Abstract
Background
Despite the increased access to facility-based delivery in Indonesia, the country’s maternal mortality remains unacceptably high. Reducing maternal mortality requires a good understanding of the care-seeking pathways for maternal complications, especially with the government moving toward universal health coverage. This study examined care-seeking practices and health insurance in instances of pregnancy-related deaths in Jember District, East Java, Indonesia.
Methods
This was a community-based cross-sectional study to identify all pregnancy-related deaths in the district from January 2017 to December 2018. Follow-up verbal and social autopsy interviews were conducted to collect information on care-seeking behavior, health insurance, causes of death, and other factors.
Findings
Among 103 pregnancy-related deaths, 40% occurred after 24 hours postpartum, 36% during delivery or within the first 24 hours postpartum, and 24% occurred while pregnant. The leading causes of deaths were hemorrhage (38.8%), pregnancy-induced hypertension (20.4%), and sepsis (16.5%). Most deaths occurred in health facilities (81.6%), primarily hospitals (74.8%). Nearly all the deceased sought care from a formal health provider during their fatal illness (93.2%). Seeking any care from an informal provider during the fatal illness was more likely among women who died after 24 hours postpartum (41.0%, OR 7.4, 95% CI 1.9, 28.5, p = 0.049) or during pregnancy (29.2%, OR 4.4, 95% CI 1.0, 19.2, p = 0.003) than among those who died during delivery or within 24 hours postpartum (8.6%). There was no difference in care-seeking patterns between insured and uninsured groups.
Conclusions
The fact that women sought care and reached health facilities regardless of their insurance status provides opportunities to prevent deaths by ensuring that every woman receives timely and quality care. Accordingly, the increasing demand should be met with balanced readiness of both primary care and hospitals to provide quality care, supported by an effective referral system.
Introduction
Indonesia, the world’s fourth most populous country, faces significant challenges in reducing maternal mortality [1]. The country’s maternal mortality ratio (MMR) of 305 per 100,000 live births in 2015 remains among the highest in the region [2, 3]. The high MMR poses a big challenge in achieving Sustainable Development Goal 3 (SDG-3) which aims to reduce the global MMR to less than 70 per 100,000 live births by 2030, with no greater than 140 per 100,000 live births in any country [4]. This situation calls for concerted action to catalyze progress toward achieving the SDG-3 targets.
Reducing maternal mortality requires a good understanding of the magnitude of the problem, causes, and underlying factors. Notably, given the increase in facility-based deliveries in Indonesia from 46% to 74% between 2007 and 2017 [5, 6], it is important to understand the care-seeking pathways that women take to shed light on why maternal mortality remains high. Social factors related to maternal health care utilization and outcomes include sociocultural beliefs and practices, lack of awareness about maternity care and danger signs in pregnancy, and household decision-making dominated by husbands and other family members, as shown by qualitative studies in Indonesia [7, 8]. Two large-scale cohort studies in Bangladesh show that only between 29% and 47% of women who experienced obstetric complications received care from trained providers, with household wealth, women’s and husbands’ education, and distance to health facility among the predictors for care-seeking [9, 10]. Studies from low- and middle-income countries, including Indonesia, indicate that cost of services has also been a barrier in access to health care, especially for the poor [11, 12].
To ensure access to safe, effective, quality, and affordable healthcare for all, as mandated by SDG-3, the Government of Indonesia has implemented the National Health Insurance (NHI) policy (Jaminan Kesehatan Nasional/JKN) since 2014, to move toward universal health coverage (UHC) [13]. By 2018, when this study was conducted, nearly 80% of the population were covered by the NHI [14]. Those who do not have any insurance and are not covered by the NHI, but are classified as poor or near-poor, may receive central and/or local government aid [15]. The rapidly growing NHI coverage, combined with the other sources of government assistance, may have successfully alleviated financial barriers for maternal and neonatal health services, although inequity in access persists particularly by different economic levels [16]. Furthermore, the influence of improved health insurance coverage on care-seeking for complications that led to pregnancy-related deaths is not well-known. Previous studies on maternal health care-seeking in the Indonesian setting were mostly done prior to, or at the early stage of, the NHI roll-out [16, 17].
A good understanding of care-seeking patterns related to complications is important to inform effective interventions to help prevent avoidable deaths in the future, yet the necessary information remains lacking. This study aimed to fill the gap by providing information about the causes of death and care-seeking pathways leading to maternal mortality, and to examine whether patterns of care-seeking vary by health insurance status.
Materials and methods
Study design
This paper used a subset of data from a large cross-sectional study on maternal and neonatal mortality, namely the ‘Every Mother and Newborn Counts’ (EMNC) study, with district-wide coverage, conducted from January to April 2019. The EMNC study was undertaken as part of the five-year USAID Jalin project [18], which aims to reduce maternal and neonatal mortality in Indonesia. Data on maternal mortality were obtained from two methods of data collection: i) the ‘Maternal deaths from Informants and Maternal deaths Follow on Review’ (MADE-IN/MADE-FOR) to identify pregnancy-related deaths [19], and ii) a Verbal and Social Autopsy (VASA) interview to ascertain the circumstances and causes of death [20]. The VASA tool integrates the 2016 World Health Organization Verbal Autopsy instrument with the Johns Hopkins University/Institute for International Programs Social Autopsy questionnaire to collect information on the medical and injury history associated with final illness, general signs and symptoms associated with the final illness, pregnancy and delivery complications, care-seeking prior to death, and household characteristics [20].
Study setting
The EMNC study was conducted in Jember District on the island of Java, home to about 2.4 million people. The study covered all 248 villages in the district [21]. The study district was selected due to the high number of maternal deaths, the large population, and the geographical and socio-cultural challenges in reducing maternal mortality. The district has reported relatively good maternal health care status as exhibited by the proportion of government-recommended antenatal care visits attended (88.5%) and deliveries in facilities (91.2%). There are 11 general hospitals in the district, of which four are Comprehensive Emergency Obstetric and Neonatal Care (CEmONC) facilities [22]. At the time of the study, nearly 60% of the population in the study district were registered under the NHI, of whom 45.5% were financed by the local government [22].
