ABSTRACT
Successful mentoring relationships allow mentees to gain the confidence and knowledge they need to reach their goals, but students from populations generally underrepresented in science and health fields have been shown to receive less mentorship than their well-represented peers. In highly competitive processes, like medical school admissions, mentoring may be particularly valuable. We investigated the prior mentoring experiences of medical students and whether their perceptions of mentoring differed based on their mentoring goals or demographics (race/ethnicity, gender identity, household income, or parental highest level of education) through surveys and interviews of medical students from three different institutions. These medical students had widely participated in mentoring, though student race and household income impacted their access to medical professionals to serve as informal mentors. Medical students shared the same gender identity as their mentor more often than would be expected under the null hypothesis. Students reported having both career and psychosocial goals for mentoring, and there was a positive association between the strength of the mentees’ goals for mentoring and the number of formal mentors the mentees had. These respondents viewed mentoring as having provided them with both career and psychosocial benefits. Mentoring programs for aspiring medical students may benefit from focusing on both career and psychosocial functions to maximize the benefits of mentoring for students from diverse backgrounds.
KEYWORDS: mentoring, premedical students, mentoring goals, demographic characteristics, mentor, higher education, STEMM, mentor availability, underrepresented students, equity and diversity, gender identity
INTRODUCTION
Mentoring is complex, and the debate for a universal definition for the role and function of a mentor is ongoing. In 1991, Jacobi (1) identified 15 different definitions across disciplines, and between 1990 and 2007 over 50 different definitions were created to define mentoring (2). The consensus in the literature is that mentorship should be beneficial for the personal and career growth of both the mentor and the mentee (3, 4).
Both career support (career guidance, networking, sponsorship) and psychosocial support (emotional support, confidence boosting, role modeling) are necessary for an effective mentoring relationship (5–7). The mentee can have both career and psychosocial goals when entering a mentoring relationship; career goals prepare them for career advancement opportunities while psychosocial goals can provide them with a sense of confidence and competence (8). Successful mentoring relationships allow mentees to clearly define their career goals, the skills they need to achieve those goals, and take the steps needed to make progress toward those goals (9). As a result, an effective mentor would support the mentee’s development by helping them gain the confidence and knowledge they need to reach their educational and career goals.
The benefits of mentoring are expected to extend beyond individuals to the broader STEMM (Science, Technology, Engineering, Mathematics, and Medicine) community by developing a more diverse talent pool and increasing access, equity, and inclusion (9). Studies researching positive outcomes of mentorship have shown that undergraduate mentored research experiences in STEMM are particularly beneficial for underrepresented (UR) students (10, 11). Additionally, undergraduate mentored research for UR students may promote a sense of fit with the scientific community (12, 13).
Mentoring can be either formal or informal. Formal mentorship is where a designated mentor and mentee are assigned to one another, usually with organizational assistance or intervention (14). In contrast, informal mentorship develops spontaneously based on the mentor’s and the mentee’s mutual interest and interpersonal comfort (15). Research on formal and informal mentoring relationships indicate that both forms of mentoring can be beneficial to the mentor and the mentee. A case study by Griffin et al. (16) showed that graduate students benefit from the support from formal relationships with advisors and dissertation committee members, as well as from informal relationships with peers and relatives. Members of UR groups, however, often have less access to the benefits of informal mentoring mentorships (9). Both formal and informal mentorship can happen through a variety of configurations, including one-on-one or group mentorship (17, 18).
Participation in mentoring relationships
A wide range of students participate in mentoring relationships, including undergraduate, graduate, and medical students. Undergraduate students’ participation in mentored research experiences have been linked to greater retention in STEMM, and mentees’ perception of mentoring effectiveness is a good prediction of enrollment in science-related doctoral programs. Graduate students who have positive mentoring relationships are more likely to persist in their academic programs and are more likely to publish their research than their counterparts who have not been mentored (9).
Despite the positive effects of mentorship, access to mentoring has been shown to disproportionately favor some demographic and socioeconomic groups over others. For example, studies have reported that students from UR groups in STEMM degree programs typically receive less mentorship than their well-represented peers (19–22). Milkman et al. (23) propose that negative stereotypes may affect women and minorities receiving mentorship during their academic journey by limiting their access to mentoring and impacting the student’s experience during mentoring. Common negative stereotypes have been shown to impact black students (24), Hispanic students (25), Asian students (26), and females (27). Thus, these groups may not have access to the same level of career and psychosocial support that students from well-represented groups have.
