Siegel R. L., Miller K. D., Jemal A. Cancer statistics, 2020. CA: a Cancer Journal for Clinicians . 2020;70(1):7–30. doi: 10.3322/caac.21590. [DOI] [PubMed] [Google Scholar]
- 2.Anghel R. M., Gales L. N., Trifanescu O. G. Outcome of urinary bladder cancer after combined therapies. Journal of Medicine and Life . 2016;9(1):95–100. [PMC free article] [PubMed] [Google Scholar]
- 3.Barth I., Schneider U., Grimm T., et al. Progression of urothelial carcinoma in situ of the urinary bladder: a switch from luminal to basal phenotype and related therapeutic implications. Virchows Archiv . 2018;472(5):749–758. doi: 10.1007/s00428-018-2354-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eun K., Ham S. W., Kim H. Cancer stem cell heterogeneity: origin and new perspectives on CSC targeting. BMB Reports . 2017;50(3):117–125. doi: 10.5483/BMBRep.2017.50.3.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ye X., Weinberg R. A. Epithelial-mesenchymal plasticity: a central regulator of cancer progression. Trends in Cell Biology . 2015;25(11):675–686. doi: 10.1016/j.tcb.2015.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kreso A., Dick J. E. Evolution of the cancer stem cell model. Cell Stem Cell . 2014;14(3):275–291. doi: 10.1016/j.stem.2014.02.006. [DOI] [PubMed] [Google Scholar]
- 7.Weil B. D., Jenkins M. J., Uddin S., et al. An integrated experimental and economic evaluation of cell therapy affinity purification technologies. Regenerative Medicine . 2017;12(4):397–417. doi: 10.2217/rme-2016-0156. [DOI] [PubMed] [Google Scholar]
- 8.Karthaus W. R., Hofree M., Choi D., et al. Regenerative potential of prostate luminal cells revealed by single-cell analysis. Science . 2020;368(6490):497–505. doi: 10.1126/science.aay0267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Flynn L., Barr M. P., Baird A. M., et al. Prostate cancer-derived holoclones: a novel and effective model for evaluating cancer stemness. Scientific Reports . 2020;10(1, article 11329) doi: 10.1038/s41598-020-68187-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu Q., Gu J., Zhang E., He L., Yuan Z. X. Targeted delivery of therapeutics to urological cancer stem cells. Current Pharmaceutical Design . 2020;26(17):2038–2056. doi: 10.2174/1381612826666200403131514. [DOI] [PubMed] [Google Scholar]
- 11.Ponta H., Wainwright D., Herrlich P. Molecules in focus the CD44 protein family. The International Journal of Biochemistry & Cell Biology . 1998;30(3):299–305. doi: 10.1016/S1357-2725(97)00152-0. [DOI] [PubMed] [Google Scholar]
- 12.Chen F., Chen X., Ren Y., et al. Radiation-induced glucocorticoid receptor promotes CD44+ prostate cancer stem cell growth through activation of SGK1-Wnt/β-catenin signaling. Journal of Molecular Medicine . 2019;97(8):1169–1182. doi: 10.1007/s00109-019-01807-8. [DOI] [PubMed] [Google Scholar]
- 13.Patrawala L., Calhoun T., Schneider-Broussard R., et al. Highly purified CD44+ prostate cancer cells from xenograft human tumors are enriched in tumorigenic and metastatic progenitor cells. Oncogene . 2006;25(12):1696–1708. doi: 10.1038/sj.onc.1209327. [DOI] [PubMed] [Google Scholar]
- 14.Zhang L., Jiao M., Li L., et al. Tumorspheres derived from prostate cancer cells possess chemoresistant and cancer stem cell properties. Journal of Cancer Research and Clinical Oncology . 2012;138(4):675–686. doi: 10.1007/s00432-011-1146-2. [DOI] [PubMed] [Google Scholar]
- 15.van Leenders G. J., Schalken J. A. Stem cell differentiation within the human prostate epithelium: implications for prostate carcinogenesis. BJU International . 2001;88(Suppl 2):35–42. doi: 10.1046/j.1464-410X.2001.00117.x. [DOI] [PubMed] [Google Scholar]