Study population
The study population was women of reproductive age (WRA), aged 13–49 years old, who died while pregnant, during labor/delivery, or within 42 days after delivery or abortion, irrespective of the cause of death. The eligibility criteria were women who were residents (proven with identity card) or who have stayed for at least six months in the study district who died between January 2017 and December 2018.
Data collection
The MADE-IN/MADE-FOR method sought to identify all pregnancy-related deaths through a listing of WRA deaths in each village. The list, with information on whether the death occurred during pregnancy, labor/delivery, or within 42 days after delivery or abortion, was used to screen for possible pregnancy-related deaths. The listing was produced by obtaining information from two networks of village informants who are considered most knowledgeable of the vital events in the community. Details of the method are described elsewhere [19, 23]. All households identified as having experienced a pregnancy-related death during the recall period were visited to verify eligibility. Once deaths were confirmed as eligible, a VASA interview was conducted [20]. The VASA was held by interviewing household respondents, primarily family member(s) who were considered as the most knowledgeable about circumstances and care-seeking actions taken during the fatal illness. A two-year recall period (2017–2018) was used to increase the likelihood of obtaining sufficient events for robust analyses while minimizing recall bias.
The term formal care provider refers to a trained or certified health care provider (i.e. doctor/Obstetrician/Gynecologist, midwife, and nurse) regardless of the place where care was provided (inside or outside health facilities). Informal care provider refers to the individual providing traditional medicines, home remedies, or non-professional treatment. We differentiated between the first and last care provider seen/visited/sought (even if the deceased did not reach the provider) during the fatal illness before death. We categorized health insurance status as (1) insured (NHI or other health insurance type), (2) government aid beneficiaries, and (3) uninsured. Government aid refers to either Jaminan Kesehatan Daerah/Jamkesda (Regional Health Insurance), which is provided through the local government financing and can be used for any type of care, or Jaminan Persalinan/Jampersal (Social Insurance for Free Delivery), which is financed by the central government and designated only for maternal and neonatal care. A proxy of the socio-economic level was measured through wealth quartiles, with Quartile 1 being the poorest and Quartile 4 the least poor. The wealth quartiles are a composite of household assets and the index was derived using principal components analysis.
Data management and quality assurance
Data were collected and directly entered on a tablet with the Open Data Kit (ODK) platform, and then transmitted electronically to the central research office for storage, management, cleaning, and analysis. Before being transmitted to the central office, data were cross-checked by a different data collector and then double-checked by the field supervisor. Transmitted data were also checked by the data management team as part of the data cleaning.
Data analysis
Data from the ODK were transferred into STATA for analysis. We analyzed the number of pregnancy-related deaths and their characteristics using descriptive statistics. Bivariate analysis was conducted to identify any distinct patterns of care-seeking that existed by health insurance status, cause of death, and other variables. Information from the VASA was analyzed to determine the causes of death, identify social factors contributing to deaths, and examine care-seeking pathways. The causes of death were assigned by the InSilicoVA computer algorithm [24]. For each death, InSilicoVA assigns the most likely underlying cause.
Ethical approval
The study was granted ethical approval from the Institutional Review Board at the Biomedical Research Alliance of New York (BRANY) and at the Faculty of Public Health, Universitas Indonesia. Written informed consent was obtained from each respondent prior to participating, and each respondent was also provided a hard-copy description of the study and a consent statement with the local Principal Investigator’s contact information.
Results
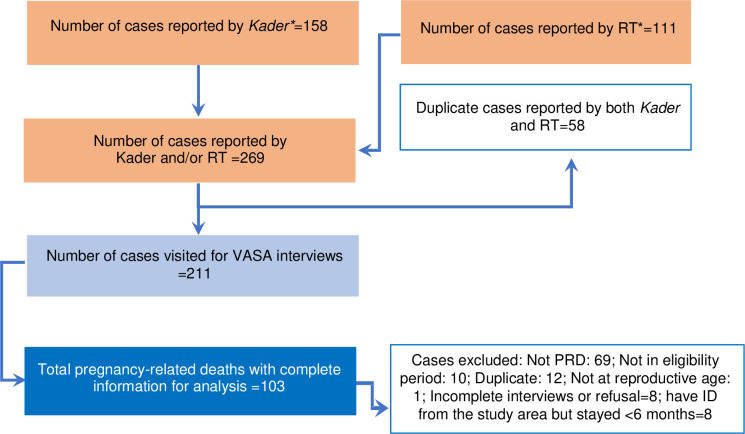
Among 269 WRA deaths reported, 211 deaths were listed as pregnancy-related deaths by the village informants. After confirmation with families of the deceased, 48.8% of the cases met our inclusion criteria and the VASA interviews were completed. The remaining (n = 108) were deemed ineligible due to i) not being pregnancy-related deaths (63.9%); ii) died outside of the 2017–18 recall period (9.3%); iii) duplicate cases (11.1%), and other reasons (Fig 1). We also matched the cases found in our study against the district’s health information system, which collects information on maternal deaths (excluding deaths due to accidental or incidental causes), and found that our study identified 26% more maternal deaths. The final analysis for this study included 103 eligible pregnancy-related deaths. The researchers decided to focus on pregnancy-related deaths in this study and included the three deaths due to accidental causes. All data presented in the tables and the figure in this section were generated from the VASA interviews.
Fig 1. Flowchart of pregnancy-related death (PRD) cases identified in Jember District, 2017–2018.
*Kader: community health volunteer; RT: head of a neighbourhood unit. These two groups are generally the most knowledgeable about vital events in the community, as shown from the previous implementation of the MADE-IN/MADE-FOR methods.
Descriptive characteristics of pregnancy-related deaths
Table 1 describes the characteristics of the pregnancy-related death cases. The mean age at death was 31 years (±7), with about one-third occurring among women aged 35 years or older. About 47% of the women were first married when less than 20 years old. The greatest number of pregnancy-related deaths occurred among women with no education or primary education only (41.8%), living in rural areas (55.3%), and of Madura ethnicity (61.2%). About one-third of the women were primiparous (28.2%) and 9.7% had four or more previous births.