Research aims
In this research study, we investigate how medical students perceive their prior mentoring experiences and whether those perceptions differ based on their mentoring goals or demographic characteristics. We focus on medical students because their insight on their mentoring experiences would be beneficial for students interested in pursuing a career in medicine. We asked four research questions. 1) How much exposure to mentoring (formal, informal, group) have the students had, and does that vary with student demographics? 2) What types of mentors did the students have? 3) What goals did students have for mentoring and what benefits did they perceive from it? 4) Was there a correlation between the strength of the goals the students had when entering mentoring and the benefits they perceived from it or the number of mentors they had?
This study advances the research on effective mentoring in higher education, specifically for populations interested in medicine. Medical students are the study population because their insights about prior mentoring relationships may be beneficial for students interested in entering medical school. Vast numbers of students enter their undergraduate degrees with the goal of attending medical school after graduation, yet only a small percentage will be successful. Thus, understanding the mentoring experiences of those successful few students could be instructive for programs designed to assist students with medical school ambitions.
METHODS
This study was conducted using a mixed methods approach, collecting both quantitative data with a survey and qualitative data through interviews. The goal of the survey was to investigate the association between students’ demographic characteristics (race/ethnicity, gender identity, household income, parental highest level of education) as well as their mentoring goals, mentoring experiences, and perceived benefits (psychosocial guidance or career guidance) of these experiences. The interviews provided context to the survey results. East Carolina University’s Institutional Review Board approved this research (UMCIRB 20–001704). Medical students from three institutions participated in this research: East Carolina University (ECU)’s Brody School of Medicine, Wake Forest School of Medicine, and University of North Carolina (UNC) at Chapel Hill School of Medicine.
Survey
The survey was created for use in this study and contained demographic questions as well as questions about students’ formal and informal mentoring experiences (Appendix 1). Check point items such as “click yes if you are paying attention” and “select strongly disagree for this question” were added throughout the survey to ensure the validity of students’ answers. In addition to the original questions written for this study, the survey included 16 validated items from Tepper et al. (28) to determine the mentees’ goals and perceived benefits. The items from Tepper et al. (28) are on a 5-point Likert scale from “strongly agree” to “strongly disagree” and four questions were reverse-coded. The items represented four different subscales (psychosocial and career perceived benefits, and psychosocial and career mentoring goals). These items were validated previously through confirmatory factor analysis in which all the factor loadings were statistically significant (P < 0.01), meaning that the items are significantly related with career and psychosocial mentoring functions (28). An exploratory factor analysis test confirmed the validity of these four subscales in our data. In addition, the items within each subscale showed satisfactory internal consistency (psychosocial benefits subscale α = 0.79, career benefits subscale α = 0.88, psychosocial mentoring goals subscale α = 0.73, and career mentoring goals subscale α = 0.88). The original and previously published items were combined into a single survey in Qualtrics (Provo, UT). Five upper-level undergraduate students pilot tested the survey and provided feedback on the flow and clarity of the questions. Three faculty members familiar with the study and item construction examined the survey to establish that the survey questions were appropriate for the purpose of the study, and the survey was revised.
The Qualtrics survey was distributed to medical students at ECU, Wake Forest, and UNC via email distribution lists in September 2020. The total enrollment of each school during this time was 343 students (ECU), 570 students (Wake Forest), and 865 students (UNC). Therefore, the survey should have reached 1,778 students in total. We were unable to send the survey to the distribution list directly and were dependent on staff at each institution to do so. Certainly not all enrolled students paid attention to the survey request in their email. We closed the survey in December 2020 allowing for about 3 months for students to complete the survey. We received 130 surveys from students, which is a 7.3% response rate. Participation in the survey was voluntary but incentivized with a $20 gift card given to a random subset of approximatively 10% of survey respondents. Survey respondents had the option to include their e-mail address to be eligible for the gift card drawing and could indicate their willingness to be contacted for a follow-up interview.
The quantitative data were analyzed using SPSS (IBM, Armonk, NY) and R Software (R Core Team, Vienna, Austria). Responses that were duplicate, had 50% or fewer of the items completed, had incorrect answers to the check point questions, were inconsistent between the regularly worded and reverse coded items, or consistently gave the same answer (e.g., strongly agree or strongly disagree) were excluded. After removing duplicate, incomplete and erroneous answers, 87 responses were retained for analysis. Because of limited sample sizes in many categories, we recoded the mentees’ race and ethnicity into three categories: white, Asian, and Underrepresented (UR). If the mentees selected more than one option (“black” or “Hispanic” + anything else) their response was coded as “UR” and “Asian” + “white” was coded as “Asian.”