- 16.Yu Y., Flint A., Dvorin E. L., Bischoff J. AC133-2, a Novel Isoform of Human AC133 Stem Cell Antigen∗. The Journal of Biological Chemistry . 2002;277(23):20711–20716. doi: 10.1074/jbc.M202349200. [DOI] [PubMed] [Google Scholar]
- 17.Kanwal R., Shukla S., Walker E., Gupta S. Acquisition of tumorigenic potential and therapeutic resistance in CD133+ subpopulation of prostate cancer cells exhibiting stem-cell like characteristics. Cancer Letters . 2018;430:25–33. doi: 10.1016/j.canlet.2018.05.014. [DOI] [PubMed] [Google Scholar]
- 18.Collins A. T., Berry P. A., Hyde C., Stower M. J., Maitland N. J. Prospective identification of tumorigenic prostate cancer stem cells. Cancer Research . 2005;65(23):10946–10951. doi: 10.1158/0008-5472.CAN-05-2018. [DOI] [PubMed] [Google Scholar]
- 19.Pfeiffer M. J., Schalken J. A. Stem cell characteristics in prostate cancer cell lines. European Urology . 2010;57(2):246–255. doi: 10.1016/j.eururo.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 20.Islam F., Gopalan V., Lam A. K. Detention and identification of cancer stem cells in esophageal squamous cell carcinoma. Methods in Molecular Biology . 2020;2129:177–191. doi: 10.1007/978-1-0716-0377-2_14. [DOI] [PubMed] [Google Scholar]
- 21.Ma S., Hirata T., Arakawa T., et al. Expression of ALDH1A isozymes in human endometrium with and without endometriosis and in ovarian endometrioma. Reproductive Sciences . 2020;27(1):443–452. doi: 10.1007/s43032-019-00041-4. [DOI] [PubMed] [Google Scholar]
- 22.Savelieva O. E., Tashireva L. A., Kaigorodova E. V., et al. Heterogeneity of stemlike circulating tumor cells in invasive breast cancer. International Journal of Molecular Sciences . 2020;21(8):p. 2780. doi: 10.3390/ijms21082780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Visus C., Ito D., Amoscato A., et al. Identification of human aldehyde dehydrogenase 1 family member A1 as a novel CD8+ T-cell-defined tumor antigen in squamous cell carcinoma of the head and neck. Cancer Research . 2007;67(21):10538–10545. doi: 10.1158/0008-5472.CAN-07-1346. [DOI] [PubMed] [Google Scholar]
- 24.Li T., Su Y., Mei Y., et al. ALDH1A1 is a marker for malignant prostate stem cells and predictor of prostate cancer patients' outcome. Laboratory Investigation . 2010;90(2):234–244. doi: 10.1038/labinvest.2009.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kalantari E., Saadi F. H., Asgari M., Shariftabrizi A., Roudi R., Madjd Z. Increased expression of ALDH1A1 in prostate cancer is correlated with tumor aggressiveness: a tissue microarray study of Iranian patients. Applied Immunohistochemistry & Molecular Morphology . 2017;25(8):592–598. doi: 10.1097/PAI.0000000000000343. [DOI] [PubMed] [Google Scholar]
- 26.Lukacs R. U., Goldstein A. S., Lawson D. A., Cheng D., Witte O. N. Isolation, cultivation and characterization of adult murine prostate stem cells. Nature Protocols . 2010;5(4):702–713. doi: 10.1038/nprot.2010.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhao L., Qiu T., Jiang D., et al. SGCE promotes breast cancer stem cells by stabilizing EGFR. Advanced Science . 2020;7(14, article 1903700) doi: 10.1002/advs.201903700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gupta S. K., Singh P., Ali V., Verma M. Role of membrane-embedded drug efflux ABC transporters in the cancer chemotherapy. Oncology Reviews . 2020;14(2):p. 448. doi: 10.4081/oncol.2020.448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Guzel E., Karatas O. F., Duz M. B., Solak M., Ittmann M., Ozen M. Differential expression of stem cell markers and ABCG2 in recurrent prostate cancer. The Prostate . 2014;74(15):1498–1505. doi: 10.1002/pros.22867. [DOI] [PubMed] [Google Scholar]