Table 1. Characteristics of pregnancy-related death cases (n = 103) in Jember District, 2017–2018.
| Characteristics | n (%) |
| Age at death (years) | |
| 15–19 | 6 (5.8) |
| 20–24 | 18 (17.5) |
| 25–29 | 19 (18.4) |
| 30–34 | 25 (24.3) |
| 35–39 | 22 (21.4) |
| 40+ | 13 (12.6) |
| Education | |
| None or Primary | 43 (41.8) |
| Junior High | 27 (26.2) |
| Senior High | 20 (19.4) |
| Academy/University | 9 (8.7) |
| Don’t know | 4 (3.9) |
| Age when first married (years) | |
| < 16 | 9 (8.7) |
| 16–19 | 39 (37.9) |
| ≥ 20 | 43 (41.7) |
| Don’t know | 12 (11.7) |
| Prior births | |
| 0 | 29 (28.2) |
| 1 | 29 (28.2) |
| 2 | 28 (27.1) |
| 3 | 7 (6.8) |
| 4 and more | 10 (9.7) |
| Residence | |
| Urban | 46 (44.7) |
| Rural | 57 (55.3) |
| Ethnicity | |
| Javanese | 40 (38.8) |
| Madura | 63 (61.2) |
| Place of delivery (among women who died during or after delivery) (n = 75) | |
| Hospital | 51 (68.0) |
| Other health facility | 10 (13.3) |
| Enroute to health facility | 8 (10.7) |
| Home | 1 (1.3) |
| Other | 5 (6.7) |
| Place of death | |
| Hospital | 77 (74.8) |
| Primary health facility | 7 (6.8) |
| Enroute to health facility | 10 (9.7) |
| Home | 9 (8.7) |
| Time of death | |
| Pregnancy | 25 (24.3) |
| Delivery or within the first 24 hours after delivery | 37 (35.9) |
| 2–7 days postpartum | 15 (14.6) |
| 8–15 days postpartum | 10 (9.7) |
| 16–42 days postpartum | 16 (15.5) |
| Insurance | |
| Insured (NHI or other insurance scheme) | 55 (53.4) |
| Government aid | 24 (23.3) |
| Uninsured | 24 (23.3) |
| Causes of deaths | |
| Obstetric haemorrhage | 40 (38.8) |
| Pregnancy-induced hypertension | 21 (20.4) |
| Pregnancy-related sepsis | 17 (16.5) |
| Other and unspecified cardiac disease | 12 (11.7) |
| Other causes* | 13 (12.6) |
*Others include abortion-related death (n = 1), anemia of pregnancy (n = 1), and digestive neoplasms (n = 1), diarrheal diseases (n = 1), liver cirrhosis (n = 1), accidental exposure to fire (n = 1), road traffic accident (n = 2), other and unspecified maternal causes (n = 4), and other and unspecified cause of death (n = 1).
The highest percentage of pregnancy-related deaths occurred more than 24 hours postpartum (40%), followed by deaths at delivery or within 24 hours postpartum (36%) and during pregnancy (24%). Among women who died during or after delivery, 81.3% delivered in health facilities, including 68% in hospitals and 13.3% in lower-level facilities. About 82% of all pregnancy-related deaths occurred in health facilities, with the majority in hospitals (74.8%) and the remainder in primary health facilities (6.8%).
Causes of death
The three leading causes of pregnancy-related death were obstetric hemorrhage (38.8%), pregnancy-induced hypertension (PIH) (20.4%), and pregnancy-related sepsis (16.5%) (Table 1). We examined cause of death in relation to pregnancy, labour and delivery. Among women who died during pregnancy, about one-third were due to PIH (32%), followed by pregnancy-related sepsis (28%). Most deaths of women who died during labour/delivery or within the first 24 hours postpartum were due to obstetric hemorrhage (78.4%), followed by PIH (10.8%). Hemorrhage, PIH, and pregnancy-related sepsis were equally represented as causes of death among women who died more than 24 hours postpartum; each contributed 22% of the deaths (S1 Table).
Care-seeking pathways
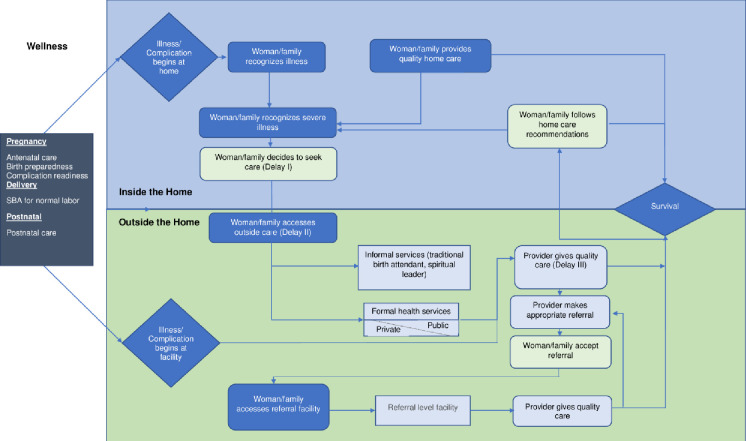
Fig 2 shows the care-seeking pathway that women may traverse during their illness prior to death. The figure was adapted from the Pathway to Survival for children developed to support the WHO/UNICEF Integrated Management of Childhood Illness approach [25]. The adapted pathway includes different points of entry for women based on where their illness began. Table 2 summarizes steps in the care-seeking pathway among all pregnancy-related deaths, stratified by time of death and insurance status. Nearly all pregnancy-related deaths in our study (95.1%) sought care at some time during the fatal illness, including 93.2% that sought formal care (either alone or a combination with informal care). Among those who reached the first formal care provider, 65.9% were referred by the first health provider. Almost all of the deceased (96.4%) complied with all the referrals made by all formal providers seen during the illness.
Fig 2. Care-seeking pathways among pregnancy-related deaths.
This pathway was adapted from the Pathway to Survival for children developed to support the WHO/UNICEF Integrated Management of Childhood Illness approach [25].