To address the first research question, we used descriptive statistics to determine the number of formal and informal mentors the students had, along with a count of the number of students who had experienced group mentoring. We performed separate analysis of variance (ANOVA) tests for each demographic factor to determine the likelihood of students having more mentors based on demographic characteristics. To address the second research question, we used descriptive statistics to determine the most common profession and the gender identity of the mentors. We calculated how frequently the gender identity of the student and the mentor was the same. In addition, we used a chi-square test to evaluate if male and female mentees would be mentored by mentors who shared their same gender identity more often than you would expect from a null hypothesis. For the third research question, we calculated the strength of the psychosocial and career goals students reported having for the mentoring by calculating the mean of the eight items that measured psychosocial goals and then the mean of the eight survey items that measured career goals (28). We repeated these steps for the perceived career and psychosocial benefits of mentoring, using those respective survey items. To address the fourth question, we performed a Pearson correlation test between the mentees’ psychosocial mentoring goals and their perceived psychosocial benefits (and then their career-related goals and career-related benefits) of mentoring. In addition, we performed two separate linear regressions to determine if students with stronger mentoring goals would have more prior mentors than students with fewer mentoring goals.
Interviews
In December 2020, we emailed a random subset of 30 survey respondents who provided their contact information to request that they participate in a follow-up interview. The goal of the interview was to further investigate the survey responses and gain a deeper understanding of the responses received from the survey. We interviewed 10 students via Cisco WebEx during the first 2 weeks of January 2021. Each interview was recorded with the interviewee’s consent. The semistructured interviews were guided by 17 original questions and followed up with clarifying or probing questions, as needed (Appendix 2). The interviews lasted 20–30 min each. Each participant received a $20 gift card for completing the interview, in addition to being eligible for the gift card raffle associated with completing the survey.
The interview videos were transcribed by a commercial service, Rev (San Francisco, CA). We created a list of 12 initial codes: “career choices,” “choice of mentor,” “emotional support,” “gender identity impact,” “mentor availability,” “mentor quality,” “mentor dislikes,” “career guidance,” “mentoring likes,” “mentoring dislikes,” “race/ethnicity impact,” “role model,” and “socioeconomic impact”; the interview transcripts were then coded iteratively using Nvivo (QSR International, Burlington, MA). Two individuals (VW and one other) coded two interview transcripts, and interrater reliability between these two coders was calculated using kappa coefficient. Any differences in coding were discussed and the code book was revised. This process was repeated until high interrater reliability was achieved (kappa coefficient of 0.87) with a final codebook of six codes (Appendix 3). The remaining transcripts were coded by one author (VW) and synthesized to identify broad themes.
RESULTS
Some of the 130 surveys completed had to be removed because they did not meet the inclusion criteria, leaving 87 responses that were retained for analysis. Most of the respondents were female, white, had a low or intermediate household income, and had at least one parent/guardian with education beyond a bachelor’s degree (Table 1). The demographics of the interviewees were similar to the survey respondents except Asian students were more heavily represented (Table 2).
TABLE 1.
Number and percentage of individuals of each a) gender identity, b) aggregated race/ethnicity; UR indicates those from a race or ethnicity that is underrepresented in medical school (e.g., Hispanic, black, mixed races identifying with Hispanic or black race), c) aggregated household income (high > $75,001, intermediate between $25,001 and $75,000, and low < $25,000), and d) aggregated parent’s highest level of income responding to the survey
| Demographic characteristic | Frequency (percentage) |
|---|---|
| Gender Identity | Male: 16 (18%) Female: 70 (80%) |
| Race/Ethnicity | Asian: 21 (24%) UR: 15 (17%) White: 51 (59%) |
| Household Income | Low: 32 (37%) Intermediate: 23 (36%) High: 14 (16%) Prefer not to answer: 18 (21%) |
| Parent’s Highest Level of Education | No Bachelor’s degree: 8 (9%) Bachelor’s degree: 30 (35%) Post Bachelor’s degree: 49 (56%) |
TABLE 2.
Percentage of interviewees from each a) gender identity, b) aggregated race/ethnicity; UR indicates those from a race or ethnicity that is underrepresented in medical school, c) level of reported annual household income (high > $75,001, intermediate between $25,001 and $75,000, and low < $25,000), and d) interviewees from each medical school
| Demographic characteristic | Percentage |
|---|---|
| Gender Identity | Male: 10% Female: 90% |
| Race/Ethnicity | Asian: 50% UR: 40% White: 10% |
| Household Income | Low: 25% Intermediate: 25% High: 50% |
| Institution | ECU: 70% UNC: 10% Wake Forest: 20% |
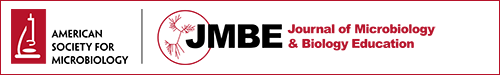
Research Question 1: We found that students had considerable exposure to both formal and informal mentoring (86% and 92% of the respondents, respectively), but not group mentoring. On average, respondents reported having 2.36 formal mentors (SD = 1.92) and 2.99 informal mentors (SD = 2.29). In the prior 5 years, only 26% of survey respondents had been mentored in a group setting. ANOVA tests revealed no significant difference in the number of formal and informal mentors as a function of household income, parental highest level of education, or student gender identity. However, further analyses showed that there was a significant difference in the number of informal mentors, but not formal mentors, based on race/ethnicity (F [2,77] = 4.36, P = 0.016). Asian students had significantly more informal mentors than white students (P = 0.017) and UR students (P = 0.056; Fig. 1). Thus, students from racial/ethnic groups less represented in medical fields had fewer mentors than Asian students who are not underrepresented in medical fields. However, there was no evidence that students from other underrepresented groups in medicine had fewer mentors. In the interviews, medical students reported they had not previously had difficulties finding mentors.