- 30.Nanayakkara A. K., Follit C. A., Chen G., Williams N. S., Vogel P. D., Wise J. G. Targeted inhibitors of P-glycoprotein increase chemotherapeutic-induced mortality of multidrug resistant tumor cells. Scientific Reports . 2018;8(1):p. 967. doi: 10.1038/s41598-018-19325-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sabnis N. G., Miller A., Titus M. A., Huss W. J. The efflux transporter ABCG2 maintains prostate stem cells. Molecular Cancer Research . 2017;15(2):128–140. doi: 10.1158/1541-7786.MCR-16-0270-T. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Patrawala L., Calhoun T., Schneider-Broussard R., Zhou J., Claypool K., Tang D. G. Side population is enriched in tumorigenic, stem-like cancer cells, whereas ABCG2+ and ABCG2- cancer cells are similarly tumorigenic. Cancer Research . 2005;65(14):6207–6219. doi: 10.1158/0008-5472.CAN-05-0592. [DOI] [PubMed] [Google Scholar]
- 33.Margraf A., Germena G., Drexler H. C. A., et al. The integrin-linked kinase is required for chemokine-triggered high-affinity conformation of the neutrophil β2-integrin LFA-1. Blood . 2020;136(19):2200–2205. doi: 10.1182/blood.2020004948. [DOI] [PubMed] [Google Scholar]
- 34.Kwon O. Y., Ryu S., Choi J. K., Lee S. H. Smilax glabra Roxb. inhibits collagen induced adhesion and migration of PC3 and LNCaP prostate cancer cells through the inhibition of beta 1 integrin expression. Molecules . 2020;25(13):p. 3006. doi: 10.3390/molecules25133006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Goel H. L., Sayeed A., Breen M., et al. β1 integrins mediate resistance to ionizing radiation in vivo by inhibiting c-Jun amino terminal kinase 1. Journal of Cellular Physiology . 2013;228(7):1601–1609. doi: 10.1002/jcp.24323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ojalill M., Parikainen M., Rappu P., et al. Integrin α2β1 decelerates proliferation, but promotes survival and invasion of prostate cancer cells. Oncotarget . 2018;9(65):32435–32447. doi: 10.18632/oncotarget.25945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ryu S., Park K. M., Lee S. H. Gleditsia sinensis thorn attenuates the collagen-based migration of PC3 prostate cancer cells through the suppression of α2β1 integrin expression. International Journal of Molecular Sciences . 2016;17(3):p. 328. doi: 10.3390/ijms17030328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Raman D., Baugher P. J., Thu Y. M., Richmond A. Role of chemokines in tumor growth. Cancer Letters . 2007;256(2):137–165. doi: 10.1016/j.canlet.2007.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wojakowski W., Kucia M., Zuba-Surma E., et al. Very small embryonic-like stem cells in cardiovascular repair. Pharmacology & Therapeutics . 2011;129(1):21–28. doi: 10.1016/j.pharmthera.2010.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Doranz B. J., Grovit-Ferbas K., Sharron M. P., et al. A small-molecule inhibitor directed against the chemokine receptor CXCR4 prevents its use as an HIV-1 coreceptor. The Journal of Experimental Medicine . 1997;186(8):1395–1400. doi: 10.1084/jem.186.8.1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rettig M. P., Ansstas G., DiPersio J. F. Mobilization of hematopoietic stem and progenitor cells using inhibitors of CXCR4 and VLA-4. Leukemia . 2012;26(1):34–53. doi: 10.1038/leu.2011.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chang G. Q., Collier A. D., Karatayev O., Gulati G., Boorgu D. S. S. K., Leibowitz S. F. Moderate prenatal ethanol exposure stimulates CXCL12/CXCR4 chemokine system in radial glia progenitor cells in hypothalamic neuroepithelium and peptide neurons in lateral hypothalamus of the embryo and postnatal offspring. Alcoholism, Clinical and Experimental Research . 