Table 2. Summary of care-seeking pathways by time of death and insurance in Jember District, 2017–2018.
| Factor | Care-seeking pathway | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Sought any care | Sought formal care only* | Formal and informal care* | Informal care only* | OR (95% CI) p-value (any informal care vs. formal care only)† | Reached 1st formal provider‡ | Referred, among those who reached 1st formal provider | Complied with all referrals‡ | Reached last formal provider, among those who were referred‡ | |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| All deaths (n = 103) | 98/103 (95.1) | 72/98 (73.5) | 24/98 (24.5) | 2/98 (2.0) |
91/91 (100) | 60/91 (65.9) |
54/56 (96.4) |
54/56 (96.4) | |
| Time of death | |||||||||
| Pregnancy (n = 25) | 24/25 (96.0) |
17/24 (70.8) |
7/24 (29.2) | 0/24 (0) |
4.4 (1.0, 19.2) 0.003 | 22/22 (100) | 18/22 (81.8) |
16/17 (94.1) |
16/17 (94.1) |
| At delivery or within 24 hr postpartum (n = 37) | 35/37 (94.6) | 32/35 (91.4) | 3/35 (8.6) | 0/35 (0) |
Reference | 34/34 (100) |
21/34 (61.8) |
18/19 (94.7) |
18/19 (94.7) |
| More than 24 hr postpartum (n = 41) | 39/41 (95.1) | 23/39 (59.0) | 14/39 (35.9) | 2/39 (5.1) |
7.4 (1.9, 28.5) 0.049 | 35/35 (100) | 21/35 (60.0) |
20/20 (100) |
20/20 (100) |
| Insurance ownership | |||||||||
| Insured (n = 55) | 52/55 (94.5) | 37/52 (71.2) | 13/52 (25.0) | 2/52 (3.8) | 1.4 (0.4, 4.4) 0.589 | 46/46 (100) | 29/46 (63.0) |
28/29 (96.6) |
28/29 (96.6) |
| Government aid (n = 24) | 24/24 (100) | 18/24 (75.0) | 6/24 (25.0) |
0/24 (0) |
1.1 (0.3, 4.4) 0.857 | 24/24 (100) | 17/24 (70.8) |
14/15 (93.3) |
14/15 (93.3) |
| Uninsured (n = 24) | 22/24 (91.7) | 17/22 (77.3) | 5/22 (22.7) | 0/22 (0) |
Reference | 21/21 (100) | 14/21 (66.7) |
12/12 (100) |
12/12 (100) |
*among those who sought care
†any informal care is a combination of seeking informal care only and both formal and informal care
‡excluded those who died prior to reaching 1st provider, died before being referred, or died before reaching the last provider.
Of all deceased women who sought care from a formal provider, the decision to seek formal care was made by the woman’s spouse in nearly half of the cases (47.9%), followed by other family members or relatives (18.8%). Decision-making by the deceased herself or jointly with the husband occurred in about 18% of the cases. Only 13.5% of respondents (13 out of 96 cases) reported facing constraints when seeking care for the deceased. The most frequently mentioned constraints were the thought that the woman was too sick to travel (35.7%; n = 5) and dissatisfaction with the available health care (21.4%; n = 3). Other constraints mentioned by a smaller number of respondents include the perception that the woman was not sick enough to need care, that it was too far to travel, and others. Distance appears to have been the major factor influencing the choice of the first provider, as 56.3% of respondents mentioned that they chose providers who are nearby. Many other respondents chose providers who they were familiar with (21.9%), or felt safe with (15.6%) (Table 3).
Table 3. Care-seeking among pregnancy-related death cases who sought formal care (n = 96) in Jember District, 2017–2018.
| Care-seeking | n (%) |
|---|---|
| Decision maker for care-seeking (n = 96) | |
| Adult deceased’s partner/spouse | 46 (47.9) |
| Relatives | 18 (18.8) |
| Adult deceased herself | 9 (9.4) |
| Both deceased and her spouse | 8 (8.3) |
| Health provider | 8 (8.3) |
| Someone else | 5 (5.2) |
| Don’t know | 2 (2.1) |
| Stated that there is concern in care-seeking (n = 96) | |
| Yes | 13 (13.5) |
| No | 79 (82.3) |
| Don’t know | 4 (4.2) |
| Constraints in care-seeking (n = 13) | |
| Too sick to travel | 5 (35.7) |
| Not satisfied with available healthcare | 3 (21.4) |
| Did not think she was sick enough | 1 (7.1) |
| Too much time from her/caregiver’s duties | 1 (7.1) |
| Too far to travel | 1 (7.1) |
| Cost (transport, healthcare, other) | 1 (7.1) |
| Other issue* | 3 (21.4) |
| Factors influencing choice of first provider (n = 96) # | |
| Provider nearby | 54 (56.3) |
| Familiarity | 21 (21.9) |
| Feel safe | 15 (15.6) |
| Recommended by doctor/midwife | 12 (12.5) |
| Comfortable | 11 (11.5) |
| Medical reason (abnormality) | 10 (10.4) |
| Modern services | 7 (7.3) |
| Few choices | 5 (5.2) |
| Cheap provider | 4 (4.2) |
| Family reason | 3 (3.1) |
| Other** | 8 (8.3) |
#multiple answers allowed
*e.g. afraid of caesarean section procedure
**includes perceived more timely or better care, better land road to reach the provider, and provider already designated by the referral system.
Care-seeking pathway by health insurance status and time of death
Table 2 does not show a distinct care-seeking pattern across insurance groups. Although the proportion of those who sought care was lowest among the uninsured group (91.7%), the difference with the insured group (94.5%) was negligible. Also, among the uninsured group who were referred, all complied with the referral. However, the data show differences in the care-seeking pattern by pregnancy status at time of death. Women who died more than 24 hours postpartum were most likely to seek any care from an informal provider (41.0%, OR 7.4, 95% CI 1.9, 28.5, p = 0.049), followed by women who died during pregnancy (29.2%, OR 4.4, 95% CI 1.0, 19.2, p = 0.003), compared to those who died during delivery or within 24 hours postpartum (8.6%) (ORs and 95% CIs are not presented in the table). The proportion of seeking any care from an informal provider is the sum of those who sought both formal and informal care, and those who sought informal care only.