FIG 1.
The mean number of formal mentors (a) that a survey respondent had did not differ with respondent race or ethnicity, but Asian survey respondents had significantly more informal mentors (b), than underrepresented (UR) or white respondents.
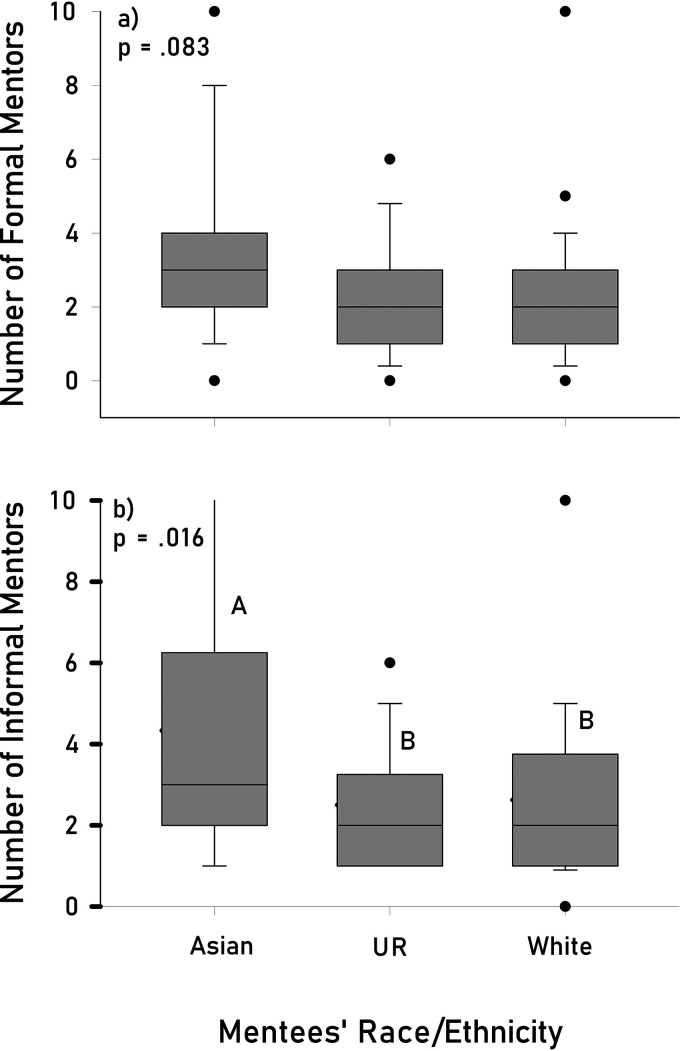
Research Question 2: The mentors were generally medical professionals or university faculty members, with mentors of female and male gender identities well represented. There was a significant association between the gender identity of the mentee and the gender identity of their first formal mentor (χ2 [2, N = 66] = 10.00, P = 0.007 and their first informal mentor χ2 [2, N = 70] = 10.75, P = 0.005. Male respondents shared the same gender identity as their first formal and informal mentors more often than would be expected under the null hypothesis of no association between gender identity of the mentee and chosen mentor (Fig. 2a). Female respondents only shared the same gender identity as their first informal mentors more often than would be expected under the null hypothesis (Fig. 2b). Thus, male and female mentees were mentored more frequently by mentors who share their same gender identity. Interviewees discussed how they sought out medical professionals as mentors because they were familiar with the medical admissions process. They also reported in the interviews that gender identity, race/ethnicity, and socioeconomic status played a role in some mentees’ access to mentors and ability to choose a mentor. For example, students in lower income households and underrepresented groups mentioned seeking mentors who are not medical professionals (e.g., faculty members) to help advance their ambition to pursue medicine because of limited access to medical professional mentors.
FIG 2.
Male respondents shared the same gender identity as their first formal (a) and informal mentors (b) more often than would be predicted at random; female respondents only shared the same gender identity as their first informal mentors (b) more often than would be predicted at random.