2020;44(4):866–879. doi: 10.1111/acer.14296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zu R., Fang X., Lin Y., et al. Peptide-enabled receptor-binding-quantum dots for enhanced detection and migration inhibition of cancer cells. Journal of Biomaterials Science Polymer Edition . 2020;31(12):1604–1621. doi: 10.1080/09205063.2020.1764191. [DOI] [PubMed] [Google Scholar]
- 44.Young B., Purcell C., Kuang Y. Q., Charette N., Dupré D. J. Superoxide dismutase 1 regulation of CXCR4-mediated signaling in prostate cancer cells is dependent on cellular oxidative state. Cellular Physiology and Biochemistry . 2015;37(6):2071–2084. doi: 10.1159/000438566. [DOI] [PubMed] [Google Scholar]
- 45.Dubrovska A., Elliott J., Salamone R. J., et al. CXCR4 expression in prostate cancer progenitor cells. PLoS One . 2012;7(2, article e31226) doi: 10.1371/journal.pone.0031226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Miki J., Furusato B., Li H., et al. Identification of putative stem cell markers, CD133 and CXCR4, in hTERT-immortalized primary nonmalignant and malignant tumor-derived human prostate epithelial cell lines and in prostate cancer specimens. Cancer Research . 2007;67(7):3153–3161. doi: 10.1158/0008-5472.CAN-06-4429. [DOI] [PubMed] [Google Scholar]
- 47.Darash-Yahana M., Pikarsky E., Abramovitch R., et al. Role of high expression levels of CXCR4 in tumor growth, vascularization, and metastasis. The FASEB Journal . 2004;18(11):1240–1242. doi: 10.1096/fj.03-0935fje. [DOI] [PubMed] [Google Scholar]
- 48.García-Caballero L., Caneiro J., Gándara M., et al. Merkel cells of human oral mucosa express the pluripotent stem cell transcription factor Sox 2. Histology and Histopathology . 2020;35(9):1007–1012. doi: 10.14670/HH-18-231. [DOI] [PubMed] [Google Scholar]
- 49.Collinson A., Collier A. J., Morgan N. P., et al. Deletion of the polycomb-group protein EZH2 leads to compromised self-renewal and differentiation defects in human embryonic stem cells. Cell Reports . 2016;17(10):2700–2714. doi: 10.1016/j.celrep.2016.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ugolkov A. V., Eisengart L. J., Luan C., Yang X. J. Expression analysis of putative stem cell markers in human benign and malignant prostate. The Prostate . 2011;71(1):18–25. doi: 10.1002/pros.21217. [DOI] [PubMed] [Google Scholar]
- 51.Malik V., Glaser L. V., Zimmer D., et al. Pluripotency reprogramming by competent and incompetent POU factors uncovers temporal dependency for Oct4 and Sox2. Nature Communications . 2019;10(1):p. 3477. doi: 10.1038/s41467-019-11054-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Li K., Liu C., Zhou B., et al. Role of EZH2 in the growth of prostate cancer stem cells isolated from LNCaP cells. International Journal of Molecular Sciences . 2013;14(6):11981–11993. doi: 10.3390/ijms140611981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gorodetska I., Lukiyanchuk V., Peitzsch C., Kozeretska I., Dubrovska A. BRCA1 and EZH2 cooperate in regulation of prostate cancer stem cell phenotype. International Journal of Cancer . 2019;145(11):2974–2985. doi: 10.1002/ijc.32323. [DOI] [PubMed] [Google Scholar]
- 54.Rybak A. P., Tang D. SOX2 plays a critical role in EGFR-mediated self-renewal of human prostate cancer stem-like cells. Cellular Signalling . 2013;25(12):2734–2742. doi: 10.1016/j.cellsig.2013.08.041. [DOI] [PubMed] [Google Scholar]