Health insurance
While 76.7% of the deceased had insurance coverage, only 44.8% used insurance at the first point of contact with a formal care provider. Table 4 shows that among deceased who were insured or received government aid and went to more than one provider (n = 55), 54.5% and 92.7% used insurance at the first and last provider, respectively. Women who had insurance were mixed by their wealth quartile, without a distinct pattern toward either the wealthy or the poor group. The proportion of women who died in health facilities was consistently high across all insurance groups. While a higher proportion of women with insurance or government aid died in a hospital than did uninsured women, the difference was not statistically significant (p = 0.110) (S2 Table).
Table 4. Health insurance use among insured or government aid beneficiaries who went to multiple providers (n = 55).
| Use of health insurance | At the last care provider | Total | ||
|---|---|---|---|---|
| Yes | No | n (%) | ||
| At the first care provider | Yes | 29 | 1 | 30 (54.5%) |
| No | 22 | 3 | 25 (45.5%) | |
| Total | 51 (92.7%) | 4 (7.3%) | 55 (100%) | |
Discussion
This study is among the few population-based studies of pregnancy-related mortality in Indonesia that sought to capture data representative at the district level. It is also the first to apply the VASA tool to determine the cause of death and to analyze relevant health system-related and social factors of pregnancy-related death in Indonesia. Using the MADE-IN/MADE-FOR method, this study identified 26% more cases of maternal deaths than the district’s routine health information system, which increases our confidence in the completeness of the data.
Causes of death
The causes of death distribution in our study population is generally consistent with findings from other studies [26]. Our study, however, observed a higher percentage of deaths due to pregnancy-related sepsis (16.5%) compared to the global figure of 10.7% [26]. The literature suggests that the global figure may underestimate the contribution of infections to pregnancy-related deaths, as they do not include deaths due to abortion-related infections or non-obstetric infections that can be aggravated by pregnancy [27]. Furthermore, there is evidence that clinicians fail to recognize the signs and symptoms of possible infections [28, 29]. A cohort study conducted in 713 health facilities in 52 low-, middle- and high-income countries showed that at least one source of infection was identified for 79.7% of women hospitalized, with the most common sources of infections being the genital (endometritis and chorioamnionitis) or urinary tract, skin or soft tissues, respiratory tract, and abortion-related. In the study, infection was the underlying cause in more than half of the in-hospital deaths [27].
A more in-depth analysis of our data showed that a high percentage of the sepsis-related cases occurred among deaths during pregnancy and more than 24 hours postpartum. Our study, however, was not able to identify the common source of infection among the sepsis-related cases to inform recommendations for control measures. Nevertheless, the relatively high proportion of sepsis-related deaths in our study population, despite good access to care, raises concerns about quality of care, early identification, and management of sepsis, particularly during the antenatal and postpartum periods. This deserves further research.
Care-seeking
Nearly all women in our study sought formal care at some time during the fatal illness, and almost all deceased complied with all the referrals made by the formal providers seen. A more in-depth analysis did not show a distinct pattern of the care-seeking pathway by insurance status. The uninsured group sought and received care from formal care providers and complied with referral recommendations to a similar degree as the insured group. Other studies, including those that include Indonesian data, found significant positive effects of health insurance coverage on maternal health care utilization [30, 31]. While several previous safety net programs designed to provide access to care for the poor were in place at the time of these studies, they predate the NHI era and efforts to expand universal access to care, which may explain the different findings.
Given that our study population of pregnancy-related deaths experienced life-threatening complications, the severity of these complications may have led the women/families to seek care regardless of their insurance status, as shown by the absence of differences in care-seeking across the insurance groups. The perceived severity of illness is one factor affecting health care utilization in some of the leading health behavior models [32, 33]. As a study from Bangladesh found, however, perceived severity can be mediated by concerns over medical costs [12]. Our study found that the proportion of deaths in the hospital was higher among the insured group and those who received government aid (78.2% and 79.2%, respectively) compared to the uninsured (62.5%), although not statistically significantly so. This finding may indicate that, despite the growing NHI, to some extent cost may still serve as a barrier especially in access to hospital care, consistent with the Bangladesh study [12].
Care-seeking from informal providers appeared to be influenced by pregnancy status. Women who died more than 24 hours postpartum or during pregnancy were more likely to seek care from an informal care provider at any time during the fatal illness, as opposed to those who died during delivery or within 24 hours postpartum. We hypothesize that the latter group may be perceived as at a greater threat than the other groups, and thus, the majority sought care directly from a formal care provider. Further examination of the causes of death appears to support this hypothesis, as about 78% of deaths during delivery or within the first 24 hours postpartum were attributable to obstetric hemorrhage. The bleeding and the fact that the women were undergoing or had just completed delivery may have triggered families to seek formal care. This premise is corroborated by a qualitative study in Jayawijaya District of Indonesia that found bleeding as a commonly recognized danger sign if present during pre-labor and that rapid decision-making usually occurred when visible symptoms of excessive bleeding began to appear [8]. PIH and pregnancy-related sepsis, which were associated with higher percentages of deaths during pregnancy and after 24 hours postpartum, may not be recognized as posing as big of a threat as bleeding. Also, once a woman has completed labour and delivery, attention may focus more on the newborn and she or her family may not consider that some complications can be life-threatening for the woman [34]. This lack of perceived urgency during many postpartum complications may have also contributed to the increased proportion of deaths during the postpartum period [34, 35]. If this is true, our findings have strong policy implications to increase the quality of postnatal care, one aspect of which would be to improve the identification and management of postnatal complications.
Other factors related to care-seeking
Consistent with literature from developing countries, this study suggests the lack of autonomy among women in deciding to seek care, as less than 10% of the deceased participated in the decision-making during final illness. This finding highlights the need to empower women to enhance their decision-making authority, while at the same time educating women and their partners and families about birth preparedness and complication readiness. Our study found that the majority of the deaths occurred in one ethnic group, the Madura. Although certain cultural practices related to ethnicity are closely associated with maternal mortality [36], we cannot determine the effect of ethnicity in our study population. Given the fact that this ethnic group mostly resides in hard-to-reach areas, geographic challenges may complicate their care-seeking, and eventually have led to poorer outcomes.
