The world is still grappling with the devastating effects of COVID-19 more than 2 years into the pandemic. Countries with high COVID-19 vaccination rates are transitioning to the new normal of living with SARS-CoV-2, but low-income and middle-income countries (LMICs) are struggling to vaccinate their populations while concurrently fighting other communicable diseases, key among them tuberculosis. The burden of tuberculosis, the leading cause of death from an infectious disease before COVID-19 emerged, has been deeply affected by the pandemic.1, 2 In the first of a Series of three papers published in The Lancet Respiratory Medicine and eBioMedicine, Keertan Dheda and colleagues3 discuss the effects of COVID-19 on efforts to end tuberculosis and the need for wide-ranging interventions to restore tuberculosis control, including the need to implement and enhance tuberculosis diagnostic tests to reduce under-diagnosis. In the second paper, Ruvandhi Nathavitharana and colleagues4 highlight progress in the development of non-sputum-based diagnostic tests with potential for decentralised deployment. Finally, Hanif Esmail and colleagues5 discuss optimal treatment regimens across the full spectrum of tuberculosis infection and tuberculosis disease, previously known as latent tuberculosis and active tuberculosis, respectively.1 Although these articles apply mainly to pulmonary tuberculosis, advances in the diagnosis and treatment of extrapulmonary tuberculosis will have to be made concurrently in addressing the substantial burden of disease. Importantly, the various sequelae after tuberculosis need to be understood and optimally managed.6 Finally, options for the prevention of tuberculosis in the form of robust vaccines need to be developed.7 Translational research will underpin progress in preventing and managing the entire spectrum of tuberculosis, and a pressing need exists for investment and support to strengthen research capacity.
To improve the diagnosis of tuberculosis, new diagnostic tools, especially non-sputum-based tests, and enhancement of existing tuberculosis diagnostic tests will be crucial. Nathavitharana and colleagues4 highlight the need to develop a sensitive and specific, rapid, non-sputum-based tuberculosis test by harnessing existing resources invested in COVID-19 detection. By use of easily accessible clinical samples, such as urine or oral swabs for diagnosis and implementing point-of-care tests, tuberculosis diagnosis could be enhanced in LMICs, where the majority of the world's tuberculosis burden is found.1 Such diagnostic tests need to be broadly applicable to all population types, including immunocompromised individuals, who tend to have atypical presentations and are often sputum-smear negative, which compromises the yield of the more rapid nucleic-acid tests.8 Additionally, the performance of existing tuberculosis nucleic-acid tests is variable across specimen types, which is less than ideal and underscores the need for better diagnostic tests. The gold-standard tuberculosis cultures and drug-susceptibility tests remain unavailable in most LMICs, but the advent of whole-genome sequencing shortens the time to determine anti-tuberculosis drug susceptibility for more effective tuberculosis treatment.9 Such technology, if made available across resource settings, would help to stem transmission of both drug-susceptible and drug-resistant Mycobacterium tuberculosis because it allows prompt initiation of effective anti-tubercular treatment.
To optimally manage tuberculosis infection and disease, new approaches to diagnosis will need to go hand in hand with improved tuberculosis prevention and treatment, for which drug discovery together with repurposing of existing drugs needs to be undertaken. Esmail and colleagues5 propose an approach in which tuberculosis treatment and management are tailored across the tuberculosis spectrum, instead of being provided within the binary framework of tuberculosis infection and tuberculosis disease. However, extensive work is needed before this concept can be realised in clinical practice. For example, the implementation of this concept requires the development of a host-based or mycobacteria-based biomarker that indicates eradication of the pathogen, applicable to both tuberculosis infection and disease states of pulmonary and extrapulmonary tuberculosis, regardless of the level of immunity. Once validated in several independent cohorts, this biomarker would be useful in guiding the duration of treatment for infection or disease. Drug discovery and repurposing of drugs takes an excruciatingly long time in the tuberculosis field, but scientific and political will can remove barriers and expedite the process, similar to progress observed in COVID-19, with the necessary funding.10
Research on extrapulmonary tuberculosis has been modest compared with that for pulmonary tuberculosis, but remains just as important, and research efforts are needed to better understand and manage extrapulmonary tuberculosis. Patients with Pott's disease (spinal tuberculosis) and central nervous system tuberculosis often have poor neurological and mortality outcomes despite effective tuberculosis treatment. The optimal treatment duration of each condition remains unclear for drug-susceptible tuberculosis, even less so for drug-resistant tuberculosis. Animal models that recapitulate features of human extrapulmonary disease states might hold promise for understanding mechanisms and allow testing of new therapeutics to improve both mortality and morbidity outcomes,11 before studies in humans in phase 2 and 3 clinical trials.
The long-term sequelae of tuberculosis should not be forgotten. It is well recognised that lung function and quality-of-life decrease after pulmonary tuberculosis disease,12 but the extent of the global burden of lung disease after tuberculosis infection is poorly defined and likely to be under-reported. Mechanisms that underlie tuberculosis tissue destruction and fibrosis are being established. Phase 2 clinical trials repurposing existing drugs, such as doxycycline and everolimus, to decrease tissue destruction hold promise in improving lung function and ameliorating sequelae from post-tuberculosis lung disease,13, 14 but their efficacy would need to be demonstrated in larger cohorts before being implemented in practice. These measures, together with measures such as pulmonary rehabilitation, need to be adopted according to an agreed clinical standard to reduce the global burden of tuberculosis sequelae.6
Altogether, tuberculosis translational research remains key to advancing prevention and management across the entire spectrum of tuberculosis, which is still a leading killer globally. Despite the catastrophic setbacks from COVID-19, researchers need to continue to push ahead to reach the ultimate goal of ending tuberculosis. As has been seen for COVID-19, a whole-of-government approach for tuberculosis is needed for the development of effective diagnostic and treatment approaches to stem transmission and save lives.