Research Question 3: On average, respondents generally agreed that they had psychosocial goals (= 5.7, SD = 0.511; 7-point Likert scale) and career goals ( = 5.6, SD = 0.893) when entering these mentoring relationships. Respondents reported perceiving (on a 5-point Likert scale) psychosocial benefits ( = 4.2, SD = 0.498) and career benefits ( = 3.6, SD = 0.795) from their mentoring. In the interviews, students reported having both psychosocial and career benefits from mentoring. They particularly discussed how they appreciated receiving recommendations and research opportunities from their mentors, as well as encouragement. They looked up to their mentors as role models and felt that they received any necessary emotional support. Additionally, many female mentees reported receiving emotional support related to gender identity and identity as a scientist from female mentors.
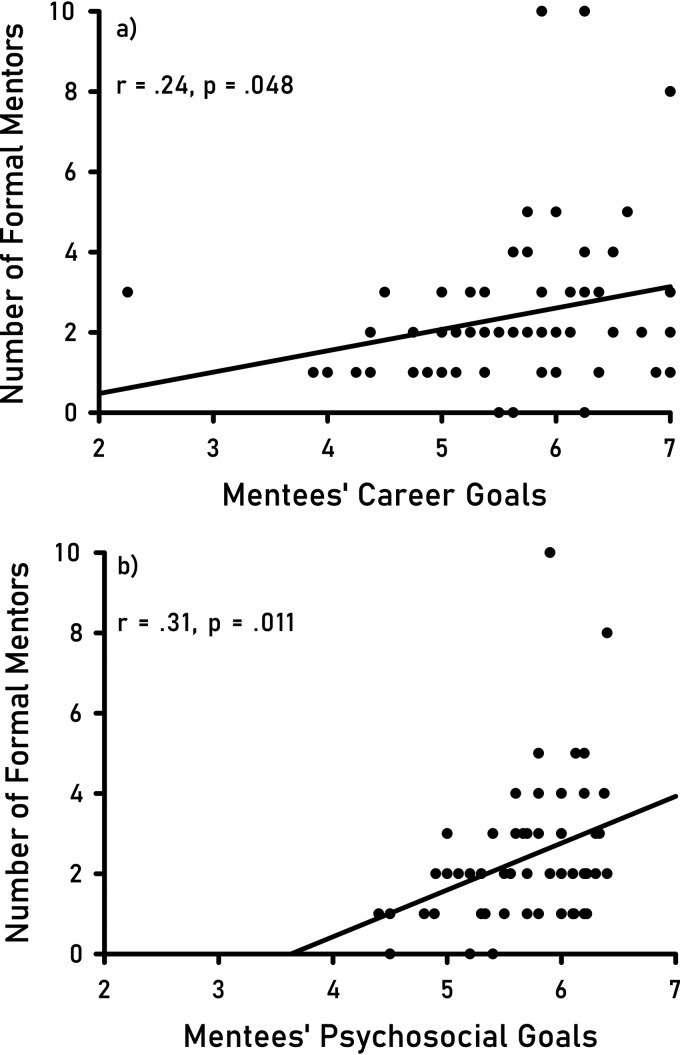
Research Question 4: A correlation test revealed a significant, positive association between the strength of mentees’ goals going into mentoring and their perceived benefits of mentoring (career benefits r = 0.57, P = 0.000; psychosocial benefits r = 0.52, P = 0.000). In addition, there was a significant, positive association between the strength of a student’s career goals for mentoring and their number of formal mentors (r [73] = 0.24, P = 0.048; Fig. 3a), but not informal mentors. Similarly, there was a significant positive association between the strength of a student’s psychosocial goals for mentoring and their number of formal mentors (r [73] = 0.31, P = 0.011; Fig. 3b), but not informal mentors. Thus, students with stronger mentoring goals had more formal mentors, but not informal mentors, than students with fewer mentoring goals. When asked about what mentees liked and disliked about their mentoring experiences during the interviews, mentees liked when their mentors were available and approachable, gave them constructive criticism, were encouraging, and were good listeners. Mentees did not like the amount of planning that mentoring required because both the mentor and mentee were busy.
FIG 3.
The more career goals (a) or psychosocial goals (b) a survey respondent had for mentoring, the greater the number of formal mentors they generally had.
DISCUSSION
This study addressed how mentees who are now medical students perceived their prior mentoring experiences and how these factors are influenced by demographic factors. We found that Asian students had significantly more informal mentors than their white and UR counterparts. This finding partially matches prior literature (9), which states that members of UR groups in STEMM have difficulty accessing informal mentoring relationships. The fact that the UR students did not have fewer informal mentors than white students could be due to this study population being highly motivated and successful medical students whereas the NASEM (9) report encompasses results from different groups, including undergraduate, graduate, and medical students. The number of formal or informal mentors a student had did not differ based on mentees’ gender identity, household income, or level of parental education. For these students, personal motivation may have driven participation in mentoring more than demographic factors.