Although our study was restricted to deaths, the fact that the majority of the women went to formal care and a relatively small proportion of respondents reported constraints when seeking care for the deceased should lead us to acknowledge at least the success of the health system in Indonesia in alleviating barriers to health care access.
Health insurance
Improvement of the health insurance scheme in Indonesia has increased access to maternal health care, predominantly among the poor and those living in less-developed areas [37]. A shift of pregnancy-related deaths from home to health facilities was evident in our previous study comparing data over a 10-year period [35]. In the current study, most deliveries and deaths also occurred in health facilities. Cost was not mentioned as a significant constraint for care-seeking, contrary to prior VASA studies of pregnancy-related deaths [38]. However, our current findings concerning both the coverage and utilization of insurance by women dying from pregnancy-related causes in this district paint a complex picture. We found, for example, no clear pattern of insurance scheme participation associated with wealth quartiles; low usage of insurance at the first formal provider consulted; and that higher use of insurance when sought care at the last providers than at the first (when multiple providers were involved).
The low usage of insurance at the first formal provider may be explained by several factors including the possibility that the preferred provider may have been a non-NHI designated provider (common among private providers), or some participants may have found that the tiered referral system of the NHI was too complicated to navigate [39–41]. Under the NHI, referral in Indonesia applies a tiered system, in which the primary care provider is designated as the entry point for care and referral to specialized care if the primary care provider is unable to handle the case, except in an emergency [13], when patients can directly seek care from referral health facilities [15]. Another possible explanation is that when they reached the last care provider many women may have required more intensive care or longer hospitalization due to the illness progression. This may lead to catastrophic expenditure, and thus, to higher use of insurance or government aid.
Study limitations
The major limitation of this study is that it only explored the experiences of women who died; there was no control group. Interpretation and generalization of results need to be made with caution. Determinants of care-seeking and maternal deaths cannot be established from the data and the findings cannot be generalized to the general population of women with obstetric complications. The retrospective nature of the data being gathered in this study may introduce recall bias. To minimize the bias, we limited our recall period to two years. However, since pregnancy-related death is a tragic event, it is more likely that family members would remember most of the details surrounding the deaths. Thus, we believe that recall bias does not affect the results and conclusions of this study. This study used data reported from interviews with family members of the deceased, and thus, information on the signs and symptoms were gathered according to the family’s perception, which may not be as accurate as the health providers’ evaluation. However, in general the causes of death distribution in this study is consistent with findings from others, and the relationship of the causes to the time of death is plausible. Also, this study was not designed to assess the quality of care at health facilities, and thus, we cannot draw conclusions about delays in receiving quality care.
This study provides a more comprehensive description of pregnancy-related deaths at sub-national level and adds to the current knowledge, particularly in the context of a high rate of facility-based deliveries and UHC. However, there are clearly several important areas that require better understanding to inform effective maternal mortality reduction strategies, which this study was unable to address. Quality of care and how health financing is functioning to improve health are clearly among the areas that call out for additional research. Our study indicates that access to care may no longer pose a major barrier, largely due to the increasing coverage of NHI. However, concerns over the quality of care remain, which NHI could not directly overcome. Implementing strategic health purchasing is recommended to link NHI with the quality of the provided service. Ensuring quality of care would ideally also require data on whether complications are managed in a certified Basic Emergency Obstetric and Neonatal Care (BEmONC) or CEmONC facility, and whether the facility is functioning properly. This information is currently lacking.
Conclusions
The fact that women sought care and reached health facilities regardless of their insurance status provides an opportunity to prevent deaths by ensuring that all women receive timely and quality care. Timely care-seeking requires increased awareness of birth preparedness and complication readiness among women and their partners and families. This can be achieved by implementing health promotion strategies to encourage formal care-seeking, especially for complications during pregnancy and beyond the immediate postpartum period, which may be perceived as less severe than complications during delivery and within 24 hours postpartum. From a health financing perspective, the lower usage of insurance at the first formal provider, compared to the last provider seen, requires better understanding of barriers to using the insurance scheme. This information is critical to ensure timely care-seeking, and eventually, to leverage the effect of the nationally rolled-out health insurance in preventing maternal mortality and morbidity. To ensure quality care, the increasing demand due to the improved health financing should be met with balanced readiness of both primary care and hospitals, including the availability of competent human resources, essential drugs and properly-equipped facilities, supported by an effective referral system.
Supporting information
*Other causes: abortion, accidental exposure to smoke fire & flames, acute cardiac disease, acute respiratory infection including pneumonia, anemia of pregnancy, breast neoplasm, diarrheal diseases, digestive neoplasm, liver cirrhosis, other & unspecified non-communicable disease, other & unspecified maternal cause of death, road traffic accident ** Fisher’s exact test.
(DOCX)
* Fisher’s exact test.
(DOCX)
Acknowledgments
The authors would like to acknowledge the support from: the governments and health offices of East Java Province and Jember District; puskesmas (community health centers), heads of sub-districts, heads of villages, and all respondents in the study areas. We would like to thank our colleagues from the Ministry of Health who provided substantial support especially in the initial phase of the study. We also would like to thank all the members of the EMNC study team, especially Ms. Nancy Kosasih, Ms. Yenny Fitrianingsih, the data collectors, and data entry team too numerous to mention all by name here; USAID Jalin project staff and the Center for Family Welfare at the University of Indonesia (CFW UI) management team who were instrumental in the implementation of the study. We thank Dr. Sigit Sulistyo of USAID for providing support to the conduct of the study. We would like to also thank Dr. Luna M Mehrain from USAID Jalin Project for providing support and input to the manuscript, as well as Mr. Omair Azam and Mr. Ali Zazri from Vital Strategies for their support in managing the implementation of the study. Last, we would like to pay our gratitude and our respect to the late Dr. Massee Bateman of USAID who has initiated this study and value its purpose.
Data Availability
The underlying data can be accessed from USAID Development Data Library website through 521-1 Jalin Every Mother and Newborn Counts (EMNC) Study 2019; access to this data may be requested through https://data.usaid.gov/access-request.