For the Tuberculosis in the time of COVID-19 Series see www.thelancet.com/series/tuberculosis-2022
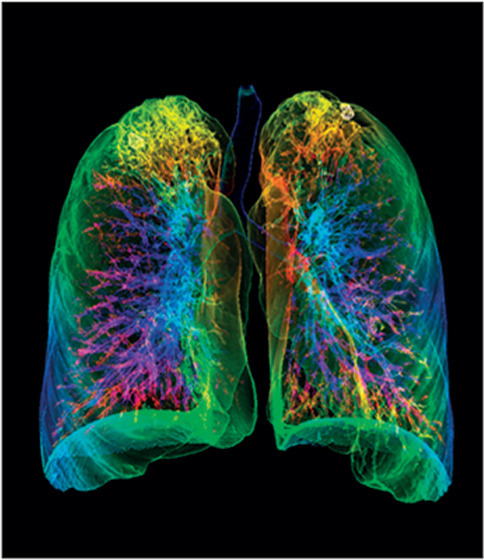
© 2022 K H Fung/Science Photo Library
CWMO has received speaking fees from Qiagen, outside this work. The other authors declare no competing interests.
References
- 1.WHO . World Health Organization; Geneva: 2021. Global tuberculosis report 2021. [Google Scholar]
- 2.Migliori GB, Thong PM, Alffenaar JW, et al. Gauging the impact of the COVID-19 pandemic on tuberculosis services: a global study. Eur Respir J. 2021;58 doi: 10.1183/13993003.01786-2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dheda K, Perumal T, Moultrie H, et al. The intersecting pandemics of tuberculosis and COVID-19: population-level and patient-level impact, clinical presentation, and corrective interventions. Lancet Respir Med. 2022 doi: 10.1016/S2213-2600(22)00092-3. published online March 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nathavitharana RR, Garcia-Basteiro AL, Ruhwald M, Cobelens F, Theron G. Reimagining the status quo: how close are we to rapid sputum-free tuberculosis diagnostics for all? EBioMedicine. 2022 doi: 10.1016/j.ebiom.2022.103939. published online March 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Esmail H, Macpherson L, Coussens AK, Houben RMGJ. Mind the gap – managing tuberculosis across the disease spectrum. EBioMedicine. 2022 doi: 10.1016/j.ebiom.2022.103928. published online March 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Migliori GB, Marx FM, Ambrosino N, et al. Clinical standards for the assessment, management and rehabilitation of post-TB lung disease. Int J Tuberc Lung Dis. 2021;25:797–813. doi: 10.5588/ijtld.21.0425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cobelens F, Suri RK, Helinski M, et al. Accelerating research and development of new vaccines against tuberculosis: a global roadmap. Lancet Infect Dis. 2022 doi: 10.1016/S1473-3099(21)00810-0. published online Feb 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Teng VYM, Chua YT, Lai EEN, et al. Lack of latent tuberculosis (TB) screening and delay in anti-retroviral therapy initiation in HIV-TB co-infection: an 11-year study in an intermediate TB-burden country. Int J Infect Dis. 2021;113:178–183. doi: 10.1016/j.ijid.2021.09.048. [DOI] [PubMed] [Google Scholar]
- 9.The CRyPTIC Consortium and the 100,000 Genomes Project Prediction of susceptibility to first-line tuberculosis drugs by DNA Sequencing. N Engl J Med. 2018;379:1403–1415. doi: 10.1056/NEJMoa1800474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chaisson RE, Frick M, Nahid P. The scientific response to TB — the other deadly global health emergency. Int J Tuberc Lung Dis. 2022;26:186–189. doi: 10.5588/ijtld.21.0734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Poh XY, Hong JM, Bai C, et al. Nos2−/− mice infected with M. tuberculosis develop neurobehavioral changes and immunopathology mimicking human central nervous system tuberculosis. J Neuroinflammation. 2022;19:21. doi: 10.1186/s12974-022-02387-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Long R, Maycher B, Dhar A, Manfreda J, Hershfield E, Anthonisen N. Pulmonary tuberculosis treated with directly observed therapy: serial changes in lung structure and function. Chest. 1998;113:933–943. doi: 10.1378/chest.113.4.933. [DOI] [PubMed] [Google Scholar]
- 13.Miow QH, Vallejo AF, Wang Y, et al. Doxycycline host-directed therapy in human pulmonary tuberculosis. J Clin Invest. 2021;131 doi: 10.1172/JCI141895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wallis RS, Ginindza S, Beattie T, et al. Adjunctive host-directed therapies for pulmonary tuberculosis: a prospective, open-label, phase 2, randomised controlled trial. Lancet Respir Med. 2021;9:897–908. doi: 10.1016/S2213-2600(20)30448-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