Over 90 percent of the medical student respondents had at least one parent with a bachelor’s or higher degree. This shows that these respondents reflect a small subset of the U.S. population whose family has unusually high levels of education. According to the American Council on Education, in 2017, only 21.3% of adults ages 25 and older in the United States. obtained a bachelor’s degree or higher (29). There was no difference in exposure to mentoring, however, in respondents from differing levels of parental education. Thus, respondents from families with low parental education who are enrolled in medical school may not be representative of the larger population of students applying to medical schools (but who are ultimately unsuccessful) from families with lower levels of parental education. Higher levels of mentoring among these first-generation students than the average first-generation student may have helped these students be more successful in their medical school admissions. Although first-generation students account for one-third of students in postsecondary education and almost half of all students enrolled at minority-serving institutions (30), they are much less represented in medical school admissions. In addition, first-generation students are less likely than continuing-generation students to begin their studies in 4-year colleges and more likely than continuing-generation peers to attend less selective colleges, including 2-year and for-profit institutions (31). First-generation students may need mentoring at a higher rate than their continuing-generation counterparts to address issues of equity and inclusion at medical schools.
Students had experienced both formal and informal mentoring, but only roughly a quarter of the respondents had experienced group mentoring. They usually selected medical professionals or university faculty as mentors. They preferred medical professionals as mentors but students with lower household incomes had less access to potential medical professional mentors. Thus, aspiring medical students may benefit from programs that help connect them with medical professionals willing to serve as mentors and provide guidance on creating goals for the mentoring and sustaining the mentoring relationship.
There was an association between the gender identity of the student and that of their mentor. During interviews, students expressed that they did not seek out mentors of a particular gender identity, but it is possible that unconscious biases influenced their choice of mentor, or the mentor had conscious or unconscious biases in their selection of mentees. Alternatively, students’ social networks may be skewed to individuals of the same gender identity and that may influence their likelihood of selecting a mentor with a particular gender identity. Female interviewees reported not intentionally seeking female mentors, but a mentoring relationship with a female mentor happened spontaneously.
Moreover, mentees’ perception of career and psychosocial support may also depend on the gender identity of the mentor. Research on gender bias in mentorship has shown that female mentees with male mentors had difficulty seeing their mentors as suitable role models (6), and women in same-gender mentoring relationships have reported significantly greater role modeling from their mentors (32). Other studies have shown that both male and female mentees perceive female mentors as offering more psychosocial support, including role modeling, and male mentors as offering more career support, which is consistent with common gender identity roles (33).
Students were motivated to enter these mentoring relationships due to a desire for psychosocial and career guidance, and the more goals they had for mentoring the more formal (but not informal) mentors they tended to have. This finding suggests that mentees may have more specific goals when entering formal mentoring relationships as opposed to informal mentoring relationships which tend to be spontaneous and are often developed without clear expectations (6, 14, 15). In the interviews, mentees reported having clear expectations for the mentoring relationship as one of the most important determinants of the success of a mentoring experience. Interviewees felt that formal mentoring provided better connections because of the set expectations for the mentor(s) and the mentee(s), whereas they felt it was harder to cultivate relationships with informal mentors because they never officially asked them to be their mentor. Mentees also reported wishing they had mentors earlier in their career and specifically for the medical field, instead of just research mentors. Therefore, mentees should establish clear expectations with their mentors for both informal and formal mentoring relationships to maximize their mentoring experiences, and they should actively seek out mentors in the medical field to guide them in their medical career goals.
As with all research, there are limitations to this study. These data on students’ mentoring goals and perceived benefits are self-reported; no direct measures of how the mentoring experiences impacted the students’ success have been included. Additionally, the study could have benefited from a bigger sample size and representation from additional medical schools to increase our confidence in the results and enhance our ability to generalize the findings. We had a response rate of 7.3%, which means that surveying more students, perhaps with more advertisement of the survey, could help raise the response rate and provide a broader sample. We used medical students from all years in medical school to increase the sample size; while most students talked about their mentoring experience prior to entering medical school, some upperclassmen may have talked about mentoring experiences during medical school. Thus, the survey would have benefited from an item that specified the student’s year in medical school. In addition, the survey or interview questions could have benefited from items inquiring about how many times the survey respondents applied to medical school before being accepted.