Funding Statement
This study is made possible by the support of the American people through the United States Agency for International Development (USAID) under the terms of the Contract Number: AID-497-C-17-00001. Information about the funder can be accessed at https://www.usaid.gov. The contents of this article are the sole responsibility of the authors and do not necessarily reflect the views of USAID or the United States Government. The funder had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.World development indicators, The World Bank [Internet]. The World Bank. 2019 [cited 2020 April 1]. Available from: https://datacatalog.worldbank.org/dataset/population-ranking.
- 2.Statistics Indonesia. Population of Indonesia: Result of the 2015 Intercensal Population Survey [Internet]. Jakarta: Statistics Indonesia; 2015. [cited 2020 May 5]. Available from: https://www.bps.go.id/publication/2015/11/30/41ccbadf0b914534f5c08a62/penduduk-indonesia-hasil-supas-2015.html. [Google Scholar]
- 3.World Health Organization. Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division: executive summary [Internet]. World Health Organization; 2019. [cited 2020 May 4]. Available from: https://apps.who.int/iris/bitstream/handle/10665/327596/WHO-RHR-19.23-eng.pdf?sequence=13&isAllowed=y. [Google Scholar]
- 4.United Nations. Sustainable Development Goal 3. Targets and indicators [cited 2020 June 5]. Available from: https://sdgs.un.org/goals/goal3.
- 5.Statistics Indonesia, Macro International. Indonesia Demographic and Health Survey 2007 [Internet]. Calverton, Maryland: BPS and Macro International; 2008. [cited 2021 April 21]. Available from: https://dhsprogram.com/pubs/pdf/FR218/FR218[27August2010].pdf. [Google Scholar]
- 6.National Population and Family Planning Board, Statistics Indonesia, Ministry of Health, ICF. Indonesia Demographic and Health Survey 2017 [Internet]. Jakarta, Indonesia: BKKBN, BPS, Kemenkes, and ICF; 2018. [cited 2021 April 21]. Available from: https://dhsprogram.com/pubs/pdf/FR342/FR342.pdf. [Google Scholar]
- 7.Probandari A, Arcita A, Kothijah K, Pamungkasari EP. Barriers to utilization of postnatal care at village level in Klaten District, Central Java Province, Indonesia. BMC Health Serv Res. 2017;17(1):541. doi: 10.1186/s12913-017-2490-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rosales A, Sulistyo S, Miko O, Hairani LK, Ilyana M, Thomas J, et al. Recognition of and care-seeking for maternal and newborn complications in Jayawijaya District, Papua Province, Indonesia: a qualitative study. J Health Popul Nutr. 2017;36(Suppl 1):44. doi: 10.1186/s41043-017-0122-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sikder SS, Labrique AB, Craig IM, Wakil MA, Shamim AA, Ali H, et al. Patterns and determinants of care seeking for obstetric complications in rural northwest Bangladesh: analysis from a prospective cohort study. BMC Health Serv Res. 2015;15(1):166. doi: 10.1186/s12913-015-0832-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khanam R, Creanga AA, Koffi AK, Mitra DK, Mahmud A, Begum N, et al. Patterns and determinants of care-seeking for antepartum and intrapartum complications in rural Bangladesh: results from a cohort study. PLoS One. 2016;11(12):e0167814. doi: 10.1371/journal.pone.0167814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kaur M, Gupta M, Pandara Purayil V, Rana M, Chakrapani V. Contribution of social factors to maternal deaths in urban India: use of care pathway and delay models. PLoS One. 2018;13(10):1–18. doi: 10.1371/journal.pone.0203209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koenig MA, Jamil K, Streatfield PK, Saha T, Al-Sabir A, El Arifeen S, et al. Maternal health and care-seeking behavior in Bangladesh: findings from a national survey. Int Fam Plan Perspect. 2007;33(02):075–82. doi: 10.1363/3307507 [DOI] [PubMed] [Google Scholar]
- 13.Agustina R, Dartanto T, Sitompul R, Susiloretni KA, Suparmi, Achadi EL, et al. Universal health coverage in Indonesia: concept, progress, and challenges. The Lancet. 2019;393(10166):75–102. doi: 10.1016/S0140-6736(18)31647-7. [DOI] [PubMed] [Google Scholar]
- 14.Ministry of Health Republic of Indonesia. Indonesia Health Profile 2018 [Internet]. Jakarta: Ministry of Health; 2019. [cited 2020 June 5]. Available from: https://pusdatin.kemkes.go.id/resources/download/pusdatin/profil-kesehatan-indonesia/PROFIL_KESEHATAN_2018_1.pdf. [Google Scholar]
- 15.Presidential of Republic of Indonesia Decree No. 82 of 2018 concerning health insurance, Cabinet Secretary of Republic of Indonesia (2018).
- 16.Teplitskaya L, Dutta A. Has Indonesia’s national health insurance scheme improved access to maternal and newborn health services?. 2018. [cited 2020 May 6]. Available from: http://www.healthpolicyplus.com/ns/pubs/8226-9416_HPPlusIndonesiaJKNAccesstoMNHservices.pdf. [Google Scholar]
- 17.Achadi EL, Achadi A, Pambudi E, Marzoeki P. Study on the Implementation of Jampersal Policy in Indonesia. Health, nutrition, and population (HNP) discussion paper [Internet]. Washington, DC: The World Bank,; 2014. Available from: doi: 10.1016/S0140-6736(14)60919-3 [DOI] [Google Scholar]
- 18.DAI. Indonesia—Jalin. Our work [cited 2020. August 30]. Available from: https://www.dai.com/our-work/projects/indonesia-jalin. [Google Scholar]
- 19.University of Aberdeen. Maternal Death from Informants and Maternal Death Follow-on review. Immpact Toolkit, Module 4, Tool 9, v2.1 [Internet]. Immpact: University of Aberdeen; 2007 [cited 2020 May 7]. Available from: https://assets.publishing.service.gov.uk.glasswall-icap.com/media/57a08bd6e5274a31e0000de4/mimf2.pdf.
- 20.Kalter HD, Salgado R, Babille M, Koffi AK, Black RE. Social autopsy for maternal and child deaths: a comprehensive literature review to examine the concept and the development of the method. Population Health Metrics. 2011;9(1):45. doi: 10.1186/1478-7954-9-45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Statistics of Jember Regency. Jember Regency in figures 2017 [Internet]. Jember: Statistics of Jember Regency; 2018 [cited 2020 April 21]. Available from: https://jemberkab.bps.go.id/publication/2017/08/20/1fa125a3b5ed88703dc88f1a/kabupaten-jember-dalam-angka-2017.html.