- 55.Vaddi P. K., Stamnes M. A., Cao H., Chen S. Elimination of SOX2/OCT4-associated prostate cancer stem cells blocks tumor development and enhances therapeutic response. Cancers . 2019;11(9):p. 1331. doi: 10.3390/cancers11091331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fossa S. D., Kaalhus O. Kerngroße und Chromatinkonzentration in den Übergangsepithelien des menschlichen Harnblasenkarzinoms. Beiträge zur Pathologie . 1976;157(2):109–125. doi: 10.1016/S0005-8165(76)80098-4. [DOI] [PubMed] [Google Scholar]
- 57.McKenney J. K., Desai S., Cohen C., Amin M. B. Discriminatory immunohistochemical staining of urothelial carcinoma in situ and non-neoplastic urothelium. The American Journal of Surgical Pathology . 2001;25(8):1074–1078. doi: 10.1097/00000478-200108000-00013. [DOI] [PubMed] [Google Scholar]
- 58.Chan K. S., Espinosa I., Chao M., et al. Identification, molecular characterization, clinical prognosis, and therapeutic targeting of human bladder tumor-initiating cells. Proceedings of the National Academy of Sciences of the United States of America . 2009;106(33):14016–14021. doi: 10.1073/pnas.0906549106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yang Y. M., Chang J. W. Bladder cancer initiating cells (BCICs) are among EMA-CD44v6+ subset: novel methods for isolating undetermined cancer stem (initiating) cells. Cancer Investigation . 2008;26(7):725–733. doi: 10.1080/07357900801941845. [DOI] [PubMed] [Google Scholar]
- 60.Zhu Y. T., Lei C. Y., Luo Y., et al. A modified method for isolation of bladder cancer stem cells from a MB49 murine cell line. BMC Urology . 2013;13(1):p. ???. doi: 10.1186/1471-2490-13-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bentivegna A., Conconi D., Panzeri E., et al. Biological heterogeneity of putative bladder cancer stem-like cell populations from human bladder transitional cell carcinoma samples. Cancer Science . 2010;101(2):416–424. doi: 10.1111/j.1349-7006.2009.01414.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Huang P., Watanabe M., Kaku H., et al. Cancer stem cell-like characteristics of a CD133(+) subpopulation in the J82 human bladder cancer cell line. Molecular and Clinical Oncology . 2013;1(1):180–184. doi: 10.3892/mco.2012.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Han X., Sterling H., Chen Y., et al. CD47, a ligand for the macrophage fusion receptor, participates in macrophage multinucleation∗. The Journal of Biological Chemistry . 2000;275(48):37984–37992. doi: 10.1074/jbc.M002334200. [DOI] [PubMed] [Google Scholar]
- 64.Gao L., Chen K., Gao Q., Wang X., Sun J., Yang Y. G. CD47 deficiency in tumor stroma promotes tumor progression by enhancing angiogenesis. Oncotarget . 2017;8(14):22406–22413. doi: 10.18632/oncotarget.9899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Shahan T. A., Ziaie Z., Pasco S., et al. Identification of CD47/integrin-associated protein and alpha (v)beta 3 as two receptors for the alpha 3 (IV) chain of type IV collagen on tumor cells. Cancer Research . 1999;59(18):4584–4590. [PubMed] [Google Scholar]
- 66.Chan K. S., Volkmer J. P., Weissman I. Cancer stem cells in bladder cancer: a revisited and evolving concept. Current Opinion in Urology . 2010;20(5):393–397. doi: 10.1097/MOU.0b013e32833cc9df. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hazama D., Yin Y., Murata Y., et al. Macrocyclic peptide-mediated blockade of the CD47-SIRPα interaction as a potential cancer immunotherapy. Cell Chemical Biology . 2020;27(9):1181–1191.e7. doi: 10.1016/j.chembiol.2020.06.008. [DOI] [PubMed] [Google Scholar]