While this study focused on the prior mentoring experiences of students in medical school, many undergraduate programs may be interested also in the mentoring experiences of students who applied, but were not accepted, into medical school. Data from this population would make a nice comparison to the current study and would allow additional exploration of some of our findings. Therefore, future studies could target students who were unsuccessful in their attempt to matriculate into medical school to give insight about their mentoring experiences and demographic characteristics.
Conclusion
This study highlights the mentoring experiences of medical students and the role that demographic factors play in mentoring relationships. Both the survey results and interviews indicate that there may be gender bias in selection of mentors. In addition, student race or ethnicity may impact students’ access to mentoring, especially informal mentoring, and household income may impact student selection of mentors as well as their goals and perceptions of mentoring. Mentoring programs for aspiring medical students may benefit from focusing on both career and psychosocial functions to maximize the benefits of mentoring for students from diverse backgrounds.
ACKNOWLEDGMENTS
Celestial Jynx Pigart-Coleman aided in the initial coding of the interview transcripts. In addition, she, Carol Goodwillie, Mark Bowler, Jennifer Teshera-Levye, and Michelle Anne Reyes provided valuable feedback on this work. We appreciate ECU, Wake Forest, and UNC distributing the survey and are grateful to the medical students who completed it.
This work was supported by funds provided by East Carolina University to Heather Vance-Chalcraft, but the sponsor had no role in the study design, collection, analysis, or writing.
Footnotes
Supplemental material is available online only.
REFERENCES
- 1.Jacobi M. 1991. Mentoring and undergraduate academic success: a literature review. Rev Educ Res 61:505–532. doi: 10.3102/00346543061004505. [DOI] [Google Scholar]
- 2.Crisp G, Cruz I. 2009. Mentoring college students: a critical review of the literature between 1990 and 2007. Res High Educ 50:525–545. doi: 10.1007/s11162-009-9130-2. [DOI] [Google Scholar]
- 3.Pololi LH, Knight SM, Dennis K, Frankel RM. 2002. Helping medical school faculty realize their dreams: an innovative, collaborative mentoring program. Acad Med 77:377–384. doi: 10.1097/00001888-200205000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Healy CC, Welchert AJ. 1990. Mentoring relations: a definition to advance research and practice. Educ Res 19:17–21. doi: 10.3102/0013189X019009017. [DOI] [Google Scholar]
- 5.Haggard DL, Dougherty TW, Turban DB, Wilbanks JE. 2011. Who is a mentor? A review of evolving definitions and implications for research. J Manage 37:280–304. doi: 10.1177/0149206310386227. [DOI] [Google Scholar]
- 6.Kram KE. 1985. Mentoring at work: developmental relationships in organizational life. Scott Foresman, Glenview, IL. [Google Scholar]
- 7.Packard BWL. 2016. Successful STEM mentoring initiatives for underrepresented students: a research-based guide for faculty and administrators. Stylus Publishing, Sterling, VA. [Google Scholar]
- 8.Kram K. 1983. Phases of the mentor relationship. Acad Manage J 26:608–625. [Google Scholar]
- 9.National Academies of Sciences, Engineering, and Medicine. 2019. The Science of Effective Mentorship in STEMM. National Academies Press, Washington, DC. doi: 10.17226/25568. [DOI] [PubMed] [Google Scholar]
- 10.Estrada M, Hernandez PR, Schultz PW, Herrera J. 2018. A longitudinal study of how quality mentorship and research experience integrate underrepresented minorities into STEM careers. CBE Life Sci Educ 17. doi: 10.1187/cbe.17-04-0066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thiry H, Laursen S. 2011. The role of student-advisor interactions in apprenticing undergraduate researchers into a scientific community of practice. J Sci Educ Technol 20:771–784. doi: 10.1007/s10956-010-9271-2. [DOI] [Google Scholar]
- 12.Estrada M, Woodcock A, Hernandez PR, Schultz PW. 2011. Toward a model of social influence that explains minority student integration into the scientific community. J Educ Psychol 103:206–222. doi: 10.1037/a0020743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hurtado S, Cabrera NL, Lin MH, Arellano L, Espinosa LL. 2009. Diversifying science: underrepresented student experiences in structured research programs. Res High Educ 50:189–214. doi: 10.1007/s11162-008-9114-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ragins BR, Cotton JL. 1999. Mentor functions and outcomes: a comparison of men and women in formal and informal mentoring relationships. J Appl Psychol 84:529–550. doi: 10.1037/0021-9010.84.4.529. [DOI] [PubMed] [Google Scholar]