- 22.Jember District Health Office. Health Profile of Jember District 2018. Jember: Jember District Health Office; 2019. [Google Scholar]
- 23.Center for Family Welfare FPH UI, Vital Strategies. Every Mother and Newborn Counts study report [Internet]. Center for Family Welfare, Universitas Indonesia & Vital Strategies; 2020 [cited 2020 April 30]. Available from: https://pdf.usaid.gov/pdf_docs/PA00X87N.pdf
- 24.McCormick TH, Li ZR, Calvert C, Crampin AC, Kahn K, Clark SJ. Probabilistic cause-of-death assignment using verbal autopsies. J Am Stat Assoc. 2016;111(515):1036–49. doi: 10.1080/01621459.2016.1152191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Waldman R. Overcoming remaining barriers: The pathway to survival. [Internet]. Arlington, VA: BASICS; 1996. [cited 2020 August 26]. Available from: https://pdf.usaid.gov/pdf_docs/PNABZ644.pdf. [Google Scholar]
- 26.Say L, Chou D, Gemmill A, Tunçalp Ö, Moller A-B, Daniels J, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014;2(6):e323–e33. doi: 10.1016/S2214-109X(14)70227-X [DOI] [PubMed] [Google Scholar]
- 27.WHO Global Maternal Sepsis Study (GLOSS) Research Group. Frequency and management of maternal infection in health facilities in 52 countries (GLOSS): a 1-week inception cohort study. Lancet Glob Health. 2020;8(5):e661–e71. doi: 10.1016/S2214-109X(20)30109-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Seacrist MJ, Morton CH, VanOtterloo LR, Main EK. Quality improvement opportunities identified through case review of pregnancy-related deaths from sepsis. J Obstet Gynecol Neonatal Nurs. 2019;48(3):311–20. doi: 10.1016/j.jogn.2019.02.007 [DOI] [PubMed] [Google Scholar]
- 29.Bonet M, Souza JP, Abalos E, Fawole B, Knight M, Kouanda S, et al. The global maternal sepsis study and awareness campaign (GLOSS): study protocol. Reproductive Health. 2018;15(1):16. doi: 10.1186/s12978-017-0437-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nasution SK, Mahendradhata Y, Trisnantoro L. Can a national health insurance policy increase equity in the utilization of skilled birth attendants in Indonesia? A secondary analysis of the 2012 to 2016 national socio-economic survey of Indonesia. Asia Pac J Public Health. 2020;32(1):19–26. doi: 10.1177/1010539519892394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang W, Temsah G, Mallick L. The impact of health insurance on maternal health care utilization: evidence from Ghana, Indonesia and Rwanda. Health Policy Plan. 2016;32(3):366–75. doi: 10.1093/heapol/czw135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10. [PubMed] [Google Scholar]
- 33.Ogden J. Health psychology: A textbook. 5th ed: Open University Press McGraw-Hill Education; 2012. [Google Scholar]
- 34.Thapa S. Risk perception of woman on pregnancy, childbirth and the postpartum phase and the association to the first delay: a case of rural Nepal. M.Sc. Thesis, the Wageningen University; 2014. Available from: https://edepot.wur.nl/400696
- 35.Center for Family Welfare. Summary tables Banten 2 Study report [Internet]. Depok: Center for Family Welfare, Universitas Indonesia; 2017 [cited 2020 August 26]. Available from: https://pdf.usaid.gov/pdf_docs/PA00TQB9.pdf.
- 36.Evans EC. A review of cultural influence on maternal mortality in the developing world. Midwifery. 2013;29(5):490–96. doi: 10.1016/j.midw.2012.04.002 [DOI] [PubMed] [Google Scholar]
- 37.Anindya K, Lee JT, McPake B, Wilopo SA, Millett C, Carvalho N. Impact of Indonesia’s national health insurance scheme on inequality in access to maternal health services: A propensity score matched analysis. J of Glob Health. 2020;10(1):010429. doi: 10.7189/jogh.10.010429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kalter HD, Mohan P, Mishra A, Gaonkar N, Biswas AB, Balakrishnan S, et al. Maternal death inquiry and response in India—the impact of contextual factors on defining an optimal model to help meet critical maternal health policy objectives. Health Res Policy Syst. 2011;9(1):41. doi: 10.1186/1478-4505-9-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cain JS, Tandon A, Yap WA, Pambudi ES, Marzoeki P. Revealing the missing link: private sector supply-side readiness for primary maternal health services in Indonesia—maternal health report. Working Paper. Washington, D.C: World Bank Group, 2017. 2017/06/21. Report No.: 116608. [Google Scholar]
- 40.Health Policy Plus, Tim Nasional Penanggulangan Kemiskinan RI. Memperluas akses pelayanan kesehatan melalui sektor swasta: Jaminan kesehatan nasional dan sektor swasta. 2018 [cited 2020 June 5]. Indonesian. Available from: http://www.healthpolicyplus.com/ns/pubs/8224-9415_IndonesiaJKNPrivateSectorBriefBahasa.pdf.
- 41.Nurfadhilah, Gustia H, Susilahati, Susilo D. The Impact of Implementation of the National Health Insurance Program to Decrease Maternal Mortality in Bogor. The 2nd International Multidisciplinary Conference; 15 November 2016; Jakarta. 2016.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
*Other causes: abortion, accidental exposure to smoke fire & flames, acute cardiac disease, acute respiratory infection including pneumonia, anemia of pregnancy, breast neoplasm, diarrheal diseases, digestive neoplasm, liver cirrhosis, other & unspecified non-communicable disease, other & unspecified maternal cause of death, road traffic accident ** Fisher’s exact test.
(DOCX)
* Fisher’s exact test.
(DOCX)
Data Availability Statement
The underlying data can be accessed from USAID Development Data Library website through 521-1 Jalin Every Mother and Newborn Counts (EMNC) Study 2019; access to this data may be requested through https://data.usaid.gov/access-request.