- 68.Black W., Vasiliou V. The aldehyde dehydrogenase gene superfamily resource center. Human Genomics . 2009;4(2):136–142. doi: 10.1186/1479-7364-4-2-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Su Y., Qiu Q., Zhang X., et al. Aldehyde dehydrogenase 1 A1-positive cell population is enriched in tumor-initiating cells and associated with progression of bladder cancer. Cancer Epidemiology, Biomarkers & Prevention . 2010;19(2):327–337. doi: 10.1158/1055-9965.EPI-09-0865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zhao A. Y., Dai Y. J., Lian J. F., et al. YAP regulates ALDH1A1 expression and stem cell property of bladder cancer cells. Oncotargets and Therapy . 2018;Volume 11:6657–6663. doi: 10.2147/OTT.S170858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Xu N., Shao M. M., Zhang H. T., et al. Aldehyde dehydrogenase 1 (ALDH1) expression is associated with a poor prognosis of bladder cancer. Cancer Epidemiology . 2015;39(3):375–381. doi: 10.1016/j.canep.2015.03.003. [DOI] [PubMed] [Google Scholar]
- 72.Thiery J. P., Sleeman J. P. Complex networks orchestrate epithelial-mesenchymal transitions. Nature Reviews Molecular Cell Biology . 2006;7(2):131–142. doi: 10.1038/nrm1835. [DOI] [PubMed] [Google Scholar]
- 73.Shousha H. I., Fouad R., Elbaz T. M., et al. Predictors of recurrence and survival of hepatocellular carcinoma: a prospective study including transient elastography and cancer stem cell markers. Arab Journal of Gastroenterology . 2020;21(2):95–101. doi: 10.1016/j.ajg.2020.04.002. [DOI] [PubMed] [Google Scholar]
- 74.He X., Marchionni L., Hansel D. E., et al. Differentiation of a highly tumorigenic basal cell compartment in urothelial carcinoma. Stem Cells . 2009;27(7):1487–1495. doi: 10.1002/stem.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sedaghat S., Gheytanchi E., Asgari M., Roudi R., Keymoosi H., Madjd Z. Expression of cancer stem cell markers OCT4 and CD133 in transitional cell carcinomas. Applied Immunohistochemistry & Molecular Morphology . 2017;25(3):196–202. doi: 10.1097/PAI.0000000000000291. [DOI] [PubMed] [Google Scholar]
- 76.Atlasi Y., Mowla S. J., Ziaee S. A., Bahrami A. R. OCT-4, an embryonic stem cell marker, is highly expressed in bladder cancer. International Journal of Cancer . 2007;120(7):1598–1602. doi: 10.1002/ijc.22508. [DOI] [PubMed] [Google Scholar]
- 77.Saeednejad Zanjani L., Madjd Z., Rasti A., et al. Spheroid-derived cells from renal adenocarcinoma have low telomerase activity and high stem-like and invasive characteristics. Frontiers in Oncology . 2019;9:p. 1302. doi: 10.3389/fonc.2019.01302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bussolati B., Bruno S., Grange C., et al. Isolation of renal progenitor cells from adult human kidney. The American Journal of Pathology . 2005;166(2):545–555. doi: 10.1016/S0002-9440(10)62276-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sagrinati C., Netti G. S., Mazzinghi B., et al. Isolation and characterization of multipotent progenitor cells from the Bowman's capsule of adult human kidneys. Journal of the American Society of Nephrology . 2006;17(9):2443–2456. doi: 10.1681/ASN.2006010089. [DOI] [PubMed] [Google Scholar]
- 80.Bruno S., Bussolati B., Grange C., et al. CD133+ renal progenitor cells contribute to tumor angiogenesis. The American Journal of Pathology . 2006;169(6):2223–2235. doi: 10.2353/ajpath.2006.060498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gassenmaier M., Chen D., Buchner A., et al. CXC chemokine receptor 4 is essential for maintenance of renal cell carcinoma-initiating cells and predicts metastasis. Stem Cells . 2013;31(8):1467–1476. doi: 10.1002/stem.1407. [DOI] [PubMed] [Google Scholar]