- 15.Zachary LJ. 2011. Creating a mentoring culture: The organization’s guide. John Wiley & Sons: Hoboken, NJ. [Google Scholar]
- 16.Griffin K, Baker V, O’Meara K, Nyunt G, Robinson T, Staples CL. 2018. Supportingscientists from underrepresented minority backgrounds: mapping developmental networks. SGPE 9:19–37. doi: 10.1108/SGPE-D-17-00032. [DOI] [Google Scholar]
- 17.Aikens ML, Sadselia S, Watkins K, Evans M, Eby LT, Dolan EL. 2016. A social capital perspective on the mentoring of undergraduate life science researchers: an empirical study of undergraduate–postgraduate–faculty triads. CBE Life Sci Educ 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Joshi M, Aikens ML, Dolan EL. 2019. Direct ties to a faculty mentor related to positive outcomes for undergraduate researchers. Bioscience 69:389–397. doi: 10.1093/biosci/biz039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gayles JG, Ampaw FD. 2011. Gender matters: an examination of differential effects of the college experience on degree attainment in STEM. New Directions for Institutional Res 2011:19–25. doi: 10.1002/ir.405. [DOI] [Google Scholar]
- 20.Helm EG, Prieto DO, Parker JE, Russell MC. 2000. Minority medical school faculty. J Natl Med Assoc 92:411–414. [PMC free article] [PubMed] [Google Scholar]
- 21.King JT, Angoff NR, Forrest JN, Jr., Justice AC. 2018. Gender disparities in medical student research awards: a 13-year study from the Yale School of Medicine. Acad Med 93:911–919. doi: 10.1097/ACM.0000000000002052. [DOI] [PubMed] [Google Scholar]
- 22.Thomas GD, Hollenshead C. 2001. Resisting from the margins: the coping strategies of black women and other women of color faculty members at a research university. J Negro Educ 70:166–175. doi: 10.2307/3211208. [DOI] [Google Scholar]
- 23.Milkman KL, Akinola M, Chugh D. 2015. What happens before? A field experimentexploring how pay and representation differentially shape bias on the pathway into organizations. J Appl Psychol 100:1678–1712. doi: 10.1037/apl0000022. [DOI] [PubMed] [Google Scholar]
- 24.Cuddy AJC, Fiske ST, Glick P. 2007. The BIAS map: behaviors from intergroup affect and stereotypes. J Pers Soc Psychol 92:631–648. doi: 10.1037/0022-3514.92.4.631. [DOI] [PubMed] [Google Scholar]
- 25.Weyant JM. 2005. Implicit stereotyping of Hispanics: development and validity of a Hispanic version of the Implicit Association Test. Hisp J Behav Sci 27:355–363. doi: 10.1177/0739986305276747. [DOI] [Google Scholar]
- 26.Kim A, Yeh CJ. 2002. Stereotypes of Asian American students. ERIC Clearinghouse on Urban Education: New York, New York. https://eric.ed.gov/?id=ED462510. [Google Scholar]
- 27.Nosek BA, Smyth FL, Hansen JJ, Devos T, Lindner NM, Ranganath KA, Smith CT, Olson KR, Chugh D, Greenwald AG, Banaji MR. 2007. Pervasiveness and correlates of implicit attitudes and stereotypes. Eur Rev Soc Psychol 18:36–88. doi: 10.1080/10463280701489053. [DOI] [Google Scholar]
- 28.Tepper K, Shaffer BC, Tepper BJ. 1996. Latent structure of mentoring functions and scales. Educ Psychol Measur 56:848–857. doi: 10.1177/0013164496056005013. [DOI] [Google Scholar]
- 29.American Council on Education. 2017. Chapter One: Population trends and educational attainment In: Race and Ethnicity in Higher Education: A status report. https://www.equityinhighered.org/indicators/u-s-population-trends-and-educational-attainment/educational-attainment-of-the-u-s-population/ (accessed July 28, 2021).
- 30.Harmon N. 2012. The role of minority-serving institutions in national college completion goals. Institute for Higher Education Policy: Washington, DC. [Google Scholar]
- 31.Cataldi E, Bennett C, Chen X. 2018. First-generation students: College access, persistence, and postbachelor’s outcomes. NCES 2018421 Institute of Education Sciences. https://nces.ed.gov/pubsearch/pubsinfo.asp?pubid=2018421 (accessed May 24, 2019). [Google Scholar]
- 32.Ragins BR, McFarlin DB. 1990. Perceptions of mentor roles in cross-gender mentoring relationships. J Vocat Behav 37:321–339. doi: 10.1016/0001-8791(90)90048-7. [DOI] [Google Scholar]
- 33.Sosik JJ, Godshalk VM. 2000. The role of gender in mentoring: implications for diversified and homogenous mentoring relationships. J Vocat Behav 57:102–122. doi: 10.1006/jvbe.1999.1734. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material. Download JMBE00209-21_Supp_1_seq6.pdf, PDF file, 0.5 MB (582.6KB, pdf)